More than ever, patients are recognizing the value of training themselves to breath, pause, rest, relax. With the explosion in availability of free resources available on smart phones, computers, magazines and handouts, the public has increased access to tools with which they can apply concepts in relaxation training, mindfulness, and meditation techniques. Which is the best strategy for our patients? That answer depends on many factors, and the truth is, with the variety of patient presentations, goals, and strategies, the patient may need to simply trial a few different approaches.
A recent radio interview I heard mentioned calm.com as a resource for relaxation training, so I decided to check it out prior to recommending the site to patients. The site is simple, with the ability to listen to 2, 5, 10, 15, or 20 minutes of guided relaxation, set a timer for the same time intervals, and download an application for the iPhone. The site is visually calming, with a very clean and intuitive interface. My sense is that users would find the site very simple to access and utilize. A simple search on the iPhone application store using the terms "free relaxation" brings up nearly 900 apps. As most of our patients (and selves, friends, families) may benefit from focused, practiced breathing and calming practices, these resources are great to know about.
There is a science behind finding balance, and one resource that has integrated much of the science behind techniques in relaxation and balance is the Institute of HeartMath. The website describes physiological coherence as a state characterized by heart rhythm coherence, increased parasympathetic activity, increased entrainment and synchronization between physiological systems, and efficient functioning of the cardiovascular, nervous, hormonal, and immune systems. In pelvic rehabilitation, we know that increased parasympathetic activity is important for patients who present with pain, with bowel, bladder, or sexual dysfunction. An imbalance in the autonomic nervous system can affect all of the physiologic functions taking place to aid pelvic health.
Two of our upcoming courses, Meditation and Pain Neuroscience and Mindfulness-Based Biopsychosocial Approach to the Treatment of Chronic Pain offer insights into clinical research as well as practical applications of strategies to affect the autonomic nervous system and therefore physiological functions. These courses take place in September and November, sign up early to save your seats!
In patients with lumbar disc herniation, how many patients have sacroiliac joint dysfunction? Answering this question was the aim of a study published in the Journal of Back and Musculoskeletal Rehabilitation in 2013. From an outpatient clinic at a university hospital, 202 patients with lumbar disc herniation (paracentral or intraforaminal) on imaging and clinical findings suggesting lumbosacral nerve root irritation were included. Excluded were patients who pregnant, had prior lumbar surgery, osteoporosis, fractures, diabetes, severe hip DJD, and neurological deficits. Clinical examination tests for SIJ dysfunction included seated forward flexion test with palpation of the PSIS, Patrick-Faber test, long-sitting test, Gillet test, Sphinx test, and palpation tests for sacral base asymmetry. Pressure provocation tests were applied to the sacrum and the pelvic innominates, palpation to long dorsal sacral ligament and lumbosacral junction. "Positive" sacroiliac dysfunction diagnosis meant that the patient had a cluster of at least 4 anatomical and 2 provocative tests. Patients ranged in age from 19-70 years with a mean age of 42.
Greater than 72% of the patient sample with known lumbar disc herniation also presented with sacroiliac joint dysfunction. Females, patients with recurrent pain, those who performed heavy work, and patients with a positive straight leg raise test were more likely to have sacroiliac joint dysfunction. Of the 72% of patients who were diagnosed with SIJ dysfunction, nearly 60% were female. No correlation was found between the presence of sacroiliac joint disease, working hours, duration of low back pain, or body mass index and the rate of SIJ dysfunction. The authors conclude that sacroiliac joint dysfunction has a "…high possibility of occurrence in low back pain" and should be included in the clinical examination and decision-making process. They also point out that while the differential diagnosis of back versus SIJ pain is well-defined in manual medicine texts, the medical books do not highlight screening of the SIJ when presented with a patient who has back pain.
If you would like to learn skills to perform differential diagnosis of the sacroiliac joint, sign up for the Sacroiliac Joint Treatment continuing education course taking place this July in Baltimore with Peter Philip.
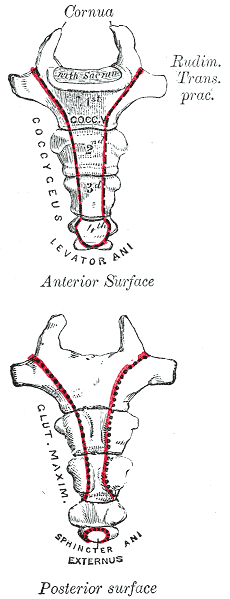
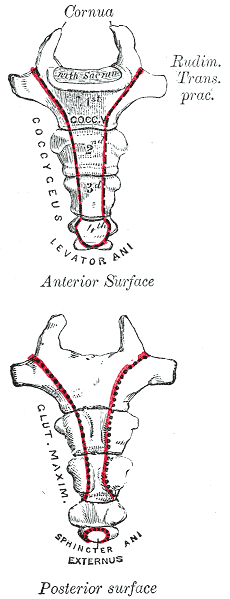
A recent publication of a case series proposes that clinicians use intranasal calcitonin, a medication prescribed for acute vertebral fractures in osteoporotic patients, for acute coccyx pain. This medication is administered as a nasal spray, has been demonstrated to have analgesic properties, and is theorized to have effects of beta-endorphin production, and inhibition of prostaglandin and cytokine production. Nasal calcitonin, a synthetic drug, is reported to have fewer and mild side effects when compared with the injectable form of the medication.
Of the 8 subjects treated and described in the case series, all had a fall on the tailbone, either landing hard into a chair on onto the stairs or floor. Some were seen within 3 months of injury date, and others were treated after 3 months from injury. The authors report that in the subjects who were treated acutely, 3 of 5 had at least 50% improvement in pain, without injections or surgery. The subjects treated in a chronic pain condition had similar levels of improvement but with the addition of coccyx injections for treatment.
Based on the lack of a control group, the small number of subjects treated, and because the mechanism of nasal calcitonin is unknown as far as effects on fracture healing in the coccyx, we would not, as rehab professionals, look to our referring providers to add nasal calcitonin routinely in the management of acute coccyx fracture. This article may, however, lead to interesting conversations with referring providers who are in a position to consider the addition of calcitonin for the proposed analgesic effect and potential bone healing augmentation. (The authors do suggest using the smallest effective dose for the shortest duration required.)
Clinically, is the difference in recovery for acute versus chronic coccyx pain of interest? Ideally, we would get to work with patients very soon after an injury, so that education is in place about self-care, self-treatment, optimal movement and thought patterns. The earlier that we can help a patient alleviate muscle tension and pain, and increase movement within tolerance, the better the outcomes usually are for the patient, as patterns of inactivity, fear, and muscle guarding are less likely to have set in. To learn much more about treatment of the coccyx, join faculty member Lila Abate in New Hampshire this September for the Coccyx Pain: Evaluation and Treatment continuing education course.
Earlier this year, when I came across this journal article about developing an interdisciplinary clinic for patients with endometriosis and pelvic pain, I was pleased to see that rehabilitation is included in this team setting. Upon reaching out to Susannah Britnell, physiotherapist, she agreed to answer some questions about her clinic and about her passion for pelvic rehab. Below you can read her responses to my questions. Stay tuned for Part 2 that will be published next week!

How long have you been working in the interdisciplinary clinic?
I’ve been working at the BC Women’s Centre for Pelvic Pain and Endometriosis in Vancouver, BC, since October 2012. We are a provincially funded program for women with chronic pelvic pain from all over the province of BC, Canada.
How long have you practiced?
I have been practicing since 1997 and love it! It is amazing how our practice can grow and move into different areas. We are truly lucky we have these opportunities.
What other settings have you worked in?
I have worked in hospital and private practice settings. I found my grounding in musculoskeletal physiotherapy, obtained my manual and manipulative therapy diploma in 2001, and worked in obstetrics for 10 years at BC Women’s hospital. I then started incorporating pelvic floor physiotherapy into my practice and developed a strong interest in chronic pain and the biopsychosocial approach to pain management. In addition to clinical practice, I teach the obstetrics component at UBC School of Rehabilitation as an annual guest lecturer and am an instructor for physiotherapy Rost Therapy courses for pelvic girdle pain, which I often co-instruct with Cecile Röst, a Dutch Physiotherapist.
How did you get involved with the interdisciplinary group?
Were you involved in the development of the center?
Our gynecologists, Dr Allaire and Dr Williams have been working at the Women’s Hospital and Health Centre for many years and identified the need for an interdisciplinary program for women with pelvic pain. After getting the funding in place, they hired a counsellor, physiotherapist, and nurse to be a part of the team. We now also have another gynaecologist, Dr Yong, as well as a Fellow. The gynecologists, counsellor, nurse, and myself along with administrative program manager worked together to develop the program. We have also had input from a Pain Specialist/anesthesiologist. I am so grateful and thankful to be a part of such a supportive and skilled team. As a physiotherapist, it truly is wonderful to have such support from the physicians
Our program consists of a full day workshop which includes pain education, life style changes, mindfulness based stress reduction and meditation techniques. We address fear of movement and give strategies for pacing and grading activity and we also include stretches, posture, and positioning advice. Women then book individual physiotherapy and counselling appointments so we can work on more specific concerns. Physiotherapy treatment may include some passive treatment techniques, but only as a bridge to more active self management. Patients will always have an active plan from the first visit. It is important that we don’t reinforce a sense that the woman needs someone to “fix” her concern and that she has no ability or power to make changes with her pain.
Our nurse is in contact with the patients from the beginning and is available if they have any questions as they go through the process. To learn more about the program, you can go to www.womenspelvicpainendo.com or contact Susannah at This email address is being protected from spambots. You need JavaScript enabled to view it..
To discover more information about working with chronic female pelvic pain, you can attend one of our series courses such as Pelvic Floor Level 2B, or our advanced course, Pelvic Floor Level 3
In Turkey, the rate of daytime urinary incontinence (DUI) was studied in primary school-aged children. A questionnaire was completed by parents of 2164 students. The Dysfunctional Voiding and Incontinence Symptoms Score Questionnaire was utilized and includes 14 questions about daytime and nighttime symptoms, voiding and bowel habits, and quality of life.
The population studied included approximately half boys and girls, with nearly half living in rural versus urban settings, and of a mean age of 10 years old. The overall prevalence of DUI was 8% (8.8% in girls, 7.3% in boys), and decreased with increasing age in this study population of children in 1st through 8th grades. 57.8% of those who did experience involuntary loss of urine were wetting less than 1x/day, 26.6% were wetting 1-2 times/day, and 15.6% were wetting greater than 2x/day. Urge incontinence was reported in nearly 59% of the children with DUI.
Independent risk factors for DUI included age, maternal educational level, family history of daytime wetting, urban versus rural setting, history of constipation or urinary tract infection (UTI), and urinary urgency. The authors conclude that "…educational programs and larger school-based screening should be carried out, especially in regions with low socioeconomic status." In this study, one of the strategies used to increase the survey response rate was to send medical and public health residents to the schools to speak about the study on 2 occasions.
Despite the numbers of therapists who have previously trained with educators such as faculty member Dawn Sandalcidi in her coursework for pediatric bowel and bladder function, the number of therapists focusing on pediatric pelvic health remains small while the need is great. Therapists who wish to expand community reach to pediatric urologists and pediatricians, and to serve the children who may unfortunately become adults who have bowel and bladder dysfunction, have the opportunity to attend the Pediatric Incontinence and Pelvic Floor Dysfunction continuing education course in Greenville, South Carolina this August.
In women with pelvic pain, is a pudendal nerve block effective, and how does the effectiveness correlate with findings of the history and clinical exam? These were the questions posed by a study published in 2012. Sixty-six patients were given a standardized pudendal nerve block, with Visual Analog Scores (VAS) and presence of numbness recorded prior to and up to 64 hours after the block. Inclusion criteria for the study involved having spontaneous or provoked pain in the distribution of the pudendal nerve, and patients were excluded if significant psychosocial issues, neurogenic or neuromuscular disorders, contraindication to sedation or allergy to utilized medication was present. A detailed history and physical examination was completed.
The pudendal nerve block was administered transvaginally and digitally, under sedation, in a lithotomy position. Following data collection, the researchers found that the presence of a positive Tinel's sign (palpation medial to the ischial spine for assessment of pain reproduction), a prior history of vulvovaginal candidiasis, or symptom worsening in the sitting position was associated with a return of the pain prior to the numbness wearing off. 92.4% of the subjects reported a "positive" response to the block, with varied lengths of time of symptom reduction. Nearly 87% of the subjects reported a reduction in one or more symptoms. This study only studied subjects for 64 hours, therefore it is not possible to discuss from this research the long-term implications of a pudendal nerve block in women with pudendal neuralgia. The authors did find a correlation between prior traumatic events including birth injuries, herniated discs, and fractures of the coccyx, pelvis or sacrum.
What does this research tell us about the role of pudendal blocks in the assessment and treatment of female pelvic pain? As already mentioned, the brevity of the data collection (only up to 64 hours) in addition to application of a non-guided block limit the ability to extrapolate this information to any long-term results. However, the correlations to clinical history and the return to pain prior to numbness ending may provide useful information as further clinical research is completed. The numbness was found to have inconsistent effects on a patient's symptoms such as bladder, bowel, sexual dysfunction, or sitting, and further research could measure the effects of a block on these functions. If you would like to discuss pudendal blocks with experts on pudendal dysfunction, sign up for the remaining spots in our August San Diego course!
Learn more about the Pudendal Neuralgia Assessment and Treatment course that we are holding at Comprehensive Therapy Services later this year.
A systematic review from July of 2013 addressed how interpersonal factors modulate pain. Four primary findings of the research that are found to affect pain-related responses are as follows: the degree to which social partners were active (or perceived to be able to be active), the degree to which participants could perceive the specific intentions of the social partners, the pre-existing relationship between the subject and the social partner, and individual differences in relating to others (including coping styles).
Some patients are negatively impacted by a partner who is attentive to pain, with increased reports of pain, worse pain outcomes when together versus alone, and with longer lasting pain states. On the other hand, some patients respond favorably to a partner's support, with lower reports of pain states when offered support such as holding the hand of a partner. Because each person's relationship and response to the pain within the context of the relationship varies, the impact of a partner on perceived pain is also varied. The authors, after describing details and evidence of pain modulation research, conclude the following: "Specifically, interpersonal exchanges affect precision or salience by socially signaling the safety or threat of the impending stimulus itself or the environment in which the stimulus occurs."
How can we take this information to heart within the pelvic rehabilitation practice? One of the ways that we offer support to a couple is by inviting a partner to attend a clinic session where he or she can learn to assist in application of soft tissue release techniques. The partner has the opportunity to be validated in both the gratitude that the therapist offers to the patient and partner for attending, and also in the fact that pelvic pain is commonly encountered. Because pelvic pain can interfere with a couple's intimacy, having such validation about the physicality of pain, when present, may be useful in a relationship. When a partner learns how to be of help in the healing process, this may also affect the factors mentioned in the cited research article, specifically, how partners are perceived to be able to be active or perception of specific intention.
It has been my clinical experience that partners are very specific in intention once being trained in how to help with pelvic pain, and that intention is to be a part of the healing process. It has also been an observation that if a partnership is struggling with their relationship, that issues can surface once asked to engage in pelvic muscle rehabilitation. This might mean that a patient chooses to pause rehabilitation and enter psychological counseling or other healing work. It also might mean that the patient chooses to not request help of the partner in the clinic or at home for the time being.
In relation to the pre-existing interpersonal factors, we do not necessarily know the extent to which the patient, partner, or the relationship has the ability to cope with challenges, or what type of relationship is in place. For that reason, we must remain nonjudgmental, and recognize that as rehabilitation professionals, we are limited by the scope of our practice and may serve the patient best by coordinating a referral to a counselor or psychologist. If you are interested in learning more about the research as well as the practical clinical implications of pain neurobiology, we still have a few seats left in our continuing education course titled Meditation and Pain Neuroscience. This course takes place in September in Illinois, and features an accomplished physical therapist as well as a psychiatrist. This course will offer an amazing learning experience as it combines the perspectives of medicine and rehabilitation, we hope you can join us!
Fascia is finally getting proper respect, rather than being that "white stuff" that was cut away during anatomy labs. Researchers continue to explore the cellular mechanisms and the total body functions that require healthy fascial layers. Fascial planes and connections are increasingly considered in strengthening programs as well, rather than only being considered in the design of stretching or flexibility programs. Tom Myers author of Anatomy Trains, and student of Rolfing founder Ida Rolf, contributes not only to the anatomical knowledge of therapists, but also to the functional applications of fascia in daily life and in exercise regimens.
Within the world of exercise training and physical fitness, muscles have often been considered in isolation, as is pointed out in this article written by Tom Myers in IDEA Fitness Journal. Yet muscles rarely work functionally as an isolated structure. Consider this fact when teaching pelvic floor muscle training. How many times have you instructed a patient to utilize thigh adductor muscles, exhale (respiratory diaphragm), or activate transversus abdominis to augment or facilitate the pelvic floor? While there is value in requesting that a patient focus on or emphasize a pelvic muscle contraction, or in teaching a patient to quiet dominant abdominals or gluteals, rarely do we find it effective to teach total isolation of a muscle in functional re-training.
Mr. Meyers uses anatomical information to drive the emphasis on fascial training, pointing out that there are ten times more sensory nerve endings in fascia than in muscles, and describes fascia as requiring our knowledge of accurate anatomy to engage the fascial planes as an "organ system of stability." Myers makes the case that fascia responds better to variation than to a repeated program when aiming to build fascial resilience. Varied tempo, varied loads, and varied movements are key to improving fascial health and efficiency. Integration of kinesthetic awareness via the fascial tissues rather than the muscles is also an important concept that is discussed- bringing awareness to movement through skin and superficial tissue movement rather than directing attention only to joint motion is another concept proposed for advancing movement training programs.
Considering these concepts may or may not change how you are currently designing your patients' fitness and rehabilitation programs, depending upon how you were trained and upon how you have continued to access continuing education and research. Breaking old habits and re-learning how to train movement does take effort on the part of the rehabilitation therapist, and fortunately, many instructors are integrating concepts of fascial planes into coursework. One such course that focuses clearly on integrating fascial training into sports-specific rehabilitation is Biomechanical Assessment of the Hip and Pelvis taking place this August in Arlington, Virginia. Instructor Steve Dischiavi, physical therapist and athletic trainer to the Florida Panthers, offers an excellent course that includes exercise concepts specific to the idea of fascial "slings" and that is sure to add some new exercises to your tool bag.

While information about "core" strengthening and pelvic dysfunction can be found in the athletic literature, often there remains a disconnect between the level of depth of knowledge among many of the coaches, trainers, and athletes when related to issues of urinary continence. The prevalence of urinary and fecal incontinence related to impact sports has been established, and it has been determined that having children is not a necessary precursor to developing symptoms of leakage. It has been my experience that the term "athlete" can mean different things to different professionals. For example, Institute founder Holly Herman has always been adamant about mothers as "athletes" regardless of the level of sport involved; the simple act of lifting strollers, car seats, children, grocery bags, and kneeling, squatting, lunging involved requires a significant level of athletic ability. With this in mind, knowing the actual requirements of the typical daily activities of any patient is critical to providing a meaningful rehabilitation approach.
So how is the pelvic floor related to athletics? Faculty member Michelle Lyons addresses this question in her new course (offered for the first time in the US this August in Ohio) titled The Athlete and the Pelvic Floor. The course is designed to "bridge the gap between pelvic floor therapists and sports medicine practitioners." Gender and sport specific issues will be covered, and participants will have the opportunity to combine concepts from respiratory, pelvic, and orthopedic perspectives.
With regards to urinary incontinence in female athletes, pelvic floor rehabilitation has been demonstrated to be an effective approach. In a study by Rivalta et al., three nulliparous women described urinary leakage during sport (volleyball) and daily life. Intervention included functional electrical stimulation with internal sensor completed 20 minutes 1x/week using a 50 Hz frequency, biofeedback 1x/week for 15 minutes, pelvic floor muscle exercises, and pelvic floor muscle exercises with a vaginal cone, all for three months. The vaginal cones were weighted, of three different weights, and used for up to 10 minutes at a time. Treatment adherence was recorded by a physician at a weekly visit. The pelvic floor muscle strengthening protocol used the "Kegel" protocol from 1952- at least 300 pelvic floor muscle contractions/day divided into six sessions, avoiding coactivation synergies. The chosen protocol is interesting to note as most therapists trained in pelvic rehabilitation would choose a functional approach to exercising, with less emphasis on avoiding co-contractions as long as the patient performs pelvic muscle contractions appropriately. The combination of biofeedback, and electrical stimulation, and cones is also not typical, yet is evidence that pelvic muscle strengthening in a relatively short period of time can ease symptoms of leakage with functional activities.
The good news is that all women at a four month follow-up were able to report involvement in sport and daily life without urinary leakage. All three women were also able to discontinue use of a panti-liner used to prevent leakage into clothing. Join Michelle Lyons as she covers a wide range of pelvic dysfunctions in athletes and how the best evidence combines with clinical practice pearls to get your patients back to function.
The goals of a recent research article were to determine the degree to which lower urinary tract symptoms (LUTS) are related to quality of life (QOL) and also the reliability of parents to accurately report on QOL disturbance in children who have urinary incontinence (UI). Outcomes tools utilized in the study include the Dysfunctional Voiding Symptom Score (DVSS) and the Pediatric Urinary Incontinence QOL tool (PIN-Q). Parents of forty children ages 5-11 (10 males and 30 females) and diagnosed with non-neurogenic daytime wetting completed the outcomes tools and responded to open-ended questions about incontinence and QOL. All children had daytime wetting, more than 50% of them had recurrent urinary tract infections (UTI's), and 89% reported urinary urgency.
According to the National Institute of Diabetes and Digestive and Kidney Disease (NIDDK), night-time wetting affects 30% of children who are 4 years of age, with the condition resolving in about 15% of children each year. Additionally, wetting at night persists in about 10% of 7 year-old, 3% of 12 year-olds, and 1% of 18 year-olds. A summary handout about Urinary Incontinence in Children is available here.
The study found that parents were reliable in reporting quality of life and symptoms in their children, as the outcomes scores completed were not different between them. (I would point out that nearly all parents involved were the patient's mothers; and it may be interesting to know more information about how the responsibility of managing urinary incontinence in children is shared among parents or caregivers.) Confirmed in the research was the knowledge that urinary dysfunction in children causes significant quality of life impact.
The subjective complaints of how some of the children avoid activities such as sleepovers, or worry that classmates can see or smell leakage is heartbreaking. The parents' complaints of feeling frustrated and angry about the issue is also understandable as there is a variable amount of support and understanding that each family has about how to manage the incontinence. A child's teacher or friends will also display a wide variety of supporting or sabotaging reactions that can add dramatic increases in stress. The authors point out that there is a significant "…need to improve teacher education and make attempts to engage the educational system to help these children."
If you would like to learn how to be a part of the solution, you can attend the Pediatric Incontinence and Pelvic Floor Dysfunction continuing education course taking place in August in South Carolina. It's the last chance to take the course this year!