Boundaries, Self-Care, and Meditation Part 1 and Boundaries, Self-Care and Meditation Part 2, scheduled for November 23, are instructed by Nari Clemons, PT, PRPC and Jenna Ross, MSPT, BCB-PMD, PRPC.
Women are often socialized to be these kinds of words: sweet, likable, giving, generous, helpful, and accommodating. If that bend of conditioning is particularly strong, it shapes our relationships and our career choices. We often choose a career that makes us feel like we are being sweet, helpful, and generous. These traits serve others around us well, and they may increase our likability with others. We begin to see our likability as how much we embody these traits, and we can see our worth to others and ourselves as how much we show up in this one-dimensional way to others.
Taken to an extreme, this starts to look like being uber-available for patients calling them on our own time, emailing from home, running over in sessions to give the patient everything they could possibly get from a session, adding in hours to accommodate a patient, writing our notes during our lunchtime, and finding that resource for our patient by searching the web for an hour.
“Tis better to give than receive” or “giving them the shirt off our back” may be mantras we use or grew up with. But is it really true? Is giving more than we receive actually sustainable as a model? And if you give someone the shirt off your back, what would you wear? So many of the models we are raised to see as virtuous are actually rooted in martyrdom and are the hallmarks of poor boundaries.
When we hyper-inflate the “likable” characteristics of ourselves, it is often because we are deeply afraid of being seen as selfish, unlikable, or worst of all, a bi#ch. But why? We make these traits shadows…the traits to deny in ourselves and go to extreme lengths to hide from ourselves and others. Maybe instead, these are the very traits that can help us to understand where we need to set a boundary, rest, or realize we really don’t want to say yes to that added demand.
They can remind us of our energy limits and draw lines that help us have more room for joy, fun, and self-care. If we could honor these shadow traits as helpful protectors of ourselves, we could consider our happiness and balance equally as important as our patients’ happiness and balance. We could find ways to leave work on time to make it to that fun dance class, and we could empower our patients to have greater self-sufficiency. Often, when we are conflicted or tired, we can do well to ask ourselves, “What would a selfish bi#ch do?” The answer is usually what our being needs for balance, but we are too afraid to embrace our shadow to acknowledge our deeper needs and wants.
By ridding ourselves of the need to be seen as syrupy sweet (and utterly drained) and by embracing self-care that may look harsh or selfish to others, we can empower ourselves to have better boundaries. This can also help our patients as we model balanced caregiving, without self-sacrifice. By embracing and honoring these important traits of self-care, self-protection, and acknowledging our needs, we set the stage for less burnout and more healthy relationships in life. So, next time you are overwhelmed by the number of obligations you have or the time you are bleeding energy for others, ask yourself “What would my selfish bi#ch do?” And, if you manage to hear and honor her, high-five yourself as you strut to better self-care and integrated self-love.
Enter the course I co-wrote and teach with Jenna Ross - Boundaries, Self-Care, and Meditation Part 2. This course was born out of our own personal and professional struggles and our journey to having a life and a practice that we love and can sustain. This class provides a safe space to facilitate deep, personal, and professional transformation through evidence-based information and practices. Join us in Boundaries, Self-Care, and Meditation Part 2 on November 23 to learn new strategies to address both oneself and one's patients with a mind, body, and spirit approach.
AUTHOR BIO
Nari Clemons, PT, PRPC

Nari Clemons, PT, PRPC (she/her) has been teaching with the institute since 2004. She has written the following courses: Lumbar Nerve Manual Assessment /Treatment, as well as Sacral Nerve Manual Assessment/Treatment. She has co-authored the PF Series Capstone course with Allison Ariail and Jen Vande Vegte, and the Boundaries, Self Care, and Meditation Course (the burnout course) with Jen Vandevegte. In addition to teaching the classes she has authored, Nari also teaches all the other classes in the PF series: PF1, PF2A, PF2B, and Capstone. She was one of the question authors for the PRPC, and she has presented at many conferences, including CSM.
Nari’s passions include teaching students how to use their hands more receptively and precisely for advanced manual therapy skills while keeping it simple enough to feel successful. She also is an advocate for therapists learning how to feel well and thrive as they care for others, which is a skill that can be developed. “Basically, I love helping therapists learn to help themselves and others more while having a lot of fun doing it”. Nari lives in Portland Oregon, where she runs a local study/mentoring group and has a private practice, Portland Pelvic Therapy. Her interests include meditation, working out, nature, and being constantly humbled from raising her three amazing teenagers!
Nari Clemons - Actually, I used to have a meditation and neuroscience class for Herman Wallace. It was a shorter class. But, I felt it was lacking in tools for the provider. For example, as an empathic provider, I felt I was very aware, very mindful that I was losing energy, that I was "picking things up" from my patients, and that I was really not enjoying my job or life balance as much as I used to. I became ill and burnt out, working in this intensive field. It felt like the joy of my life was kind of being sucked up by my job. Jen and I launched our own journeys, together, trying to understand how this world of boundaries and balance could help us in our own lives. So much changed and grew from that. So, in time we decided to combine the two into one class, to help practitioners integrate meditation into their practice and life, but also how to come back to loving their jobs with balance, as we were able to.
What are the top 3 takeaways a practitioner could hope to gain from this class?
NC - 1. Better self-care in and out of the clinic. 2. A more effective and less taxing way to interact with clients, share responsibility, and communicate in more helpful ways for both practitioner and patient. 3. enjoying their life and having more energy for their life outside of work.
JVV - 1. You don’t have to do it all. 2. We want to support you with tools to help your patients take more responsibility for their care and their outcomes. 3. YOU ARE VALUABLE…and here are ways you can care for yourself, have healthy boundaries, and align your actions with your priorities so you can leave work at work and truly enjoy your life outside of work.
Who do you think needs to take this class?
NC - Any practitioner who is finding work more and more emotionally taxing or draining. Really, there are a few patterns that benefit from this class. People who over-give and over-function in relationships in their life, including patient relationships. Often there can be a bit of a people-pleasing tendency in these situations. Also and especially if a participant is one of those people who have always been a little sensitive to energy: feel things, pick up things, notice their energy changes when they interact with others. I feel like this is the only class I know of that specifically gives tools and strategies for this kind of provider.
JVV - EVERYONE! LOL. People who are wrestling with healthy work/life balance, who find themselves staying late after work or working through lunch, health care providers who tend to care more for their patients than they do for themselves, those of us who leave work drained and only have meager offerings of energy for our families.
What was your favorite feedback from participants in taking this class?
NC - We hear a lot from participants that other classes made them have better clinical skills, but this class has helped them to enjoy their own life and their job more and to feel more balanced and professional as they employ better boundaries and shared responsibility.
JVV - Ahhh, it is true joy when participants are empowered and equipped to set healthy boundaries, care for themselves, and feel more joy in their lives.
How is this class different from other classes through H&W?
NC - Kind of along the same lines, this class does give you skills for use with patients, but they are the skills that help your life feel better, and your job feels better. They give you permission to change your paradigm of treatment from "how much can I possibly give" to "how do I shift my job, self, and communication, to allow my job to be just one part of my life that is enjoyable and doesn't take so much energy away from the other parts of my life."
JVV - This is the only class that focuses both on skills to use for patients and skills to use FOR YOURSELF. To keep yourself healthy, balanced, and whole as a medical provider in a demanding, challenging role.
Why are there two parts to this class?
NC - Because it is a lot of information, a lot of life changes to integrate. It takes time. We like the idea of a month of growth and change. Participants do pre-work to prepare for the first weekend, which starts the process of change. Then, they do work in the following month and really work on the intensive integration, new habits, new patterns, and new neuronal networks. Then, we come back for another day for the second part of learning that participants will be ready for after integrating some of the basics of the first weekend.
JVV - We just had SO MUCH we wanted to share!! And we found having two classes spaced a month or so apart really lets participants ingest and apply one level of change before being ready and hungry for the next level. The first part focuses on establishing good boundaries with patients, self-care practices including meditation, and identifying areas of their lives that need support or intervention to be healthier. The second class dives deeper into thoughts, emotions, and actions. Practices like gratitude, visualization, and deeper mediation practices.
Boundaries, Self-Care, and Meditation - Part 1
Course Dates: March 18
Price: $400
Experience Level: Intermediate
Contact Hours: 12.5
Description: The instructors recommend completing this series in two parts to allow time to process and implement one leg of the journey before undertaking the next. Both Part One and Part Two have a significant amount of pre-work to digest and practice before meeting via Zoom. Please plan for up to 12 hours of pre-course work. This sets the stage for you to find your path to experiencing more joy, energy and balance.
In Part One, participants begin their process of study, meditation, and self-reflection in the weeks prior to the start of the class. Pre-work includes focus on the neuroscience of pain trauma, PTSD, and meditation. Participants will learn about the powerful influence both negative and positive experiences have on our nervous system’s structure and function. Personal meditation practice and instruction will create changes in the participant's own nervous system. Participants will also learn how to prescribe meditation for various patient personalities and needs, as well as analyze yourself through inventories on coping, self-care, empathy, burnout, values, as well as track how you spend your time. Commitment to pre-work will facilitate rich discussion as we put what you have learned into practice around building a shared responsibility model of patient care, language to support difficult patients, and both visualizing and planning steps to create new, healthier patterns in your life and in your practice.

Amanda Davis, PT, DPT, PRPC can be found online at https://www.makeandmanifest.com/. She has generously shared her recent blog with The Pelvic Rehab Report. "Got 30 Minutes? 4 Underestimated Daily Practices to Make Your Lunch Break More Life-Giving" can be found in its original post on her website here: http://www.makeandmanifest.com/blog-lunchbreak/.
Hey there, I'm Amanda. Pelvic rehab therapist, endo warrior, girl mama (despite that whole endo thing), and creator of this space where I'm sharing the story of practicing what I preach and the wins and losses I gather along the way. I love early morning espresso, podcast binging, yoga pants, and scrolling Pinterest for my next obsession (heyyyy fellow libras!). My mission is to help women see the difference between "common" and "normal" and to take their physical, mental, and emotional health beyond the "that's just the way it is" mentality.
Hats off to my fellow 9-5ers who head home after a long day to jump right into their 5-9. If you’re like me, that second “career” includes (but definitely is not limited to) caregiver, dog walker, master gardener, professional organizer, chef, and housekeeper to name a few. Add in friendships that need energy, relationships that need time, those hobbies you swore you’d keep alive, and self-care you promised yourself you’d do…aaaaand the whole multi-passionate, multi-talented, multi-hyphenate thing can get overwhelming quick.
After a glorious five-month maternity leave, I’ve officially been a working mom for a year. I love my job and I love my girl, and while trying to fit both in a 24 day is challenging and exhausting, it’s what’s right for me in the season I’m in. Plus there’s something about pursuing my calling outside of the home and knowing Sloan’s watching me do it.
RELATED POST: 9 Ways to Practice Self-Love as a New Mom on Maternity Leave
We’ve all chased that ultimate goal of a *perfect* balance and ~seamless~ blend between work and home, but in full disclosure, I’ve gotta tell ya— it’s hard for me to do. I’ve found myself coming home drained, dying for a break, wishing I could just lock myself in a quiet room, and feeling guilty for all of the above. Being with my daughter is the best part of my day, but I’m often just too depleted to enjoy it.
Maybe you can relate? Maybe you’re also trying to work to live but find those words flipping themselves around more than you care to admit.
I recently took an online course called Boundaries, Self-Care, and Meditation for the Pelvic Rehab Therapist, Part 1 (part 2 is on June 12). As a PT I’m required to take continuing education to keep my skillset relevant and knowledge fresh, but the pending burnout I shared with you above led me to [this] course instead. To put it simply, it was [insert explosion sound here] mind-blowing; and call me dramatic, but I consider my practice, my patients, and myself as a person and professional forever changed because of it.
While I could write at least ten posts on all the things I learned in this class, the concept that’s been most life-altering for me was how I spend my lunchtime. Yep!…just a few tweaks to those 30 minutes mid-day and not only are my afternoons more pleasant and productive, but I’m going home refreshed, renewed, and ready to spend my time and energy on alllllllllll the other people and things that mean the most to me.
RELATED POST: Your Day Starts at Bedtime: 25 Easy Habits for a Better Night’s Sleep
What you’ll find next is how I structure my lunchtime for life-giving success— a strategy that serves me most. We all have different work environments, different physical and mental needs, and different priorities. As long as your cup feels full(er) at the end of your break, I can confirm you’re doin’ it right.
SHUT YOUR DOOR
I fully realize that not everyone has an office door they can shut during lunchtime, but as long as you can get somewhere semi-quiet and remotely alone, that should do the trick (heck…I’ve been known to go out to my car in a pinch). Creating a calm and centered environment has proven paramount to taking a true “break” from the day and will make all of my recommendations to follow that much more enjoyable.
If you’re worried about appearing “selfish” or “standoffish”…I was too. But after a week’s worth of lunches behind a closed door, I realize the positives of this practice far outweigh the negatives I was creating in my head. I’m still a team player. My coworkers still know where I am if they need me. But I’m a better colleague the other eight hours of the day when I take these 30 minutes to myself, and to my knowledge, there have been no complaints so far.
STOP TO EAT
To my fellow multi-tasking queens— if you only read one part of this post, let [this] be it as I believe this one change has made the biggest difference.
I used to spend my lunch catching up on paperwork, tending to emails, paying bills, online shopping, and then resort to scrolling social media if all of that was done. But I was eating during all of it and realized that not only was it taking me twice as long to complete tasks, but I wasn’t tasting, appreciating, or ultimately enjoying my food, all huge components of appetite, digestion, and ultimately nutrition and health.
My lunches aren’t anything fancy; in fact, 99% of the time they’re leftovers from earlier in the week (helloooooooo my trusty 3-day-old grilled chicken). But stopping to eat with intention and nothing other than a little music or podcast playing in the background has surprisingly, but positively, affected how much I consume, how my gut feels afterward, and the amount of energy I have for the rest of the day.
PS- What you eat can make a huge impact here too. I aim for whole, quality foods full of healthy fats and filling proteins to set me up for success. I’m someone who can eat the same thing again and again, so you’ll typically find my lunchbox full of that good ol’ grilled chicken, boiled eggs, fruit, cheese, and rice noodles if I’m feelin’ feisty.
LEARN
On top of that podcast I have playing while I eat, I’ve started spending ten to fifteen minutes learning during lunch. I literally set a timer, pull out a book, and read about something that fuels my brain.
In order to make these minutes a 10/10, here’s a few tips to uplevel the experience:
- Get comfortable. Find a place to prop your feet up or lean that car seat back (this is in part why I set a timer…juuuuuuuust in case I fall asleep). Have water nearby, a blanket tucked away if it’s cold, and don’t hesitate to indulge in all the ways even if for just a short period of time.
- Read about something unrelated to your occupation. For instance…I’m a pelvic rehab therapist but you won’t see me catching up on the latest research in anatomy and physiology. I typically grab a book on self-improvement, business and marketing, or homesteading, and my brain feels so much more recharged when it gets to focus on something that builds me up as a passionate person outside of my profession.
- Use a physical book. Seriously…no kindle, no phone apps, no audiobooks. Chances are you’re looking at a screen, listening to people talk, or a combo of the two all day long. Digging into an actual hard copy will access other parts of your brain that you may not be tapping into as regularly and result in faaaaaaaar more feel-good-ness.
When I became a mom I went from devouring a few books a month to being able to count my yearly reads on one hand. Reading on my lunch break has made me excited to learn again and reminded me of who I am outside of motherhood too (in turn making me a better mama). Even if reading isn’t your “thing”, at least give this one a try. Bonus if you utilize your local library because their books just smell better and we’re going for indulgent here…remember?
MOVE
Eat…ten minutes. Learn…ten minutes. If you’re like me and have ten more minutes to spare, then I encourage you to move your body with that time. While the options are endless, I try to avoid sweating too much in the middle of the work day, so walking, stretching, and even deep breathing exercises are more my speed. Whatever you decide to do, make sure you have the shoes, yoga mat, or whatever it is you need ready to go.
RELATED POST: Easy + Impactful Ways to Use Your Time Confetti to Improve Your Pelvic Floor Health
Not only does research show that movement improves your mood and elevates your energy, but there are also the physical benefits (duh!) and mental resilience that comes with knowing you’re taking care of yourself when you could be doing something else. Once fearful of wasting precious energy, I now consider my mid-day movement the boost I need to ensure I’m ready to go when I get home because let me tell ya…one year olds don’t quit.
One look at my Pinterest boards and you’ll see I’m a girl who has a lot she wants to accomplish (I see you dream house, list of must-reads, vacation itineraries, and yummy recipes just dyyyyyying to be made). But with a 24-hour day divided in thirds between work, sleep, and “other”, I have to use my time wisely to see success in a life where I’m more often than not choosing the option of (D) ALL OF THE ABOVE.
I don’t mean to be dramatic, but hacking my 30-minute lunch has ~literally~ changed my life and I’m a better physical therapist, caregiver, dog walker, master gardener, professional organizer, chef, and housekeeper (to name a few) because of it. There’s a saying that if you can’t go big, go home, but this is an instance where you can’t underestimate the power of a few minutes spent intentionally where it counts.
I’d love to hear in the comments what you do for work, if these strategies work for you, and ways you’ve made them your own. And don’t hesitate to share this one with a coworker who could use these strategies too! Nothing makes me happier than picturing us all spending half an hour in that 11-2 time frame-filling our cups for full-day success. I have a feeling you’ll be surprised at the impact this can have, and I can’t wait to watch you grow one lunchtime at a time.
Boundaries, Self-Care, and Meditation - Part 2 - Remote Course - June 12, 2022
This course focuses on personal and professional growth for the participant, with a deeper dive into meditation and self-care practices. Yoga is introduced as a means of mindful movement and energy balance. Participants will learn to identify unhealthy relational patterns in patients and others, and skills on how to use language and boundaries to create shifts that keep the clinician grounded and prevent excessive energic and emotional disruptions. There is a lecture on using essential oils for self-care and possibly patient care. Learning new strategies to preserve energy, wellness, and passion while practicing appropriate self-care and boundaries will lead to helpful relationships with complex patients. This course also includes a discussion of energetic relationships with others as well as the concept of a "Higher Power". The discussion will also include refining life purpose, mission, and joy potential, unique to the individual participant. The goal is that the participating clinician will walk away from this experience equipped with strategies to address both oneself and one's patients with a mind, body, and spirit approach.
This week Jennafer Vande Vegte and Nari Clemons sat down to share their course Boundaries, Self-Care, and Meditation with us to give a peek into the why, what, and how of it all.
What are boundaries? Boundaries are when we need to set a limit. It’s that capacity to say here’s where I need to draw the line so that I stay grounded and centered and feel good about myself. Self-care is what we do to replenish those energy reserves every day. To replenish our joy. To replenish our sense of awe and gratitude. Then meditation is a beautiful way to rewire the brain. To get to the reasons and roots of why we are getting depleted, we need to have a high level of honesty and introspection.
This is a course that gives you that permission and a lot of tangible tools. Nari shares that students have told her that "all of the other courses give us manual skills, but this course changed my life." Jen adds to this, "BUT you got to put in the work. This course is science and research-based and used in a way to transform lives." Part one is a deep dive into the science of the brain. Pain, trauma, PTSD and how that changes the brain, and how that has changed the brains of patients and of us. Meditation practices are explained from a scientific perspective about how they can come in and rewire the nervous system and help your patterns.
Part two is about a month later and gets a little bit softer. In this portion, Nari and Jenn focus on relationships, not just with our patients but with ourselves and the people that we love in our lives. How to construct healthy relationships and build that patient shared responsibility model in our practices. They also dive into the visualization of what we want in our practices and lives, self-care, and meditation. The course comes to a close with case studies and an action plan to bring what you’ve learned into the clinic. They’ve also established an online network where you can sign up for continued community. We’re all going through this journey together.
Boundaries, Self-Care, and Meditation Part 1 is scheduled for April 24th.
Boundaries, Self-Care, and Meditation Part 2 is scheduled for June 12th.

Part 1: Burnout
Let’s get real for a minute.
You are a highly educated professional. If you are reading this blog, I can assume you are invested in your career and your continued education. You are probably pretty skillful, and you help a lot of people.
BUT
How are you doing once you leave work?
Does your life outside of work give you joy and fulfillment?
Or do you leave your work setting completely drained, snippy with your loved ones, and too tired to care for yourself?
You have at least one advanced degree, probably some certifications, but did anyone ever teach you how to get your paperwork done on time?
Or how to leave work at work and not have your patients popping into your head day and night?
What about energy conservation? In fact, we may have been taught to give our ALL to work, to our patients, to strive for productivity and accomplishment. But where does that leave us?
BURNED OUT.
Part 2: Mindset
Taking continuing education classes was my pathway to becoming a better physical therapist.
But I had to go to therapy to learn how to survive as a physical therapist.
There were struggles.
Paperwork. I could NEVER finish in a timely way.
Timeliness. I was OFTEN running behind for patients.
Discharge. I had some patients for YEARS because I did not know how to discharge them even though they weren’t getting better. They depended on me, and I also depended on them.
Boundaries. I had none.
And here’s something that surprised me.
I had to change the way I THOUGHT before I could change my BEHAVIOURS.
I had to change my mindset.
I used to show up at work with the idea of Helping People. I felt responsible for their outcomes. If they weren’t doing well, I assumed I was missing something.
The shift looked like this:
I can show up at work to coach people who are responsible for their own outcomes. If they aren’t doing well, we can have honest communication about next steps (medical or otherwise), discharge, or resistance.
My patients are not my family, they are not my friends. I show up as a coach who is very interested in understanding their story and helping them reach their goals through a shared responsibility model of care.
My free time is sacred. I need to protect it for my mental, physical, spiritual, and emotional health. Because I am a priority, I will use 5 minutes of each treatment session to complete the patient’s treatment by doing paperwork.
Now, therapy is INVALUABLE. Don’t get me wrong, but paperwork, timeliness, discharge, and healthy boundaries are things MANY of us struggle with. So Nari Clemons and I designed a Continuing Education COURSE. We believe that therapists deserve to learn skills to preserve our wellbeing and strengthen our resilience against burnout.
Especially since the pandemic, more and more health care workers are reporting very high levels of burnout. Nari Clemons and I went through a period of burnout earlier in our careers. The tools and techniques we learned to heal ourselves and develop new patterns of delivering care are powerful. We know you might also be struggling and we want to help. So we developed a course to equip you. We would love to learn with you at Boundaries, Self-Care, and Meditation. A two-part, online journey toward experiencing a practice you enjoy and a life you love.
Boundaries, Self-Care, and Meditation is a two-part series intended to be completed in order. Participants should register for Part 1 and Part 2 at the same time, or complete Part 1 and wait to complete Part 2 at a later date. This course was developed by Nari Clemons, PT, PRPC, and Jennafer Vande Vegte, PT, PRPC and was "born out of our own personal and professional struggles and our journey to having a life and a practice that we love and can sustain." The intention of this class is deep, personal, and professional transformation through evidence-based information and practices. Both Part One and Part Two have a significant amount of pre-work to digest and practice before meeting via Zoom. Nari shares that "This sets the stage for you to find your path to experiencing more joy, energy, and balance."
Boundaries, Self-Care, and Meditation - Part 1 - Remote Course
In Part One, participants begin their process of study, meditation, and self-reflection in the weeks prior to the start of the class. Pre-work includes focusing on the neuroscience of pain, trauma, PTSD, and meditation. Participants will learn about the powerful influence both negative and positive experiences have on our nervous system’s structure and function. Personal meditation practice and instruction will create changes in the participant's own nervous system. Participants will also learn how to prescribe meditation for various patient personalities and needs, as well as analyze yourself through inventories on coping, self-care, empathy, burnout, values as well as track how you spend your time. Commitment to pre-work will facilitate rich discussion as we put what you have learned into practice around building a shared responsibility model of patient care, language to support difficult patients, and both visualizing and planning steps to create new, healthier patterns in your life and in your practice.
Boundaries, Self-Care, and Meditation - Part 2 - Remote Course
Part Two continues the focus on personal and professional growth for the participant, with a deeper dive into meditation and self-care practices. Yoga is introduced as a means of mindful movement and energy balance. Participants will learn to identify unhealthy relational patterns in patients and others, and skills on how to use language and boundaries to create shifts that keep the clinician grounded and prevent excessive energic and emotional disruptions. There is a lecture on using essential oils for self-care and possibly patient care. Learning new strategies to preserve energy, wellness, and passion while practicing appropriate self-care and boundaries will lead to helpful relationships with complex patients. This course also includes a discussion of energetic relationships with others as well as the concept of a "Higher Power". Course discussion will also include refining life purpose, mission, and joy potential, unique to the individual participant. The goal is that the participating clinician will walk away from this experience equipped with strategies to address both oneself and one's patients with a mind, body, and spirit approach.

Rachna Mehta, PT, DPT, CIMT, OCS, PRPC is the author and instructor of the new Acupressure for Pelvic Health course. Rachna brings a wealth of experience to her physical therapy practice and has a personal interest in various eastern holistic healing traditions. Her course Acupressure for Optimal Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional, and energy body.
Constipation is a common functional gastrointestinal disorder, with prevalence in the general population of approximately 20%. In the elderly population, the incidence of constipation is higher compared to the younger population, with elderly females suffering more often from severe constipation (1).
Is there a magic button in the perineum that makes it easier to defecate? In case you have wondered, the answer is YES!!!
A study done recently by Dr. Ryan Abbott and colleagues at UCLA’s Department of Medicine found just that. A randomized control trial was conducted with 100 subjects who had functional constipation, half randomized to treatment and half to the control group. The treatment group received training in self perineal acupressure along with standard treatment options. The control group only received information about standard constipation treatment options.
Perineal self-acupressure technique was found to be remarkably effective with statistically significant and clinically meaningful improvements in Patient Assessments of Constipation Quality of Life (PAC-QOL All), modified Bowel Function Index (BFI), and the Short-Form Health Survey (SF-12v2). Patients in the treatment group also reported substantial satisfaction with perineal self-acupressure technique:
- 72% of the treatment group reported that the perineal pressure technique helped them to “break up, soften, or pass stools."
- 54% reported that the technique helped them to “avoid having hemorrhoid or lessened the impact of existing hemorrhoid."
- 72% reported that the technique helped them to “avoid or better manage the effects of constipation."
- 82% of the treatment group patients indicated that they would continue to use the technique, and 72% indicated that they would recommend the technique to family and friends (2).
In this study, perineal acupressure was applied at the Acupressure point Huiyin or CV 1 located at the perineum. Huiyin is used in Traditional Chinese Medicine (TCM) not only to treat constipation, but also a variety of conditions including impotence, hemorrhoids, rectal prolapse, and dysmenorrhea. In addition, there are several key Acu-points like St 36 on the Stomach meridian and CV 6 which can help with constipation and digestive disorders.
Acupressure is based on Traditional Chinese meridian theory in which acupuncture points are pressed to stimulate the flow of energy or Qi and these points reflect disorders of visceral conditions and organs.
Acupuncture meridians are believed to form a network throughout the body, connecting peripheral tissues to each other and to the central viscera. This tissue network is also continuous with more specialized connective tissues such as periosteum, perimysium, perineurium, pleura, peritoneum, and meninges (3).
Dr. Abbott’s study suggests that clinicians should consider incorporating perineal self-acupressure technique as a first-line treatment for constipation, along with conventional interventions such as increased exercise and dietary fiber intake. Benefits include being non-invasive and non-pharmacological treatment intervention for constipation with likely a lower risk for side effects and complications than commonly used medications such as stool softeners, fiber supplements, stimulants, laxatives, and lubricants (2).
As medical providers, we are uniquely trained to combine our orthopedic skills with mindfulness-based holistic interventions to empower our patients by giving them the tools and self-care regimens to live healthier pain-free lives.
The upcoming remote course Acupressure for Optimal Pelvic Health, scheduled for July 24-25, 2021, brings a unique evidence-based approach on the use of potent Acupressure points for treating a wide variety of pelvic health conditions including chronic pelvic pain, dysmenorrhea, constipation, digestive disturbances and urinary dysfunctions to name a few.
The course also offers an introduction to Yin yoga and explores Yin poses within each meridian to channelize energy through neurodynamic pathways with powerful integrative applications across multiple systems.
References
- Vazquez Roque M, Bouras EP. Epidemiology and management of chronic constipation in elderly patients. Clin Interv Aging. 2015;10:919-930.
- Abbott R, Ayres I, Hui E, Hui KK. Effect of perineal self-acupressure on constipation: a randomized controlled trial. J Gen Intern Med. 2015;30(4):434-439.
- Kaptchuk TJ. 2000. The web that has no weaver. Understanding Chinese medicine. Chicago: Contemporary Publishing Group, Inc.
5. Lee EJ, Frazier SK. The efficacy of acupressure for symptom management: a systematic review. J Pain Symptom Manage. 2011;42(4):589-603.
It’s OK to be feeling (insert feeling) right now. (maybe: sad, fearful, angry, denial, numb, anxious, avoidant, bored?)
 It’s OK to acknowledge those feelings.
It’s OK to acknowledge those feelings.
It’s also OK to create a plan and direction about what we may do about our feelings, thoughts, and actions.
We can change how we think, what we do and ultimately how we feel.
Breathe. Place a hand on your chest and a hand on your abdomen. Practice inhaling long and deep as if you were pouring the air into your body- first filling the lower hand and then filling the top hand. Pause for a moment when you feel your canister is full and then exhale slowly (top to bottom or bottom to top- either works fine). I prefer breathing through my nose for inhale and exhale but know if you are congested, mouth breathing is fine or you can inhale through the nose and exhale through the mouth- find what works for you. Work on increasing the number counted (silently in your mind) while you inhale, pause briefly and then exhale- making that number count on exhale the same or even longer. Make it a game to see how long and deep your breath can become. Reduce intensity if feeling lightheaded.
Focus on your breath and feel calmness. Return to this breathing whenever you can.
Body Scan/Progressive Relaxation. Take a moment and scan your body for pain or tension. You can start at the top of your body or where your feet are grounded to floor. Notice your body and allow it to be, without judgement. Then starting from the top of your body or the bottom, contract your muscles systematically and then relax. Or focus on the muscle group and allow the muscles to relax and slacken. Maybe send your long, deep breath to each area? Maybe think of color washing each area? Make your scan personal and positive for you. Check-in to your body without judgement and send gratefulness for the work your amazing body does.
Stand Big. Find a wall and place your backside onto it. Pretend there is a string at the crown of your head and imagine your head being pulled up towards the ceiling. Lift your chest as you are standing tall and use your slow, steady, deep breathing to create bigness and calmness. Relax your shoulders. Maybe place the back of your hands onto wall and feel the opening of your chest. Once you have practiced this posture, you can refer to this posture during your day. Stand big, breathe big, be big.
Intentionally SCHEDULE into your life what you love. Schedule time listening to your favorite music. Maybe take up playing an instrument? Practice singing in the shower or car. Set a timer and dance fervently. Create time to draw or paint or write. Make a recipe. Get frozen berries and make smoothies. Maybe add frozen spinach to your smoothie?
Pick up a book. Play a game, cards or even solitaire. Practice Sudoku. Take a bath or shower. Go for a long walk while keeping your distance from others. Find a workout you can do at home that makes you feel powerful. Whatever you love, turn it into a scheduled ritual. Make one small goal and work towards it. Focus on what we can do instead of what we cannot. Find some activity and fulfill a passion just for you. Make sleep a priority and know if you have a bad night, that the next night you will likely sleep better. Perhaps create a sleeping ritual? Call others and ask what they are doing for themselves? Remember to forgive yourself and to feel or express the feelings that are within you. We are all going through this together. Make you a priority and schedule yourself some HAPPY.
Lastly- try to limit the news, your phone and the frig. All of these can create negative feelings that do not fulfill us.
Breathe. Find love in positive activities. Be brave. Be grateful. Forgive.
We are all in this together.
Lauren Mansell DPT, CLT, PRPC is the author and instructor of the Trauma Awareness for the Pelvic Therapist course. She is also offering several courses via Zoom video conference during the Covid-19 pandemic, which can be found on our Remote Learning Opportunities page. Prior to becoming a physical therapist, Lauren counseled suicidal and homicidal SES at-risk youth who had survived sexual violence. Lauren was certified as a medical and legal advocate for sexual assault survivors in 1999 and has advocated for over 130 sexual assault survivors of all ages in the ED. Lauren's physical therapy specialty certifications include Certified Lymphedema Therapist (CLT), Pelvic Rehabilitation Professional Certificate (PRPC) and Certified Yoga Therapist (CYT). She is a board member of Chicagoland Pelvic Floor Research Consortium, American Physical Therapy Association Section of Women's Health and Section of Oncology.
A Weekend of Transformation
Let me start this plog (picture/blog?) by saying it had been almost 2 years since Nari Clemons and I taught Boundaries, Self Care, and Meditation for the first time. Nari had some amazing ideas to change some of the course material to reflect more of our hearts’ intention for personal reflection and transformative change. We were excited and nervous to see how our second run of this material would be received. We were also profoundly aware of how the (at times painful) events in our lives that led up to the development of the course have molded and shaped us into much healthier versions of ourselves. We wanted to share a bit about what we have learned and how it has changed us.
We met up in beautiful San Diego on Thursday. Because this course was Saturday to Mononday we had an added bonus of extra time to spend together. We decided to spend our time practicing what we talk about in class.
1. Get out in nature:
Tory Pines State Park provided much needed rejuvination. Ahh sea air.
2. Self-care is mandatory:
We spent Friday relaxing at a beautiful resort in Del Mar. We are learning we don’t need to justify or feel bad about caring for ourselves. It’s necessary and important. We are responsible for meeting our own needs and for refueling ourselves when we provide care for others.
3. Get out of your comfort zone:
The robes we got from the resort were super cozy and it was chilly on the beach, so why not walk the beach in a robe? We laughed at ourselves and others laughed at us and with us. But we were comfy and warm.
4. Do the work when it is time to do the work:
Instead of thinking and talking about the course all day we committed ourselves to being in the moment. When it came time to discuss the details of the next three days, a plan came together with relative ease. This is us working at the resort.
5. Challenges can change your perspective. And a change in perspective can help you with challenges:
This is a (terrible, sorry) picture of us interrupting our morning run to climb a tree. It was a fun challenge and gave us an interesting perspective on our day.
A little more about the course. Woah. The people who showed up came with open minds and hearts, ready and ripe for change. We had powerful times of sharing, listening, learning, and supporting. Meditation and yoga and a healing, honest and real atmosphere brought about transformation in the most beautiful awe-inspiring way. We were profoundly moved. The changes Nari suggested were PERFECT and I was grateful for her innovations. We were all pretty much out of our comfort zones, but that is where change happens.
In the words of one student, “This course couldn’t have come at a more appropriate time because I was in major burnout. I was becoming an unhappy person both professionally and personally. I needed to make a change. Now I am leaving this course empowered to care for myself so I can help patients in a healthy way and enjoy my job again. I am walking away from this course with so many valuable strategies and also feel so much more relaxed and hopeful”
6. Be silly sometimes:
Laugh a lot. Especially at work. Play jokes, have fun. You know what they say about all work and no play. Play.
7. At the end of the day Shake it off (and use pain science as needed):
Our last day we took a run to the beach. When crossing a rail line I tripped and bashed the HECK out of my lower leg. Since I could still run I repeated the mantra “Hurt not harm!!” (which we discuss in class) with great vigor until the throbbing subsided, and we enjoyed a beautiful sunset and the conclusion of our time in San Diego.
Last words of Wisdom:
Gratitude can change us in powerful ways.
A huge and heart felt thank you to Herman & Wallace, our host site, and for each and every participant. We couldn’t do what we do without you and for this we are eternally grateful.
Thank you. Thank you. Thank you.

Part 3: Carefully Choosing to Say Yes or No (or The Summer that Almost Wasn’t)
*Disclaimer: this essay is meant to be read in a voice of complete transparency and humility.
 Two summers ago I was anxiously anticipating a break. I was wrapping up home school for my girls and had scheduled some down time from writing my contribution to “Boundaries, Meditation and Self-Care” when I got the call…
Two summers ago I was anxiously anticipating a break. I was wrapping up home school for my girls and had scheduled some down time from writing my contribution to “Boundaries, Meditation and Self-Care” when I got the call…
Rewind a bit. Two years prior I also got a call. Would I be interested in writing a chapter in a Urology textbook on alternative care for pelvic pain conditions…edited by and partnering with a big name in pelvic floor rehab? Oh yes indeed I would! I have always dreamed of seeing my name in print. Was I scared out of my mind? Heck yes! I was working 20 hours a week, part time home schooling my girls and teaching for Herman & Wallace. I had one day a week to myself for cleaning, errands, the occasional book reading or interacting with friends. I decided I could spend my next year of Fridays researching, writing and editing said chapter. Oh, I also started therapy for the anxiety increase that came with the project. My therapist suggested I hire help with house cleaning, which I did. She also suggested meditation, mindfulness and using essential oils. I opted not to enact these suggestions. It was a crazy year, but I learned a ton and was proud of my contribution to the publication.
In the brief time that I caught my breath from the book chapter, I was invited to be part of the team writing the Pelvic Floor Capstone course. What an honor! I had always wanted to try writing a course and this would be a perfect opportunity to collaborate with others on such a big project. I committed, worsening my anxiety with heart palpitations which escalated to a level that required medication. My Fridays and evenings were again occupied for quite some time. Luckily, I still had the cleaning help and the therapist which were really just the skinniest strings that were maintaining my sanity.
While teaching our first Capstone class, although both of us were struggling with burnout, Nari Clemons and I had a moment of euphoria, seeing everything come together and watching students learn. We decided we would design and write another course and put together an outline and a plan for Boundaries, Self-Care and Meditation.
I think you might be getting a picture of my prior lifestyle. If there was time, I filled it. If there was an opportunity, I took it. If I did something once, I could do it again. But applying the concepts of our boundaries course to myself changed everything.
Nari and I knew we were burning out and needed change. I have always had anxiety, but it had escalated to the point of requiring both therapy and medication. I was giving my all, my best, to everyone else and my family got my scrappy leftovers, the worse of me. I had been functioning in these patterns my whole life and had no idea how to get off the hamster wheel.
As we developed Boundaries, Meditation and Self Care I became my own research study, incorporating the material we would be teaching into my own life. I finally started setting priorities and boundaries that helped put my family first and give them the best of me. I said no to a variety of opportunities that I then delegated to colleagues who were delighted to step up. I started meditating, practicing mindfulness and using essential oils as part of my self-care as my therapist suggested a year ago. I even enrolled my kids in full time school for the upcoming year. I was feeling so much better!
So when the next call came, I was prepared.
The editor and famous pelvic floor PT I had worked with on the book chapter was in need of an editor for an article that was going to be published in a medical journal. There was a lot of editing that needed to be done and time was of the essence. My contribution as editor would list me as a co-author. How many of you also dream of seeing your name attached to an article in a peer reviewed medical journal? Because of what I had learned through therapy and practiced with meditation I had the ability to pause, reflect, and make an informed choice that considered how this opportunity lined up with my priorities. I replied with much gratitude for the offer, but this time I said no. It was difficult to say no, and I had to work through some regret, but in the end I made the right choice and we had a great summer.
Life is funny sometimes and lessons in humility are plentiful. Back track again to when the urology text came out a few years ago. I excitedly ordered a print copy. When I opened to the chapter which I contributed, I discovered another person’s name had accidently been printed where mine should have been. The mistake was corrected for the ebooks but more paper copies were not printed. I may never see my name in print, but the Summer That Almost Wasn’t taught me that there are more important things in life.
If you find yourself struggling with boundaries, saying no, and prioritizing the things that are important to you personally and as a therapist, know that you are not alone, and you can get support. Consider talking with your supervisor, a counselor, reading a good book on the subject or taking Boundaries, Meditation and Self Care, a course offering through Herman and Wallace that was designed to help pelvic health professionals stay healthy and inspired while equipping therapists with new tools to share with their patients.
We hope you will join us for Boundaries, Meditation and Self Care this November 9-11, 2019 in San Diego, CA.
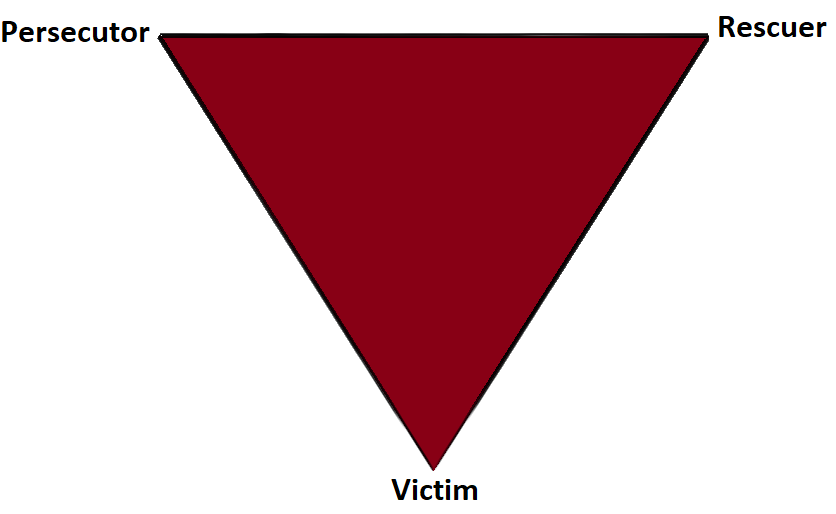
Part 2: The Drama Triangle
This is part two of a three-part series on self-care and preventing practitioner burnout from faculty member Jennafer Vande Vegte, MSPT, BCB-PMD, PRPC. Part One is available here. Jennafer is the co-author and co-instructor of the along with Nari Clemons, PT, PRPC.
Augh, I was so frustrated with myself. I fell for it again. Here’s the scenario: a patient came in suffering excruciating pain. She had been to see a pelvic health professional as well as various medical professionals and was unable to get relief and answers for her rectal pain. She was desperate and called me “her last hope.” Phrases used included, “I need you! Fix me! I hear you are a miracle worker! If you can’t help me no one can!” And just like that I took on the role of Rescuer.
In 1968 a psychiatrist named Stephen Karpman developed a model of personal interaction that he called the Conflict Triangle. It has also become known as the Karpman Triangle, The Drama triangle or the Victim triangle. Per Wikipedia:
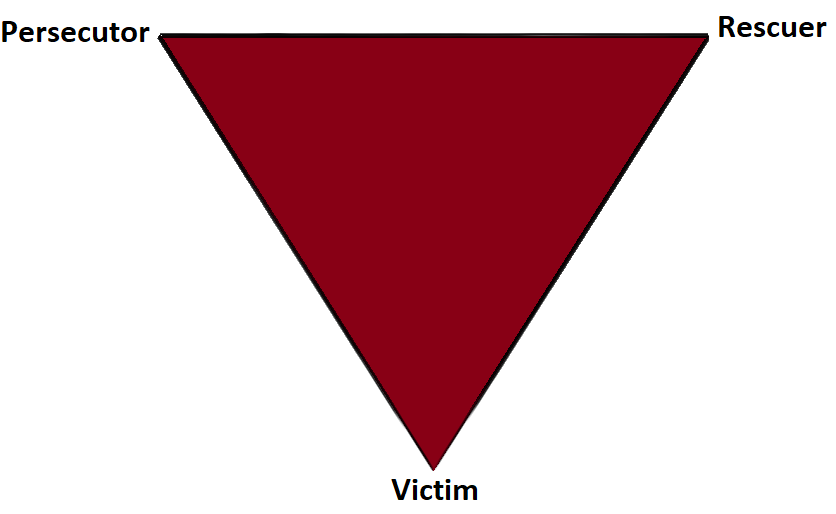
The Victim: The Victim's stance is "Poor me!" The Victim feels oppressed, helpless, hopeless, powerless and ashamed. They seem unable to make decisions, solve problems, take pleasure in life or achieve insight. The Victim, if not being persecuted, will seek out a Persecutor and also a Rescuer who may save the day, but may also perpetuate the Victim's negative feelings.
The Rescuer: The Rescuer's line is "Let me help you." A classic enabler, the Rescuer feels guilty if they don't rush to the rescue. Yet their rescuing has negative effects: It keeps the Victim dependent and gives the Victim permission to fail. The rewards derived from this rescue role are that the focus is taken off of the Rescuer. When they focus their energy on someone else, it enables them to ignore their own anxiety and issues. This rescue role is also pivotal because their actual primary interest is really an avoidance of their own problems disguised as concern for the victim’s needs.
The Persecutor: (a.k.a. Villain) The Persecutor insists, "It's your fault." The Persecutor is controlling, blaming, critical, oppressive, angry, authoritative, rigid, and superior.
 What is interesting about this triangle is that the roles are constantly shifting. In full rescuer mode, I gladly took on this patient, intent on solving her problems. Over time, I saw that my consistent coaching for lifestyle change and self-care was falling on deaf ears. My patient was not following through with anything I asked of her; therefore my treatment plan was not working. The patient began to get frustrated with me. I then cast myself as the victim. She became my persecutor! While perhaps in her mind, I had failed as the rescuer, she was still the victim and I had become her persecutor. At the time, I did not have the skills to know how to navigate this situation in a positive or helpful way. Finally I sought the advice of my supervisor and my therapist to draw up a contract with this patient. The contract outlined each of our responsibilities. If either of us didn’t fulfill our responsibilities, the consequence would be ending our professional relationship. When she persisted, unwilling to do her part, I discharged her per our agreement.
What is interesting about this triangle is that the roles are constantly shifting. In full rescuer mode, I gladly took on this patient, intent on solving her problems. Over time, I saw that my consistent coaching for lifestyle change and self-care was falling on deaf ears. My patient was not following through with anything I asked of her; therefore my treatment plan was not working. The patient began to get frustrated with me. I then cast myself as the victim. She became my persecutor! While perhaps in her mind, I had failed as the rescuer, she was still the victim and I had become her persecutor. At the time, I did not have the skills to know how to navigate this situation in a positive or helpful way. Finally I sought the advice of my supervisor and my therapist to draw up a contract with this patient. The contract outlined each of our responsibilities. If either of us didn’t fulfill our responsibilities, the consequence would be ending our professional relationship. When she persisted, unwilling to do her part, I discharged her per our agreement.
I learned so much from this experience. Here are some things that I have implemented and may be helpful in your practice if you have similar challenges.
- In an initial visit with a new patient I explain that the patient and I make a team and we each have a role to play in reaching the patient’s goals.
- If someone says, “Fix me!” I say, “Think of me as your coach, I can show you how to help your body heal, but it’s your job to do the work.”
- When I hear, “Everyone says you are a miracle worker.” I say, “That is so kind, but it doesn’t work that way. Healing is complicated and everyone has their own journey.”
- In this way, with baby steps, we can get OUT of the drama triangle and into healthy relationships with our patients and the people in our lives.
- Consider the Winner's Triangle published by Acey Choy in 1990.
In her blog NextMeCoaching, Jessica Vader coaches on turning Drama and Control into a Winning situation.
The three roles in the Winner’s Triangle.
Vulnerable – a victim should be encouraged to accept their vulnerability, problem solve, and be more self-aware.
Assertive – a persecutor should be encouraged to ask for what they want, be assertive, but not punishing.
Caring – a rescuer should be encouraged to show concern and be caring, but not over reach and problem solve for others.
If you struggle with professional and personal boundaries, you are not alone, and you can get support. Consider talking with your supervisor, a counselor, reading a good book on the subject, and or taking Boundaries, Mediation and Self Care, a course offering through Herman and Wallace that was designed to help pelvic health professionals stay healthy and inspired while equipping therapists with new tools to share with their patients.
We hope you will join us for Boundaries, Mediation and Self Care this November 9-11, 2019 in San Diego, CA.
Look forward to my next blog where saying no takes an unexpected turn.