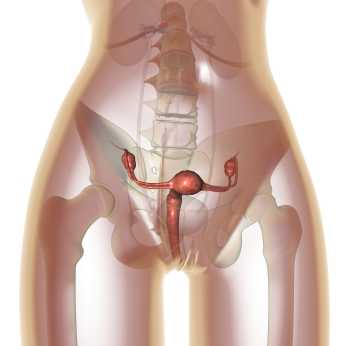
In women who have endometriosis, ablation procedures are commonly completed to destroy endometrial tissue lining the uterus. A goal of ablation is to disrupt severe bleeding that can lead to other conditions including anemia. Research published in last month's Obstetrics & Gynecology identified the risk factors for pain and subsequent hysterectomy following ablation procedures for endometriosis. Of 300 women, 270 completed follow-up, and the resultant data was reported:
- -23% developed new onset or worsening pain after the ablation
- -19% proceeded to hysterectomy
- -a history of dysmenorrhea increased the risk of developing pain by 74%
- -a history of tubal sterilization increased the risk of developing pain by > 50%
- -women of white race were 45% less likely to develop pain
- -a history of cesarean delivery more than doubled risk of hysterectomy
- -uterine abnormalities such as leiomyoma, adenomyosis, thickened endometrial strip, or polyps quadrupled the risk for hysterectomy
For the nearly 20% of these women who had a hysterectomy after ablation therapy, the most common indication for the hysterectomy was pain. Regarding the increased risk of pain after ablation in non-white women, the authors proposed the higher rates of leimyomatous uteri in African American women (largest population of non-white women in the study) as a source. Because pain is a potential complication of endometrial ablation, the authors of this article recommend that providers consider patient characteristics when educating patients about the potential benefits and risks of the procedure.
Although in pelvic rehabilitation we do not counsel for or against surgical procedures, knowledge of the potential risk factors for our patients who have had or who are having a uterine ablation can assist in our screening and interventions. If a patient asks our opinion about uterine ablation, pointing out research such as the linked article may help her discuss pros and cons with us and with her providers. The need for patients to understand the potential side effects of a uterine ablation and to actively manage her recovery may be important in avoiding hysterectomy, if that is the patient's goal. Endometriosis is one of the main topics in a new course offered by faculty member Michelle Lyons. The new continuing education course "Special Topics in Women's Health: Endometriosis, Infertility, and Hysterectomy" will be offered in March in San Diego and the Chicago area in May.
This post was written by H&W instructor Peter Philip, PT, ScD, COMT, PRPC, who authored and instructs the Sacroiliac Joint Evaluation and Treatment course. The next SI Joint course will be taking place this January in Seattle.

Patient one:
55 year old female with complaints of pelvic pain. States that her pain is noted along the deep inguinal region, involving her pubis and labia majora. States that intercourse is difficult, and that she is quite anxious to initiate or participate. She denies trauma, only that she’d been increasing her fitness activities as she’s going to Florida for a winter get-away. She denies changes in her bowel and bladder function, other than intermittent SUI with ‘heavy exercise’.
Clinical testing:
ALROM is negative. During forward flexion there was no reversal of the lordosis.
Segmental myotomal and dermatomal testing is unremarkable.
ASLR and PSLR are negative.
Gillet’s and forward flexion are apparently negative.
There are palpable “marbles” to palpation along bilateral SIJ, and the sacrum is ~40? of nutation.
FABER, FAIR and McCarthy tests are negative. Iliac compression is modestly provocative for patient’s symptoms, while the sacral thigh thrust was provocative for ipsilateral symptom provocation.
While in prone, the patient demonstrated a positive Dead Butt Syndrome bilaterally and there were significant restrictions to fascial rolling throughout the lumbosacral region.
The clinical question is: What to do next? What would you do?
I chose to provide a local traction to each SIJ, followed by a mobilization with movement directed at S3 to promote counter nutation. After treatment, the patient arose from the plinth and remarked that her pain was significantly reduced. On follow up, her pain was 10% that of her initial pain at evaluation.
My questions to you are:
1. What caused her “pelvic pain”?
2. Why did her pain subside? 3. Would you have done an internal evaluation?
These and other questions will be addressed at Sacroiliac Joint and Pelvic Ring Evaluation & Treatment in Seattle, Washington January 25th to the 26th.

Catastrophizing is a buzzword in relation to pain, but what does it really mean for our patients and for our plan of care? Catastrophizing, according to Iwaki and colleagues is a maladaptive response to pain, with research supporting the idea that level of catastrophizing behavior may predict a patient's level of function. A terrific blog post on the Psychology Today website by Alice Boyles, PhD, translates the term into everyday symptoms of this behavior. She describes catastrophizing as having 2 parts: predicting a negative outcome, and then concluding that if the negative outcome happens, this would be a catastrophe. Imagine our patients who develop a painful condition, and then jump into a "worst case scenario." A patient who develops pelvic pain may think "I will never get rid of this pain", and then perhaps, "I will never have a partner and a healthy sex life."
Several prior blog posts on the Herman & Wallace website have specifically addressed different conditions and the role of catastrophizing. Some of the posts include the following topics:
Catastrophizing in Male Chronic Pelvic Pain
Lumbopelvic Pain and Catastrophizing in Pregnancy
Psychological Factors in Female Pelvic Pain
The study by Iwaki and colleagues also reported on subdomains of catastrophization and reported that the trait of helplessness was predictive of pain intensity, pain interference and depression, and that magnification of symptoms was predictive of anxiety. Regardless of the extent to which catastrophization impacts healing, being able to reframe pain and healing for our patients becomes a necessity so that the patient can focus on the steps involved in healing. The Institute now offers several continuing education courses designed to teach the therapist skills to address catastrophization including Meditation for Patients and Providers, and Mindfulness-based Biopsychosocial Approach to the Treatment of Chronic Pain.

If pelvic floor muscle training (PFMT) is instructed as part of a general exercise class during pregnancy, can this (PFMT) prevent urinary incontinence? A recent post on our site described the systematic review by Bo and colleagues in which the researchers suggested that fitness instructors and coaches should be trained in effective pelvic floor muscle training approaches. A recent article describes such an approach in which a Physical Activity and Sports Sciences graduate instructed in a general exercise class for pregnant women and the class also included PFMT. Nulliparous women completed participation in a pregnancy exercise class (n=63) or a control group (n=89), and in the exercise group, pelvic floor muscle exercises were included. The classes took place 3x/week, for 55-60 minutes each session, for up to 22 weeks, and 8-12 women were in each group class.
Within each exercise class, a typical prenatal program was followed consisting of an 8 minute warm-up, 30 minutes of aerobic training including 10 minutes of strength training, 10 minutes of PFMT and a 7 minute cool-down period. A heart rate monitor and a Borg Rating of Perceived Exertion Scale was used and the women were asked to exercise at a 12-14 on the Borg scale. For pelvic floor muscle training, women were instructed in the anatomy and function of the PFM and in the role of the PFM in urinary incontinence. Although the participants were not formally assessed for correct contractions, the women were instructed in methods of confirming a correct contraction at home such as stopping the flow of urine, self-palpation, or using a mirror to confirm contraction. The PFM exercises started with 1 set of 8 contractions, and the class included both long (6 seconds) and short (1 second) contractions. The participants worked up to a total of 100 exercise contractions that included a combination of short and long contractions, and they were also encouraged to complete the same number of exercises on days outside of class.
Women in the control group received "usual care" including care from a midwife and instruction in pelvic floor muscle health. The outcome tool completed by both groups included the International Consultation on Incontinence Questionnaire- Urinary Incontinence Short Form (ICIQ-UI SF) which was completed prior to and directly following intervention. At the end of the intervention, a significant difference was observed in the women in the exercise group (EG), as 95% of the EG denied leakage, whereas 61% of the control group denied leakage. Of those reporting leakage in the exercise group, the amount of leakage reported was small, and in the control group, amount leaked ranged from small to large. The key points of interest in this study include that first, participation in an exercise group that includes pelvic floor muscle training can prevent urinary incontinence in pregnancy, Secondly, although pelvic muscle function assessment is optimal, participants who did not have PFM contraction confirmed still had positive outcome from the treatment. And because most studies of PFMT are conducted by a physical therapist, this study is unique in its design of having a Physical Activity and Sports Science graduate conduct the intervention.
To learn more about training the pelvic floor, find out which course in the Pelvic Floor Series is right for you. If you have not been trained yet in internal pelvic muscle assessment, the Pelvic Floor Level 1 (PF1) continuing education course is a great place to start. This course fills up many months ahead of time, so check the dates on our website for the best course for you!

One of the challenges in assessing pelvic muscle function in women who have pain is to avoid triggering pain with the assessment tool. This challenge was met by the use of external measuring of pelvic floor muscles using transperineal four-dimensional (4D) ultrasound in this study by Morin and colleagues. Women who were asymptomatic (n=51) and symptomatic (n=49) were assessed with 4D ultrasound in supine with pelvic floor muscles (PFM) at rest and at maximal contraction. The women who were symptomatic were diagnosed with provoked vestibulodynia (PVD) and all of the women in the study were nulliparous. The data collected using the 4D transperineal US included anorectal angle, levator plate angle, displacement of the bladder neck, and levator hiatus.
Results of the study indicated that women with provoked vestibulodynia had a significantly smaller hiatus, smaller anorectal angle, and at rest, a larger levator plate angle. These differences suggested an increase in pelvic floor muscle tone. Additionally, when the PFM were assessed at maximal contraction, subjects with PVD demonstrated smaller changes in levator hiatus narrowing were noted, with decreased displacement of the bladder neck and decreased changes in levator plate and anorectal angles. These changes are believed to demonstrate pelvic floor muscle weakness.
The authors describe the value of the assessment technique, 4D ultrasonography, as having terrific advantage over other research methods due to the lack of required insertion of the US. While pelvic rehabilitation providers may concur that increased pelvic floor muscle tone in association with pelvic muscle weakness is a common clinical finding, research that describes the phenomenon is needed and much appreciated. We continue to find answers in research such as this article that answers the fundamental question: do women who present with pelvic dysfunction demonstrate differences in pelvic muscle health than a pelvic-healthy population? If you would like to learn more about provoked vestibulodynia including evaluation and management, join faculty member Dee Hartmann at the Assessing and Treating Women with Vulvodynia continuing education course. We are currently confirming dates for this course, and if you would like to host the Vulvodynia course, contact us at the Institute!

The American Heart Association/American Stroke Association Guidelines for Prevention of Stroke in Women reports that although stroke is not common during pregnancy, pregnant women are more at risk for stroke than non-pregnant young women. The guidelines describe the pregnancy-related physiologic factors of venous stasis, lower extremity edema, and blood hypercoagulability as factors in increased risk of stroke. Hypertensive disorders during pregnancy including preeclampsia can also increase maternal and fetal risk, with risk factors of obesity, age over 40, multiple pregnancy, and diabetes.
Postpartum hypertensive issues can also be a concern, and providers should be alert to the symptom of headaches as a potential marker of elevated blood pressure. Although rehabilitation professionals should routinely measure blood pressure in patients, numerous studies have demonstrated that we do not. The referenced guidelines give parameters for blood pressure readings for mild, moderate, and severely high blood pressure readings in pregnancy.
| High Blood Pressure in Pregnancy
|
Diastolic (mm Hg)
|
Systolic (mm Hg) |
| Mild | 90-99 | 140-149 |
| Moderate | 100-109 | 150-159 |
| Severe | ≥110 | ≥160 |
The third trimester and the postpartum period bring the highest risk for stroke, and the authors of the guidelines point out that a stroke can occur with even moderately elevated blood pressure readings. Even if a woman recovers from elevated blood pressure in the peripartum period, she may remain at risk for developing further cardiovascular disease including stroke. Having gestational diabetes, which can later develop into Type 2 diabetes, can also increase stroke risk, meaning that every woman's history related to pregnancy and postpartum cardiovascular health should be taken with interest. Measuring blood pressure regularly is also a habit that therapists must develop.
In addition to screening for elevated blood pressure in the peripartum period, rehabilitation providers can educate women in healthy lifestyle choices, safe exercise activities, and in management of musculoskeletal disorders that may inhibit physical activity. If you are interested in learning more about caring for women in the peripartum period, look ahead at dates for the continuing education course Care of the Pregnant Patient or Care of the Postpartum Patient
A recent on-line, national survey completed in Australia asked women who had completed treatment for breast cancer to answer questions about exercise. 432 women were surveyed about their perceived exercise barriers as well as potential benefits. Although the answers may not be entirely surprising to practitioners who work with women who are participating in cancer rehabilitation, we may be able to learn about ways to support women who are interested in increasing their exercise activities. Women reported challenges of feeling weak, lacking self-discipline, and not making exercise a priority as barriers to exercising. Women also reported enjoying exercising, having improved sense of well-being, and decreased tension and stress when participating in exercise. The authors in this study describe the potential physical benefits of exercise in survivors of breast cancer to include improved cardiorespiratory fitness, strength, energy levels, more effective weight management, and decrease in risk of heart and circulatory disease. Further benefits towards emotional and psychological health are also described in the study and include improved self-esteem, decreased anxiety and depression, and better mood.
With all of these known benefits, what limits exercise participation in women? Consider that a woman who is already dealing with cancer-related fatigue has a small reserve of extra energy. If she participates in exercise, will she have enough energy to prepare healthy foods, or to finish her work, or to interact with her family? Even though the exercises may in the long run increase a woman's energy levels, understanding the choices that she has to make on any given day can help guide the therapist's recommendations. How can you help a patient avoid procrastination, one of the largest perceived barriers to exercise in this study? Perhaps you can help her trouble-shoot the obstacles that she may face in her day and give examples of actions that can set her up for success. These strategies might include preparing her exercise clothing to bring with her for a lunch time walk, or taking a nap at work so that she has enough energy to exercise in the evenings. Engaging a friend to join her for exercise activities or helping her find a comfortable bra- one of the commonly mentioned barriers in the referenced study- may help a woman participate in exercise.
Many pelvic rehabilitation providers are working with women who are dealing with the challenging recovery associated with oncology issues such as breast cancer. Although women may know that exercise is beneficial, the barriers to exercise can limit participation in lifelong healthy habits such as daily exercise. Regardless of the type of cancer a woman is woman is recovering from, being able to dialog about perceived barriers to exercise is valuable. If you are interested in working with more women who are recovering from cancer, or in general would like to know more about exercise and oncology issues, the Institute has an oncology series with topics in breast cancer and pelvic cancer, among others.

In patients who failed to respond to biofeedback therapy alone for anismus, authors in this study reported a beneficial, although temporary, effect of using botulinum toxin type A injection (BTX-A injection) to the puborectalis and external sphincter muscles. Anismus is more commonly referred to as dyssynergic defecation, or an inability to properly lengthen the pelvic floor muscles during emptying of the bowels. 31 patients who had been treated with and failed "simple biofeedback training" were then treated with BTX-A injection followed by biofeedback training. 18 males and 13 females with a mean age of 50 and a mean duration of constipation of 5.6 years were diagnosed with defecation dysfunction, or anismus. Diagnosis of animus was made using anorectal manometry, balloon expulsion test, surface electromyography (EMG) of the pelvic floor, and defecography.
Pelvic floor muscle training included biofeedback therapy consisting of intra-anal surface EMG and electrotherapy (although the way the methods are described make determining if both EMG and electrotherapy were completed with internal sensors difficult). Treatment occurred 1-2 times/day for 30 minutes per session (15 minutes of electrotherapy and 15 minutes of biofeedback). Frequency of the electrotherapy was 10 Mz, 10 seconds of "considerable sensation without…pain" and 10 seconds of rest. During biofeedback sessions, pelvic muscle strengthening and relaxation was also instructed. Therapy occurred for up to one month, and patients were instructed to continue with therapeutic exercises at home. The researchers followed up one month after the injection and therapy, and 6-12 months after intervention by telephone.
The subjects in this study suffered from difficult and incomplete evacuation, use of laxatives, and chronic straining during defecation. The repeated measures for diagnostic criteria that were completed after intervention found improvements in the subjects' resting anal canal pressures and with the balloon expulsion test and constipation scoring system. The authors also reported adverse effects of BTX-A injections including fecal incontinence. Conclusions of the article include that the botox injections were considered a temporary treatment for defecation dysfunction, whereas the botox injection combined with pelvic floor biofeedback training is "a more valid way to treat."
What is missing from this study? Manual therapy, muscle coordination retraining in combination with abdominal wall activation, and functional training related to positioning. While the authors suggest that injections should be used with biofeedback training, the potential negative effects of botox injections cannot be overlooked. Infection, pain, and bleeding are complications that have been highlighted in the literature, and in this study, fecal incontinence (although reported as mild) occurred. The research design appears to fail to recognize the chronic tension and holding pattern of the pelvic floor muscles, and unless the goal of repeated contractions is to elicit a contract/relax effect, the pelvic floor strengthening per se does not align with the ideal therapeutic goal, which should be to correct the dyssynergic pattern of defecation. Relaxing the pelvic floor muscles is not the same as a functional bearing down or lengthening of the pelvic floor involved in defecation. If you are interested in learning more about training defecation patterns and pelvic muscle rehabilitation for bowel dysfunction, check out Pelvic Floor Level 2A (PF2A) which discusses in detail fecal incontinence, constipation, and other colorectal conditions. The next opportunity to take this course is in Wisconsin in March. If you have already taken PF2A, you might find a course focused on Bowel Pathology, Function, Dysfunction & the Pelvic Floor, with the next course taking place in Kansas City in April.
Pelvic rehabilitation therapists working with men who have sexual dysfunction may be aware of the work of Grace Dorey, who published a randomized, controlled trial about pelvic muscle strengthening for erectile dysfunction. A recent article published in the Journal of the American Physical Therapy Association confirms the conclusion of Dorey and colleagues that pelvic muscle rehabilitation is beneficial in improving erectile dysfunction.
In the study out of France by Lavosier and colleagues, 122 men with erectile dysfunction and 108 men with premature ejaculation completed twenty 30-minute sessions of pelvic muscle strengthening with active contraction and electrical stimulation. In the study, a penile cuff placed around the shaft of the penis measured intracavernous pressure, electrodes applied to the "upper face of the penis shaft" provided electrostimulation at 80 Hz to the ischiocavernosus muscles, and a vibrator device applied to the glans penis provided stimulation for erection. A large computer screen displayed contractions, and the patient was allowed to increase the level of electrotherapy stimulation to maximal sensory stimulation below pain threshold. Contractions were completed at the patient's own pace in regards to frequency and duration, but each patient did have feedback about his contraction on the computer monitor in front of him. Patients were also given an intracavernosal injection aimed to create an erection lasting 30 minutes.
The authors describe the erection process as being both vascular and muscular, with the ischiocavernosus muscle having a significant role in erections and in ejaculation. The ischiocavernosus muscle, which is a muscle of the superficial layer in the perineum, attaches along the ischiopubic ramus and wraps around the proximal superior portion of the penis to have an effect on penile rigidity. Contractions of the ischiocavernosus appear to maintain the rigidity of the penis through compression of the roots of the corpus cavernosum, the upper portions of the penis where blood fills in the spaces.
This is a very interesting study with equipment and software created specifically for the study. Because ischiocavernosus muscle force could not be directly obtained, force variations were measured using intracavernosal pressure changes during and after pelvic muscle contractions. The authors provide a detailed description of the analysis methods as well as the challenges of measuring the ischiocavernosus muscle with other methods. The lack of uniformity in the contractions and the likelihood that all components (pharmacological, electrotherapy, vibratory stimulation, and feedback) would not be a form of therapy available to all patients in a rehabilitation setting make this study challenging to extrapolate to patient care. However, further evidence that pelvic muscle strengthening can alleviate erectile dysfunction is promising, and the study components also bring into question if patients should be utilizing vibratory therapy, performing home exercise programs for longer periods of time (up to 30 minutes), and if patients should be completing their exercises during states of penile erections. Further research will help us understand the role of each component in pelvic rehabilitation and perhaps to also learn why the results of the study were not as encouraging for premature ejaculation.
To learn more about male sexual health and pelvic floor rehabilitation, you can attend the Male Pelvic Floor Function, Dysfunction, and Treatment continuing education course, with the next opportunity scheduled in Nashville in March.

Incontinence-associated dermatitis causes a range of signs and symptoms, and yet the potential impact of skin breakdown may lead to serious, even life-threatening consequences. Although patients of any functional status or within any treatment setting may be at risk for developing the condition. An article from Beeckman et al. in the British Journal of Nursing describes both the chemical and physical irritation of the skin that occurs when urine or feces remains in contact with the perineal skin. According to this article, urine and feces can cause an increase in the pH levels, and subsequently increase skin permeability, reduce barrier function, and increase the risk of bacterial colonization. Rubbing of the skin on clothing, pads or diapers, or surfaces such as a bed or chair creates friction and can further irritate the skin. The linked article focuses on the differentiation between incontinence-associated dermatitis (AID) and pressure ulcers, and is available for free, full access via the link above if you are interested in learning more about the concept.
If the skin dysfunction is limited to IAD, the pelvic rehabilitation provider may observe rash and erythema with possible skin breakdown, or infections such as candidiasis. Unless a therapist is trained in assessing for pressure ulcers, any new or worsened skin breakdown should be brought to the attention of a physician, nurse, or physician extender who is working with the patient. One of the challenges in perineal skin irritation is that the patient may not be able to easily observe the skin and report new onset or worsening of symptoms. In an outpatient setting, even when working with patients who do not have limited mobility or self-care skills, observing the perineal skin remains critical in documenting skin integrity, persistent issues, or a worsening of a condition. Because, as the authors of this study point out, care for skin ulcers and incontinence-associated dermatitis are different, early recognition and proper diagnosis aids in healing.
Following are some recommendations by Beeckman and colleagues for avoiding skin irritation in the presence of incontinence:
•A perineal cleanser should be used that has a pH range of 5.4-5.9
•Perineal skin should be cleaned quickly following an episode of fecal incontinence, whereas avoiding too-frequent skin washing with continual episodes of urinary incontinence is important
•Moisturizing the skin (with emolient-based rather than humectant-based moisturizer) is valuable in aiding healing and preventing further irritation
•Use a skin protectant to create a barrier between the skin and feces or urine
•Absorptive or containment products (catheter or stool diversion system) can further help keep irritants away from the skin surface
Ideally, issues of incontinence, topics covered at length in the Institute's introductory pelvic floor course series are treatable. Even in the case of refractory incontinence, patients should be made aware of appropriate treatment options and screening by appropriate medical providers can direct patients to proper diagnostic testing and referrals. Because pelvic rehabilitation providers may be the first to notice skin breakdown or risk for infections, recognizing our role in patient education and referral to proper providers remains essential.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/







































