As a small business owner, I’m grateful to have weathered the COVID-19 storm. When reflecting on the 5 year anniversary of the shutdown, I remember how we adapted day after day — masking up, running air filtration systems, and feeling grateful that we could continue to do our work safely. Yet, despite prioritizing sleep, nourishing my body with fresh food, staying active, and hydrating well, I sometimes still feel myself carrying a lingering undercurrent of stress and tension in my physical body.
We have spent years holding our breath—both literally and figuratively. The weight of collective uncertainty, change, and grief may have left some imprints on our bodies. I was reminded of this when a sudden flare of lumbopelvic pain forced me to pay closer attention to my own breath patterns. It became clear that I needed to soften, to release layer by layer of held tension, and to deepen my own breathwork and meditation practice.
As healthcare providers, our work extends beyond addressing physical concerns. We are honored to hold space for our patients' grief—whether it stems from physical trauma, medical challenges, gaslighting, or life's hardships.
They trust us, not just for guidance on optimizing their pelvic health, but as guides on their healing journeys. And yet, we too are human. We experience burnout, fatigue, and emotional strain.
We often teach our patients that breath is a bridge—connecting the nervous system, digestion, spine, pelvic floor, and our emotional state. It is one of the most powerful tools we have to remind the body that it is safe. And yet, even with this knowledge, we may find ourselves unconsciously holding our breath because we are humans living in this unpredictable and sometimes challenging world. When we resist feeling something, we don’t breathe. When we are afraid, we hold tension in our ribs. Even in moments when we think we are relaxed, we can sometimes still be bracing our jaw, back, or pelvic floor.
Let’s take a moment to pause.
Notice your body. Try not to make any adjustments to “fix” your posture.
- Where is your ribcage in relation to your pelvic floor?
- Does the breath feel deep or shallow, smooth, or restricted?
- Where do you sense movement—your chest, ribs, belly?
- What temperature is the air as it enters your nose?
What does it feel like to exhale?
- Does your breath release with ease or feel held back?
- Can you soften just a little more with each out-breath?
- Notice if there is a natural pause before your next inhale—what does that moment of stillness feel like?
If you're sitting, allow yourself to slouch for a moment.
- How does your breath feel in this position?
- Is it shallow or restricted?
- Now, gently imagine your head and spine being drawn upward, as if a magnet is lifting you toward the ceiling. Take another breath. Does it feel different? Notice any shifts in ease of expansion or softening more fully after the exhale.
Now, let’s zoom into the intercostal spaces.
- Imagine this space expanding with each inhale and softening with each exhale.
- Can you soften any more in your ribcage?
- Picture your shoulders softening, warm water is dripping down the upper trap and down the arms.
- Let your jaw unclench, your tongue relax, the space between your eyebrows melt.
Take another long, conscious breath.
- What do you notice?
- Does your body feel a little softer, a little more open, or is there still a place holding tension, waiting for a little more attention?
As practitioners, we give so much to others all day long and sometimes forget to remember to check in with ourselves. Staying connected to our own breath and body serves us just as much as it serves our patients. When we remain grounded and at ease, we can reduce fatigue, physical discomfort, and emotional exhaustion.
So, let’s remind ourselves—throughout the day—to take long easy breaths, soften our jaws, and allow our bodies to move with greater ease. It is not only a gift to ourselves to prevent burn out, but also helps us facilitate co-regulation with our patients’ nervous systems.
If you enjoyed this article, then join Dustienne in her upcoming remote course Yoga for Pelvic Health, on May 3-4, 2025. This two-day remote course offers participants an evidence-based perspective on the value of yoga for patients with chronic pelvic pain and focuses on two of the eight limbs of Patanjali’s eight-fold path: pranayama (breathing) and asana (postures) and how they can be applied for patients who have hip, back and pelvic pain. The course will describe the role of yoga within the medical model, discuss contraindicated postures, and explain how to incorporate yoga home programs as therapeutic exercise and neuromuscular re-education both between visits and after discharge.
AUTHOR BIO
Dustienne Miller PT, MS, WCS, CYT

Dustienne Miller PT, MS, WCS, CYT (she/her) is the creator of the two-day course Yoga for Pelvic Pain and an instructor for Pelvic Function Level 1. Born out of an interest in creating yoga home programs for her patients, she developed a pelvic health yoga video series called Your Pace Yoga in 2012. She is a contributing author in two books about the integration of pelvic health and yoga, Yoga Mama: The Practitioner’s Guide to Prenatal Yoga (Shambhala Publications, 2016) and Healing in Urology (World Scientific). Prior conference and workshop engagements include APTA's CSM, International Pelvic Pain Society, Woman on Fire, Wound Ostomy and Continence Society, and the American Academy of Physical Medicine and Rehabilitation Annual Assembly.
Her clinical practice, Flourish Physical Therapy, is located in Boston's Back Bay. She is a board-certified women's health clinical specialist recognized by the American Board of Physical Therapy Specialties. Dustienne weaves yoga, mindfulness, and breathwork into her clinical practice, having received her yoga teacher certification through the Kripalu Center for Yoga and Health in 2005.
Dustienne's love of movement carried over into her physical therapy and yoga practice, stemming from her previous career as a professional dancer. She danced professionally in New York City for several years, most notably with the national tour of Fosse. She bridged her dance and physical therapy backgrounds working for Physioarts, who contracted her to work backstage at various Broadway shows and for the Radio City Christmas Spectacular. She is currently an assistant professor of jazz dance at Boston Conservatory at Berklee.
Dustienne passionately believes in the integration of physical therapy and yoga within a holistic model of care. Her course aims to provide therapists and patients with an additional resource centered on supporting the nervous system and enhancing patient self-efficacy.
Leeann Taptich DPT, SCS, MTC, CSCS is Co-Author of the new Herman & Wallace offering, Breathing and Diaphragm: Pelvic and Orthopedic Therapist. Leeann leads the Sports Physical Therapy team at Henry Ford Macomb Hospital in Michigan where she mentors a team of therapists. She also works very closely with the pelvic team at the hospital which gives her a very unique perspective of the athlete.
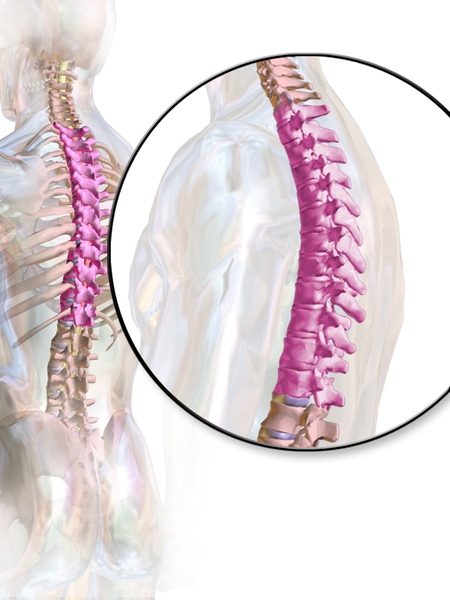
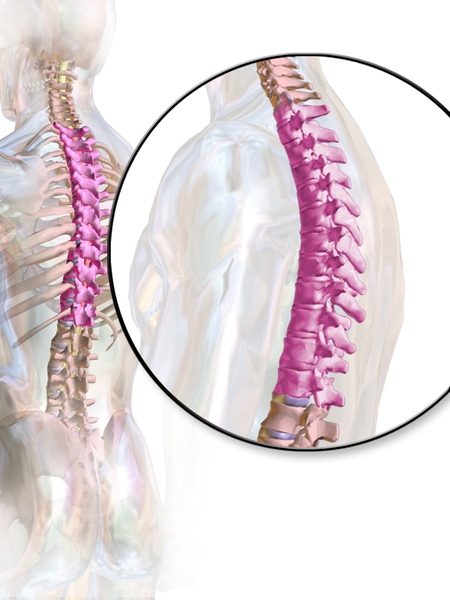 According to a paper from Manual Therapy, the thoracic spine is the least understood part of the spine, despite the huge role it plays in both movement and in regulation of our Autonomic Nervous System.1 Researchers found that the thoracic spine is the least studied of the three spinal regions; thoracic, cervical, and lumbar. I am frequently asked by fellow therapists for help in objectively assessing and treating the thoracic region which has led to the realization that even amongst experienced therapists the thoracic spine’s importance is less understood especially in terms of its function.
According to a paper from Manual Therapy, the thoracic spine is the least understood part of the spine, despite the huge role it plays in both movement and in regulation of our Autonomic Nervous System.1 Researchers found that the thoracic spine is the least studied of the three spinal regions; thoracic, cervical, and lumbar. I am frequently asked by fellow therapists for help in objectively assessing and treating the thoracic region which has led to the realization that even amongst experienced therapists the thoracic spine’s importance is less understood especially in terms of its function.
Anatomically, the thoracic spine along with the ribs and sternum provide a frame that supports and protects the lungs and heart. Despite the rigidity that is required to fulfill that function, the thoracic spine contributes significantly to a person’s ability to rotate.2
One of the biggest roles the thoracic spine plays is in the regulation of the Sympathetic Nervous System, which is a part of the Autonomic Nervous System. The sympathetic nervous system, also known as the “Fight or Flight” system is in overdrive in our patients who present with pain. One of the many complications that arise from an upregulated sympathetic system is increased respiratory rate and/or dysfunctional breathing.3 Carefully applied manual therapy techniques to the thoracic region can help regulate the Autonomic Nervous System by affecting the diaphragm, the intercostals, and other respiratory musculature.4 Specific thoracic mobilizations/manipulations can improve respiratory function.4
In the Breathing and Diaphragm course, Aparna Rajagopal and I discuss the importance of the thoracic spine from both a regional and global perspective. Thoracic spine assessment is taught along with multiple mobilization techniques and manipulations all of which will help the clinician link the thoracic spine to the treatment of pelvic pain, low back pain, and breathing pattern disorders. Join Aparna and I in either Sterling Heights, MI this March or Princeton, NJ in December for Breathing and the Diaphragm: Pelvic and Orthopedic Therapists: From Assessment to Clinical Applications for Pelvic and Orthopedic Therapists!
1. Heneghan NR, Rushton A. Understanding why the thoracic region is the ‘Cinderella’ region of the spine. Man Ther. 2016; 21: 274-276.
2. Narimani M, Arjamand N. Three-dimensional primary and coupled range of motions and movement coordination of the pelvis, lumbar, and thoracic spine in standing posture using inertial tracking device. Journal of Biomechanics. 2018; 69: 169-174.
3. Bernston GG. Stress effects on the body: Nervous system. American Psychological Association. https://www.apa.org/helpcenter/stress/effects-nervous. January 18, 2020.
4. Shin DC, Lee YW. The immediate effects of spinal thoracic manipulation on respiratory functions. Journal of Physical Therapy Science. 2016; 28: 2547-2549.
Aparna Rajagopal, PT, MHS is the lead therapist at Henry Ford Macomb Hospital's pelvic dysfunction program, where she treats pelvic rehab patients and consults with the sports therapy team. Her interests in treating peripartum patients and athletes allowed her to recognize the role that breathing plays in pelvic dysfunction. She has just joined the Herman & Wallace faculty and co-authored the new course, "Breathing and the Diaphragm: Pelvic and Orthopedic Therapists", which helps clinicians understand breathing mechanics and their relationship to the pelvic floor.
Aparna was kind enough to introduce herself to us here on The Pelvic Rehab Report.
 Thank you for your time Aparna! To start, tell us a little bit about yourself.
Thank you for your time Aparna! To start, tell us a little bit about yourself.
My name is Aparna. I’ve been a physical therapist for 22 years. About 16 years ago I switched focus from orthopedics to treating pregnancy and postpartum patients and that’s where my initial interest in pelvic care started. In 2006 following my pregnancy and birth of my daughter, my interest in pelvic care grew with my special interest becoming pelvic pain.
I teach and mentor the pelvic health therapists within the fairly large hospital system that I work at and collaborate with our spine center team and our sports team.
What can you tell us about this new breathing course that is not mentioned in the “course description” and “objectives” that are posted online?
Physical therapy has evolved and continues to evolve as we speak. Regional inter dependence, wherein the different systems interplay, and one structure influences another, is fascinating. No longer is the body considered and treated as independent fragmented pieces. The ‘core’ with the contribution of the Diaphragm and the pelvic floor is so much more than just the Transverse Abdominis and the Multifidus working together. Fascial restrictions of the lower abdomen and the pelvis can influence how the low back feels, thoracic stiffness can influence the interplay between the various abdominal muscles by way on their insertion into the lower ribs, musculo- skeletal pain and postural deviations can stem from incorrect breathing patterns etc.
Normal breathing rate is about 10 times every minute. Breathing incorrectly reinforces wrong movement patterns tens of thousand times a day with negative consequences on the musculoskeletal system.
This course offers an in depth look at the diaphragm from the perspective of both orthopedic and pelvic therapists and attempts to tie in the diaphragm to the thoracic spine, the ribs, the pelvic floor, the core, posture and finally the athlete.
What essential skills does the breath course add to a practitioner’s toolkit?
The practitioner will walk away with the ability to view the patient as a “whole”. It offers a different perspective on neck and back pain, posture/ alignment along with the ability to assess for and connect breathing and the diaphragm to stability/ the core, continence issues and the Autonomic Nervous System.
As therapists we already do a great job of addressing strength issues, assessing and correcting posture, mobilizing etc. You can add to your treatment options by learning how the diaphragm works in concert with other muscles (especially the abdominals) and systems, identifying breathing pattern dysfunctions and postures, and movement patterns which may be linked to breathing pattern dysfunctions. This understanding is beneficial for both orthopedic and pelvic patients.
What inspired you to create this course? What void does this new offering fill?
I have used breathing and evaluation of the diaphragm as a part of pelvic care for several years now. As the mentor for the pelvic program at my hospital, and as a part of the spine team and sports team, I work with pelvic therapists, orthopedic therapists, manual certified therapists, and sports certified therapists. Through my interactions I have come to realize that although many of the therapists are aware that the Diaphragm and breathing are important, they are unsure of how to assess for dysfunctions and address those dysfunctions. I initially started conducting classes within the hospital system. At the same time Leeann who is a sports certified therapist and holds a manual therapy certificate and I started collaborating on our patients. Using a combination of her knowledge and effective manual techniques with my pelvic care and breathing techniques we realized that along with my pelvic patients; our back and neck patients, and her sports patients were all benefitting from this combined approach. We realized along the way that we had information worth sharing with our colleagues that would benefit them in treating their patients, and started classes within the hospital system and that is how this class was born!
What was your process like creating this course?
As a trained pelvic therapist, I have incorporated and used breath and the diaphragm in my treatment for over a decade. Leeann and I have created this course using a combination of our clinical experiences, our education in our respective chosen paths of patient care, and most importantly using recent and relevant research articles from journals to guide us extensively in creating this course.
Breathing and the Diaphragm: Pelvic and Orthopedic Therapists is a new course being offered next March 27-29, 2020 in Sterling Heights, MI, and again on December 11-13, 2020 in Princeton, NJ. It is created and taught by Aparna Rajagopal, PT, MHS and Leeann Taptich, PT, DPT. Come learn how the diaphragm and breathing can affect core and postural stability through intra-abdominal pressure changes. As an integrated approach, the course looks at structures from the glottis and the cervical region to the pelvic floor and helps in understanding a multi component system that works together.
As so many of our patients are shallow breathers, I found this research on the effects of mindful attention to the breath (MATB) on prefrontal cortical and amygdala activity especially informative and relevant to patient care. Twenty-six healthy volunteers with no prior meditation experience were introduced to MATB by an experienced meditation teacher and instructed to practice a 20-minute audio guided MATB meditation daily for 2 weeks.1 At the end of the 2-week training period, subjects underwent fMRI scanning while viewing distressing emotional images with MATB and with passive viewing (PV). Participants were shown aversive pictures or no pictures and were instructed to “Please focus your attention on your breath as you were instructed in the training” or “Please watch the picture without changing anything about your feelings.” Subjects indicated their current affect on a 7 point scale ranging from -3 (very negative) to +3 (very positive).
Breathing frequency significantly decreased during MATB compared to PV. Researchers controlled for this by including breathing frequency as a covariate in further behavioral and brain data analysis.
Analysis of affective ratings showed that participants felt significantly less negative affect when viewing distressing visual stimuli during MATB than PV. During negative visual stimuli, MATB significantly decreased bilateral amygdala activation compared to PV. Also, right amygdala activation decrease specifically correlated with successful emotional regulation. That is, those participants with greater reductions in right amygdala activation reported greater reductions in aversive emotions during the MATB. In addition, emotion-related functional connectivity increased between the prefrontal cortex and amygdala during the viewing of negative images and MATB.
It’s exciting to have some initial science behind the benefits of MATB. I teach all of my patients MATB and have found it rewarding to get feedback from participants in my courses about their integration of MATB into their own patient care. Patients with complex pain conditions can be challenging to treat, however sometimes a simple practice of taking 2 to 3 minutes prior to and/or at the end of a treatment to have a patient calmly focus on their breath with the mindful attitudes of acceptance, kindness and curiosity can help a person shift from tension and distress to calm and confidence. I look forward to presenting this and additional research on the impact of mindful meditation on brain structure and function in my upcoming course, Mindfulness-Based Pain Treatment, in Seattle, November 4 and 5. Hope to see you there!
1. Doll A, Holzel BK, Bratec SM, et al. Mindful attention to breath regulates emotions via increased amygdala-prefrontal cortex connectivity. Neuroimage. 2016;134:305-313.