Herman & Wallace has more than 55 different courses with over 200 individual course events scheduled throughout the year to choose from. Our course catalog is growing all the time with new courses, new instructors, more course dates, and even more satellite locations!
In 2022 there are already six BRAND NEW courses available, with more to be planned. H&W is kicking off the new year strong with Dr. Michael Hibner on January 9th with Pudendal Dysfunction: The Physician's Perspective. Kristina Koch is back in 2022 with her newly updated and reformated course, Pharmacologic Considerations for the Pelvic Health Provider which is scheduled for April 10, July 9, and November 19th.
Do you live near Salt Lake City, Utah? Our first live, in-person course since the pandemic will be there on March 12-13, 2022: Dry Needling and Pelvic Health.
- Disclaimer: Due to the nature of this course content, it will be delivered in the traditional "in-person" manner. This means the course instructors will be teaching at a single location, and it will not be possible to join the course remotely via video conference. As with all Herman & Wallace courses, this course content is only intended for practitioners who are licensed appropriately, and for whom dry needling is within their scope of practice. It is the responsibility of every course registrant to check with their state boards to ensure that the content of a Herman & Wallace course that they attend is within their state-specific scope of practice.
Interested in women's health? There are 3 new courses appearing this year:
- Perinatal Mental Health: The Role of Pelvic Rehab Therapist - February 5, 2022
- Menopause Transitions and Pelvic Rehab - March 5-6, 2022
- Pregnancy and Postpartum Considerations for High-Intensity Athletics - May 21, 2022
Are you thinking about taking a course, but not sure if it is for you? H&W courses are for licensed practitioners interested in the field of pelvic rehabilitation. The most common registrants that we see in our courses include:
- Doctor of Osteopathic Medicine (DO)
- Doctor of Chiropractic (DC)
- Nurse-Midwives (CNM)
- Nurse Practitioners (ARNP)
- Occupational Therapists (OT)
- Occupational Therapists Assistants (OTA)
- Physical Therapists (PT)
- Physical Therapists Assistants (PTA)
- Doctor of Medicine (MD)
- Physicians Assistants (PA)
- Registered Nurses (RN)
H&W courses are classified as Beginner (no prerequisites), Intermediate (one prerequisite), or Advanced (two or more prerequisites). A Beginner course can be taken by a licensed practitioner without prior coursework requisites. Therapists interested in registering for an Intermediate or Advanced course must review the prerequisites on the course description and honestly assess/report their fulfillment of the published prerequisites.
For example, courses that have Pelvic Floor Level 1 as a prerequisite require a working knowledge of performing internal assessments. It is never recommended that a participant skip this introduction without prior training or experience performing an internal exam. Some courses are part of a series and it is not recommended that they be taken out of order. On the Continuing Education Courses page, you can click the Experience Level tab to see courses organized by level of difficulty.
Clinical experience or alternative coursework may be a substitute for the published course requirements, and it is recommended that a therapist considering opting out of a published prereq review the objectives of the required course and assert that said objectives have been met. Review the Course Overview and Objectives on each course page and ask yourself what your treatment goals (in both the long and short term) are and what patient population you are targeting. All courses list the learning objectives, which will give you a lot of information about what you'll be learning at a given course.
If you would like additional guidance on which course offering best fits your goals and target patient population, please contact us! We are here to guide you into an event that best suits your needs.
Fears about treating men’s health conditions are limiting access to care or are creating potential for harm in the field of pelvic health. Many cisgender women (women whose gender identify matches the sex likely assigned at birth) express concerns about working with cisgender men beyond a lack of knowledge about conditions related to prostate issues, urinary leakage, or genital pain. Are these fears warranted, are they fair? Rather than assert that ciswomen should simply move beyond their concerns, the field of pelvic health and the patients with whom we work may be better served by digging in and talking more openly about such fears. Following are some of the concerns or comments I have heard expressed by cisgender women within the context of treating men’s health matters:

- (Regarding palpation of the penis:) “Is that legal?”
- “I worry about being alone in a room with a man.”
- “What if he gets an erection?”
- “My husband doesn’t want me to work with other men for pelvic health stuff.”
- “I’ve never seen a man’s genitals before and I’m not comfortable with it.”
- “My religion teaches that I should not touch a man other than my husband.”
- “I don’t know what to say when men make suggestive comments.”
- “My supervisor is forcing me to do this work with men when I don’t want to.”
- “I only treat them in side lying because then I don’t have to see their stuff.”
Rather than a reader making a judgement about the above comments, we should ask ourselves as a profession if the above topics have been properly addressed in our training or if we are encouraged to work through this area of professional and personal intersecting concerns. We could view the concerns expressed through the lens of providing equal care, in other words, are we discriminating against someone based on their genitals? Or through a lens of safety- is there an actual (as well as perceived) threat from a cisgender woman who is alone in a treatment room with a cisgender man? If that’s potentially true, how are we mitigating this risk? Where does the anatomical line end between personal beliefs such as “I can touch another man’s shoulder, but not perineal area”? Are we practicing ethically if we are denying access to care or providing less than comprehensive care? Is a therapist truly worried about their primary relationship by doing this work because their partner does not approve? And more importantly, can we provide needed guidance or support to address some of the above obstacles?
I commonly have the opportunity to work with men who have seen other self-identified female therapists first. Here is what I often hear:
- “I could tell that they weren’t comfortable talking to me about this issue.”
- “It didn’t seem like they knew what to do with me.”
- “I got switched over to another therapist after asking some questions about using a penile pump.”
- “I felt really shamed about my condition because they would change the subject.”
- “I called many places and they rejected seeing me because I’m a man.”
- “When I asked if they were going to examine where the pain is [genital area] they said it would be a last resort.”
- “No one ever examined me, just gave me a biofeedback sensor to put in.”
This information is not shared to shame the caring professionals in our field. What needs to happen, however, for elevating the inclusiveness of care, is a continual dialogue and recognition of the support needed to work with sensitive conditions and the vulnerabilities of both patients and providers. It is potentially harmful to reject patients based on gender, or to provide lesser care based on genitals. To further this conversation, the Institute has partnered with author and educator Leticia Nieto, who holds a degree in psychology and who wrote Beyond Inclusion, Beyond Empowerment: A Developmental Strategy to Liberate Everyone. Join Leticia and me (Holly Tanner) for our first 3-hour discussion that emphasizes talking, feeling, and thinking through some of the above concerns and challenges. The class will focus on discussion more than lecture, and will aim to provide a space within which we can speak openly about how to move forward with the goal of improving comfort when working with men’s health issues and improving access to much needed pelvic health care. Note: this class is welcoming to all people with any gender identification, however, the emphasis will be on the topics discussed in this post.
 Rachna Mehta, PT, DPT, CIMT, OCS, PRPC is the author and instructor of the new Acupressure for Pelvic Health course. She is Board certified in Orthopedics, is a Certified Integrated Manual Therapist and is also a Herman and Wallace certified Pelvic Rehab Practitioner. An alumni of Columbia University, Rachna brings a wealth of experience to her physical therapy practice with a special interest in complex orthopedic patients with bowel, bladder and sexual health issues. Rachna has a personal interest in various eastern holistic healing traditions and she noticed that many of her chronic pain patients were using complementary health care approaches including Acupuncture and Yoga. Building on her orthopedic and pelvic health experience, Rachna trained with renowned teachers in Acupressure and Yin Yoga. Her course Acupressure for Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional and energy body. Rachna is a member of the American Physical Therapy Association and a member of APTA’s Pelvic Health section.
Rachna Mehta, PT, DPT, CIMT, OCS, PRPC is the author and instructor of the new Acupressure for Pelvic Health course. She is Board certified in Orthopedics, is a Certified Integrated Manual Therapist and is also a Herman and Wallace certified Pelvic Rehab Practitioner. An alumni of Columbia University, Rachna brings a wealth of experience to her physical therapy practice with a special interest in complex orthopedic patients with bowel, bladder and sexual health issues. Rachna has a personal interest in various eastern holistic healing traditions and she noticed that many of her chronic pain patients were using complementary health care approaches including Acupuncture and Yoga. Building on her orthopedic and pelvic health experience, Rachna trained with renowned teachers in Acupressure and Yin Yoga. Her course Acupressure for Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional and energy body. Rachna is a member of the American Physical Therapy Association and a member of APTA’s Pelvic Health section.
According to the National Center for Complementary and Integrative Health (NCCIH), a branch of NIH, pain is the most common reason for seeking medical care1. Over the last several decades there has been an increasing interest in safe and efficacious treatment options as our healthcare system faces a crisis of pills and opioid use. Among complementary medicine approaches, Acupressure has come forth as an effective non-pharmacologic therapeutic modality for symptom management.
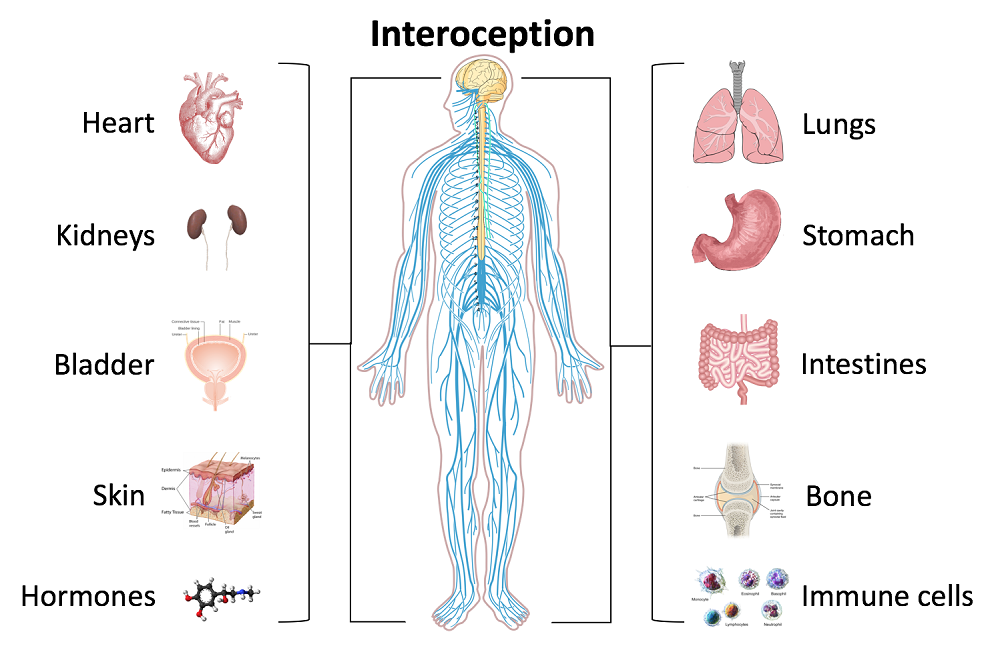
Acupressure is widely considered to be a noninvasive, low cost, and efficient complementary alternative medical approach to alleviate pain. It is easy to do anywhere at any time and empowers the individual by putting their health in their hands. Acupressure involves the application of pressure to points located along the energy meridians of the body. These acupoints are thought to exert certain psychologic, neurologic, and immunologic effects to balance optimum physiologic and psychologic functions2. Acupressure can be used for alleviating anxiety, stress and treating a variety of pelvic health conditions including Chronic Pelvic Pain, Dysmenorrhea, Constipation, digestive disturbances and urinary dysfunctions to name a few.
Acupressure uses the same points as Acupuncture; however, it is a very active practice in that we can teach our patients potent acupressure points as part of a wellness self-care regimen to manage their pain, anxiety and stress in addition to traditional physical therapy interventions. Traditional Chinese Medicine (TCM) believes in Meridian theory and energy channels which are connected to the function of the visceral organs. There is emerging scientific evidence of Acupoints transmitting energy through interstitial connective tissue with potentially powerful integrative applications through multiple systems.
Acupressure has also been used with various types of mindfulness and breathing practices including Qigong and Yoga. Yoga is an umbrella term for various physical, mental, and spiritual practices originating in ancient India, Hath Yoga being the most popular form of Yoga in western society. Yin Yoga, a derivative of Hath Yoga, is a much calmer meditative practice that uses seated and supine postures, held three to five minutes while maintaining deep breathing. Its focus on calmness and mindfulness makes Yin Yoga a tool for relaxation and stress coping, thereby improving psychological health3. Yin Yoga facilitates energy flow through the meridians and can be used for stimulating acupressure points along specific meridian and energy channels bringing the body to its physiological resting state.
As Pelvic health rehabilitation specialists, we are uniquely trained to combine our orthopedic skills with mindfulness based holistic interventions to improve the quality of life of our patients. We can empower our patients to recognize the mind-body-energy interconnections and how they affect multiple systems, giving them the tools and self-care regimens to live healthier pain free lives. Please join me on this evidence-based journey of holistic healing and empowerment as we explore Acupressure and Yin Yoga as powerful tools in the realm of energy medicine to complement our best evidence-based practices.
1. Pain: Considering Complementary Approaches published by National Center for Complementary and Integrative Health.2019.
2. Monson E, Arney D, Benham B, et al. Beyond Pills: Acupressure Impact on Self-Rated Pain and Anxiety Scores. J Altern Complement Med. 2019;25(5):517-521.
3. Daukantaitė D, Tellhed U, Maddux RE, Svensson T, Melander O. Five-week yin yoga-based interventions decreased plasma adrenomedullin and increased psychological health in stressed adults: A randomized controlled trial. PLoS One. 2018;13(7).
 Pauline H. Lucas, PT, DPT, WCS, NBC-HWC joins the Herman & Wallace faculty with her new course, Mindfulness for Rehabilitation Professionals. The course launches January 2021 and discusses the impact of chronic stress on health and wellbeing, and the latest research on the benefits of mindfulness training for both patients and healthcare providers. The following comes from Pauline, who hopes you will join her for her course.
Pauline H. Lucas, PT, DPT, WCS, NBC-HWC joins the Herman & Wallace faculty with her new course, Mindfulness for Rehabilitation Professionals. The course launches January 2021 and discusses the impact of chronic stress on health and wellbeing, and the latest research on the benefits of mindfulness training for both patients and healthcare providers. The following comes from Pauline, who hopes you will join her for her course.
As an integrative physical therapist treating people with pelvic pain, digestive issues, headaches, and various persistent pain conditions, I council my patients on strategies to reduce a chronically activated stress response (sympathetic dominance). Many of them are living stressful lives, and their medical condition can be an additional stressor. I share with them that by reducing their stress level and improving their overall awareness of what makes them feel better and worse, they may affect their condition in a positive way. When I ask if they have any experience with meditation, I often get the response: “Oh I tried that many years ago and I’m really bad at it; I just can’t meditate.” When I ask them to explain a bit more, they tell me that their mind is always super busy, they are always thinking, and when they try to stop the thoughts during meditation, it doesn’t work.
This is when I explain one of the essential concepts of meditation: It’s okay to have thoughts. In fact, it’s completely normal to become more aware of the busy thoughts when you first sit down to meditate. The trick is to allow the thoughts to be there, and at the same time keeping awareness with the focus of the meditation practice (i.e., the breath, a mantra, etc.). When we don’t resist the thoughts, the mind naturally gradually calms down, resulting in fewer and calmer thoughts. This is when I typically see relief on my patient’s face when they realize they may not be a bad meditator after all, and they are often willing to give the practice another try.
To learn more about using mindfulness and meditation in your personal life and in patient care, please join our 1 day virtual course Mindfulness for Rehabilitation Professionals.
Leeann Taptich DPT, SCS, MTC, CSCS is Co-Author of the new Herman & Wallace offering, Breathing and Diaphragm: Pelvic and Orthopedic Therapist. Leeann leads the Sports Physical Therapy team at Henry Ford Macomb Hospital in Michigan where she mentors a team of therapists. She also works very closely with the pelvic team at the hospital which gives her a very unique perspective of the athlete.
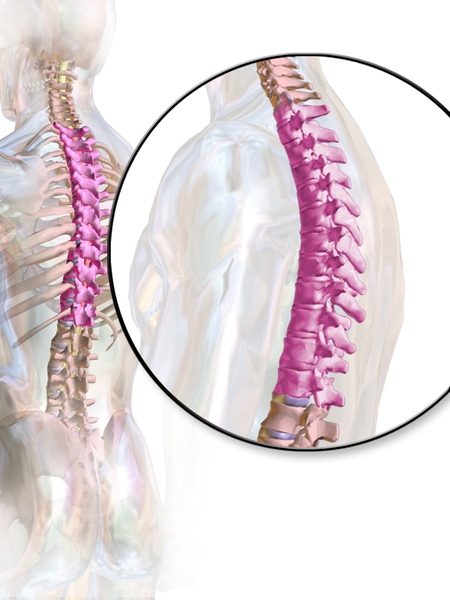
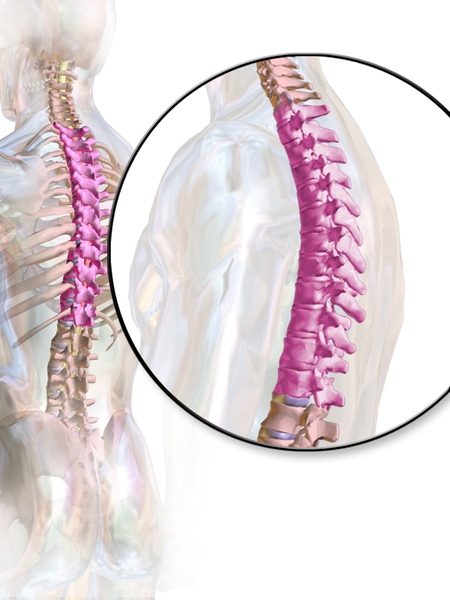 According to a paper from Manual Therapy, the thoracic spine is the least understood part of the spine, despite the huge role it plays in both movement and in regulation of our Autonomic Nervous System.1 Researchers found that the thoracic spine is the least studied of the three spinal regions; thoracic, cervical, and lumbar. I am frequently asked by fellow therapists for help in objectively assessing and treating the thoracic region which has led to the realization that even amongst experienced therapists the thoracic spine’s importance is less understood especially in terms of its function.
According to a paper from Manual Therapy, the thoracic spine is the least understood part of the spine, despite the huge role it plays in both movement and in regulation of our Autonomic Nervous System.1 Researchers found that the thoracic spine is the least studied of the three spinal regions; thoracic, cervical, and lumbar. I am frequently asked by fellow therapists for help in objectively assessing and treating the thoracic region which has led to the realization that even amongst experienced therapists the thoracic spine’s importance is less understood especially in terms of its function.
Anatomically, the thoracic spine along with the ribs and sternum provide a frame that supports and protects the lungs and heart. Despite the rigidity that is required to fulfill that function, the thoracic spine contributes significantly to a person’s ability to rotate.2
One of the biggest roles the thoracic spine plays is in the regulation of the Sympathetic Nervous System, which is a part of the Autonomic Nervous System. The sympathetic nervous system, also known as the “Fight or Flight” system is in overdrive in our patients who present with pain. One of the many complications that arise from an upregulated sympathetic system is increased respiratory rate and/or dysfunctional breathing.3 Carefully applied manual therapy techniques to the thoracic region can help regulate the Autonomic Nervous System by affecting the diaphragm, the intercostals, and other respiratory musculature.4 Specific thoracic mobilizations/manipulations can improve respiratory function.4
In the Breathing and Diaphragm course, Aparna Rajagopal and I discuss the importance of the thoracic spine from both a regional and global perspective. Thoracic spine assessment is taught along with multiple mobilization techniques and manipulations all of which will help the clinician link the thoracic spine to the treatment of pelvic pain, low back pain, and breathing pattern disorders. Join Aparna and I in either Sterling Heights, MI this March or Princeton, NJ in December for Breathing and the Diaphragm: Pelvic and Orthopedic Therapists: From Assessment to Clinical Applications for Pelvic and Orthopedic Therapists!
1. Heneghan NR, Rushton A. Understanding why the thoracic region is the ‘Cinderella’ region of the spine. Man Ther. 2016; 21: 274-276.
2. Narimani M, Arjamand N. Three-dimensional primary and coupled range of motions and movement coordination of the pelvis, lumbar, and thoracic spine in standing posture using inertial tracking device. Journal of Biomechanics. 2018; 69: 169-174.
3. Bernston GG. Stress effects on the body: Nervous system. American Psychological Association. https://www.apa.org/helpcenter/stress/effects-nervous. January 18, 2020.
4. Shin DC, Lee YW. The immediate effects of spinal thoracic manipulation on respiratory functions. Journal of Physical Therapy Science. 2016; 28: 2547-2549.
Mia Fine, MS, LMFT, CST joins the Herman & Wallace faculty in 2020 with her new course on Sexual Interviewing for Pelvic Health Therapists! The new course is launching this April 4-5, 2020 in Seattle, WA; Lecture topics include bio-psycho-social-spiritual interviewing skills, maintaining a patient-centered approach to taking a sexual history, and awareness of potential provider biases that could compromise treatment. Labs will take the form of experiential practice with Bio-Psycho-Social-Spiritual-Sexual Interviewing Skills, case studies and role playing. Check out Mia's interview with The Pelvic Rehab Report, then join her for Sexual Interviewing for Pelvic Health Therapists!
 Tell us about yourself, Mia!
Tell us about yourself, Mia!
My name is Mia Fine, MS, LMFT, CST and I’ve been a Licensed Marriage and Family therapist for four years. I am an AASECT Certified Sex Therapist and my private practice is Mia Fine Therapy, PLLC. I see these kinds of patients: folks with Erectile Dysfunction, Pre-mature Ejaculation, Vaginismus, Dyspareunia, Desire Discrepancy, LGBTQ+, Ethical Non-monogamy, Anxiety, Depression, Trauma, Relational Concerns, Improving Communication.
What can you tell us about the new course?
This course will offer a great deal of current and empirically-founded sex therapy and sex education resources for both the provider as well as the patient. This course will add the extensive skills of interviewing for sexual health. It also offers the provider a new awareness and self-knowledge on his/her/their own blind spots and biases.
How will skills learned at this course allow practitioners to see patients differently?
Human beings are hardwired for connection, intimacy, and pleasure. Our society often tells us that there is something wrong with us, or that we are defective, for wanting a healthy sex life and for addressing our human needs/sexual desires. This course will broaden the provider’s scope of competence in working with patients who experience forms of sexual dysfunction and who hope to live their full sexual lives.
What inspired you to create this course?
This course was inspired by the need for providers who work with pelvic floor concerns to be trained in addressing and discussing sexual health with their patients.
What resources were essential in creating your course?
Becoming a Licensed Marriage and Family Therapist and a Certified Medical Family Therapist requires three years of intensive graduate school. Additionally, a minimum of two years of training to become an AASECT Certified Sex Therapist and hundreds of hours of direct client contact hours, supervision, and consultation. I attend numerous sex therapy trainings and continuing education opportunities on a regular and ongoing basis. I also train incoming sex therapists on current modalities and working with vulnerable client populations.
How do you think these skills will benefit a clinician in their practice?
It is vital that providers working with pelvic floor concerns have the necessary education and training to work with patients on issues of sexual dysfunction. It is also important that providers be aware of their own biases and be introduced to the various sexual health resources available to providers and patients.
What is one important technique taught in your course that everybody should learn?
Role playing sexual health interview questions is an important experience in feeling the discomfort that many providers feel when asking sexual health questions. This offers insight not only into the provider experience but also the patient’s experience of uncomfortability. Role playing this dynamic illustrates the very real experiences that show up in the therapeutic context.
Sexuality is core to most human beings’ identity and daily experiences. When there are concerns relating to our sexual identity, sexual health, and capacity to access our full potential, it affects our quality of life as well as our holistic well-being. Working with folks on issues of sexual health and decreasing sexual dysfunction encourages awareness and encourages healing. Imagining a world where human beings don’t walk around holding shame or traumatic pain is imaging a world of health and happiness.
Herman & Wallace is excited to announce an upcoming course on pelvic rehab for the gender diverse patient, written and instructed by Dr. Laura Meihofer, DPT, ATC. As Dr. Meihofer indicated in a recent blog, "[t]he number of individuals who identify as transgender is growing each year. The Williams Institute estimated in 2016 that 0.6% of the U.S. population or roughly 1.4 million people identified as transgender (Flores, 2016)... With the rise of individuals who identify as transgender, gender non-binary and intersex, healthcare professionals have equally seen an influx of patients who require care throughout their discovery and transition."
The new course from Dr. Meihofer is called "Gender Diversity and Pelvic Health: Comprehensive Care for Transgender Men and Women", and it will be debuting on May 29-31, 2020 in Livingston, NJ.
Dr. Meihofer was kind enough to share some thoughts about the new course, her practice, and herself with The Pelvic Rehab Report. Thank you, Laura!
Tell us about yourself, Laura!
My name is Laura Meihofer and I’ve been a physical therapist for 7 years. I work at Mayo Clinic and I see patients throughout the gender spectrum who most commonly struggle with pelvic floor dysfunctions relating to overactive muscles such as: chronic and acute pelvic pain, urinary frequency/urgency/incontinence/hesitancy, constipation, pain with intercourse, low back and hip pain.
 What can you tell us about your new course, "Gender Diversity and Pelvic Health"?
What can you tell us about your new course, "Gender Diversity and Pelvic Health"?
Currently there are roughly 1.25 million transgender identified individuals in the United States and this number is growing. This course will help to dispel the idea of “other” when treating this demographic and demonstrate how much sameness there is when treating pelvic floor dysfunction.
These skills will greatly benefit any practice as this population is so underserved, they are looking for allies that are not just nice but competent. When you are able to successfully treat gender diverse patients, they spread the word about the great care they received and you now have a strong referral base. Taking this course opens up a whole new referral base of amazing people.
This course will not only feature videos from thought leaders in the field but will also highlight testimonials from patients and caregivers who have undergone their own gender transitions.
What essential skills does your course add to a practitioner’s toolkit?
I think the most important technique that attendees will learn will be how to assess a trans women and trans man after they have undergoing genital reconstruction surgery. Attendees will gain competence in the care of the gender diverse patient at any stage during their gender transition.
What was your inspiration to create this course for trans-identified patients?
Working at a major medical institution, I found that it was difficult finding providers in a patient’s area that were competent in care of a transgender patient. As I talked more and more with various physical therapists I realized they were thirsty for knowledge on how to serve these individuals. So I created the course!
What prepared you to create this course?
The most important thing I have done for this course is treat hundreds of patients who are trans identified throughout their gender journey. This allowed me to not only see all the medical interventions they went through but also to hear their personal journey of transition. These experiences expanded my empathy for what they go through and inspired me to search within myself on how I can be better for them. This desire to improve opened a creative well inside of me from which this course grew.
Discuss the effect conditions covered in your course have on a patient’s quality of life, your experience treating patients with this condition, and how their quality of life has increase after successful treatment.
Individuals who identify as transgender suffer from pelvic floor dysfunction just like our cis gender folks. There is no current data to capture the prevalence of pelvic floor issues in this specific population to date, however there is research to support the overall lack of care these individuals receive. Based on the results from the U.S. Transgender Survey which surveyed 28,000 respondents, the numbers in the health care field were staggering.
33% of respondents had at LEAST one negative experience with a health care provider in the last year due to being transgender. Negative experiences were qualified as verbal harassment, refusal of treatment or having to teach the health care provider about transgender people to receive appropriate care. 23% of respondents did not see a doctor when they needed to due to fear of being mistreated as a transgender person.
This course aims has two primary aims:
1) Educate providers on the unique concerns that transgender individuals experience related to hormone replacement and surgical techniques.
2) Equip attendees to provide competent care for this demographic
Join Dr. Meihofer for Gender Diversity and Pelvic Health this May 29-31, 2020 in Livingston, NJ!
Aparna Rajagopal, PT, MHS is the lead therapist at Henry Ford Macomb Hospital's pelvic dysfunction program, where she treats pelvic rehab patients and consults with the sports therapy team. Her interests in treating peripartum patients and athletes allowed her to recognize the role that breathing plays in pelvic dysfunction. She has just joined the Herman & Wallace faculty and co-authored the new course, "Breathing and the Diaphragm: Pelvic and Orthopedic Therapists", which helps clinicians understand breathing mechanics and their relationship to the pelvic floor.
Aparna was kind enough to introduce herself to us here on The Pelvic Rehab Report.
 Thank you for your time Aparna! To start, tell us a little bit about yourself.
Thank you for your time Aparna! To start, tell us a little bit about yourself.
My name is Aparna. I’ve been a physical therapist for 22 years. About 16 years ago I switched focus from orthopedics to treating pregnancy and postpartum patients and that’s where my initial interest in pelvic care started. In 2006 following my pregnancy and birth of my daughter, my interest in pelvic care grew with my special interest becoming pelvic pain.
I teach and mentor the pelvic health therapists within the fairly large hospital system that I work at and collaborate with our spine center team and our sports team.
What can you tell us about this new breathing course that is not mentioned in the “course description” and “objectives” that are posted online?
Physical therapy has evolved and continues to evolve as we speak. Regional inter dependence, wherein the different systems interplay, and one structure influences another, is fascinating. No longer is the body considered and treated as independent fragmented pieces. The ‘core’ with the contribution of the Diaphragm and the pelvic floor is so much more than just the Transverse Abdominis and the Multifidus working together. Fascial restrictions of the lower abdomen and the pelvis can influence how the low back feels, thoracic stiffness can influence the interplay between the various abdominal muscles by way on their insertion into the lower ribs, musculo- skeletal pain and postural deviations can stem from incorrect breathing patterns etc.
Normal breathing rate is about 10 times every minute. Breathing incorrectly reinforces wrong movement patterns tens of thousand times a day with negative consequences on the musculoskeletal system.
This course offers an in depth look at the diaphragm from the perspective of both orthopedic and pelvic therapists and attempts to tie in the diaphragm to the thoracic spine, the ribs, the pelvic floor, the core, posture and finally the athlete.
What essential skills does the breath course add to a practitioner’s toolkit?
The practitioner will walk away with the ability to view the patient as a “whole”. It offers a different perspective on neck and back pain, posture/ alignment along with the ability to assess for and connect breathing and the diaphragm to stability/ the core, continence issues and the Autonomic Nervous System.
As therapists we already do a great job of addressing strength issues, assessing and correcting posture, mobilizing etc. You can add to your treatment options by learning how the diaphragm works in concert with other muscles (especially the abdominals) and systems, identifying breathing pattern dysfunctions and postures, and movement patterns which may be linked to breathing pattern dysfunctions. This understanding is beneficial for both orthopedic and pelvic patients.
What inspired you to create this course? What void does this new offering fill?
I have used breathing and evaluation of the diaphragm as a part of pelvic care for several years now. As the mentor for the pelvic program at my hospital, and as a part of the spine team and sports team, I work with pelvic therapists, orthopedic therapists, manual certified therapists, and sports certified therapists. Through my interactions I have come to realize that although many of the therapists are aware that the Diaphragm and breathing are important, they are unsure of how to assess for dysfunctions and address those dysfunctions. I initially started conducting classes within the hospital system. At the same time Leeann who is a sports certified therapist and holds a manual therapy certificate and I started collaborating on our patients. Using a combination of her knowledge and effective manual techniques with my pelvic care and breathing techniques we realized that along with my pelvic patients; our back and neck patients, and her sports patients were all benefitting from this combined approach. We realized along the way that we had information worth sharing with our colleagues that would benefit them in treating their patients, and started classes within the hospital system and that is how this class was born!
What was your process like creating this course?
As a trained pelvic therapist, I have incorporated and used breath and the diaphragm in my treatment for over a decade. Leeann and I have created this course using a combination of our clinical experiences, our education in our respective chosen paths of patient care, and most importantly using recent and relevant research articles from journals to guide us extensively in creating this course.
Breathing and the Diaphragm: Pelvic and Orthopedic Therapists is a new course being offered next March 27-29, 2020 in Sterling Heights, MI, and again on December 11-13, 2020 in Princeton, NJ. It is created and taught by Aparna Rajagopal, PT, MHS and Leeann Taptich, PT, DPT. Come learn how the diaphragm and breathing can affect core and postural stability through intra-abdominal pressure changes. As an integrated approach, the course looks at structures from the glottis and the cervical region to the pelvic floor and helps in understanding a multi component system that works together.
In an effort to provide the best possible educational experience for clinical rehabilitation application of neuroanatomy, I was on a mission. Having a core, base knowledge review of the nervous system is essential when leading into talking about dysfunction and disease of that system. I went on a search for anatomical depictions that could clearly identify the structures and processes I was trying to portray. New books from the library and books I own from when I was in college serve as great resources when trying to get back into studying the specifics, but do not offer the opportunity to easily get these images into a powerpoint. Online resources are also challenging. I am learning how time consuming the process can be to determine who owns the online image, if it is free to copy, save and utilize for my own teaching purposes, or if I need to go through the process of requesting permissions for use.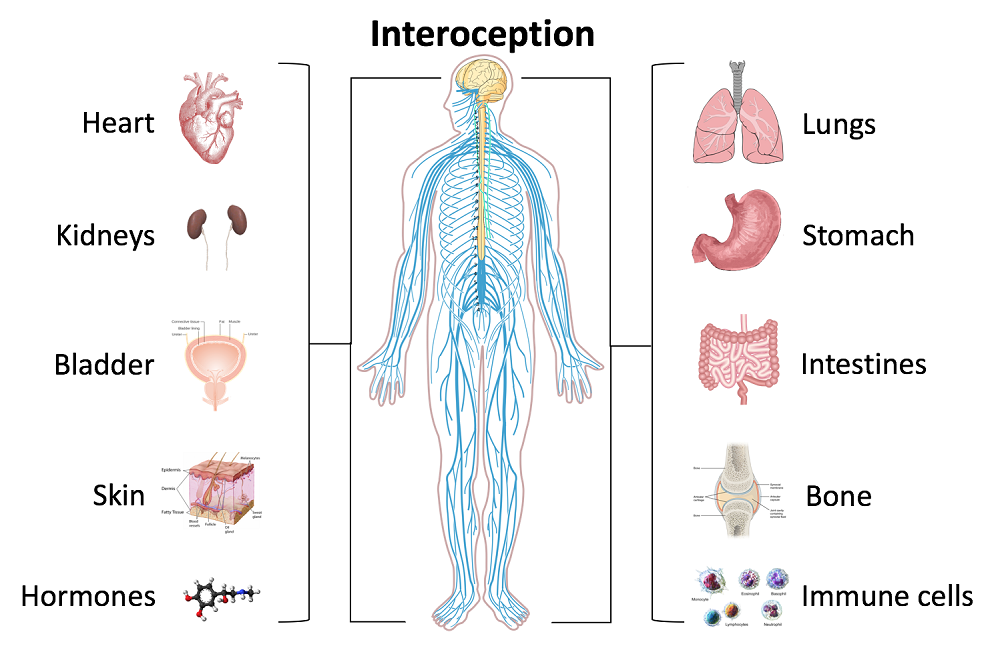
Through my employer, where I treat patients in the clinic, I have access to a program called Primal Pictures. I had used this in the past for clinic related marketing presentations and educational materials for patients and other clinicians I have mentored. Looking into the product further, I came to find out that there is a newer version of the program which offered so many more options. A truly unlimited amount of images which can be manipulated into an optimal position depicting the most clear neuroanatomical views I have ever been able to find. Not only does it provide me with the images I need in order to depict the treacherous pathways of the nerves in our body, but it also provides some amazing depictions of the physiological processes that occur within our nervous system to allow for healthy day to day functioning and protection of our bodies.
I also came across the title of a journal article that I was sure would provide some excellent depictions of neuroanatomy. The article titled, Sectional Neuroanatomy of the Pelvic Floor, provides cross sectional views of both the male and female pelvises. I obtained the article which has an excellent color-coded system, each nerve colored the same as the muscles and skin surface it innervates, going from superior to inferior cross sections. This makes for a clear understanding of each structures anatomical position. It is a great reference when looking at the anatomical relationships to adjacent structures and can help guide palpation skills. The article was more specifically written for physicians to best direct needle procedures/injections in the most accurate location possible when targeting nerves and structures. Neuroanatomy and physiology can be essential to understanding certain patient populations we encounter as we practice pelvic floor rehabilitation. Having clear depictions to refer to can help you provide the best possible base knowledge to your patients as you help them understand the challenges they face and how to overcome them.
Kass, J. S., Chiou-Tan, F. Y., Harrell, J. S., Zhang, H., & Taber, K. H. (2010). Sectional neuroanatomy of the pelvic floor. Journal of computer assisted tomography, 34(3), 473-477.
While my dad was visiting Michigan, we had the day to ourselves as my kids were in school. I was so excited to have quality time with my dad. Unfortunately it was pouring down rain. We decided on a leisurely brunch and then a movie. Dad chose the movie, “Wind River.” While not a movie I would normally pick, I was happy to go along. A little more than half way through…there was a horribly violent scene against a young women. I panicked, plugged my ears and closed my eyes. Unfortunately some images were burned into the back of my mind. When the movie was over, I remained seated and tears just came. My dad held me while I cried. I was able to calm down and leave the theater, but the images continued to bother me. During the next few days, I made it a priority to care for myself and allow my nervous system to process and heal.
 What happened to me? I have never had any traumatic personal experience. Why did I react so strongly? I talked with my therapist about it and she suggested I might have experienced secondary traumatic stress. We know, as pelvic health therapists, we need extra time to hear the “stories” of new patients. We do our best to create a safe space for them so they can trust us and we can help them discover pathways to healing. Yet no one has taught us what we are supposed to do with the traumatic stories our patients share. How are we to cope with holding space for their pain? How do we put on a happy face as we exit the room to get the next patient?
What happened to me? I have never had any traumatic personal experience. Why did I react so strongly? I talked with my therapist about it and she suggested I might have experienced secondary traumatic stress. We know, as pelvic health therapists, we need extra time to hear the “stories” of new patients. We do our best to create a safe space for them so they can trust us and we can help them discover pathways to healing. Yet no one has taught us what we are supposed to do with the traumatic stories our patients share. How are we to cope with holding space for their pain? How do we put on a happy face as we exit the room to get the next patient?
Teaching Capstone over the last few years, Nari Clemons and I have talked with many of you who were feeling emotionally overloaded especially when treating chronic pelvic pain and trauma survivors. Some of you were experiencing job burnout, others were deciding maybe it was time for a career shift, away from the pelvis. We realized something needed to be done as our field was losing talented pelvic health therapists. We have also struggled ourselves with various aspects of our profession.
There are no studies that directly look at job burn out, secondary traumatic stress, and compassion fatigue among pelvic health physical therapists. Yet these problems are common among social workers, physicians and other people groups in health care. There are individual as well as institutional risk factors that lead to the development of each. The solution, as one self-help module puts it, is developing resilience. A large part of this skill is making self-care a priority. The basics such as adequate sleep, nutrition, and exercise are foundational. Meditation, mindfulness, therapy, and spiritual practices, as well as supportive friends/groups are also imperative.
Nari and I realized that training to develop resilience in therapists was missing. Initially we equipped ourselves to have better boundaries, ground ourselves with meditation, mindfulness and exercise, which enhanced our skills in dealing with complex, chronic patients. We compiled what we have learned and want to share it with you. We would like to invite you to attend Holistic Interventions and Meditation: Boundaries, Self-Care, and Dialogue. We have designed this 3 day course to be partially educational and absolutely experiential. We are going to dig deeper into ways to calm our patient’s and our own nervous systems, explore and practice the latest recommendations on treatment of persistent pain, we will mediate and learn about mediation, play with essential oils, learn some new hands on techniques, and support and encourage one another as we build communication skills. We want you to leave feeling refreshed and equipped to continue to treat patients without losing yourself in the process. We want to invest in you so you can continue the investment you have made in your career and avoid job burnout, compassion fatigue and secondary trauma. We invite you to develop the resilience you need for a rewarding career in pelvic health physical therapy by joining us in Tampa this January.
Cieslak, R., Shoji, K., Douglas, A., Melville, E., Luszczynska, A., & Benight, C. C. (2014). A meta-analysis of the relationship between job burnout and secondary traumatic stress among workers with indirect exposure to trauma. Psychological services, 11(1), 75.
Meadors, P., Lamson, A., Swanson, M., White, M., & Sira, N. (2010). Secondary traumatization in pediatric healthcare providers: Compassion fatigue, burnout, and secondary traumatic stress. OMEGA-Journal of Death and Dying, 60(2), 103-128.
Sodeke-Gregson, E. A., Holttum, S., & Billings, J. (2013). Compassion satisfaction, burnout, and secondary traumatic stress in UK therapists who work with adult trauma clients. European journal of psychotraumatology, 4(1), 21869.
Stearns, S., & Benight, C. C. (2016). Organizational Factors in Burnout and Secondary Traumatic Stress. In Secondary Trauma and Burnout in Military Behavioral Health Providers (pp. 85-113). Palgrave Macmillan US.