This week The Pelvic Rehab Report sat down with some of our favorite Occupational Therapists to discuss the role of OTs in the field of pelvic rehabilitation. The following blog is provided by Tiffany Ellsworth Lee MA, OTR, BCB-PMD, PRPC, Lindsey Vestal, MS, OT, and Laura Rowan OT/L.
Most people associate pelvic health with PTs- so many are surprised to see OTs in this specialty. Herman and Wallace faculty and instructor Tiffany Ellsworth Lee MA, OTR, BCB-PMD, PRPC, LPF-CT has been an OT for 28 years and has spent the last 20 years specializing in pelvic health. She recalls, “My first Herman and Wallace course was PF1 11 years ago. I was the only OT in a class of 50. I was so appreciative of H&W’s foresight to include OTs in the course offerings. A PT sat down next to me and said, “Why are you here? I didn’t know OTs could treat pelvic health!” Yes, we can! It is within our scope of practice and the majority of therapist specialized learning comes post-graduation.
Lindsey Vestal, OTR/L has been an OT for 11 years and her private practice focuses on pre and postnatal people. She is a moderator of the Facebook group “OTs for Pelvic Health” with over 3,100 members. She is bringing awareness to the PH specialty by educating OTs on the best way to treat and collaborate with PTs and other providers in the field. She says, “ Just as OTs and PTs work side-by-side in other fields of rehab, there's a huge need for us to work collaborating in pelvic health. In grad school, OTs study motivational interviewing, nonverbal communication, we have mental health classes and a strong background in sensory approaches, energy conservation, self-regulation strategies, the involvement of the nervous system, time management, working with trauma, habits, routines, ADLs, the musculoskeletal system, functional movement, and activity grading. Pelvic floor function is a crucial part of a much broader functional task of toileting and intimacy, both of which have broader connections within a person’s emotional, cognitive, and social abilities. It's also important to consider the social implications for people with pelvic floor issues such as withdrawal from social and recreational activities, social isolation, disempowerment, lack of self-esteem, anxiety, depression, and the impact on close relationships such as with our spouse, our friends, and our children. This OT-specific background has given me a great foundation to serve my PF population.”
Another seasoned PHOT is Laura Rowan, OT/L who has been an OT for 21 years and the last 14 years has dedicated her practice to pelvic health. She works with all gender diversities across the lifespan with a focus on complex pain patients and athletes. Laura provides manual therapy courses and mentorship for OTs starting in this specialty. She says, “OTs are great at analyzing how the client is executing functional tasks and offering new strategies, adaptations, and compensation techniques for a less provoking and safer way to accomplish the task at hand. OT’s will often see progress using a whole person approach where a client may have plateaued with a less holistic treatment plan”

Laura shares about her start in the PH journey - “My success did not come without challenges. The vast majority of PTs did not share the same acceptance of OTs as Herman and Wallace. Due to a lack of understanding that continues to exist today, OTs struggle to begin their career in pelvic health. It took me 8 years after PF1 to officially break into the field. I felt like a lone OT in a PT world due to the lack of OT presence and support. I didn’t understand the roadblocks I was facing as pelvic health seemed a natural fit for OTs. OT practitioners have long been lending our expertise in the areas of functional restoration, psychosocial considerations, behavioral modifications, time management, stress management, coping strategies, and task analysis. These are major components of a comprehensive plan of care for individuals with pelvic health dysfunction in relation to their Activities of Daily Living (ADL’s) and Instrumental Activities of Daily Living (IADL’s). I am thankful for the many PTs that mentored me along the way. I was hired by a PT clinic with mentorship and continuing education opportunities. This provided strong foundations for me to later branch out and start a successful private practice. I have further developed into an educator and mentor role to provide the emerging OT practitioners the support I received starting out but through the unique lens of an OT.”
Tiffany adds, “OTs and PTs working collaboratively is a winning combination. We can share patients and focus on treating the whole person. For example, a patient with constipation, dyspareunia, SI dysfunction, and urinary incontinence can work with both OT and PT. I may address their constipation and UI using behavioral therapy, biofeedback, and lifestyle modifications while my PT co-worker addresses the spine, hip, and back dysfunction. If you work in an outpatient setting, you are able to bill separately and treat the same patient. We are taking the same courses side-by-side and learning the same skills. Our backgrounds are diverse and we can serve our patients with a multidisciplinary approach. Instead of being divisive and noninclusive, we should be supporting each other and collaborating. There is plenty of business to go around and PH therapists are some of the most compassionate and empathetic people I have ever met!”
Laura agrees and says, “Pelvic Health is too large of a specialty to be a generalist and have all the answers. It’s always beneficial to have a second set of eyes and even better to have a diverse background for a comprehensive whole-person approach to client-centered care. It’s not about the therapist and their discipline, rather taking a multisystem approach to meet the needs of our clients and how we can better serve them with an interdisciplinary team. We often run out of time to address all of the underlying impairments contributing to the client’s symptoms. OTs and PTs working together allow for all of the contributing factors to be addressed with the appropriate amount of attention required for successful outcomes.”

Lindsey chimes in, “It can take a village to care for pelvic health clients, so why not lean on our colleagues for their areas of strength? I mean isn’t that why we are rehab professionals? To ultimately serve our clients the best way possible? Pelvic health is a very underserved population and in my opinion, there's space for us all.”
Tiffany, Lindsey, and Laura have thriving private practices serving the PH population and each has PH continuing education companies that offer courses and mentoring. They are passionate about spreading awareness of the OT's role in pelvic health and the many benefits of working alongside PTs to meet the needs of this underserved population. By bridging the gap in understanding the valuable role of the PHOT, we can start to decrease extensive waitlists, and open up jobs to qualified passionate OT’s eager to begin their pelvic health careers. You can reach them through email -
tiffany@tiffanyleeot.com or www.pelvicfloorbiofeedback.com
laura@essentialpelvichealth.com or www.essentialpelvichealth.com
lindseyvestal@functionalpelvis.com or www.functionalpelvis.com
The world needs more clinicians who can treat pelvic pain, pelvic organ prolapse, urinary incontinence, diastasis recti, and the many other conditions that constitute pelvic floor/pelvic girdle dysfunction. Most clinicians who specialize in pelvic rehabilitation are Physical Therapists (PT) or Occupational Therapists (OT), though other licenses also allow you to work with patients who have pelvic floor dysfunction. Many doctors, nurses, and internationally licensed medical professionals are beginning to explore the field of pelvic rehabilitation.
In an interview for the Pelvic Rehab Report, faculty and instructor Tiffany Ellsworth Lee MA, OTR, BCB-PMD, PRPC, shared that "Occupational therapists wishing to pursue pelvic floor have a few options. The first thing is to find a pelvic floor clinical setting...or check to see if they can start a women's health program with a strong focus on the pelvic floor. OTs quite often do not start out in pelvic health directly after school. Since this is a newer area as compared to other certifications such as the NDT and PNF, it takes a little bit of research, time, and effort to find one’s exact niche. To get started, an OT should seek out courses that teach the basics of bladder and bowel management. It is important to understand the anatomy and physiology of the bladder, bowel, and sexual systems."
Once you have a license to practice, you can start learning to specialize in pelvic rehabilitation. The best place to start is with the H&W Pelvic Floor Level 1 satellite lab course, which offers immediately applicable clinical skills for evaluating and treating urinary incontinence or the musculoskeletal components of urogynecologic pain syndromes. Most practitioners who take Pelvic Floor 1 return to study in the next courses in the series.
You can learn all about the colorectal system, and how to treat conditions such as coccyx pain, pudendal neuralgia, and male pelvic pain in the Pelvic Floor 2A course, and in Pelvic Floor 2B you can expand your knowledge in topics such as movement assessment and re-training, prolapse, and pelvic pain. Then in the Pelvic Floor Capstone course, the final advanced course, you dive deep into topics such as hormones and their influence on conditions, surgeries and recovery, and skilled manual therapy techniques. Once you know your patient demographic, you can check out our growing list of specialty courses that include series topics including yoga, oncology, pregnancy, fascial mobilization, and much more.
Once you have gained experience in the field, you may consider sitting for the Pelvic Rehabilitation Practitioner Certification (PRPC). This certification recognizes expertise in pelvic rehabilitation for patients of all genders throughout the lifecycle. To be eligible to sit for the exam, applicants must have completed 2000 licensed hours of direct pelvic patient care in the past eight years, 500 of which must have been in the last two years.
The following is our interview with Jose Antonio (Tony) Rodriguez Jr, COTA. Tony practices in Laredo, TX where he is also studying Athletic Training at the Texas A & M University. He recently attended Pelvic Floor Level 1 and plans to continue pursuing pelvic rehabilitation with Herman & Wallace. He was kind enoguh to share some thoughts about his experiences with us. Thank you, Tony!
Tell us a bit about yourself!
I am a COTA in Laredo where I was born and raised. My goal is to provide pelvic floor therapy to my community. I have been in school for quite some time. I have associate's degrees as a paramedic and occupational therapy assistant. I studied nursing briefly (finished my junior year). My bachelors is in psychology. I’m currently studying athletic training in Texas A & M International University in Laredo. My ultimate academic goal is acquiring my doctorate in physical therapy.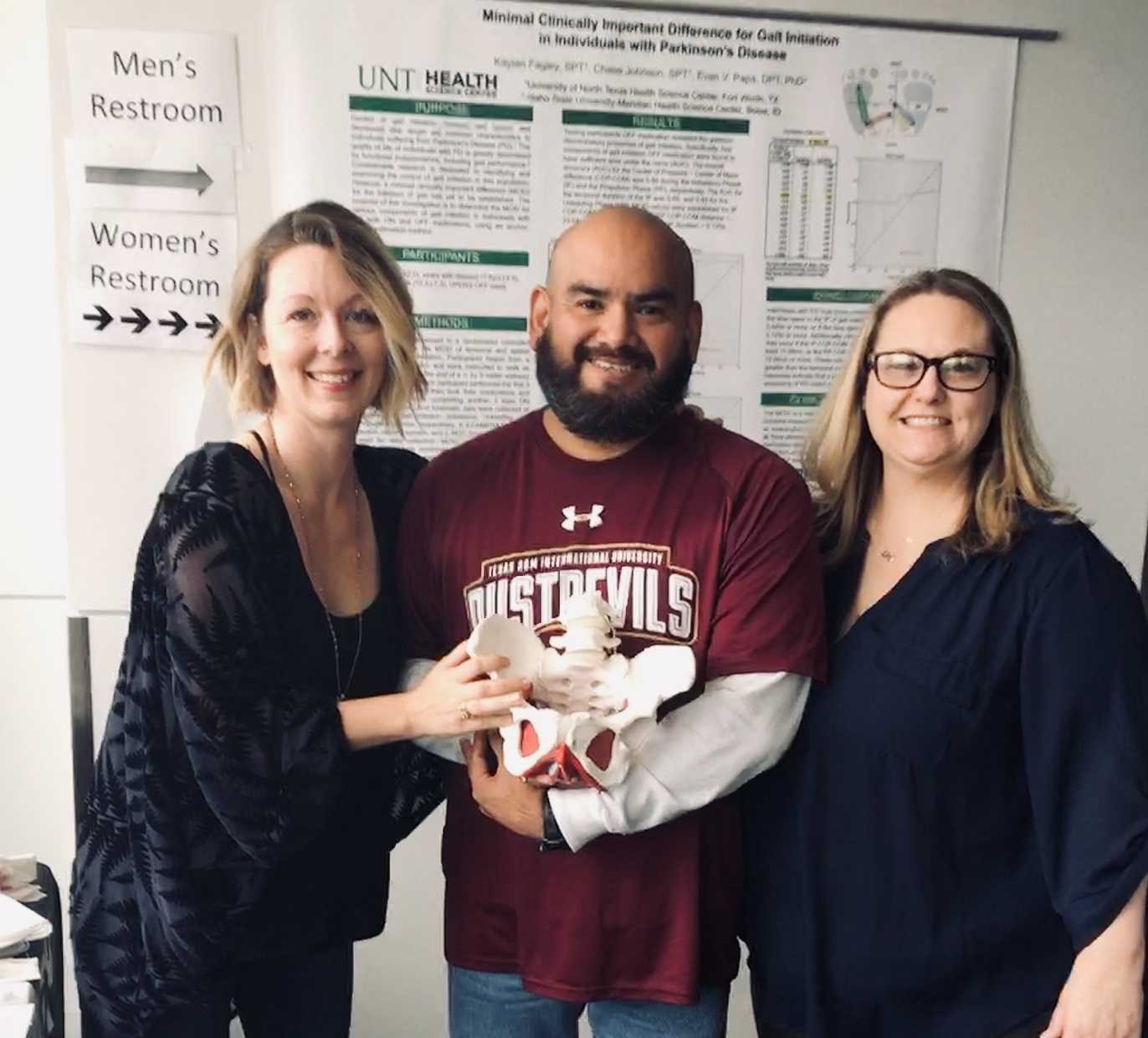
What/who inspired you to become involved in pelvic rehabilitation?
I first came across pelvic floor when reading the description of a CE course where it mentions its relation to SI joint dysfunction so I figured I could use this as a trouble shooting tool for those athletes that had recurrent low back pain or suspected SI problems. I figured at the very least I would know when I was confronted with something that I needed to refer. Little did I know how important of a “puzzle piece” this type of knowledge would become in helping me see a more complete picture of the human body. I was often confronted with athletes that would have recurring lower back pain, hip pain, glute tightness, sciatic nerve pain, adductor tightness or pain, and felt I was missing something to be able to help them. Even with a basic understanding of pelvic floor rehab I was able to help athletes with the previously mentioned complaints. As my understanding grew, I felt it was necessary I take these Herman & Wallace courses so that I could actually treat my patients in a holistic manner.
What is your clinical environment like, and how can you implement pelvic rehab into your practice?
My clinical environment varies between outpatient pediatrics, outpatient geriatrics, and D2 university athletics. I use my pelvic rehabilitation tool box at the university. Mostly I am still learning but I try to screen for and educate my athletes on the important role the pelvic floor muscles play in every activity they carry through out the day. I try to convey the importance not just in sports but also in activities of daily living such as any difficulty with going to the bathroom to pain during sex. I figure the more young people I educate about pelvic floor therapy the better they’ll be to make an informed decision today or later on in life.
Do you feel your background and training as a COTA brings anything unique to your pelvic rehab patients?
I could probably say that my COTA training makes it easier to pick up on some of the behaviors people might be relying on to carry out their day while dealing with pelvic floor issues. They may or may not be aware they have a pelvic floor dysfunction but simply think that’s just how they are. Behaviors such as avoiding social events because such activities don’t fit well with their voiding schedule.
How does your background as a COTA influence your approach to patient care?
My approach as a COTA would force me to see a balance in life. I would have to ask myself all the ways pelvic floor dysfunction may affect my client's daily activities from the basics like voiding, resting, sleep, to enjoying their leisure activities. A person cannot rest adequately if they’re in pain. He or she cannot enjoy social activities being worried of an urge.
What patients or conditions are you hoping to start treating as you continue learning pelvic rehab?
I wish to continue learning and exposing myself to different areas pelvic floor rehabilitation may take me. I wish to look at this therapy through a wide lens. This way I can learn, help many, and keep myself a well-rounded therapist. If in the future I feel more drawn to a specific area I wish to pull from all the different areas I should have learned by then.
What role do you see pelvic health playing in general well-being?
I often tell my athletes that there is probably not a single gross motor movement that doesn’t cross the pelvic region directly or through fascia connection. It is simply how we are built. To try and pretend or ignore the importance of the pelvic floor is just leaving our patients out of the appropriate care they need. And now that I know about the role pelvic floor muscles have in our body it would be unethical not to advocate for my patients’ COMPLETE well-being, pelvic floor muscles included.
What's next for you and your practice?
My short-term goal is acquiring my athletic training state license. After that continue with the last four or five prerequisite classes I need to apply to a DPT program. The DPT is my ultimate goal within the next five or six years.
Tiffany Ellsworth Lee MA, OTR, BCB-PMD joined the Herman & Wallace faculty to teach a course on biofeedback along with Jane Kaufman, PT, M.Ed, BCB-PMD. The month of April is Occupational Therapy month, and we are celebrating by highlighting the role that Occupational Therapists play in pelvic floor rehabilitation. Tiffany founded a biofeedback program at Central Texas Medical Center in San Marcos in 2004, and currently runs her a pelvic rehab private practice .
 Working in this area of biofeedback is extremely rewarding and fulfilling to help change peoples’ lives. I have a private practice now exclusively dedicated to treating patients with pelvic floor dysfunction. I became involved in working with patients with incontinence and pelvic floor disorders because of many opportunities along my career path. I have been an Occupational Therapist since 1994. Both of my parents are also OTs, so I think I was born to do this!
Working in this area of biofeedback is extremely rewarding and fulfilling to help change peoples’ lives. I have a private practice now exclusively dedicated to treating patients with pelvic floor dysfunction. I became involved in working with patients with incontinence and pelvic floor disorders because of many opportunities along my career path. I have been an Occupational Therapist since 1994. Both of my parents are also OTs, so I think I was born to do this!
Erica Vitek, MOT, OTR, BCB-PMD, PRPC wrote a blog recently about the role of OTs in pelvic health. She writes:
“As we look closer at the framework and the definition of OT (Occupational Therapy Practice Framework: Domain and Process, 3rd edition 2014), there is clear evidence that the occupational therapist (OT) has a role in the treatment of pelvic health conditions. Importantly, occupations are defined by this document as ‘…various kinds of life activities in which individuals, groups, or populations engage, including activities of daily living (ADL), instrumental activities of daily living (IADLs), rest and sleep, education, work, play, leisure, and social participation.”
The clearest examples of the OT’s role in pelvic health occupations within this section include:
- ADL section: toileting and hygiene (continence needs, intentional control of bowel movements and urination) and sexual activity.
- IADLs section: sleep participation (sustaining sleep without disruption, performing nighttime care of toileting needs).
- Achieving full participation in work, play, leisure, and social activities, requires one to be able to maintain continence in a socially acceptable manner in which they can feel confident and comfortable to fulfill their roles and duties.
"We believe that the great patient need that exists can be better served by having trained OTs able to treat pelvic health conditions"
How to get started as an OT
Occupational therapists wishing to pursue pelvic floor have a few options. The first thing is to find a pelvic floor clinical setting or work with their respective settings to check to see if they can start a women's health program with a strong focus on pelvic floor. OTs quite often do not start out in pelvic health directly after school and since this is a newer area as compared to other certifications such as the NDT and PNF it takes a little bit of research, time and effort to find one’s exact niche. To get started, an OT should seek out courses that teach the basics of bladder and bowel management. It is important to understand the anatomy and physiology of the bladder, bowel, and sexual systems.
Incontinence and pelvic floor disorders have a profound impact on occupation, the daily activities that give life meaning! OTs should have a larger role in treating this patient population. Offering hope to our patients is imperative when he/she is dealing with pelvic floor dysfunction!
Keep an eye out for an upcoming post from Tiffany with some inspiring clinical case studies. You can join Tiffany and Jane Kaufman in Biofeedback for Pelvic Muscle Dysfunction to get lots of hands-on time with surface eletromyography, and to work toward BCIA certification!
The Institute has welcomed occupational therapists since our founding in 2006. In addition, three OTs: Richard Sabel, MA, MPH, OTR, GCFP, Erica Vitek, MOT, OTR, BCB-PMD, PRPC, and Tiffany Ellsworth Lee MA, OTR, BCB-PMD all teach courses as members of our faculty. (Erica Vitek is also one of several OTs who holds certification as a Pelvic Rehabilitation Practitioner through H&W).
Recently, the Institute was contacted by an Occupational Therapist who has attended many of our courses, regarding a challenge she was experiencing obtaining CEUs in her state (Oregon) for courses on Pelvic Rehab and Biofeedback. In light of this, the Institute has been discussing with some of the occupational therapists on our faculty, as well as representatives of the BCIA and Marquette University, and how to spread awareness about and recognition of OT’s roles in pelvic rehab. Below, we’ve asked faculty member Erica to share a bit more about her journey and the role of the pelvic rehab occupational therapist.
 As an OT student, I had a professor who brought in practicing clinicians to discuss their unique roles out in the field. Pelvic health happened to be one of the topics of the day. I was completely intrigued by the clinician, who had such passion about the role of OT in pelvic health. It became clear that helping people with impaired basic bodily functions was imperative to fulfilling life roles and participation; it was OT. I knew from that moment that I wanted to help people deal with these challenging, private issues.
As an OT student, I had a professor who brought in practicing clinicians to discuss their unique roles out in the field. Pelvic health happened to be one of the topics of the day. I was completely intrigued by the clinician, who had such passion about the role of OT in pelvic health. It became clear that helping people with impaired basic bodily functions was imperative to fulfilling life roles and participation; it was OT. I knew from that moment that I wanted to help people deal with these challenging, private issues.
In my journey, I did not immediately start out in pelvic health, but instead in an acute care hospital that had a women’s health program with a strong interest in pelvic health. A very experienced OT and her team of 2 additional OTs were doing great work in that department already. The window of opportunity opened for me to mentor with that group and I eventually was able to begin to get my own referrals and develop a robust hospital-based outpatient practice. At that time, ALL of my experience had been with OTs doing this work and I was naïve to the fact that outside of my world, most of the clinicians doing this type of work were physical therapists (PT). I asked to join a highly trained and skilled group within my health system of all women’s health PTs. Overtime, I was able to demonstrate my level of competency within the group of PTs and contribute valuable things to our organization. Herman and Wallace Rehabilitation Institute was instrumental in my quest to demonstrate competency as they allowed OTs a clear pathway for enrollment in their coursework and application for the Pelvic Rehabilitation Practitioner Certification examination. I can be proud to have those credentials to my name.
My challenges in the area of pelvic health practice have thankfully been minimal, nearly nonexistent, and it has come to my awareness in recent weeks that this is not the case for OTs around the country trying to develop themselves as pelvic health practitioners. My original OT mentors reassured me with the AOTA’s published document titled Occupational Therapy Practice Framework: Domain & Process, detailed a clear place in the role of pelvic health. This document has gone through 3 revisions over the course of its first publication in 2002. The 2nd edition was published in 2008 and the 3rd edition in 2014. I’d like to cite a few important areas of the document that I find to be helpful in an OT’s quest to demonstrate our role in pelvic health rehabilitation.
I’d first like to quote the definition occupational therapy according to the 3rd edition, “occupational therapy is defined as the therapeutic use of everyday life activities (occupations) with individuals or groups for the purpose of enhancing or enabling participation in roles, habits, and routines in home, school, workplace, community, and other settings. Occupational therapy practitioners use their knowledge of the transactional relationship among the person, his or her engagement in valuable occupations, and the context to design occupation-based intervention plans that facilitate change or growth in client factors (body functions, body structures, values, beliefs, and spirituality) and skills (motor, process, and social interaction) needed for successful participation. Occupational therapy practitioners are concerned with the end result of participation and thus enable engagement through adaptations and modifications to the environment or objects within the environment when needed. Occupational therapy services are provided for habilitation, rehabilitation, and promotion of health and wellness for clients with disability- and non-disability-related needs. These services include acquisition and preservation of occupational identity for those who have or are at risk for developing an illness, injury, disease, disorder, condition, impairment, disability, activity limitation, or participation restriction. “
As we look closer at the framework and the definition of OT, there is clear evidence that the occupational therapist (OT) has a role in the treatment of pelvic health conditions. Importantly, occupations are defined by this document as “…various kinds of life activities in which individuals, groups, or populations engage, including activities of daily living (ADL), instrumental activities of daily living (IADLs), rest and sleep, education, work, play, leisure, and social participation.” The clearest examples of the OT’s role in pelvic health occupations within this section include: 1) ADL section: toileting and hygiene (continence needs, intentional control of bowel movements and urination) and sexual activity. 2) IADLs section: sleep participation (sustaining sleep without disruption, performing nighttime care of toileting needs). 3) Achieving full participation in work, play, leisure, and social activities, requires one to be able to maintain continence in a socially acceptable manner in which they can feel confident and comfortable to fulfill their roles and duties.
Client factors as defined in this document are “Specific capacities, characteristics, or beliefs that reside within the person and that influence performance in occupations. Client factors include values, beliefs, and spirituality; body functions; and body structures.” Client factors are further identified as affecting the performance skills and participation of the clients we work with. OT’s role per definition is to “facilitate change and growth in client factors”. In order to fully enhance our client’s performance skills/participation related to change and growth in client factors, OT’s have to examine the whole person, including pelvic health impairments, which have a negative influence on performance. Within client factors, the document defines body structures as, “Anatomical parts of the body, such as organs, limbs, and their components that support body function.” Within this category, one can refer to multiple items named that relate to the care that OTs provide in pelvic health rehabilitation, including but not limited to, structures related to the digestive, metabolic, and endocrine systems and structures related to the genitourinary and reproductive systems.
Since the first email from this individual in Oregon, we have been reached by several other OTs asking about similar challenges and questions about scope of practice. Because of our commitment to honoring the AOTA’s Practice Framework, and because we believe that the great patient need that exists can be better served by having trained OTs able to treat pelvic health conditions, the Institute is working with members of our faculty and professional network to advocate for recognition of OTs in pelvic rehab and resolve confusion about scope of practice. For those interested in further resources, please check out:
- Pelvic Floor Biofeedback
- The Women’s Health 4 OT Facebook Group
- The OTs for Pelvic Health Facebook Group
- Occupation Therapy in Postpartum Care Facebook Group
- Womens Health Occupational Therapy Australia Facebook Group
American Occupational Therapy Association. (2002). Occupational therapy practice framework: Domain and process. American Journal of Occupational Therapy, 56, 609-639.
American Occupational Therapy Association. (2008). Occupational therapy practice framework: Domain and process (2nd ed.). American Journal of Occupational Therapy, 62, 625-683.
American Occupational Therapy Association. (2014). Occupational therapy practice framework: Domain and process. American Journal of Occupational Therapy, 68, S1-S48.