Kelley Kukis, DPT, PRPC sat down with The Pelvic Rehab Report this week to discuss herself and how she came to TA for Herman & Wallace.
Who are you? Describe your clinical practice.
I’m Kelley Kukis, DPT, PRPC, and I’m a pelvic PT at East Sacramento Physical Therapy, or East Sac PT as we are referred to locally. East Sac PT has been a pelvic health clinic for over 30 years, and early on the owners, Risa and Jim MacDonald had to educate other medical providers about what pelvic PT was and how it would help their patients. Now the clinic treats adult and pediatric patients of all genders with pelvic dysfunction as well as adult patients with orthopedic conditions.
I also organize the Sacramento Pelvic and Sexual Health Professionals Network (Sac PuSHPiN), which is a network of PTs, MDs, mental health therapists, sex educators, and more, who meet quarterly and share ideas about pelvic and sexual health.
In addition to being a lead TA for Herman & Wallace, I do some guest teaching at my alma mater, California State University, Sacramento (CSUS).
What has your educational journey as a pelvic rehab therapist looked like? Where did you start?
Some of my earliest jobs were movement related. I taught swim lessons, yoga classes, and dance classes in high school and college. I earned a teaching credential and had a career as an elementary teacher for a few years. Unfortunately, I entered teaching in the midst of a difficult economy. As a newer teacher, I was laid off every year due to uncertain education budgets and had to reapply each fall, which became very stressful after 5 years.
I decided to go back to school to be a school PT because as a teacher, I was familiar with rehab in a school setting, but I was pretty naive about what getting into and completing PT school meant. Because I didn’t have a kinesiology degree, I had to take a few years of prerequisite classes while I worked as a dance instructor and professional dancer. I got into the PT program at CSUS and was exposed to the wide variety of settings available for PTs to practice in. When I did a clinical rotation at East Sac PT, I fell in love with pelvic health and never looked back. I took Pelvic Floor 1 as a student in preparation for my clinical rotation, and I completed the rest of the pelvic series after graduation. I earned my PRPC the following year.
How did you get involved in the pelvic rehabilitation field?
One thing that drew me to pelvic rehabilitation was the amount of time we get to spend really getting to know patients. Patients will often tell us things they haven’t told other medical providers, and I love helping patients solve mysteries about their bodies and make new connections. I also love that the little things we do can make a big difference. I gave a constipated patient an abdominal massage, and she returned and called me a “poop doula”.
What patient population do you find most rewarding in treating and why?
I love treating dyspareunia because it’s often something that people have lived with for a long time and thought was either normal or untreatable. I also love working with the LGBTQIA+ community because as a queer person I know that finding queer-competent healthcare providers is more difficult than it should be.
If you could get a message out to physical therapists about pelvic rehab what would it be?
Ask every patient specific questions about their pelvic health. Often patients won’t tell you that they are having incontinence or pelvic pain unless you ask them specifically. These are things that should be screened for at every PT evaluation. PTs also need to get really comfortable asking these questions because if you as the PT are nervous or embarrassed, your patient won’t be honest with you.
What lesson have you learned in a course, from an instructor, or from a colleague or mentor that has stayed with you?
I’ve learned so much from my mentor Risa MacDonald, but one of the most useful things I observed from her is the phrase “you’re right”. She starts nearly every bit of patient education with it, and it’s magic. If you start out telling a patient something they’re right about, they’ll listen to almost anything you have to say after that.
What do you find is the most useful resource for your practice?
I love podcasts. I listen to them while I’m getting ready for work or while I’m working around the house on the weekends. There are so many, but some of the podcasts in my rotation right now are At Your Cervix, Decolonizing Fitness, Foreplay Radio, Pain Science and Sensibility, The Nutrition Diva, The Penis Project, and Tough to Treat. One of my all-time favorite podcasts is Ologies, which is not a pelvic health-specific podcast but which does have some pelvic health-themed episodes, such as “Phallology”, which is what got me hooked.
What is in store for you in the future as a clinician?
I am loving the journey of continuing to learn about different aspects of pelvic health. I’d love to work more in PT education, and I have plans to own a clinic at some point in the future.
What books or articles have impacted you as a clinician?
I’ve just registered for Diane Lee’s ISM series, so I’m working my way back through The Pelvic Girdle and The Thorax right now. Both are such a dense wealth of information that give me new perspectives each time I go through them. I aspire to understand anatomy at as deep a level as Diane Lee.
What has been your favorite Herman & Wallace Course and why?
Megan Pribyl’s Nutrition Perspectives course dramatically changed both the way I eat and the way I talk to patients about nutrition. I recommend it to people every time I TA. I also learned so much in Lila Abbate’s Pudendal Neuralgia course.
What lesson have you learned from a Herman & Wallace instructor that has stayed with you?
I started fermenting things and sprouting grains after taking Megan Pribyl’s course. I’ve also fashioned several pelvic models out of pipe cleaners after taking Jen Vande Vegte’s courses.
What do you love about assisting at courses?
I love meeting other PTs and learning things from them. Our field has so many passionate and talented PTs with so many interesting ideas. It’s also really fun to see how other clinics are set up and run. And even when I’ve TA’ed a course several times, it’s always valuable to hear the material with a new instructor and practice it with a different set of PTs. I learn so many new things each time.
What is your message to course participants who are just starting their journey?
Assume nothing! Even with the most open mind, patients will make you realize the assumptions and biases you’re bringing into the treatment room. Just when you get comfortable, a patient will throw you an absolute curve ball. This is what makes our specialty interesting though!
Bethany Blake, PT, DPT, PRPC sat down with The Pelvic Rehab Report this week to discuss herself and how she came to TA for Herman & Wallace.
Who are you? Describe your clinical practice.
I’m Bethany Blake. I co-own Arkansas Pelvic Health and use social media (@thebladderbaddies previously @thekegelchronicles) to educate about pelvic health.
At Arkansas Pelvic Health we believe everyone should be able to live their life confidently, without pelvic pain or leakage. We believe pelvic therapy should be a standard, not a luxury, and we are on a mission to change this, one pelvis at a time. That's why we started this business, to raise the standard of care in women's health.
As a patient at Arkansas Pelvic Health, you will be paired one-on-one with a Doctor of Physical Therapy, never a tech or computer. You will never be rushed, and your pain and symptoms will be validated. We’re tired of doing things like they've always been done, and we’re tired of women's pain being ignored. We practice evidence-based, patient-centered, compassionate care to get you lasting relief from your pelvic symptoms and get you back to living your life!
What has your educational journey as a pelvic rehab therapist looked like? Where did you start?
I really jumped all in. I took Pelvic Floor Level 1, Pelvic Floor Level 2A, and Pelvic Floor Level 2B all within a month of each other. Very shortly after that, I took a visceral class with Ramona Horton and started teaching courses. I love learning and refuse to settle with not knowing something.
How did you get involved in the pelvic rehabilitation field?
I started my career as an outpatient orthopedic therapist. I picked this site as a clinical rotation because of one therapist in particular, Amanda Brooks-Ritchie. I liked the training that she had and the certifications she was working toward. I had a lot of pregnant and postpartum patients there and worked with a team of pelvic health therapists. Anytime treatment didn’t involve actual vaginal exams, they got “kicked out” to ortho…me. I learned a lot about pelvic health during that time and eventually decided to jump on board the pelvic health ship. I love zooming in and out of the pelvis and bringing the orthopedic background into pelvic health. Soon after I took the courses, I got my PRPC. I realized when studying for that certification, I wanted to merge my orthopedics and pelvic floor, which looked different from how I was practicing at my then-current job. I reached out to a classmate, colleague, and friend, Beth Anne Travis, who had previously approached me about starting a clinic, and told her I was ready to go!
What patient population do you find most rewarding in treating and why?
I love treating pain patients - pelvic pain in general, interstitial cystitis, pudendal neuralgia, and pain with intercourse. It is so rewarding to give people a part of their life back that they hate and to help their bodies work for them instead of against them.
If you could get a message out to physical therapists about pelvic rehab what would it be?
If you suspect pelvic floor issues with your patient, don’t try to manage them yourself. You are potentially doing more harm than good by blindly issuing Kegels and TA contractions. If you aren’t sure, call your friendly neighborhood pelvic PT, and they would be very happy to help you with your patient. I also love the Cozean pelvic floor screening tool.
What lesson have you learned in a course, from an instructor, or from a colleague or mentor that has stayed with you?
Pelvic floor issues are complex. The evaluation is an ongoing process. You won’t know everything for everyone, but you know how to research, you have colleagues you can talk to, and don’t stop trying. Pain is absolutely not part of being a woman.
What do you find is the most useful resource for your practice?
My colleagues. We have a weekly hour where we chat about cases, practice new techniques, and review. It is the best time of the week.
What is in store for you in the future as a clinician?
Arkansas Pelvic Health is growing and expanding. I see opportunities for growth in space and location. I will continue patient care (it’s my favorite part) and also educating the public on social media and through different PT schools.
What books or articles have impacted you as a clinician?
The Interstitial Cystitis Solution
Come As You Are
Headache in the Pelvis
The Body Keeps the Score
Netter’s Anatomy
and many articles!
What has been your favorite Herman & Wallace Course and why?
Pelvic Floor Level 2B is my all-time favorite because I love treating pain conditions. I also really enjoyed the Nutrition Perspectives for the Pelvic Rehab Therapist course.
What lesson have you learned from a Herman & Wallace instructor that has stayed with you?
Progress is not linear!
What do you love about assisting at courses?
I love teaching people about the pelvis, knowing that they will go out and help so many people. I love the updated evidence at the courses, reconnecting with colleagues, and meeting new ones.
What is your message to course participants who are just starting their journey?
Sometimes the load is heavy, but you get stronger, and colleagues help carry it! This is the most rewarding job you will ever have. It is an honor that people let you help them with a vulnerable issue, don’t take it lightly.
Maricel Briones, DPT, CMTPT, OCS sat down with The Pelvic Rehab Report this week to discuss herself and how she came to TA for Herman & Wallace. You can find Maricel this fall TA'ing Pelvic Floor Level 2B in Virginia Beach, VA.
Hi Maricel, can you share a little bit about yourself and your clinical practice?
Hi, I'm Maricel Briones, DPT, CMTPT, OCS and I've lived in Virginia Beach, VA my whole life. I graduated from Old Dominion University with a Bachelor in Exercise Science and followed that up with a Doctorate of Physical Therapy degree. I am now a Partner, Area Director, and Co-Leader of Pelvic Health with Ivy Rehab and have been a practicing therapist since 2012. I became an Orthopedic Clinical Specialist and Certified Myofascial Trigger Point Specialist for Dry Needling and recently became a Pelvic Health Therapist in 2020. My current clinic opened in December 2021, located in the Town Center area of Virginia Beach, VA. We are in the middle of expanding. We are a mix of outpatient orthopedic and pelvic health for men and women. My whole clinic is trained to support each other with all cases, even with pelvic health, and work together as a team for each patient's visit.
What has your educational journey as a pelvic rehab therapist looked like? Where did you start?
I started in early 2020 with Herman & Wallace (H&W) Pelvic Floor Level 1 in Virginia Beach, VA, then continued and took Pelvic Floor Level 2B towards the summer. It started a little slow because of Covid but it picked up in October 2022 and has been very busy since. In 2021, I continued taking more H&W courses including Pelvic Floor Level 2A, Male Pelvic Floor, and Pelvic Floor Capstone. I continued to host around 5-7 H&W courses to review the material and encourage local ortho therapists to join the pelvic health world. I eventually became a teaching assistant (TA) for H&W and have been loving it ever since. I became a Senior TA earlier this year.
How did you get involved in the pelvic rehabilitation field?
My regional director first asked and brought it to my attention, but I declined. A year later, she further explained the impact we can have for patients with pelvic floor conditions and got me convinced. I gave it a shot in 2020 and realized it was where I should be. It's the most rewarding type of treatment we can provide for a patient. We are helping a hidden population that we did not know exists right in front of us. Helping them with critical functions needed in life, voiding, BM, sex, etc.
What patient population do you find most rewarding in treating and why?
Either the pediatric or geriatric population for urinary incontinence (UI). I enjoy teaching them good bladder habits and how to properly contract their pelvic floor muscles. My first patient was an 80-year-old who had urinary incontinence for 20 years and after 1 week of pelvic therapy, she went from changing her pad around 8 times a day to only 2. I had my first pediatric patient who had seen 4 specialists in 1 year for UI. After 2 weeks of pelvic floor rehab, she went from having 4-6 accidents a day to 1-2 every other day.
If you could get a message out to physical therapists about pelvic rehab what would it be?
Don't be afraid of the "V". A lot of PTs are uninterested and do not realize how much pelvic floor muscle training is similar to orthopedic, either stretch it or strengthen it, and provide a lot of education on habits. Also, it's all about functional movement, so connect the pelvic floor with the upper and lower body for optimal outcomes. I did an internal Ivy Rehab Ted Talk in Florida for our Director's Summit in May 2021, titled "Don't be afraid of the 'V'". What you're nervous of or afraid of, may actually be where you are meant to be or do.
What lesson have you learned in a course, from an instructor, or from a colleague or mentor that has stayed with you?
Continue to learn no matter what, and never settle. My treatment programs and assessments evolve every year because of continued learning and advice from colleagues. Always be open to different approaches and be patient with all complex cases.
What do you find is the most useful resource for your practice?
Facebook groups such as Global Pelvic Physio (run by Michelle Lyons), Pelvic PT Newbies (run by Jessica and Andrew Reale), Pelvic PT Huddle (run by PelvicSanity and Nicole Cozean), and Pelvic Floor Biofeedback (run by Tiffany Ellsworth Lee) have been my go-to for learning about cases, ideas, etc.
What is in store for you in the future as a clinician?
I plan to take the PRPC exam soon for board certification. I am also working with Ivy Rehab to create a year-long Pelvic Health Specialization program.
What has been your favorite Herman & Wallace Course and why?
Pelvic Floor Level 2B, since I learned more in-depth manual therapy for the pelvic floor and it helped nail down the anatomy of the pelvic region. I also love the manual therapy skills that we learned in Capstone.
What lesson have you learned from a Herman & Wallace instructor that has stayed with you?
Lengthen before strengthen!
What do you love about assisting at courses?
It's an information refresher. The more you hear it, the more it sticks. I also love teaching the students the concepts and anatomy that were originally confusing for me.
What is your message to course participants who are just starting their journey?
Continue to take more courses on pelvic floor rehab as there are so many different pelvic health conditions. Take the same concepts you learned about muscle training for any body part and apply them to the pelvic region. Connect the pelvic region to the whole body and focus on actively training it with function. It's not just about motor control of the pelvic floor muscles, it's coordinating it with the abdominals, hips, back, etc. Not all visits are hands-on one-on one-on-one. If you create a robust well-rounded program for them and they will progress quicker than you expect.
Aparna Rajagopal, PT, MHS is the lead therapist at Henry Ford Macomb Hospital's pelvic dysfunction program, where she treats pelvic rehab patients and consults with the sports therapy team. Her interests in treating peripartum patients and athletes allowed her to recognize the role that breathing plays in pelvic dysfunction. She has just joined the Herman & Wallace faculty and co-authored the new course, "Breathing and the Diaphragm: Pelvic and Orthopedic Therapists", which helps clinicians understand breathing mechanics and their relationship to the pelvic floor.
Aparna was kind enough to introduce herself to us here on The Pelvic Rehab Report.
 Thank you for your time Aparna! To start, tell us a little bit about yourself.
Thank you for your time Aparna! To start, tell us a little bit about yourself.
My name is Aparna. I’ve been a physical therapist for 22 years. About 16 years ago I switched focus from orthopedics to treating pregnancy and postpartum patients and that’s where my initial interest in pelvic care started. In 2006 following my pregnancy and birth of my daughter, my interest in pelvic care grew with my special interest becoming pelvic pain.
I teach and mentor the pelvic health therapists within the fairly large hospital system that I work at and collaborate with our spine center team and our sports team.
What can you tell us about this new breathing course that is not mentioned in the “course description” and “objectives” that are posted online?
Physical therapy has evolved and continues to evolve as we speak. Regional inter dependence, wherein the different systems interplay, and one structure influences another, is fascinating. No longer is the body considered and treated as independent fragmented pieces. The ‘core’ with the contribution of the Diaphragm and the pelvic floor is so much more than just the Transverse Abdominis and the Multifidus working together. Fascial restrictions of the lower abdomen and the pelvis can influence how the low back feels, thoracic stiffness can influence the interplay between the various abdominal muscles by way on their insertion into the lower ribs, musculo- skeletal pain and postural deviations can stem from incorrect breathing patterns etc.
Normal breathing rate is about 10 times every minute. Breathing incorrectly reinforces wrong movement patterns tens of thousand times a day with negative consequences on the musculoskeletal system.
This course offers an in depth look at the diaphragm from the perspective of both orthopedic and pelvic therapists and attempts to tie in the diaphragm to the thoracic spine, the ribs, the pelvic floor, the core, posture and finally the athlete.
What essential skills does the breath course add to a practitioner’s toolkit?
The practitioner will walk away with the ability to view the patient as a “whole”. It offers a different perspective on neck and back pain, posture/ alignment along with the ability to assess for and connect breathing and the diaphragm to stability/ the core, continence issues and the Autonomic Nervous System.
As therapists we already do a great job of addressing strength issues, assessing and correcting posture, mobilizing etc. You can add to your treatment options by learning how the diaphragm works in concert with other muscles (especially the abdominals) and systems, identifying breathing pattern dysfunctions and postures, and movement patterns which may be linked to breathing pattern dysfunctions. This understanding is beneficial for both orthopedic and pelvic patients.
What inspired you to create this course? What void does this new offering fill?
I have used breathing and evaluation of the diaphragm as a part of pelvic care for several years now. As the mentor for the pelvic program at my hospital, and as a part of the spine team and sports team, I work with pelvic therapists, orthopedic therapists, manual certified therapists, and sports certified therapists. Through my interactions I have come to realize that although many of the therapists are aware that the Diaphragm and breathing are important, they are unsure of how to assess for dysfunctions and address those dysfunctions. I initially started conducting classes within the hospital system. At the same time Leeann who is a sports certified therapist and holds a manual therapy certificate and I started collaborating on our patients. Using a combination of her knowledge and effective manual techniques with my pelvic care and breathing techniques we realized that along with my pelvic patients; our back and neck patients, and her sports patients were all benefitting from this combined approach. We realized along the way that we had information worth sharing with our colleagues that would benefit them in treating their patients, and started classes within the hospital system and that is how this class was born!
What was your process like creating this course?
As a trained pelvic therapist, I have incorporated and used breath and the diaphragm in my treatment for over a decade. Leeann and I have created this course using a combination of our clinical experiences, our education in our respective chosen paths of patient care, and most importantly using recent and relevant research articles from journals to guide us extensively in creating this course.
Breathing and the Diaphragm: Pelvic and Orthopedic Therapists is a new course being offered next March 27-29, 2020 in Sterling Heights, MI, and again on December 11-13, 2020 in Princeton, NJ. It is created and taught by Aparna Rajagopal, PT, MHS and Leeann Taptich, PT, DPT. Come learn how the diaphragm and breathing can affect core and postural stability through intra-abdominal pressure changes. As an integrated approach, the course looks at structures from the glottis and the cervical region to the pelvic floor and helps in understanding a multi component system that works together.
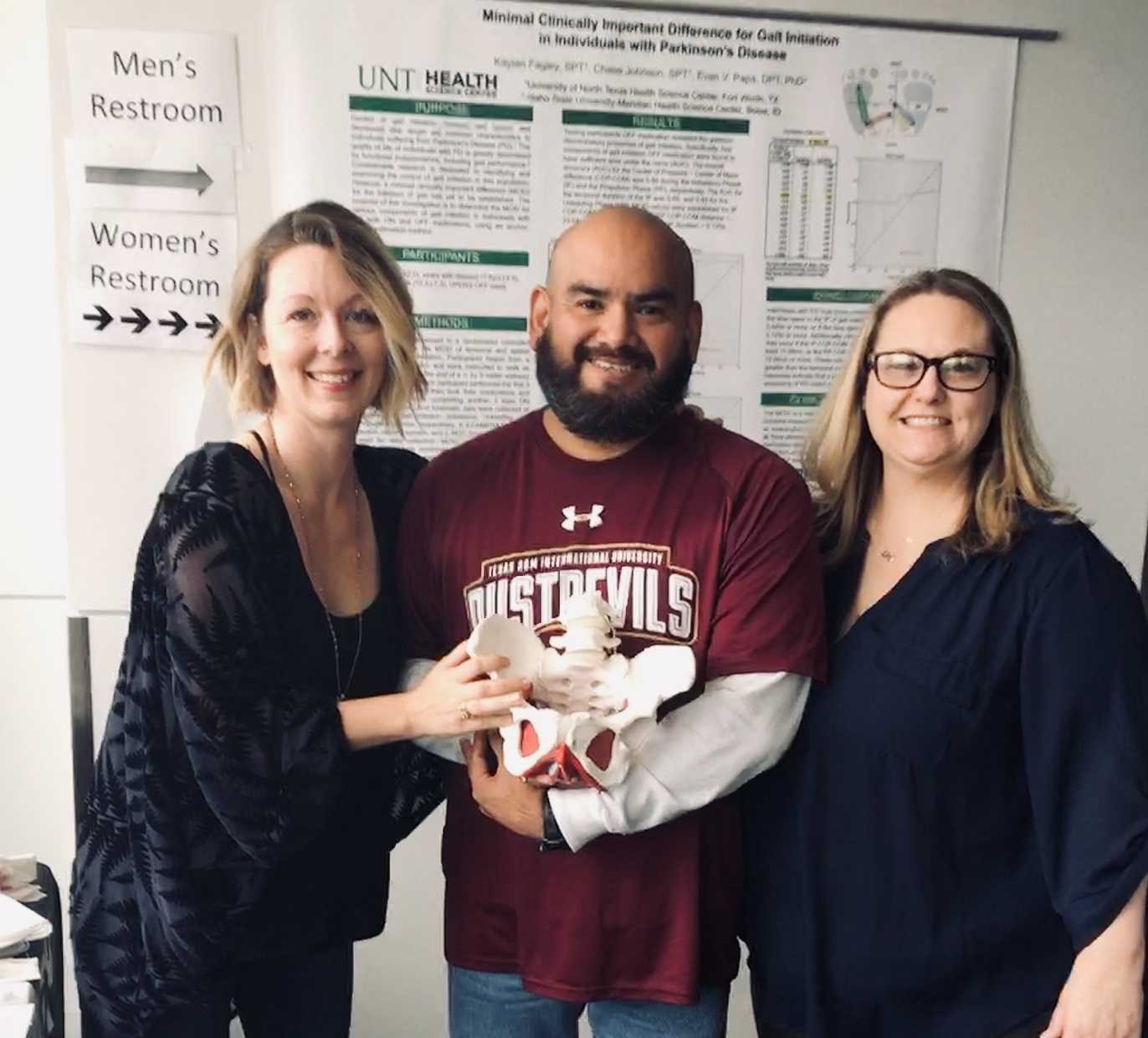
The following is our interview with Jose Antonio (Tony) Rodriguez Jr, COTA. Tony practices in Laredo, TX where he is also studying Athletic Training at the Texas A & M University. He recently attended Pelvic Floor Level 1 and plans to continue pursuing pelvic rehabilitation with Herman & Wallace. He was kind enoguh to share some thoughts about his experiences with us. Thank you, Tony!
Tell us a bit about yourself!
I am a COTA in Laredo where I was born and raised. My goal is to provide pelvic floor therapy to my community. I have been in school for quite some time. I have associate's degrees as a paramedic and occupational therapy assistant. I studied nursing briefly (finished my junior year). My bachelors is in psychology. I’m currently studying athletic training in Texas A & M International University in Laredo. My ultimate academic goal is acquiring my doctorate in physical therapy.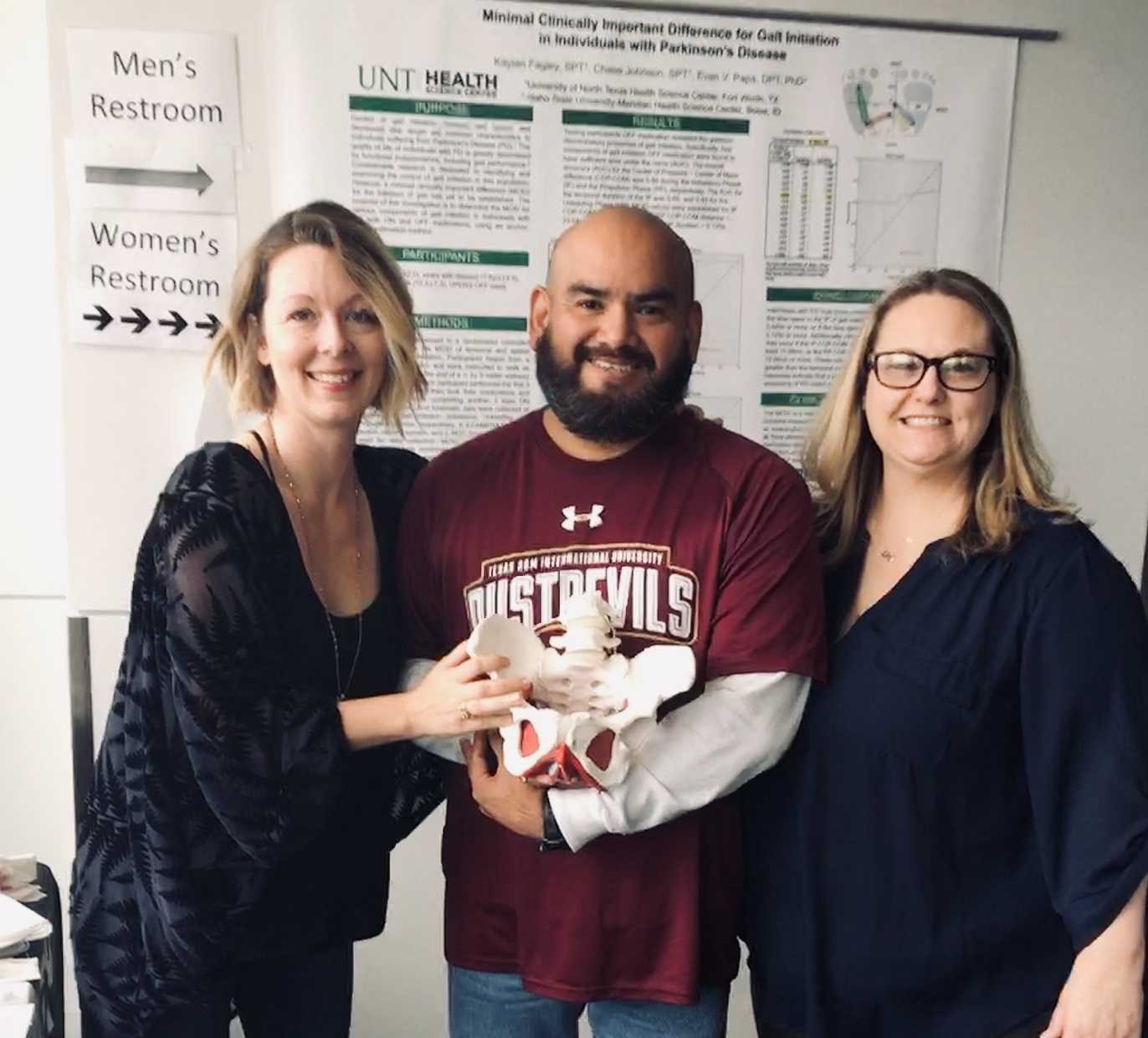
What/who inspired you to become involved in pelvic rehabilitation?
I first came across pelvic floor when reading the description of a CE course where it mentions its relation to SI joint dysfunction so I figured I could use this as a trouble shooting tool for those athletes that had recurrent low back pain or suspected SI problems. I figured at the very least I would know when I was confronted with something that I needed to refer. Little did I know how important of a “puzzle piece” this type of knowledge would become in helping me see a more complete picture of the human body. I was often confronted with athletes that would have recurring lower back pain, hip pain, glute tightness, sciatic nerve pain, adductor tightness or pain, and felt I was missing something to be able to help them. Even with a basic understanding of pelvic floor rehab I was able to help athletes with the previously mentioned complaints. As my understanding grew, I felt it was necessary I take these Herman & Wallace courses so that I could actually treat my patients in a holistic manner.
What is your clinical environment like, and how can you implement pelvic rehab into your practice?
My clinical environment varies between outpatient pediatrics, outpatient geriatrics, and D2 university athletics. I use my pelvic rehabilitation tool box at the university. Mostly I am still learning but I try to screen for and educate my athletes on the important role the pelvic floor muscles play in every activity they carry through out the day. I try to convey the importance not just in sports but also in activities of daily living such as any difficulty with going to the bathroom to pain during sex. I figure the more young people I educate about pelvic floor therapy the better they’ll be to make an informed decision today or later on in life.
Do you feel your background and training as a COTA brings anything unique to your pelvic rehab patients?
I could probably say that my COTA training makes it easier to pick up on some of the behaviors people might be relying on to carry out their day while dealing with pelvic floor issues. They may or may not be aware they have a pelvic floor dysfunction but simply think that’s just how they are. Behaviors such as avoiding social events because such activities don’t fit well with their voiding schedule.
How does your background as a COTA influence your approach to patient care?
My approach as a COTA would force me to see a balance in life. I would have to ask myself all the ways pelvic floor dysfunction may affect my client's daily activities from the basics like voiding, resting, sleep, to enjoying their leisure activities. A person cannot rest adequately if they’re in pain. He or she cannot enjoy social activities being worried of an urge.
What patients or conditions are you hoping to start treating as you continue learning pelvic rehab?
I wish to continue learning and exposing myself to different areas pelvic floor rehabilitation may take me. I wish to look at this therapy through a wide lens. This way I can learn, help many, and keep myself a well-rounded therapist. If in the future I feel more drawn to a specific area I wish to pull from all the different areas I should have learned by then.
What role do you see pelvic health playing in general well-being?
I often tell my athletes that there is probably not a single gross motor movement that doesn’t cross the pelvic region directly or through fascia connection. It is simply how we are built. To try and pretend or ignore the importance of the pelvic floor is just leaving our patients out of the appropriate care they need. And now that I know about the role pelvic floor muscles have in our body it would be unethical not to advocate for my patients’ COMPLETE well-being, pelvic floor muscles included.
What's next for you and your practice?
My short-term goal is acquiring my athletic training state license. After that continue with the last four or five prerequisite classes I need to apply to a DPT program. The DPT is my ultimate goal within the next five or six years.
Adina Leifer, PT, DPT, PRPC recently passed the Pelvic Rehabilitation Practitioner Certification exam and was kind enough to discuss her career with us. Adina Leifer, PT, DPT, PRPC practices at ABLe Pelvic Physical Therapy in Atlanta, GA. Thank you for the interview, Dr. Leifer, and congratulations on earning your certification!
 How did you get involved in the pelvic rehabilitation field?
How did you get involved in the pelvic rehabilitation field?
After graduating from Touro College, and receiving my Doctorate of Physical Therapy. I began to work in an outpatient sports rehab setting. While looking for continuing education courses, I happened upon Herman and Wallace through the Touro College website. They were hosting PF1 at their New York City campus. I knew nothing about pelvic health and rehabilitation at that time. Holly Herman and Tracy Sher taught that first class, after 3 days of class, I was hooked. I knew that pelvic health and wellness was my calling. It has been 9 years since I took that first course and I could not be happier.
What patient population do you find most rewarding in treating and why?
Not sure I can pick one diagnosis or patient population as my favorite. I feel that with each patient that comes to see me, they have either lost ability or do not have normal function of their bladder, bowel or sexual functioning. When I can treat them successfully and educate patients in proper strength and mobility of their pelvic muscles. When I can provide them with the tools so that they can function in their lives, there is nothing more rewarding then that.
Describe your clinical practice:
I currently have my own outpatient practice in Atlanta, GA. I treat adult men and women with any and all pelvic muscle dysfunction and diagnoses.
What has been your favorite Herman & Wallace Course and why?
My favorite course from Herman & Wallace was the capstone course given by Nari Clemons and Jennafer Vande Vegte. I felt this course was informative with practical hands on information for everyday patient treatment. As well as, really helping me to prepare for the PRPC exam.
What motivated you to earn PRPC?
Having practiced for over 9 years and taken many courses through Herman & Wallace, I felt my knowledge and experience made me a specialist. As I was building my own practice, I felt that I wanted the credentials and letters after my name to prove that I was truly a specialist in this field.
What advice would you give to physical therapists interested in earning PRPC?
Go for it! Study the coursework and anatomy. Trust in the knowledge that you have and take the test! You will be very happy that you did.
Certified Pelvic Rehabilitation Practitioners have experience treating a wide variety of pelvic floor dysfunction conditions in men and women throughout the lifecycle. Each certified practitioner has passed a comprehensive exam, and has directly treated pelvic patients for more than 2,000 hours. To learn more about the Pelvic Rehabilitation Practitioner Certification, visit our certification page.
Today we are excited to share an interview with Beth Anne Travis, PT, DPT, PRPC! While Dr. Travis became a certified practitioner in November 2016, she has been plying her trade with pelvic rehab patients specifically since March of 2015, practicing in North Little Rock, AR. Thank you for talking with us, Dr. Travis, and congratulations on the certification!!

Tell us about your practice
Advanced Physical Therapy is an outpatient clinic in North Little Rock, AR where I treat women, men and children with pelvic floor dysfunction and associated orthopedic conditions.
How did you get involved in the pelvic rehabilitation field?
I thought about the pelvic floor rehabilitation in school but took my first job in pediatrics. Soon after accepting the position, I realized it was not what I envisioned and a pelvic floor career opportunity was presented to me. I took Pelvic Floor Level 2B after accepting the pelvic floor position and began treating my first patients a week later. I know this is what the Lord called me to do.
What/who inspired you to become involved in pelvic rehabilitation?
I was inspired by my mentors and how quickly their patients improved within weeks.
What patient population do you find most rewarding in treating?
I truly enjoy treating individuals with pelvic pain. Relieving them of chronic pain they have endured for years and giving them their life back is what I find rewarding.
What has been your favorite Herman & Wallace Course?
Pelvic Floor Level 2B. This was my first course and I took it with very little knowledge of the subject. I had an instructor who helped me the entire time during lab so I could receive the full benefit of the course. It was very important to the instructor that I had complete confidence in what I was learning and doing.
What lesson have you learned from a Herman & Wallace instructor that has stayed with you?
Stacy Futterman advised me during her course to not only focus on the pelvis. So many times we tend to forget to look at the motor control aspect of the body in its entirety.
What do you find is the most useful resource for your practice?
My mentors. I worked with a group of women who have been practicing pelvic floor therapy since 1992. Their knowledge has been incredibly beneficial to me. It’s always comforting to know I have other professionals to brainstorm with.
What motivated you to earn PRPC?
I am continually striving to better myself as a clinician. There was only one certified practitioner in Arkansas who I gratefully had the opportunity to work with. It was my goal to obtain more credibility to improve patient rapport.
What makes you the most proud to have earned PRPC?
Many times in pelvic floor therapy, we are presented with skeptical patients. I use this opportunity to talk with the patient about the course and what it took to gain the certification. I have found that after talking with them, they have more confidence in me. With a lot of studying, hard work and dedication, I have complete faith that I became a better clinician. I am now one of two clinicians with PRPC in the state of Arkansas.
What advice would you give to physical therapists interested in earning PRPC?
It is incredibly beneficial. Studying the information allows you to reflect on information your may have forgotten from PT school
If you could get a message out to physical therapists about pelvic rehabilitation what would it be?
Ask questions! Incontinence and pain with sexual intercourse are very common. If your patient has hip, low back pain or abdominal pain that isn’t improving with orthopedic therapy, refer them to a pelvic floor therapist.
What is in store for you in the future?
It is my goal to become a teaching assistant in the Herman & Wallace courses. I would be honored to teach and inspire others to embrace pelvic floor therapy and what it does to help patients get their life back.
What role do you see pelvic health playing in general well-being?
Pelvic health is vital for our bodies and well-being. Pelvic floor therapy improves the quality of life for so many people. I have personally watched patients get back to the things they loved most before their pelvic health deteriorated.
Lee Sowada, PT, DPT, PRPC is a newly minted Certified Pelvic Rehabilitation Practitioner (PRPC) who treats patients in rural Wyoming. Within her community, she relishes the chance to bring pelvic rehab to a more rural environment and provide care that many people in the community didn't know existed. Dr. Sowada was kind enough to share her story with us. Thanks, Lee, and congratulations on earning your certification!
How did you get involved in the pelvic rehabilitation field?
 I fell into pelvic health rehab by accident as a student when I was placed in a “Women’s Health” rotation at the last minute. Initially I was disappointed as this was my last clinical rotation and among the longest. However, I fell in love with this line of work almost right away. It was evident from the start that pelvic rehab makes an enormous impact on a person’s life in a way that most outpatient rehab doesn’t. The impairments were private and sometimes embarrassing and they often resulted in social isolation and loneliness with the inability to share it and the assumption that nothing could be done. It was so rewarding to provide support, information and much needed treatment. After that, I never looked back.
I fell into pelvic health rehab by accident as a student when I was placed in a “Women’s Health” rotation at the last minute. Initially I was disappointed as this was my last clinical rotation and among the longest. However, I fell in love with this line of work almost right away. It was evident from the start that pelvic rehab makes an enormous impact on a person’s life in a way that most outpatient rehab doesn’t. The impairments were private and sometimes embarrassing and they often resulted in social isolation and loneliness with the inability to share it and the assumption that nothing could be done. It was so rewarding to provide support, information and much needed treatment. After that, I never looked back.
What patient population do you find most rewarding in treating and why?
While I’m continually fascinated and challenged by nearly all pelvic rehabilitation, I really love treating pelvic pain. I love the problem solving and detective work with a required knowledge of urology, gynecology and gastro-intestinal health (along with the musculoskeletal system). I always look at the body as a whole and study functional alignment, myofascial restriction, strength and tone asymmetries, and try to connect the patient with the other appropriate health care providers. I work in a rural area with little access to pelvic health and these patients are always so grateful for any help.
What has been your favorite Herman & Wallace course?
I really enjoyed the Capstone course. I was blown away by all the great minds attending and teaching the course. The discussions were extremely beneficial and the material addressed many of the questions that had developed, including thorough education regarding diet, hormones, inflammation and chronic disease processes. It was very helpful and I left all the more inspired to treat complicated patients.
What motivated you to earn PRPC?
I was motivated to earn the Pelvic Rehabilitation Practitioner Certification (PRPC) for a few reasons. First, there were details about the anatomy, physiology and pharmacology that I had to research, even after thousands of patient care hours. I wanted those details to be very accessible to me in treatments. I found that studying always improved my patient care. I was able to deliver information about current research that I’d forgotten along the way. Secondly, I wanted to be the clear choice for my referral sources. I was proud of my knowledge base and experience but, to many of them, nothing separated me from other PTs who dabbled in pelvic health. I wanted my commitment to this line of work to be obvious.
Interested in becoming a certified pelvic rehabilitation practitioner? The next testing window is May 1 - May 15, 2017. Learn more at https://www.hermanwallace.com/pelvic-rehabilitation-practitioner-certification.
On November 15th, 2016 a new class of Pelvic Rehabilitation Practitioner Certification was crowned! Today we get to celebrate with Andrea Wood, PT, DPT, PRPC from New York. Andrea was kind enough to share some of her thoughts on pelvic rehabilitation and what certification means to her. Thank you Andrea, and congratulations on earning your PRPC credential! Describe your clinical practice:
Describe your clinical practice:
I work in an orthopedic clinical practice that has one on one care which I think is valuable. I joined my practice to help offer another view that included pelvic floor knowledge to various patient cases. My coworkers and I collaborate a lot because we both may see things differently, and exchanging ideas is always invaluable for optimal patient outcomes. I really believe the best health care practitioners can admit when they don’t know everything and seek out other viewpoints to learn.
How did you get involved in the pelvic rehabilitation field?
I actually had no idea I originally wanted to do pelvic floor rehab. I was lucky to fall into it right out of graduate school up in Boston at a wonderful place called Marathon Physical Therapy. I found it fascinating how important it was to consider in a lot of patients, especially those presenting with hip, back, or pelvic pain. Two years into working, I found out I had mild congenital hip dysplasia in my left hip and underwent a periacetabular osteotomy to correct it. Going through the rehab on the other side as a patient and having to experience what it means to practice a lot of the principles I teach patients made me excited to continue to help people overcome obstacles. I’m a better physical therapist now because of my personal history. It taught me to always give patients the means to keep moving within their means and not provide only passive treatments. My two physical therapists that helped me through that became my biggest role models on how to approach complicated patient problems.
What patient population do you find most rewarding in treating and why?
I find it most rewarding to work with pelvic pain patients. I like to think of them as a puzzle. With those patients, I’m an orthopedic physical therapist first, because of how much influence other parts of the body can have on the pelvis. I also am a big advocate of collaborative health care with those patients, and when you bring a team of different views together (i.e. medical doctor, physical therapy, nutritionist, and psychologist to name a few) I find I learn something new each time.
If you could get a message out to physical therapists about pelvic rehabilitation what would it be?
It is not just about 3 layers of muscles in your pelvic floor and Kegels. Your pelvis is a center of your body with various biomechanical, vascular, and neurological influences. For example, erectile dysfunction in males can be influenced by pelvic floor muscle dysfunction, cardiovascular health, and psychological or neurological conditions. A woman with painful intercourse could have various contributing factors ranging from a back or hip problem to a dermatological skin issue. I think physical therapists not properly educated on pelvic floor rehab oversimplify it unknowingly.
What has been your favorite Herman & Wallace Course and why?
My favorite Herman & Wallace course was the Pudendal Neuralgia and Nerve Entrapment. That course opened my eyes up to pain science and how much we really don’t know about pain as a medical community.
What lesson have you learned from a Herman & Wallace instructor that has stayed with you?
That the amount of pain a patient may have does not always signify the amount of damage that is present. When patients realize this, they feel a lot more hopeful and in control.
What do you find is the most useful resource for your practice?
I love learning from other physical therapy blogs. Blog About Pelvic Pain by Sara Saunder and Julie Weibe’s blogs are two of my favorites to follow. I lend the book Pelvic Pain Explained to a lot of my patients.
What motivated you to earn PRPC?
I like to challenge myself, and I felt it was a good test to access areas I need improvement in and should study more or seek out further continuing education.
What makes you the proudest to have earned PRPC?
I’m proud to have earned the PRPC because I earned something that I am passionate about. Some people don’t get that blessing.
What advice would you give to physical therapists interested in earning PRPC?
Just being passionate and asking a lot of questions about what I don’t know in clinical practice provided me with best tools to prepare for the exam.
What is in store for you in the future?
Continuing to learn as much as I can. I plan on seeking out some continuing education in areas of physical therapy like neurology or cardiovascular issues that can all still influence the pelvic floor. I think its important to be a well rounded physical therapist.
Danielle is among the latest class of Certified Pelvic Rehabilitation Practitioners! Her experience treating patients and owning Core 3 Physical Therapy prepared her to pass the exam in flying colors. Read her bio here and check out our interview below. Congratulations, Danielle!
 What/who inspired you to become involved in pelvic rehabilitation?
What/who inspired you to become involved in pelvic rehabilitation?
A patient was the first one to inspire me to improve my knowledge and treatment abilities in pelvic rehabilitation. I was working with a postpartum patient, while carrying my first child, and she felt that my guidance had been so helpful in her care that it made me interested learning more about the pelvic floor. Most of my fellow colleagues could discuss my orthopedic questions but I didn’t have any mentors that could offer advice in more advanced pelvic floor cases so I started attending the Herman and Wallace classes. They have been an invaluable at improving my ability to care for patients with pelvic pain which has even improved my treatment of orthopedic patients with low back pain and sacroiliac dysfunction.
What patient population do you find most rewarding in treating and why?
I enjoy working with chronic pelvic pain patients because it's rewarding to be able to bring relief to someone who has been living with pain, limited quality of life or even social anxiety and has not received any benefit with other treatment options. Being able to help this patient population understand the pelvic floor muscles and function as well as providing justification to why they are in pain and then help them progress through various treatment approaches makes my job rewarding.
If you could get a message out to physical therapists about pelvic rehabilitation what would it be?
PT's are uniquely trained to provided internal pelvic floor muscle release. This is something that no other health care professional is licensed or has the schedule/time to perform. This technique can provide relief and feedback to your patients that is possible in no other way. If you do not want to address this region or feel comfortable providing this treatment, find a therapist local to you who has experience with pelvic floor and refer when appropriate. Additionally, we as physical therapists are often the first line of defense in recognizing and educating patients about the ability to address a wide variety of symptoms that they believe is "just a normal part of life". Asking the in-depth questions and providing a multimodal approach to their symptoms is not only a boon to the patient but to our profession.
What lesson have you learned from a Herman & Wallace instructor that has stayed with you?
"Your most valuable tool is your finger." It is rare to treat an orthopedic patient without incorporating any hands on approach and the same holds true for the pelvic floor. With an internal exam you can make your most accurate assessment while providing valuable feedback to the patient.
What makes you the most proud to have earned PRPC?
I think it has helped me gain respect with my fellow health care professionals for my expertise in the area of pelvic floor treatment. It has broadened my knowledge base and provided me a strong guide for furthering my ability to treat patients with pelvic pain and dysfunction.
What is in store for you in the future?
I would like to become involved in research to further evidence based evaluation and treatment of pelvic conditions. I hope to facilitate the effectiveness and value in pelvic floor rehabilitation via physical therapy.
What role do you see pelvic health playing in general well-being?
It should become a staple for all pelvic floor surgeries just like a physical therapy is the staple post total knee surgery. Currently in my region I find it very underutilized despite the research behind our treatment. This is largely due to the general population not being aware of the treatment benefits physical therapy can play in pelvic dysfunction. European countries make it a standard of care in this area and I hope we progress to adopt a similar view of treatment.