In this brief blog, I hope to explore several lifestyle medicine strategies (sleep hygiene, stress management, social connectedness) and how they may be included in therapeutic interventions to improve clinical outcomes. Frates and colleagues define lifestyle medicine as "The use of evidence-based lifestyle therapeutic approaches, such as a predominately whole-food and plant-based diet, regular physical activity, adequate sleep, stress management, avoidance of risky substance use, and other non-drug modalities to treat, oftentimes reverse, and prevent the lifestyle-related, chronic disease that's all too prevalent."1 Figure 1, adapted from the American College of Lifestyle Medicine, outlines the six pillars of lifestyle medicine.

Figure 1. Components of lifestyle medicine
Sleep Hygiene in Patient Education
The following are some simple patient education strategies that may help patients improve sleep:2-5
- Establish a regular bedtime and waking hours (avoid or minimize "social jet lag" that may be due to work, school, or your personal schedule).
- Create a comfortable room that is cool, dark, and quiet.
- Sleep in a comfortable bed and make sure it's not too old.
- Use a supportive and comfortable pillow and ensure it's not too old.
- Eliminate nighttime caffeine and limit daytime caffeine.
- Do not wear tight or restrictive clothing during sleep
- Avoid alcohol within 3 hours of bedtime.
- Do not smoke or use nicotine.
- Eliminate/limit after-dinner and late-night snacking.
- Limit or avoid computer use and smartphone use near bedtime.
- Avoid intense exercise near bedtime. However, do exercise and be physically active during the day.
- Maintain a healthy body mass index (BMI).
- Avoid watching intense television shows before bedtime.
- Turn off the radio and television before going to sleep.
- Avoid bright light near bedtime, but do increase daytime exposure to sunlight.
- Consider reducing your fluid intake near bedtime to avoid (or minimize) getting up to go to the bathroom, but maintain adequate hydration during the day.
- Minimize sugar and salt intake near bedtime as it may cause increased trips to the bathroom.
- Learn strategies to reduce daily stress so it does not result in poor quality and quantity of sleep.
- Minimize a tense or stressful lifestyle since this may carry over into sleep.
- Embrace mindfulness before bedtime
- Consider meditating close to bedtime or using a body scan or progressive muscle relaxation technique.
- Consider tai chi, qigong, or yoga later in the day.
- Establish a bedtime ritual such as:
- One hour before going to sleep, shut down all phone and computer devices. Then you can either read a book or watch a funny television show (drama may be too stimulating).
- Five minutes before you go to sleep, brush your teeth and floss, wash your hands and face with lavender soap, and shut off all the lights before slipping into your cozy bed with gratitude and pleasant thoughts.
Stress Management Patient Education
The following are some simple patient education strategies that may help patients manage stress:6
- Try yoga, tai chi, qigong
- Use aromatherapy (such as lavender)
- Engage in outdoor physical activities such as walking, hiking, and biking
- Engage in outdoor activities such as gardening
- Participate in hobbies such as reading, pottery, painting, and playing music
- Play with pets
- Get a massage
- Get involved in social activities such as volunteering, coaching, and community dancing
- Listen to music
- Smile and laugh more by watching comedy movies or television shows
Social Connectedness Patient Education
The following are some simple patient education strategies that may help patients improve socialization and social connectedness to form nurturing and constructive relationships:7-13
- Attend local sporting events, music performances, or art and museum exhibits.
- Connect with family and friends locally or on Zoom.
- Connect with your physician, therapist, wellness, or fitness professional via telehealth-delivered services.
- Create or join a community garden club.
- Create or join a lunchtime walking, yoga, or tai chi club.
- Engage in conventional group exercises such as softball, volleyball, basketball, pickleball, paddle tennis, or tennis.
- Engage in mind-body exercises such as yoga, tai chi, or Pilates.
- Engage in work-related community activities and fitness programs.
- Engage in small conversations with cashiers and employees at various stores you visit.
- Engage with members at your community place of worship.
- Enroll in art-based community activities, such as art, dance, drama, music, poetry, pottery, or expressive writing classes.
- Enroll at a local or community college to take cooking, history, or astronomy classes.
- Get a library card and participate in book club events.
- Get involved in nature-based activities, such as bird watching, botanical garden and park visits, farmer's market shopping, forest bathing or hiking, gardening, or walks at a lake, river, or beach.
- Join a group, such as a local bicycling club, chess, or table tennis club, or participate in your favorite hobby.
- Join a gym or fitness center.
- Join self-help groups.
- Join social media platforms like LinkedIn, Facebook, Twitter, Instagram, or TikTok.
- Play with your pets.
- Volunteer at a community center, hospital, school, or library.
- Volunteer to coach sports or mentor students.
- Walk with a mall club or create one in your neighborhood
If you are interested in learning more about these topics and others, please see my course Integrative and Lifestyle Medicine Toolbox for Rehab and Pain Management with Herman & Wallace.
Resources for Clinicians:
Learn how to include integrative and lifestyle medicine into your clinical practice with these resources:
- Academy of Integrative Health & Medicine
- American College of Lifestyle Medicine
- American College of Preventive Medicine
- Institute of Lifestyle Medicine
- National Center for Complementary and Integrative Health
Instructor Bio:
 Ziya "Z" Altug, PT, DPT, MS, OCS is a board-certified doctor of physical therapy with 32 years of clinical experience treating musculoskeletal injuries. Z currently provides outpatient physical therapy in the home setting in Los Angeles, California, and serves as a continuing education instructor.
Ziya "Z" Altug, PT, DPT, MS, OCS is a board-certified doctor of physical therapy with 32 years of clinical experience treating musculoskeletal injuries. Z currently provides outpatient physical therapy in the home setting in Los Angeles, California, and serves as a continuing education instructor.
Z received his Bachelor of Science in Physical Therapy at the University of Pittsburgh in 1989, Master of Science in Sport and Exercise Studies in 1985 and Bachelor of Science in Physical Education in 1983 from West Virginia University, and a Doctor of Physical Therapy from the College of St. Scholastica in 2015. Z is a long-standing member of the American Physical Therapy Association and a member of the American College of Lifestyle Medicine. He has attended workshops in yoga, tai chi, qigong, Pilates, Feldenkrais Method, and the Alexander Technique.
Z is the author of the books Integrative Healing: Developing Wellness in the Mind and Body (2018), The Anti-Aging Fitness Prescription (2006), and Manual of Clinical Exercise Testing, Prescription, and Rehabilitation (1993). In 2020, he published the chapter Exercise, Dance, Tai Chi, Pilates, and Alexander Technique in The Handbook of Wellness Medicine. In 2021, he published the article Lifestyle Medicine for Chronic Lower Back Pain: An Evidence-Based Approach in the American Journal of Lifestyle Medicine.
References:
- Frates, B., Bonnet, J.P., Joseph, R., & Peterson, J.A. (2019). Lifestyle Medicine Handbook: An Introduction to the Power of Healthy Habits. Monterey, CA: Healthy Learning.
- Altug Z. Integrative Healing: Developing Wellness in the Mind and Body. Springville, UT: Cedar Fort, Inc.; 2018.
- Kryger MH, Roth T, Goldstein CA. Principles and Practice of Sleep Medicine (2 Volume set), 7th ed. Philadelphia, PA: Elsevier; 2021
- Matsuo T, Miyata Y, Sakai H. Effect of salt intake reduction on nocturia in patients with excessive salt intake. Neurourol Urodyn. 2019;38(3):927-933.
- Vitale KC, Owens R, Hopkins SR, Malhotra A. Sleep hygiene for optimizing recovery in athletes: review and recommendations. Int J Sports Med. 2019;40(8):535-543.
- American College of Lifestyle Medicine. Handout: Lifestyle stress reduction. American College of Lifestyle Medicine; 2019.
- Leavell MA, Leiferman JA, Gascon M, Braddick F, Gonzalez JC, Litt JS. Nature-based social prescribing in urban settings to improve social connectedness and mental well-being: a review. Curr Environ Health Rep. 2019;6(4):297-308.
- National Institutes of Health. Social Wellness Toolkit. Bethesda, MD: National Institutes of Health. Accessed on June 2022.
- Roland M, Everington S, Marshall M. Social prescribing - transforming the relationship between physicians and their patients. N Engl J Med. 2020;383(2):97-99.
- Choi NG, Pepin R, Marti CN, Stevens CJ, Bruce ML. Improving social connectedness for homebound older adults: randomized controlled trial of tele-delivered behavioral activation versus tele-delivered friendly visits. Am J Geriatr Psychiatry. 2020;28(7):698-708.
- Davidson KW, Krist AH, Tseng CW, et al. Incorporation of social risk in US Preventive Services Task Force recommendations and identification of key challenges for primary care. JAMA. 2021;326(14):1410-1415.
- Eder M, Henninger M, Durbin S, et al. Screening and interventions for social risk factors: technical brief to support the US Preventive Services Task Force. JAMA. 2021;326(14):1416-1428.
- Steinman L, Parrish A, Mayotte C, et al. Increasing social connectedness for underserved older adults living with depression: a pre-post evaluation of PEARLS. Am J Geriatr Psychiatry. 2021;29(8):828-842.
Integrative and Lifestyle Medicine Toolbox for Rehab and Pain Management

Course Dates:
January 21, 2023
Price: $125
Experience Level: Beginner
Contact Hours: 4.5
Description: This course was written and developed by Ziya “Z” Altug, PT, DPT, MS, OCS, a board-certified doctor of physical therapy with 32 years of experience in treating musculoskeletal conditions, Brief lectures on the research and resources and labs will cover a toolbox approach for creating clinically relevant pain, anxiety, depression, and stress management strategies using lifestyle medicine, integrative medicine, expressive and art-based therapies, and the impact of nature on health. Participants will be able to practice Tai Chi/Qigong, expressive and art-based therapies including Music, Dance, and Drama Therapy, nature and aromatic therapies, self-hypnosis, and self-massage.
Kristina Koch, PT, DPT, is a board-certified clinical specialist in women’s health physical therapy and a certified lymphedema therapist. Kristina has been treating pelvic health conditions in individuals of all ages and genders since 2001 and works in private practice in Colorado Springs, CO. She has served as a guest lecturer for the pelvic health curriculum at Regis University in Denver and for the 3rd year medical students at the University of Colorado, Colorado Springs campus. She is the creator of Pharmacologic Considerations for the Pelvic Health Provider.
Although it is not within the scope of practice for rehab therapists to manage medications, it’s important that we review patient medications during the initial evaluation and on an ongoing basis. Therapists have a duty to assess medications impact on treatment and patient outcomes and to ensure patient safety. The population is aging and many patients over the age of 65 are on more than 5 medications, increasing the risk of medication side effects, adverse drug reactions, and drug interactions.
Primary care providers spend approximately 14-17 minutes with a patient during a visit, and the patient gets about 5 minutes to discuss their concerns, leaving little time for medication reconciliation or discussion regarding medication side effects (Tai-Seale, McGuire & Zhang, 2007). As therapists, we tend to see our patients for longer periods of time and more frequently, giving the patient more of an opportunity to discuss their signs and symptoms. Additionally, patients referred for pelvic health issues are often seeing multiple specialty providers (Ob/Gyn, urology, urogynecology, pain management, etc.) for their care, and each one is typically prescribing medications, potentially leading to polypharmacy. Understanding a medication’s actions, its impact on therapy, the side effects, and potential adverse drug reactions, can help guide treatment and improve patient outcomes.
A recent patient example is a post-menopausal cisgender female, referred by her primary care physician, for urinary urgency and nocturia. Her past medical history was significant for breast cancer. Her medications included an aromatase inhibitor, antihistamine due to seasonal allergies, and Vitamin C. After reviewing her medications and history, I recommended a non-hormonal vaginal lubricant and within 2 weeks her symptoms were 80% improved. Understanding the side effects of her medications allowed me to educate the patient about the effects of her medication and how to manage her symptoms.
More and more patients are attending therapy through direct access. As the first point of contact for patients, it's imperative that rehab professionals have a foundational knowledge of the medications often prescribed to treat pelvic floor conditions, GI, GU, and reproductive health issues. The ability to have educated conversations with our patients and other healthcare providers involved in their care can greatly improve the quality of care and outcomes, and maintain patient safety. The ability to discuss medications, vitamins, and supplements or complementary alternatives, that can minimize side effects, have fewer impacts on quality of life, and enhance function is an integral part of comprehensive patient care.
Join Kristina on Saturday, January 7, 2023, for Pharmacologic Considerations for the Pelvic Health Provider. This one-day, remote course will discuss the importance of understanding pharmacology and medication review, the current research regarding the pharmacologic treatment of numerous pelvic and reproductive health conditions and their side effects, drug interactions, and non-pharmacologic alternatives that are available for pelvic and reproductive health. Registration information and additional details are available at www.hermanwallace.com. #hermanwallacepelvicrehab, @hermanwallacepelvicrehab
References:
Ciccone, C. D. (2007). Pharmacology in Rehabilitation. (4th ed.). F.A. Davis Company.
Tai-Seale, M., McGuire, T.G., & Zhang, W. (2007). Time allocation in primary care office visits. Health Services Research. 42(5), 1871-1894. Doi: 10.1111/j.175-6773.2006.00689.x
Janes, M., & Kornetti, D. (2017). Medications: defining the role and responsibility of physical therapy practice. https://www.fsbpt.org/Portals/0/documents/free-resources/WinterForum2017Medications.pdf?ver=pf8bn4ZwoorAAg1PECZLfw%3D%3D
Pharmacologic Considerations for the Pelvic Health Provider

Course Dates:
January 7, 2023
Price: $200
Experience Level: Beginner
Contact Hours: 7.5
Description: This seven-and-a-half hour, one-day remote learning course will discuss medications used for the treatment of pelvic floor and genitourinary conditions as well as common side effects of medications routinely used for pelvic floor dysfunction. This course will be taught by Kristina Koch, PT, DPT via Zoom. Medications for constipation and GI dysfunction, as well as pelvic pain conditions such as Vulvodynia, Chronic Prostatitis, and Endometriosis, will be covered. The course will also cover medications and side effects in Gender-Affirming Care for patients who are transitioning.
Sandra Gallagher has served on varied committees and boards at the state and national level, most recently as the chair of the CAPP-OBC committee for the Academy of Pelvic Health of the APTA. She has presented on the role of PT in gender-affirming vaginoplasty at UCSF Transgender Health Summit, APTA Combined Sections Meeting, and at the 2018 international meeting of the World Professional Association for Transgender Health (WPATH). Join Transgender Patients: Pelvic Health and Orthopedic Considerations with instructors Sandra Gallagher, PT, DPT, WCS & Caitlin Smigelski, PT, DPT on April 29th.
In working with surgeons that perform and patients undergoing gender-affirming genital surgery I’ve had the chance to recognize that some of our most basic skills of assessing tissue and tissue healing play a huge role and optimizing healing. I personally have loved taking another look at some of the wound healing principles that I used early in my career in the 90s, to assist in developing timelines for post-surgical recoveries of gender surgeries.
In addition to the basic science of tissue healing, we’ve integrated current and novel neuroscience to develop Graded Motor Imagery guidelines to improve the sensory outcomes of vaginoplasty and phalloplasty surgeries. Graded Motor Imagery (GMI) is a treatment approach commonly associated with treating pain. It is generated from understanding the underlying neuroplasticity of complex pain conditions such as phantom limb pain. (1) Graded Motor Imagery in rehabilitation means that the focus is placed on synaptic exercise and health. The use of neuroplasticity to change sensory experiences occurs in other parts of rehab and goes under different names. Sensory integration, cortical integration, or mapping, are some other terms used. In addition to being used for reducing pain in complex regional pain syndrome, the techniques are used for reducing limb neglect in stroke rehab, and restoring limb function in complex hand surgeries (2,3,4,5). In pelvic rehab, we are using these concepts with urinary urgency suppression and in cis females with vaginal pain. There are handfuls of article exploring the presence and phenomena of phantom penis in trans men (6,7,8)
Using GMI for Phalloplasty
When using GMI for phalloplasty, the primary goal is to improve erogenous sensation in the penis. This is done with three main techniques: visualization of static and dynamic functions of the penis, tactile stimulation starting with a simple touch and progressing toward sensory stimulation, and sexual/erogenous stimulation (9). As people move through the process they use stimulation of the buried erectile tissue and other erogenous parts of their body while touching the penis. This can be a partnered or independent activity. This can be adapted regardless of the number of stages involved in the surgery.
Using GMI for Vaginoplasty
With vaginoplasty, the attaining pain-free and erogenous sensation typically progresses more directly than in phalloplasty, as there are fewer complications with vascular and nerve recovery. The clitoris and its neurovascular bundle are intact and continue to be perineal tissue. We use traditional pelvic rehab interventions of clinical EMG, and a robust home program of dilation, exercise, TENS, and self-care including patient-directed manual interventions. The addition of GMI guidelines for vaginoplasty more commonly is directed toward reducing vulvovaginal pain. Whereas the phalloplasty sensory protocol is initiated early in the surgical process, the vaginoplasty guidelines are more commonly applied when post-surgical pain limits someone's function. The GMI process here uses visualization and activities of seeing vulvas in one's surrounding environment, such as flowers, folded fabrics, and Georgia O'Keefe artworks. This is intended to be a neutral practice. Similar to the desensitization process in limb rehab, using various textures and depth of touch, combined with watching the light touch can help with pain reduction. As pain abates using stimulation of other erogenous tissue while touching the vulva or dilating can be added.
For providing optimal care, knowledge of the intricacies of gender transition is essential. Join me in Transgender Patients: Pelvic Health and ORTHO Considerations on April 29th to learn more regarding gender-affirming genital surgeries, discussion of other gender-affirming surgeries, and medical interventions that people transitioning might choose. We provide that overview in this course. Topics covered include:
- Societal influence on gender transition including interactions with healthcare providers
- Recognizing the difference between sex, sexuality, and gender
- Understanding the complexities of the legal system for the person transitioning genders
- Tips and tools for a trauma-informed intake and examination
- Health effects of hormones for gender transition as related to differential diagnosis in rehabilitation
- Supporting healing after gender-affirming surgery
- Operative procedures for face and chest
- Operative procedures for masculinizing and feminizing genital surgery
- Preoperative evaluation, treatment, and education issues
- Post-operative evaluation, treatment, education and follow-up for genital surgeries
- Outcome measures with rehab focus for people undergoing gender-affirming surgeries
- Fertility and pregnancy in gender-diverse people
References:
- Moseley GL. Graded motor imagery for pathologic pain: a randomized controlled trial. Neurology. 2006 Dec 26;67(12):2129-34. doi: 10.1212/01.wnl.0000249112.56935.32. Epub 2006 Nov 2. PMID: 17082465.
- Smart KM, Wand BM, O'Connell NE. Physiotherapy for pain and disability in adults with complex regional pain syndrome (CRPS) types I and II. Cochrane Database Syst Rev. 2016 Feb 24;2(2): CD010853. doi: 10.1002/14651858.CD010853. Pub2. Update in: Cochrane Database Syst Rev. 2022 May 17;5:CD010853. PMID: 26905470; PMCID: PMC8646955.
- Leifert-Fiebach G, Welfringer A, Babinsky R, Brandt T. Motor imagery training in patients with chronic neglect: a pilot study. NeuroRehabilitation. 2013;32(1):43-58. doi: 10.3233/NRE-130822. PMID: 23422458.
- Simon JJ, Welfringer A, Leifert-Fiebach G, Brandt T. Motor imagery in chronic neglect: An fMRI pilot study. J Clin Exp Neuropsychol. 2019 Feb;41(1):58-68. doi: 10.1080/13803395.2018.1500527. Epub 2018 Aug 6. PMID: 30080434.
- Kahn LC, Moore AM. Donor Activation Focused Rehabilitation Approach: Maximizing Outcomes After Nerve Transfers. Hand Clin. 2016 May;32(2):263-77. doi: 10.1016/j.hcl.2015.12.014. PMID: 27094897.
- Chris Straayer (2020) Phantom Penis: Extrapolating Neuroscience and Employing Imagination for Trans Male Sexual Embodiment, Studies in Gender and Sexuality, 21:4, 251-279, doi: 10.1080/15240657.2020.1842075.
- Ramachandran VS, McGeoch PD. Occurrence of phantom genitalia after gender reassignment surgery. Med Hypotheses. 2007;69(5):1001-3. doi: 10.1016/j.mehy.2007.02.024. Epub 2007 Apr 8. PMID: 17420102.
- Gherovici, Patricia. (2020). A Phantom Phallus? Studies in Gender and Sexuality. 21. 296-301, doi: 10.1080/15240657.2020.1842070.
- Peters BR, Annen AA, Berli JU, Gallagher S, Smigelski C, Kahn LH, Skelton HE. Neurosensory Re-education following Gender-affirming Phalloplasty: A Novel Treatment Protocol. Plast Reconstr Surg Glob Open. 2022 Oct 24;10(10):e4616. DOI: 10.1097/GOX.0000000000004616. PMID: 36299822; PMCID: PMC9592297.
Transgender Patients: Pelvic Health and ORTHO Considerations
Price: $500 .00 Experience Level: Beginner Contact Hours: 17 hours
This course is appropriate for any physical rehabilitation professional, regardless of their specialty area, who has an interest in better serving the people who are gender diverse. There is specific content aimed at teaching pelvic health therapists how to expand their skills for working with people of all gender identities. There will be particular education regarding gender-affirming genital surgeries as well as discussion of other gender-affirming surgeries and medical interventions that people transitioning might choose.
Course Dates: April 29 and August 19
Allison Ariail, PT, DPT, CLT-LAANA, BCB-PMD is one of the creators of the Herman & Wallace Oncology of the Pelvic Floor Course Series. Allison Ariail is a physical therapist who started working in oncology in 2007 when she became certified as a lymphatic therapist. She worked with breast cancer, lymphedema patients, head and neck cancer patients, and the overall oncology team to work with the whole patient to help them get better. When writing these courses, Allison was part of a knowledgeable team that included Amy Sides and Nicole Dugan among others.
June is National Cancer Survivor Month. When individuals talk about “survivorship,” they are referring to the process of navigating their life experiences and the difficulties that they have as a result of their cancer diagnosis. Survivorship begins at the time of diagnosis and includes those individuals that are undergoing treatment, those after treatment with no signs of cancer, those undergoing extended treatment to control the cancer, those undergoing extended treatment to reduce the risk of the return of cancer, and those individuals with advanced cancer. According to cancer.net, there were 18 million people in the United States living with a history of cancer.1 Considering the number of people surviving cancer, and the degree of medical treatment can vary for each of them, there will be a wide range of needs from cancer survivors. Rehabilitation professionals are in a unique position where we can help patients in many different ways to help improve their function, ability to participate in activities that they enjoy and improve their quality of life.
There are multiple studies that show how rehabilitation can help cancer survivors. The research varies in its focus; it could be examining specific side effects such as chemotherapy-induced peripheral neuropathy, looking at the effects of fatigue after treatment, or to sexual health after cancer diagnoses. In January of this year, a study came out that showed a physical rehabilitation program of moderate intensity promoted a relief of general and physical fatigue.2 This is huge for cancer patients! Fatigue is an immense problem that survivors suffer from. Another study from 2019 showed that a 12-week exercise-based training program can negate some of the deficits that occur in strength and physical function that occur from the medical treatment of cancer.3 The exercise program, which included both aerobic and resistance training, helped both middle-aged and older adults improve their physical function and strength. In 2018 Dennet et al performed a qualitative study of cancer survivors’ experiences of an exercise-based rehabilitation program. They determined that an exercise-based cancer rehabilitation program was important in facilitating a ‘return to normal’ and helped patients increase their ability to participate in physical activities.4
We as clinicians should embrace this research and work to get these patients referred to us for rehab! As we can see from the above research, this is a population that could greatly use rehabilitation, yet they may not be getting the referrals they need. In 2022, Thorsen et al surveyed almost 1000 young adult survivors. They found that a large proportion of long-term young adult cancer survivors report needing information about lifestyle and rehabilitation more than a decade after they completed their treatment.5 Let’s get these and other aged survivors in for treatment so we can help them feel better and get back to living their lives! Working with oncology patients can be very rewarding. When asked how therapy has influenced her, one patient responded “My PT has played a significant role in my recovery from surgery and the side effects of cancer treatment. She pays attention to and treats ‘the little things’ that are often forgotten about but yet have the biggest impact on my quality of life. She is there helping me long after my other doctors are done treating me.”
Herman & Wallace offers an Oncology Series that can help you gain the knowledge and skills to be able to help these patients. In Oncology of the Pelvic Floor Level 1, we cover general oncology. In this course, we learn about cancer treatment, short-term side effects, and long-term side effects, and learn rehab techniques to help these patients. In Oncology of the Pelvic Floor Level 2A and Oncology of the Pelvic Floor Level 2B we go more in-depth with pelvic-related cancers. In Level 2A we cover topics related to testicular cancer, prostate cancer, penile cancer, and colorectal cancers while in Level 2B we cover topics related to gynecological cancers and bladder cancer. In both courses, you learn hands-on treatment techniques to help patients recover function, and feel better. Please join us by taking this series to be able to help these patients!
Resources:
- What is cancer survivorship? Cancer.net. 7/2021 https://www.cancer.net/survivorship/what-cancer-survivorship
- Penna GB, Otto DM, D Silva T, et al. Physical rehabilitation for the management of cancer-related fatigue during cytotoxic treatment” a systemic review with meta-analysis. Support Care Cancer 31 (2023). https://doi.org/10.1007/s00520-022-07549-7
- Dittus K, Toth M, Priest J, et al. Effects of an exercise-based oncology rehabilitation program and age on strength and physical function in cancer survivors. Support Care Cancer 28, 3747-3754 (2020). https://doi.org/10.1007/s00520-019-05163-8
- Dennett AM, Peiris CL, Taylor NF, et al. “A good stepping stone to normality’: a qualitative study of cancer survivors’ experiences of an exercise-based rehabilitation program. Support Care Cancer 27, 1729-1736. (2019). https://doi.org/10.1007/s00520-018-4429-1
- Thorsen L, Bohn SK.H, Lie HC, et al. Needs for information about lifestyle and rehabilitation in long-term young adult cancer survivors. Support Care Cancer. 30, 521-533 (2022). https://doi.org/10.1007/s00520-021-06418-z
*Certified Lymphatic Therapists may skip Oncology of the Pelvic Floor Level 1 and move on to the Level 2A and Level 2B courses.*
Oncology of the Pelvic Floor Level 1
No partner needed for registration
Price: $550.00 Experience Level: Beginner Contact Hours: 17.5 hours
Description: The course will address issues that are commonly seen in a patient who has been diagnosed with cancer such as cardiotoxicity, peripheral neuropathy, and radiation fibrosis. Some holistic medicine topics, including yoga and mindfulness, will be discussed in order to fully prepare the participant to be able to competently work with cancer survivors.
The basics of the lymphatic system will be covered, as well as when to refer the patient to a lymphatic specialist for further treatment. Red flags and warning symptoms will be discussed so the participant feels comfortable with knowing when to refer the patient back to their medical provider for further assessment.
This introductory course is aimed to get the participant comfortable with working with oncology patients and as part of an interdisciplinary oncology team.
Course Dates: July 8-9 and December 2-3
Oncology of the Pelvic Floor Level 2A
Participants MUST register with a partner, or plan to have a volunteer available to work on during course labs.
Price: $495.00 Experience Level: Intermediate Contact Hours: 17.25 hours
This course was designed to build on the information that was presented in Oncology of the Pelvic Floor Level 1.
Description: Information will be provided focusing on male pelvic cancers, colorectal cancer, and anal cancer including risk factors, diagnosis, and prognosis. The participant will also understand the sequelae of the medical treatment of cancer and how this can impact a patient’s body and quality of life. Other topics will include rehabilitation and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy.
Course Dates: September 23-24
Oncology of the Pelvic Floor Level 2B
Participants MUST register with a partner, or plan to have a volunteer available to work on during course labs.
Price: $600.00 Experience Level: Intermediate Contact Hours: 19.25 hours
This course was designed to build on the information that was presented in Oncology of the Pelvic Floor Level 1.
Description: Information will be provided focusing on gynecological and bladder cancers including risk factors, diagnosis, and prognosis. The participant will also understand the sequelae of the medical treatment of cancer and how this can impact a patient’s body and quality of life. Other topics include rehabilitation and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy.
Course Dates: December 9-10
Allison Ariail, PT, DPT, CLT-LAANA, BCB-PMD is one of the creators of the Herman & Wallace Oncology of the Pelvic Floor Course Series. Allison Ariail is a physical therapist who started working in oncology in 2007 when she became certified as a lymphatic therapist. She worked with breast cancer, lymphedema patients, head and neck cancer patients, and the overall oncology team to work with the whole patient to help them get better. When writing these courses, Allison was part of a knowledgeable team that included Amy Sides and Nicole Dugan among others.
As pelvic rehab professionals, we know the importance of the microbiome of the digestive tract and how this can influence issues our bowel patients may experience. You also may know that the GI microbiome can influence immune function as well as mental health. Did you know that the urinary bladder has its own microbiome? Recent developments in next-generation sequencing and bioinformatic platforms have allowed for the detection of microbial DNA in the urinary tract.(1) This could be a game changer for those who suffer from chronic urinary tract infections. However, it could be even more important as a way to prevent bladder cancer. May is Bladder Cancer Awareness Month. In honor of this month, let’s further discuss how the urinary microbiome may influence the development of bladder cancer.
Dysbiosis of the urinary microbiome could be related to bladder cancer through chronic inflammation in the urothelial microenvironment. Chronic inflammation is a hallmark of genomic instability and the development of cancer. A study in 2021 compared the urinary microbiome of patients with muscle-invasive and non-muscle-invasive bladder cancer. They found the microbial profiles differed in patients with cancer compared to healthy individuals. They also found that there were different microbial profiles from the less invasive non-muscle invasive versus the more invasive types of bladder cancer.(2)
The urinary microbiome is a growing area of research and I would expect to see more information come out on this, what influences the urinary microbiome, as well as how modulating this can prevent and fight urothelial cell carcinoma. I would anticipate more treatment options including some new immunotherapy agents to emerge that can help to fight bladder cancer.
If you do not know much about bladder cancer and would like to learn more, Oncology of the Pelvic Floor Level 2B covers topics on bladder cancer and gynecological cancers. Join us to learn more about these diagnoses, medical treatments, and ways a pelvic rehab professional can help these patients recover.
Resources:
1. Neugent ML, Hulyalkar NV, Nguyen VH, Zimmern PE, and De Nisco NJ. Advances in understanding the human urinary microbiome and its potential role in urinary tract infection. mBio. 2020; 11(2): e00218-20.
2. Hussein AA, Elsayed AS, Durrani M, et al. Investigating the association between the urinary microbiome and bladder cancer: an exploratory study. Urol Oncol. 2021; 39(6): 370.e9-370e19.

*Certified Lymphatic Therapists may skip Oncology of the Pelvic Floor Level 1 and move on to the Level 2A and Level 2B courses.*
Oncology of the Pelvic Floor Level 1 - no partner needed for registration
Price: $550.00 Experience Level: Beginner Contact Hours: 17.5 hours
Description: The course will address issues that are commonly seen in a patient who has been diagnosed with cancer such as cardiotoxicity, peripheral neuropathy, and radiation fibrosis. Some holistic medicine topics, including yoga and mindfulness, will be discussed in order to fully prepare the participant to be able to competently work with cancer survivors.
The basics of the lymphatic system will be covered, as well as when to refer the patient to a lymphatic specialist for further treatment. Red flags and warning symptoms will be discussed so the participant feels comfortable with knowing when to refer the patient back to their medical provider for further assessment.
This introductory course is aimed to get the participant comfortable with working with oncology patients and as part of an interdisciplinary oncology team.
Course Dates: July 8-9 and December 2-3
Oncology of the Pelvic Floor Level 2B - partner needed for registration
Price: $600.00 Experience Level: Intermediate Contact Hours: 19.25 hours
This course was designed to build on the information that was presented in Oncology of the Pelvic Floor Level 1.
Description: Information will be provided focusing on gynecological and bladder cancers including risk factors, diagnosis, and prognosis. The participant will also understand the sequelae of the medical treatment of cancer and how this can impact a patient’s body and quality of life. Other topics include rehabilitation and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy.
Course Dates: December 9-10
Megan Pribyl, PT, CMPT is a physical therapist at the Olathe Medical Center in Olathe, KS treating a diverse outpatient population in orthopedics including pelvic rehabilitation. Megan’s longstanding passion for both nutritional sciences and manual therapy has culminated in the creation of her remote course, Nutrition Perspectives for the Pelvic Rehab Therapist, designed to propel understanding of human physiology as it relates to pelvic conditions, pain, healing, and therapeutic response.
I have always viewed resultant health as the sum total of nutrition, exercise, lifestyle factors, environmental/toxicant & chemical exposure, genetics, and spiritual confluences. In balance, health and vitality flourish. Out of balance, health struggles manifest. If we take a look around, we bear witness to modern culture’s harmful effects upon our physiology – and specifically on our blood-brain barrier (BBB). Health struggles affecting the brain and impacted by BBB dysfunction are diverse and can include anxiety, depression, chronic pain, and neurodevelopmental disorders. Other disorders linked to a compromised BBB include Alzheimer’s disease, dementia, Parkinson’s Disease, and MS. So we ought to care a lot about our BBB – yet most of us don’t make conscious lifestyle choices based on protecting this vital gatekeeping system. Perhaps if we examine one specific angle of this issue - that diet and short-chain fatty acids influence the integrity of the blood-brain barrier – we might decide to care a lot more about protecting our brain – like we mean it.
For starters, it helps to acknowledge that our entire body IS an immune system – one that is constantly surveying potential threats to our existence. It is very well established that 70% of our immune system resides in our gut. This placement makes sense because the very act of eating exposes our inner workings to whatever “food” passes through the alimentary canal. Our digestive tract is a frontline sorting station that decides what can pass through the intestinal barrier and what cannot. Having a strong intestinal barrier is critical to maintain health as evidenced by a wealth of both animal and human studies.
Most of us also don’t constantly think about our intestinal barrier – but science contends that we should. Because what happens there impacts our entire body and all systems – including our nervous system. A recent study even describes a “Gut Spinal Cord Immune Axis” wherein the health of our spinal cord itself is dependent on immune factors regulated by the gut microbiota. (3) That’s how far your gut health influence goes.
So, let’s talk about one way our gut, a.k.a. microbiome, keeps us healthy. The microbes in our large intestine should be numerous and diverse. These microbes thrive in the presence of prebiotic fiber components (sources of prebiotic fiber are diverse, from the plant world and include things like Jerusalem artichoke, bananas, onions, berries, garlic, and other herbs and spices) which arrive in the colon because they are consumed by the host – us. When your microbes feast on the prebiotic fibers, they produce a by-product, and this byproduct is SCFA’s or short-chain fatty acids. It is well established that these SCFAs play a powerful immunomodulatory role both locally (in the intestine) and distantly (e.g. at the blood-brain barrier). This is the best way to create healthy short-chain fatty acids so they can do what they do best in our system – modulate inflammation.
But what happens if we don’t have richness (as in ample number) or diversity (as in different health-promoting species) of microbes in our large intestine? We can’t produce as many SCFAs.
What happens if we don’t consume the food (eg. prebiotic fiber) our microbes like to eat? Or if we aren’t eating foods that contain microbes (eg. cultured foods)? We can’t produce as many SCFAs.
What happens if we are deficient in healthy SCFAs? We may end up with undesirable physiological sequelae such as systemic inflammation. Which can include blood-brain barrier inflammation. (2)
Remember that we have nerves everywhere in our body – centrally and peripherally. If any of the nerves in our body (peripheral nerves), brain (CNS), or gut (ENS) are inflamed, this can be termed neuroinflammation. Neuroinflammation in the CNS leads to blood-brain barrier inflammation resulting in increased permeability – this ultimately allows substances to reach the brain that shouldn’t.
Neuroinflammation is at the root of many of the health sequelae we currently see in non-communicable conditions. (5) Maybe in your patient it manifests as chronic pain. Maybe in your friend, it’s anxiety and depression. Maybe in your aunt it’s MS, your uncle it’s Alzheimer’s. Maybe in your neighbor it’s fibromyalgia. Neuroinflammation has many faces.
When we look at factors that contribute to blood-brain barrier dysfunction, many can be traced to the cumulative effects of a standard American diet and lack of nutrient density. Further, and more ubiquitous – is our unseen exposure to toxicants such as herbicides and pesticides as well as a multitude of other potential cell health disruptors. (1, 4)
Because of the massive implications of human disease states, we need to pay attention to what the literature is telling us about the interconnected nature of health and lifestyle. We must stop polluting our human physiology and we must start feeding ourselves food that isn’t paradoxically decimating our microbiome. It’s that simple. And complicated. At the same time.
Taking a deep breath is the first step. A crucial second step is staring down the truth of our country’s health care and agricultural realities. The third is gaining perspective on what actions each of us can take today – wherever we live, whatever our socioeconomic status, and whatever our current health status. There is much work to do.
I invite you to an opportunity to learn about many actions we can take today and examine nutritional concerns in depth that have implications not only for the population you treat as a pelvic rehab therapist but for yourself, your friends, and your extended human family.
We must prioritize protective health choices. We must care for our gut, propagate healthy short-chain fatty acids, and therefore care for our blood-brain barrier. And subsequently, protect our brain - like we mean it. Because our modern culture will not do that for us. Solving our nation’s health crises will take each of us collectively to make a difference. The health status of our nation can improve – one protected brain at a time.
Join us for our next offering of Nutrition Perspectives for the Pelvic Rehab Therapist scheduled for June 10-11, 2023.
References:
- Abou Diwan M, Lahimer M, Bach V, Gosselet F, Khorsi-Cauet H, Candela P. Impact of Pesticide Residues on the Gut-Microbiota-Blood-Brain Barrier Axis: A Narrative Review. Int J Mol Sci. 2023 Mar 24;24(7):6147. doi: 10.3390/ijms24076147. PMID: 37047120; PMCID: PMC10094680.
- Fock E, Parnova R. Mechanisms of Blood-Brain Barrier Protection by Microbiota-Derived Short-Chain Fatty Acids. Cells. 2023 Feb 18;12(4):657. doi: 10.3390/cells12040657. PMID: 36831324; PMCID: PMC9954192.
- Raue KD, David BT, Fessler RG. Spinal Cord-Gut-Immune Axis and its Implications Regarding Therapeutic Development for Spinal Cord Injury. J Neurotrauma. 2023 Mar 10. doi: 10.1089/neu.2022.0264. Epub ahead of print. PMID: 36509451.
- Sharma T, Sirpu Natesh N, Pothuraju R, Batra SK, Rachagani S. Gut microbiota: a non-target victim of pesticide-induced toxicity. Gut Microbes. 2023 Jan-Dec;15(1):2187578. doi: 10.1080/19490976.2023.2187578. PMID: 36919486; PMCID: PMC10026936.
- Takata F, Nakagawa S, Matsumoto J, Dohgu S. Blood-Brain Barrier Dysfunction Amplifies the Development of Neuroinflammation: Understanding of Cellular Events in Brain Microvascular Endothelial Cells for Prevention and Treatment of BBB Dysfunction. Front Cell Neurosci. 2021 Sep 13;15:661838. doi: 10.3389/fncel.2021.661838. PMID: 34588955; PMCID: PMC8475767.
Nutrition Perspectives for the Pelvic Rehab Therapist

Price: $525.00 Experience Level: Beginner Contact Hours: 17.5 hours
Course Dates: June 10-11, September 16-17, and December 2-3
Description: Participants will be introduced to the latest research in nutrition through immersive lectures and hands-on labs. The course will cover essential digestion concepts, nourishment strategies, and the interconnected nature of physical and emotional health across the lifespan. Further, clinicians will delve into nutritional relevancies in bowel and bladder dysfunction, pelvic health, pain, and healing. Labs throughout include insightful demonstrations and breakout sessions. The course participant will acquire new, readily applicable tools for patient empowerment, engagement, and self-management utilizing presented principles.
Mora Pluchino is instructing her ethics course, Ethical Considerations from a Legal Lens, which is scheduled for June 3, 2023. This remote course covers ethical considerations from a legal lens for professionals working in the area of Pelvic Health. Health Care Professionals have many day-to-day ethical considerations to “do no harm” including basic decisions for billing, patient care, safety, and compliance. Pelvic Rehabilitation comes with additional layers of vulnerability and ethical challenges, and the legalities of pelvic health can add further complications for patient care, business, and clinical practice decisions.
The patient is a 70 cis-gender female:
- Primary complaints - Painful sitting, terrible tailbone pain x 2 years
- Secondary complaints - SUI, fecal urgency, mild POP
- Prior therapy - multiple, most recent Hospital Based OPPT 3 x per week x 8 weeks (24 visits)
- Progress - minimal to none, the patient actually thinks her symptoms are worsening, pain is unbearable
- Other diagnoses - Parkinson’s Disease, HTN, high cholesterol
- Primary Insurance - Medicare
SEPTEMBER
The patient presents to the provider for specialized pelvic floor therapy. The patient is seen 1 x per week for a total of 6 visits. The patient reports a 75% reduction in symptoms, adheres to her HEP, and attends all scheduled visits.
Treatment Included:
- Internal rectal musculature work (Instructed in Pelvic Floor Level 2A)
- Body mechanics and coccyx mobilization - internal and external (Instructed in Coccydynia & Painful Sitting)
- Sacral nerve release techniques (Instructed in Sacral Nerve Manual Assessment and Treatment)
NOVEMBER
The patient is now able to participate in her ADL, regular exercise routine, and her social life and she has noticed how her endurance and balance have declined as she tries to return to normal. She starts to come in 2 x per week, one day a week focusing on her pelvic floor complaints and one day a week focusing on her endurance, balance, and Parkinson’s symptoms. She completes an additional round of therapy 2x per week for 8 weeks. She progresses slowly but objectively measures small therapy gains.
Additional treatment:
- General strength and endurance training and conditioning
- Large amplitude movement program
- Education for a home walking program
- Connection to a Parkinson’s boxing program in the community
FEBRUARY
The patient gets sick, misses 2 weeks of therapy, and has a return in her coccyx pain and an exacerbation of her Parkinson’s symptoms. Her tremors became so bad that she has to cancel multiple sessions at the last minute. She is now also having swallowing and speech problems. She finally gets in with her neurologist who explains her Parkinson’s has progressed. They recommend changing her medications, assessment for a brain stimulator, and trying an intensive LSVT BIG Program 4x per week for 4 weeks.
Please pause and take a moment to think about a few things that may pop up for a provider from an ethical or legal lens!
SOME ETHICAL + LEGAL CONSIDERATIONS FOR THE CASE
- Prior to beginning the LSVT BIG program, the patient is already at 46 visits in total
- Your practice is a small, niche market practice that specializes in Pelvic Health - this patient only ended up with you due to her tailbone pain - your location is small and does not have “big gym” equipment or space
- You do have two providers that have prior LSVT BIG training
- This patient has worked with and reports feeling safe and comfortable with both providers
- Sitting in the car for more than 45 minutes is again a challenge for the patient and you are the closest qualified provider to her home
- You are the only Pelvic Floor clinic within the 15-mile radius
- To accommodate this patient’s scheduling needs will make your waitlist longer for others
- Medicare has an annual cap for services which changes based on practice setting. Physical therapy and Speech therapy share this cap.
- This patient has been plateauing/ possibly worsening as her Parkinson’s progresses and sessions are feeling like maintenance therapy.
- There are hospital-based LSVT BIG programs 55 minutes away from the patient's home.
The fun and challenging part about ethics is that the possibilities and scenarios are many and ever-changing. This is a real live case and an example of what therapists have to navigate on a day-to-day basis. Sadly, there is no right or wrong. Ethics and Law are areas of more gray than black and white.
Ethical Considerations from a Legal Lens has the following goals:
- Define basic Ethical Framework topics
- Perform Core Values Self Assessment
- Identify the components of the RIPS model and the Model Rules of Professional Conduct
- Explore Pelvic Health from a Legal Lens
- Apply the RIPS model to real-life legal scenarios
- Devise a plan of action or solution to legal and ethical scenarios
The hope is that with this understanding of things like beneficence (balance harms and benefits), non-malfeasance (do no harm), justice (fairness), and autonomy (respect for self-determination) as well as being well-versed in patient care topics like consent, abuse, misconduct, discrimination, and our individual practice acts, providers will feel more comfortable in their ethical decision making.
Ethical Considerations from a Legal Lens and Ethical Concerns for the Pelvic Health Professionals both offer the information needed to have these conversations and start problem-solving these decisions. It is encouraged as part of the precourse work to send in the ethical concerns that have you stuck in the clinic or keep you awake at night!
Ethical Considerations from a Legal Lens
Price: $175.00 Experience Level: Beginner Contact Hours: 6 hours
Course Dates: June 3 and November 12
Description: This one-day remote course covers ethical considerations from a legal lens for professionals working in the area of Pelvic Health. In general, Health Care Professionals have many day to day ethical considerations to “do no harm.” This includes basic decisions for billing, patient care, safety and compliance. Pelvic Rehabilitation comes with additional layers of vulnerability and ethical challenges, and the legalities of pelvic health can add in further complications for patient care, business and clinical practice decisions.
Ethical Concerns for the Pelvic Health Professionals

Price: $175.00 Experience Level: Beginner Contact Hours: 6 hours
Course Dates: September 16
Description: This one day remote course covers ethical considerations for professionals working in the area of Pelvic Health. In general, Health Care Professionals have many day to day ethical considerations to “do no harm.” This includes basic decisions for billing, patient care, safety, and compliance. Pelvic Rehabilitation comes with additional layers of vulnerability and ethical challenges due to the anatomical areas being treated, topics being discussed, and intimacy of sessions.

Dawn Sandalcidi PT, RCMT, BCB-PMD is a trailblazer and leading expert in the field of pediatric pelvic floor disorders. She graduated from SUNY Upstate Medical Center in 1982 and is actively seeing patients in her clinic Physical Therapy Specialists, Centennial CO. Additionally, she runs an online teaching and mentoring platform for parents and professionals at www.kidsbowelbladder.com.
Dawn is a national and international speaker in the field, and she has gained so much from sharing experiences with her colleagues around the globe. In addition to lecturing internationally on pediatric bowel and bladder disorders, You can join Dawn Sandalcidi with H&W in her courses, Pediatrics Level 1 - Treatment of Bowel and Bladder Disorders and Pediatrics Level 2 - Advanced Pediatric Bowel and Bladder Disorders. This year H&W is excited to announce that Dawn will be teaching live for the first time since 2020, join her at the Pediatrics Level 1 course in Syracuse NY on June 3-4, 2023.
Why you should have these tools in your toolbox today.
As a clinician, it can be challenging to take a step back and look at every single patient as a whole person. Time constraints, hectic schedules, and never-ending notes make it difficult for you to do everything you’d like. Have you ever fantasized about an all-inclusive, multi-disciplinary center where physical therapists, occupational therapists, speech therapists, and other professionals gather weekly to assess a caseload of patients and make recommendations personalized to those patients?
Although clinics like this are not very common, you can bring a sense of this comprehensive approach to your clinic by expanding what you offer. As you know, many pediatric clinics offer PT, OT, Speech, and maybe aquatic therapy or early intervention services. Clinics offering pediatric pelvic floor therapy are more limited but on the rise.
You can bring these much needed services to your own clinic, and gain this knowledge without even leaving your home! If you’ve never considered expanding your services to include pelvic floor therapy for your pediatric patients, it’s time to explore exactly how this skill set can impact your patients’ lives.
Who Needs Pediatric Pelvic Floor Therapy?
Pediatric pelvic floor therapy is for children with bowel and bladder issues. Many of them also have special needs and will frequent your pediatric therapy centers. Since these patients in need will already be in your clinic, why not address as many of their issues as possible, all in one place?
Neurotypical children, as well as those with special needs (like children with cerebral palsy, spina bifida, sensory processing disorders, and other developmental or behavioral issues) often struggle with bowel and bladder conditions in addition to their chief complaints. These families may struggle on a daily basis to manage exercises, feeding, play, and oftentimes, toileting troubles as well.
You may be thinking that bowel and bladder issues are reserved only for children with more severe conditions, however many children with bowel and bladder issues do not have any underlying neurological conditions. Oftentimes, these bowel and bladder issues in children are due to pelvic floor dysfunction (PFD).

It’s not as easy for children to communicate when something is wrong, PFD can go undetected for long periods of time in this population. A study from 2019 found that 46% of constipated children and 67% of children with fecal incontinence rated bowel habits as good or very good. The authors also noted 50% of constipated children did not mention their symptoms to anyone.
Parents don’t always know what’s normal and even when they do figure out there’s an issue, they often don’t have a clue about where to start, or what pediatric pelvic floor therapy even is.
What is Pediatric Pelvic Floor Therapy?
Pediatric pelvic floor therapy is a specialty area with a focus on pelvic conditions and symptoms for children up to 18 years old. Pelvic conditions and symptoms will frequently affect both bowel and bladder function in children.
Pediatric pelvic floor therapy is one of several treatment methods under the umbrella of “Urotherapy”. Urotherapy is a non-standardized conservative based treatment option for children with voiding dysfunctions.2 Dysfunctional voiding (DV) refers to a group of abnormal lower urinary tract (LUT) symptoms such as straining, hesitancy, and dysuria. Other LUT symptoms involved are related to bladder storage, such as frequency, urgency, and incontinence.
Pediatric pelvic floor therapy is a great first-line treatment option for functional constipation. This refers to a vicious cycle of stool retention in the rectum which eventually leads to distention, loss of urge, and more constipation. Functional constipation is directly related to LUT symptoms and DV. It is estimated that up to 50% of children suffer from LUT symptoms with constipation at some point.
A majority of children with bowel and bladder dysfunction can be successfully treated with pediatric pelvic floor therapy. Your treatment plan may include education, lifestyle changes, bowel and bladder diaries, pelvic floor and trunk muscle retraining, sEMG, and more. In order to provide the best recommendations for families with children suffering from bowel and bladder dysfunction, it’s important to begin with a thorough initial evaluation.
What Does a Pediatric Pelvic Floor Therapy Evaluation Involve?
I would argue that almost every child could benefit from a pediatric pelvic floor therapy evaluation. Just like with pelvic floor therapy for adults, much of what you’ll do for pediatric pelvic floor patients is completely external. So many children will have significantly improved quality of life with basic behavioral changes.

Pediatric pelvic floor therapy evaluations involve first investigating the source of bowel and/or bladder dysfunction. Tools such as questionnaires and subjective assessments are integral to your assessment and provide measures for tracking success. Ultrasound is another tool commonly used to help gather information and make bowel and bladder dysfunction diagnoses in children.
This may seem obvious, but the orthopedic physical assessment you regularly perform as a pediatric therapist is another very useful tool used in determining sources of bowel and bladder dysfunction. You may be surprised to learn how frequently side-to-side discrepancies or overactive hip muscles play a role in bowel and bladder dysfunction. As with all diagnoses, determining the root of the problem will drive your treatment planning.
What Treatments Are Involved in Pediatric Pelvic Floor Therapy?
Pediatric pelvic floor therapy can be intimidating to therapists who have never treated PFD before. First, know that success can be achieved without any internal examination or treatment at all.
Pediatric pelvic floor therapy treatments may include bowel and bladder diaries, breath work, stretches, abdominal massage, behavioral modification, and exercises to achieve balance in trunk and lower extremity strength, length, and function. Parents are often encouraged to be involved in treatment techniques as they’re with their children a majority of the time.

Where Do Pediatric Patients with Pelvic Floor Dysfunction Currently Receive Care?
You may be wondering, “If pediatric bowel and bladder issues are so common, who is treating all these patients?” This is a great question, and the answer will likely disappoint you.
Since I started doing pediatric pelvic floor therapy over 30 years ago, I’ve met thousands of children from birth to 17 years old. I can’t count how many older children are referred to my clinic with issues they’ve had for as long as they can remember. PFD in children often goes untreated — this population is severely underserved.
Children suffer from embarrassment, isolation from peers, and decreased quality of life because of bowel and bladder dysfunction. Parents often don’t know where to go for help or what options exist, so the issues commonly persist into adulthood.
If a child is lucky enough to be referred to someone aware of pediatric pelvic floor therapy, this is the best first-line treatment. Oftentimes, however, parents and pediatricians alike are unaware of this option, and they never make it to our offices. Children may be treated by pediatricians with medication, or referred to specialists.
When is Medical Treatment Indicated over Pediatric Pelvic Floor Therapy?
It’s pretty mainstream to recommend physical or occupational therapy for children with fine or gross motor delays, but how often are pediatricians recommending therapy for bedwetting, incontinence, or constipation? Physicians are great gatekeepers and it’s your job as a therapist to partner with local pediatricians in your area so they know who you are and how you can help them, especially if you decide to add pediatric pelvic floor therapy as a service in your clinic.
Many children are unnecessarily referred to gastroenterology or urology for bowel and bladder issues that could be managed with pediatric pelvic floor therapy (and without the need for medication). I would argue that medications are often used more quickly than necessary, but that doesn’t mean they don’t have a place in the management of pediatric bowel and bladder dysfunction.

Laxatives are commonly recommended to treat constipation. There are also medications that can be prescribed for bedwetting and incontinence. Enemas are used for chronic constipation issues that either do not respond to initial treatment or are medically indicated for other reasons.
I almost always recommend trying dietary, behavioral, and physical interventions first. If a child is not responding well to these interventions after 30-60 days of treatment, medical intervention may be indicated. In my courses I go in depth about titrating medications and how you can assist families in finding the best overall treatment regimen for them in conjunction with their pediatrician.
How Can You Get Training for Pediatric Pelvic Floor Therapy?

You likely didn’t learn much of anything about pediatric pelvic floor therapy in school. Now that you know the basics about pediatric pelvic floor therapy and the dire need for more professionals trained in helping these patients, you’re likely wondering how you can dive in and help.
I offer live and online courses to train healthcare professionals interested in treating pediatric bowel and bladder disorders. Why not offer your patients more than the standard, “hopefully you’ll grow out of it”? Your patients and their families deserve the best care available, and if I were a betting person, I’d bet on you!
Click below to learn more about my online and live course offerings for pediatric pelvic floor therapy. Hope to see you there!
This blog originally was posted on August 9, 2022, by Dawn Sandalcidi at https://kidsbowelbladder.com/why-add-pediatric-pelvic-floor-therapy-to-your-treatment-arsenal/.
Pediatrics Level 1 - Bowel and Bladder Disorders - Syracuse, NY
Price: $625
Experience Level: Beginner
Contact Hours: 19.5
Description: This two day, in-person course includes pre-recorded learning followed by a live, in-person course taught by instructor Dawn Sandalicidi, PT. The pre-recorded learning must be viewed in Teachable before Day One of the course.
This course begins with instruction in anatomy, physiology, and in development of normal voiding reflexes and urinary control. The participant will learn terminology from the International Children's Continence Society, medical evaluation concepts for bowel and bladder dysfunction, and common dysfunctions in voiding and defecation. Common causes of incontinence in the pediatric patient will be covered, and a comprehensive approach to evaluation will be instructed including video examinations of the pelvic floor and surface electromyography (or sEMG, a form of biofeedback).
Pediatrics Level 1 - Bowel and Bladder Disorders
Price: $625
Experience Level: Beginner
Contact Hours: 19.5
Description: This two day, in-person course includes pre-recorded learning followed by a live, in-person course taught by instructor Dawn Sandalicidi, PT. The pre-recorded learning must be viewed in Teachable before Day One of the course.
This course begins with instruction in anatomy, physiology, and in development of normal voiding reflexes and urinary control. The participant will learn terminology from the International Children's Continence Society, medical evaluation concepts for bowel and bladder dysfunction, and common dysfunctions in voiding and defecation. Common causes of incontinence in the pediatric patient will be covered, and a comprehensive approach to evaluation will be instructed including video examinations of the pelvic floor and surface electromyography (or sEMG, a form of biofeedback).
Pediatrics Level 2 - Advanced Pediatric Bowel and Bladder Disorders
Price: $600
Experience Level: Intermediate
Contact Hours: 15
Description: This course will give you the confidence to treat any pediatric patient with bowel or bladder issues. Forget the days of a referral coming across your desk and thinking, “what in the world?”, then frantically searching the web for more information. This course gives you a lifetime of access to all things advanced pediatric pelvic floor, such as:
- In-depth rib cage assessment
- Next-level core evaluation and treatment techniques
- Updated DRA/pressure system exercise guidance
- Full-body movement analysis as it relates to the pelvic floor
- A deep dive into how specific disorders change a patient's movement and what to do about it
Emily McElrath, PT, DPT, MTC, CIDN is instructing her upcoming course Pregnancy & Postpartum Considerations For High Intensity Athletics scheduled on May 21, 2023. This one-day remote continuing education course is designed to educate practitioners on the unique considerations of pregnant and postpartum athletes engaging in high intensity interval training (HIIT).
Emily is a native of New Orleans and received her undergraduate degree in Athletic Training at the University of Southern Mississippi and went on to receive her Doctorate of Physical Therapy from the University of St. Augustine for Health Sciences. She is highly trained in Sports and Orthopedics and has a passion for helping women achieve optimal sports performance. Emily is certified in manual therapy and dry needling, which allows her to provide a wide range of treatment skills including joint and soft tissue mobilization. She is an avid runner and Cross-fitter and has personal experience modifying these activities during pregnancy and postpartum.
Introduction: Although routine exercise has long been recommended throughout pregnancy by medical professionals, High Intensity Athletics like Crossfit, weightlifting, and HIIT have received mixed approval amongst healthcare providers. There seems to be limited knowledge on how this form of exercise affects the pelvic floor and abdominal wall throughout pregnancy and postpartum, thus creating a limited understanding of proper recommendations by healthcare providers in regard to how and when a patient can safely continue and/or return to high intensity athletics during pregnancy and postpartum. Unfortunately, some (likely well-intended) medical professionals have gone so far as to instruct their patients to completely avoid these types of exercise throughout pregnancy. But are these limitations really necessary? Does the research support these recommendations? Or is there a way we can help these women continue to safely participate in high intensity athletics throughout pregnancy, and return appropriately in the postpartum phase?
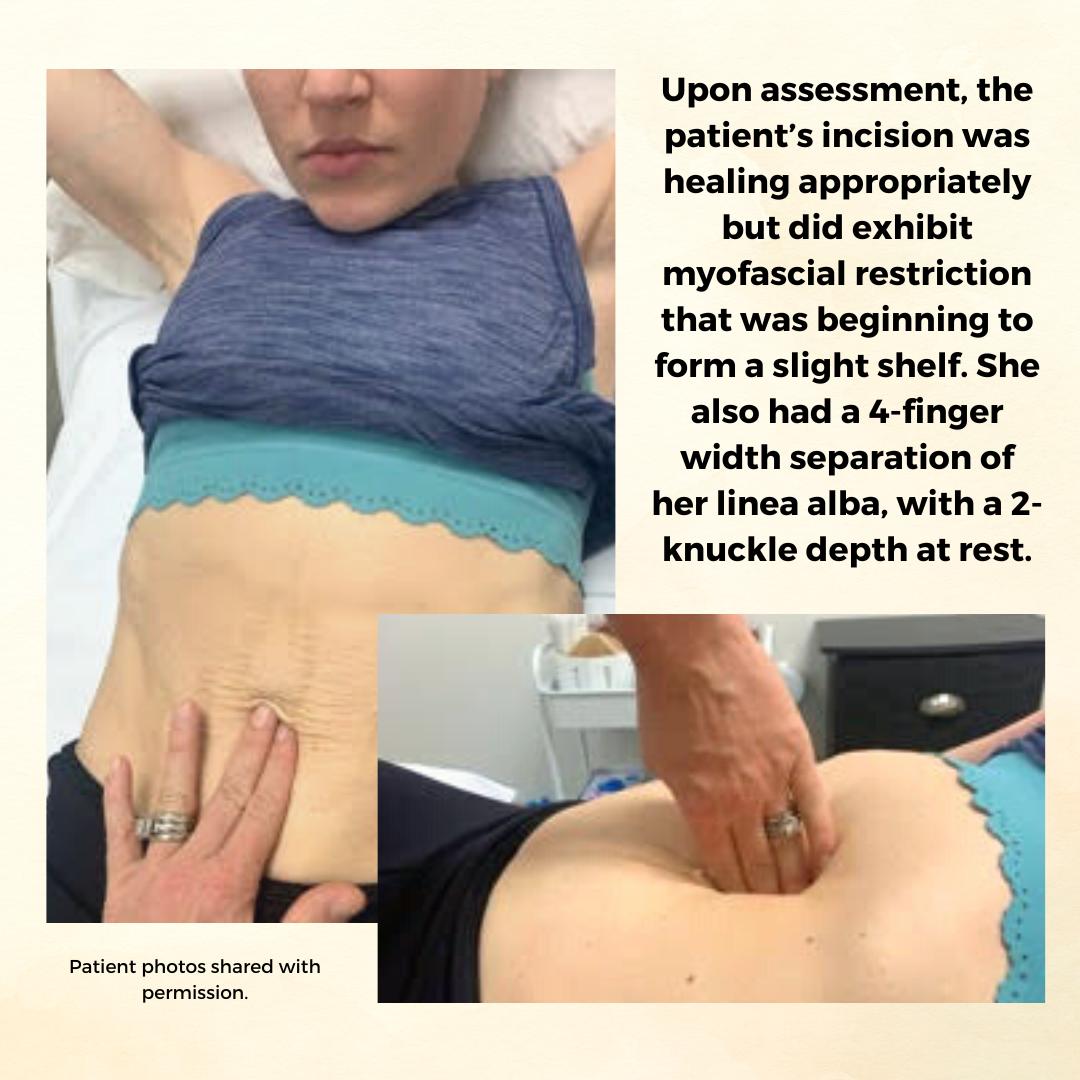
Background: The patient is a 34 y/o female who reported to the Physical Therapy clinic at 2 months postpartum from a cesarean delivery of twins. The patient was seen prior to her delivery (beginning at 24 weeks gestation) to prepare for a vaginal delivery, address chronic constipation, and to receive guidance on how to safely continue Crossfitting during pregnancy. She had been a Crossfitter (5-6 x weekly) for roughly 10 years at the time of her evaluation and was a track athlete and distance runner prior to that. Prior to pregnancy, the patient competed in local and regional Crossfit competitions in the RX division. The patient continued to Crossfit throughout her pregnancy and was able to avoid any pelvic floor dysfunction with proper modification and guidance. The patient returned for postpartum assessment at 8 weeks. At the time of the evaluation, she had begun taking short walks and performing body weight strengthening exercises. Her main concern at the time of the evaluation was a significant diastasis recti (DRA), and a self-reported decrease in core control and awareness. While the patient no longer desired to compete in local or regional competitions, she did want to continue Crossfit 5-6 x weekly and wanted to make sure she was able to safely do so with her DRA. Upon assessment, the patient’s incision was healing appropriately but did exhibit myofascial restriction that was beginning to form a slight shelf. She also had a 4-finger width separation of her linea alba, with a 2-knuckle depth at rest. Initially, the patient was unable to perform a proper transverse abdominus (TrA) contraction and was subsequently unable to create good tension across the gap. She also demonstrated compensatory recruitment of her obliques with attempts to perform a TrA contraction. The patient demonstrated mildly improved TrA recruitment in standing and following treatment, which consisted of myofascial release to her abdominal wall and incision, dry needling to her obliques, and internal trigger point release to her pfm. The pt exhibited limited pfm motor control at the time of her postpartum evaluation, and her PERF score was 2/6/5/2. The pt also exhibited myofascial restriction of her thoracolumbar fascia, proximal adductors, and B glutes. The pt continued to be seen for roughly 1 year following the delivery of her twins. In that time a variety of treatment strategies and techniques were used.
Methods: The methods used to treat this patient included education on proper pressure management strategies (including modification to breathing strategies during exercise), exercise scaling and modification, internal trigger point release to the pfm, followed by neuromuscular re-education once the normal resting tone of the pfm had returned, myofascial release to her abdominal wall and cesarean scar, dry needling, and education on a home exercise program (HEP). The pressure management strategies provided to the patient focused primarily on the various breathing patterns she could utilize to prevent breath holding, improve pelvic floor contraction, and reduce intra-abdominal pressure. The use of the Valsalva was not re-introduced until the patient had normal pfm motor control, exhibited proper tension across her DRA with no evidence of doming or conning, and only in limited circumstances (primarily when the weight was over 80% of her max for that movement). Pelvic floor motor control was assessed via internal palpation, in standing, and with a load (ie back squat and deadlift). Activity modification included modification of the speed of various movements, the load (weight) of various movements, the velocity of various movements (barbell cycling versus slow reps and strict gymnastics versus kipping), and the volume of various movements (number of repetitions or rounds/time of time of a metcon). If the patient’s tissues still could not handle the load with the above modifications, the movement was changed altogether (i.e. mountain climbers versus toe to bar). Measures used to indicate tissue tolerance to the load included: abdominal doming or coning, urinary incontinence, pelvic pain or heaviness, pulling or pain along her incision, and low back pain. If the patient experienced any of these symptoms, the movement was modified until she was able to complete the movement without symptoms. Additionally, the patient received internal trigger point release to the pfm, dry needling to the abdominal wall, glutes, proximal adductors, and lumbar paraspinals, myofascial release to the same muscle groups, neuromuscular re-education, and kinesiotaping to the abdominal wall.
Results: At the time of her discharge, the patient was able to fully return to all desired Crossfit activity. This process took roughly 1 year and required a gradual loading of her tissues through activity modification, to allow them to properly manage the load placed on them. For her, gymnastics movements on the rig took the longest to return to. She did not fully return to these movements (pull-ups, toes to bar, chest to bar pull-ups, and muscle-ups) until roughly 8-9 months postpartum. At the time of her discharge, she was able to create good tension across the gap and had improved her DRA to only less than 1 finger width separation and less than 1 knuckle of depth at rest. When performing a TrA contraction, there was no depth or width of separation. The pt also had an improved PERF score of 5/10+/10/8. The pt exhibited normal pfm motor control and excellent pressure management at the time of discharge.
Conclusion: While there is not a large amount of research available on the effects of high intensity athletics on the function of the pelvic floor and abdominal wall, we are beginning to see an increase in research on new, and more functional approaches to evaluating and treating Diastasis recti (DRA). There has also been a recent increase in research looking at the effects of various breathing techniques during exercise (including the Valsalva) and how it affects both the mother and the baby. Consistent review of the most current research, a thorough understanding of the mother’s anatomy and how it changes during pregnancy and postpartum, as well as each patient’s unique history and goals is necessary for clinicians to provide the highest quality of care for each patient. This is how we can move away from blanketed natal and postnatal exercise recommendations, and develop patient centered, sport-specific treatment plans that will allow each patient safely and effectively participate in high intensity athletics.
Pregnancy & Postpartum Considerations For High Intensity Athletics

Price: $225.00 Experience Level: Beginner Contact Hours: 8.25 hours
Course Dates: May 21, September 10, and November 19
Description: This one-day remote course is designed to educate practitioners on the unique considerations of pregnant and postpartum athletes engaging in high intensity interval training (HIIT). In this cours participants will review the current literature, discuss the unique needs of pregnant and postpartum high intensity athletes, and learn how to most effectively treat these patients as practitioners. The main focus of this course will be to learn how exercising throughout pregnancy, or returning to exercise postpartum may look different for a high intensity athlete versus a non HIIT athlete.
Participants will discuss how anatomical and hormonal changes will affect training for the pregnant and postpartum athlete, and review various modifications for this population. We will also discuss how various stresses placed on the body during these activities may affect pelvic floor muscle function, and review various pressure management strategies that can be utilized during high intensity interval training. The lab will be broken up into pregnancy considerations and postpartum considerations. During the pregnancy lab, we will review specific exercise modifications for pregnancy, utilization of breathwork to properly support the pelvic floor during pregnancy, and review how to assess for and tape for diastasis recti. In the postpartum lab we will review how to determine proper activity modification based on ability to manage pressure, review specific activity modifications and breathwork, review accessory work for return to activity, and discuss how to assess pelvic organ prolapse in standing.

Rivki Chudnoff, MSPT is instructing her new course, Cultural Sensitivity: Treating Conservative Religious Patients, which debuts on May 7, 2023. Save 10% off registration with discount code NEWCOURSE10. We look forward to seeing you in class! This course is designed to provide guidance and skills for engaging patients from religiously conservative backgrounds in a culturally sensitive manner and will gain a foundational understanding of the various traditions, customs, laws, and values associated with Muslim, Jewish, Hindu, and Christian faiths as they pertain to sexuality and pelvic health.
CASE STUDY: Sarah is a 23-year-old woman who presents to your office for an evaluation. Upon scheduling, she did not wish to disclose to your office manager what kind of pelvic health issue she wants to be seen for.
Upon patient interview, Sarah reveals that she has been married for 8 months and all attempts at intercourse have been unbearably painful. She reports a 14/10 on a pain scale and that she has vocally cried out in pain with any attempts at penetration. She is feeling hopeless that this will ever get better, and is concerned that something is wrong with her and that her vagina is “too small” for intercourse. Sarah admits that she has never examined her own vaginal opening or seen it in a mirror because it “grosses her out”.
Sarah is otherwise in good health but has never had a gynecological exam. She and her husband are both from a conservative religious background and were educated in religious schools with limited sex education, and were provided with little information about sex prior to marriage. Neither of them had been sexually active prior to marriage. Sarah currently ascribes to her religious beliefs and practice which prohibits any conversations about sex with anyone other than her partner. She expresses an aversion to sexual activity and to her husband’s genitalia and semen. Sarah confides that she feels guilty that she is not able to have intercourse and “make her husband happy”.
Although she denies any discomfort with sitting or wearing tight-fitted garments and has no other pain in her body, recently she has started to have pain in her vulvar area that starts before attempting intercourse. After attempts at penetration, she has difficulty falling asleep due to her pain.
She has a self-diagnosed “tiny bladder” and frequently has to urinate every hour. Sarah reports a long history of constipation, with bowel movements about once a week with straining (type 1-2 on the Bristol stool scale)
She reports regular periods, but excruciating pain the first 2-3 days that can be debilitating at times. She has never successfully inserted a tampon.
Sarah’s personal goals for treatment are:
- To have intercourse without pain
- To become pregnant as soon as possible, as is expected in her social circles and close-knit community
What other questions would you like to ask this patient?
What is your next move?
What would your treatment plan look like for this patient?
What other healthcare providers might you refer her to?
Cultural Sensitivity: Treating Conservative Religious Patients has the following goals:
- Demonstrate a foundational understanding of the various traditions, customs, laws, and values associated with Christian, Hindu, Jewish and Muslim faiths.
- Identify potential challenges and barriers to care unique to pelvic health patients from conservative religious backgrounds.
- Describe five strategies for increasing comfort and confidence in interfacing with patients from different religious backgrounds.
- Apply cultural sensitivity to patient interviewing and education techniques.
- Discuss collaborative approaches to evaluation and treatment that are compliant with the patient’s religious and cultural norms.
- Evaluate culturally sensitive intervention in a case study format with your peers.
As pelvic health providers, we go into this special field with the desire to provide the best care for our patients in the most sensitive way possible. It can be particularly daunting when we encounter patients from religious backgrounds and cultures that are unfamiliar to us. In our attempts to be sensitive, we may be tempted to shy away from asking patients the questions that really need to be asked. We may avoid providing patient education we may have otherwise provided because we don’t want to offend, or may tiptoe around a treatment session where we may have otherwise taken a more confident approach. My hope is that practitioners will leave my course, Cultural Sensitivity: Treating Conservative Religious Patients, confident in their abilities to provide the highest level of care with confidence, sensitivity, and compassion for all of their patients.
Who are you? Describe your clinical practice.
I’m a mom of a bunch of adolescent kids and a dog. I drive a minivan with the sunroof open blasting Bon Jovi, Janet Jackson, Madonna, and Lizzo down the New Jersey Turnpike with a trunk full of mall returns and reusable shopping bags like a wild woman. Fun fact - I’m married to a gynecologist (no it’s not weird, and no, he’s not my gynecologist, because that would actually be weird).
My secret identity is as a pelvic health physical therapist at my private practice in Bogota, NJ where I hide from said teenagers.
I have been privileged to be involved in the field of pelvic health for the last two decades, both treating patients with a wide variety of pelvic health issues as well as providing community outreach and developing educational initiatives.
I have been joyfully teaching the pelvic floor series at Herman & Wallace for the last several years both in person and in the remote format. This is my maiden voyage teaching my own course for the Institute. I’m working on the accompanying soundtrack for the course and am taking requests.
What made you want to create this course?
At one of the first H&W courses I attended as a participant, I noticed it was a combination of women of different faiths (myself, an Orthodox Jew included) that were all treating each other behind the modesty curtains during lab. I remember thinking, “Cool, it’s like a pelvic health United Nations going on back here”.
I realized I was not alone. Individuals from a myriad of different backgrounds have challenges navigating the intersection of their religious world, its culture of modesty and conservative religious values, and the world of pelvic and sexual health. The very rules, spoken and unspoken that govern religious cultures and are innate to its members, can be mysterious and even surprising to people from more secular backgrounds. My hope is for this course to be the bridge between the two worlds, to be traveled comfortably by all those who wish to partake in the journey.
What need does your course fill in the field of pelvic rehabilitation?
Having expert clinical, diagnostic, and treatment skills are essential components of providing effective treatment. However, seasoned clinicians know these skills will only get their patients halfway there. My course, Cultural Sensitivity: Treating Conservative Religious Patients, falls under the other half of care: bedside manner, and building a therapeutic alliance. The focus of this course is the way we frame the care we are providing, and the way we interact with the human element within ourselves and within our patients that is more than muscles, nerves, joints, ligaments, and fascia.
Who, what demographic, would benefit from your course?
Anyone who treats patients with pelvic health concerns will leave this course with something they can incorporate into their practice. As pelvic health providers, we go into this special field with the desire to provide the best care for our patients in the most sensitive way possible. The problem is, we don’t always know what that is supposed to look like. It can be particularly daunting when we encounter patients from religious backgrounds and cultures that are unfamiliar to us. Most of us did not learn this in school. In our attempts to be sensitive, we may be tempted to shy away from asking patients the questions that really need to be asked. We may avoid providing patient education we may have otherwise provided because we don’t want to offend, or may tiptoe around a treatment session where we may have otherwise taken a more confident approach. My hope is that practitioners will leave this course confident in their abilities to provide the highest level of care with confidence, sensitivity, and compassion for all of their patients.
Cultural Sensitivity: Treating Conservative Religious Patients

Course Date: May 7th - Save 10% off registration with discount code NEWCOURSE10
Experience Level: Beginner
Contact Hours: 9.75 hours
Description: This course is designed to provide guidance and skills for engaging patients from religiously conservative backgrounds in a culturally sensitive manner. Participants will gain a foundational understanding of the various traditions, customs, laws, and values associated with Muslim, Jewish, Hindu, and Christian faiths as they pertain to sexuality and pelvic health.