George Thiele, MD, published several articles relating to coccyx pain as early as 1930 and into the late 1960's. His work on coccyx pain and treatment remains relevant today, and all pelvic rehabilitation providers can benefit from knowledge of his publications. Thiele's massage is a particular method of massage to the posterior pelvic floor muscles including the coccygeus. Dr. Thiele, in his article on the cause and treatment of coccygodynia in 1963, states that the levator ani and coccygeus muscles are tender and spastic, while the tip of the coccyx is not usually tender in patients who complain of tailbone pain. The same article takes the reader through an amazing literature review describing interventions for coccyx pain in the early 20th century.
Examination and physical findings, according to Dr. Thiele, include slow and careful sitting with weight often shifted to one buttock, and frequent change of position. He also describes poor sitting posture, with pressure placed upon the middle buttocks, sacrum, and tailbone. Postural dysfunction as a proposed etiology is not a new theory, and in Thiele's article he states that poor sitting posture is "…the most important traumatic factor in coccygodynia…" and even referred to postural cases as having "television disease."
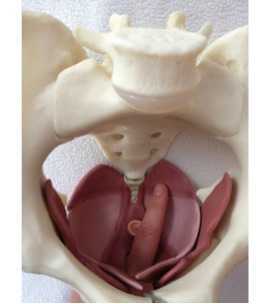
In reference to treatment, Thiele suggests putting a patient in Sims' position (left lateral side lying or recumbent position), and placing the gloved index finger into the rectum with the thumb over the coccyx externally, palpating the coccyx between the thumb and index finger. The finger is then moved laterally, in contact with the soft tissues of the coccygeus, levator ani, and gluteus maximus muscles. The finger is moved with moderate pressure "…laterally, anteriorly, and then medially, describing an arc of 180 degrees until the finger tip lies just posterior to the symphysis pubis." The massaging strokes, applied to a patient's tolerance, are applied 10-15 repetitions on each side with the patient being asked to bear down during the massage strokes. Dr. Thiele recommended daily massage 5-6 days, then every other day for 7-10 days, and gradually less often until symptoms are resolved.
Thiele's massage for coccygodynia is one excellent tool in the treatment of coccyx pain. For a comprehensive view of coccyx pain, check out faculty member Lila Abatte's Coccyx Pain Evaluation and Treatment continuing education course, coming up in New Hampshire in September!

Posttraumatic Stress Syndrome, also known as PTSD, is an unfortunate consequence of many women's birth experiences. While there are known risk factors, there is not currently a standardized screening method for identifying symptoms of PTSD in the postpartum period. One recent meta-analysis of 78 research studies identified a prevalence of postpartum PTSD as 3.1% in community samples and as 15.7% in at-risk or targeted samples. Risk factors for PTSD included current depression, labor experiences (including interactions with medical staff), and a history of psychopathology. In the targeted samples, risk factors included current depression and infant complications. Other authors have explored the relationships between preterm birth and PTSD, preeclampsia or premature rupture of membranes, and infants in the neonatal intensive care unit.
One of the main concerns of failing to identify and treat for PTSD in the postpartum period is the potential negative effect on the family. High levels of anxiety, stress, and depression may impact not only the mother's health, but also may affect her ability to meet her new infant's needs, or complete usual functions in work and home life. One study suggested that "…maternal stress and depression are related to infants’ ability to self-sooth during a stressful situation." Clearly, healthy moms promote healthy families, and each mother deserves the attention that her new infant often receives from the world!
How can we be a part of the solution? We have previously posted on the blog about screening for depression in the postpartum period. The US Department of Veterans Affairs lists multiple screening tools for PTSD as well. Here's another bit of exciting news: yoga has been identified as a method to reduce symptoms of PTSD. In a randomized, controlled clinical trial, the treatment arm was given 10 weeks (1x/week at 1 hour sessions) of "trauma-informed" yoga, whereas the control group was given information about women's health and self-efficacy in various domains. Interestingly, while both groups showed positive effects from intervention in the first half of the treatment, the yoga group maintained the improvements during the latter half of the study, while the control group relapsed.
You can learn about yoga for postpartum mothers, and learn how to integrate strategies to help heal postpartum symptoms of PTSD this summer at Ginger Garner's Yoga as Medicine for Labor & Delivery and Postpartum. The continuing education course takes place in Seattle, and we still have a few spots left! Don't miss this chance to add more amazing tools to your toolbox in support of women of any postpartum age.

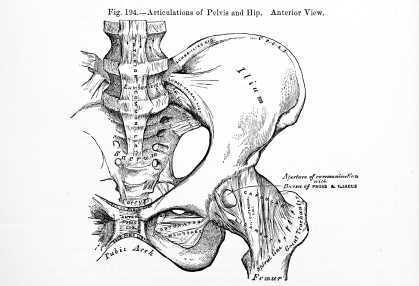
While many of the Herman & Wallace Pelvic Rehabilitation continuing education courses focus on study of the pelvic floor muscles, the inclusion and consideration of the trunk, breathing, form and force closure, and posture are also needed to truly understand the pelvis. Our professional education does not prepare us well in regards to understanding the pelvic floor and pelvic girdle, and the foundational concepts that provide clinical meaningfulness come from a variety of research camps. If you feel that you were never provided this foundational information about the pelvic girdle and trunk, and wish to better apply practical concepts in movement and muscle facilitation (or inhibition), you might be looking for the Pelvic Floor/Pelvic Girdle continuing education course that is coming to Atlanta in late September.
The course covers interesting topics such as pelvic floor muscle activation patterns in health and in dysfunction, use of load transfer tests such as the active straight leg raise, orthopedic considerations of pelvic dysfunction, pelvic floor muscle (PFM) exercise cues, risk factors for pelvic dysfunction, and treatment of the coccyx. If you (or a friend you want to take a course with) is not quite sure about internal pelvic floor coursework at this time, the good news is that this course addresses pelvic dysfunction using an external approach. Experienced therapists can appreciate the research-based approach to muscle dysfunctions that can cause or perpetuate a variety of symptoms, and newer therapists have the chance to learn how to integrate pelvic floor/pelvic girdle concepts into current practice. A biofeedback lab introduces use of surface electromyography (sEMG) as well.
There is still time to sign up for the September course in Atlanta, the only remaining opportunity to take the Pelvic Floor/Pelvic Girdle continuing education course this year. Bring a friend, or a colleague, and work together to combine external and internal approaches to pelvic dysfunction.
In this study investigators tested the hypothesis that following hip arthroscopy, the number of patients who developed pudendal neuralgia would exceed 1%. Development of pudendal neuralgia symptoms following hip arthroscopy was assessed in 150 patients (female = 79, male = 71) who were operated on in one facility by a single surgeon. Indications for the surgery included post-trauma foreign-body, osteochondromatosis, and labral lesion resection. The Nantes criteria were utilized for diagnosis, which includes as "essential" criteria the following: pain in the region of the pudendal nerve; pain that is worsened by sitting, relieved by sitting on a toilet seat; pain does not interrupt sleep, pain with no objective sensory impairment and that is relieved by a pudendal nerve block.
The operated hip was placed in a position of 30 degrees of adduction, internal rotation and flexion. The hip was operated on with a single anterolateral approach in most cases, with a second anterolateral approach needed in eight cases. Study results include an incidence rate of 2% in the population of 150 patients. 3 of the patients (2 female, 1 male) were diagnosed with pudendal neuralgia presenting in all 3 as "pure sensory" with symptoms of perineal hypoesthesia and dysesthesia on the operated side. The 3 cases resolved spontaneously within 3 weeks to 6 months. Two cases of sciatica following hip arthroscopy were documented, and these cases resolved without intervention other than a short course of analgesics. The patients also presented with gluteus medius insertion tenderness.
Although the study also aimed to determine risk factors for development of pudendal neuralgia following hip scope, the small number of patients who developed symptoms made the analysis for risk factors difficult. The authors also point out that the one-way surgical technique (not the standard surgical technique) also may have created some bias in the study. In conclusion, although the cited study reported a low incidence of pudendal neuralgia onset following hip arthroscopy, larger numbers have appeared in the literature, and according to the authors, surgical risk factors for developing nerve complications following a hip scope include the amount of traction placed on the joint, the length of surgery, and appropriate pelvic support bilaterally. The take-home point for pelvic rehabilitation providers is that patients are at some risk for pelvic nerve dysfunction following hip arthroscopy, and we have a role in educating providers and in screening patients for such conditions.
The Herman & Wallace Pelvic Rehabilitation Institute offers many relevant courses regarding the hip and pelvis, and if you are interested in learning more about the pudendal nerve, hurry to sign up for the continuing education course "Pudendal Neuralgia Assessment, Treatment, and Differentials." You can also attend "Biomechanical Assessment of the Hip & Pelvis" continuing education course to learn all about testing, treatment, and diagnosis of the hip and pelvis.
This post was written by H&W instructor Steve Dischiavi, MPT, DPT, ATC, COMT, CSCS. Dr. Dischiavi will be instructing the course that he wrote on "Biomechanical Assessment of the Hip and Pelvis" in Virginia this August.

In an outpatient sports medicine clinic the traditional model of physical therapy evaluation typically includes the therapist reviewing a patients chart and subjective symptom questionnaire of some sort. Then the therapist will bring the patient to an area to begin a subjective history and then onto a physical exam. After these procedures have been completed the therapist will typically assign a working clinical diagnosis and then begin treatment. In short, I would like to suggest a paradigm shift to this traditional model of thinking. Instead of starting the exam on a table with a static assessment of the structures involved and identifying the pain generator, I suggest the therapist begin with a specific set of movements used as an evaluative tool to identify movement dysfunction within the anatomical system as a whole.
All human interactions on earth occur between ground reaction force and gravity, our bodies are mostly just stuck in the middle of this constant battle and typically we succumb to whichever power exposes the weakest link in our biomechanical chains. One of the reasons the biomechanical chains in our bodies are so pliable and vulnerable to constant ground reaction force and gravity acting on them is because we are basically bones or struts suspended in a bag of skin all connected by soft tissue. Suggesting that without skin, fascia, and connective tissue supporting us, we would collapse to the ground in a pile of bones! Ingber (1997), suggested this concept, known as tensegrity, was the “architecture of life.” So in summary, the tensegrity structures are mechanically stable not because of the strength of the individual bones, but because of the way the entire human body distributes and balances mechanical stresses through the use of polyarticular muscle chains called slings. There will be more on slings in the upcoming blogs.
If there is truly a paradigm shift with the way we initially assess our clients and we begin our evaluations with whole system movement patterns it would be because we want to actually see how this tensgerity model is essentially collapsing under the stress of gravity. We would get a first hand glimpse in real time how energy leaks and blocks occur during human movement. These concepts are the foundation for the course Biomechanical Assessment of the Hip & Pelvis.
Ingber, D.E. (1997). Tensegrity: the architectural basis of cellular mechanotransduction.
Annual Review of Physiology, 59, 575-59.
Dr. Dischiavi's course is designed to elevate the participant’s skill level through advanced training in hip and pelvic biomechanics, functional “slings” created by the myofascial system, and through use of sports medicine theory and applied science. Biomechanical Assessment of The Hip & Pelvis will be taking place in August in Arlington, VA

The term "sports hernia" has been used over time to describe a variety of issues, and the medical and rehabilitation community has recently been provided with more clear definitions and descriptions of the condition. Sports hernia has referred to groin and pubic injuries and dysfunctions, as well as abdominal wall disruptions. Clinical diagnosis and treatment has often been challenging because of the inconsistency in definitions, recognition of signs, symptoms, and optimal treatment approaches. A clinical article update published last year states that the term "sports hernia" is a misnomer as there is no classical herniation of soft tissue. The article further describes how the term has become synonymous with sportsman's hernia, athletic pubalgia, and Gilmore's groin.
Improved terminology to describe a sports hernia may be an "inguinal disruption" as referenced in this website of Dr. William Brown. (His site, www.sportshernia.com also includes anatomy images and descriptions of a sports hernia.)The anatomy most often involved is the oblique muscles and accompanying aponeurotic fascia, the adductor attachments to the pubic bone, and occasionally the pubic bone itself. Sports medicine literature, and research involving hockey players in particular, has been rich with reports of players who have had a repair of the aponeurotic fascia and/or oblique muscles, followed by a short period of rehabilitation and a full return to sport. Other commonly involved athletes are those who participate in football, soccer, and tennis. Any sport that may include explosive stops and starts with twisting, turning, and lower extremity rotations can result in a sports hernia.
Institute faculty member Steve Dischiavi has been on the front line of treating athletes with abdominopelvic injuries, and he has prepared an outstanding continuing education course complete with many videos, assessment techniques and intervention strategies. To learn more about differential diagnosis and treatment of the lumbo-pelvic-hip complex, join Dr. Dischiavi this August in Arlington, VA for Biomechanical Assessment of the Hip & Pelvis.
More than ever, patients are recognizing the value of training themselves to breath, pause, rest, relax. With the explosion in availability of free resources available on smart phones, computers, magazines and handouts, the public has increased access to tools with which they can apply concepts in relaxation training, mindfulness, and meditation techniques. Which is the best strategy for our patients? That answer depends on many factors, and the truth is, with the variety of patient presentations, goals, and strategies, the patient may need to simply trial a few different approaches.
A recent radio interview I heard mentioned calm.com as a resource for relaxation training, so I decided to check it out prior to recommending the site to patients. The site is simple, with the ability to listen to 2, 5, 10, 15, or 20 minutes of guided relaxation, set a timer for the same time intervals, and download an application for the iPhone. The site is visually calming, with a very clean and intuitive interface. My sense is that users would find the site very simple to access and utilize. A simple search on the iPhone application store using the terms "free relaxation" brings up nearly 900 apps. As most of our patients (and selves, friends, families) may benefit from focused, practiced breathing and calming practices, these resources are great to know about.
There is a science behind finding balance, and one resource that has integrated much of the science behind techniques in relaxation and balance is the Institute of HeartMath. The website describes physiological coherence as a state characterized by heart rhythm coherence, increased parasympathetic activity, increased entrainment and synchronization between physiological systems, and efficient functioning of the cardiovascular, nervous, hormonal, and immune systems. In pelvic rehabilitation, we know that increased parasympathetic activity is important for patients who present with pain, with bowel, bladder, or sexual dysfunction. An imbalance in the autonomic nervous system can affect all of the physiologic functions taking place to aid pelvic health.
Two of our upcoming courses, Meditation and Pain Neuroscience and Mindfulness-Based Biopsychosocial Approach to the Treatment of Chronic Pain offer insights into clinical research as well as practical applications of strategies to affect the autonomic nervous system and therefore physiological functions. These courses take place in September and November, sign up early to save your seats!
This post was written by H&W instructor Ginger Garner, MPT, ATC, PYT. Ginger will be instructing the course that she wrote on "Yoga as Medicine for Labor and Delivery and Postpartum" in Washington this August.
Note: This post is for colleagues, patients, and friends whose greatest desire is to have a healthy baby via natural childbirth. In this article, natural childbirth refers to an unmedicated delivery of your baby, assisted with natural, non-pharmaceutical means. While not all women have the luxury of natural childbirth, and some choose other means, please know that Ginger’s course supports all women and their personal decisions about birth.

My first natural birth was December 27, 2005. After a long, hard labor that started on Christmas, my son Michael arrived safe and healthy into my arms.
But something was missing.
I could have better prepared for birth. Bradley technique had reinforced that yoga was a wonderful way to relax and give into the sensations of contractions. Prenatal Pilates and walking, along with yoga, had also provided me with the endurance to go the long 36-hour distance during labor.
What was missing was my active, deliberate, and planned participation during birth.
A birth plan helps to organize your thoughts, but a mother needs her own, personal birth plan too. After Michael’s birth, I began to create my own future personal birth plan, which also changed the way I saw, and helped, my own prenatal patients.
That personal birth plan carried me beautifully (and with less pain and more control) through my next two births, William and James. An n of 2 (subject size of 2, in research terms) was small, but very soon after science began investigating the actual effects of using yoga for childbirth preparation and actual labor and delivery. The results are very promising, as I’ll discuss below.
Expectant women should work directly with an experienced physical therapist to create their own personal birth plan based on their individual mind-body needs. Mind-body needs should consider the following variables:
- Physical Labor Needs: Adapt labor and birth positions based on the patient’s specific orthopaedic injuries or aches and pains that can prevent focus or certain positioning during birth. This could include but is not limited to problems like hip impingment, shoulder impingement, sacroiliac joint pain, back pain, limitations in ROM, or existing pelvic pain.
- Psychoemotional/Physical Labor Needs: Consider previous birth trauma or history such as prior C-section, episiotomy, or difficulty with pain management or dilation that may affect labor progression.
- Psychoemotional/Energetic/Spiritual Labor Needs: Establish adequate birth support during labor. A 2012 Cochrane review of RCT’s found that women with continuous support were more likely to have a spontaneous vaginal birth, less likely to have pain medications, epidurals, negative feelings about childbirth, vacuum or forceps-assisted birth, and C-sections. Women with support also had shorter labors by 40 minutes, higher APGAR scores, and the best overall outcomes. Constant support means a mother has someone continuously at her side during the entirety of labor. That person must also be an active, knowledgeable participant in the labor process, not just a warm body taking up space.
- Intellectual Labor Needs: Educate the mother and her birth partner about how to execute the personal birth plan, which can include yogic breathing, a bevy of yoga posture options for individualized labor and birth positions, guided imagery and/or motor imagery techniques, and hands-on manual therapy techniques.
- Psychoemotional/Energetic Labor Needs: Address any previous birth or sexual trauma which could create anxiety and fear. Anxiety and fear of childbirth can prolong labor more than 90 minutes (Adams et al 2012).
Yoga is an amazing, proven method to directly diminish perceived pain during labor, immediate postpartum pain, and shorten labor duration, as well as improve maternal comfort and birth outcome scores, as found in a 2008 randomized trial of 78 pregnant Thai women.
Ginger’s course, Yoga as Medicine for Labor, Delivery, and Postpartum prepares the physical therapist to meet the needs of the laboring mother with an evidence-based mind-body holistic perspective, which includes designing individualized birth plans for labor and delivery. Future posts will also address the postpartum curriculum included in the course. To learn more about Ginger’s course, visit Yoga as Medicine for Labor, Delivery, and Postpartum.
Last week in our blog, you learned about Susannah Britnell, a physiotherapist who works in a multidisciplinary pelvic pain treatment setting. I learned of her clinic when I came across this journal article) about developing an interdisciplinary clinic for patients with endometriosis and pelvic pain. Below is Part 2 of the questions that she was kind enough to answer for us so that we can hear more from her perspective!

What do you find rewarding as a therapist in working in this setting?
Working with people in pain can be challenging but also extremely rewarding. I really value being able to help women realize what they can do, how they can shape their current life experience and their future. We provide tools and strategies that they can put into practice successfully. I love being able to be a part of moments when there is a shift in thinking, an opening of opportunity, when women who have seen nothing but barriers and hopelessness realize that there could be the possibility of positive change. I really find satisfaction in helping women perform daily activities, manage bladder, bowel and sexual pain concerns and increase overall activity and participation in life.
What would you say is powerful for the patients in terms of having the team available?
Patients have a great sense of support being a part of this team. Gynecological, musculoskeletal and psychosocial components are addressed with a synergistic approach. Patients are searching for answers and once they receive a diagnosis, whether its endometriosis, pelvic girdle pain, sensitization or a combination, this does help them to move forward. More often than not, the diagnosis will be a combination of gynecological, musculoskeletal, and psychosocial components, with central sensitization. When they are aware that appropriate full medical management has taken place, a readiness for change and acceptance of the active role self- management can be fostered. Our patients learn self management tools in our workshop and then we support them as they practice these and integrate them into their lives.
Our team ensures that our language and message is consistent, supportive and empowering. We work hard to avoid any language that perpetuates confusion, fear or loss of hope and we clarify any misinformation or myths patients have encountered in the past. So many women have had negative past medical experiences and feel they have not been heard, or they have been told their pain is not real. This is obviously distressing for them, so to have a team that listens, supports and then helps to give strategies for change can be a big relief.
If a concern or question comes up during a session, we can usually address this with the appropriate team member before the patient leaves the clinic. This is important as it saves time for the patient and practitioner, but also helps to resolve those unanswered questions or worries that can lead to rumination and anxiety.
Our team has weekly meetings to communicate about treatment plans, discharge planning and for problem solving particular concerns. This is invaluable for communication and helps to give our team cohesion.
What do you sense are some barriers to others creating this type of environment?
Funding would be a big barrier. The reality is that these programs cost money to run. Many of these women have experienced pain and disability for years, which of course affects all facets of life, including being able to work. They often are unable to pay for private treatment and so without a publically funded program they go without. It is challenging to decide how best to use our limited resources so that we can try to meet the needs of so many patients.
Another barrier is that there are not enough physiotherapists and counsellors that have the experience or even the interest in working with women with chronic pelvic pain, so ongoing community support and follow-up in the patient’s communities can be difficult. We have a yearly Fellowship program for gynecologists who have an interest in this area. Part of our outreach plan is to help provide educational opportunities for physicians, physiotherapists and counsellors in BC.
A common perception from the medical side is that there is no hope for these patients and that nothing can be done for them. Isolated practitioners have a high burn out rate working in the area of chronic pelvic pain. However, with a supportive team, working in this area can be rewarding and exciting.
In an ideal world, are there some disciplines that you would love to see added to this group?
It would be fabulous to have a yoga Instructor and a dietician trained in biopsychosocial approach to chronic pain.
Are there any particular patient populations or conditions you love to work with or learn about?
I love working with women with chronic pelvic pain, in particular chronic pelvic girdle pain, dyspareunia, and bladder and bowel pain.
Thank you to Susannah for sharing her knowledge and experiences in our blog! If you would like to contact Susannah she can be reached via email at sbritnell@cw.bc.ca, and her clinic website is www.womenspelvicpainendo.com. To discover more information about working with chronic female pelvic pain, you can attend one of our series courses such as Pelvic Floor Level 2B or our advanced course, Pelvic Floor Level 3. These courses always sell out, so sign up soon!
In patients with lumbar disc herniation, how many patients have sacroiliac joint dysfunction? Answering this question was the aim of a study published in the Journal of Back and Musculoskeletal Rehabilitation in 2013. From an outpatient clinic at a university hospital, 202 patients with lumbar disc herniation (paracentral or intraforaminal) on imaging and clinical findings suggesting lumbosacral nerve root irritation were included. Excluded were patients who pregnant, had prior lumbar surgery, osteoporosis, fractures, diabetes, severe hip DJD, and neurological deficits. Clinical examination tests for SIJ dysfunction included seated forward flexion test with palpation of the PSIS, Patrick-Faber test, long-sitting test, Gillet test, Sphinx test, and palpation tests for sacral base asymmetry. Pressure provocation tests were applied to the sacrum and the pelvic innominates, palpation to long dorsal sacral ligament and lumbosacral junction. "Positive" sacroiliac dysfunction diagnosis meant that the patient had a cluster of at least 4 anatomical and 2 provocative tests. Patients ranged in age from 19-70 years with a mean age of 42.
Greater than 72% of the patient sample with known lumbar disc herniation also presented with sacroiliac joint dysfunction. Females, patients with recurrent pain, those who performed heavy work, and patients with a positive straight leg raise test were more likely to have sacroiliac joint dysfunction. Of the 72% of patients who were diagnosed with SIJ dysfunction, nearly 60% were female. No correlation was found between the presence of sacroiliac joint disease, working hours, duration of low back pain, or body mass index and the rate of SIJ dysfunction. The authors conclude that sacroiliac joint dysfunction has a "…high possibility of occurrence in low back pain" and should be included in the clinical examination and decision-making process. They also point out that while the differential diagnosis of back versus SIJ pain is well-defined in manual medicine texts, the medical books do not highlight screening of the SIJ when presented with a patient who has back pain.
If you would like to learn skills to perform differential diagnosis of the sacroiliac joint, sign up for the Sacroiliac Joint Treatment continuing education course taking place this July in Baltimore with Peter Philip.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/








































