Herman & Wallace is committed to providing courses on pelvic rehabilitation for all people across the spectrum. This week the featured courses are those focused on women's health!
Take a look and see if there is one that is a good fit for you.
Breastfeeding Conditions Remote Course - Remote Course
July 16 and November 19
This course provides a thorough introduction to the physiology of the lactating breast, dysfunction and treatment interventions, the therapist's role in breastfeeding and pumping support, as well as when to refer to other health professionals.
Lectures will include the anatomy and physiology of lactation, blocked ducts and mastitis, and breast pain through a biopsychosocial lens. During labs, participants will have the opportunity to systematically assess the breast and practice therapeutic breast massage and manual milk expression. Participants will learn to assess and treat breast inflammation and pain such as mastitis, blocked ducts, milk blebs, and cracked nipples.
Breastfeeding Conditions - July 16-17, 2022
Breastfeeding Conditions - November 19-20, 2022
Menstruation and Pelvic Health - Remote Course
July 16-17, 2022

Menstruation and Pelvic Health is a two-day remote course is designed for clinicians who want to obtain advanced knowledge and skills to educate patients on non-hormonal, non-surgical, and non-prescription interventions for improving the Menstrual Experience. Developed by Nicholas Gaffga, MD, MPH, FAAFP, and presented together with Amy Meehan, PT, DPT, MTC, this course is geared toward the pelvic rehab provider looking to impart Menstrual Interventions that:
- Put control in the hands of people who menstruate to identify and carry out the interventions that are appropriate to them
- Use a holistic approach and advanced knowledge and familiarity with body and mind
- Emphasize healthy practices that can positively impact the Menstrual Experience and beyond, in areas such as mental health and chronic diseases
- Discover root causes of issues, rather than quick fixes, to have benefits that are sustainable across the lifespan.
Postpartum Rehabilitation - Remote Course
offered monthly through November

The client who is postpartum may be one of the most overlooked clients in health care. Knowing the specific rehabilitation needs to help with common problems and prevent future problems is the goal of this beginner-level course. For the orthopedic-based practitioner, this course will solidify awareness of the common orthopedic needs of the postpartum client. For the non-orthopedic practitioner, this course will provide a foundation for working with clients experiencing common postpartum-related musculoskeletal conditions.
This course will cover examination considerations and modifications specific to postpartum, as well as specific questions to ask during history taking and methods for identifying red flags in postpartum. More comfortable positions during the examination/treatment and common posture/gait/balance changes during postpartum are covered. The participant in this course will understand necessary biomechanics training for daily activities, child care, and breastfeeding. As an expansion from the pregnancy rehabilitation course, participants will be taken through progression in diastasis rectus abdominis (DRA) assessment and rehabilitation, including DRA exercises in lecture and lab.
Postpartum Rehabilitation - July 23-24, 2022
Postpartum Rehabilitation - August 20-21, 2022
Doula Services and Pelvic Rehab Therapy - Remote Course
August 6 and December 10
A growing number of pelvic health therapists are recognizing the importance of preparing their clients for the physical and mental challenges of labor and delivery. In some cases, this is extending to a desire to be present during labor for support as a Doula. The purpose of this course is to present the unique challenges of merging a rehab practice with Doula services in order to help the participant better discern whether or not this is a journey worth taking.
Doula Services and Pelvic Rehab Therapy - August 6, 2022
Doula Services and Pelvic Rehab Therapy - December 10, 2022
Fertility Considerations for the Pelvic Therapist - Remote Course
August 13

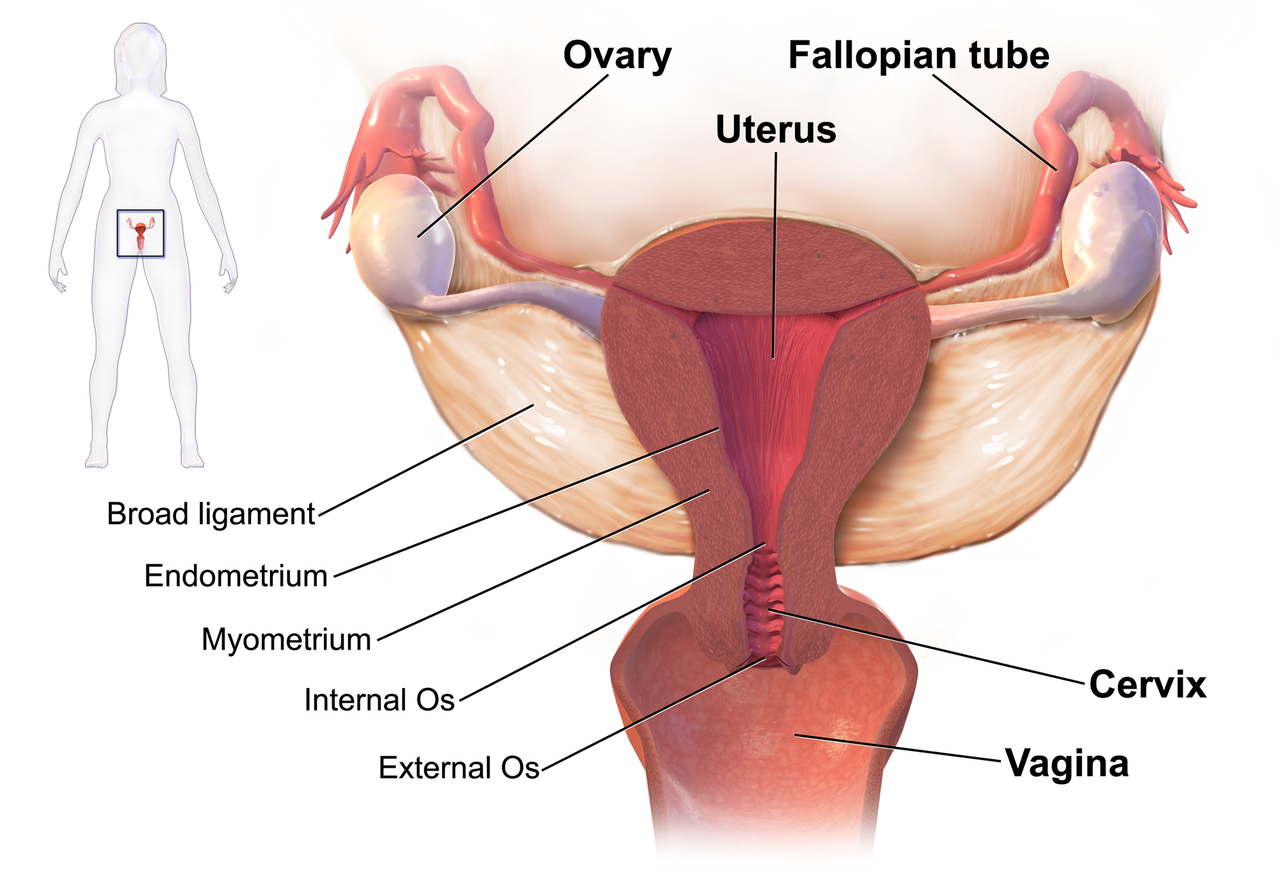
This course is for practicing pelvic rehabilitation therapists and covers the role of rehabilitation therapists in optimizing female fertility. This course was written and will be instructed by Dr. Yeni Abraham, who is a Dallas-Ft.Worth-based Pelvic Physical Therapists specializing in the treatment of Gynecologic and Fertility related conditions. Lecture topics include medical infertility labs, pertinent information on charting cycles, assisted reproductive technologies and their impact on treatment, hormone regulation, the relationship between inflammation and infertility, amongst other topics. Lab activities/break-out sessions will include manual techniques to influence uterine and ovarian Mal-positions.
*This course will require that each student have a live model that will allow participants to practice the lab techniques on a human body. Due to the nature of labs, please be sure your model partner is not pregnant and does not have an IUD for safety. Additionally, those with hydrosalpinx will not be able to participate in uterine mobility techniques but can still attend the course.
Fertility Considerations for the Pelvic Therapist - August 13, 2022
Menopause Transitions and Pelvic Rehab - Remote Course
August 27-28th and November 12-13th

Menopause Transitions and Pelvic Rehab is a two-day course is designed for the clinician that wants to understand the multitude of changes that are experienced in the menopause transition and how they affect the aging process. Upon completion of this course, participants will have a basic understanding of the hormonal changes during menopause, the impact on various health systems, and interventions that can assist with improving this transition.
This is an excellent opportunity to understand the physiological consequences to the body as hormones decline, in order to assist our patients in lifestyle habits for successful aging. Topics will include cardiovascular changes, metabolic syndrome, bone loss and sarcopenia, neurological changes (headache, brain fog, sleeplessness), Alzheimer’s risk, and urogenital changes. Symptoms and treatment options will also be discussed, including hormone replacement, non-hormonal options, dietary choices, and exercise considerations.
Menopause Transitions and Pelvic Rehab - August 27-28, 2022
Menopause Transitions and Pelvic Rehab - November 12-13, 2022
Medical Perspective in Peripartum Care - Remote Course
September 17-18th

Medical Perspective in Peripartum Care is a two-day course instructed by Dina Gordon, MD, FACOG, a practicing OB/GYN in the Seattle area, and will discuss common conditions encountered in the peripartum period from the medical perspective. Topics include medical screening; medical management of high-risk patients (bed rest, activity limitations, medications, surveillance); and interventions common in the peripartum period
The course is built from the medical perspective, the design of the course aims to share knowledge so that rehabilitation care planning is optimized.
Medical Perspective in Peripartum Care - September 17-18 2022
Pregnancy and Postpartum Considerations for High Intensity Athletics
September 11

The main focus of this course will be to learn how exercising throughout pregnancy, or returning to exercise postpartum may look different for a high-intensity athlete versus a non-HIIT athlete. Participants will discuss how anatomical and hormonal changes affect training for the pregnant and postpartum athlete, review various modifications for this population, learn how various stresses placed on the body during these activities may affect pelvic floor muscle function, and review various pressure management strategies that can be utilized during high-intensity interval training. This one-day remote continuing education course is designed to educate practitioners on the unique considerations of pregnant and postpartum athletes engaging in high-intensity interval training (HIIT).
During the pregnancy lab, we will review specific exercise modifications for pregnancy, utilization of breathwork to properly support the pelvic floor during pregnancy and review how to assess for and tape for diastasis recti. In the postpartum lab, we will review how to determine proper activity modification based on the ability to manage pressure, review specific activity modifications and breathwork, review accessory work for return to activity, and discuss how to assess pelvic organ prolapse in standing.
Pregnancy and Postpartum Considerations for High Intensity Athletics - September 11, 2022
Perinatal Mental Health: The Role of the Pelvic Rehab Therapist
October 22

This one-day continuing education course covers mental health considerations during pregnancy and postpartum and is targeted to the pelvic rehab clinician treating patients in the peripartum period. Topics include common mental health concerns in the postpartum period including depression, anxiety, OCD, and PTSD, as well as the connectedness between mental health and physical dysfunction.
The course will introduce useful screening tools and how to connect patients to resources and diagnosing professionals. Labs will include partnered breakout sessions to practice listening and dialogue skills. The course also includes a review of coping techniques to support mental health and physical symptoms.
Perinatal Mental Health: The Role of the Pelvic Rehab Therapist - October 22, 2022
Pregnancy Rehabilitation - Remote Course
October 29-30 and November 5-6

Learn how to safely examine and treat the pregnant patient in this beginner-to-intermediate course.
Lectures cover terminology, fertilization, trimesters, medical testing/interventions, imaging, and medications. Participants will learn to differentiate between false labor, progressive labor, and other musculoskeletal pain as well as learn to understand typical hormonal and systemic changes during pregnancy. Examination, evaluation, and treatment of common lumbopelvic conditions will be provided with an introduction to diastasis rectus abdominis, pelvic floor dysfunction, breathing, and deep core assessment/treatment.
Discussions also include general examination considerations and modifications specific to pregnancy, including a discussion of modalities and manual therapy techniques considered safe or precautioned during pregnancy, with further lectures on pelvic girdle examination, diagnosis, and treatment strategies. Finally, to prepare the pregnant client for labor and birth, instruction in perineal stretching, hip and trunk flexibility activities and TENS for labor will be discussed. Lab practice will include labor and birthing positions, with a focus on consideration for positional strategies for women with pre-existing musculoskeletal problems.
Pregnancy Rehabilitation - October 29-30, 2022
Pregnancy Rehabilitation - November 5-6, 2022

The following is an excerpt from an interview between Niko Gaffga, MD, FAAFP, MPH (NG) and Holly Tanner (HT) about why he is interested in women’s health and the menstrual experience. Niko and Amy Meehan, PT, DPT, MTC have co-authored a specialty course for H&W all about Menstruation and Pelvic Health – to learn more join us in the upcoming remote course on July 16th-17th, 2022. You can watch the full video interview below, or on the Herman & Wallace YouTube Channel.
HT – So menstruation as a topic, what is it that got you so passionate about this particular topic?
NG -Throughout my career and my training, women’s health and OB have been one of my favorite parts of my job. In recent years there was a patient who really inspired me. I came into the room, and she was sitting in the corner in the exam room of the clinic where I worked and she was crying. I came in and I asked, she only spoke Spanish…and I asked her “ How are you doing? What’s happening?” and she was very reluctant to say anything.
I found out through a little bit of discussion that she was feeling pain, and she couldn’t make the pain go away. That she had seen many doctors about it and no one had been able to help her. She was reluctant to show me where on her body – maybe it’s because I’m a man, or maybe it was because she was from a different country – she didn’t feel secure. So I drew a little picture on a piece of paper, and I said “Just point to me on this paper where you feel the pain.” After a while of pointing, talking, and smiling I got to a point where she could explain to me what was happening.
It turns out that she had painful bladder syndrome, or interstitial cystitis, and we worked over the months to get that better. And I have to say, that the next time that I walked into that the next time that I walked into that same room and she was there – she was smiling. She stood up and she gave me a hug – and I said to myself, “This is why I do medicine.”
I think really the breakthrough came when I met her where she was. I took the time to talk to her in her language, show her a piece of paper, and wait for her to say what she felt. Cause many doctors, you know how they only have two or three minutes to talk with their patients. When I met her halfway, she was able to talk to me about the pain she was feeling, about her menstrual cycles – which I don’t think she had ever discussed with any doctors before.
So that started me down the road in being interested in what can I do – what more can I do to help women. When I see women in the clinic a lot of them don’t want to say anything about their menstrual cycle, and again maybe it’s because I’m a man. Maybe it’s because it’s just a difficult topic to discuss, but I realize that in society we don’t have a lot of chance as men or women to talk about the menstrual cycle.
I feel that it is a disservice to women that they don’t have a chance to talk about things that genuinely interest them, are concerning to them, or have questions and are curious about. I feel that there is a stigma, and I think that this course will begin to address it within a small group. But I think eventually, training and working with healthcare providers is one step in making that message available to other people, and to other patients all around the country. So that is how it evolved for me.
One of the most important things for me is that talking about the menstrual experience and women’s health, in general, allows me to change, to give people information, to make decisions in their life that are in alignment with the way that they see the world. I think that not many professions can say that. You know medical professions, physical therapists, doctors, and many other professions - we help people do what they want to do for themselves, and that’s powerful. That’s very powerful.
I think that the most important thing is that I can make a difference in someone else’s life. I’ve seen it when talking to women in the clinic who I’ve seen before. Discussing their menstrual cycle and having them tell me this is the first I’ve spoken about to anyone, much less to a female or a male provider. Hearing someone say that is meaningful. It is a lot of trust that they place in someone to tell them these kinds of things because they are difficult topics. Seeing that you can make a difference in someone else’s life...it means a lot to me, and this is the reason why [I’m so passionate about women’s health and the menstrual experience].

Menstruation and Pelvic Health - July 16-17 2022
The Menstrual cycle is one of the most natural of all human processes and is experienced by half of the population of the world. At any given time, 800 million individuals are menstruating. The Menstrual cycle occurs roughly once a month for roughly 35 to 40 years in a lifetime. That ends up being almost 3000 days, or about 8 years of menses. Many menstruators experience “period shaming” and other forms of socialized stigma around the menstrual experience. It is therefore important to become familiar with this experience and provide care to patients that takes into account their Menstrual Experience.
This two-day remote continuing education course is designed for clinicians who want to obtain advanced knowledge and skills to educate patients on non-hormonal, non-surgical, and non-prescription interventions for improving the Menstrual Experience. Developed by Nicholas Gaffga, MD, MPH, FAAFP, and presented together with Amy Meehan, PT, DPT, MTC, this course is geared toward the pelvic rehab provider looking to impart Menstrual Interventions that:
- Put control in the hands of people who menstruate to identify and carry out the interventions that are appropriate to them
- Use a holistic approach and advanced knowledge and familiarity with body and mind
- Emphasize healthy practices that can positively impact the Menstrual Experience and beyond, in areas such as mental health and chronic diseases
- Discover root causes of issues, rather than quick fixes, to have benefits that are sustainable across the lifespan.
A different approach to treating prostatectomy patients.
The Pelvic Rehab Report sat down with Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC to discuss her upcoming courses Rehabilitative Ultrasound Imaging - Orthopedic Topics and Rehabilitative Ultrasound Imaging: Women's Health and Orthopedic Topics scheduled for November 12-14, 2021. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain.
As a pelvic floor clinician, you may have worked with patients who are suffering from urinary incontinence following prostatectomy. During a prostatectomy the prostate, seminal vesicles, prostatic urethra, and some connective tissues are removed. The extent of the removal will depend on the size of the tumor and if the tumor has spread into the surrounding tissues. Because of the surgery, and the loss of smooth muscle surrounding the urethra, there is an inherent risk that these patients will suffer from urinary incontinence. Recently, there have been studies that examined the difference between patients who return to continence and those who do not return to continence following prostatectomy. They found that continent prostatectomy men demonstrated increased displacement of the striated urethral sphincter, bulbocavernosus, and puborectalis compared to incontinent men. They also found that continent prostatectomy patients demonstrated better puborectalis and bulbocavernosus function than controls! (1) This has made researchers conclude that continent men following prostatectomy compensate for the loss of smooth muscle by having better than normal function in their pelvic floor.
In another recent article, researchers put together recommendations for a rehabilitation program. They argue that traditional methods that have been used in pelvic floor therapy are based on applied principles for stress incontinence in women, not men. Men suffer from incontinence for a different reason than women. Thus, their treatment should be approached differently as well. Additionally, the authors state that examining the pelvic floor muscles via a digital rectal exam does not allow the examiner to assess the underlying issue that leads to incontinence in men, the striated urethral sphincter. Instead, a digital rectal exam identifies issues in the external anal sphincter and puborectalis. They highly recommend the use of transperineal ultrasound imaging in order to view the contraction of the pelvic floor and confirm where the contraction is originating from. They also highly recommend the use of ultrasound in treatment for the use of motor re-learning(2).
We will discuss this more in-depth as well as learn how to use ultrasound imaging to help both male and female patients suffering from incontinence. We also will be learning how to use ultrasound imaging to address orthopedic conditions such as back pain, sacroiliac joint pain, and diastasis rectus. The course “Rehabilitative Ultrasound Imaging for the Pelvic Girdle” is now being offered with satellite locations as well as a limited number of self-hosted online groups and is scheduled for November 12-14, 2021. There are two courses being offered. The 2-day version, Rehabilitative Ultrasound Imaging - Orthopedic Topics, addresses the use of ultrasound imaging to help back and lumbopelvic conditions. While the 3-day course, Rehabilitative Ultrasound Imaging: Women's Health and Orthopedic Topics, includes more pelvic floor related conditions such as prolapse and post-prostatectomy issues. The course includes ample lab time so participants leave with the clinical skills to be able to use ultrasound imaging in their practice.
- Stafford R.E., Couglin G., Hodges P. Comparison of dynamic features of pelvic floor muscle contraction between men with and without incontinence after prostatectomy and men with no history of prostate cancer. Neurourology and Urodynamics. 2020; 39:170-180.
- Hodges, PW., Stafford RE, Hall L., et al. (2020). Consideration of pelvic floor muscle training to prevent and treat incontinence after radical prostatectomy. Urologic Oncology: Seminars and Original Investigations. 38: 354-371
September is Gynae Cancer Awareness Month – but how aware are we as clinicians of the signs and symptoms, the epidemiology and the sequalae of treatment afterwards? As pelvic rehab specialists, we have the privilege of helping women live well after cancer treatment ends, both on a ‘local’ pelvic area (bladder, bowel, sexual and pelvic pain management strategies) but also on a more ‘global’ level – dealing with issues such as cancer related fatigue, bone health and cardiovascular concerns.
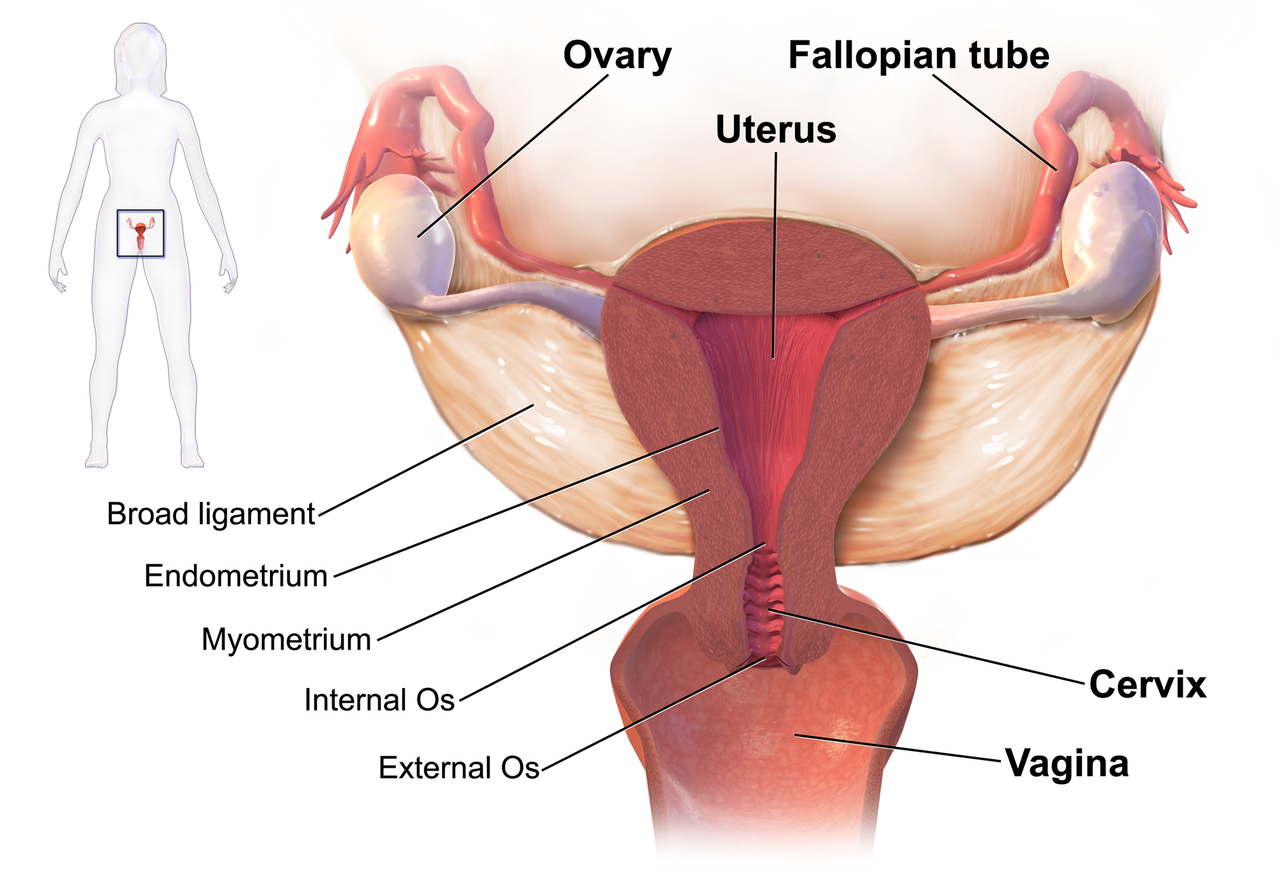 We know that women who are diagnosed with cancer of the vulva, vagina, cervix, endometrium or ovaries are treated with a combination of surgery, radiation or chemotherapy. However, with improving treatment and better survival rates, there is evidence that a variety of pelvic health concerns may arise for these women, both during and after treatment. (Hazewinkel et al 2010). For example, urinary incontinence is reported in 80% of women treated for endometrial cancer, with more severe symptoms and impact on quality of life in those who had adjuvant radiation (Erekson et al 2009) In Malone’s 2017 paper, ‘The patient’s voice: What are the views of women on living with pelvic floor problems following successful treatment for pelvic cancers?’, the author notes that ‘…there is currently a lack of knowledge regarding the effects of PFD on QoL in this cohort. Patients do not always report these problems to their health care providers and clinicians may underestimate symptoms…In the context of having survived cancer, PFD may be seen as relatively trivial. However, in the context of resuming normal living, the symptoms experienced by the survivors may be significant’.
We know that women who are diagnosed with cancer of the vulva, vagina, cervix, endometrium or ovaries are treated with a combination of surgery, radiation or chemotherapy. However, with improving treatment and better survival rates, there is evidence that a variety of pelvic health concerns may arise for these women, both during and after treatment. (Hazewinkel et al 2010). For example, urinary incontinence is reported in 80% of women treated for endometrial cancer, with more severe symptoms and impact on quality of life in those who had adjuvant radiation (Erekson et al 2009) In Malone’s 2017 paper, ‘The patient’s voice: What are the views of women on living with pelvic floor problems following successful treatment for pelvic cancers?’, the author notes that ‘…there is currently a lack of knowledge regarding the effects of PFD on QoL in this cohort. Patients do not always report these problems to their health care providers and clinicians may underestimate symptoms…In the context of having survived cancer, PFD may be seen as relatively trivial. However, in the context of resuming normal living, the symptoms experienced by the survivors may be significant’.
This can present a clinical conundrum – often pelvic rehab therapists are nervous when working with a patient who has a current or previous gynecologic cancer diagnosis, but similarly oncology rehab specialists may have qualms about dealing with pelvic health issues, with the result that these women fall through the cracks and do not have their pelvic health issues managed properly (or at all). Theodore Roosevelt once said ‘No one cares how much you know, until they know how much you care’ and this is especially relevant for oncology pelvic rehab. Often you may be the first clinician to ask about bladder, bowel or sexual function or dysfunction. An understanding of the effects of cancer treatments on the pelvis is important but so too is the wealth of information you may already have about bladder, bowel and sexual health as well as neuroscience and pain education.
The most important thing is to ask these women about their pelvic health concerns – the National Coalition for Cancer Survivorship defined cancer survivorship as extending from ‘the time of diagnosis and for the balance of life’. An emphasis on quality of life has been emphasised – if we know that cancer survivors may not independently volunteer information about their pelvic floor dysfunction, it is our responsibility to ask the questions and comprehensively treat and advocate for these women, in order to help them live well after cancer treatment ends.
- Hazewinkel MH. Sprangers MA, Velden Jvd, Vaart CH, Stalpers LJ, Burger MP ‘Longterm cervical cancer survivors suffer from pelvic floor dysfunction symptoms: A cross-sectional matched cohort study’ Gynecol Oncol 2010;117(2):381-6
- Erekson EA, Sung VW, Disilvestro PA, Myers DL ‘Urinary symptoms and impact on quality of life in women after treatment for endometrial cancer’ Int Urogynecol J 2009;20(2):159-63
- Malone P, Danaher D, Galvin R, Cusack T ‘The patient’s voice: What are the views of women on living with pelvic floor problems following successful treatment for pelvic cancers?’ Physiotherapy Practice and Research 38(2017)93-102