Hi, I’m Deb Gulbranson, co-creator of the course Osteoporosis Management: An Introductory Course for Healthcare Professionals. Along with my partner, Frank Ciuba, we have created a program based on the works of Sara Meeks, whom we taught with for many years.
We know that posture is important, and we may include it in our evaluations, but how do we objectively measure it? How much time do we spend on education, training, exercises, and return demonstration? Chances are, not as much as we should.
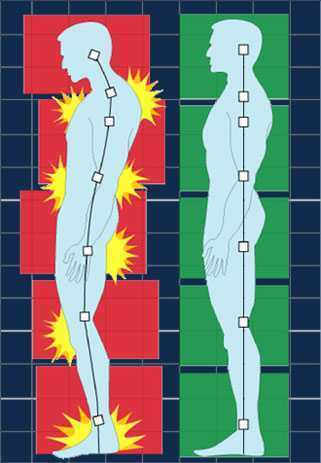
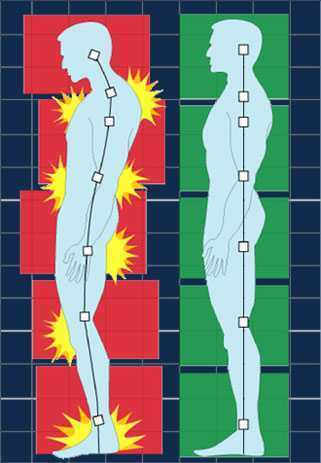
Optimal alignment affects our breathing, balance, efficiency of gait, digestion, AND bone density.
In order to increase bone density, we need to weight bear through the skeleton, not in front of it. Compression fractures occur along the anterior aspect of the vertebral bodies. Strengthening the back extensors has also been shown to increase bone density. Therefore, someone with a hyper-kyphotic posture of the thoracic spine is at risk for fracture due to increased pressure anteriorly and overstretched, weakened musculature posteriorly. Statistics show that 1:2 women and 1:4 men will have a fragility fracture due to low bone mass.
How do we objectively measure and describe a person’s alignment?
 A quick and simple way is using a wall and measuring tape. Have your patient stand with their heels, sacrum, and thoracic apex of the spine against the wall. There are two options to measure using the OWD or the TWD. Occiput to Wall Distance or Tragus to Wall Distance. The Tragus is the small bump of cartilage in front of the ear canal. Both OWD and TWD have a positive relationship with the Cobb angle, and although they’re not as specific, they are both equally effective. It’s a matter of preference. Frank prefers the TWD since it’s easier to see and measure. However, the score does not tell you how far away from the wall the head is. There will always be a positive number based on the size and shape of the head.
A quick and simple way is using a wall and measuring tape. Have your patient stand with their heels, sacrum, and thoracic apex of the spine against the wall. There are two options to measure using the OWD or the TWD. Occiput to Wall Distance or Tragus to Wall Distance. The Tragus is the small bump of cartilage in front of the ear canal. Both OWD and TWD have a positive relationship with the Cobb angle, and although they’re not as specific, they are both equally effective. It’s a matter of preference. Frank prefers the TWD since it’s easier to see and measure. However, the score does not tell you how far away from the wall the head is. There will always be a positive number based on the size and shape of the head.
I prefer the OWD because whatever the measurement is, it tells me how far forward the head is. 0 equals optimal alignment. The downside is that it’s a little harder to pinpoint the most prominent point of the occiput.
In both cases, the measurement gives us a baseline to measure against. These can be used as screens in a health fair, during a PT screen for patients without a diagnosis of low bone density, and certainly as part of a full eval for patients with known osteoporosis, a compression fracture, or even osteopenia.
These measures, taken periodically, can be very motivating for patients. Generally, we see not only a decrease in the hyper-kyphosis distance but also an increase in height.
This is only one of several ways to assess and describe posture and alignment. We hope you’ll consider joining us to learn more about the treatment protocols and exercise programs in our upcoming Osteoporosis Management course on April 26th.
AUTHOR BIO
Deb Gulbrandson, PT, DPT
 Deb Gulbrandson, DPT (she/her) has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb Gulbrandson, DPT (she/her) has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb is a graduate of Indiana University and a former NCAA athlete, where she competed on the IU Gymnastics team. She has always been interested in movement and function and is grateful to combine her skills as a PT and Pilates instructor. She has been certified through Polestar Pilates since 2005, a Certified Osteoporosis Exercise Specialist through the Meeks Method since 2008, and a Certified Exercise Expert for the Aging Adult through the Geriatric Section of the APTA.
As musculoskeletal specialists, we are adept at identifying postural dysfunction. I often explain to patients how their ribcage might shift posteriorly relative to the plumb line and how gravity can amplify forces on specific structures. To help patients understand the difference between their habitual non-optimal posture and a more optimally aligned posture, many occupational and physical therapists use the IPA’s Vertical Compression Test (VCT). This test effectively demonstrates how improved alignment facilitates better weight transfer through the base of support. Sometimes this test reproduces back or pelvic pain which allows the patient to understand how their posture might be a contributing factor to them not feeling their best. In addition to the VCT, I incorporate Mountain Pose as an additional kinesthetic tool for postural retraining.
 Many moons ago, I was working with a lovely client on embodied postural awareness using Mountain Pose. I suggested she could close her eyes if she felt comfortable (some people will feel safer lowering their gaze instead of closing their eyes). Working from the ground up, she realized her weight was predominantly in her heels. When I guided her to shift her weight forward by hinging from the talocrural joint, she experienced an “aha moment,” saying, “It feels like my pelvic floor just sighed.” She hadn’t been aware that her habitual posture involved standing with her weight behind the plumb line, which contributed to overactivity of the posterior pelvic floor. Once she adjusted her base of support from the ground up, she felt a significant release in her habitual tension.
Many moons ago, I was working with a lovely client on embodied postural awareness using Mountain Pose. I suggested she could close her eyes if she felt comfortable (some people will feel safer lowering their gaze instead of closing their eyes). Working from the ground up, she realized her weight was predominantly in her heels. When I guided her to shift her weight forward by hinging from the talocrural joint, she experienced an “aha moment,” saying, “It feels like my pelvic floor just sighed.” She hadn’t been aware that her habitual posture involved standing with her weight behind the plumb line, which contributed to overactivity of the posterior pelvic floor. Once she adjusted her base of support from the ground up, she felt a significant release in her habitual tension.
At our follow-up visit, the client noted an increase in her postural awareness. She was surprised by how frequently she noticed her pelvic floor gripping in a state of overactivity. She also reported enhanced awareness during her standing yoga postures in class. Grounding down through the feet, cued as imagining the soles of the feet getting magnetically drawn into the floor, can be a useful verbal cue to assist with letting go of unnecessary gripping. The experience of achieving embodied optimal alignment has given her greater self-efficacy, and she’s successfully translated this improved postural awareness into her daily life. Self-awareness and empowerment are central goals in my physical therapy practice, and integrating yoga into this process makes my clinical work even more fulfilling.
To learn more, join Dustienne in her remote course Yoga for Pelvic Pain this September 14-15! This course discusses a variety of pelvic conditions including interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia. Dustienne also describes the role of yoga within the medical model, contraindicated postures, and how to incorporate yoga home programs as therapeutic exercise and neuromuscular re-education both between visits and after discharge in this course.
Author Bio:
Dustienne Miller PT, MS, WCS, CYT

Dustienne Miller is the creator of the two-day course Yoga for Pelvic Pain and an instructor for Pelvic Function Level 1. Born out of an interest in creating yoga home programs for her patients, she developed a pelvic health yoga video series called Your Pace Yoga in 2012. She is a contributing author in two books about the integration of pelvic health and yoga, Yoga Mama: The Practitioner’s Guide to Prenatal Yoga (Shambhala Publications, 2016) and Healing in Urology (World Scientific). Prior conference and workshop engagements include APTA's CSM, International Pelvic Pain Society, Woman on Fire, Wound Ostomy and Continence Society, and the American Academy of Physical Medicine and Rehabilitation Annual Assembly.
Her clinical practice, Flourish Physical Therapy, is located in Boston's Back Bay. She is a board-certified women's health clinical specialist recognized by the American Board of Physical Therapy Specialties. Dustienne weaves yoga, mindfulness, and breathwork into her clinical practice, having received her yoga teacher certification through the Kripalu Center for Yoga and Health in 2005.
Dustienne's love of movement carried over into her physical therapy and yoga practice, stemming from her previous career as a professional dancer. She danced professionally in New York City for several years, most notably with the national tour of Fosse. She bridged her dance and physical therapy backgrounds working for Physioarts, who contracted her to work backstage at various Broadway shows and for Radio City Christmas Spectacular. She is an assistant professor of musical theater and jazz dance at the Boston Conservatory at Berklee.
Dustienne passionately believes in the integration of physical therapy and yoga within a holistic model of care. Her course aims to provide therapists and patients with an additional resource centered on supporting the nervous system and enhancing patient self-efficacy.
Deb Gulbrandson, PT, DPT is teaming up with Frank J Ciuba DPT, MS to create a new course called Osteoporosis Management: A Comprehensive Approach for Healthcare Professionals! This new course is launching remotely this July 25-26, 2020, and it emphasizes visual imagery cues which leads to enhanced performance for patients. Both course authors are trained by Sara Meeks, and have adapted her method to create this updated, evidence-based course on osteoporosis management.
How many times have you told your patients to stand up straight and stop looking down while walking? How’d that work out? Probably not so good. At best you may have noticed a temporary correction only for the patient to return to the formerly mentioned poor posture. We know that balance is affected by alignment of our trunk and spine. 1 Everyone needs to avoid falls but it’s particularly important with osteoporosis patients due to bone fragility.
 We want our patients not only to move, but to move with optimal alignment. According to Fritz, et al 2 in the vhitepaper: “Walking Speed: The Sixth Vital Sign”, walking is a complex functional activity. Our ability to influence motor control, muscle performance, sensory and perceptual function, endurance and habitual activity level can result in a more efficient and safer gait.
We want our patients not only to move, but to move with optimal alignment. According to Fritz, et al 2 in the vhitepaper: “Walking Speed: The Sixth Vital Sign”, walking is a complex functional activity. Our ability to influence motor control, muscle performance, sensory and perceptual function, endurance and habitual activity level can result in a more efficient and safer gait.
Visual imagery cuing had been popular in the sports world for decades. By changing one or two words, physical performance has been shown to improve. 3 In a study involving standing long jump, Wu et al instructed undergraduate students to either “Jump as far as you can and think about extending your legs” (internal focus) or “Jump as far as you can and think about jumping as close to the green target as possible” (external focus). The external focus group jumped 10% farther. Lohse et al 4 and Zachry et al 5 surmised that an external focus reduces the "noise" in the motor system which affects muscular tension and optimal function.
It Starts with Posture
Before you can expect your patients to walk well, they have to stand well- stability before mobility. Assess their posture from all angles and determine where to start. One visual image may change a host of problems. A common postural fault, “slumping” is seen as forward head, increased thoracic kyphosis accompanied with either lumbar hyper or hypo lordosis. Your goal is to get the optimal alignment image that you have in your mind……. into their body.
Most people think in pictures rather than words. 6 Yet the medical industry uses words to communicate. Often we say, “Don’t slouch. Don’t look down.” Telling your patient what not to do is not helpful. Our brain hears the words, “Slouch or look down.” We don’t discern the negative. If I say to you, “Don’t think of a pink elephant,” what does your mind see? How can you not see a pink elephant?
Below are five common visual cues to improve a patient’s posture in standing and walking. These tend to follow the Pareto Principle. 20% of your cues work 80% of the time.
- “In standing, imagine a bungee cord running from the top of your head to the ceiling. Visualize a mother cat lifting her kitten up by the scruff of the neck.”
- “When breathing, imagine an umbrella inside your ribcage, opening up upon inhale, and closing on exhale. Breathe in all directions including into the back of your lungs as if you were filling up the sails of a sailboat.”
- “When walking, widen your collarbones as if they were arrows, shooting off the tips of your shoulders. Imagine your head is a floating balloon, gliding along above your shoulders.”
- “Pretend you are the King (or Queen) of England as you walk among your subjects. “
- “Slide your shoulder blades down toward your opposite hip pockets.”
Choose a cue and instruct your patient. Observe changes in posture, alignment, efficiency of movement, or length of step during gait. Ask your patient for feedback. “What did you notice?” Certain cues resonate more than others. Give them variety and options. The best cues are the ones they create themselves. When a patient says, “You mean like………..?” you know it’s a great cue for them. They have an intuitive understanding and relate to it which translates into their body. A patient’s response to the bungee cord cue was, “You mean like a Christmas ornament hanging from the tree?” My response? Absolutely!
While some visual cues may seem too flowery or not “medical” enough, the research is solid the impact powerful. Plus your patients love it! Visual cues are sticky. They help remind us when we’re out in the real world. Isn’t that the ultimate goal – helping patients become independent in their pursuit of health and safety?
1. Shiro Imagam, et all. Influence of spinal sagittal alignment, body balance, muscle strength, and physical ability on falling of middle-aged and elderly males. Eur Spine J. 2013 Jun;
2. Fritz S. et al White Paper: “Walking Speed: The Sixth Vital Sign” J Geriatr Phys Ther. 2009
3. Wu, et al Effect of Attentional Focus Strategies on Peak Force and Performance in the Standing Long Jump. Joun of Strength and Conditioning Research 2012
4. Lohse and Sherwood Defining the Focus of Attention: Effects of Attention on Perceived Exertion and Fatigue
5. Zachry, T et al. Increased Movement Accuracy and Reduced EMG Activity as a Result of Adopting an External Focus of Attention. Brain Research Bulletin Oct 2005
6. Dynamic Alignment Through Imagery. Franklin, Eric. Second Edition, 2012
So many physiological changes occur to a woman’s body during pregnancy, it is no wonder that pregnant women have back and lower extremity aches and pains. These women experience hormonal changes, weight gain, reduced abdominal strength, and their center of mass shifts anteriorly. These physiological changes result in altered spinal and pelvic alignment, and increased joint laxity. Also, many women report increases in size of their feet and a tendency to have flatter arches during and after pregnancy. Alignment changes may influence pain. Altered alignment could change the physical stresses placed upon different tissues of the body, which that specific tissue was not adapted to, therefore, causing pain or injury to that tissue.
 A recent study published in 2016, in the Journal of Women’s Health Physical Therapy1, investigated if there may be a relationship between anthropometric changes of the foot that occur with pregnancy, and pregnancy related musculoskeletal pain of the lower extremity. The study included 15 primigravid women and 14 weight matched controls. This study was a repeated-measurements design study, where the investigators measured foot length, foot width, arch height index, arch rigidity index (ARI), arch drop (AD), rear foot angle, and pelvic obliquity during the second and third trimesters and post-partum. The subjects were surveyed on pain in the low back, hips/buttocks, and foot/ankle.
A recent study published in 2016, in the Journal of Women’s Health Physical Therapy1, investigated if there may be a relationship between anthropometric changes of the foot that occur with pregnancy, and pregnancy related musculoskeletal pain of the lower extremity. The study included 15 primigravid women and 14 weight matched controls. This study was a repeated-measurements design study, where the investigators measured foot length, foot width, arch height index, arch rigidity index (ARI), arch drop (AD), rear foot angle, and pelvic obliquity during the second and third trimesters and post-partum. The subjects were surveyed on pain in the low back, hips/buttocks, and foot/ankle.
The author’s findings were that measures of arch flexibility (ARI and AD) correlated with pain at the low back and the foot and ankle. They concluded that medial longitudinal arch flexibility may be related to pain in the low back and foot. The more flexible arches were associated with more pain in the study participants. They reported the participants in their study did not have very high pain levels in general, and recommend further studies to compare pregnant women who experience severe pain with women who do not while comparing their alignment factors. This article is a good reminder for physical therapists to consider the changes that occur to the foot including changes in arch height, arch flexibility, and foot size and how that influences the pelvis and lower extremity for prevention and treatment of musculoskeletal pain during pregnancy.
Educating our pregnant patients on shoe wear seems even more important now. Making recommendations, unique to each individual patient based on their objective data, foot type, and arch flexibility status seems like an appropriate addition to a well-rounded treatment plan. Doesn’t it seem prudent to wear shoes that provide some arch support to hopefully reduce musculoskeletal pain associated with pregnancy changes? I have observed some patients who are pregnant arrive to physical therapy wearing unsupportive flip flops and other poor shoe wear choices. I understand there are barriers for pregnant patients, I remember from when I was pregnant that reaching your feet to put shoes on can be very difficult, and sometimes your feet are swelling so it may be near impossible to physically get shoes on your feet. You might even need a new pair of shoes, as your shoes may no longer fit. However, an article such as this one, seems like something I could easily share with a patient to help persuade them of the importance of good shoe wear or at least proper arch support. Being able to discuss a recent scientific study with a patient can be powerful and motivating to a patient. Additionally, an article such as this reminds a practitioner of specific objective data to monitor such as arch height and flexibility as it changes throughout the patient’s pregnancy. How does the patient’s changing arch height and flexibility influence their specific pelvic, hip, knee, and ankle alignment? How does swelling play a part in the patients’ foot anthropometrics day to day, trimester to trimester? Ask more questions about their daily activities, are they ‘barefoot and pregnant’? Could something as simple as having them wear appropriate, arch supportive shoes while in the home reduce their lower extremity or back pain?"
Harrison, K. D., Mancinelli, C., Thomas, K., Meszaros, P., & McCrory, J. L. (2016). The Relationship Between Lower Extremity Alignment and Low Back, Hip, and Foot Pain During Pregnancy: A Longitudinal Study of Primigravid Women Versus Nulliparous Controls. Journal of Women’s Health Physical Therapy, 40(3), 139-146.
In our blog, we have highlighted the importance of recognizing and screening for postpartum depression. What relationships exist between a person's posture and depression in the postpartum period? Prior research reporting on four studies of posture (Riskind & Gotay, 1982) noted that subjects placed in a slumped physical posture appeared to develop helplessness more easily than those placed in an upright posture. These authors also stated that physical posture was a valuable clue for an observer who attempted to identify states of depression. Results of the fourth study include that "…subjects who were placed in a hunched, threatened physical posture verbally reported self-perceptions of greater stress than subjects who were placed in a relaxed position."
A recent study addressed depression, back pain and postural alignment in eighty women between 2 and 30 weeks postpartum. Depressive symptoms were measured with the Edinburgh Postnatal Depression Scale (EPDS). Pain scales included a visual analog scale (VAS) and the Nordic Musculoskeletal Questionnaire (NMQ while posture was assessed with visual observation. Findings of the study include that VAS pain scores were elevated in the women who were depressed. Back pain intensity and postpartum depression were also strongly associated. The authors suggest that back pain may be a risk factor for postpartum depression as well as a comorbidity. The article further states that physical therapists "…should be prepared to identify depressive symptoms as a comorbidity associated with posture changes and recurrent symptoms, signs of remission and recurrence that generate difficulties for treatment progression."
Can we look at this issue as a chicken and egg discussion, as in, is poor posture causativeto depression, or vice versa? And,if smiling has been determined to have the ability to improve happiness, can improved posture positively affect symptoms of depression? We know that postural dysfunction and pain can be a vicious cycle in our patients. Is screening for depression an equally important aspect of postural correction? Could postural taping, support, or re-training positively affect postpartum depression, and if so, should we be assessing and re-assessing our patients for depression as a means to document therapy benefits? The fun thing about reading research results is that the studies often lead to more questions, further hypotheses, and curiosity in relationship to how we interact with our patients. Can patients understand the relationship between postural correction and emotional health? Sounds like an opportunity for more research, and for dialoging with our patients!
If you are interested in learning more about postpartum health, click here for more information about the second course in our Peripartum series, Care of the Postpartum Patient. The next opportunities to take this class are June in Houston, and Chicago in September!