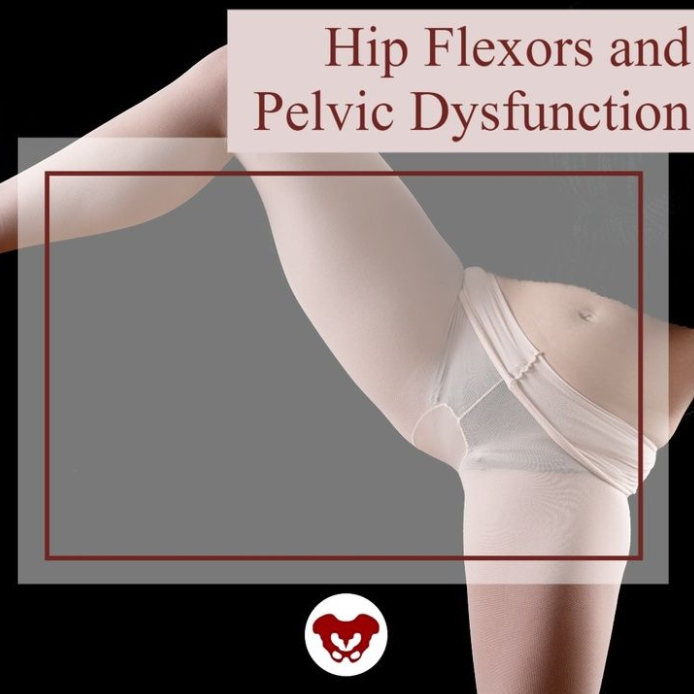
The hip flexor muscles include the Iliopsoas group (Psoas Major, Psoas Minor, and Iliacus), Rectus Femoris, Pectineus, Gracillis, Tensor Fascia Latae, and Sartorius. When the hip flexors are tight it can cause tension on the pelvic floor. This can pull on the lower back and pelvis as well as change the orientation of the hip socket, lead to knee pain, foot pain, bladder leakage, prolapse, and so much more. The ramifications of iliacus and iliopsoas dysfunctions are discussed in Ramona Horton's visceral course series:
- Mobilization of the Visceral Fascia: The Gastrointestinal System
- Mobilization of the Visceral Fascia - The Urinary System
- Mobilization of the Visceral Fascia - The Reproductive System
You can also learn about this in a contemporary and evidence-based model with Steve Dischiavi in his Sacroiliac Joint Current Concepts and Athletes & Pelvic Rehabilitation remote courses.
A common issue with the iliacus and hip flexors is that they can shorten over time due to a lack of stretching or a sedentary lifestyle. When this happens, the muscle adapts by becoming short, dense, and inflexible and can have trouble returning to its previous resting length. A muscle that resides in this chronic contraction can become ischemic, develop trigger points, and distort movement in the body.
If you are treating patients with pain in their lower abdomen, sacroiliac joint, or that wraps around the lower back and buttocks, it could be because the hip flexors are tight. Traditional testing performed by medical practitioners tends to come back negative as many tests do not evaluate soft tissue issues. The best way to diagnose these concerns is through assessment with skilled palpation and structural evaluation.
One assessment test used for the iliopsoas is discussed in the Athletes & Pelvic Rehabilitation course. This is the Thomas Test which measures the flexibility of the hip flexors. In this test, the patient is supine while flexing the unaffected, contralateral leg at the hip until lumbar lordosis disappears. The length of the iliopsoas is determined by the angle of hip flexion displayed by the patient. The test is positive when the patient is unable to keep their lower back and sacrum against the table, the hip has a posterior tilt (or hip extension) greater than 15°, or the knee is unable to meet more than 80° flexion. A positive test indicates a decrease in flexibility iliopsoas muscles.
Treatment plans for the iliacus and hip flexors include stretching. An example includes the hip extension stretch or other active isolated stretches. Manual therapy, including trigger point release, can be used in conjunction with stretching to help muscle adhesion and release muscle tension. As with all treatment, the practitioner should discuss the risks, benefits, and treatment options, and obtain consent with patients. Prior to proceeding with manual therapy treatment make sure to establish a pain scale, assess the patient's range of motion and strength, and (if needed) perform the appropriate neurologic testing.
To learn more about manual therapy options for the visceral fascia, join Ramon Horton in her Mobilization of the Visceral Fascia Satellite Lab Course Series (multiple satellite locations available):
- Mobilization of the Visceral Fascia: The Gastrointestinal System - October 15-17, 2021
- Mobilization of the Visceral Fascia: The Urinary System- September 17-19, 2021
- Mobilization of the Visceral Fascia: The Reproductive System - October 1-3, 2021
To learn more about treatment philosophies for the pelvis and pelvic floor and global considerations of how these structures contribute to human movement you can join Steve Dischiavi:
- Athletes & Pelvic Rehabilitation Remote Course - September 18-19, 2021
- Sacroiliac Joint Current Concepts Remote Course - August 21, 2021
The world needs more clinicians who can treat pelvic pain, pelvic organ prolapse, urinary incontinence, diastasis recti, and the many other conditions that constitute pelvic floor/pelvic girdle dysfunction. Most clinicians who specialize in pelvic rehabilitation are Physical Therapists (PT) or Occupational Therapists (OT), though other licenses also allow you to work with patients who have pelvic floor dysfunction. Many doctors, nurses, and internationally licensed medical professionals are beginning to explore the field of pelvic rehabilitation.
In an interview for the Pelvic Rehab Report, faculty and instructor Tiffany Ellsworth Lee MA, OTR, BCB-PMD, PRPC, shared that "Occupational therapists wishing to pursue pelvic floor have a few options. The first thing is to find a pelvic floor clinical setting...or check to see if they can start a women's health program with a strong focus on the pelvic floor. OTs quite often do not start out in pelvic health directly after school. Since this is a newer area as compared to other certifications such as the NDT and PNF, it takes a little bit of research, time, and effort to find one’s exact niche. To get started, an OT should seek out courses that teach the basics of bladder and bowel management. It is important to understand the anatomy and physiology of the bladder, bowel, and sexual systems."
Once you have a license to practice, you can start learning to specialize in pelvic rehabilitation. The best place to start is with the H&W Pelvic Floor Level 1 satellite lab course, which offers immediately applicable clinical skills for evaluating and treating urinary incontinence or the musculoskeletal components of urogynecologic pain syndromes. Most practitioners who take Pelvic Floor 1 return to study in the next courses in the series.
You can learn all about the colorectal system, and how to treat conditions such as coccyx pain, pudendal neuralgia, and male pelvic pain in the Pelvic Floor 2A course, and in Pelvic Floor 2B you can expand your knowledge in topics such as movement assessment and re-training, prolapse, and pelvic pain. Then in the Pelvic Floor Capstone course, the final advanced course, you dive deep into topics such as hormones and their influence on conditions, surgeries and recovery, and skilled manual therapy techniques. Once you know your patient demographic, you can check out our growing list of specialty courses that include series topics including yoga, oncology, pregnancy, fascial mobilization, and much more.
Once you have gained experience in the field, you may consider sitting for the Pelvic Rehabilitation Practitioner Certification (PRPC). This certification recognizes expertise in pelvic rehabilitation for patients of all genders throughout the lifecycle. To be eligible to sit for the exam, applicants must have completed 2000 licensed hours of direct pelvic patient care in the past eight years, 500 of which must have been in the last two years.
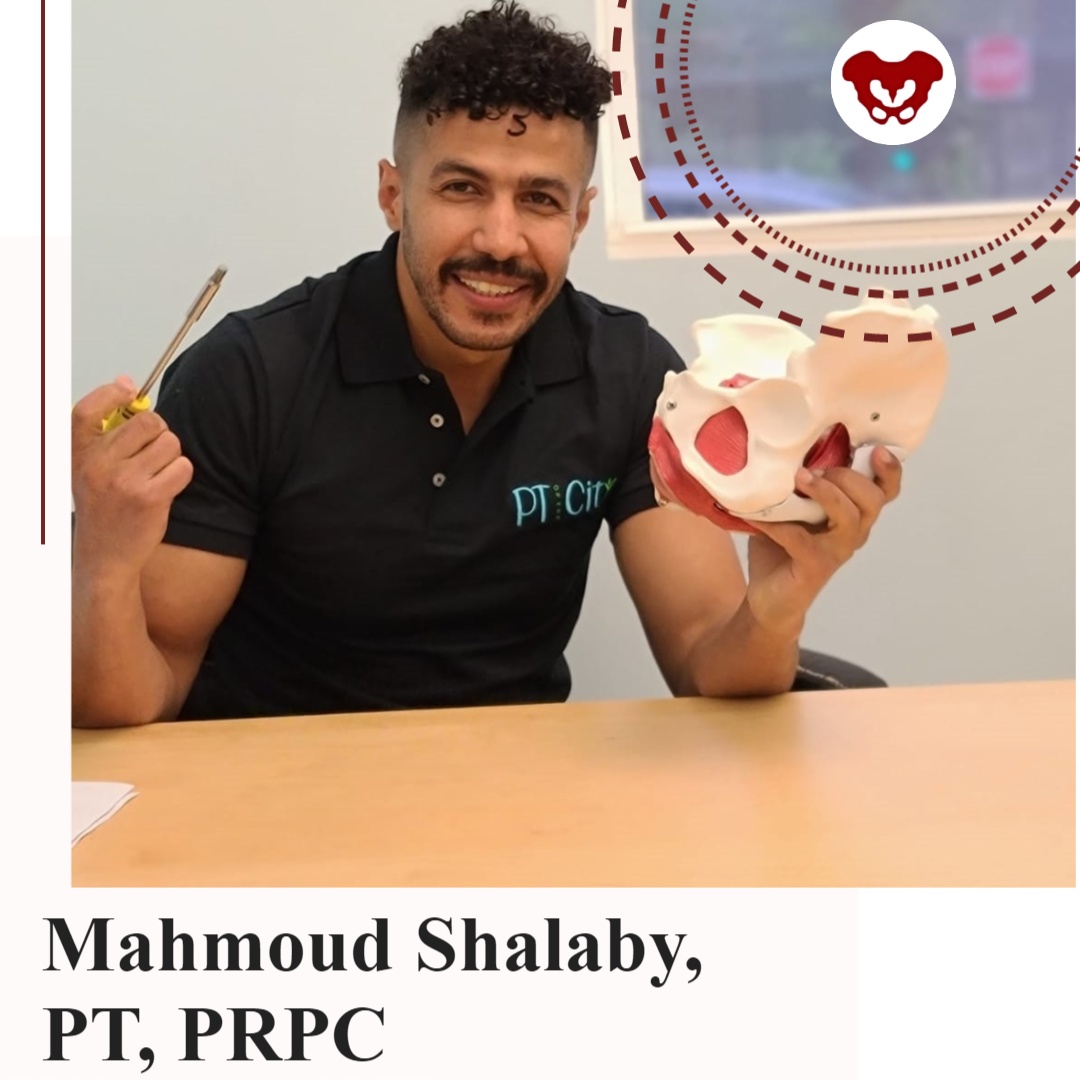
The following is our interview with Mahmoud Shalaby, PT, MS, DPT, PRPC. Mahmoud recently passed the Pelvic Rehabilitation Practitioner Certification (PRPC) exam. He practices at PT of The City in Brooklyn, NY, and is a Teaching Assistant for local New York satellite courses with H&W. Mahmoud was kind enough to share some thoughts about his career with us. Thank you, Mahmoud - and congratulations on receiving your PRPC!
In 2016, I was offered the chance to shadow a senior PT who specialized in pelvic rehab. This specialty was mysterious for me. I didn't think that there was much we could offer to patients with pelvic issues like incontinence, prolapse, IC, and such until I started to treat them. Once I commenced learning more, it never ends.
There is always more to discover and I've always been impressed with the role of physical therapists in assessing and treating pelvic issues. I continue to be very excited to learn more and to develop my experience while further participating in studies to improve my skills and tools in improving people's quality of life.
Herman & Wallace institute has always been my partner in success, they knew how to get me on the track and impressively integrate all resources across body systems to make me confident and skillful to help patients.
When I`ve attended the courses at Herman & Wallace, I have looked at their great Pelvic Rehab certification and immediately I`ve decided to become a certified pelvic rehab specialist for many reasons. To begin with, we must keep high standards to provide such a specific skilled service, in addition to improving my skills, knowledge, and quality to help patients. There are a lot of people suffering from those issues, they either do not know how to address those issues or they do not know where to go.
In particular cultures and religions, the gender of the doctor matters, especially when it comes to sensitive topics, and I am proud to be among the two or three male certified pelvic rehab specialists across the country and I am always happy to get the patients comfortable and confident to be able to address their issues and help them reach their goals.
Working as a teaching assistant at Herman & Wallace is a great opportunity to learn more and explore how newbie therapists think, and help them to see the great skills and tools at this specialty.
As pelvic rehab specialists, we have a great responsibility to raise awareness and educate the community and let them know that we are here for them.
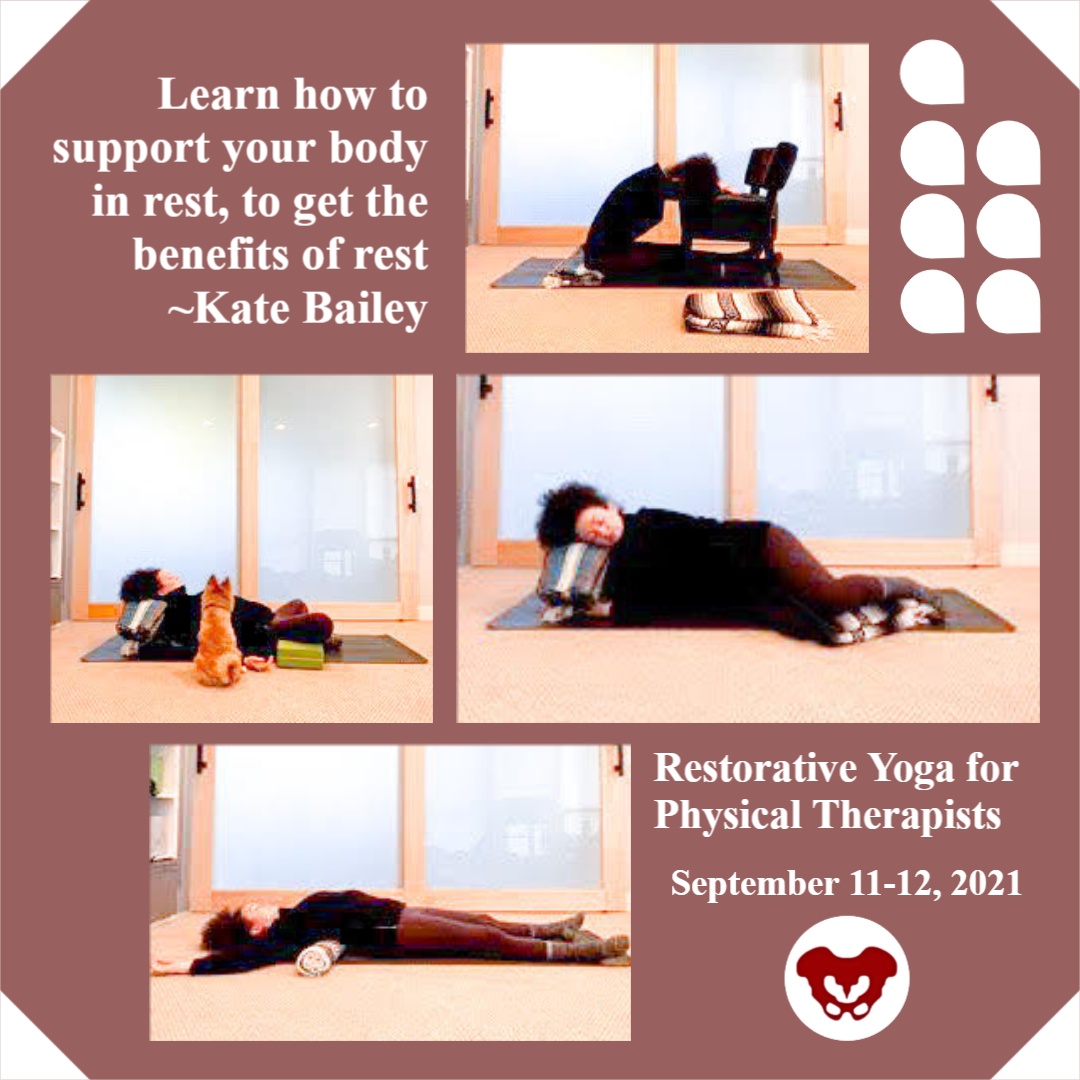
Kate Bailey, PT, DPT, MS, E-RYT 500, YACEP, Y4C, CPI curated and instructs the remote course on Restorative Yoga for Physical Therapists, which is scheduled for September 11-12, 2021. Kate brings over 15 years of teaching movement experience to her physical therapy practice with specialties in Pilates and yoga with a focus on alignment and embodiment. Kate’s pilates background was unusual as it followed a multi-lineage price apprenticeship model that included the study of complementary movement methodologies such as the Franklin Method, Feldenkrais, and Gyrotonics®. Building on her Pilates teaching experience, Kate began an in-depth study of yoga, training with renown teachers of the vinyasa and Iyengar traditions. She held a private practice teaching movement prior to transitioning into physical therapy and relocating to Seattle.
Without a doubt, these past couple of years have been tough with this global pandemic of a virus that caused major shifts in how we work, play, learn and socialize. Wherever you live on this planet, it is nearly impossible not to have been affected by the stress and trauma that the Covid-19 virus has created. Just like with any other stressor, the first step of management is recognition. Check, done.
Step two involves making conscious choices about how we want to live. This is where we have some options, including self-care. “Self-care” is one of my least favorite phrases. Not because at its core, self-care is not important. But because it's another thing on an overflowing to-do list and can create even more of a sense of imbalance, lack of accomplishment, and self-defeat. Yet, learning how to manage stress is a skill we all need: individually and communally.
However, there is a step before stress management that we need to address first. Interoception, defined by Porges, Ph.D., is the process that describes both conscious feelings and unconscious monitoring of bodily processes by the nervous system. As a clinician, this is a key aspect of every single patient care plan. I am a big fan of embodied decision making, and yet our somatic intelligence (or interoceptive skills) is widely underdeveloped.
Just as emotional intelligence is getting some wonderful development, through the work of researchers and educators like Marc Brackett, Ph.D. of Yale Center for Emotional Intelligence, our wellbeing and access to wellness are dependent on our ability to understand the sensations and signals throughout our body and then make a choice. This is important since you can’t make an embodied choice (step 2) before you have the data (step 1 - interoception). An example would be to imagine if you never felt the sensation of hunger, or the ‘hangry’ feeling when it’s been too long since the last boost of nourishment…how would you determine that you are hungry?
So, what to do? Many of us (clinicians and patients alike) live in a world full of overstimulation, productivity requirements, and constant stress. To develop interoception, finding little periods of stillness can be really useful. In yoga, there is a dedicated practice called pratyahara. Translated from Sanskrit to English as ‘withdrawal of the senses.’ The senses, in this case, includes all the sense organs: sight, smell, sound, touch, taste, movement (vestibular), and spatial placement (proprioception). Traditionally this is an aspect of meditation.
In my experience as a yoga teacher and physical therapist, I find this practice more accessible in the restorative yoga practice. It can take some graded exposure, but at the heart of the restorative yoga practice is stillness, darkness, silence, and support from props so that the body doesn’t have to do anything. These are also the essential components described by Herbert Benson, MD in his work on the Relaxation Response. In his work, he showed the relaxation response to be effective in decreasing heart and respiration rate triggering the benefits of the vagal nerve; which we are learning has so much to do with our ability to neuroregulate and participate in individual and communal stress management.
Restorative yoga is a practice of wakefully resting. Immordino-Yang et al, studied the brain in functional MRI when individuals were wakefully resting. The study found that during wakeful rest (without a meditative component where the brain has a task of concentration) the brain goes into a mode of neural processing called default mode. In default mode, the brain supports memory recall, imagining the future, and developing socio-emotional intelligence. In relationship to stress management, this is so important because it re-centers us, and allows for connection for even more neuroregulation.
For my patients, I often joke about lying on the floor. Really, it is not a joke at all. Lying on the floor for 15 minutes is savasana. Savasana is a wakeful resting and a practice of relaxation response. It seems easy: you always have access to a floor. You don’t need anything fancy. Aside from the neuroregulatory benefits of rest, savasana also gives the postural muscles a break. It allows the hip flexors to re-lengthen and the cervicothoracic junction to realign.
It is pretty great, and really accessible for most people. For those who are not comfortable flat, that’s where the props used in restorative yoga come into play. As physical and occupational therapists, we are so well primed to help people learn how to support their bodies in rest to get the benefits of rest.
Burnout, the Secret to unlocking the stress cycle by Emily Nagoski, Ph.D. and Amelia Nagoski, DMA
Polyvagal Theory, Stephen W Porges, PhD
Immordino-Yang et al. - Perspectives on Psychological Science - 2012
The Relaxation Response by Herbert Benson, MD, and Miriam Z Klipper

Mia Fine, MS, LMFT, CST, CIIP is the author and instructor of the Sexual Interviewing for Pelvic Health Therapists remote course scheduled for August 14-15, 2021. Mia’s specialties are sexual health concerns, eroticism, intimacy, alternative sex and relationships (kink/BDSM and non-monogamy), LGBTQIA+ genders/orientations/sexualities, and desire discrepancy. Her course Sexual Interviewing for Pelvic Health Therapists is intended for pelvic rehab therapists who want to learn tools and strategies from a sex therapist’s toolkit. Mia shares the following blog detailing some of the books that have influenced her.
As a science, psychology, somatics, and sexuality education nerd, books are my go-to psychoeducation sources. The books listed below are resources that I offer to my clients, send to family and friends for birthdays and holidays, and inform the work I do as a clinical supervisor, professor, and therapist. I’m excited to share some of my favorites that might help you and the patients with whom you work.
A prerequisite for anyone with a vulva (or who is partnered with someone with a vulva) is the book Come As You Are written by Emily Nagoski. Before a therapeutic intake session, I invite my clients who have vulvas to read this book. It is important to me that my clients and I share the same language that is offered in this fabulous resource. Nagoski illustrates the Dual Control Model for sexual arousal, interest, and desire in ways that are accessible and digestible for all. When clients understand the difference between Spontaneous Arousal and Responsive Arousal, and why these happen, and when, it is a game-changer for them and their partner. This book is a must for anyone who works with pelvic floor pain. And excitingly, these topics will be covered in my upcoming Herman & Wallace course!
The Politics of Trauma written by Staci Haines (also the author of Healing Sex) is a deep dive into, well, the politics of trauma. In this book, she explores the somatic experiences we humans have when we are activated. Her detailed description of fight, flight, freeze, fawn, and dissociate is nothing short of brilliant. This book is a must for those who are interested in exploring the impact that social justice, racial justice, transformative justice, and restorative justice have on our lived experiences of trauma.
The Body is Not An Apology is another brilliant book by Sonya Renee Taylor. It highlights the many effects of the “isms and obias” (such as Sexism, Racism, Fat-phobia, Transphobia) embedded in our everyday life and how identifying these frees us of the barriers they place on our quality of life. The isms and obias she explores impact the way we view ourselves, talk to ourselves, and relate to others. This book is incredibly inspiring, as is the author, Sonya Renee Taylor.
Additional books I love, many of which are written by close friends and colleagues include:
- Trans Sex by Lucie Fielding
- Wild Side Sex: the Book of Kink by Midori
- Gender Trauma by Alex Iantaffi
- Polyvagal Exercises for Safety and Connection by Deb Dana
- Becoming Cliterate by Laurie Mintz
- Better Sex Through Mindfulness by Lori A. Brotto
- The Art of Giving and Receiving: The Wheel of Consentby Betty Martin, Robyn Dalzen
These books have improved, and informed, my therapeutic work with clients and are recommendations I offer on a weekly, if not daily, basis. For additional resources, check out my website:https://miafinetherapy.com/. I look forward to exploring more comprehensive and accessible resources with you at my upcoming course Sexual Interviewing for Pelvic Health Therapists remote course scheduled for August 14-15, 2021!
The majority of practitioners begin their pelvic rehabilitation journey by taking Pelvic Floor Level 1, which is an excellent starting point. This course provides the basics of anatomy, techniques, and knowledge needed to start treating patients.
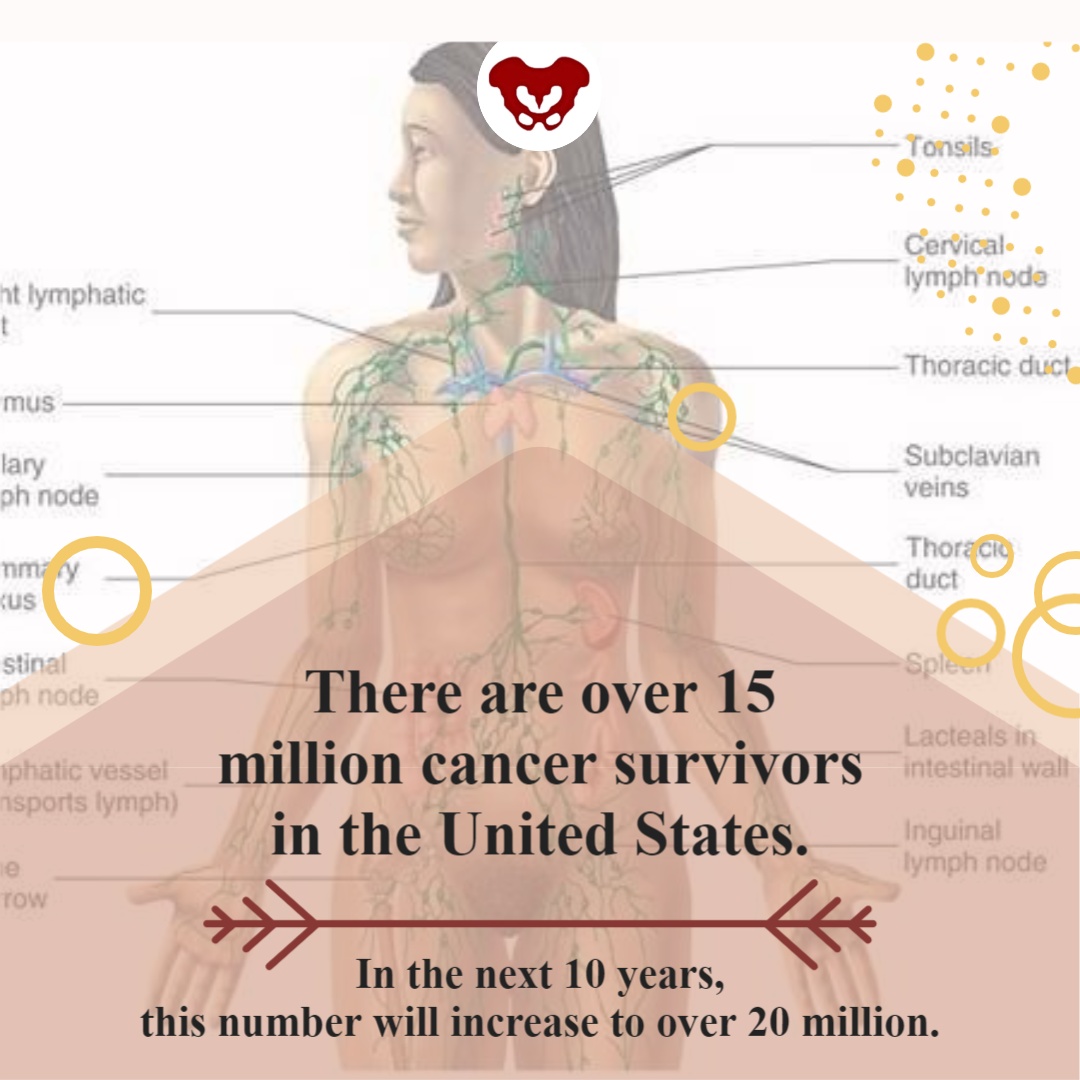
Another option for your pelvic floor journey is the Oncology of the Pelvic Floor Level 1 remote course. Caring for patients with cancer begins at diagnosis, and as a pelvic rehabilitation practitioner, you are an integral part of the oncology team. This course addresses the issues commonly seen in a patient who has been diagnosed with cancer.
Several cancers can affect the pelvic region and pelvic floor. Such cancers include bladder, colorectal, prostate, and ovarian cancers. Treatments for pelvic cancers include surgery, radiation therapy, hormone therapy, chemotherapy, and pelvic rehabilitation. These treatment options depend on the tumor size, location, or stage and negatively affect pelvic floor function and quality of life.
Cancer patients also often have intimacy issues that stem from their diagnosis and treatment. Holly Tanner shares that "...cancer treatment can change relational roles, finances, work-life, independence, and other factors including hormone levels. Exhaustion (on the part of the patient and the caregiver), role changes, changes in libido, and performance anxiety can create further challenges." A pelvic rehabilitation practitioner can assist the patient in their recovery and reframing of intimacy.
In addition to sexual function, the pelvic floor helps to maintain bladder/bowel control (emptying, urges), organ support, and stabilization of the spine/pelvis. Pelvic issues that originate from cancer treatment vary from scar tissue restriction or swelling, fibrosis causing narrowing and hardening of tissues, sexual issues, and lymphedema, among other issues. While some patients may not display symptoms at all, others can develop issues immediately after treatment, or even months after treatment has ended.
There are over 15 million cancer survivors in the United States. In the next 10 years, this number will increase to over 20 million. The need for trained practitioners to treat patients with cancer diagnoses will only be increasing in the future. Join H&W on August 15-16 in Oncology of the Pelvic Floor Level 1 and learn to be part of an interdisciplinary oncology team.
How do healthcare practitioners improve patient satisfaction? Patient satisfaction is a cognitive evaluation of an emotional reaction to their health-care experience. According to multiple studies, the most significant predictor of patient satisfaction is the quality of their conversations with their medical practitioners.
Patients care about:
- Being listened to
- Being treated courteously and respectfully
- Being involved in decisions about their healthcare
- Receiving clear explanations about their medical status and treatment
This is good news because they are all factors that you can control. Practitioners who take the time to communicate clearly, listen intently, understand each patient as an individual, and respond compassionately can improve their patients’ satisfaction and treatment outcomes. As Lauren Mansell stated in an interview with H&W, you have to “know what questions to ask patients for treatment. Our patients often feel alone, are frustrated with medical treatments, and feel like no one can address their symptoms.”
When patients are facing a difficult or new medical situation, they are in a threat state. This means that emotions get triggered, the limbic system gets activated, and the prefrontal cortex starts to deactivate. This results in patients who are not thinking clearly, listening well, or who appreciate a different mindset.
Herman & Wallace offers courses on treating the pelvic floor, and also the whole patient. Strengthen your clinical interactions with one of their courses:
- Sexual Interviewing for Pelvic Health Therapists – with Mia Fine, MS, LMFT, CST, CIIP
- Trauma Awareness for the Pelvic Therapist – with Lauren Mansell DPT, CLT, PRPC
- Inclusive Care for Gender and Sexual Minorities – with Brianna Durand, PT, DPT
One of the most important things that a practitioner can learn is to never assume that you know how your patient feels or identifies. No two people are the same. Faculty member, Brianna Durand shares that “Ultimately, the best method to providing compassionate and competent care is to minimize your assumptions.” Brianna shares this example in a recent interview, “if you find yourself assuming someone’s gender identity based on their name or appearance, I’d challenge you to practice using the gender-neutral they/them pronoun until you learn how they identify. If you are unsure, it is okay to privately ask them!”
Faculty member, Mia Fine further stresses that “It is important that providers be aware of their own biases and be introduced to the various sexual health resources available to providers and patients.” Listen to your patient to understand what they are saying and feeling. Do not respond defensively. Remember that this can feel like a threatening situation for patients.
Happy patients are more likely to return to your practice in the future, recommend your practice to their friends, and pay their bills on time and in full. Patients want to have quality interactions with a healthcare provider who cares about them. As a practitioner, your satisfied patient is more likely to make follow-up appointments and maintain their prescribed treatment plan, which can lead to more positive outcomes.

The following is our interview with Jennifer Eller, PT, DPT, PRPC. Jenni recently passed the Pelvic Rehabilitation Practitioner Certification (PRPC) exam. She practices at Enloe Medical Center in Chico, CA and is a Teaching Assistant for local California satellite courses with H&W. Jenni was kind enough to share some thoughts about her career with us. Thank you, Jenni - and congratulations on receiving your PRPC!
Q: Who are you? Describe your clinical practice.
A: My name is Jenni Eller, and I am a pelvic floor physical therapist at Enloe Rehabilitation Center (hospital-based outpatient clinic) in Chico, CA. I specialize in pelvic floor, orthopedic, and oncological diagnoses. Specifically, conditions related to incontinence, pelvic pain, dyspareunia, vaginismus, interstitial cystitis, and the post-surgical pelvis, as well as pelvic floor issues, post-oncological treatment pelvic floor issues, pre and postnatal issues, male pelvic floor dysfunction, and other pelvic floor dysfunctions.
Q: How did you get involved in the pelvic rehabilitation field, and what has your educational journey as a pelvic rehab therapist looked like?
A: I grew up in Oregon and Washington, and completed my undergraduate degree in Exercise Science at Linfield College in 2009. I completed my Doctorate Degree in Physical Therapy at Regis University in Denver, CO in 2013.
After graduate school, I worked in a small rehabilitation hospital but quickly transitioned to outpatient rehabilitation and started working with the orthopedic and oncological patient population. The hospital system I was in had hired 3 new gynecology oncologists and were interested in developing the pelvic health program there. I started my training for pelvic floor physical therapy with Herman and Wallace in 2015. I have completed the Herman and Wallace Pelvic Floor series in 2017 and passed the Pelvic Rehabilitation Practitioner Certification in May 2021.
Q: What patient population do you find most rewarding in treating and why?
A: Over the past 6 years, I have enjoyed helping both women and men with issues related to their pelvic floor, connecting it to their spine, hip, abdominal, and lower extremity issues. I help them return to an active lifestyle and feel empowered over something so limiting and invisible to others.
Patients with pelvic floor dysfunction are often overlooked because their symptoms are too sensitive to speak about. I truly believe they deserve the best care possible and am grateful to be part of a team that focuses on patient-centered care. Treating both pelvic floor dysfunction and the oncological patient population benefits under-served patient populations. Both demographics have my heart for personal reasons. I always knew I wanted to help those who are in need able to get much support.
Q: What has been your favorite Herman & Wallace Course and why?
A: I have enjoyed the whole pelvic floor series, but Pelvic Floor Level 1 and Level 2B, taught by Tina Allen and Holly Tanner, were so great! These courses just inspired me to give my full attention to pelvic health. They are easy to learn from and full of so much knowledge.
Q: What is in store for you in the future as a clinician?
A: Right now, I am focused on building the pelvic health program in this smaller northern California city and hopefully bringing more providers to serve this community. I have a dream of teaching in the future and helping build the next generation of physical therapists and pelvic floor physical therapists.

Portions of this blog are from an interview with Dustienne Miller. Dustienne is the creator of the two-day course Yoga for Pelvic Pain. She passionately believes in the integration of physical therapy and yoga in a holistic model of care, helping individuals navigate through pelvic pain and incontinence to live a healthy and pain-free life.
Have you noticed when you are afraid or don’t want to feel something you hold your breath? Imagine what it's like to have daily pain that limits function and how that could impact rib cage, abdominal and pelvic floor expansion. Dustienne Miller discusses this in her remote course, Yoga for Pelvic Pain, upcoming on July 31 - August 1, 2021. Her course focuses on two of the eight limbs of Patanjali’s eightfold path: pranayama (breathing) and asana (postures) and how they can be applied for patients who have hip, back, and pelvic pain.
Dustienne explains "We teach our patients how breathing patterns inform our digestion, our spine, our emotional state, our pelvic floor, etc. It’s one of the most powerful tools we have to inform our system that we are safe. Despite this knowledge, we will often find ourselves holding our breath or breathing in non-optimal ways without even realizing it." Dustienne focuses her practice on introducing yoga to patients within the medical model. Yoga can be included in pelvic rehabilitation in so many ways, including incorporating yoga home programs as therapeutic exercise and neuromuscular re-education (both between visits and after discharge).
Pelvic conditions that can be positively impacted by yoga are interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia. Treatment for these conditions often involves an individualized approach that may include both pharmacologic therapies (prescription drugs, analgesics, and NSAIDs) and nonpharmacologic interventions such as exercise, muscle strength training, cognitive behavioral therapy, movement/body awareness practices, massage, acupuncture, and nutrition.
A systematic review of the 2017 clinical practice guidelines evaluated 14 randomized controlled trials and found that yoga was associated with lower pain scores (1). Similarly, in 2020 there was a review of 25 randomized controlled trials that examined the effects of yoga on back pain. Out of these trials, 20 studies reported positive outcomes in pain, psychological distress, and energy (2).
The great thing about yoga is that the asanas (postures) can be modified to accommodate your strength, experience, and health conditions. An example of this is the Downward Facing Dog pose. There are so many ways to made Downward Facing Dog work for your body. Use straps, the wall, or the plinth/countertop to provide support for your body as needed, which might look different each day.
Some folks think you need to be flexible to have a yoga practice. Dustienne stresses "What is necessary is to be flexible with understanding that every day might feel different. If you are in an active pain flare your practice will look different than on the days you are feeling better. That can be a challenging aspect of a mindful practice - embracing that every day is different. Have the courage not to judge yourself, but to celebrate that you are meeting your needs with kindness."
People have been doing yoga for thousands of years. It is a mind-body and exercise practice that combines breath control, meditation, and movements to stretch and strengthen muscles. Join Dustienne Miller in Yoga for Pelvic Pain on July 31 - August 1, 2021, to learn more about incorporating yoga into your clinical practice.
No prior experience with teaching yoga is required to attend the course. However, all participants must possess a working knowledge of pelvic pain conditions and foundational rehabilitation principles.
- Chou R, Deyo R, Friedly J, et al. Nonpharmacologic therapies for low back pain: a systematic review for an American College of Physicians clinical practice guideline. Ann Intern Med. 2017; 166(7):493-505.
- Park J, Krause-Parello CA, Barnes CM. A narrative review of movement-based mind-body interventions: effects of yoga, tai chi, and qigong for back pain patients. Holist Nurs Pract. 2020;34(1):3-23.

Erica Vitek, MOT, OTR, BCB-PMD, PRPC has attended extensive post-graduate rehabilitation education in the area of Parkinson disease and exercise. She is certified in LSVT (Lee Silverman Voice Treatment) BIG and is a trained PWR! (Parkinson Wellness Recovery) provider, both focusing on intensive, amplitude, and neuroplasticity-based exercise programs for people with Parkinson disease. Erica has taken a special interest in the unique pelvic floor, bladder, bowel, and sexual health issues experienced by individuals diagnosed with Parkinson disease. You can learn more about this topic in Erica's course, Parkinson Disease and Pelvic Rehabilitation, scheduled for July 23-24, 2021.
Parkinson disease (PD) non-motor symptoms can be even more impactful on quality of life than the cardinal motor symptoms most are familiar with, bradykinesia, rigidity, tremor, and postural instability. The list of non-motor symptoms is extensive affecting many body systems including cognitive, sensory, and autonomic.
Constipation is one of the most common autonomic non-motor symptoms experienced by people with Parkinson disease with studies showing 20-89% prevalence (1). As the disease progresses, individuals are more likely to experience symptoms that suggest a strong relationship between neurodegeneration and bowel dysfunction, such as, decreased frequency of bowel movements, difficulty expelling stool, and diarrhea (2). Constipation has also been hypothesized to be an early indicator for the development of Parkinson disease, and there is ongoing research in this area. It has yet to be shown that constipation is specific enough to predict the development of PD.
Developing an understanding of Parkinson disease constipation and how it differs from other individuals with constipation can have a strong impact on our recommended pelvic rehabilitation plans of care. In a study published by Zhang, M. et al., 2021, they looked at the characteristics of Parkinson disease with constipation (PDC) compared to functional constipation (FC). Functional constipation is generally defined as difficult, infrequent, or incomplete defecations (3). One of the main findings in this study was a significant difference between the groups when looking at resting rectal and anal canal pressures. In the PDC group, resting rectal and anal pressures were significantly lower. These resting pressures are mainly controlled by the internal anal sphincter resting tension which is supported by the autonomic nervous system. This leads the researchers to speculate there may be autonomic nervous system neuropathy in people with PD
They then looked at simulated defecation, which also showed that the PDC group had significantly lower rectal defecation pressure and a lower anal relaxation rate. Since rectal pressures during defecation assist in effective anal relaxation, the researchers state, “a coordinated movement disorder results” and that people with PD may have “pelvic floor cooperative motion disorder” (1). Additionally, the researchers noted that abnormal abdominal pressure is another main contributing factor to the low rectal defecatory pressure in PDC. Abdominal pressure is a key factor in driving complete and efficient rectal defecation. This is also a finding in numerous other studies in the literature unique in PDC.
The results of Zhang, M. et al., 2021 reveal the need for pelvic health practitioners to help train coordinated defecation efforts in people with Parkinson disease. In my course, Parkinson disease and Pelvic Rehab, we will have an in-depth discussion about how training defecatory dynamics is different in people with PD. Muscle training principles in this population are very unique. Understanding the underlying causal factors of dysfunction will have a significant impact when helping patients with Parkinson disease manage constipation.
- Zhang, M., Yang, S., Li, X. C., Zhu, H. M., Peng, D., Li, B. Y., ... & Tian, C. (2021). Study on the characteristics of intestinal motility of constipation in patients with Parkinson's disease. World Journal of Gastroenterology, 27(11), 1055.
- Sakakibara, R. (2021). Gastrointestinal dysfunction in movement disorders. Neurological Sciences, 1-11.
- Lacy, B. E., Mearin, F., Chang, L., Chey, W. D., Lembo, A. J., Simren, M., & Spiller, R. (2016). Bowel disorders.Gastroenterology 150 (6), 1393-1407.