The world needs more clinicians who can treat pelvic pain, pelvic organ prolapse, urinary incontinence, diastasis recti, and the many other conditions that constitute pelvic floor/pelvic girdle dysfunction. Most clinicians who specialize in pelvic rehabilitation are Physical Therapists (PT) or Occupational Therapists (OT), though other licenses also allow you to work with patients who have pelvic floor dysfunction. Many doctors, nurses, and internationally licensed medical professionals are beginning to explore the field of pelvic rehabilitation.
In an interview for the Pelvic Rehab Report, faculty and instructor Tiffany Ellsworth Lee MA, OTR, BCB-PMD, PRPC, shared that "Occupational therapists wishing to pursue pelvic floor have a few options. The first thing is to find a pelvic floor clinical setting...or check to see if they can start a women's health program with a strong focus on the pelvic floor. OTs quite often do not start out in pelvic health directly after school. Since this is a newer area as compared to other certifications such as the NDT and PNF, it takes a little bit of research, time, and effort to find one’s exact niche. To get started, an OT should seek out courses that teach the basics of bladder and bowel management. It is important to understand the anatomy and physiology of the bladder, bowel, and sexual systems."
Once you have a license to practice, you can start learning to specialize in pelvic rehabilitation. The best place to start is with the H&W Pelvic Floor Level 1 satellite lab course, which offers immediately applicable clinical skills for evaluating and treating urinary incontinence or the musculoskeletal components of urogynecologic pain syndromes. Most practitioners who take Pelvic Floor 1 return to study in the next courses in the series.
You can learn all about the colorectal system, and how to treat conditions such as coccyx pain, pudendal neuralgia, and male pelvic pain in the Pelvic Floor 2A course, and in Pelvic Floor 2B you can expand your knowledge in topics such as movement assessment and re-training, prolapse, and pelvic pain. Then in the Pelvic Floor Capstone course, the final advanced course, you dive deep into topics such as hormones and their influence on conditions, surgeries and recovery, and skilled manual therapy techniques. Once you know your patient demographic, you can check out our growing list of specialty courses that include series topics including yoga, oncology, pregnancy, fascial mobilization, and much more.
Once you have gained experience in the field, you may consider sitting for the Pelvic Rehabilitation Practitioner Certification (PRPC). This certification recognizes expertise in pelvic rehabilitation for patients of all genders throughout the lifecycle. To be eligible to sit for the exam, applicants must have completed 2000 licensed hours of direct pelvic patient care in the past eight years, 500 of which must have been in the last two years.
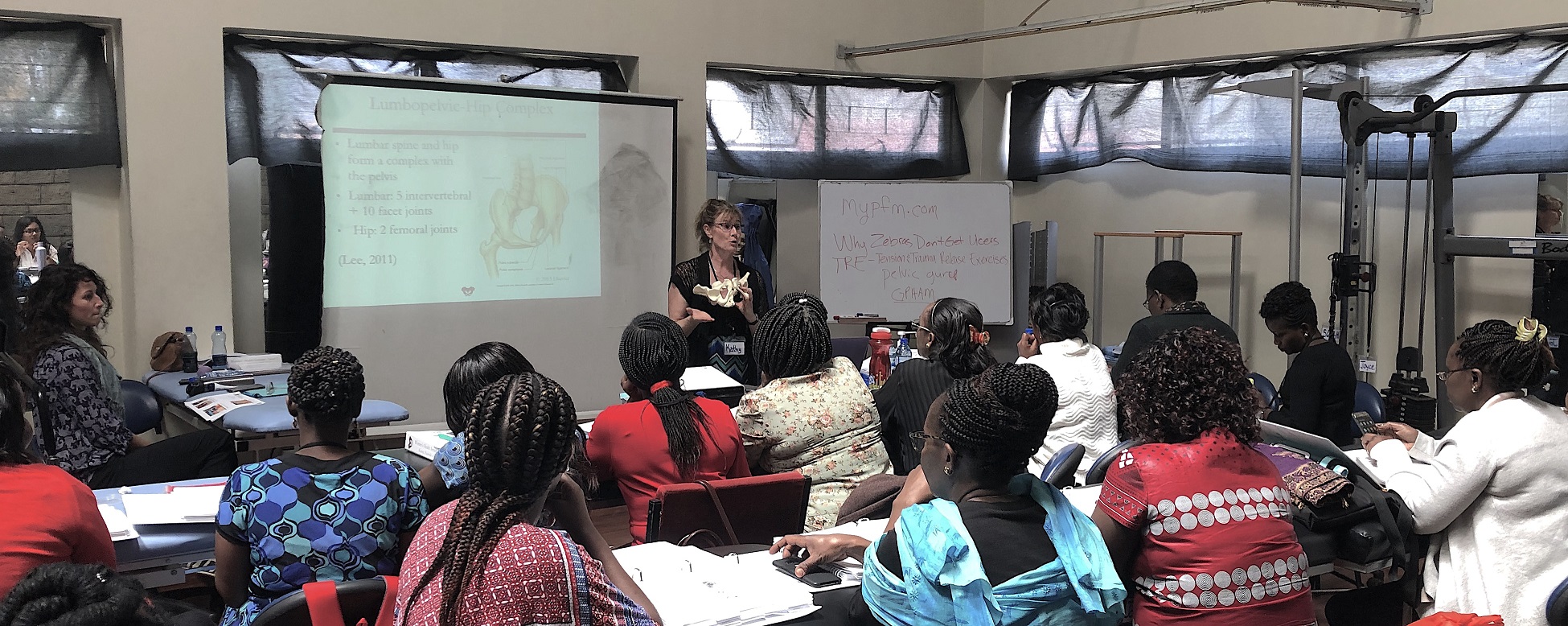
Earlier this year, Herman & Wallace sponsored the first ever pelvic rehab course for physios in Nairobi, Kenya in partnership with The Jackson Clinics Foundation. After returning from that course, Kathy Golic, PT spent months writing a new course, adapting information from Pelvic Floor Level 1, Level 2A, and the Pregnancy and Postpartum series. This October, Kathy (along with co-instructors Casie Danenhauer and Sherine Aubert) returned to teach her follow-up course that expanded on the first module, introducing lectures and labs tailored to the community of pelvic physios in Kenya. This dispatch comes from instructor Kathy Golic, PT, who sent in this article shortly after returning from the course. Huge thanks to Kathy and her colleagues Sherine Aubert and Casie Danenhauer for doing this important work!
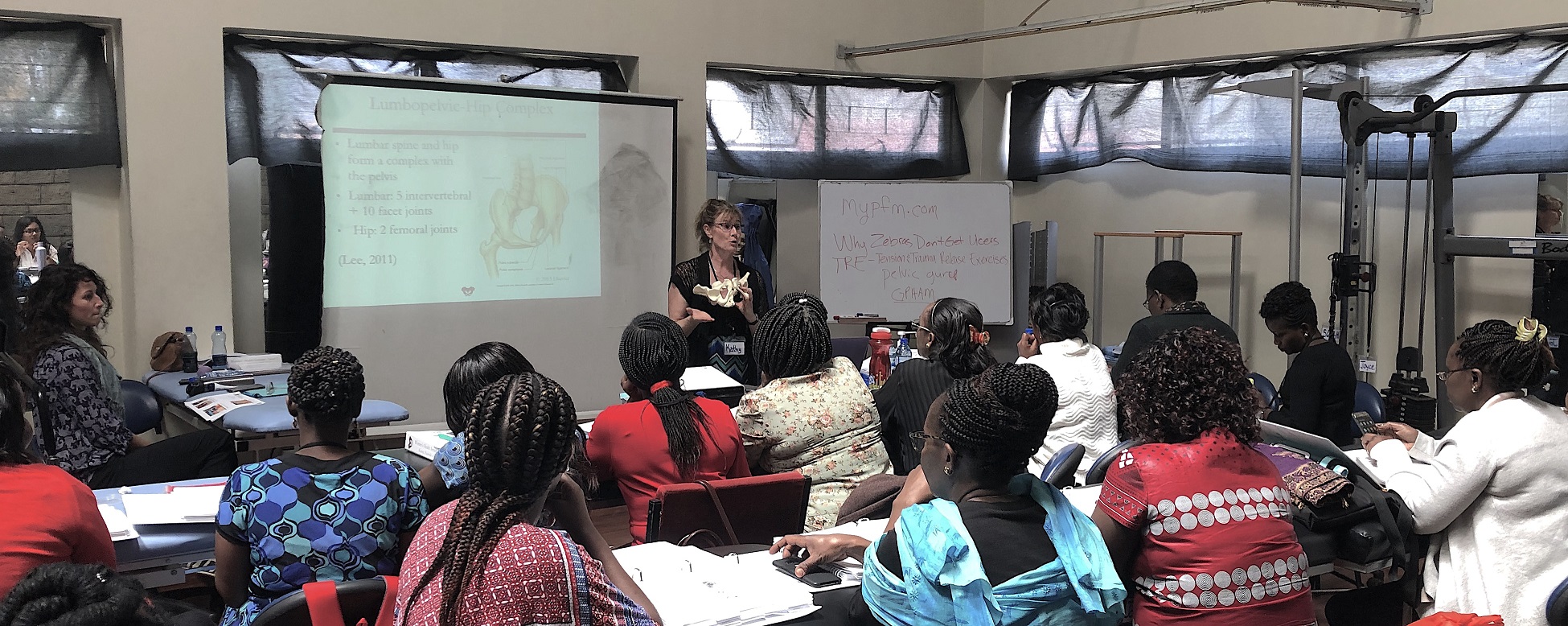 It has been a week now, and as I type looking out on the windy rainy day, it is hard to believe that I was so recently in a warm, sheltered classroom sequestered from the hustle and bustle of Nairobi. A place which has captured my heart. Really it is the people, especially my new “sisters” who I spent so much time with during this last two-week course module. Once again, I experienced chill bumps every day from witnessing the growth, the stories, the wisdom and the compassion of these bright, motivated, committed physiotherapists who came back for the 2nd module in our series to help them become experts in the field of Pelvic Health. This module covered topics of Pregnancy, Postpartum care, Prolapse, Colorectal Conditions including fecal incontinence and constipation, and Coccydynia. We had a terrific printed course manual for this 2nd in the series, thanks to the partnership of Herman and Wallace and Jackson Clinics Foundation. With my wonderful and resourceful, skilled colleagues from LA, Casie Danenhaur, and Sherine Aubert, we included comprehensive lectures, lively demonstrations, hands on creative experiential learning opportunities, and awesome supervised lab training sessions. We also had a lot of case study discussions, and live case studies where we assisted the students, who are practicing physiotherapists, in conducting thorough assessments and clinical reasoning processes to treat and make plans to further the progress of their patients.
It has been a week now, and as I type looking out on the windy rainy day, it is hard to believe that I was so recently in a warm, sheltered classroom sequestered from the hustle and bustle of Nairobi. A place which has captured my heart. Really it is the people, especially my new “sisters” who I spent so much time with during this last two-week course module. Once again, I experienced chill bumps every day from witnessing the growth, the stories, the wisdom and the compassion of these bright, motivated, committed physiotherapists who came back for the 2nd module in our series to help them become experts in the field of Pelvic Health. This module covered topics of Pregnancy, Postpartum care, Prolapse, Colorectal Conditions including fecal incontinence and constipation, and Coccydynia. We had a terrific printed course manual for this 2nd in the series, thanks to the partnership of Herman and Wallace and Jackson Clinics Foundation. With my wonderful and resourceful, skilled colleagues from LA, Casie Danenhaur, and Sherine Aubert, we included comprehensive lectures, lively demonstrations, hands on creative experiential learning opportunities, and awesome supervised lab training sessions. We also had a lot of case study discussions, and live case studies where we assisted the students, who are practicing physiotherapists, in conducting thorough assessments and clinical reasoning processes to treat and make plans to further the progress of their patients.
 All of this in itself was incredibly rewarding. But there was more. The power of sacrifice we witnessed. The power of solidarity and true generosity. Most of these women continued to have to work after class even while in this two-week module; in class from 8-4, but then going on their way, some of them through heavy Nairobi traffic, to treat patients in their offices, or to work hospital shifts. One student heading out after a Wed. afternoon class told me that she was going to work from 7- midnight, then would sleep until 4am, then back to work until 7 am, before returning to class at 8 am. She also had to miss one class to participate in her mentorship for her ortho advanced diploma, so had to make up a test with us the next day. (she aced the test!) Now for the generosity. I will share just 1 of many stories. One of the physios asked a patient of hers whom she felt she could use some help with, if she would mind traveling to the KMTC classroom where we were teaching so the other students could learn, while we the visiting instructors, would help guide in her assessment and care. This woman agreed, and got up at 3:30 am, traveled by bus for 3 hours to come for her treatment. She willingly shared her story, and it was tough to hear. She worked as a vegetable vendor carrying produce on her back, lifting it, and sitting on a stone for hours each day. She, a mother of 5 grown children with an unemployed husband. Her physio and the class did quite well in their assessment and with treatment and suggestions. She seemed pleased. Then as she prepared to leave, some of the physio students “passed the hat” and collected 7,000 kshillings (about $70.00) and presented this humble lady with the money so that she could afford transportation home. It is my understanding that most Kenyans spend 50% of their income on food, so sharing with this patient was a true sacrifice. But for these ladies, there was no question about it. This is how they live and how they work. They are themselves so grateful for the knowledge, skills and experience that they are getting through this program, and they will pay it backwards and forwards. My colleagues this time and last time, are also indebted to them for all they have taught us. It is truly an honor and privilege to be part of this great program, and I too am thankful for all the team players in this venture.
All of this in itself was incredibly rewarding. But there was more. The power of sacrifice we witnessed. The power of solidarity and true generosity. Most of these women continued to have to work after class even while in this two-week module; in class from 8-4, but then going on their way, some of them through heavy Nairobi traffic, to treat patients in their offices, or to work hospital shifts. One student heading out after a Wed. afternoon class told me that she was going to work from 7- midnight, then would sleep until 4am, then back to work until 7 am, before returning to class at 8 am. She also had to miss one class to participate in her mentorship for her ortho advanced diploma, so had to make up a test with us the next day. (she aced the test!) Now for the generosity. I will share just 1 of many stories. One of the physios asked a patient of hers whom she felt she could use some help with, if she would mind traveling to the KMTC classroom where we were teaching so the other students could learn, while we the visiting instructors, would help guide in her assessment and care. This woman agreed, and got up at 3:30 am, traveled by bus for 3 hours to come for her treatment. She willingly shared her story, and it was tough to hear. She worked as a vegetable vendor carrying produce on her back, lifting it, and sitting on a stone for hours each day. She, a mother of 5 grown children with an unemployed husband. Her physio and the class did quite well in their assessment and with treatment and suggestions. She seemed pleased. Then as she prepared to leave, some of the physio students “passed the hat” and collected 7,000 kshillings (about $70.00) and presented this humble lady with the money so that she could afford transportation home. It is my understanding that most Kenyans spend 50% of their income on food, so sharing with this patient was a true sacrifice. But for these ladies, there was no question about it. This is how they live and how they work. They are themselves so grateful for the knowledge, skills and experience that they are getting through this program, and they will pay it backwards and forwards. My colleagues this time and last time, are also indebted to them for all they have taught us. It is truly an honor and privilege to be part of this great program, and I too am thankful for all the team players in this venture.

As more and more patients seek care for pelvic floor dysfunction, the need for more qualified practitioners is becoming apparent. Many patients prefer to see a clinician who they identify with, which is why it is important for practitioners of all genders to learn to treat pelvic floor dysfunction. Because much of the public's awareness of pelvic rehab comes out of women's health, the vast majority of pelvic health practitioners are women.
There is currently a shortage of male pelvic health practitioners. To help us understand why it is so important to fix that, we reached out to several male clinicians who have attended the Male Pelvic Floor: Function, Dysfunction, and Treatment course to ask them about the need for more men in the field. Here are some answers to the question:
“Why is it important to have male providers available to treat male patients in the field of pelvic health?”
Grant Headley of Bridgetown Physical Therapy of Portland, Oregon (www.bridgetownpt.com)
While as PT’s we all approach our patients with interest in helping them as individuals, some of our patients feel more comfortable sharing certain details with a provider of the same gender. Many of the hang-ups some men have about receiving care from a female provider are related to an older generation, to certain traditional or religious cultural beliefs, or to certain beliefs about propriety related to receiving care.
As acknowledged in our coursework, generally men have cultural barriers that traditionally do not permit sharing of vulnerability or weakness, especially in the sexual domain. Here are a few unsolicited statements I feel encapsulate what my own male patients have told me: Some heterosexual men feel more comfortable sharing the details of their dysfunction with a man because they find it difficult to admit vulnerability in the presence of a female. Some men prefer not to relay the clinically pertinent details of dysfunctional sexual encounters with a female because they do not wish to make the female practitioner uncomfortable. Many men feel that they can relay more detail about the mechanics of the sexual dysfunction or signs of improvement to a male provider. Some men have told me that they felt their sexual dysfunction was minimized or that they have been treated with patronizing language by a female pelvic PT in the past. Unfortunately, these patients attribute this negative experience to the PT being female, and they are not comfortable having a second opinion with a female.
 Although we strive to present as open-minded and neutral to our patients, they may have an affinity for a male provider. This could foster a more constructive clinical partnership towards working on their goals if they perceive fewer communication barriers. I can offer my own experience as a past patient suffering with pelvic floor dysfunction; I was so desperate for help and I felt so grateful that there was a physical therapist in my city at all that was willing to help me. I did not care that she was female and that I had to receive treatment at a women's health clinic for new mothers in the University Hospital. Many female therapists reading this article have likely transferred lifesaving PT care to scores of men. This organization of H&W that does so much good for a sensitive aspect of men's care is dominated by women- this needs to be acknowledged as a net positive but also appreciated that much of the education and application of care is an adaptation from what has worked for women in the past. Many men will be so grateful to receive care and get better. Some men unfortunately will have barriers to receiving care and for those patients, we can seek out and encourage our male colleagues to get involved in pelvic rehab so we can all provide more access to care.
Although we strive to present as open-minded and neutral to our patients, they may have an affinity for a male provider. This could foster a more constructive clinical partnership towards working on their goals if they perceive fewer communication barriers. I can offer my own experience as a past patient suffering with pelvic floor dysfunction; I was so desperate for help and I felt so grateful that there was a physical therapist in my city at all that was willing to help me. I did not care that she was female and that I had to receive treatment at a women's health clinic for new mothers in the University Hospital. Many female therapists reading this article have likely transferred lifesaving PT care to scores of men. This organization of H&W that does so much good for a sensitive aspect of men's care is dominated by women- this needs to be acknowledged as a net positive but also appreciated that much of the education and application of care is an adaptation from what has worked for women in the past. Many men will be so grateful to receive care and get better. Some men unfortunately will have barriers to receiving care and for those patients, we can seek out and encourage our male colleagues to get involved in pelvic rehab so we can all provide more access to care.
Lance Frank of Flex Physical Therapy in Atlanta (www.flexptatl.com)
Personally, as a male provider in pelvic health, I find that the men I treat are much more comfortable and at ease discussing topics like erections (or lack thereof) and sexual dysfunction, as well as incontinence, or pelvic pain. In a female dominated sub-specialty of physical therapy, sometimes as a male it can be intimidating and even embarrassing for some men to discuss these topics at all, let alone with a female; so having the option to speak and be treated by another male who may better understand the changes, anatomy, and problems they’re experiencing may feel a bit less daunting. Our culture has made male masculinity fragile and I think some populations of men who need pelvic floor rehab may feel embarrassed to be treated by a female clinician if their perception of being seen by a female is emasculating. Ultimately, I think there needs to be more men in this field because there needs to be better visibility of male pelvic health providers in general, as well as better representation of men acknowledging that male pelvic floor disorders exist and are willing and able to treat them.
Eddie Gordon of Flow Rehab in Seattle (www.flowrehab.com)
There are far fewer male physiotherapists treating men with pelvic floor dysfunctions, but I am hopeful this will change for the better. Lack of access to male pelvic physios is a relative barrier to care because some men are more comfortable seeing a male pelvic provider the same way most women would prefer seeing a female pelvic physio. In general, men do not typically seek treatment as frequently or early enough the way most women do. If male pelvic physios are not available, then men may more likely delay treatment, which could potentially worsen their problem. Ironically, when it comes to men with pelvic floor dysfunctions, men are underrepresented, but I am hopeful that more male PT’s will be joining the movement to educate the male population.
Milan Patel of Comprehensive Therapy Services in San Diego (comprehensivetherapy.com)
I believe it's important to have male providers in the pelvic health field for many reasons, one being the opportunity for connection. I think we connect best with reflections of ourselves and for men seeking out a pelvic health provider that can be hard to find. In my experience, pelvic physical therapy works best when your patient can be open and honest, and establishing a strong connection between therapist and patient is the first step. Another reason is that people should have options for the provider they want. In San Diego I am the only male pelvic physical therapy provider which means most men seeking pelvic floor therapy have no choice but to see a female. If you switched the genders in the last sentence you could see how that is problematic. Many women prefer to have their pelvic PT be a female, I just think guys should get the same choice.
Steven Lavender of The Physical Therapy Practice NYC in New York (thephysicaltherapypractice.nyc)
In my experience as a gay male practitioner practicing pelvic floor physio on only men:
Gay male patients usually prefer a gay provider because they feel like they don’t have to explain lifestyle issues and choices, they may be unused to being touched by women, and maybe misogynistic.
Some straight men have told me that they think a male practitioner would know more about their pelvic issues than a woman. Some men don’t think women are strong enough nor have long enough fingers to get to the places they need to be. Some straight men report they might be attracted to a female therapist and get an erection or feel embarrassed about appearing unmanly with their particular pelvic condition.
For some men being touched by a woman is a religious issue so many males of the Jewish and Muslim faiths prefer to see a male practitioner.
Some men could not care less who sees them as long as they get better.
One woman called me for advice or for an appointment from some distance because they "figured a gay man in New York City just might know more about my ass and ass pain than any local jack-assed doctor in my neck of the woods." True story.
If you are interested in learning to treat male patients, the Male Pelvic Floor: Function, Dysfunction, and Treatment course is a great place to start! The course is taking place twice more in 2019, this September 13-15, 2019 in Pasadena, CA, and again in Fort Myers, FL on October 19-21, 2019. We are already booked four times in 2020 as well, so be sure to check out the full course schedule for all available dates.
This post was written by the teaching team of Nancy Cullinane, PT, MSH, Kathy Golic, PT, and Terri Lannigan DPT, who took their talents to Nairobi, Kenya to teach a modified version of Herman & Wallace's Pelvic Floor Level 1 course.
 At the end of week 1 of Kenyan Pelvic Floor Level 1, we are pleased to report that 35 physiotherapists are embracing pelvic health physical therapy. Our students are primarily from the Nairobi area, however a handful have traveled from rural areas. The majority of them have some aspect of women's health in their job duties, however, only two have previously performed internal pelvic floor muscle techniques. On the first day of class, we spent significant introductory time discussing course objectives, students' clinical experience, Kenyan healthcare delivery, and what they hoped to gain from us. One student described teaching herself skills she is using in her clinical practice from watching YouTube videos. Another student commented, "the only tool I have to treat my patients is the kegel exercise and it isn't working for many of my patients. I know I'm missing something and I hope to find it here." The concept of internal pelvic floor muscle evaluation and treatment is new in Kenya and this is the first presentation of this coursework. There was significant anxiety surrounding internal pelvic muscle examination lab in the course. Several participants were not aware what "internal examination" meant in the course description when they registered. One student did not return on day two because of it. Nonetheless, as soon as the first internal assessment lab was completed, the pace picked up considerably.
At the end of week 1 of Kenyan Pelvic Floor Level 1, we are pleased to report that 35 physiotherapists are embracing pelvic health physical therapy. Our students are primarily from the Nairobi area, however a handful have traveled from rural areas. The majority of them have some aspect of women's health in their job duties, however, only two have previously performed internal pelvic floor muscle techniques. On the first day of class, we spent significant introductory time discussing course objectives, students' clinical experience, Kenyan healthcare delivery, and what they hoped to gain from us. One student described teaching herself skills she is using in her clinical practice from watching YouTube videos. Another student commented, "the only tool I have to treat my patients is the kegel exercise and it isn't working for many of my patients. I know I'm missing something and I hope to find it here." The concept of internal pelvic floor muscle evaluation and treatment is new in Kenya and this is the first presentation of this coursework. There was significant anxiety surrounding internal pelvic muscle examination lab in the course. Several participants were not aware what "internal examination" meant in the course description when they registered. One student did not return on day two because of it. Nonetheless, as soon as the first internal assessment lab was completed, the pace picked up considerably.
 These pioneering physiotherapists have developed new skills this past week for treating overactive bladder, mixed urinary incontinence, overactive pelvic floor muscles, prolapse, and diastasis recti. We have delved into discussion regarding sexual trauma and how cultural differences here in Kenya will impact the students' potential strategies in initiating conversations with their patients. Nine of our students are employed at Kenyatta National Hospital, the largest public hospital in Nairobi. Several are employed in private hospitals, who serve those citizens who pay to receive care in their respective systems. Many of our students are under-employed and some see patients privately in their homes, often for cash.
These pioneering physiotherapists have developed new skills this past week for treating overactive bladder, mixed urinary incontinence, overactive pelvic floor muscles, prolapse, and diastasis recti. We have delved into discussion regarding sexual trauma and how cultural differences here in Kenya will impact the students' potential strategies in initiating conversations with their patients. Nine of our students are employed at Kenyatta National Hospital, the largest public hospital in Nairobi. Several are employed in private hospitals, who serve those citizens who pay to receive care in their respective systems. Many of our students are under-employed and some see patients privately in their homes, often for cash.
We have additional Herman & Wallace Pelvic Floor Level 1 curriculum planned for week two, but we will also present the additional curriculum we have written specifically for these Kenyan physiotherapists. We will dedicate ample time toward connecting these motivated students with global mentoring resources, but we will also lay groundwork in helping them to set up a support network for pelvic health PT with each other.
We are honored and grateful to Herman & Wallace for donating Pelvic Floor Level 1 curriculum and to The Jackson Clinics Foundation for its history in changing physical therapy delivery in Kenya, including the financing of travel for this course. We are also thankful to Kenya Medical Training College for covering the cost of instructor lodging. At the half way mark of level 1, we feel we have already received so much more than we have given. We are especially grateful to the 35 course participants who will be changing the face of women's health physical therapy in Kenya from here on. Improving the quality of life for women improves the quality of life for families, and has an overall positive impact on the community.
The photography from this course is the creation of Marielle Selig, who acted as both technical support and official photographer for the Kenya Pelvic Floor Level 1 course. More of her work will be posted at https://mariselig.pixieset.com/.

This post is a follow-up to the February 20th post written by Nancy Cullinane, "Pelvic Floor One is Heading to Kenya"
By the time folks are reading this, Nancy Cullinane, PT, MHS, WCS, Terri Lannigan, PT, DPT, OCS, and I will likely be in a warm, crowded classroom in Nairobi, Kenya helping 30+ “physios” navigate the world of misbehaving bladders, detailed anatomy description, and their first internal lab experiences. No doubt it will be both challenging and extremely rewarding. We are so grateful to the Herman & Wallace Pelvic Rehab Institute for sharing their curriculum in partnership with the Jackson Clinics Foundation to allow us to offer their valuable curriculum in order to affect positive health care changes.
I personally am humbled and honored to get to play a small but key role in the development of foundational knowledge and skills for these women PT’s who will no doubt change the lives of countless Kenyan women, and, consequently, their families.
My adventure truly began when I offered to write lectures on the topics of Fistula and FGM/C (female genital mutilation/cutting) and I began the process of crash course learning about these topics. The quest has taken me on a deep dive into professional journals, NGO websites, surgical procedure videos and insightful interviews with some of the pioneers working for years including “in the field” to help women in Africa and in countries where these issues are prevalent.
Before I began my research on the topic of fistula, I pretty much thought of a fistula as a hole between two structures in the body where it doesn’t belong, and narrowly thought of in terms of anal fistulas, acknowledging how lucky we are that there are skilled colorectal surgeons who can fix them. But after more research, my world view changed. (Operative word here being “world”).
A fistula is an abnormal or surgically made passage between a hollow or tubular organ and the body surface, or between two hollow or tubular organs. For our purposes here today, I am referring to an abnormal hole or passage between the vagina and the bladder, or rectum, or both. When the fistula forms, urine and/or stool passes through the vagina. The results are that the woman becomes incontinent and cannot control the leakage because the vagina is not designed to control these types of body fluids.
According to the Worldwide Fistula Fund, there are ~ 2 million women and girls suffering from fistulas. Estimates range from 30 to 100 thousand new cases developing each year; 3-5 cases/1000 pregnancies in low-income countries. A woman may suffer for 1-9 years before seeking treatment. For women who develop fistula in their first pregnancy, 70% end up with no living children.
Vesicovaginal fistulas (VVF) can involve the bladder, ureters, urethra, and a small or large portion of the vaginal wall. Women with VVF will complain of constant urine leakage throughout the day and night, and because the bladder never fills enough to trigger the urge to void, they may stop using the toilet altogether. During the exam there may be pooling of urine in the vagina.
Rectovaginal Fistula is less common, and accounts for ~ 10% of the cases. Women with RVF complain of fecal incontinence and may report presence of stool in the vagina. These women often will also have VVF.
In Kenya, most fistulas are obstetric fistulas, which occur as a result of prolonged obstetric labor (POL). These are also called gynecologic, genital, or pelvic fistulas. Traumatic fistulas account for 17-24 % of the cases and are caused by rape, sexual or other trauma, and sometimes even from FGM/C. The other type of fistula by cause is iatrogenic, meaning unintentionally caused by a health care provider during procedures such as during a C-section, hysterectomy, or other pelvic surgery. Most fistulas seen in the US are of this type.
Prolonged Obstructed Labor most often occurs when the infant’s head descends into the pelvis, but cannot pass though because of cephalo-pelvic disproportion (mismatch between fetus head and mother’s pelvis) thus creating sustained pressure on the tissues separating the tissues of the vagina and bladder or rectum, (or both) leading to a lack of blood flow and ultimately to necrosis of the tissue, and the development of the fistula. Those who develop this type of fistula spend an average of 3.8 days in labor (start of uterine contractions), some up to a week. In these cases, family members or traditional birth attendants may not recognize this is occurring, and even if they do, they may not have the instrumentation, the facilities or the skills necessary to handle the situation with an instrumental delivery or a C-section. And many of these women are in remote locations without transportation to appropriate facilities or lack the money to pay for procedures.
There are many adverse events and medical consequences that can result as a result of untreated obstetrical fistulas including the death of the baby in 90% of the cases. Physical effects besides the incontinence previously mentioned can include lower extremity nerve damage, which can be disabling for these women, along with a host of other physical and systemic health issues. The social isolation, ostracization by community, divorce, and loss of employment can lead to depression, premature lifespan, and sometimes suicide.
The good news is there are several great organizations making a difference.
In most cases, surgery is needed to repair the fistula. Sometimes, however, if the fistula is identified very early, it may be treated by placing a catheter into the bladder and allowing the tissues to heal and close on their own, and this is more viable in high-income countries after iatrogenic fistulas, but unfortunately, most women in the low-income countries have to wait for months or years before they receive any medical care.
There is an 80-90% cure rate depending on the severity, but according to the Worldwide Fistula Fund, 90% are left untreated, as the treatment capacity is only around 15,000 per year for the 100,00 new patients requiring it. Prevention is vital.
Despite successful repair of vesicovaginal fistulas, research shows that 15-35% of women report post-op incontinence at the time of discharge from the hospital, and that 45-100% of women may become incontinent in the years following their repair. Studies suggest that scar tissue-fibrosis of the abdominal wall and pelvis, and vaginal stenosis are strongly associated with post-operative incontinence.
According to research by Castille, Y-J et al in Int. J Gynecology Obstet 2014, there can be improved outcome of surgery both in terms of successful closure of vesicovaginal fistula and reduced risk of persistent urinary incontinence if women are taught a correct pelvic floor muscle contraction and advised to practice PFM exercise. Other studies have shown a positive effect from pre and post op PT in both post op urinary incontinence and PFM strength and endurance with a reduction of incontinence in more than 70% of treated patients, with improvements maintained at the 1year follow up. SO, THIS IS ONE REASON WE ARE SO EXCITED TO BE GOING TO KENYA!
I inquired about the use of dilators via email communication with surgeon Rachel Pope , MD MPH who has done extensive work in Malawi with women who have suffered from fistula, including the use of dilators, and her response was: “in women who have had obstetric fistula the dilators seem only marginally helpful after standard fistula repairs. The key is to have a good vaginal reconstructive surgery where skin flaps that still maintain their blood supply replace the area in the vagina previously covered by scar tissue. The dilators work exceedingly well when there is healthy tissue in place, and I think the overall outcomes are better for women in those scenarios compared to the cement-like scar we often see in women with fistulas.”
In the US, there are specialist surgeons who provide surgical repairs. While genitourinary fistulas can occur because of obstructed labor and operative deliveries in high income countries, they can also occur in a variety of pelvic surgeries, post pelvic radiation, as well as in cases of cancer, infections, with stones, and as well etiology includes instrumentations such as D&Cs, catheters, endoscopic trauma, and pessaries, and as well in cases of foreign bodies, accidental trauma, and for congenital reasons. As pelvic therapists it is important to know your patients’ surgical and medical history and to pay special attention to the patient’s history regarding their incontinence description and onset and be mindful during exam to notice possible pooling of urine in the vagina. Though rare in terms of occurrence, we should be aware of the possibility and may play a role in referring the patient to a physician who can do further diagnostic testing
In conclusion, I want to thank UK physiotherapist Gill Brook MCSP (DSA) CSP MSC, president of the IOPTWH who shared with me by interview her knowledge of fistula and experiences with the Addis Ababa Fistula Hospital in Ethiopia, which she has been visiting for 10 years, as well as Seattle’s Dr. Julie LaCombe MD FACOG who has performed fistula surgeries in Uganda and Bangladesh and met with me personally to share about obstetrical trauma and fistula surgery and management.
Nancy, Terri and I will look forward to sharing photos and more about our journey and experiences, upon our return. In the meantime, check out the Campaign to End Fistula and join the campaign.
In the spring of 2019, myself and two lab assistants will have the privilege of teaching PF1 to Kenyan physical therapists through the Kenya Medical Training College (KMTC) in Nairobi, Kenya. The program at KMTC started six years ago by Washington DC-based physical therapist Richard Jackson, and The Jackson Clinics Foundation (Teachandtreat.org), with a focus on orthopedic manual therapy. A neuro rehab program ensued two years later, and the aim for this women’s health program is to build a three level course series similar to the way it is taught in the United States. The goal of all of these programs is to transition them to Kenyan faculty within six years, which has recently occurred in the orthopedic component. Herman & Wallace Pelvic Rehab Institute has graciously agreed to donate curriculum content to the women’s health course component.
 Teaching assistant Terri Lannigan, PT, DPT, OCS, who has taught the lumbopelvic girdle course in the orthopedic program, and also practices women’s health physical therapy in the US, began laying the groundwork for this program with her students and in the Nairobi community last December. “Not only is there a tremendous need, but there is a lot of excitement from a group of students currently taking courses in the program, that women’s health education is coming to KMTC!”
Teaching assistant Terri Lannigan, PT, DPT, OCS, who has taught the lumbopelvic girdle course in the orthopedic program, and also practices women’s health physical therapy in the US, began laying the groundwork for this program with her students and in the Nairobi community last December. “Not only is there a tremendous need, but there is a lot of excitement from a group of students currently taking courses in the program, that women’s health education is coming to KMTC!”
Over the past month, I have been editing the Pelvic Floor 1 course to tailor it to our Kenyan physical therapist audience. The overwhelming majority of Kenyan PT’s do not have access to biofeedback or electric stim, so those sections will be omitted. As there are no documentation or coding requirements in the Kenyan health system, those sections of curriculum will also be edited out. Many of Terri’s PT students complained of significant underemployment, so we will keep the marketing component in our lectures, in hopes to promote expansion of women’s health PT to a larger segment of the Kenyan population.
Meanwhile, teaching assistant Kathy Golic, PT of Overlake Hospital Medical Center’s Pelvic Health Program in Bellevue, WA has headed up the data collection for a lecture on managing fistula and obstetric trauma. Kathy has accumulated data from many sources and conferred with several PTs currently involved in both clinical education as well as direct patient care in multiple African nations, to help us to create relevant, meaningful and culturally appropriate curriculum for this section of the PF1 course.
Pelvic Floor Level 1 will be offered between March 25 – April 6, 2019 at Kenya Medical Training College. We will post photos and additional information of our class and our experiences. We are grateful to Herman and Wallace and The Jackson Clinics Foundation for allowing us to be involved in this exciting endeavor.
Faiq Shaikh, M.D. is a dual fellowship-trained nuclear medicine physician & Informaticist, with a focus on translational research in the domains of Cancer imaging, Radiomics, Genomics, Informatics and Machine learning applications in Medicine. He has written more than 35 scientific articles and abstracts and 3 book chapters on related topics.
Introduction
Pelvic floor weakening is a common (occuring in half of women 50+) condition that leads to descent of the urinary bladder, uterovaginal vault, and rectum in the females, leading to urinary and fecal incontinence, and in extreme cases, pelvic organ prolapse.
Causes
Pelvic floor weakness is caused by a variety of factors, most of which increase the intra-abdominal pressure, such as pregnancy, multiparity, advanced age, menopause, obesity, connective tissue disorders, smoking, chronic obstructive pulmonary disease, etc. All these conditions lead to weakness of the pelvic musculature, ligaments, and fascia support result in descent of the pelvic floor organs.
Anatomy
The pelvic floor is divided into three compartments:
- Anterior compartment: contains the urinary bladder and urethra
- Middle compartment: contains the uterus, cervix, and vagina
- Posterior compartment: contains the rectum.
The structures in these compartments are supported by muscles, fascia, and ligaments anchoring them to the bony pelvis.
The endopelvic fascia is the most superior layer and covers the levator ani muscles and the pelvic viscera. Laterally, it forms the arcus tendineus. It attaches the cervix and vagina to the pelvic side wall as the parametrium and paracolpium. Posteriorly, the endopelvic fascia forms the rectovaginal fascia between the posterior vaginal wall and the rectum.
These fascial condensations are not well visualized on conventional MRI but their defects may be seen indirectly through secondary findings. These ligaments are not visualized on conventional MRI but may be visualized with an endovaginal coil which allows higher resolution and signal-to-noise ratio.
The levator ani muscles lie deep in relation to the endopelvic fascia and comprise of the puborectalis and the iliococcygeus muscles. Posteriorly and in the midline, the iliococcygeus condenses to form the levator plate. These are all well visualized on MRI. The perineal membrane lies inferior to the levator ani muscles and separates the vagina and rectum, which may be damaged during vaginal delivery when episiotomy is performed.
Pathophysiology
Pelvic floor relaxation is the weakness of the supporting muscles, fascia, and ligaments. This weakness progresses with age and may be related to hypoestrogenic states, such as menopause.
- occurs when the urinary bladder prolapses into the anterior vaginal wall, which may cause urinary incontinence.
- occurs due to weakness of the rectovaginal fascia, prolapsing rectum into the posterior vaginal wall, which may cause fecal incontinence.
- The parametrium and paracolpium weakness causes prolapse of the cervix and uterus.
- occurs when the small bowel prolapses through the rectovaginal fascia.
Accurate assessment of all compartments of the pelvic floor is necessary for surgical planning in order to minimize the risk of recurrence.
Diagnostics
Methods for the assessment of pelvic floor weakness include urodynamics, voiding cystourethrography, ultrasonography of the bladder neck and anal sphincter, fluoroscopic cystocolpodefecography, and MRI - which m is now the standard-of-care for preoperative planning for pelvic floor dysfunction, although it’s still not used for routine assessment.
Magnetic resonance imaging
MRI visualizes all three compartments of the pelvic floor and the pelvic support muscles and organs. We perform dynamic MRI of the pelvic floor with the patient in the supine or lateral decubitus positions. Conversely, MRI defecography or fluoroscopic cystocolpodefecography are performed in the sitting position, which is closer to the physiologic state. MR defecography is not superior to dynamic supine MRI for depiction of clinically relevant bladder descent and rectoceles. Overall, MRI accurately detects enteroceles and its contents when compared with fluoroscopic cystodefecography.
The preferred MRI pelvis protocols include: Ultrafast, large-field-of-view, T2-weighted sequences such as single-shot fast spin-echo (SSFSE), and half-Fourier acquisition turbo spin-echo (HASTE). After the dynamic examination is completed, small-field-of-view (20–24 cm) T2-weighted axial fast spin-echo (FSE) or axial turbo spin-echo (TSE) sequences are acquired to obtain high-resolution images of the muscles and fascia of the pelvic floor. The entire examination is typically completed in 20 minutes. This exam is performed with a torso phased-array coil wrapped around the pelvis. Endovaginal coil may be used to improve the spatial resolution of the pelvic ligaments, but it is invasive and can be uncomfortable.
MRI visualizes the uterus, cervix, and rectovaginal space. Ultrasonic gel may be administered into the vagina and rectum for better visualization. Also, incompletely voiding the urinary bladder improves visualization of the bladder and anterior vaginal wall prolapse.
For patients with a rectocele, patient is imaged after having evacuated the rectal contents. Chronic constipation and perineal hernias show as ballooning of the iliococcygeus muscle. The level of the pelvic floor is demarcated radiologically on the midsagittal image using the pubococcygeal line (from the most inferior portion of the pubic symphysis to the last horizontal sacrococcygeal joint). The levator plate should be parallel to the pubococcygeal line in normal cases.
The H line (5 cm) extends from the inferior symphysis pubis to the posterior anorectal junction on the midsagittal image and depicts the levator hiatus. The M line (2 cm) goes perpendicular from the pubococcygeal line to the most distal aspect of the H line and depicts the descent of the levator hiatus from the pubococcygeal line. Pelvic floor prolapse causes sloping of the levator plate and increasing length of the H and M lines, indicating widening and descent of the levator hiatus.
The T2-weighted axial images of the pelvic floor should be analyzed for signal intensity, symmetry, thickness, and fraying of the pelvic floor muscles. Bladder neck at strain should be less than 1 cm away from the pubococcygeal line. Descent of the bladder neck below the pubococcygeal line depicts the prolapse of the urinary bladder through the anterior vaginal wall resulting in a cystocele. Descent of the bladder neck during strain results in clockwise rotational descent of the bladder neck and proximal urethra. Distortion of the periurethral and paraurethral ligaments is seen in stress urinary incontinence. The normal butterfly shape of the vagina may also be altered by weakening of the paravaginal ligaments as it is displaced posteriorly. Prolapse of the middle compartment is associated with the vaginal apical prolapse and damage to the paracolpium seen in post-hysterectomy patients. On midsagittal MR images, descent of the uterus, cervix and vagina usually suggests disruption of the uterosacral or cardinal ligaments and elongated H and M lines. Pelvic organ prolapse increases the urogenital hiatus in the levator muscles. Caudal angle of more than 10° between the levator plate and the pubococcygeal line on midsagittal image is a sign of pelvic floor weakness.
On the midsagittal image, rectocele is identified by a rectal bulge of more than 3 cm (from anal canal and the tip of the rectocele). Contrast-enhanced MR shows hyperintense T2 signal in peritoneal fat contents in peritoneoceles, the hyperintense fluid-filled small-bowel loops in enteroceles, and the hyperintense gel-filled rectum/sigmoid colon in rectoceles/sigmoidoceles. Intussusception of the rectum on MR is seen as rectum invaginating distally toward the anal canal (MR defecography is superior to dynamic supine MR for this indication).
Performing MRI for pelvic floor dysfunction when indicated for surgical planning and the assessment if the extent of disease may reduce the risk of surgical failure.
This information is extremely useful to urogynecologists and surgeons.
MRI of pelvic floor dysfunction: review. Law YM, Fielding JR. AJR Am J Roentgenol. 2008.
"Over the next 30 years, growth in demand for services to care for female pelvic floor disorders will increase at twice the rate of growth of the same population. Demand for care for pelvic floor disorders comes from a wide age range of women… These findings have broad implications for those responsible for administering programs to care for women, allocating research funds in women’s health and geriatrics, and training physicians to meet this rapidly escalating demand"
- Karl M. Luber, MD, Sally Boero, MD, Jennifer Y. Choe, MD. The demographics of pelvic floor disorders: Current observations and future projections. Presented at the Sixty-seventh Annual Meeting of the Pacific Coast Obstetrical and Gynecological Society, Kamuela, Hawaii, November 14-19, 2000.
Patients with pelvic floor dysfunction have suffered for many years without knowing the names of their ailments. Chronic pain, constipation, incontinence, sexual dysfunction, and other pelvic conditions have a long history of being under-reported, misdiagnosed, and untreated. Shelby Hadden recounts in her animated documentary "Tightly Wound" being told by her doctor to treat vaginismus with a glass of wine before intimacy. She is not the only woman to be given such advice. It is going to take many voices to break through the years of misinformation and stigma that has impeded patients' ability to get treatment.
Thankfully the healthcare landscape has begun to shift. We seem to be on the cusp of a renaissance in pelvic care as patients become more aware of their treatment options. It is the mission of Herman & Wallace to help patients access a higher quality of care, through our courses and through our practitioner directory at https://pelvicrehab.com/. Patient education resources and practitioner directories are a big step in bringing about this awakening, and we believe that the more information the public has access to, the better. Ours is just one of several websites where patients can find learn about their conditions and find qualified clinicians to evaluate them and craft treatment regimens.
We hope that patients find pelvicrehab.com useful, and also encourage them to check out some other great resources. The Section on Women's Health operates a PT Locator available at https://ptl.womenshealthapta.org, and Pelvic Guru has been doing incredible work (see their robust patient portal at https://pelvicguru.com/for-patients/). Patients can also find helpful information via the International Pelvic Pain Society (IPPS) website at https://pelvicpain.org.
As an Institute, we've had the privilege of working with so many impassioned therapists, and we are excited to see so many of them out there in the world spreading awareness and knowledge so that patients get the care they need. We know there are many others working in the field and we hope you will tag and share your patient resources in the comments on this post.