Sacroiliac joint pain can be a challenging condition to treat. One of the clinical pearls that I feel changed my practice for the better is the palpation and direct treatment of the dorsal sacral ligament. At a course many years ago, I listened to Diane Lee describing Andry Vleeming's work addressing the potential role of the long dorsal sacral ligament (LDL) in pelvic pain. His valuable research was conducted on women who had complaints of peripartum pain, and it has been my experience that the information is easily extrapolated to other patient populations.
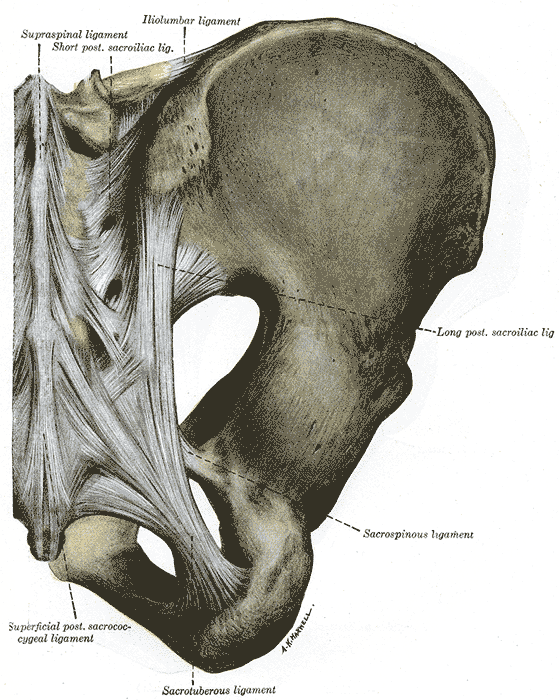
Vleeming and colleagues describe the long dorsal sacroiliac ligament anatomy as attaching to the lateral crest of the 3rd and 4th sacral segments (and sometimes to the 5th segment), and as having connections to the aponeurosis of the erector spine group, the thoracolumbar fascia, and the sacrotuberous ligament. Functionally, nutation in the sacroiliac joint will slacken the ligamentous tension in the LDL and counternutation will tension the ligament. This structure can be palpated directly caudal to the posterior superior iliac spine (PSIS).
The referenced study examined women who had tenderness in the LDL and were also diagnosed with peripartum pelvic pain. Patients included in the study had pain in the lumbopelvic region, pain beginning with pregnancy or within 3 weeks of childbirth, were not pregnant at the time of the study, and were between the ages of 20-40. In patients with peripartum pelvic pain, 76% of the women reported tenderness in the LDL- this number increased to 86% when only patients scoring positively on the active straight leg raise test and posterior pelvic pain provocation (PPPP) test were included.
The study proposes that strain in the LDL may occur from a counter-stated sacrum and/or an anterior pelvic tilt position. In my clinical experience and as instructed to many pelvic health therapists by expert clinicians such as Diane Lee, balancing the pelvic structures, activating stabilizing muscles of the inner core (pelvic floor, multifidi, transverses abdominis), and addressing soft tissue dysfunction in the ligament frequently resolve long-standing localized pain in the sacroiliac joint area. The authors of the study conclude that "…knowledge of the anatomy and function of the LDL and the simple use of a pain provocation test…could help gain a better understanding of peripartum pelvic pain." They also reported that combining tests such as the ASLR, the PPPP test, and the long dorsal sacral ligament palpation test "seems promising" in the differentiation of patients categorized as having pelvic pain versus lumbar pain.
To learn more about sacroiliac joint anatomy and function, diagnosis, and treatment then sign up for Steve DIschiavi's upcoming remote course Sacroiliac Joint Current Concepts scheduled for August 4, 2024.
Reference:
1. Vleeming A, de Vries HJ, Mens JM, van Wingerden JP. Possible role of the long dorsal sacroiliac ligament in women with peripartum pelvic pain. Acta Obstet Gynecol Scand. 2002 May;81(5):430-6. doi: 10.1034/j.1600-0412.2002.810510.x. PMID: 12027817.
Diagnosing sacroiliac joint (SIJ) dysfunction can be tricky. Therapists need to rule out lumbar spine and the hip, and sometimes there is more than one area causing pain and limiting functional mobility. Typically, ruling in SIJ dysfunction is done by pain provocation tests and load transfer tests. Once the SIJ has been ruled in, then therapists can use a variety of treatments. Often those treatments include therapeutic exercise, joint manipulation, and Kinesio tape. But which intervention is the most effective?
A recent study looked at three physical therapy interventions for treatment for SIJ (sacroiliac joint) dysfunction and assessed which was the most effective (Al-Subahi, M 2017). The authors did a systematic review of the literature. The articles were from 2004-2014, written in English, with male and female participants. This review included a variety of experiment types from randomized control trials to case studies. Of the 1114 studies, only 9 met the inclusion and exclusion criteria. Four of the nine studies used manipulation, three used Kinesio Tape, and the three used exercise. One study did both exercise and manipulation, and was looked at in both interventions. All categories had at least one randomized control trial.
For the manipulation intervention, all studies showed a decrease in pain and disability at follow up. The follow ranged from 3 to 4 days to 8 weeks. Disability was measured using the Oswestry Disability Index. One study did manual high velocity and low amplitude thrust manipulation to lumbar and SIJ manipulation and showed improvement with manipulation to SIJ or SIJ and lumbar. The review did not disclose the type of lumbar manipulation, but did state the SIJ manipulation was a side bend and rotation position with an inferior and lateral force to ASIS (anterior superior iliac spine). Another study did either a SIJ manual high velocity and low amplitude thrust manipulation or a mechanical force with manual assistance. One studied did manipulation and home exercises but did not record exercise interventions. The last study did the same SIJ manual high velocity and low amplitude thrust manipulation as in previous study combined with exercise. The exercises are mentioned below.
For the exercise intervention, the studies did primarily stabilization exercises that were either isometric or isotonic eccentric or concentric. Quick PT school review, in isometric exercises the muscle does not change length, while in isotonic eccentric exercises the muscle is being lengthened under load, and isotonic concentric is the muscle shortening under load. All three studies showed decrease in pain. The first study had 7 participants and combined manipulation and exercise. The exercises consisted of 12% max voluntary contraction and eccentric loading quads in supine with hips at 90 degrees, and concentrically loading hamstrings in prone. The second study was a case study and performed 8 lumbo-pelvic-femoral stabilization exercises for 8 weeks. Fun fact: this case study was written by my Therapeutic Exercise teacher in PT school who did a lot of Postural Restoration based exercises. The last study, had 22 participants and educated and provided exercises on deep abdominal and multifidus muscles and do complete these exercises during functional movements throughout the day. These participants were follow up a year later and had decreased pain compared to laser group.
For the Kinesio tape (Kinesio tape) intervention, the studies did not find that Kinesio tape was not an effective intervention, however the follow up ranged from immediately after applying tape to 4 weeks afterwards. In the first study, a randomized controlled trial with 60 participants, the Kinesio tape was applied in sitting with 25% tension of 4 strips making a star pattern over the point of maximal pain. The Kinesio tape was compared to placebo tape and showed equal improvement in pain and disability. The other two studies applied a different taping technique where the Kinesio tape was applied. One applied the tape over erector spinae and internal oblique muscles bilaterally and in the other study the Kinesio tape was applied with 25% tension over external obliques, a second strip was placed from ASIS to PSIS in side-lying, and then a third strip was placed along rectus abdominis muscle. In this same study the tape was applied for weeks (6x/week for 9 hours/day).
In summary, the authors note that all three interventions help decrease pain and disability in women and men with SIJ dysfunction. The authors suggest that manipulation may be the most effective. Kinesio tape showed no significant difference between placebo tape. Exercise was effective, but less so than manipulation.
This review has a lot of limitations. The variety of experiment types with varying degrees of evidence, small number of participants, and lack of blinding. Most studies had a limited follow up ranging from 3-4 days to 12 months. The outcome measures varied greatly. Most studies had pain scores as the outcome measure, though one study only used inclination meter of anterior pelvic tilt. Use of a consistent objective measure in addition to perceived pain and disability would have helped. Only 1 study did pain provocation tests and that study was a case study whose intervention focused on Kinesio-taping.
As physical therapists we want to provide effective evidence-based practice, and we want to provide individualized compassionate care. It is hard to make a direct line between this study’s recommendations and clinical application based on the numerous limitations. I agree with the authors that manipulation and exercise are bread and butter to physical therapists. I disagree about Kinesio tape not being an effective treatment. Is Kinesio tape going to create boney alignment changes? Likely not. Is Kinesio tape (or any other tape) going to give proprioceptive feedback and possibly help calm sensory pathways? Yes. If a patient likes being taped, and thinks it will help, then I will tape them. Even if taping is just placebo effect; it’s still an effect.
Al-Subahi, M., Alayat, M., Alshehr, M.A., et al. (2017) The effectiveness of physiotherapy interventions for sacroiliac joint dysfunction: A systematic review. J Phys. Ther. Sci. 29: 1689-1694.
Consider combing long, curly hair. Untangling the top layer is not so bad, but once half the hair is tamed, there is often a mangled mess lurking underneath. Sometimes the lumbar spine gets all the primping to relieve pain, but the sacroiliac joint is harboring the knots, such as when a lumbar rhizotomy leaves a patient’s satisfaction a little fuzzy.
 A 2017 study by Rimmalapudi and Kumar investigated the incidence of sacroiliac (SI) joint dysfunction being diagnosed in patients after undergoing lumbar radiofrequency rhizotomy of the medial branches of lower lumbar dorsal rami for chronic facet-mediated low back pain. The authors used a retrospective chart review of 96 patients who had the procedure performed, and 50 subjects responded to the 2 follow ups and were included in the study. Their choice of control was a limitation in this study, as they compared the results to a different study (DePalma et al., 2011) with a similar population that did not have the lumbar rhizotomy performed. Of the 50 patients (66% female, 34% male), 35 (70%) were subsequently diagnosed with SI joint pain; whereas, in the comparison study, only 18% of the patients had SI pain. The assessment of SI dysfunction in this study was by clinical exam, and the DePalma et al. study used diagnostic tests. The authors concluded the following: clinicians should suspect underlying SI joint pain post-lumbar rhizotomy; careful evaluation of the SI joint should be performed pre and post procedure; and, diagnostic joint blocks should be performed to confirm SI dysfunction. They suggested using criteria of 80-100% relief as opposed to the currently accepted >50% after a diagnostic facet block because residual pain from an underlying condition may arise after lumbar rhizotomy.
A 2017 study by Rimmalapudi and Kumar investigated the incidence of sacroiliac (SI) joint dysfunction being diagnosed in patients after undergoing lumbar radiofrequency rhizotomy of the medial branches of lower lumbar dorsal rami for chronic facet-mediated low back pain. The authors used a retrospective chart review of 96 patients who had the procedure performed, and 50 subjects responded to the 2 follow ups and were included in the study. Their choice of control was a limitation in this study, as they compared the results to a different study (DePalma et al., 2011) with a similar population that did not have the lumbar rhizotomy performed. Of the 50 patients (66% female, 34% male), 35 (70%) were subsequently diagnosed with SI joint pain; whereas, in the comparison study, only 18% of the patients had SI pain. The assessment of SI dysfunction in this study was by clinical exam, and the DePalma et al. study used diagnostic tests. The authors concluded the following: clinicians should suspect underlying SI joint pain post-lumbar rhizotomy; careful evaluation of the SI joint should be performed pre and post procedure; and, diagnostic joint blocks should be performed to confirm SI dysfunction. They suggested using criteria of 80-100% relief as opposed to the currently accepted >50% after a diagnostic facet block because residual pain from an underlying condition may arise after lumbar rhizotomy.
Stelzer et al., (2017) published another retrospective study on lumbar neurotomy or SI joint lateral branch cooled radiofrequency (RF) neurotomy, looking at pain reduction and medication decrease, depending on BMI, gender, and sports. Facet-mediated pain is accountable for 31-45% of low back pain, and 18-30% is SI joint mediated. The study started with 160 patients who had undergone procedures, and Visual Analog Scale (VAS) pain scores, quality of life, BMI, medication use, and pain management satisfaction were assessed before, 1 month after (n=160), 6 months after (n=73), and 12 months (n=89) after treatment. Group 1 (n=43) had neurotomy of the medial branch of L4-5 and L5-S1 facet joint, medial branch L3 and L4, and dorsal ramus L5. Group 2 (n=109) received cooled RF treatment of the SIJ, SIJ lateral branch of the posterior rami S1–S3, and rami dorsalis of L5. Group 3 (n=8) had various areas treated according to their disease process. The authors determined from these treatments that a 95% probability of significant pain reduction could last 12 months; medication usage decreased; lower BMI had slightly better results than >30BMI; no significant difference between males and females; and, involvement in sports 1-3 times a week for 30 minutes showed improvement in quality of life.
These studies prove we need to evaluate our lumbar and sacroiliac joint patients as thoroughly as possible in order to avoid unnecessary procedures or at least to help direct the treatment to the appropriate area. We should always equip ourselves with knowledge of medical procedures our patients may undergo and expand our own clinical competence and skill. Patients benefit from what is inside our heads and how we use it, not how well-groomed our hair appears.
Rimmalapudi, V. K., & Kumar, S. (2017). Lumbar Radiofrequency Rhizotomy in Patients with Chronic Low Back Pain Increases the Diagnosis of Sacroiliac Joint Dysfunction in Subsequent Follow-Up Visits. Pain Research & Management, 2017, 4830142. http://doi.org/10.1155/2017/4830142
M. J. DePalma, J. M. Ketchum, and T. Saullo. (2011). What is the source of chronic low back pain and does age play a role? Pain Medicine. 12(2), 224–233.
Stelzer, W., Stelzer, V., Stelzer, D., Braune, M., & Duller, C. (2017). Influence of BMI, gender, and sports on pain decrease and medication usage after facet–medial branch neurotomy or SI joint lateral branch cooled RF-neurotomy in case of low back pain: original research in the Austrian population. Journal of Pain Research, 10, 183–190. http://doi.org/10.2147/JPR.S121897
In this “quick fix” society, few people accept that musculoskeletal pain will require a commitment to following an exercise program for an extended period of time. If a hypomobile joint just needs to get moving and lubricated, one may get relief with a few manual therapy treatments and exercise sessions. However, if a joint is hypermobile (unstable) or degenerative and provokes a high level of pain, the rehab requires more time. The sacroiliac (SI) joint is one of those areas often requiring patients to work harder for the resolution of pain and dysfunction, but many seek surgical intervention instead.
 Polly et al. (2016) performed a randomized controlled trial of minimally invasive sacroiliac joint fusion (SIJF) with placement of a system of triangular titanium implants using a lateral transiliac approach versus non-surgical management (NSM) for SI dysfunction. Of the 148 subjects, 102 underwent SIJF and 46 had NSM. The NSM group received medication, physical therapy per American Physical Therapy Association guidelines, steroid injections and radiofrequency ablation of sacral nerve root lateral branches. The surgical group showed superior outcomes at a 2 year follow up, as clinical improvement per VAS pain score was 83.1% and ODI was 68.2%. The NSM group showed <10% improvement.
Polly et al. (2016) performed a randomized controlled trial of minimally invasive sacroiliac joint fusion (SIJF) with placement of a system of triangular titanium implants using a lateral transiliac approach versus non-surgical management (NSM) for SI dysfunction. Of the 148 subjects, 102 underwent SIJF and 46 had NSM. The NSM group received medication, physical therapy per American Physical Therapy Association guidelines, steroid injections and radiofrequency ablation of sacral nerve root lateral branches. The surgical group showed superior outcomes at a 2 year follow up, as clinical improvement per VAS pain score was 83.1% and ODI was 68.2%. The NSM group showed <10% improvement.
Sachs et al. (2016) studied outcomes of patients ≥3 years after SIJF for chronic (>5 years) SIJ dysfunction secondary to degenerative sacroiliitis or SIJ disruption. One hundred and seven patients participated in the study, and minimally invasive transiliac SIJF was definitively correlated with decreased pain, low disability scores, and improvements in activities of daily living performance. Sadly, these authors stated, “there is no high-quality evidence that physical therapy is effective in chronic SIJ pain.”
Even radiofrequency neurotomy or neural ablation revealed positive results for patients according to Reddy et al. (2016). The authors explored 14 patients’ responses 1 year after Simplicity radiofrequency (RF) of the lateral branches of S1-S3 in a retrospective review. Improvements in global health per SF12 as well as pain reduction were statistically significant.
Jonely et al. (2015) presented a case study of a woman with a 14-year history of SIJ pain whose symptoms persisted after 2 months of physical therapy. A multi-modal approach was then pursued with success, even at the 1 year follow up. The patient received 4 prolotherapy injections, SIJ manipulation into nutation, a pelvic girdle belt, and specific stabilization exercises. Over a 12-month period, the patient had 20 physical therapy sessions. Her Oswestry Disability score improved from 34% to 14% at 6 months and was 0% at 1 year. Numeric pain scale rating improved to 4/10 at 6 months and 0/10 at 1 year. The authors concluded a multimodal approach can be successful to manage SIJ dysfunction.
Clearly, if quality of life is so poor a person cannot function because of SIJ pain and therapy has failed, surgery may be the only choice. I exhaust all conservative measures before I cry “uncle” for a surgical fix. Despite a paucity of literature on manual therapy and sacroiliac treatment, I know there are clinicians successfully treating patients with SI dysfunction. Taking the Sacroiliac Joint Evaluation and Treatment can broaden your scope of understanding the SI joint and how to provide the most effective treatment, possibly preventing more invasive techniques for patients.
Polly, D. W., Swofford, J., Whang, P. G., Frank, C. J., Glaser, J. A., Limoni, R. P., … and the INSITE Study Group. (2016). Two-Year Outcomes from a Randomized Controlled Trial of Minimally Invasive Sacroiliac Joint Fusion vs. Non-Surgical Management for Sacroiliac Joint Dysfunction. International Journal of Spine Surgery, 10, 28. http://doi.org/10.14444/3028
Sachs, D., Kovalsky, D., Redmond, A., Limoni, R., Meyer, S. C., Harvey, C., & Kondrashov, D. (2016). Durable intermediate-to long-term outcomes after minimally invasive transiliac sacroiliac joint fusion using triangular titanium implants. Medical Devices (Auckland, N.Z.), 9, 213–222. http://doi.org/10.2147/MDER.S109276
Anjana Reddy, V. S., Sharma, C., Chang, K.-Y., & Mehta, V. (2016). “Simplicity” radiofrequency neurotomy of sacroiliac joint: a real life 1-year follow-up UK data. British Journal of Pain, 10(2), 90–99. http://doi.org/10.1177/2049463715627287
Jonely, H., Brismée, J.-M., Desai, M. J., & Reoli, R. (2015). Chronic sacroiliac joint and pelvic girdle dysfunction in a 35-year-old nulliparous woman successfully managed with multimodal and multidisciplinary approach. The Journal of Manual & Manipulative Therapy, 23(1), 20–26. http://doi.org/10.1179/2042618614Y.0000000086
Pain with sitting is a common complaint that patients may present to the clinic with. While excess sitting has been shown to be detrimental to the human body, sitting is part of our everyday culture ranging from sitting at a meal, traveling in the car, or doing work at a desk. Often, physical therapists disregard the coccyx or tailbone as the possible pain generator, simply because they are fearful of assessing it, have no idea where it is, or have never learned about it being a pain generator in their education.
Coccydynia is the general term for “pain over the coccyx.” Patients with coccydynia will complain of pain with sitting or transitioning from sit to stand. Despite the coccyx being such a small bone at the end of the spine, it serves as a large attachment site for many important structures of interest that are important in pelvic floor support and continence: ¹
- Anterior: Levator ani muscles, Sacrococcygeal ligament
- Lateral: Coccygeal muscles, Sacrospinous ligament, Sacrotuberous ligament, Glute maximus muscle fibers
- Inferiorly: Iliococcygeus
 Along with serving as a major attachment site for the above structures it provides a support for weightbaring in the seated position and provides structural support for the anus. Women are five times more likely to develop coccydynia than men, with the most common cause being an external trauma like a fall, or an internal trauma like a difficult childbirth. 1,2 In a study of 57 women suffering from postpartum coccydynia, most deliveries that resulting in coccyx pain were from use of instruments such as a forceps delivery or vacuum assisted delivery. A BMI over 27 and having greater than or equal to 2 vaginal deliveries resulted in a higher rate of coccyx luxation during birth. ³ Other causes of coccyx pain can be non traumatic such as rapid weight loss leading to loss of cushioning in sitting, hypermobility or hypomobility of the sacrococcygeal joint, infections like a pilonidal cyst, or pelvic floor muscle dysfunction. ¹ When assessing a patient with coccyx pain, it is also of the upmost importance to rule out red flags, as there are multiple cases cited in the literature of tumors such as retrorectal tumors or cysts being the cause of coccyx pain. These masses must be examined by a doctor to determine if they are malignant or benign, and if excision is necessary. Sometimes these masses can be felt as a bulge on rectal examination. 4,5
Along with serving as a major attachment site for the above structures it provides a support for weightbaring in the seated position and provides structural support for the anus. Women are five times more likely to develop coccydynia than men, with the most common cause being an external trauma like a fall, or an internal trauma like a difficult childbirth. 1,2 In a study of 57 women suffering from postpartum coccydynia, most deliveries that resulting in coccyx pain were from use of instruments such as a forceps delivery or vacuum assisted delivery. A BMI over 27 and having greater than or equal to 2 vaginal deliveries resulted in a higher rate of coccyx luxation during birth. ³ Other causes of coccyx pain can be non traumatic such as rapid weight loss leading to loss of cushioning in sitting, hypermobility or hypomobility of the sacrococcygeal joint, infections like a pilonidal cyst, or pelvic floor muscle dysfunction. ¹ When assessing a patient with coccyx pain, it is also of the upmost importance to rule out red flags, as there are multiple cases cited in the literature of tumors such as retrorectal tumors or cysts being the cause of coccyx pain. These masses must be examined by a doctor to determine if they are malignant or benign, and if excision is necessary. Sometimes these masses can be felt as a bulge on rectal examination. 4,5
A multidisciplinary approach including physical therapy, ergonomic adaptations, medications, injections, and, possibly, psychotherapy leads to the greatest chance of success in patients with prolonged coccyx pain. 1 Special wedge shaped sitting cushions can provide relief for patients in sitting and help return them to their social activities during treatment. Physical therapy includes manual manipulation and internal work to the pelvic floor muscles to alleviate internal spasms and ligament pain. Intrarectal coccyx manipulation can potentially realign a dislocated sacrococcygeal joint or coccyx. 1 Taping methods can be used as a follow up to coccyx manipulation to help hold the coccyx in the new position and allow for optimal healing. Often coccyx pain patients have concomitant pathologies such as pelvic floor muscle dysfunction, sacroilliac or lumbar spine pain, and various other orthopedic findings that are beneficial to address. When conservative treatments fail, injections or a possible coccygectomy may be considered.
Luckily conservative treatment is successful in about 90% of cases. ¹ All of the above conservative tools will be taught in the upcoming Coccyx Pain Evaluation and Treatment course on April 23-24th, 2016 in Columbia, MO taught by Lila Abbate PT, DPT, OCS, WCS, PRPC. By learning how to treat coccyx pain appropriately, you will be a key provider in solving many unresolved sitting pain cases that are not resolved with traditional orthopedic physical therapy.
1. Lirette L, Chaiban G, Tolba R, et al. Coccydynia: An overview of the anatomy, etiology, and treatment of coccyx pain. The Ochsner Journal. 2014; 14:84-87.
2. Marinko L, Pecci M. Clinical Decision Making for the Evaluation and Management of Coccydynia: 2 Case Reports. JOSPT. 2014; 44(8): 615
3. Maigne JY, Rusakiewicz F, Diouf M. Postpartum coccydynia: a case series study of 57 women. Eur J Phys Rehabil Med. 2012; 48 (3): 387-392.
4. Levine R, Qu Z, Wasvary H. Retrorectal Teratoma. A rare cause of pain in the tailbone. Indian J Surg. 2013; 75(2): 147-148.
5. Suhani K, Ali S, Aggarwal L, et al. Retrorectal cystic hamartoma: A problematic tail. J Surg Tech Case Rep. 2104; 6(2): 56-60.
Herman & Wallace faculty member Eric Dinkins, PT, MS, OCS, Cert. MT, MCTA teaches the Manual Therapy for the Lumbo-Pelvic-Hip Complex: Mobilization with Movement and Laser-Guided Feedback for Core Stabilization course for Herman & Wallace. He is one of only 13 practitioners in America credentialed to teach the Mulligan Concept of Manual Therapy, and is a published author. Join him in Arlington, VA on August 20-21, 2016 to learn new joint mobilization, evaluation, and treatment skills.
Much research has been published regarding evaluation and diagnosis of the Sacroiliac Joint (SIJ). Low back pain and pelvic girdle pain is a common complaint with patients in all clinic settings. Laslett (Manual Therapy 2005) gave our profession valuable insight into categorizing a cluster of tests to try to ensure Physical Therapists and Chiropractors know if the SI joint is a pain source of our patients. We now also have several articles reaffirming the validity of the Active Straight Leg Raise (ASLR) and Stork testing for SIJ dysfunction (Manual Therapy 2008; JBMR 2012; PT 2007). However, after talking with clinicians who attend my Mobilization with Movement classes, as well as many colleagues in the outpatient orthopedic setting, there is a definitive lack of understanding how to use this information to translate over to successful treatment. This is understandable considering there have been several articles published regarding the poor validity and consistency between clinicians regarding palpation skills and bony landmarks in the lumbar spine and pelvis (ex: Manual Therapy 2012). But perhaps the fault is not in the clinician proficiency, but rather in the nature that we are attempting to diagnose an SIJ dysfunction?
 If you were to consult with experts in body kinematics, gait analysis, and biomechanics regarding the true movement of the SIJ, there will be many different answers depending on the action that they were describing. Particularly when it comes to dysfunction. Disagreements abound when describing conditions such as “upslips”, “inflares”, etc and virtually all back their arguments with clinical anecdotal success rates. These arguments often leave clinicians with inconsistencies in treatment and increased failures.
If you were to consult with experts in body kinematics, gait analysis, and biomechanics regarding the true movement of the SIJ, there will be many different answers depending on the action that they were describing. Particularly when it comes to dysfunction. Disagreements abound when describing conditions such as “upslips”, “inflares”, etc and virtually all back their arguments with clinical anecdotal success rates. These arguments often leave clinicians with inconsistencies in treatment and increased failures.
This blog is meant to be a persuasive argument for using function-improving or pain- eliminating techniques for diagnosis and treatment of SIJ dysfunction. The logic of this approach is often misunderstood. But if applied correctly, satisfies most theory surrounding the SIJ, and provides immediate feedback for knowing how to resolve the condition and what you are treating.
We have pain provocative testing that is most commonly used in attempting to diagnose a SIJ dysfunction. However, after interpreting these tests, the clinician is still left without a true diagnosis as to the nature of what is happening at this joint to cause pain or dysfunction. This is likened to the "painful shoulder" or "low back pain" prescription we see. The error rates, even in the cluster, still leaves room for inaccurate assessment and therefore potential misguided treatment. Lumbar facet, musculature, hip capsule imbalance, are just some examples that can produce false positives on the typical SIJ tests that are used in clinic. Therefore, it is necessary to understand that pain provocative testing ONLY tells us that pain is coming from that structure that is being tested. And NOT that it is “THE” source of the dysfunction.
Now consider using function-improving or pain-eliminating techniques for your evaluation. The ALSR test, as an example, function improving special test. Compression applied to various aspects of the pelvis or supporting musculature yield a positive finding if the SLR is now easier if the force is applied. Combing this information with the faulty kinetic testing of the Stork and/or leg pull test to determine the involved side yield an immediate feedback for both the clinician and the patient as to what forces are needed to correct the dysfunction that is limiting the functional activity and restore normal motion. Treatment would then be applied by creating a force on the innominate, sacrum, or both and would then be maintained throughout the movement and can be considered a form of active exercise (manual assisted active exercise). If retesting of the affected motion yields a sustained improvement, the accurate diagnosis has now been made. And surely this diagnosis would be upheld if the patient returned at a later date to demonstrate no regression occurred.
If the force applied to the pelvis was directed toward posterior rotation at the innominate and/or an anterior rotation at the sacrum, and the affected motion cleared without pain or limited motion, it would be confirmed that these forces were necessary to correct the dysfunction on the involved side regardless of the "ambiguous diagnosis' including the potential of a previously held thought of an anterior rotation of the pelvis (making the argument of what actually happened at the pelvis mute). This may have been achieved through altering inputs viewed as a potential "threat" by the system, or mechanics stresses, etc. Regardless, if manual correction of this condition was applied and the dysfunction was correction through re-creating this without pain, one would conclude that this dysfunction was the primary eitiology of the symptoms. If the symptoms returned or the functional test was not normalized, an easy conclusion would then be that despite manual correction eliminating pain during the activity, this correction was not addressing the source of the dysfunction. And therefore the clinician should consider treatment elsewhere.
In essence, the body is capable of directing what it needs in order to return to a normal functioning homeostasis…without the application of pain. Now this pain-eliminating testing becomes your assessment, treatment and potentially your home exercise program!
To conclude, it is my suggestion to all manual based physiotherapists and chiropractors to strongly consider pain-eliminating techniques for both evaluation and treatment in their practice.
Did I mention yet that your patient already voted for that….?
Laslett, M, et al. "Diagnosis of Sacroiliac Joint Pain: Validity of individual provocation tests and composites of tests" Manual Therapy 10 (2005) 207-218
M. de Groot, et al. "The active straight leg raising test (ASLR) in pregnant women: Differences in muscle activity and force between patients and health subjects" Manual Therapy 13 (2008) 68-74
Hungerford, B, et al. "Evaluation of the Ability of Physical Therapists to Palpate Intrapelvic Motion with the Stork Test on the Support Side" Phys Ther. 2007 Jul;87(7):879-87.
O'Surrivan PB, Beales DJ. "Diagnosis and classification of pelvic girdle pain disorders—Part 1: A mechanism based approach within a biopsychosocial framework" Man Ther. 2007 May;12(2):86-97.
Arab AM, Abdollahi I, Joghataei MT, Golafshani Z, Kazemnejad A. "Inter- and intra-examiner reliability of single and composites of selected motion palpation and pain provocation tests for sacroiliac joint" Man Ther. 2009 Apr;14(2):213-21. doi: 10.1016/j.math.2008.02.004. Epub 2008 Mar 25.
Rarely does a patient with sacroiliac joint dysfunction come to see us with a goal of having surgery. Sometimes surgery winds up being the last resort for relief if our efforts and the patient’s commitment to physical therapy and prescribed exercises fail. Some of the most recent research shows positive results from minimally invasive surgery; however, the bottom line is to make sure the most educated, clinically accurate diagnosis has been made in implicating the SI joint as the source of pain.
Capobianco et al (2015) performed a prospective multi-center trial regarding SI joint fusion using a minimally invasive technique in women with post-partum pain in the pelvic girdle. Eligibility for the study required subjects to have 3 out of 5 positive SI joint stress tests and at least 50% relief with image-guided intra-articular SI joint block with a local anesthetic. Of the 172 subjects in the study, 20 of the 100 females had post-partum pelvic girdle pain, and 52 subjects were male. Significant improvements in pain, quality of life, and function were found for not only the post-partum group but all groups 12 months after surgery. Worth noting is one to three weeks after surgery, the subjects engaged in physical therapy, two times per week for six weeks.
Whang et al (2015) assessed the 6-month outcomes of SI joint fusion using triangular titanium implants versus non-surgical management in a prospective randomized controlled trial. Of the 148 subjects chosen based on similar diagnostic criteria as the study mentioned above, 102 underwent surgery, and 46 had non-surgical management. Non-surgical management involved appropriate pain medication administration, physical therapy, intra-articular SI joint steroid injections, and radiofrequency ablation of sacral nerve roots, all based on individual needs. The surgical group subjects in this study were also asked to have physical therapy two times per week for six weeks anywhere from one to three weeks post-op. The results in a six month follow up showed “clinical success” of >80% in the surgical group and <25% in the non-surgical management group.
The Journal of Neurosurgery: Spine presented an article in July 2015 by Zaidi et al with results of a systematic review of literature regarding the surgical and clinical effectiveness of SI joint fusion. The studies included open as well as minimally invasive surgery, and the causes of surgery included SI joint degeneration and arthritis, SIJ dysfunction, postpartum instability, posttraumatic, idiopathic, pathological fractures, and HLA-B27+/rheumatoid arthritis. A mean rate of satisfaction with open surgery was 54%; whereas, the mean was 84% with minimally invasive surgery. Ultimately, the authors concluded, “serious consideration of the cause of pain” is necessary before embarking on SI joint fusion as the evidence for the surgery’s efficacy is lacking.
So, who is responsible for making the definite diagnosis for SI joint dysfunction? As many patients get minimal time in doctor offices, we have a professional responsibility to competently perform a thorough evaluation for our patients. When the diagnosis is “SI joint dysfunction,” rule out the lumbar spine and hip; and, of course, when “low back pain” or “hip pain” fills the diagnosis line, rule out/in the SI joint. If you are confused about how, it is time to consider taking the Sacroiliac Joint Evaluation and Treatment course!
References:
Capobianco, R., Cher, D., & for the SIFI Study Group. (2015). Safety and effectiveness of minimally invasive sacroiliac joint fusion in women with persistent post-partum posterior pelvic girdle pain: 12-month outcomes from a prospective, multi-center trial. SpringerPlus, 4, 570. http://doi.org/10.1186/s40064-015-1359-y
Zaidi, Hasan A., Montoure, Andrew J., and Dickman, Curits A. (2015). Surgical and clinical efficacy of sacroiliac joint fusion: a systematic review of the literature. Journal of Neurosurgery: Spine. (23)1:59-66. DOI: 10.3171/2014.10.SPINE14516
Whang, P., Cher, D., Polly, D., Frank, C., Lockstadt, H., Glaser, J., … Sembrano, J. (2015). Sacroiliac Joint Fusion Using Triangular Titanium Implants vs. Non-Surgical Management: Six-Month Outcomes from a Prospective Randomized Controlled Trial. International Journal of Spine Surgery, 9, 6. http://doi.org/10.14444/2006
You’ve done a thorough evaluation of the lumbar spine. You’ve done all the special tests for hip pathology, but something is missing. Of course it could be a pelvic floor issue, but what else? Think about the middle child who gets ignored even if making a commotion or goes unnoticed unless being tripped over when standing still. Perhaps the missing link to your patient’s dysfunction is the sacroiliac joint, that “in between” area. If you are unsure how to assess and deal with the “middle child,” learning more about Sacroiliac Joint and Evaluation is something to add to your professional bucket list.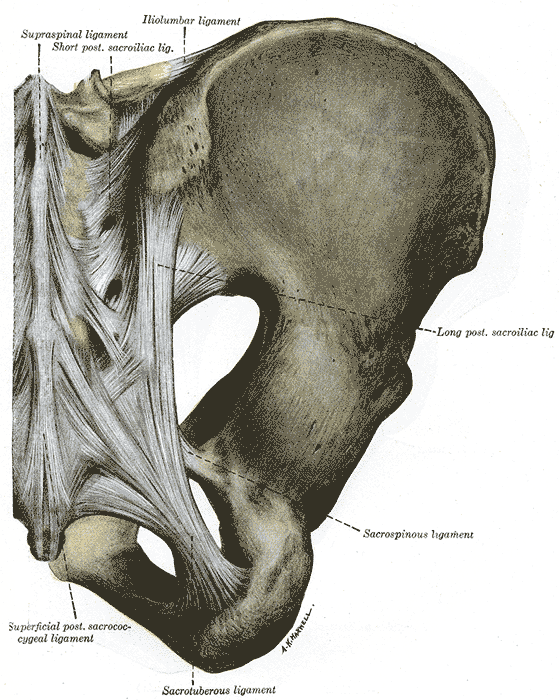
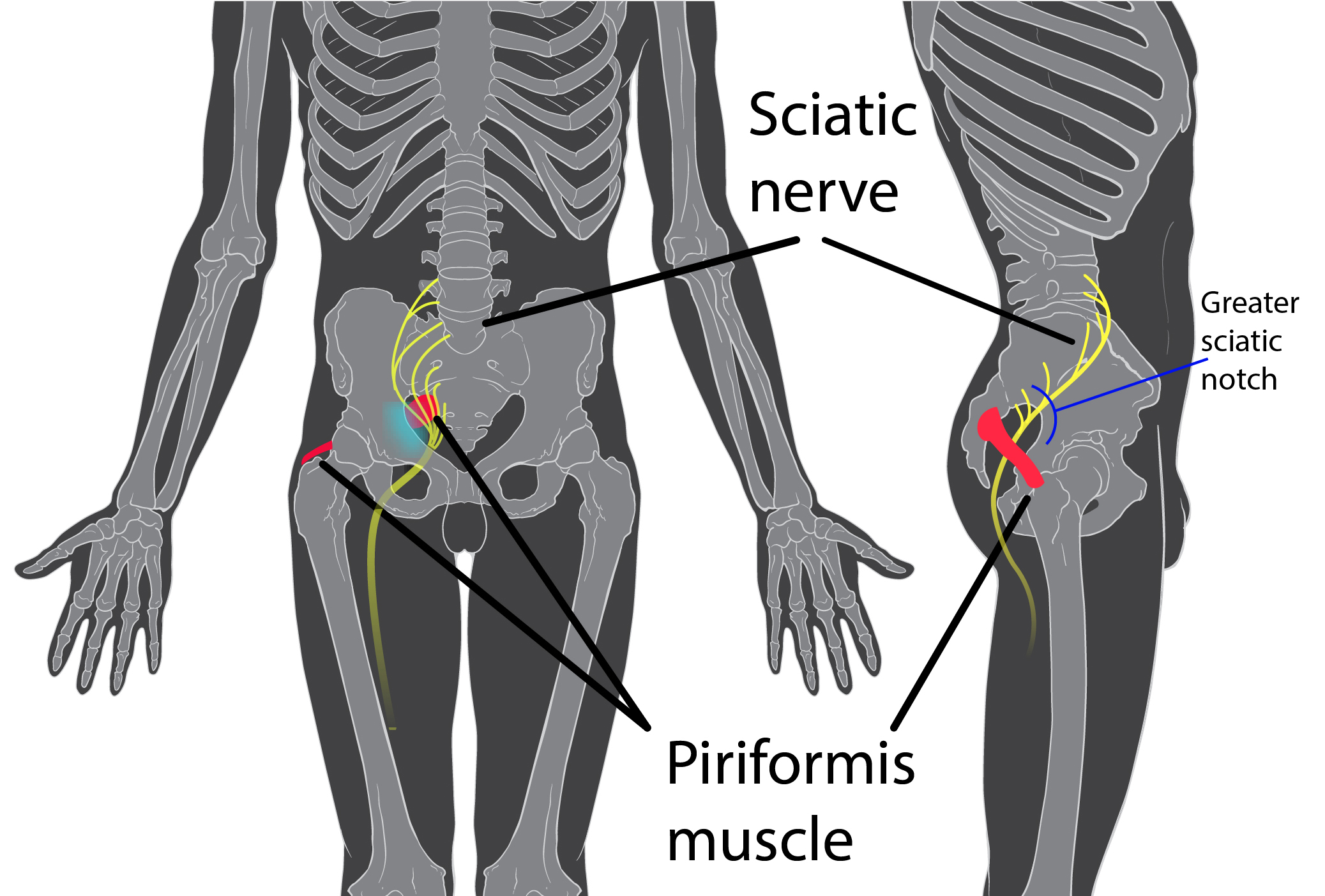
According to the special tests book by Chad Cook, a pain mapping test suggests a referral pattern of SI dysfunction as pain in the buttock unilaterally, below the level of L5, without symptoms in the midline. Often we are on a mission to make the lumbar spine the source of symptoms, but this provides some guideline as to where the pain would be located if the SI joint were the guilty party. If pain is found above L5, the SI joint is likely not the primary tissue in lesion. If the pain is bilateral, the issue is more than just SI joint.(Cook, 2013)
The special tests to diagnose SI joint dysfunction have been considered in a cluster. According to Laslett, distraction, compression, thigh thrust, Gaenslens, and Patricks are the primary tests used to assess SI dysfunction. Three or more of these tests being positive can help a clinician rule in SI joint as a diagnosis, with SI joint blocks being just as predictive. When pain cannot be centralized, and three of the tests are positive, there is a 77% probability the SI joint is the source of pain; and, in the pregnant population, there is an 89% chance the SI joint is the culprit of pain.(Laslett, 2008)
While parents keep up with the oldest and youngest, the middle child can be hard at work causing dysfunction that disrupts the whole family. Likewise, the sacroiliac joint can be hypermobile, hypomobile or have ligamentous strain, yet we therapists may ignore any signs until the lumbar spine or hip or pelvic floor are suddenly provocative. The longer an SI joint dysfunction goes undiagnosed and untreated, the greater the likelihood of pelvic floor dysfunction, secondary to its intimate relationship to the area. A catawampus ilium position on the sacrum can cause hip pain, and the ilium’s relationship to the sacrum can aggravate the lumbar spine. We just need to use all our diagnostic tools to discern what is making our patients symptomatic and then prioritize the treatment.
Taking the upcoming sacroiliac course through Herman Wallace (Sep. 12-13 in New Orleans) will make the “middle child” become respected, understood, and never left wanting again. Review the anatomy, explore and proficiently perform the special tests, and effectively implement treatment and stabilization of the SI joint during this course. You owe your patients the ability to understand the lumbar region and pelvic ring in their entirety and leave no source of pain a mystery.
References:
Cook, C., & Hegedus, E. (2013). Orthopedic physical examination tests: An evidence-based approach. Upper Saddle River, N.J.: PearsonPrentice Hall.
Laslett, M. (2008). Evidence-Based Diagnosis and Treatment of the Painful Sacroiliac Joint. The Journal of Manual & Manipulative Therapy, 16(3), 142–152.
An interesting study aimed to objectively answer the following question: Does applying kinesiotape to promote a posterior pelvic tilt improve an active straight leg raise (ASLR) test in women who have sacroiliac joint pain and who habitually wear high-heeled shoes? To explain some of the rationale for the chosen technique and target population, the authors first describe prior research pointing out that use of high heels can lead to an anterior pelvic tilt position and increased lumbar lordosis. This position can slacken the sacrotuberous ligament and therefore reduce the ability of the ligament to create proper form closure, according to the article.
The research included 16 women with a mean age of 23.63. Inclusion criteria is as follows: having a habit of wearing high-heeled shoes (at least 4 times/week for 4 consecutive hours over at least 1 year), and having pain in both sacroiliac joints with the active straight leg raise test (ASLR). Additionally, having symptoms for at least 3 months, no proximal SIJ pain referral to the lumbar spine, and at least 3 of 5 positive SIJ tests (posterior shear test, pelvic torsion test, sacral thrust test, distraction and compression test) were needed for inclusion in the study.
Anterior pelvic tilt was measured using a palpation meter (PALM) before, immediately after application, 1 day after tape application, and immediately after removal of tape. ASLR was measured at same time points. The ASLR was self-scored on a 6-point scale ranging from “not difficult at all”” to unable to perform”. Kinesiotape was applied for a posterior pelvic tilt taping, and the tape was applied in the target position. I-type strips with ~50% of available tension were applied over the rectus abdominis and external oblique muscles. I-type strips with ~75% tension were placed from ASIS to PSIS aiming for mechanical correction of the anterior tilt.
Results of the study indicated a decrease inanterior pelvic tilt, both during and after tape application, and an improved active straight leg raise test. As this was a preliminary study, the results cannot be extrapolated to SIJ pain and dysfunction with other activities than the ASLR test. The degree of anterior pelvic tilt cannot also directly be correlated to sacroiliac joint pain and dysfunction, yet this research is very interesting, and demonstrates a simple method for affecting in the short term a patient’s mechanics as well as reports of function on the ASLR test, a very clinically simple and useful exam.
If you would like to learn more about evaluating and treating dysfunctions related to the sacroiliac joint, join Peter Philip at Sacroiliac Joint Evaluation and Treatment - New Orleans, LA this Sep 12, 2015 - Sep 13, 2015.