Allison Ariail, PT, DPT, CLT-LAANA, BCB-PMD is one of the creators of the Herman & Wallace Oncology of the Pelvic Floor Course Series. Allison Ariail is a physical therapist who started working in oncology in 2007 when she became certified as a lymphatic therapist. She worked with breast cancer, lymphedema patients, head and neck cancer patients, and the overall oncology team to work with the whole patient to help them get better. When writing these courses, Allison was part of a knowledgeable team that included Amy Sides and Nicole Dugan among others.
March is Colorectal Cancer Awareness Month. Did you know that the incidence rate of colorectal cancers is increasing? According to the International Agency for Research on Cancer, 1.9 million new cases of colorectal cancer were identified worldwide in 2020. This number is expected to grow even more. It is predicted that by 2040 the number of new cases of colorectal cancer will rise to 3.2 million new cases a year, and 1.6 million annual deaths worldwide. Additionally, did you know due to the fact that the incidence rate is increasing and it is being diagnosed in younger individuals, the age for screening for colorectal cancer has lowered to 45? At age 45 individuals should begin regular screening for colorectal cancer either via stool-based testing or visual-based screening via a colonoscopy. If someone has risk factors they may need to begin screening at a younger age.
Colorectal cancer can often be preventable through modifiable risk factors. Changing some of these risk factors, alongside the detection and removal of precancerous lesions can lower someone's risks. However, if a diagnosis is made, treatment can help to prolong the life of the patient. The treatment can include various surgeries, chemotherapy, and radiation. All of these treatments can cause changes to a patient's body. A rehab professional that has knowledge about both the body and how the medical treatment of cancer causes changes, can make all the difference in the world for that patient returning to activities that they enjoy and love after treatment.
There are not many opportunities for rehab professionals to learn about these changes and how we can help these patients. However, Herman & Wallace has a series focused on helping oncology patients. In this series, techniques are learned that can help colorectal cancer patients recover from their diagnosis and the medical treatment they go through. The oncology series is online and offered several times a year. You can attend the upcoming oncology courses on: Oncology of the Pelvic Floor Level 1 scheduled for July 8-9 and December 2-3, Level 2A scheduled for May 20--21, and Level 2B scheduled for December 9-10.
Reference:
Morgan E, Arnold M, Gini A, et al. Global burden of colorectal cancer in 2020 and 2040: incidence and mortality estimates from GLOBOCAN. Colon. 2023; 72(2).
*Certified Lymphatic Therapists may skip Oncology of the Pelvic Floor Level 1 and move on to the Level 2A and Level 2B courses.*

Oncology of the Pelvic Floor Level 1 - no partner needed for registration
Price: $550.00 Experience Level: Beginner Contact Hours: 17.5 hours
The basics of the lymphatic system will be covered, as well as when to refer the patient to a lymphatic specialist for further treatment. Red flags and warning symptoms will be discussed so the participant feels comfortable with knowing when to refer the patient back to their medical provider for further assessment.
This introductory course is aimed to get the participant comfortable with working with oncology patients and as part of an interdisciplinary oncology team.
Course Dates: July 8-9 and December 2-3
Oncology of the Pelvic Floor Level 2A - partner needed for registration
Price: $495.00 Experience Level: Intermediate Contact Hours: 17.25 hours
This course was designed to build on the information that was presented in Oncology of the Pelvic Floor Level 1.
Information will be provided focusing on male pelvic cancers, colorectal cancer, and anal cancer including risk factors, diagnosis, and prognosis. The participant will also understand the sequelae of the medical treatment of cancer and how this can impact a patient's body and quality of life. Other topics include rehabilitation and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy.
Course Dates: May 20--21
Oncology of the Pelvic Floor Level 2B - partner needed for registration
Price: $600.00 Experience Level: Intermediate Contact Hours: 19.25 hours
This course was designed to build on the information that was presented in Oncology of the Pelvic Floor Level 1.
Information will be provided focusing on gynecological and bladder cancers including risk factors, diagnosis, and prognosis. The participant will also understand the sequelae of the medical treatment of cancer and how this can impact a patient’s body and quality of life. Other topics include rehabilitation and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy.
Course Dates: December 9-10
Nari Clemons - Actually, I used to have a meditation and neuroscience class for Herman Wallace. It was a shorter class. But, I felt it was lacking in tools for the provider. For example, as an empathic provider, I felt I was very aware, very mindful that I was losing energy, that I was "picking things up" from my patients, and that I was really not enjoying my job or life balance as much as I used to. I became ill and burnt out, working in this intensive field. It felt like the joy of my life was kind of being sucked up by my job. Jen and I launched our own journeys, together, trying to understand how this world of boundaries and balance could help us in our own lives. So much changed and grew from that. So, in time we decided to combine the two into one class, to help practitioners integrate meditation into their practice and life, but also how to come back to loving their jobs with balance, as we were able to.
What are the top 3 takeaways a practitioner could hope to gain from this class?
NC - 1. Better self-care in and out of the clinic. 2. A more effective and less taxing way to interact with clients, share responsibility, and communicate in more helpful ways for both practitioner and patient. 3. enjoying their life and having more energy for their life outside of work.
JVV - 1. You don’t have to do it all. 2. We want to support you with tools to help your patients take more responsibility for their care and their outcomes. 3. YOU ARE VALUABLE…and here are ways you can care for yourself, have healthy boundaries, and align your actions with your priorities so you can leave work at work and truly enjoy your life outside of work.
Who do you think needs to take this class?
NC - Any practitioner who is finding work more and more emotionally taxing or draining. Really, there are a few patterns that benefit from this class. People who over-give and over-function in relationships in their life, including patient relationships. Often there can be a bit of a people-pleasing tendency in these situations. Also and especially if a participant is one of those people who have always been a little sensitive to energy: feel things, pick up things, notice their energy changes when they interact with others. I feel like this is the only class I know of that specifically gives tools and strategies for this kind of provider.
JVV - EVERYONE! LOL. People who are wrestling with healthy work/life balance, who find themselves staying late after work or working through lunch, health care providers who tend to care more for their patients than they do for themselves, those of us who leave work drained and only have meager offerings of energy for our families.
What was your favorite feedback from participants in taking this class?
NC - We hear a lot from participants that other classes made them have better clinical skills, but this class has helped them to enjoy their own life and their job more and to feel more balanced and professional as they employ better boundaries and shared responsibility.
JVV - Ahhh, it is true joy when participants are empowered and equipped to set healthy boundaries, care for themselves, and feel more joy in their lives.
How is this class different from other classes through H&W?
NC - Kind of along the same lines, this class does give you skills for use with patients, but they are the skills that help your life feel better, and your job feels better. They give you permission to change your paradigm of treatment from "how much can I possibly give" to "how do I shift my job, self, and communication, to allow my job to be just one part of my life that is enjoyable and doesn't take so much energy away from the other parts of my life."
JVV - This is the only class that focuses both on skills to use for patients and skills to use FOR YOURSELF. To keep yourself healthy, balanced, and whole as a medical provider in a demanding, challenging role.
Why are there two parts to this class?
NC - Because it is a lot of information, a lot of life changes to integrate. It takes time. We like the idea of a month of growth and change. Participants do pre-work to prepare for the first weekend, which starts the process of change. Then, they do work in the following month and really work on the intensive integration, new habits, new patterns, and new neuronal networks. Then, we come back for another day for the second part of learning that participants will be ready for after integrating some of the basics of the first weekend.
JVV - We just had SO MUCH we wanted to share!! And we found having two classes spaced a month or so apart really lets participants ingest and apply one level of change before being ready and hungry for the next level. The first part focuses on establishing good boundaries with patients, self-care practices including meditation, and identifying areas of their lives that need support or intervention to be healthier. The second class dives deeper into thoughts, emotions, and actions. Practices like gratitude, visualization, and deeper mediation practices.
Boundaries, Self-Care, and Meditation - Part 1
Course Dates: March 18
Price: $400
Experience Level: Intermediate
Contact Hours: 12.5
Description: The instructors recommend completing this series in two parts to allow time to process and implement one leg of the journey before undertaking the next. Both Part One and Part Two have a significant amount of pre-work to digest and practice before meeting via Zoom. Please plan for up to 12 hours of pre-course work. This sets the stage for you to find your path to experiencing more joy, energy and balance.
In Part One, participants begin their process of study, meditation, and self-reflection in the weeks prior to the start of the class. Pre-work includes focus on the neuroscience of pain trauma, PTSD, and meditation. Participants will learn about the powerful influence both negative and positive experiences have on our nervous system’s structure and function. Personal meditation practice and instruction will create changes in the participant's own nervous system. Participants will also learn how to prescribe meditation for various patient personalities and needs, as well as analyze yourself through inventories on coping, self-care, empathy, burnout, values, as well as track how you spend your time. Commitment to pre-work will facilitate rich discussion as we put what you have learned into practice around building a shared responsibility model of patient care, language to support difficult patients, and both visualizing and planning steps to create new, healthier patterns in your life and in your practice.
Lila Abbate, PT, DPT, MS, OCS, WCS, PRPC is a Board-Certified Specialist by the American Physical Therapy Association in Orthopedics (OCS) 2004 and Women’s Health (WCS) 2011. She has obtained the Certified Pelvic Rehabilitation Practitioner (PRPC) in 2014. She is a Diane Lee/LJ Lee, Integrated Systems Model (ISM) graduate and completed the New York series in 2012. Dr. Abbate is Senior Faculty with Herman & Wallace and can be found instructing the Pelvic Floor Series as well as her own courses Coccydynia and Painful Sitting and Bowel Pathology and Function.
Pain with sitting is a common complaint that patients may present to the clinic with. While excess sitting has been shown to be detrimental to the human body, sitting is part of our everyday culture ranging from sitting at a meal, traveling in the car, or doing work at a desk. Often, physical therapists disregard the coccyx or tailbone as the possible pain generator, simply because they are fearful of assessing it, have no idea where it is, or have never learned about it being a pain generator in their education.
Coccydynia is the general term for “pain over the coccyx.” Patients with coccydynia will complain of pain with sitting or transitioning from sitting to standing. Despite the coccyx being such a small bone at the end of the spine, it serves as a large attachment site for many important structures of interest that are important in pelvic floor support and continence:¹
- Anterior Tip: Iliococcygeus and pubococcygeus, Sacrococcygeal ligament
- Lateral: Coccygeal muscles which runs parallel with the sacrospinous ligament
- Posteriorly: Fibers of gluteus maximus and sacrotuberous ligament
Along with serving as a major attachment site for the above structures it provides support for weight bearing in the seated position and provides structural support for the anus. However, the coccyx is only 10% weightbearing, so what seems to go wrong that this bone is taking the brunt of the weightbearing? Women are five times more likely to develop coccydynia than men, with the most common cause being an external trauma like a fall or an internal trauma like a difficult childbirth.1,2 In a study of 57 women suffering from postpartum coccydynia, most deliveries that resulted in coccyx pain were from the use of instruments such as forceps delivery or vacuum-assisted delivery. A BMI over 27 and having greater than or equal to 2 vaginal deliveries resulted in a higher rate of coccyx luxation during birth. ³ Other causes of coccyx pain can be non-traumatic such as rapid weight loss leading to loss of cushioning in sitting, hypermobility or hypomobility of the sacrococcygeal joint, infections like a pilonidal cyst, or pelvic floor muscle dysfunction.¹ When assessing a patient with coccyx pain, it is also of the utmost importance to rule out red flags, as there are multiple cases cited in the literature of tumors such as retro rectal tumors or cysts being the cause of coccyx pain. These masses must be examined by a doctor to determine if they are malignant or benign and if excision is necessary. Quite often, these masses can be felt as a bulge on rectal examination.4,5
A multidisciplinary approach including physical therapy, ergonomic adaptations, medications, injections, and, possibly, psychotherapy leads to the greatest chance of success in patients with prolonged coccyx pain.1 Special wedge-shaped sitting cushions can provide relief for patients in sitting and help return them to their social activities during treatment. Physical therapy includes manual manipulation and internal work to the pelvic floor muscles to alleviate internal spasms and ligament pain. Intrarectal coccyx manipulation can potentially realign a dislocated sacrococcygeal joint or coccyx.1 Unique taping methods demonstrated in video by Dr. Abbate, can be used as a follow-up to coccyx manipulation to help hold the coccyx in the new position and allow for optimal healing. Often coccyx pain patients have concomitant pathologies such as pelvic floor muscle dysfunction, sacroiliac or lumbar spine pain, and various other orthopedic findings that are beneficial to address. When conservative treatments fail, injections or a possible coccygectomy may be considered.
Luckily conservative treatment is successful in about 90% of cases.¹ Join Lila Abbate in her upcoming Coccydynia and Painful Sitting remote course on March 31st. By learning how to treat coccyx pain appropriately, you will be a key provider in solving many unresolved sitting pain cases that are not resolved with traditional orthopedic physical therapy.
References:
1. Lirette L, Chaiban G, Tolba R, et al. Coccydynia: An overview of the anatomy, etiology, and treatment of coccyx pain. The Ochsner Journal. 2014; 14:84-87.
2. Marinko L, Pecci M. Clinical Decision Making for the Evaluation and Management of Coccydynia: 2 Case Reports. JOSPT. 2014; 44(8): 615
3. Maigne JY, Rusakiewicz F, Diouf M. Postpartum coccydynia: a case series study of 57 women. Eur J Phys Rehabil Med. 2012; 48 (3): 387-392.
4. Levine R, Qu Z, Wasvary H. Retrorectal Teratoma. A rare cause of pain in the tailbone. Indian J Surg. 2013; 75(2): 147-148.
5. Suhani K, Ali S, Aggarwal L, et al. Retrorectal cystic hamartoma: A problematic tail. J Surg Tech Case Rep. 2104; 6(2): 56-60.
Coccydynia and Painful Sitting
Course Dates: March 31, June 17, September 22, and December 10
Price: $175
Experience Level: Intermediate
Contact Hours: 5.5
Description: Coccyx pain is a common, frustrating condition for the patient who often has difficulty sitting, one of the most important tasks necessary for daily activity. Patients who find help from a pelvic rehabilitation provider have often experienced pain near the tailbone for long periods of time, leading to chronic pain in addition to neuromusculoskeletal dysfunctions. This one-day, remote continuing education course allows the therapist to focus on this vital, sensitive area to learn and refine skills in assessment and treatment. Anatomy, pathology, and palpation skills of the coccyx region are instructed.
This course includes a video lab on both internal and external neuromuscular taping techniques which can immediately be applied in the clinic. This course also includes a review of seating options to reduce pain.
Fun fact: Did you know that the pelvis fans and folds just like the hand and foot?
Ischial tuberosities change position and move medial to lateral and back based on the functional task. Pelvic floor muscles length and fascial integrity and its ability to conform to demands become an important factor in treating painful sitting.
The one-day course gives you a basic anatomy review and discusses the biomechanics of sitting and the difference of quadruped and its assessment. External coccyx treatments are explained and reviewed through video format along with a discussion to assist patients in making good decisions using sitting relief pillows. You will learn 5 basic tips to know if your patient has true coccydynia or if the pain is being driven from elsewhere up or down the chain. A review of the literature and how the medical community views basic coccydynia and which medical interventions can assist patients with long-standing sitting pain.
Pelvic Rehab Report
The official Herman & Wallace blog. New blogs post every Friday on topics relating to the field of pelvic floor dysfunction.
Sarah Hughes PT, DPT, OCS, CF - L2 has been practicing PT since 2007 and opened her private practice, Arrow Physical Therapy in 2016. She now owns and operates Arrow remotely while residing in the Chicago area and practicing at Outlier Physical Therapy. Her specialties include dance medicine, the CrossFit and weightlifting athlete and conditions of the hip and pelvis such as femoroacetabular impingement and labral tears. Dr. Hughes earned a BS in exercise science from Gonzaga University and a DPT from the University of Washington, she wrote and instructs Weightlifting and Functional Fitness Athletes.
Mobility. What is it and how can we get more of it?? In the CrossFit world, athletes can be really fixated on mobility.
- This feels tight.
- That feels restricted.
- I can’t squat below parallel because my ankles are tight.
- I can’t press fully overhead because my lats are locked up.
- I know I just need to foam roll more.
- I’ve been doing this mobility program but I still can’t make progress

Don’t let these athletes fool you. They may be strong and look capable in their functional fitness, but often there is a REASON they feel tight, and it’s not because they need more passive motion. Many CrossFit athletes spend their warm-up time lying on foam rollers, stretching with heavy resistance bands, static stretching, and using percussion guns and other mobility tools.
But, what IS mobility? Mobility is defined as the ability of a joint to move actively through a range of motion. Mobility is about controlling your body through a full range of active movement; much different than passively stretching into a position. And, mobility can only be achieved with strength training, neuromotor retraining, appropriate exercise prescription and PRACTICE. Keep these athletes in your sights as they perform the exercises. Don’t get caught giving them too much freedom to only see you for manual work and then do a home program alone. No online program that they can purchase will ever replace your education and ability to help them with mobility drills.
Are your patients stretching and stretching without the increased mobility they are looking for? Are you doing manual work that is targeted and effective but only getting you so far with them? Try some stability drills and strength training exercises! In the Weightlifting and Functional Fitness Athletes - Remote Course we will look at different CrossFit requirements and what these athletes need. HINT: it's not more foam rolling!!
Weightlifting and Functional Fitness Athletes

Course Dates: March 4, May 13, and October 14
Price: $295
Experience Level: Beginner
Contact Hours: 9
Description: When it comes to Crossfit and Weightlifting, opinions are divided among Physical Therapists and other clinicians. Why is it that these sports cause such strong differences among rehab professionals? In this half-day, remote continuing education course, instructor Sarah Haran PT, DPT, OCS, CF-L2 looks at the realities and myths related to Crossfit and high-level weight-lifting with the goal of answering “how can we meet these athletes where they are in order to keep them healthy, happy and performing in the sport they love?"
This course will review the history and style of Crossfit exercise and Weightlifting, as well as examine the role that therapists must play for these athletes. Common orthopedic issues presented to the clinic will be examined. Labs will introduce and practice the movements of Crossfit and Weightlifting, discussing the points of performance for each movement. The practitioner will not only learn how to speak the language of the athlete but will experience what the movement feels like so that they may help their client to break it down into its components for a sport-specific rehab progression. The goal of this course is to provide a realistic breakdown of what these athletes are doing on a daily basis and to help remove the stigma that this type of exercise is bad for our patients. It will be important to examine the holes in training for these athletes as well as where we are lacking as therapists in our ability to help these individuals. We will also discuss mindset and culture issues such as the use of exercise gear (i.e. straps or a weightlifting belt), body image, and the concept of "lifestyle fitness". Finally, we will discuss marketing our practices to these patients.
Rachna Mehta, PT, DPT, CIMT, OCS, PRPC, RTY 200 is the author and instructor of the Acupressure for Optimal Pelvic Health course. Rachna brings a wealth of experience to her physical therapy practice and has a personal interest in various eastern holistic healing traditions.
As I walked into the room to greet a new patient, I quickly glanced at the prescription for Pelvic Floor Physical Therapy in her chart. The words “urinary retention” caught my attention. As I gathered her history, I learned that this patient had a history of high anxiety and had been to the ER twice within a few weeks with symptoms of urinary retention. She was now taught to self-catheterize herself to manage her symptoms. After comprehensive testing by her urologist ruled out obstructive and neurological causes, she was referred to pelvic floor therapy with a diagnosis of pelvic floor muscle tension and inability to relax her pelvic floor muscles.
Urinary retention, or the inability to voluntarily void urine, is one of the most prevalent presenting urologic complaints in the emergency department. Voluntary urination requires close coordination between muscles of the pelvic floor, bladder, and urethra, as well as the nerves innervating them.
Female urinary retention is either acute or chronic and can be categorized according to the International Continence Society as:
- Complete (full retention) or partial (high post-void residuals)
- Acute or chronic
- Symptomatic or asymptomatic
- Mechanism (obstructive or non-obstructive)
Two of the most common causes of chronic urinary retention in women are bladder muscle dysfunction and obstruction. The condition is important as it can lead to significant clinical problems if left untreated, such as bladder decompensation, hydronephrosis, renal failure, vesicoureteral reflux, nephrolithiasis, and urinary tract infections, as well as symptoms including suprapubic pain, feelings of incomplete emptying, weak urinary stream, urgency, and incontinence1.
The patient was anxious and worried and could not step out more than an hour away from her home as she feared she would need to return home to void. She could only void at her own home and her social life was extremely limited due to these voiding restrictions. Given her high anxiety, I initiated Acupressure points for Anxiety in her program as an evidence-based holistic practice.
Acupressure is widely considered to be a powerful Complementary & Alternative Medicine (CAM) therapy and is gaining acceptance within the medical community as part of an Integrative medicine approach. It draws its roots from Acupuncture which is part of Traditional Chinese Medicine (TCM) believed to be over 3000 years old. TCM is based on Meridian theory where key Acupressure points (or Acupoints ) lie along specific meridian lines and are connected to the visceral functions of vital organ systems.
Research shows that Acupressure points have been used with Emotional Freedom Techniques (EFT) as well as for the management of pain, anxiety, nausea, fatigue, urinary incontinence, constipation, and symptom management. Studies over the past few decades have found that Acupressure points transmit energy or the vital Qi (life force energy ) through interstitial connective tissue with potentially powerful integrative applications through multiple systems.
Acupressure has demonstrated the ability to improve heart rate variability, and thus decrease sympathetic nervous system activity. By decreasing sympathetic nervous system stimulation, the release of stress hormones such as epinephrine and cortisol is decreased, and the relaxation response can be augmented, which may correlate with decreasing levels of pain, stress, and anxiety2.
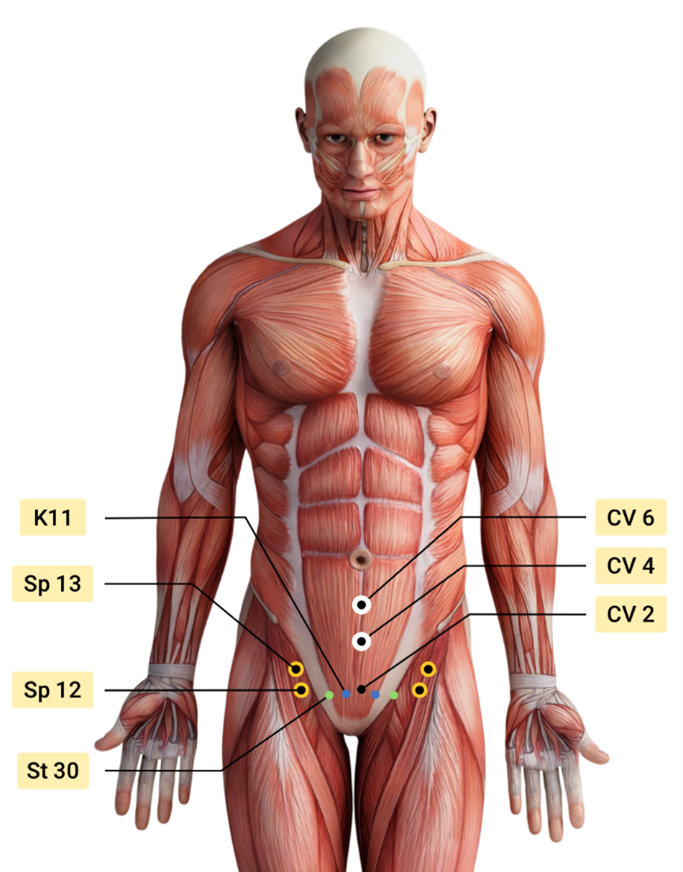
Over the next few weeks, the patient was treated by a multidisciplinary team including her Primary Care Physician, Psychologist, Acupuncturist, and Pelvic floor Physical Therapist. Integrating Acupressure along with manual therapy, behavioral modifications, exercises, breath work and stretching, key potent points in the Central Channel, Kidney, Stomach, Spleen, and Bladder meridians were utilized to down-regulate her nervous system and improve the physiological functioning of her vital organs.
The patient was also taught to use perineal acupressure points for the management of intermittent constipation. The patient learned and practiced daily an Acupressure Anxiety points regimen along with traditional rehabilitation exercises, and became calmer and more mindful with complete resolution of urinary retention symptoms. She could now step outside her home and use public bathrooms which socially was a big achievement for her.
The course Acupressure for Optimal Pelvic Health next offered on Feb 4th -5th 2023 explores Acupressure as an evidence-based modality for the management of Anxiety, Stress, Pain, and Symptom management. The course also teaches two programs with specific potent points for Anxiety and for Daily Wellness and introduces Yin Yoga as a complementary practice to Acupressure. This course is curated and taught by Rachna Mehta PT, DPT, CIMT, PRPC, RYT 200. Rachna has integrated Acupressure as part of her rehabilitation toolbox for several years now bringing holistic healing and wellness to her patients.
References
- Leslie SW, Rawla P, Dougherty JM. Female Urinary Retention. [Updated 2022 Nov 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538497/
- Monson E, Arney D, Benham B, et al. Beyond Pills: Acupressure Impact on Self-Rated Pain and Anxiety Scores. J Altern Complement Med. 2019;25(5):517-521.
- Au DW, Tsang HW, Ling PP, Leung CH, Ip PK, Cheung WM. Effects of acupressure on anxiety: a systematic review and meta-analysis. Acupunct Med. 2015;33(5):353-359. doi:10.1136/acupmed-2014-010720
- Son CG. Clinical application of single acupoint (HT7). Integr Med Res. 2019;8(4):227-228.
- Kwon CY, Lee B. Acupuncture or Acupressure on Yintang (EX-HN 3) for Anxiety: A Preliminary Review. Med Acupunct. 2018;30(2):73-79.
- Abbott, R., Ayres, I., Hui, E. et al. Effect of Perineal Self-Acupressure on Constipation: A Randomized Controlled Trial. J GEN INTERN MED30, 434–439 (2015).
Acupressure for Optimal Pelvic Health
Course Dates:
February 4-5, June 3-4, October 14-15
Price: $450
Experience Level: Beginner
Contact Hours: 12.50
Description: This continuing education course is a two-day seminar that offers participants an evidence-based perspective on the application of Acupressure for evaluating and treating a host of pelvic health conditions including bowel, bladder, and pelvic pain issues. The course explores a brief history of Acupressure, its roots in Acupuncture and Traditional Chinese Medicine (TCM), and presents current evidence that supports the use of complementary and alternative medicine as an adjunct to western medicine. TCM concepts of Meridian theory and energy channels are presented with scientific evidence of Acupoints transmitting energy through interstitial connective tissue with potentially powerful integrative applications through multiple systems.
Lectures will present evidence on the use of potent Acupressure points and combinations of points for treating a variety of pelvic health conditions including chronic pelvic pain, dysmenorrhea, constipation, digestive disturbances, and urinary dysfunctions to name a few. Key acupoints for decreasing anxiety, stress, and bringing the body back to a state of physiological balance are integrated throughout the course.
Participants will be instructed through live lectures and demonstrations on the anatomic location and mapping of acupressure points along five major meridians including the spleen, stomach, kidney, urinary bladder, and gall bladder meridians. Key associated points in the pericardium, large intestine, small intestine, lung, and liver meridians as well as the governing and conception vessels will also be introduced. The course offers a brief introduction to Yin yoga and explores Yin poses within each meridian to channelize energy through neurodynamic pathways to promote healing across multiple systems. Participants will learn how to create home programs and exercise sequences and will be able to integrate acupressure and Yin yoga into their orthopedic and pelvic health interventions.
Hina Sheth MS, PT, OCS, MTC, IADN-cert is the owner and practitioner of Rebalance Physical Therapy, a one-on-one holistic manual physical therapy practice in Philadelphia, PA. She is a board-certified physical therapist, and orthopedic specialist, as well as a certified manual therapist with more than 22 years of specialization in the limbo-pelvic-hip complex. Sheth’s practice in functional health coaching helps clients adopt behavioral changes that nourish improved health.
A respected colleague and community leader, Sheth shares her expertise in public forums as well as the academy, offering lectures on a host of physical therapy topics including spinal dysfunction and pelvic pain. A writer for the American Physical Therapy Association (APTA) women’s specialist exam, Sheth has participated in National Institutes of Health (NIH) funded studies for pelvic health. Sheth’s articles appear in two urologic volumes, and her insights about physical therapy and wellness are frequently featured by local and national media outlets including NPR, Livestrong, IC today, mainline health, and Philly magazine.
Pelvic health has become more accepted in the healthcare field, especially with social media helping reach those in search of more pelvic health knowledge. But there needs to be more public awareness on the topic of pelvic pain and sexual pain - in all genders. When TEDx reached out to me to develop this talk, I was so excited. Finally, what years ago, used to be a “taboo” topic was now gaining attention as something that needed to be voiced and spread on a larger platform.
The TED community is a perfect platform for those seeking validity to their symptoms as well as a way for them to communicate their symptoms to their friends and family. I focused on making this often difficult topic approachable. I hope that this talk helps those dealing with these issues feel understood, supported, and empowered. I also hope that this talk can be used to help teach their loved ones and other healthcare professionals that this is something that can be helped by pelvic floor therapists around the world. I hope you all can help this message spread!
Herman & Wallace faculty member Dr. Heather Rader has created an all-inclusive pelvic rehabilitation course for physical and occupational therapists who treat patients in the home health setting Home Health and Pelvic Rehab - External Skills for the Home Environment.
61% of females and 38% of males over the age of 65 have some form of urinary and fecal incontinence, and nearly half of the patients receiving home health care have incontinence1. Despite these statistics, bladder and bowel symptoms are relegated to being part of the medical history rather than treatable impairments.
Home health therapists are required to ask about the presence of urinary and fecal incontinence as part of the admittance form, known as the OASIS. That’s typically where the conversation ends. This course will teach therapists how to quickly screen for the type of urinary incontinence, constipation, and pelvic pain conditions with simple and unintimidating interview skills. This can open the door to meaningful treatment interventions.
One of the challenges that home health therapists have with conventional pelvic health education is the emphasis on internal pelvic floor examination. Home health therapists don’t have access to a hi-lo examination table or the necessary supplies for a typical pelvic floor muscle examination. This course teaches external examination skills that can be performed in a living room chair or on a couch.
Teaching pelvic floor exercises (Kegels) can be difficult in any setting or population. Cognitive impairments bring additional challenges. Learn how to teach “Kegel-less” exercises to facilitate pelvic floor strength through hip and trunk movements. The pelvic floor has anatomical and physiological relationships with the hip joint, spine, and abdominal muscles. Incontinence clusters with falls, balance, and gait dysfunction. Learning what these conditions have in common with each other allows the informed therapist to treat them together as co-morbidities.
This course is also a great place to start for therapists who want to explore pelvic rehabilitation techniques but aren’t ready for internal examination coursework. While the clinical examples are home health based, the concepts can be applied to any rehab setting.
Home health therapists are uniquely positioned to help our older population reduce the burden of incontinence, constipation, and untreated pelvic pain conditions. This course teaches easy-to-follow treatment pathways customized to the home care experience, giving the participant confidence to ask about and treat pelvic floor dysfunctions. Join Heather Rader on February 25th for Home Health and Pelvic Rehab.
Reference
- Prevalence of Incontinence Among Older Americans U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics. Prevalence of incontinence among older Americans. Hyattsville, Maryland, 2014. Print.

Course Date:
February 25th
Price: $450
Experience Level: Beginner
Contact Hours: 15
Description: This remote continuing education course includes 8 hours of pre-recorded lectures and one day of live remote content covering external pelvic rehab skills for the rehabilitation professional who works with patients in Home Health, Adult Day Care, Assisted Living, Extended Care, or Memory Care. This course is intended for therapists treating patients with the goal of staying in their current home setting and toileting as independently as possible. Topics include functional pelvic anatomy, function and dysfunction, and geriatric comorbidities, as well as pelvic health documentation skills. Topics specific to the home health setting include gaining consent in the home setting, how to include caregivers and staff in the pelvic rehab process, and external examination options and techniques. The live remote lecture will cover rehab strategies for urinary and fecal incontinence, constipation, and pelvic pain.
This course will focus on real-world examples of home health experiences in rehabilitation External evaluation and treatment techniques adapted to the home and bedside environment, including the use of biofeedback for pelvic floor muscle dysfunction and treatment protocols for co-morbidities, such as UTIs, falls and balance, and gait disorders.
Obtaining patient and caregiver consent for pelvic floor examinations and treatment adaptations to accommodate variable treatment surfaces (bed, chair, couch, wheelchair) will be discussed. Participants will receive reproducible handouts for patient and caregiver education and have skills labs on documentation compliance. This course will prepare the home health therapist to be ready and able to meet the urological and colorectal therapeutic needs of the homebound population.
Equipment needed for Labs: Home Health Bag, TheraBand, small air-filled ball, gait belt
Darla Cathcart, PT, DPT, WCS, CLT graduated from Louisiana State University (Shreveport, LA) with her physical therapy degree, performed residency training in Women’s Health PT at Duke University, and received her Ph.D. from the University of Arkansas Medical Sciences. Her dissertation research focus was on using non-invasive brain stimulation to augment behavioral interventions for women with lifelong vaginismus, and her ongoing line of research will continue to center around pain with intercourse. Darla is part of Herman & Wallace's core faculty and instructs Pelvic Floor Level 1, Level 2A, and Level 2B, the Pregnancy & Postpartum Series, and recently launched her own course Vaginismus and Vulvovaginal Dyspareunia.
How is this class different from the information in Pelvic Floor 2B?
The main difference is in the questions that these two courses answer: "what treatments can I use" versus "how can I use those treatments effectively?" In Pelvic Floor Level 2B, participants are told about various methods for addressing pain with intercourse (such as using vaginal trainers/dilators and manual therapy techniques), with brief descriptions of how to use some of these tools. In this Vaginismus and Vulvovaginal Dyspareunia course, we go into depth on how to use these treatments specifically based on a patient's examination findings and goals.
What are the top 5 takeaways a practitioner could hope to gain from this class?
1. Vaginal Trainers (dilators) can be more effective when going beyond "just sticking them in."Traditionally, patients have been taught to just insert "dilators" to a point of stretching and discomfort, and to hold that stretch, maybe even distract themselves from the activity by watching TV or reading a book. As with other areas of the body, using active methods to increase tissue flexibility, such as incorporating contract-relax and breathing techniques, can really enhance the treatment! During the labs in this 100% remote course (a combination of self-paced preview videos and live online instruction), participants will be guided through step-by-step instructions for using and progressing through vaginal trainers and other treatments (the same step-by-step instructions you can use with your patients on Monday morning!). Additionally, as in other areas of the body, focusing on the body part that is being worked on is beneficial for increasing motor control, which is also desirable for addressing pelvic floor muscles that have too much tone and tenderness or pain with attempts at insertion. Participants will also be walked through activities that increase the brain's connection with and control of the pelvic floor and genitals, thus tapping into contemporary pain science concepts as well. And speaking of pain science . . .
2. As a practitioner, you likely already know that our words, verbiage for questions and instruction, and analogies and stories matter! Throughout the course, we will talk about why some words or terms can be harmful or less helpful, and how to replace them with healing or more neutral terms. For instance, we will talk about how the traditional term "dilator" can be a bit scary and anxiety-provoking for someone who has had lifelong vaginismus; but the term "trainer" suggests that the muscles are being taught and retrained on how to function. We will also walk through examples of approaching and discussing sexual abuse and trauma, general sexual history and activity, and patient goals. We will review some basics about contemporary pain science, and analogies that we can share with our patients to help decrease their fear and anxiety surrounding treatment for and engaging in sexual function. Participants should leave the course feeling more confident in talking about sex with their patients!
3. How do we incorporate the female sexual cycle/response (arousal, desire, orgasm), sexual positioning, and sexual assist devices and props into helping our patients? These are topics that will be tackled and broken down in both the preview material, with key concepts being reviewed or covered during the live remote portion of the course. We will talk about using the timing of sexual responses to a patient's advantage with transitioning to sexual function.
4. When should a patient move from vaginal trainers to the bedroom? Should the patient's partner(s) be involved? How do I answer questions about specific sexual positions? How do I answer my patient's questions about libido concerns? These are all concepts that will be tackled, with both specific examples and cases and also with general guidelines for applying the information to your individual patients.
5. You will have the opportunity to practice or follow along with the very things you will teach your patients during the live remote lab portion of the course, from the privacy of your own home or private treatment room in your office. I believe a great advantage that rehabilitation professionals have in treating patients is that we have experienced many of the examination and treatment techniques while practicing them in a class, course, or another setting. Personally testing out these techniques gives you, as a practitioner, a strong advantage in knowing how to best describe the nuances of applying treatments to aid in your patient's understanding. It also gives you a good dose of empathy for being the person on the table!
What special interest do you have in this topic?
As a pelvic health therapist for over 20 years, working with patients who have lifelong vaginismus, acquired vaginismus, and dyspareunia has been one of my primary passions. In completing a Ph.D. in 2020, my line of research began with a clinical randomized controlled trial working with patients with lifelong vaginismus and vaginal trainers, using neuroscience and pain science concepts to incorporate contract-relax and breathing techniques to enhance treatment. I never tire of having a patient return to the clinic excited that they finally had pain-free intercourse! I am passionate about teaching other therapists, healthcare providers, patients, and their partners about the concepts I've learned in my many years of practice.
Who is the audience for this class?
This course is for any pelvic health rehabilitation or health care provider who is a novice or wants to enhance their skills for working with patients with vaginismus and vulvovaginal dyspareunia.
Why was it needed and developed?
This course, Vaginismus and Vulvovaginal Dyspareunia, is needed to move beyond the basic concepts about what we can do to help patients having pain with intercourse. This course takes a deep dive into the detail of how to make the rubber meet the road to not only get treatment started but to really help progress a patient into a satisfying sex life. This course was developed so that the participant could leave this course and understand how to really approach the examination, history taking, and step-by-step procedures in instructing and using vaginal trainers and other tools for patients having painful intercourse. Additionally, this course should increase the practitioner's confidence in incorporating instructions and education related to a patient's concerns about the female sexual cycle and response (arousal, desire, orgasm), sexual positioning, lubrication, and partner integration.
Vaginismus and Vulvovaginal Dyspareunia
Course Date:
February 4
Price: $375
Experience Level: Beginner
Contact Hours: 15
Description: This course is for the pelvic health practitioner who is new to treating patients with vaginismus/vulvovaginal dyspareunia or to vaginal trainer(dilator) use or pelvic health rehabilitation; or for the experienced practitioner who has found that patients with vaginismus/vulvovaginal dyspareunia plateau with vaginal trainers or other treatments. In this course, pelvic health rehabilitation providers will learn about the different types of vaginismus and dyspareunia. Definitions and history of terminology will be explained related to pain with sexual activity and intercourse, including Genito-Pelvic Pain/Penetration Disorder, Lifelong or Primary Vaginismus, Acquired or Secondary Vaginismus, Dyspareunia, Vulvodynia, and others.
From a pain-science viewpoint, verbiage and terminology to reduce patient fear and anxiety will be discussed and incorporated throughout the course. Evidence for focalized dystonia as a component of lifelong vaginismus and how that impacts treatment will be reviewed. Causes for acquired vaginismus (such as postpartum healing or hormonal changes) will be addressed. Treatment approaches for reducing patient fear and anxiety, addressing medical and/or sexual trauma/abuse history, and promoting patient empowerment will be covered. The remote live portion of the course will also focus on rehabilitation treatments, including walking the participant through the functional use of vaginal trainers (commonly known as dilators), and methods for progressing their use. Clinical cases will be provided to illustrate a variety of treatment approaches based on different patients’ treatment goals, history, examination findings, and sexual pain diagnosis.

Hello Practitioners!
This Monday I would like to share a very special invitation with you. Join us in Seattle, WA for HWConnect 2023 - the first-ever conference from Herman & Wallace, the leading provider of continuing education to pelvic rehabilitation professionals. HWConnect 2023 will run Friday, October 6 - Sunday, October 8 and comprises 10+ contact hours of continuing education.
The Saturday night Keynote Presentation will be given by Diane Lee, an internationally-recognized expert with 40 years of clinical experience in thoracic, lumbar, and pelvic disability and pain. Diane will be delivering our Saturday night keynote address and will be presenting her latest research on diastasis rectus abdominis.
Registration includes access to all scheduled lectures and receptions, as well as a Teachable (a digital learning platform) course which will contain additional resources and a conference manual. Cocktail receptions will follow the speakers on Friday and Saturday evenings, so attendees will have a chance to have fun and socialize with each other, HW faculty, and conference presenters.
We have secured a room block and special pricing for registrants of this conference. Staying at the host hotel will be the most convenient option, so we highly encourage everyone to make arrangements via this URL before the room block is full!
After years of pandemic quarantine and Zoom meetings, we feel the need to gather together and connect our community again. HW Connect is an opportunity to meet with colleagues and friends old and new, and a unique chance to learn new skills and information from some of the leading voices in our field. Speakers will cover a range of topics related to pelvic rehab.
We’re several years into our COVID pivot, and while the remote and satellite learning options work great for delivering education, what’s missing is the opportunity to connect face-to-face with our community. Participants miss the chance to gather in person, and so do we.
HWConnect is a chance for friends and colleagues old and new to connect with one another and with some of the founding pioneers in our industry. Putting on a big conference is something we’ve wanted to do for years. After two years of Zoom meetings, now is the time.
We can’t wait to connect with you in October!
HWConnect

Announcement Week Registration Price Until January 28th:
$525
Early registration before March 15th: $545
Full price: $595
Schedule:
Friday, October 6th
5:30 PM - 8:30 PM
Saturday, October 7th
9:00 AM - 8:30 PM
Sunday, October 8th
9:00 AM - 12:15 PM