When discussing the use of ultrasound imaging in my clinical practice, I am often asked, “What type of patient is your favorite to use ultrasound with?” This is a hard question for me to answer because ultrasound is so beneficial for several types of patients.
Ultrasound is used in a wide range of clinical scenarios, including sacroiliac joint (SIJ) and lumbar spine pain, guiding core strengthening for oncology or post-surgical patients, supporting recovery after prostatectomy, and assessing pediatric and adolescent pelvic floor function. I often highlight that ultrasound imaging is particularly valuable when internal pelvic assessments are not possible, for example, in the immediate postpartum period when pelvic rest is prescribed. In such cases, transabdominal ultrasound can help confirm whether patients are correctly engaging their pelvic floor muscles following a vaginal delivery.
A recent study in the Journal of Women’s & Pelvic Health Physical Therapy explored the use of ultrasound imaging in the early postpartum period. The study included 75 women between 0 and 5 days after vaginal delivery. Each participant took part in a single in-person session where ultrasound was used both as an assessment tool for the clinician and as biofeedback for the patient.
The study concluded that with only one session, using ultrasound as biofeedback improved contractions for participants. Vertical bladder excursion during a pelvic floor contraction was improved, especially in those patients who initially presented with paradoxical excursions, and those who suffered perineal trauma during delivery. Participants were satisfied with the experience of using ultrasound imaging and receiving early postpartum PFM rehabilitation.
This is an exciting development, especially for those of us working in hospital settings! The ability to visit patients shortly after childbirth and begin pelvic floor rehabilitation right away presents a major opportunity. It allows us to reach more patients early, provide essential education, and address potential issues before they progress. With today’s smaller, more portable ultrasound units, which can even connect to a smartphone or tablet, therapists can easily bring them onto the labor and delivery unit to examine patients within the first few days after delivery.
The Course: Rehabilitative Ultrasound Imaging: Pelvic Health & Orthopedic Topics
This course examines how rehabilitative ultrasound imaging can benefit various patient populations. You'll learn how to apply ultrasound in both orthopedic and pelvic health settings. There are two course options: a two-day version tailored for orthopedic therapists, and a three-day version designed for pelvic floor therapists, which includes deeper training on pelvic floor-specific conditions. Join me September 5–7 to learn how to integrate ultrasound imaging into your clinical practice. Satellite Options for the September 5-7 course date include:
- Rehabilitative Ultrasound: Orthopedic Topics - September 5-6
Indianapolis IN
Seattle WA
Self-Hosted - Rehabilitative Ultrasound Imaging Pelvic Health - September 5-7
Indianapolis IN
Seattle WA
Self-Hosted
AUTHOR BIO
Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC
 Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC (she/her) has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health, including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion to help oncology patients, particularly gynecological, urological, and head and neck cancer patients.
Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC (she/her) has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health, including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion to help oncology patients, particularly gynecological, urological, and head and neck cancer patients.
In 2009, Allison collaborated with the Primal Pictures team for the release of the Pelvic Floor Disorders program. Allison's publications include: “The Use of Transabdominal Ultrasound Imaging in Retraining the Pelvic-Floor Muscles of a Woman Postpartum.” Physical Therapy. Vol. 88, No. 10, October 2008, pp 1208-1217. (PMID: 18772276), “Beyond the Abstract” for Urotoday.com in October 2008, “Posters to Go” from APTA combined section meeting poster presentation in February 2009 and 2013. In 2016, Allison co-authored a chapter in “Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies.”
Allison works in the Denver metro area in her practice, Inspire Physical Therapy and Wellness, where she works in a more holistic setting than traditional therapy clinics. In addition to instructing Herman and Wallace on pelvic floor-related topics, Allison lectures nationally on lymphedema, cancer-related changes to the pelvic floor, and the sacroiliac joint. Allison serves as a consultant to medical companies and physicians.

At Herman & Wallace, we know that pelvic rehabilitation is a dynamic and ever-evolving field. While foundational courses like Pelvic Function Level 1 and Dry Needling and Pelvic Health often get the spotlight, there are several highly valuable courses that tend to fly under the radar. These courses offer practitioners the opportunity to deepen their knowledge, broaden their skills, and better serve patients with complex needs.
Here are five underrated courses that can have a powerful impact on your practice:
1. Nutrition Perspectives for the Pelvic Rehab Therapist
 Pelvic health doesn’t exist in isolation from the rest of the body, and nutrition plays a critical role in tissue healing, inflammation, digestion, and pelvic pain syndromes. This course introduces pelvic rehab practitioners to the fundamentals of nutrition as it relates to pelvic health.
Pelvic health doesn’t exist in isolation from the rest of the body, and nutrition plays a critical role in tissue healing, inflammation, digestion, and pelvic pain syndromes. This course introduces pelvic rehab practitioners to the fundamentals of nutrition as it relates to pelvic health.
Participants learn how to recognize when dietary factors may be contributing to issues such as constipation, bladder irritation, vulvar pain, or chronic inflammation. While not a course that trains clinicians to act as dietitians, it empowers them to screen for red flags, collaborate with nutrition professionals, and make basic, evidence-informed recommendations that can significantly impact patient outcomes.
2025 Course Date Options: October 11-12, December 6-7.
2. Oncology and the Pelvic Floor Series
 (OPF1: Foundations, OPF2A: Male Pelvic & Colorectal Cancers, and OPF2B: Female Pelvic & Bladder Cancers)
(OPF1: Foundations, OPF2A: Male Pelvic & Colorectal Cancers, and OPF2B: Female Pelvic & Bladder Cancers)
Pelvic health isn’t just for perinatal or orthopedic populations. People undergoing treatment for pelvic and abdominal cancers face unique and complex challenges, including incontinence, pelvic pain, sexual dysfunction, and scar tissue restrictions.
The Oncology and the Pelvic Floor series offers a comprehensive framework for working with patients at every stage of the cancer journey, and provides the knowledge and sensitivity needed to support this underserved population, integrating trauma-informed care, manual therapy, exercise, and interdisciplinary collaboration.
2025 Course Date Options: Level 1 September 13-14, Level 2A December 6-7, Level 2B November 1-2.
3. Pharmacologic Considerations for the Pelvic Health Provider
 Medications have a profound impact on the pelvic floor—often in ways that are overlooked. Whether it’s constipation from opioids, hormonal changes from contraceptives, or bladder irritation from certain antibiotics, understanding pharmacology is crucial.
Medications have a profound impact on the pelvic floor—often in ways that are overlooked. Whether it’s constipation from opioids, hormonal changes from contraceptives, or bladder irritation from certain antibiotics, understanding pharmacology is crucial.
This course demystifies medications commonly encountered in pelvic health practice. It helps clinicians understand how drugs can influence bowel, bladder, sexual function, pain processing, and healing. Armed with this knowledge, practitioners can engage in more informed discussions with patients and other members of the healthcare team, helping to troubleshoot barriers to progress.
2025 Course Date Option: September 13.
4. Yoga for Pelvic Pain
 Yoga is more than stretching—it’s a mind-body practice with proven benefits for nervous system regulation, pain management, and muscular balance. Yoga for Pelvic Pain teaches practitioners how to integrate evidence-based yoga principles into rehabilitation for patients with chronic pelvic pain.
Yoga is more than stretching—it’s a mind-body practice with proven benefits for nervous system regulation, pain management, and muscular balance. Yoga for Pelvic Pain teaches practitioners how to integrate evidence-based yoga principles into rehabilitation for patients with chronic pelvic pain.
This course goes beyond asana (physical postures) to incorporate breathwork, mindfulness, and gentle movement tailored to the needs of people with complex pain syndromes. Participants leave with practical tools they can immediately incorporate into one-on-one sessions or group classes, supporting both physical function and emotional well-being.
2025 Course Date Option: September 13-14.
5. Rehabilitative Ultrasound Imaging: Pelvic Health & Orthopedic Topics
 Rehabilitative Ultrasound Imaging (RUSI) provides real-time feedback for both clinicians and patients. It’s an invaluable tool for assessing muscle activation, motor control, and coordination - particularly for the deep core and pelvic floor muscles.
Rehabilitative Ultrasound Imaging (RUSI) provides real-time feedback for both clinicians and patients. It’s an invaluable tool for assessing muscle activation, motor control, and coordination - particularly for the deep core and pelvic floor muscles.
This course covers both pelvic health applications (like visualizing pelvic floor contractions) and broader orthopedic topics (like assessing the transverse abdominis or multifidus). Practitioners gain hands-on experience in using ultrasound to refine exercise prescription, improve patient engagement, and objectively document progress. Despite its transformative potential, RUSI remains underutilized in many pelvic rehab settings.
2025 Course Date Options for September 5-7: Self-hosted, Indianapolis IN, Seattle WA.
Don’t Overlook These Gems
Expanding your clinical toolbox with specialized knowledge can transform your patient care. Whether it’s understanding how nutrition, medications, cancer treatments, or mind-body practices influence the pelvic floor—or learning to harness the power of ultrasound imaging—these courses provide essential insights that go beyond the basics.
Ready to elevate your practice? Explore these courses and others at Herman & Wallace and continue your journey as a lifelong learner in pelvic rehabilitation.

Any pelvic floor rehabilitation provider knows that pregnancy can lead to changes in the pelvic floor and the abdominal wall. In the postpartum period, many individuals would like to strengthen their pelvic floor and abdominal muscles in an attempt to return to fitness and previous exercise routines. Is there a difference in how someone approaches training these muscles in the postpartum period? Will activating the muscles cause harm for our patients? This can be controversial amongst pelvic rehabilitation providers. I have heard some clinicians say that once a patient has had a pregnancy and vaginal birth, then they should never do sit-ups again, instead they should work the abdominal muscles in different ways. Others argue it depends on the individual patient.
A recent study examined the effects of different types of abdominal contractions on the positioning of the pelvic organs in nulliparous and postpartum women. Six different pelvic floor and abdominal contractions were tested, and the bladder positioning was examined using ultrasound imaging. There was significantly more lift of the bladder base when a submaximal contraction of the pelvic floor and transverse abdominis were performed with an elongation of the back. With a curl-up contraction, there was a significant amount of descent of the bladder base (Martinez-Bustelo, 2021). This increased descent of the bladder demonstrates that the choice of abdominal activation does make a difference and influences the pelvic organs. However, the overall individuality of the patient makes a difference as well. The overall management of the internal pressure system for the individual can influence the descent of the pelvic organs positively or negatively. Additionally, patients who have a diastasis recti abdominis may have additional precautions when wanting to exercise their abdomen and core.
How can clinicians observe the supportive component of the pelvic floor?
Ultrasound imaging can be performed quickly and easily, allowing the practitioner to view the pelvic organs and their response to different types of contractions. This can allow us to customize a program for post-partum individuals that are wanting to return to fitness and exercise activities and make sure that the patient is not exerting pressure into their pelvic area in a way that is not ideal. Ultrasound imaging also allows clinicians to treat postpartum patients sooner. We can treat them immediately in the postpartum period. We do not need to wait until the patient is cleared for internal work or deal with lochia for an external assessment. We are able to immediately help our post-partum patients through abdominal imaging.
You can learn to use ultrasound imaging through Herman & Wallace’s Rehabilitative Ultrasound Course. This course guides you through the process of learning to use ultrasound imaging transabdominally and transperineally to assist your post-partum patients in regaining core and pelvic organ strength. This tool is also useful for other diagnoses including anyone with lumbopelvic pain, pelvic floor weakness, and pelvic organ prolapse. Join us this April to learn more about ultrasound imaging!
Upcoming course details:
- Rehabilitative Ultrasound Imaging - Pelvic Health and Orthopedic Topics is a 3-day course that presents both ideal and abnormal responses of real-time imaging of the transverse abdominals, rectus abdominis, deep multifidus, levator ani, bladder, bladder neck, urethra, and vagina during contraction and Valsalva. Imaging methods used during labs will consist of transabdominal viewing as well as transperineal/translabial viewing methods. Prior experience with perineal and vaginal assessments is required to take the course.
- Rehabilitative Ultrasound Imaging - Orthopedic Topics is a 2-day course that presents both ideal and abnormal responses of real-time imaging of the transverse abdominals, rectus abdominis, deep multifidus, levator ani, bladder, and bladder neck.
- You can also meet Allison and get a hands-on demonstration of rehabilitative ultrasound at HWConnect.
Reference:
- Martínez-Bustelo, S., Ferri-Morales, A., Corral-Gómez, L. et al. Transabdominal ultrasound to assess the displacement of the bladder base during abdominal and pelvic floor contractions in continent parous versus nulliparous women. Int Urogynecol J 33, 2257–2266 (2022). https://doi.org/10.1007/s00192-021-04756-4
AUTHOR BIO
Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC
 Allison Ariail has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
Allison Ariail has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
In 2009, Allison collaborated with the Primal Pictures team for the release of the Pelvic Floor Disorders program. Allison's publications include: “The Use of Transabdominal Ultrasound Imaging in Retraining the Pelvic-Floor Muscles of a Woman Postpartum.” Physical Therapy. Vol. 88, No. 10, October 2008, pp 1208-1217. (PMID: 18772276), “Beyond the Abstract” for Urotoday.com in October 2008, “Posters to Go” from APTA combined section meeting poster presentation in February 2009 and 2013. In 2016, Allison co-authored a chapter in “Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies.”
Allison works in the Denver metro area in her practice, Inspire Physical Therapy and Wellness, where she works in a more holistic setting than traditional therapy clinics. In addition to instructing Herman and Wallace on pelvic floor-related topics, Allison lectures nationally on lymphedema, cancer-related changes to the pelvic floor, and the sacroiliac joint. Allison serves as a consultant to medical companies, and physicians.

There are currently two scheduled course offerings available for Modalities and Pelvic Function: Philadelphia PA in April 6-7 and Manchester NH in August 24-25. If neither of these work for your location or schedule then consider hosting! The hosting requirements and interest form can be found on the Host a Course page.
The new Modalities and Pelvic Function - Pelvic Health Clinical Toolkit is an in-person two-day continuing education course targeted to pelvic health clinicians covering frequently used modalities in pelvic health, including biofeedback and EStim. This course was designed to answer the clinician’s need to understand how to choose and access the right tools, both for in-clinic care and for patient self-care application.
One of the course co-creators, Mora Pluchino shared “This class will be unlike one you've taken before. The H&W curriculum team sat down and thought about how we could make this the most interactive, hands-on, and practical course while still staying evidence-based and professional. This will be an in-person learning opportunity with 2 days of lab, demonstration, and interactive learning opportunities. If there is a modality that exists in pelvic health, it will likely have a debut here. This class is made for anyone who wants to learn to apply modalities in the variety of uses possible for pelvic health!"
Biofeedback and electrical stimulation are covered in this course, as are introductions to understanding tools such as shockwave, dry needling, real-time ultrasound, laser, and electrotherapies. With hands-on lab time and learning modules grouped into tools specific to pelvic health conditions such as bowel dysfunction and sexual health challenges, practitioners will have the opportunity to trial various tools and applications that previously may have only been available as an image in a presentation.
When our popular Pelvic Function Level 1 course, which introduces participants to the world of pelvic health, was transitioned to a satellite lab course one of the content pieces that was left out was the modalities focus - simply because the equipment was too difficult to ship to multiple satellite locations around the country. Herman & Wallace is thrilled to announce that not only have we solved this issue, but designed a way for clinicians to learn about dozens of modalities in an environment that allows the clinician to move beyond theoretical and soundly into the practical delivery of a variety of technologies and tools.
Current Medical Technologies will be in-person with us as we design this learning experience and will be available to answer your questions about products and clinical set-up. The interactive environment has been designed to be stimulating and allow the clinician to apply a variety of learning strategies including tactile opportunities to try things on themselves or a lab partner. This is a unique course that provides a foundational understanding of technology and tools, clinical practice research, and recommendations in an in-person environment. Many equipment providers have been generous in providing sample products for trial and even some giveaways to take home!
We believe this Modalities course is so foundational to our skillset in pelvic health that we have added it to our core Pelvic Function Series. This course is intended to be taken after Pelvic Function Level 1 and can be taken at any point following the introductory course as you work your way through the PF Series. If you’re wondering “When should I take this course?” the answer is “as soon as you can!”
A different approach to treating prostatectomy patients.
The Pelvic Rehab Report sat down with Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC to discuss her upcoming courses Rehabilitative Ultrasound Imaging - Orthopedic Topics and Rehabilitative Ultrasound Imaging: Women's Health and Orthopedic Topics scheduled for November 12-14, 2021. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain.
As a pelvic floor clinician, you may have worked with patients who are suffering from urinary incontinence following prostatectomy. During a prostatectomy the prostate, seminal vesicles, prostatic urethra, and some connective tissues are removed. The extent of the removal will depend on the size of the tumor and if the tumor has spread into the surrounding tissues. Because of the surgery, and the loss of smooth muscle surrounding the urethra, there is an inherent risk that these patients will suffer from urinary incontinence. Recently, there have been studies that examined the difference between patients who return to continence and those who do not return to continence following prostatectomy. They found that continent prostatectomy men demonstrated increased displacement of the striated urethral sphincter, bulbocavernosus, and puborectalis compared to incontinent men. They also found that continent prostatectomy patients demonstrated better puborectalis and bulbocavernosus function than controls! (1) This has made researchers conclude that continent men following prostatectomy compensate for the loss of smooth muscle by having better than normal function in their pelvic floor.
In another recent article, researchers put together recommendations for a rehabilitation program. They argue that traditional methods that have been used in pelvic floor therapy are based on applied principles for stress incontinence in women, not men. Men suffer from incontinence for a different reason than women. Thus, their treatment should be approached differently as well. Additionally, the authors state that examining the pelvic floor muscles via a digital rectal exam does not allow the examiner to assess the underlying issue that leads to incontinence in men, the striated urethral sphincter. Instead, a digital rectal exam identifies issues in the external anal sphincter and puborectalis. They highly recommend the use of transperineal ultrasound imaging in order to view the contraction of the pelvic floor and confirm where the contraction is originating from. They also highly recommend the use of ultrasound in treatment for the use of motor re-learning(2).
We will discuss this more in-depth as well as learn how to use ultrasound imaging to help both male and female patients suffering from incontinence. We also will be learning how to use ultrasound imaging to address orthopedic conditions such as back pain, sacroiliac joint pain, and diastasis rectus. The course “Rehabilitative Ultrasound Imaging for the Pelvic Girdle” is now being offered with satellite locations as well as a limited number of self-hosted online groups and is scheduled for November 12-14, 2021. There are two courses being offered. The 2-day version, Rehabilitative Ultrasound Imaging - Orthopedic Topics, addresses the use of ultrasound imaging to help back and lumbopelvic conditions. While the 3-day course, Rehabilitative Ultrasound Imaging: Women's Health and Orthopedic Topics, includes more pelvic floor related conditions such as prolapse and post-prostatectomy issues. The course includes ample lab time so participants leave with the clinical skills to be able to use ultrasound imaging in their practice.
- Stafford R.E., Couglin G., Hodges P. Comparison of dynamic features of pelvic floor muscle contraction between men with and without incontinence after prostatectomy and men with no history of prostate cancer. Neurourology and Urodynamics. 2020; 39:170-180.
- Hodges, PW., Stafford RE, Hall L., et al. (2020). Consideration of pelvic floor muscle training to prevent and treat incontinence after radical prostatectomy. Urologic Oncology: Seminars and Original Investigations. 38: 354-371
If you work with orthopedic patients, I am sure that you have had a back-pain patient that you have discharged, only for them to return a year later suffering from another episode of pain. We all know that once someone suffers from a back injury, they are more likely to develop a chronic issue. Even patients with insidious back pain and no specific injury often develop chronic issues and can have pain that waxes and wanes after the initial episode.
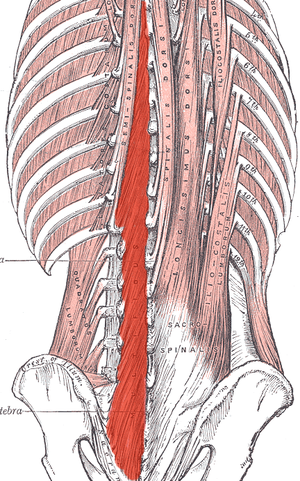
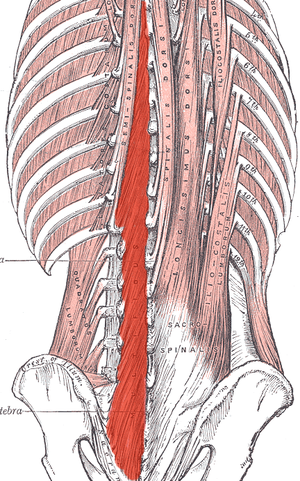 What happens in the body to cause this? Most of us have learned that the pelvic floor, transverse abdominus, and the deep fibers of the lumbar multifidus play an important role in stabilization. With injury, these muscles can become less effective in stabilizing the spine and pelvis. Studies have shown that muscle atrophy in the lumbar multifidus has been shown to occur with injuries and persist after resolution of the pain.1
What happens in the body to cause this? Most of us have learned that the pelvic floor, transverse abdominus, and the deep fibers of the lumbar multifidus play an important role in stabilization. With injury, these muscles can become less effective in stabilizing the spine and pelvis. Studies have shown that muscle atrophy in the lumbar multifidus has been shown to occur with injuries and persist after resolution of the pain.1
I recently did additional research to find out other reasons that cause these local stabilizing muscles to not function optimally. I found that these muscles also can suffer from arthrogenic muscle inhibition after an episode of low back pain.2 Arthogenic inhibition is a deficit in neural activation to a muscle. It is thought to occur due to a change in the discharge of articular sensory receptors due to swelling, inflammation, joint laxity, and damage to afferent nerves.2 EMG studies have shown reduced neural activity in the deeper fibers of the multifidus in patients with back pain.3
Another thing that fascinated me was that cortical changes in the brain also occur with low back pain. Changes in cortical representation of the multifidus and the body’s ability to voluntarily activate the muscle has been noted.4 Motor retraining has been shown to reorganize the motor cortex with regards to the transverse abdominus.5 Also, improvement in brain organization and function occurs after resolution of back pain.6
This is good news for patients! As therapists, we may not be able to do anything with respects to arthogenic inhibition. However, we can work on motor retraining for the core muscles. It has been shown that specific training that targets the multifidus can restore the neural activity to the multifidus and lead to improvement of pain and function.7,8 Training the multifidus can be difficult for therapists to teach. However, studies have found that ultrasound guided biofeedback is helpful for patients to learn to contract their multifidus.9,10
Come learn more about the multifidus and how it relates to back pain and stability. In Rehabilitative Ultrasound Imaging: Women's Health and Orthopedic Topics we will go over how to help your patients learn to activate and strengthen their multifidus. Join me on February 28 - March 1st in Raleigh, NC to learn new ways to help your patients!
1. Hides JA, Richardson CA, Jull GA. Multifidus muscle recovery is not automatic after resolution of acute, first‐episode low back pain. Spine 1996;21:2763–2769.
2. Russo M, Deckers K, Eldabe S, et al. Muscle control and non-specific chronic low back pain. Neuromodulation: Technology at the neural interface. 2018; 21 (1): 1-9.
3. D'Hooge R, Hodges P, Tsao H, Hall L, Macdonald D, Danneels L. Altered trunk muscle coordination during rapid trunk flexion in people in remission of recurrent low back pain. J Electromyogr Kinesiol 2013;23:173–181
4. Massé‐Alarie H, Beaulieu L‐D, Preuss R, Schneider C. Corticomotor control of lumbar multifidus muscles is impaired in chronic low back pain: concurrent evidence from ultrasound imaging and double‐pulse transcranial magnetic stimulation. Exp Brain Res 2015; 234:1033–1045.
5. Tsao H, Galea MP, Hodges PW. Driving plasticity in the motor cortex in recurrent low back pain. Eur J Pain 2010;14:832–839.
6. Seminowicz DA, Wideman TH, Naso L et al. Effective treatment of chronic low back pain in humans reverses abnormal brain anatomy and function. J Neurosci 2011;31:7540–7550
7. França FR, Burke TN, Caffaro RR, Ramos LA, Marques AP. Effects of muscular stretching and segmental stabilization on functional disability and pain in patients with chronic low back pain: a randomized, controlled trial. J Manipulative Physiol Ther 2012;35:279–285.
8. Goldby LJ, Moore AP, Doust J, Trew ME. A randomized controlled trial investigating the efficiency of musculoskeletal physiotherapy on chronic low back disorder. Spine. 2006;31:1083–1093.
9. Ghamkhar L, Emami M, Mohseni‐Bandpei MA, Behtash H. Application of rehabilitative ultrasound in the assessment of low back pain: a literature review. J Bodyw Mov Ther 2011;15:465–477.
10. Van K, Hides JA, Richardson CA. The use of real‐time ultrasound imaging for biofeedback of lumbar multifidus muscle contraction in healthy subjects. J Orthop Sports Phys Ther 2006;36:920–925
Ultrasound imaging is being used more frequently in the physical therapy clinical setting. Physical therapists are using ultrasound (US) imaging in varying ways. Some are using it as a training tool for the patient to learn neuromuscular control. Others are using it to guide needle placement while performing dry needling. In a recent article authored by several well-known physiotherapists, the various uses of US imaging were defined, as well as discussions regarding the scope of practice, and training for physiotherapists using ultrasound imaging.
 Four uses of US imaging have been reported by physical therapists. The first and most common use of US imaging is the evaluation of muscle structure and function to aid in neuromuscular control. Essentially, the US images are being used as a source of biofeedback. This has been coined Rehabilitative Ultrasound Imaging (RUSI). Additional uses have emerged in recent years including Diagnostic US imaging which is the diagnosis and monitoring of pathology; and interventional US imaging which is using the US images to guide percutaneous procedures involving dry or wet needling. These three categories are performed during clinical care and fall under the umbrella term “point of care ultrasound.” The last category of US imaging use in physical therapy is paired with performing research.
Four uses of US imaging have been reported by physical therapists. The first and most common use of US imaging is the evaluation of muscle structure and function to aid in neuromuscular control. Essentially, the US images are being used as a source of biofeedback. This has been coined Rehabilitative Ultrasound Imaging (RUSI). Additional uses have emerged in recent years including Diagnostic US imaging which is the diagnosis and monitoring of pathology; and interventional US imaging which is using the US images to guide percutaneous procedures involving dry or wet needling. These three categories are performed during clinical care and fall under the umbrella term “point of care ultrasound.” The last category of US imaging use in physical therapy is paired with performing research.
In this article, some thoughts and areas for improvement were brought to light regarding each type of US imaging as well as the scope of practice and training for each type of US use. It was mentioned that RUSI sits almost entirely within the scope of the physical therapy profession, however, it can be difficult for therapists to receive training for this use. Therapists interested in learning diagnostic or interventional US imaging have more options for training because these uses of US have established criteria for training, competence, and regulation outlined by the World Health Organization (WHO), as well as oversight from the World Federation for Ultrasound in Medicine and Biology. These programs often are intended for other healthcare practitioners (radiologists, and sonographers), but physical therapists are able to take the courses. However, it was stated that both diagnostic and interventional US imaging do not fall within the scope of practice for a majority of physical therapists around the world. So, although training may be more available for these types of US use; therapists taking these courses gain increased experience with non-physical therapy applications, and therefore are at risk for operating outside the scope of their practice.
The authors continued with distinct recommendations for needed training for the four different types of US imaging. Several of the listed skills were fundamental knowledge that a therapist should obtain before utilizing any of the four types of US into their practice such as basic physics for US, terminology, safety, among other knowledge. Then there were skills that were specific to the particular type of US being performed. Since point-of-care use of US is generally not included as part of entry level physical therapy education programs, this knowledge needs to be obtained in a postgraduate education format. For therapists who wish to learn diagnostic application of US imaging, there are multiple courses available from schools that train sonographers. However, according to this article, the form of US imaging that sits more within the scope of practice for physical therapists, rehabilitative ultrasound imaging, does not have as many educational opportunities as diagnostic US imaging does.
Herman & Wallace offers a course that provides fundamental skills of US imaging (such as history, and knowledge of the physics needed for US imaging), as well as specific skills for real-time ultrasound imaging. The schedule of the course includes a lot of lab time with multiple US units available so the ratio of participant to US unit low. You will leave the course being able to interpret US images and use it as an assessment tool or biofeedback tool for the patient. Using RUSI will change how you treat patients! The Rehabilitative Ultrasound Imaging course is offered three more times this year. Join me in Columbia, MO this August; Madison, WI in September; or Chicago, IL in December to learn how to use this form of ultrasound imaging in your clinical practice!
Whittaker J, Ellis R, Hodges P, et al. Imaging with ultrasound in physical therapy: what is the PT’s scope of practice a competency-based educational model and training recommendations. Br. J Sports Med. Apr. 2019; 0:1-7.
Rehabilitative ultrasound imaging has been used in clinical practice for well over a decade now. It has been used for core stabilization, as well as with female incontinence patients. In recent years, transperineal ultrasound imaging has emerged as a useful tool for assessing prolapses and identifying other women’s health issues in the anterior compartment.
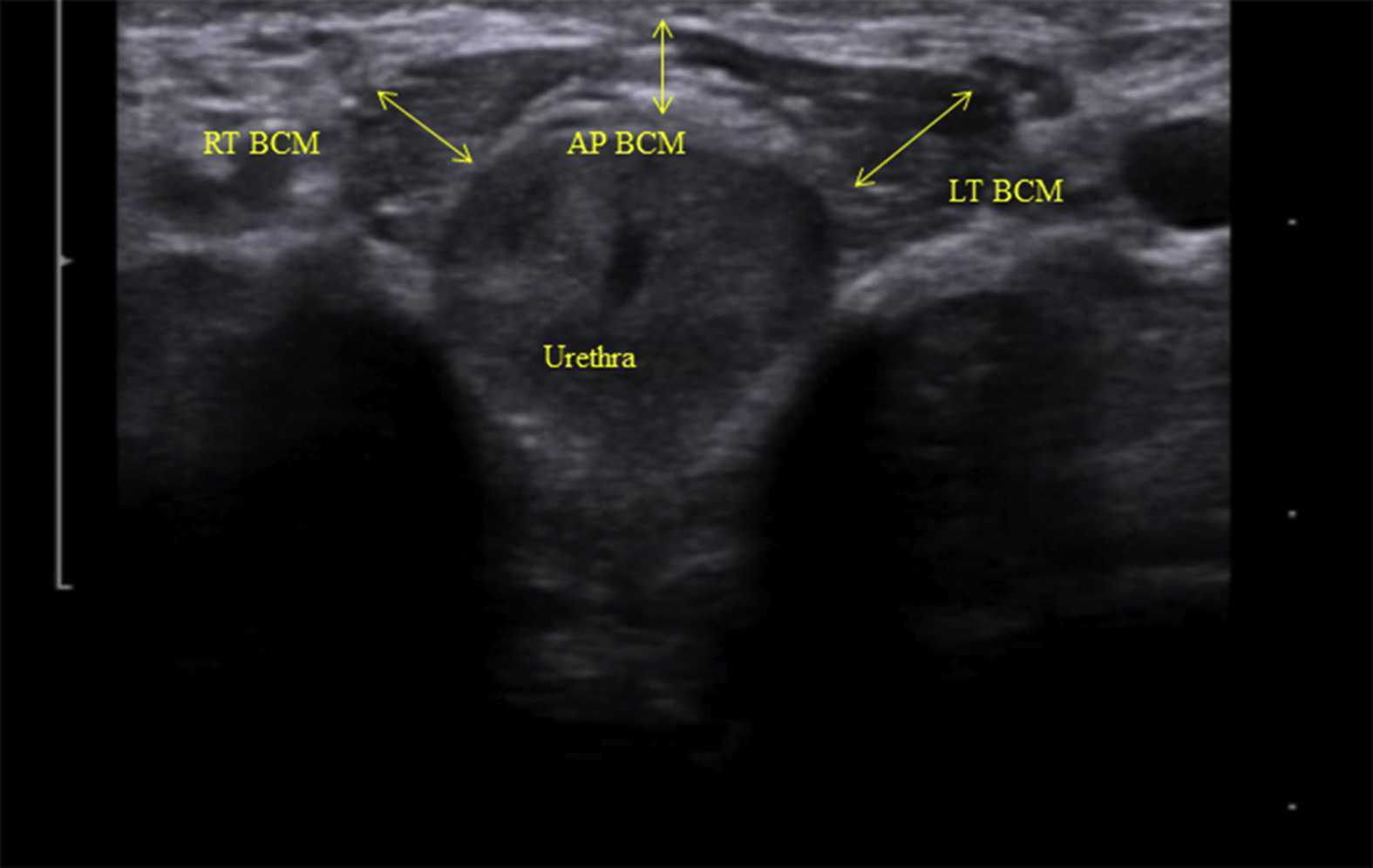
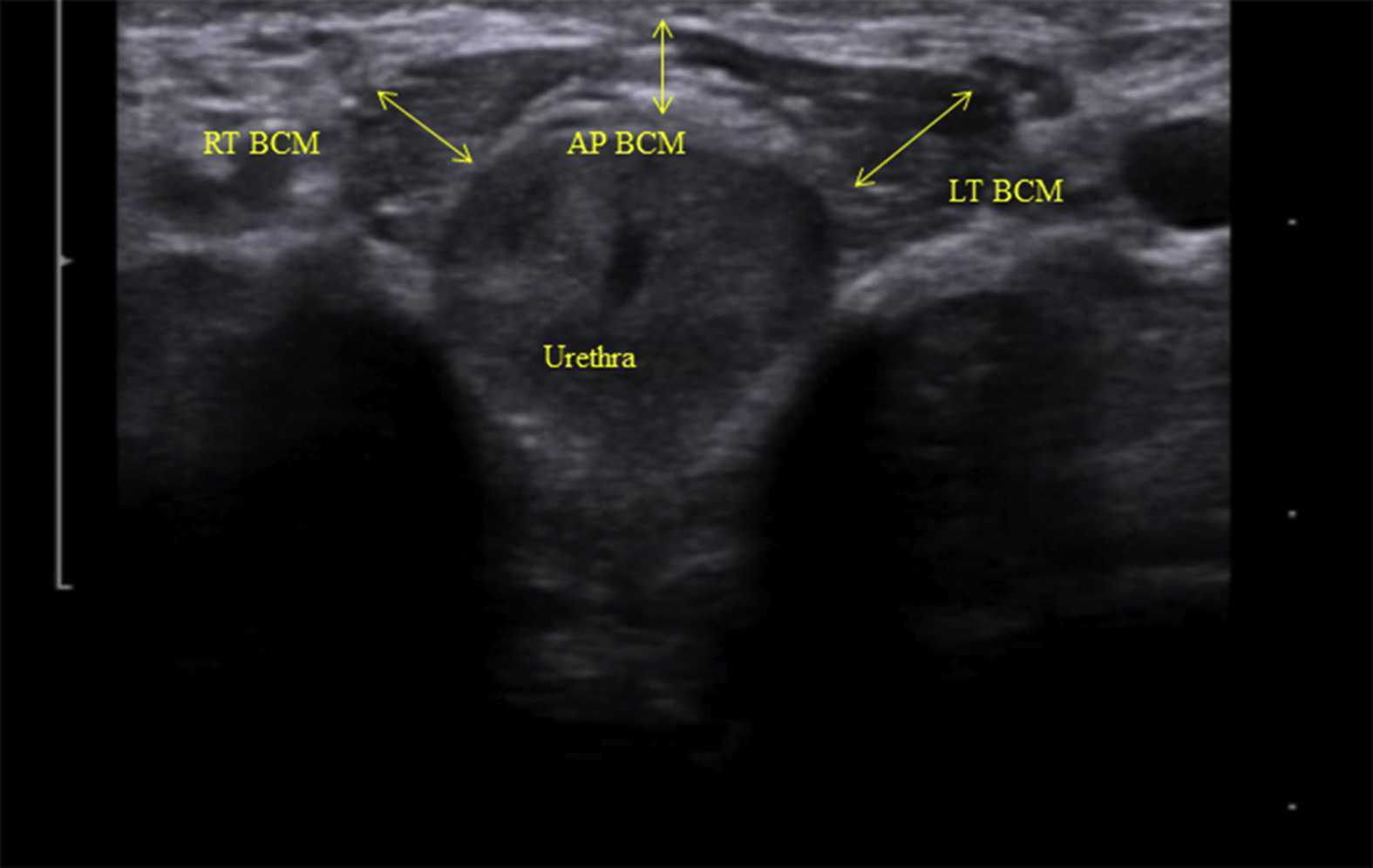 Like other things in men’s pelvic health, the use of ultrasound imaging for rehabilitation has lagged behind that in women’s pelvic health. Ryan Stafford is a researcher that is working to change that. In 2012, Stafford began looking at the normal responses to pelvic floor contractions and what is seen on ultrasound in men. He has since taken his research further to examine differences in men that present with post-prostatectomy incontinence. Stafford, van den Hoorn, Coughlin, and Hodges performed a study looking at the dynamic features of activation of specific pelvic floor muscles, and anatomical parameters of the urethra. The study included forty-two men who had undergone prostatectomy. Some of these men were incontinent and others remained continent. Transperineal ultrasound imaging was used to obtain images of the pelvic structures during a cough, and a sustained maximal contraction. The research team calculated displacements of pelvic floor landmarks with contraction, as well as anatomical features including urethral length, and resting position of the ano-rectal and urethra-vesical junctions.
Like other things in men’s pelvic health, the use of ultrasound imaging for rehabilitation has lagged behind that in women’s pelvic health. Ryan Stafford is a researcher that is working to change that. In 2012, Stafford began looking at the normal responses to pelvic floor contractions and what is seen on ultrasound in men. He has since taken his research further to examine differences in men that present with post-prostatectomy incontinence. Stafford, van den Hoorn, Coughlin, and Hodges performed a study looking at the dynamic features of activation of specific pelvic floor muscles, and anatomical parameters of the urethra. The study included forty-two men who had undergone prostatectomy. Some of these men were incontinent and others remained continent. Transperineal ultrasound imaging was used to obtain images of the pelvic structures during a cough, and a sustained maximal contraction. The research team calculated displacements of pelvic floor landmarks with contraction, as well as anatomical features including urethral length, and resting position of the ano-rectal and urethra-vesical junctions.
The data was analyzed and combinations of variables that best distinguished men with and without incontinence were reported. Several important components were identified in the study. Striated urethral sphincter activation, as well as bulbocavernosus and puborectalis muscle activation were significantly different between men with and without incontinence. When these two parameters were examined together, they were able to correctly identify 88.1% of incontinent men. They further reported that poor function of the puborectalis and bulbocavernosus could be compensated for if the man had good striated urethral sphincter function. However, the puborectalis and bulbocavernosus had less potential to compensate for poor striated urethral sphincter function. This is important for a therapist that works with post prostatectomy patients to know. This can explain part of why some men improve and do so well after a prostatectomy and others don’t, even with therapy to help. If the striated urethra sphincter is damaged and its normal responses are changed during surgery, then incontinence after prostatectomy may be more likely.
Using ultrasound imaging, the therapist can examine and see exactly where a man is deficient in response; whether it is the puborectalis, or the striated urethra sphincter. It is exciting to see this new research and see how rehabilitative ultrasound imaging can influence men’s pelvic health! Come and learn how to use ultrasound imaging for your men’s pelvic health patients as well as your women’s health and back pain patients! You will see how ultrasound imaging can change your practice and how much your patients will enjoy seeing real-time images of their contractions! Thanks to our partnership with The Prometheus Group, this course includes hands-on training on the latest in pelvic ultrasound imaging.
1. Stafford R, Ashton-Miller J, Constantinou C, et al. Novel insights into the dynamics of male pelvic floor contractions through transperineal ultrasound imaging. J. Urol. 2012; 188: 1224-30.
2. Stafford RE, van den Hoorn W, Couglin G, Hodges P. Postprostatectomy incontinence is related to pelvic floor displacements observed with trans-perineal ultrasound imaging. Neurol and Urodyn. 2018; 37:658-665.
Image credit Gupta et al. 2016 https://doi.org/10.1016/j.ajur.2016.11.002 https://www.sciencedirect.com/science/article/pii/S2214388216300881#fig2
Authors: Tamara Rial, PhD, CSPS, Kathleen Doyle-Elmer, PT, DPT and Rebecca Keller, PT, MSPT, PRPC
Tamara Rial, PhD, CSPS, co-founder and developer of Low Pressure Fitness will be presenting the first edition of Low Pressure Fitness and Abdominal Massage for Pelvic Floor Care Level 2 and 3 in Princeton, New Jersey in September, 2019. Rebecca Keller and Kathleen Doyle-Elmer are certified Low-Pressure Fitness specialists with training in rehabilitative ultrasound imaging. In this article, the authors discuss and explore the use of transabdominal ultrasound during Low Pressure Fitness on the abdominal and pelvic floor structures.
Real-time ultrasound imaging is a reliable and valid method to evaluate muscle structure, activity and mobility. Over the past few years, there has been increasing interest in the use of transabdominal ultrasound in the field of rehabilitation. The additional value of ultrasound imaging is that it allows for real-time analysis and visual feedback during the performance of pelvic floor and abdominal exercises (Hides et al., 1998). In the field of pelvic health, this is of notable importance when assessing proper movement of the deep abdominal and pelvic muscles during voluntary muscle actions. Transabdominal ultrasound has been found to be a safe, noninvasive, and accurate method to assess and observe muscular and fascial activity (Khorasani et al., 2012). When therapists learn how to properly use and apply ultrasound imaging, this technique can be a comprehensive tool for the clinician and a comfortable procedure for the patient. Moreover, it may be the method of choice for some patients who don’t want to have an internal pelvic examination (Van Delft, Thakar & Sultan, 2015). In this regard, a cross-sectional study found a moderate-to-strong correlation between ultrasound measurements and both digital examination and perineometry for the assessment of pelvic floor muscle actions (Volløyhaug et al., 2016).
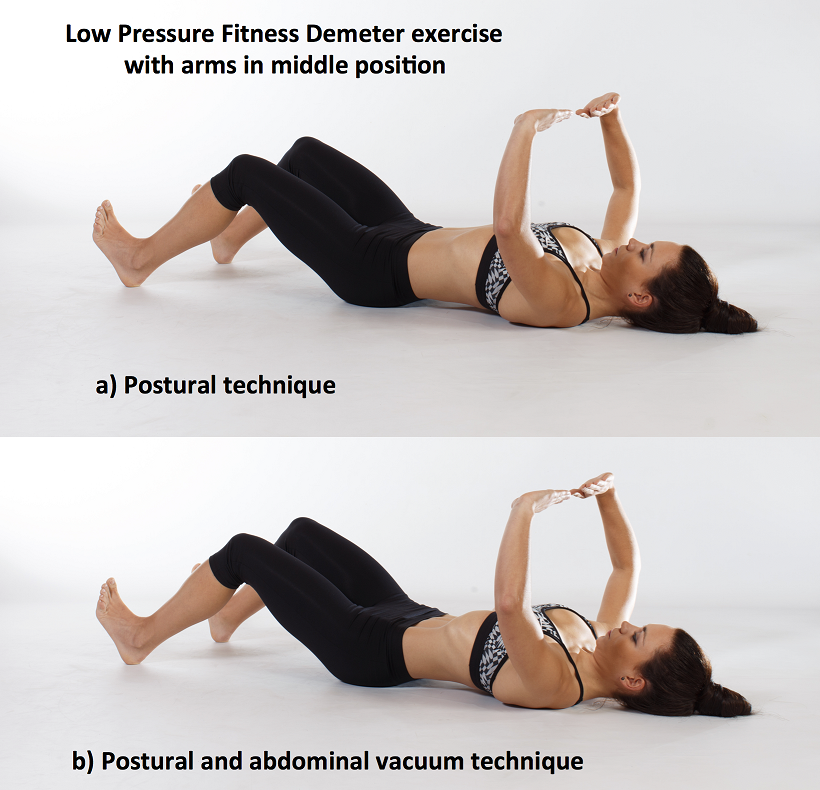
Recently, Low Pressure Fitness has gained popularity as a pelvic floor training program aimed at reducing pressure on the pelvic structures while engaging the stabilizing muscles through postural and breathing exercises. In order to evaluate proper execution of Low-Pressure Fitness exercises as well as abdomino-pelvic muscle function during this type of training, real-time transabdominal ultrasound can be a clinically relevant tool.
Sagittal and Transverse Pelvic Floor/Urinary Bladder Assessment
The amount of movement of the bladder base on transabdominal ultrasound is considered an indicator of pelvic floor muscle mobility during pelvic floor muscle exercises (Khorasani et al., 2012). When properly executed, the Low-Pressure Fitness technique will allow the bladder to lift and the pelvic floor muscles to contract. These observed actions can be cued and progressed due to the real-time imaging biofeedback of the ultrasound. Because of the postural activation and diaphragm lift occurring during Low Pressure Fitness, the bladder fascial support system is tensioned resulting in a desirable bladder lift.
For example, we used a Pathway® Musculoskeletal Rehabilitative Ultrasound Imaging unit with a curvilinear transducer and Prometheus Pathway® rehabilitative ultrasound software utilizing the pre-set parameters (Abdominal Wall 7.5MHz and Bladder 5.0MHz) during a Low-Pressure Fitness basic supine posture. A standardized bladder filling protocol was used before imaging to ensure sufficient bladder filling to allow clear imaging of the base of the bladder and pelvic floor muscles.
For the transverse view, radiologic standards were used, and the ultrasound transducer was placed in the transverse plane suprapubically and angled in a caudal/ posterior direction to obtain a clear image of the inferior-posterior aspect of the bladder. The participant was asked to perform the Low-Pressure Fitness Demeter exercise in the supine position with a neutral pelvis and knees flexed (Figure 1).
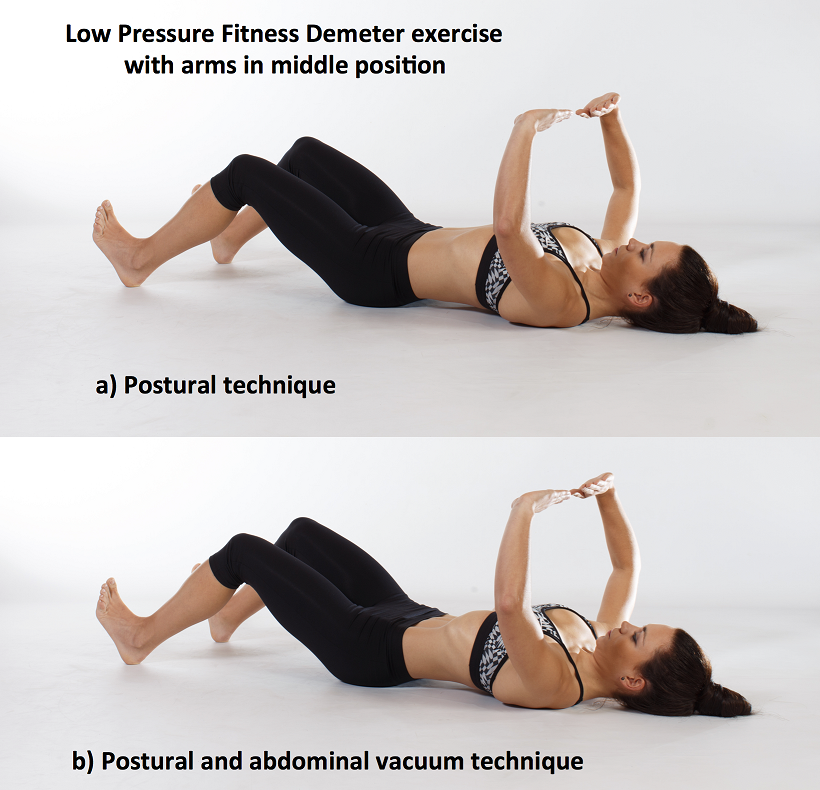
Figure 1. Demeter exercise with postural technique and with postural and abdominal vacuum technique combined.
The following video illustrates the pelvic floor/urinary bladder during: a) resting position; b) active pelvic floor contraction; c) Low Pressure Fitness Demeter exercise and; d) Low Pressure Fitness Demeter exercise combined with a voluntary pelvic floor muscle contraction. It is noticeable a greater bladder lift and pelvic floor activation with the postural and breathing cueing added to an active pelvic floor contraction than with the pelvic floor contraction alone.
Video of the behavior of the pelvic floor muscles in a sagital and transversal view during the supine position of Low Pressure Fitness and with the combination of an active pelvic floor muscle contraction.
Lateral Abdominal Wall Assessment
The lateral abdominal muscle ultrasound assessment allows us to observe the structural changes produced in the transversal section of the abdominal muscles in the midpoint between the anterior iliac crest and the costal angle. At low levels of contraction, the extent of transverse abdominis thickening measured using ultrasound is reported to be a valid method of assessment compared with either fine wire electromyographic measures of transverse activity (McMeeken et al., 2004). It is well established in the scientific literature that the lateral abdominal muscles provide stability to the trunk in different functional activities. Therefore, the assessment of the size, thickness and sliding of the abdominal wall is important for patients who present with lumbo-pelvic and/or pelvic floor dysfunctions. In this regard, patients with low back pain show different abdominal wall muscle activation patterns (i.e. less slide of the abdominal fascia and muscle thickness) than those without low back pain (Gildea et al., 2014; Unsgaard-Tondel et al., 2012).
Figure 2 shows the three muscle layers of the lateral wall in the resting position. The superficial layer corresponds to the external oblique, the middle layer to the internal oblique and the deep layer to the transverse abdominal muscle.
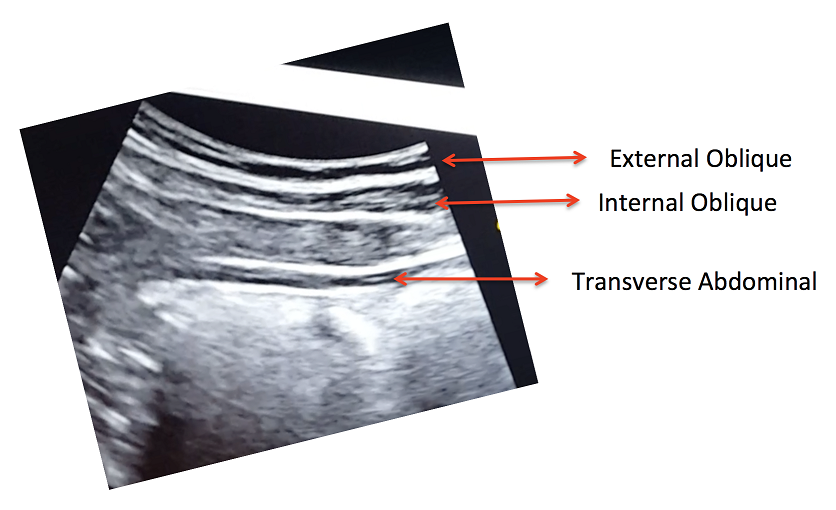
Figure 2. View of the right lateral abdominal wall at rest.
A key breathing component of the Low-Pressure Fitness program is the abdominal vacuum which manipulates intra-abdominal, intra-thoracic and intra-pelvic pressures during the breath-holding phase. Another key aspect of Low-Pressure Fitness is the shoulder girdle activation, spine elongation and ankle-dorsiflexion (Rial & Pinsach, 2017). Of note, previous studies have demonstrated greater transverse abdominis activation when performing ankle dorsi-flexion (Chon et al., 2010). We used transabdominal ultrasound to assess the lateral abdominal wall response during ankle dorsiflexion, shoulder girdle activation and the abdominal vacuum during Low Pressure Fitness.
In the following video, a voluntary (active) abdominal contraction is performed in order to distinguish this action from the involuntary abdominal contractions during Low Pressure Fitness. Afterwards, the postural technique of ankle dorsiflexion and shoulder girdle activation are performed in the Demeter exercise with arms in middle position (Figure 1). Lastly, an abdominal vacuum maneuver is added to the postural technique. If the exercises are properly executed, the progressive sliding and thickness of the abdominal muscles throughout exercise sequence should be observable (Figure 3).
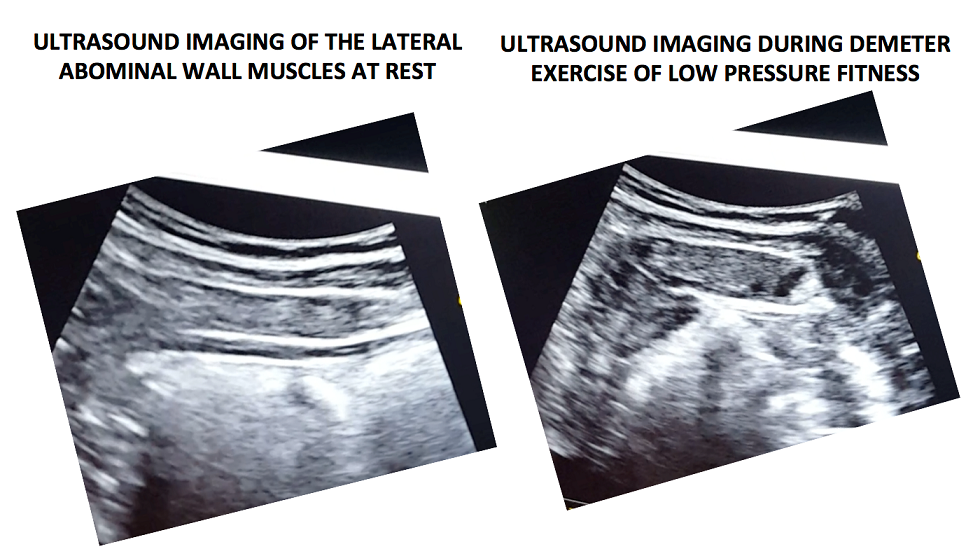
Figure 3. Ultrasound imaging at rest and during the complete LPF technique.
Video of a voluntary (active) abdominal contraction or draw-in maneuver is performed in order to distinguish this action from the involuntary abdominal contractions that occur during Low Pressure Fitness in a supine position
Muscle thickness of the transverse and internal oblique as well as a noticeable slide of the anterior abdominal fascia are observable during the Demeter exercise of Low-Pressure Fitness. This exercise pattern reflects an abdominal draw-in maneuver and a “corseting effect”. In this regard, notice the lateral pull or displacement of the edge of the anterior fascial insertion of the transverse the internal oblique muscle.
Navarro et al., (2017) used transabdominal ultrasound to assess the muscular responses of the pelvic floor and abdominal muscles in a group of women who underwent pelvic physiotherapy over two months. They found a significant increase in the transversal section of the transverse abdominis, external oblique, and internal oblique muscles when compared to resting in the supine position. Similar to the position assessed by Navarro et al. (2017), we also assessed the pelvic floor and abdominal muscle responses during a Low-Pressure Fitness supine exercise.
Transabdominal ultrasound can provide a noninvasive and informative visual biofeedback when training patients with Low Pressure Fitness. This ultrasound imaging can be a valuable tool to both the client and the clinician to objectify progress, assist with validating correct Low-Pressure Fitness form with positioning and vacuum/hypopressive maneuver as well as a motivational technique for the client. As demonstrated during our rehabilitative ultrasound imaging, observable bladder lift, pelvic floor activation and desirable lateral abdominal muscular corseting (slide and thicking) occurs during Low Pressure Fitness postural exercises and breathing. Since Low Pressure Fitness is a progressive exercise program, qualified instruction, technique driven progression and understanding pelvic floor health are needed to optimize patient outcomes.
Chon SC, Chang KY, You JS. Effect of the abdominal draw-in manoeuvre in combination with ankle dorsiflexion in strengthening the transverse abdominal muscle in healthy young adults: a preliminary, randomised, controlled study. Physiotherapy 96: 130-6, 2017.
Gildea JE, Hides JA, Hodges PW. Morphology of the abdominal muscles in ballet dancers with and without low back pain: a magnetic resonance imaging study. J Sci Med Sport. 17(5): 452-6, 2014.
Khorasani B, Arab AM, Sedighi Gilani MA, Samadi V, Assadi H. Transabdominal ultrasound measurement of pelvic floor muscle mobility in men with and without chronic prostatitis/chronic pelvic pain syndrome. Urology, 80: 673-7, 2012.
McMeeken JM, Beith ID, Newham DJ, Milligan P, Critchley DJ. The relationship between EMG and change in thickness of transversus abdominis. Clin Biomech 19: 337–342, 2004.
Hides JA, Richardson CA, Jull GA. Use of real-time ultrasound imaging for feedback in rehabilitation. Man Ther. 3:125-131,1998.
Navarro B, Torres M, Arranz B, Sanchez O. Muscle response during a hypopressive exercise after pelvic floor physiotherapy: Assessment with transabdominal ultrasound. Fisioterapia 39: 187-94, 2017.
Rial T, Pinsach P. Practical Manual Low Pressure Fitness Level 1. International Hypopressive & Physical Therapy Institute, Vigo, 2017.
Unsgaard-Tøndel M, Lund Nilsen TI, Magnussen J, Vasseljen O. Is activation of transversus abdominis and obliquus internus abdominis associated with long-term changes in chronic low back pain? A prospective study with 1-year follow-up. Br J Sports Med, 46(10): 729-34, 2012.
Van Delft K, Thakar R, Sultan AH. Pelvic floor muscle contractility: digital assessment vs transperineal ultrasound. Ultrasound Obstet Gynecol, 45: 217-22, 2015. Volløyhaug I, Mørkved S, Salvesen Ø, Salvesen KÅ. Assessment of pelvic floor muscle contraction with palpation, perineometry and transperineal ultrasound: a cross-sectional study. Ultrasound Obstet Gynecol 47: 768-73, 2016.
 Several weeks ago, I evaluated a patient who was referred to me from a fellow physical therapist. The patient was suffering from sacroiliac joint and low back pain. The patient is a 34-year-old nulliparous woman who is physically fit and participates in several outdoor activities. The therapist had fully evaluated the patient and did not find any articular issues within her spine or pelvis. What she did find was weakness in her local stabilizing muscles and tightness in her global stabilizing muscles. The therapist has an ample amount of clinical experience at treating low back and pelvic pain issues. She is adept at using different verbal cues, positions, and tactile cueing in order to help encourage proper activation of the local core muscles. However, the therapist knew the patient was not getting her local core muscles to fire properly. She didn’t know what else to do with this patient in order to get her to properly activate these muscles. She had tried numerous positions, verbal and tactile cueing without success.
Several weeks ago, I evaluated a patient who was referred to me from a fellow physical therapist. The patient was suffering from sacroiliac joint and low back pain. The patient is a 34-year-old nulliparous woman who is physically fit and participates in several outdoor activities. The therapist had fully evaluated the patient and did not find any articular issues within her spine or pelvis. What she did find was weakness in her local stabilizing muscles and tightness in her global stabilizing muscles. The therapist has an ample amount of clinical experience at treating low back and pelvic pain issues. She is adept at using different verbal cues, positions, and tactile cueing in order to help encourage proper activation of the local core muscles. However, the therapist knew the patient was not getting her local core muscles to fire properly. She didn’t know what else to do with this patient in order to get her to properly activate these muscles. She had tried numerous positions, verbal and tactile cueing without success.
Do you ever have patients where you feel stuck, who are not progressing as you would like them to in treatment? We all do! It is frustrating, isn’t it? The physical therapist called me and asked me to evaluate the patient using real-time ultrasound imaging. The therapist said “If the patient can just see what she is doing, she will then be able to learn how to work the muscles correctly.” She referred the patient to me so I could use ultrasound imaging within the treatment to better assess her activation strategies and use the imaging for biofeedback for with the patient. The patient was amazed with the ability to see what the different layers of muscles were doing. We found she was contracting her TA but only on her left side, and her deep multifidus was not firing at all. Using the ultrasound images, the patient was able to learn the proper way to activate her muscles. She is now working on a strengthening program for her local core muscles including her TA, pelvic floor, and multifidus. Within two treatments, the patient was able to fire her muscles in a different way and reports her back has felt better than it has in years!

The Pathway Ultrasound Imaging System, available from The Prometheus Group, is a portable ultrasound solution for pelvic rehab
I cannot emphasize enough how using ultrasound might change your practice! It not only can help you when you are stuck with a patient’s progress, but it can attract more patients to your practice. There are a lot of visual learners out there and access to visual images in therapy can influence progress and the results that are achieved. You not only can use the ultrasound to retrain the local core muscles for back and pelvic instability patients, but you can use it for incontinence patients, prolapse patients, and post prostatectomy patients as well. You can strengthen the pelvic floor without having to disrobe the patient each visit. How many men and women would appreciate that?
If you are interested in learning more about how you can use ultrasound in your practice, join me in August in New Jersey, or in November in California for Rehabilitative Ultrasound Imaging - Women's Health and Orthopedic Topics! See you there!