Pelvic pain is a common diagnosis that we see as pelvic floor therapists. Pelvic pain is pain located in the lower abdomen, but above pubic symphysis, and is associated with various causes; myofascial pain, neuropathies, endometriosis, painful bladder, and irritable bowel syndromes. A common symptom of pelvic pain is deep dyspareunia or pain with deep vaginal penetration. Vulvar pain is different, as it is below pubic symphysis, and has several sub-classifications. These sub-classifications can often be confusing. The National Vulvodynia Association has a free online education that explains the different sub-types very succinctly. This article focuses on provoked vestibulodynia, which is the most commonly studied.
 PVD or Provoked Vestibulodynia often has superficial dyspareunia which can negatively affect sexual functioning, which can lead to changes in psychological function and quality of life. Women with PVD often complain of greater pain during and after intercourse, pain catastrophization, and allodynia when compared to women with superficial dyspareunia but without PVD. These symptoms indicate central nervous system upregulation or sensitivity. This study sought to investigate the impact of these symptoms.
PVD or Provoked Vestibulodynia often has superficial dyspareunia which can negatively affect sexual functioning, which can lead to changes in psychological function and quality of life. Women with PVD often complain of greater pain during and after intercourse, pain catastrophization, and allodynia when compared to women with superficial dyspareunia but without PVD. These symptoms indicate central nervous system upregulation or sensitivity. This study sought to investigate the impact of these symptoms.
Pelvic pain encompassed a variety of complaints: “dysmenorrhea, deep dyspareunia, dyschezia, chronic pelvic pain, back pain, or diagnosed or suspected endometriosis”. Participants were excluded if postmenopausal or if self reported never sexually active.
One hundred twenty nine participants were divided into those with pelvic pain and PVD (43), and those with pelvic pain alone (87). For this study PVD was diagnosed as superficial dyspareunia (>4/10) and positive Q-tip test with a fixed pressure of 30g. Those with did not meet this criteria were considered to have pelvic pain alone.
The two groups were compared for superficial and deep sexual discomfort severity, sexual quality of life; fear avoidance, feelings of guilt, frustration, etc, physical examination of trigger points along abdominal wall (positive Carnett test), and numeric pain scale of various painful lumbo-pelvic regions.
Of the 129 participants notable findings in both the two groups include 31% had confirmed endometriosis, 40% suspected of endometriosis, and in the remaining 18% had no confirmed or suspected endometriosis. The authors found that the pelvic pain + PVD group had significantly more superficial dyspareunia (p=<.001) and deep dyspareunia (p=.001) which was rated >7/10 for both. This group was also had greater (3x more likely to have) depression symptoms, greater anxiety, and catastrophizing, and was more likely to have painful bladder syndrome than the pelvic pain alone group. There were no differences between the two groups for irritable bowel syndrome or abdominal wall tenderness.
This research is consistent with other research findings. The authors explore various causes of the findings including; cross- sensitization - where there may be cross talk of nerve signals from viscera to viscera and viscera to muscular structures that converge in the spinal cord. The authors note that the poor relationship between PVD and irritable bowel and PVD and abdominal wall tenderness limit that theory. They explore the psychological symptoms may be a consequence of pelvic pain or it may be that having anxiety/depression may make women more sensitive to developing pelvic pain and PVD. This sounds like a little chicken or egg theory. The authors suggest that those with PVD and pelvic pain may benefit from a more intensive multi-disciplinary approach including; “medical, surgical, psychological, or physical therapy approaches”.
Bao, C., Noga, H, Allaire, C. et al. “Provoked Vestibulodynia in Women with Pelvic Pain” Sex Med 2019; 1-8
The following is a guest submission from Alysson Striner, PT, DPT, PRPC. Dr. Striner became a Certified Pelvic Rehabilitation Practitioner (PRPC) in May of 2018. She specializes in pelvic rehabilitation, general outpatient orthopedics, and aquatics. She sees patients at Carondelet St Joesph’s Hospital in the Speciality Rehab Clinic located in Tucson, Arizona.
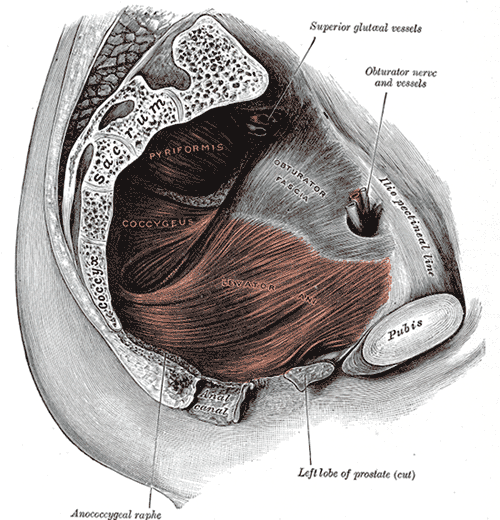
Myofascial pain from levator ani (LA) and obturator internus (OI) and connective tissues are a frequent driver of pelvic pain. As pelvic therapists, it can often be challenging to decipher whether pain is related to muscular and/or fascial restrictions. A quick review from Pelvic Floor Level 2B; overactive muscles can become functionally short (actively held in a shortened position). These pelvic floor muscles do not fully relax or contract. An analogy for this is when one lifts a grocery bag that is too heavy. One cannot lift the bag all the way or extend the arm all the way down, instead the person often uses other muscles to elevate or lower the bag. Over time both the muscle and fascial restrictions can occur when the muscle becomes structurally short (like a contracture). Structurally short muscles will appear flat or quiet on surface electromyography (SEMG). An analogy for this is when you keep your arm bent for too long, it becomes much harder to straighten out again. Signs and symptoms for muscle and fascial pain are pain to palpation, trigger points, and local or referred pain, a positive Q tip test to the lower quadrants, and common symptoms such as urinary frequency, urgency, pain, and/or dyspareunia.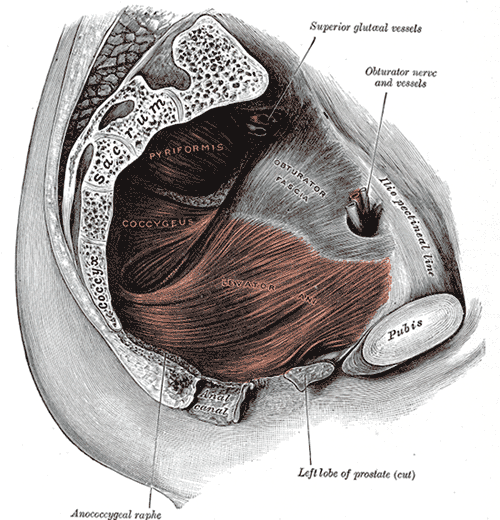
For years in the pelvic floor industry there has been notable focus on vocabulary. Encouraging all providers (researchers, MDs, and PTs) to use the same words to describe pelvic floor dysfunction allowing more efficient communication. Now that we are (hopefully) using the same words, the focus is shifting to physical assessment of pelvic floor and myofascial pain. If patients can experience the same assessment in different settings then they will likely have less fear, and the medical professionals will be able to communicate more easily.
A recent article did a systematic review of physical exam techniques for myofascial pain of pelvic floor musculature. This study completed a systematic review for the examination techniques on women for diagnosis of LA and OI myofascial pain. In the end, 55 studies with 9460 participants; 99.8% were female, that met the inclusion and exclusion criteria were assessed. The authors suggest the following as good foundation to begin; but more studies will be needed to validate and to further investigate associations between chronic pelvic pain and lower urinary tract symptoms with myofascial pain.
The recommended sequence for examining pelvic myofascial pain is:
- Educate patient on examination process. Try to ease any anxiety they may have. Obtain consent for an examination
- Ask the patient to sit in lithotomy position
- Insert a single, gloved, lubricated index finger into the vaginal introitus
- Orient to pelvic floor muscles using clock face orientation with pubic symphysis at 12 o'clock and anus at 6 o'clock
- Palpate superficial and then deep pelvic floor muscles
- Palpate the obturator internus
- Palpate each specific pelvic floor muscle and obturator internus; consider pressure algometer to standardize amount of pressure
Authors recommend bilateral palpation and documentation of trigger point location and severity with VAS. They recommend visual inspection and observation of functional movement of pelvic floor muscles.
The good news is that this is exactly how pelvic therapists are taught to assess the pelvic floor in Pelvic Floor Level 1. This is reviewed in Pelvic Floor Level 2B and changed slightly for Pelvic Floor Level 2A when the pelvic floor muscles are assessed rectally. Ramona Horton also teaches a series on fascial palpation, beginning with Mobilization of the Myofascial Layer: Pelvis and Lower Extremity. I agree that palpation should be completed bilaterally by switching hands to make assessment easier for the practitioner who may be on the side of the patient/client depending on the set up. This is an important conversation between medical providers to allow for easy communication between disciplines.
Meister, Melanie & Shivakumar, Nishkala & Sutcliffe, Siobhan & Spitznagle, Theresa & L Lowder, Jerry. (2018). Physical examination techniques for the assessment of pelvic floor myofascial pain: a systematic review. American Journal of Obstetrics and Gynecology. 219. 10.1016/j.ajog.2018.06.014