A prostate cancer diagnosis often brings more than concerns about survival. It can impact urinary control, sexual function, pelvic comfort, and overall quality of life. Men who undergo radical prostatectomy or radiation therapy frequently experience urinary incontinence and erectile dysfunction, sometimes lasting months or years. Pelvic rehabilitation offers structured, evidence-based strategies to restore function, manage symptoms, and rebuild confidence during recovery.
Understanding Prostate Cancer and Its Impact on Pelvic Health
Prostate cancer is among the most common cancers in men. Risk factors include advancing age, family history, genetic predispositions (such as BRCA2 mutations), race or ethnicity, and lifestyle factors including diet and obesity. Diagnosis typically involves PSA screening, biopsy, and imaging to determine disease stage.
Treatment for localized disease often includes radical prostatectomy, external beam radiation therapy (EBRT), or brachytherapy. Each approach carries potential side effects that can affect urinary, sexual, and pelvic function. Even a nerve-sparing prostatectomy can lead to neuropraxia and disruption of pelvic structures, resulting in urinary leakage and erectile dysfunction (5). Radiation therapy can induce fibrosis, vascular injury, and tissue changes that affect erectile function, bladder, and bowel coordination (3). Combined or salvage treatments can further compound these effects (2).
Urinary Incontinence: The Role of Pelvic Floor Training
Urinary incontinence is one of the most common and distressing post-prostatectomy complications. Pelvic floor muscle training (PFMT) is widely recommended as a first-line intervention. Evidence demonstrates that men who engage in PFMT pre- or early postoperatively regain continence faster and experience less severe leakage than those who do not (3).
Effective PFMT focuses on both slow- and fast-twitch muscle contractions, integrating exercises into functional activities, and employing biofeedback or ultrasound to ensure proper engagement (4). Although differences in long-term continence may diminish, early training significantly improves quality of life and independence during the initial recovery months.
 Addressing Erectile Dysfunction Through Rehabilitation
Addressing Erectile Dysfunction Through Rehabilitation
Erectile dysfunction (ED) affects 30–80% of men after prostate cancer treatment, depending on nerve-sparing technique, age, baseline function, and comorbidities. Neurovascular damage, fibrosis, and ischemia are key contributors.
Radiation therapy further increases risk over time (1).
Penile rehabilitation, initiated early, promotes tissue health and functional recovery. Strategies include PDE5 inhibitors, vacuum erection devices, intracavernosal injections, and emerging techniques such as low-intensity shockwave therapy. PFMT complements these strategies by strengthening pelvic floor support, reducing coexisting muscle hypertonicity, and enhancing neuromuscular coordination. Combined interventions yield better outcomes than single-modality approaches.
Managing Pain, Fibrosis, and Pelvic Discomfort
Men may also experience pelvic pain, scar adhesions, muscle hypertonicity, or radiation-induced fibrosis, which can interfere with mobility and rehabilitation adherence. Pelvic rehabilitation addresses these challenges through manual therapy, myofascial release, scar mobilization, neural desensitization, stretching, and relaxation techniques. A holistic approach ensures that pain and fibrosis do not amplify guarding or disrupt neuromuscular coordination, allowing patients to regain functional independence.
Integrating Rehabilitation into Recovery
Prehabilitation by initiating pelvic floor training before surgery can “prime” the neuromuscular system, improving early outcomes. Interventions should be individualized, taking into account anatomy, treatment modality, and comorbidities. Functional progression from isolated contractions to daily activities ensures that strength and coordination translate into meaningful improvements in continence, sexual function, and mobility.
Interdisciplinary collaboration with urologists, radiation oncologists, sexual medicine specialists, psychologists, and nurses enhances recovery, supports timely referrals, and addresses psychosocial aspects of treatment. Realistic expectations and patient education about recovery timelines are critical; while continence may return within months, sexual function may take longer.
Case Example: A 62-year-old man undergoing nerve-sparing robotic prostatectomy began PFMT preoperatively and continued structured pelvic rehabilitation postoperatively. Eight weeks after surgery, he initiated penile rehabilitation with PDE5 inhibitors and vacuum devices alongside ongoing PFMT. At six months, he regained urinary continence, and by 12 months reported meaningful improvements in erectile function. This phased, individualized approach exemplifies how rehabilitation supports functional recovery and quality of life.
Conclusion
Prostate cancer treatment affects multiple systems: neuromuscular, vascular, connective tissue, and psychological. Pelvic rehabilitation offers structured strategies to address urinary incontinence, erectile dysfunction, pelvic pain, and mobility deficits. By combining PFMT, penile rehabilitation, manual therapy, and individualized functional progression, rehabilitation professionals play a crucial role in helping men regain independence and confidence.
This two-day course focuses on male pelvic cancers, including prostate, penile, and testicular cancers, as well as colorectal and anal cancers. Participants will learn about diagnosis, prognosis, medical treatment sequelae, rehabilitation strategies, nutritional considerations, and home program interventions. Hands-on labs provide immediate application of skills, and participants must register with a partner or arrange a volunteer for rectal and perineal exams. Register today to expand your clinical expertise and elevate the care you provide to men recovering from pelvic cancers.
References:
- Nicolai, M., Urkmez, A., Sarikaya, S., Fode, M., Falcone, M., Albersen, M., Gul, M., Hatzichristodoulou, G., Capogrosso, P., & Russo, G. I. (2021). Penile Rehabilitation and Treatment Options for Erectile Dysfunction Following Radical Prostatectomy and Radiotherapy: A Systematic Review. Frontiers in Surgery, 8, 636974. https://doi.org/10.3389/fsurg.2021.636974
- Al Hussein Al Awamlh B, Wallis CJD, Penson DF, et al. Functional Outcomes After Localized Prostate Cancer Treatment. JAMA. 2024; 331(4): 302–317. doi:10.1001/jama.2023.26491. https://jamanetwork.com/journals/jama/fullarticle/2814131
- Milios, J.E., Ackland, T.R. & Green, D.J. Pelvic floor muscle training in radical prostatectomy: a randomized controlled trial of the impacts on pelvic floor muscle function and urinary incontinence. BMC Urol 19, 116 (2019). https://doi.org/10.1186/s12894-019-0546-5
- Milios JE, Ackland TR, Green DJ. Pelvic Floor Muscle Training and Erectile Dysfunction in Radical Prostatectomy: A Randomized Controlled Trial Investigating a Non-Invasive Addition to Penile Rehabilitation. Sex Med. 2020 Sep; 8 (3): 414-421. doi: 10.1016/j.esxm.2020.03.005. Epub 2020 May 14. PMID: 32418881; PMCID: PMC7471070. https://pmc.ncbi.nlm.nih.gov/articles/PMC7471070/
- Newman, D. (2024, December 9). Pelvic muscle rehabilitation after radical prostatectomy. UroToday. https://www.urotoday.com/video-lectures/localized-prostate-cancer/video/4446-pelvic-muscle-rehabilitation-after-radical-prostatectomy-diane-newman.html

Over the last few years, a growing body of studies has expanded our understanding of male pelvic floor dysfunction and refined the approach to treatment within pelvic rehabilitation. The latest evidence supports a multifaceted, neuro-muscular strategy grounded in early intervention, individualized care, and integration of tools like electrical stimulation and manual therapy. Below, are a few key findings that are reshaping clinical protocols and outcomes in male pelvic rehab.
Post-Prostatectomy Urinary Incontinence
Pelvic floor muscle training (PFMT) remains the first-line therapy for post-prostatectomy incontinence (PPI). A 2022 meta-analysis by Park et al, involving 21 randomized controlled trials, found that PFMT nearly tripled continence rates compared to no PFMT. Patients also showed significant improvements in both objective measures (e.g., pad counts) and subjective continence scores.
While long-term benefits are well established, recent research emphasizes the importance of early initiation. Multiple studies support beginning PFMT preoperatively or immediately postoperatively to optimize outcomes, particularly after nerve-sparing robotic-assisted radical prostatectomy. Timed, progressive PFMT, especially when started early, is essential for maximizing continence recovery, even more so in cases involving nerve-sparing approaches that may affect pelvic floor coordination.
Combining PFMT with Electrical Stimulation
A 2025 meta-analysis by Lunardi et al examined 885 female patients and found that pelvic floor muscle training (PFMT) combined with electrical stimulation significantly outperformed PFMT alone in improving continence, pelvic floor strength, and quality of life. However, these findings are limited to women and do not directly translate to male populations.
In contrast, evidence in male patients, particularly those with post-prostatectomy incontinence, is more mixed. A randomized, placebo-controlled trial by Yamanishi et al. in 2010 that involved 56 men found that PFMT combined with anal electrical stimulation significantly improved continence rates during the early recovery period (1–6 months) compared to “sham” stimulation. However, by 12 months, the difference between groups was no longer statistically significant, suggesting that the benefits may be short-term.
While adjunctive electrical stimulation appears to provide early benefit in some men, especially those with severe leakage or poor initial voluntary contraction, the long-term advantage remains uncertain. Patients with limited neuromuscular control may benefit from neuromuscular electrical stimulation (NMES) to enhance recruitment and early adherence, but expectations should be managed regarding sustained continence outcomes beyond the first 6–12 months.
Pelvic Floor Therapy for Sexual Dysfunction
Emerging literature from Pastore et al. (2021) supports pelvic rehab in the management of erectile dysfunction, premature ejaculation, and chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). Integration of manual therapy, PFMT, and behavioral retraining has yielded meaningful gains in function and reduction in nociceptive signaling.
A 2024 study utilizing High-Intensity Focused Electromagnetic (HIFEM) therapy further points to new frontiers in non-invasive intervention for erectile dysfunction and male urinary control.
These findings highlight the evolving role of pelvic floor therapy as a cornerstone in the multidisciplinary management of male sexual dysfunction. Whether through traditional rehabilitation approaches—such as PFMT, manual therapy, and behavioral retraining—or through emerging technologies like HIFEM, pelvic health interventions demonstrate tangible benefits in improving sexual function, alleviating pelvic pain, and restoring urinary control.
Clinical Patterns Worth Noting
In clinical practice, several common patterns emerge when treating male pelvic floor dysfunction. Patients with chronic pelvic pain frequently present with pelvic floor overactivity, often accompanied by restrictions in the obturator internus, adductor magnus, and piriformis muscles. This hypertonicity is commonly associated with neural sensitization and can be exacerbated by postural imbalances or stress-related bracing strategies.
Men recovering from prostatectomy may exhibit compensatory recruitment of accessory muscles, such as the gluteal and abdominal muscles, due to impaired pelvic floor motor control. This can reduce the effectiveness of voluntary pelvic floor muscle contractions and contribute to persistent urinary leakage despite exercise adherence. Thorough neuromuscular re-education is often required to facilitate isolated pelvic floor activation and restore continence.
Erectile dysfunction in this population is frequently compounded by contributing factors such as pelvic asymmetry, altered respiratory diaphragm coordination, and increased thoracolumbar tension. These findings emphasize the importance of a whole-body biomechanical and neuro-myofascial assessment, as pelvic floor dysfunction in men rarely presents in isolation. Recognizing and addressing these interrelated impairments is key to achieving lasting functional outcomes.
August Satellite Lab: Pelvic Function Level 2C
Herman & Wallace invites you to refine your clinical reasoning and hands-on skills at the upcoming Pelvic Function Level 2C Satellite Lab Course, held August 16–17.
This intermediate-level course emphasizes:
- Recognizing the key signs and symptoms that lead to impairment, functional limitations, and disabilities in men’s health
- Use of an evaluation/outcome tool relating to patient condition(s)
- Designing a multi-modal plan of care for pelvic rehabilitation
- Performing clinical interventions based on the patient's presentation and goals
Clinical treatment interventions include patient education, neuro re-education, therapeutic exercise, manual therapy, therapeutic activities, instruction in self-care, and recommendations for relevant modalities.
It’s essential that pelvic rehabilitation continues to evolve beyond the historically female-centered framework to address the full spectrum of pelvic dysfunction, including the complex needs of male patients. Evidence indicates that targeted, neuromuscular-driven rehabilitation strategies can significantly improve outcomes for men experiencing urinary, sexual, and pain-related pelvic conditions.
The August course is available in 9 different satellite locations as well as self-hosted. Satellite locations for Pelvic Function Level 2C: Men’s Pelvic Health and Rehabilitation include:
-
 Columbus OH
Columbus OH - Danvers MA
- Katy TX
- Milwaukee WI
- New Orleans LA
- New York NY
- Palm Beach FL
- Paso Robles CA
- Tacoma WA
- Self-Hosted
References
- Park JJ, Kwon A, Park JY, Shim SR, Kim JH. Efficacy of Pelvic Floor Exercise for Post-prostatectomy Incontinence: Systematic Review and Meta-analysis. 2022 Oct;168:175-182. doi: 10.1016/j.urology.2022.04.023. Epub 2022 May 5. PMID: 35526757. https://pubmed.ncbi.nlm.nih.gov/35526757/
- Lunardi AC, Foltran GC, Carro DF, Silveira LTY, Haddad JM, Ferreira EAG. Efficacy of electrical stimulation in comparison to active training of pelvic floor muscles on stress urinary incontinence symptoms in women: a systematic review with meta-analysis. Disabil Rehabil. 2025 Jun;47(13):3256-3267. doi: 10.1080/09638288.2024.2419424. Epub 2024 Oct 28. PMID: 39467254. https://pubmed.ncbi.nlm.nih.gov/39467254/
- Yamanishi T, Mizuno T, Watanabe M, Honda M, Yoshida K. Randomized, placebo-controlled study of electrical stimulation with pelvic floor muscle training for severe urinary incontinence after radical prostatectomy. J Urol. 2010 Nov;184(5):2007-12. doi: 10.1016/j.juro.2010.06.103. Epub 2010 Sep 20. PMID: 20850831. https://pubmed.ncbi.nlm.nih.gov/20850831/
- Pastore AL, Palleschi G, Fuschi A, Maggioni C, Rago R, Zucchi A, Costantini E, Carbone A. Pelvic floor muscle rehabilitation for patients with lifelong premature ejaculation: a novel therapeutic approach. Ther Adv Urol. 2014 Jun;6(3):83-8. doi: 10.1177/1756287214523329. PMID: 24883105; PMCID: PMC4003840. https://pmc.ncbi.nlm.nih.gov/articles/PMC4003840/
- Yaacov D, Nelinger G, Kalichman L. The Effect of Pelvic Floor Rehabilitation on Males with Sexual Dysfunction: A Narrative Review. Sex Med Rev. 2022 Jan;10(1):162-167. doi: 10.1016/j.sxmr.2021.02.001. Epub 2021 Apr 27. PMID: 33931383. https://pubmed.ncbi.nlm.nih.gov/33931383/
- Brandeis J. Improving Male Pelvic Health: Efficacy of HIFEM Muscle Stimulation for Urinary Function and Sexual Dysfunction in Men. Reproductive System & Sexual Disorders: Current Research. Research Article. 2024; 13(1). ISSN: 2161-038X. https://www.longdom.org/open-access/improving-male-pelvic-health-efficacy-of-hifem-muscle-stimulation-for-urinary-function-and-sexual-dysfunction-in-men-106497.html
Often pelvic floor therapists see men for post-prostatectomy urinary leakage. However, at least for me, that quickly led to seeing male patients for pelvic pain and sexual dysfunction. Male sexual dysfunction is a broad category and can consist of erectile dysfunction (ED), ejaculation disorders including premature ejaculation (PE), and low libido -- often there is a pelvic floor muscle (PFM) dysfunction component. Conservative treatment frequently consists of pharmacological and lifestyle changes for this population.
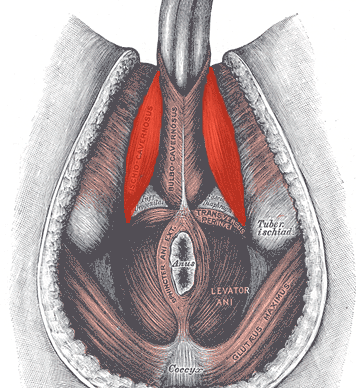
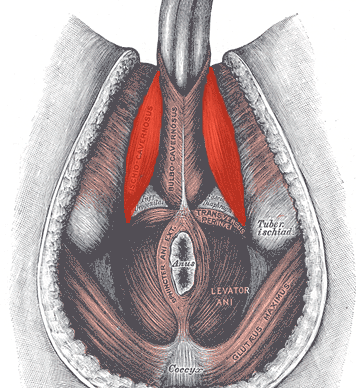
In normal sexual function, the male superficial pelvic floor musculature (bulbocavernosus and ischiocavernosus) work together to create increased intracavernosus pressure by limiting venous return, resulting in an erection. Ejaculation is created by rhythmic contractions of the bulbocavernosus muscle.
 The authors of this systematic review were curious if pelvic floor muscle training was effective for treating erectile dysfunction and premature ejaculation diagnoses, and if so to determine whether there is a treatment protocol. Ten studies were found that met the inclusion criteria, five that focused on ED and five that focused on PE. In total, there were 668 participants ranging in age from 30-59 years old. Studies were excluded if participants were post-prostatectomy and/or had a neurological diagnosis. The intervention was a pelvic floor program, and pelvic floor muscle contractions were either taught or supervised. Studies also included supportive treatment including biofeedback, lifestyle changes, and electrical stimulation.
The authors of this systematic review were curious if pelvic floor muscle training was effective for treating erectile dysfunction and premature ejaculation diagnoses, and if so to determine whether there is a treatment protocol. Ten studies were found that met the inclusion criteria, five that focused on ED and five that focused on PE. In total, there were 668 participants ranging in age from 30-59 years old. Studies were excluded if participants were post-prostatectomy and/or had a neurological diagnosis. The intervention was a pelvic floor program, and pelvic floor muscle contractions were either taught or supervised. Studies also included supportive treatment including biofeedback, lifestyle changes, and electrical stimulation.
The studies focused on erectile dysfunction listed a combination of hormonal, psychogenic, arteriogenic, and venogenic causes. The pelvic floor training ranged from 5-20 visits over 3-4 months and included a home exercise program. Pelvic floor training was similar in all studies and consisted of maximal quick contractions over one second and submaximal endurance holds over 6-10 seconds. Compliance to home exercise program was not assessed. Between 35% and 47% of participants reported a full resolution of symptoms. Subjective improvements were supported by improved maximal anal pressure and intracavernosus pressure. One study used the International Index of Erectile Function (IIEF) and showed significant improvement (p<0.05).
The studies focused on premature ejaculation noted participants had either lifelong or secondary PE. The pelvic floor training in these studies ranged from 12-20 sessions over 1-3 months. All studies used electrical stimulation as part of the pelvic floor muscle training. Four studies also used biofeedback. Only one study listed a home exercise program but did not report on compliance. The pelvic floor muscle training was compared to nothing in three studies, and to a selective serotonin reuptake inhibitor (SSRI) in the other two studies. Patient reported full resolution of symptoms was 55-83% in two studies, and there was a significant improvement in delay in heterosexual penetrative ejaculation (p<0.05) in three studies.
For both erectile dysfunction and premature ejaculation, pelvic floor muscle exercise prescription was 2-3 times per week with pelvic floor muscle contractions both maximal quick contractions and submaximal endurance holds. Significant results were shown with participants who were taught pelvic floor muscle contractions through a combination of verbal and physical means (typically biofeedback). Specific verbal cues were not reported. The authors suggest that electrical stimulation was helpful for training recruitment patterns; however, there was not a significant difference in outcomes for those with ED when using electrical stimulation. The authors suggest that pelvic floor muscle training can be part of a conservative treatment. It may be used with oral pharmacology for quick results, and may be beneficial with electrical stimulation and biofeedback, though more research is indicated.
If you are interested in learning more about treating male patients, consider attending Male Pelvic Floor: Function, Dysfunction, and Treatment!
Myers, C., Smith, M. “Pelvic floor muscle training improves erectile dysfunction and premature ejaculation: a systematic review” Physiotherapy 105 (2019) 235–243