When a woman is interested in a trial of labor after previous cesarean delivery (TOLAC), she and her health care providers will consider the pros and cons of delivery methods. Researchers have aimed to predict success with vaginal birth after cesarean section (CS), with the intention of limiting the risk factors for both the mother and the fetus. A failed trial of labor following a CS may be associated with higher maternal and perinatal morbidity, according to the American College of Obstetricians and Gynecologists (ACOG) practice bulletin.
The goal of a study published last year was to develop a model for predicting success in women desiring a vaginal birth after cesarean (VBAC) section. All women had one prior CS, all were carrying singletons. Transvaginal ultrasound was utilized to evaluate the Cesarean scar (CS) at 11-13, 19-21, and 34-36 weeks' gestation in 320 women. The measurement of the scar was termed residual myometrial thickness (RMT), and the measurements also included the change in RMT from the 1st to 2nd trimester. With increased evidence that CS healing and myometrial thickness in the lower uterus may improve success with VBAC, this study is the first to assess scar dimensions across the first and second trimesters.
The CS scar was visible in 89% of the women. Of these, 153 of the 284 were excluded from the prediction model development due to having had more than one prior cesarean delivery, so the hospital protocol of scheduling cesarean was followed. The remaining women were offered a vaginal birth trial, with 10 of the 131 undergoing CS prior to labor for varied reasons. The final count of women included in the analysis was 121, and of these cases, 74 had successful VBAC, 47 experience failed trials of labor, primarily due to fetal distress, failure to progress, or possible scar rupture. (In the women who did not have a visible scar, 82% had a successful vaginal delivery.)
The median residual myometrial thickness, or RMT, was higher in patients who had a successful VBAC. Clinical usefulness, according to the study, is that use of the model may lead to fewer emergency CS deliveries through identification of women who will be successful with VBAC.
The authors concluded that measurements of a CS, when applied to a mathematical model, can predict success of a vaginal birth after CS. This information may be very interesting to discuss with our referring providers, our colleagues, as well as our patients. Any research that sheds light on variables to predict success with a VBAC may promote vaginal deliveries and hopefully prevent emergency cesarean deliveries. Educating our patients so they can be more informed and advocate for themselves is a key role. While we are always mindful of not overstepping our scope of practice, such as advising a woman if she should choose one method of delivery over another, the information about the scar thickness in predicting VBAC success may be very useful to both her and providers. For more information about peripartum issues, check out our Peripartum Course Series on the course page. There is still time to sign up for the Care of the Postpartum Patient continuing education course later this month in Chicago!

A systematic review aimed to identify the burden of the most significant complications of postoperative abdominopelvic adhesions. Of the nearly 200 studies included in the review, the following categories were included: small bowel obstruction (n=125), difficulties during subsequent operation (n=62), infertility (n=11), and chronic pain (n=5). The incidence of postoperative small bowel obstruction, assessed among nearly 108,000 patients in 92 studies, was 9% overall. The incidence of adhesive small bowel obstruction was 2.4% and was highest in pediatric and in lower gastrointestinal tract surgery. The authors report a high rate of chronic abdominal pain in patients who were followed after lower gastrointestinal tract surgery, with adhesions identified as a significant cause of this pain. Following colorectal surgery for small bowel disease, pregnancy rates were found to be dramatically lower than the pregnancy rates in those who were medically treated. Additionally, patients who have had a prior surgery may require additional time in a subsequent procedure due to scar tissue, and adhesiolysis, used to break up adhesions, can lead to bowel injury.
Patients with postoperative adhesions, according to the systematic review, are most often treated by providers other than the one who did the surgery; the lack of awareness of the complication may be one reason that the incidence of adhesions is underestimated. The value of being aware of the higher incidence of postoperative adhesions may be in early recognition of a complication, surgical decision-making, and patient counseling. While the research is young in relation to adhesions and pelvic rehabilitation, one study that we previously discussed in the blog addresses visceral mobilization techniques in an animal model. While the animal model research is promising, there are numerous case reports describing the positive effects of visceral mobilization techniques for abdominopelvic pain, and therapists always report on the equally positive changes to their clinical practice outcomes after adding visceral techniques to their toolbox.
There are 2 upcoming opportunities to learn visceral mobilization: Level 1 in Scottsdale covering the Urologic system and Level 2 in Boston covering the reproductive system.
One of the questions we frequently receive at the Institute is "Do you have any research about ___________?" At times, therapists are looking for information that can help with patient care, or they might be looking for support in a claims denial letter, or foundational material for a presentation. If you have been taught how to find articles, this may seem like a simple task. Many of us therapists went to school when the only use of a computer was for word processing, if we were lucky enough to have progressed from the typewriter or even the electronic typewriter. (Imagine no Google, no Wikipedia, and no Amazon to purchase textbooks!) There are basic search skills that can be shared so that every person interested in a particular topic can find recent articles in free search engines. While the full article may not be available, many times you will have access to full articles that synthesize recent works. (One website that you can use that offers full text article access is PubMed Central.) If you are not interested in reading articles, but prefer to read a scholarly summary of a health topic, check out www.uptodate.com, where you can subscribe to have full access to excellent evidence-based summaries. You can read through the reference lists on the site as well to see if there is a resource that you want to track down.
One method of finding articles is to go to www.googlescholar.com. In the search bar, type in the topic you are interested in, such as "urinary incontinence." You will then be provided with a list of all articles that have urinary and/or incontinence in the title or in the key words of the research. An even more refined way to conduct your search is by using Boolean terms, in which you connect your search words by "AND" or other key terms. To see this in action, let's say you want to know if there is any research about urinary incontinence and prostatectomy surgery. Try completing a google scholar search by typing in the following: "urinary incontinence" AND "prostatectomy". (Be sure to use the quotation marks and type the word "AND" in capital letters.) You will see that you come up with some very nice articles about the specific topic you searched. To make sure you are looking at recent articles, go to the left side of the search page and under the words "Any time" choose an option such as "Since 2010" so that you are seeing articles from within the last 5 years. Next, maybe you want to know if there is evidence for rehabilitation. Add the word rehabilitation, like this: "urinary incontinence" AND "prostatectomy" AND "rehabilitation". You will see that you now have even more results specific to rehabilitation of the condition. On the right side of the page you might see a link that starts with [PDF] where, if you click on it, you will usually be brought to the full article rather than just the abstract. If you see an article that you think fits your search, you can also click on "Related articles" located under the brief description of the article.
Being able to look up articles serves many purposes, including staying updated on patient care, and discussing evidence with peers, providers, and patients. Another valuable reason to find your own research is when studying for certification exams such as the Pelvic Rehabilitation Practitioner Certification (PRPC). On the PRPC certification page on our website, you can find a list of some articles for which we have added links. (Remember that there is no need to print out articles anymore! Save a tree and simply save the articles as a PDF file. You can name the article by the author's last name, year and main topic, and store in a folder on your computer so it is easy to access- no file drawer required!) If you are thinking about taking the PRPC exam, there is no time like the present to get your application put together! The deadline for applying is October 1 of this year, with the test taking place in the first couple weeks of November. Personally, I have enjoyed reading the blog posts introducing therapists who have earned their PRPC title- the reasons for seeking the distinction are very interesting and meaningful. We would love to see your name on the list of certified therapists, so check out the details on the website and contact us if you have any questions about the PRPC application process!
In an article describing vascular dysfunction in women with chronic pelvic pain (CPP), Foong and colleagues describe the common finding of pelvic venous congestion. This study aimed to determine changes in microcirculatory function in women with chronic pelvic pain compared to controls. Eighteen women presenting with chronic pelvic pain of at least 1 year and 13 women without pelvic pain or congestion were evaluated for isovolumetric venous pressure, miscrovascular filtration capacity, and limb blood flow. All women were of reproductive age, menstruating regularly, and measurements were made during the mid follicular and the midluteal stages of the same 28 day cycle. The 18 women with CPP fit previously established criteria for pelvic congestion.
The women in the patient group were re-evaluated at 5-6 months following treatment for pelvic congestion, with treatment including medication-induced suppression of ovarian function for 6 months, and in 4 patients, hysterectomy and bilateral salpingo-oopherectomy. All of the patients received daily hormone replacement therapy (Premarin and Provera) "…to minimize the hypo-oestrogenic effects of treatment."
Findings of the research include an elevation in isovolumetric venous pressure, or Pvi in women with CPP compared to controls. Interestingly, there were no changes related to menstrual cycle in measures of microvascular filtration capacity and and limb blood flow. The conclusion of this study is that women with chronic pelvic pain may present with systemic microvascular dysfunction. The noted increase in Pvi "…may be attributable to systemic increases in post capillary resistance secondary to neutrophil activation." Following treatment for pelvic congestion, the value changes in isovolumetric venous pressure were no longer present.
This research highlights the noted changes in microcirculatory function in women with chronic pelvic pain. The obligatory chicken and egg conversation weighs in: does pelvic congestion lead to pelvic pain, or does pelvic pain always precede pelvic congestion? While the answer is probably that either condition can cause and perpetuate the other, as pelvic rehabilitation providers, our first thought might be: what would the research outcomes be if the treatment were not medication-induced ovarian suppression or surgery, but therapy directed to the pelvic pain and congestion? The Institute offered, for the first time last year, a course that allows the therapist to address pelvic pain through treatment of pelvic lymphatic drainage. The Lymphatic Drainage for Pelvic Pain continuing education course is a 2-day class instructed by Debora Hickman, a certified lymphedema therapist. Sign up now to save your seat in October in San Diego, and if you can't make this course, contact us to let us know you are interested in this special topics course, and we will keep you informed of any new course bookings!
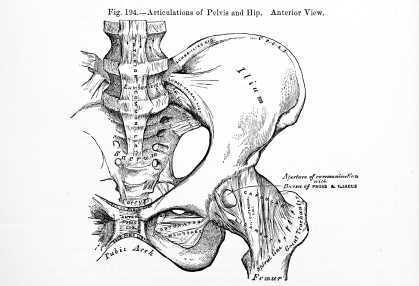
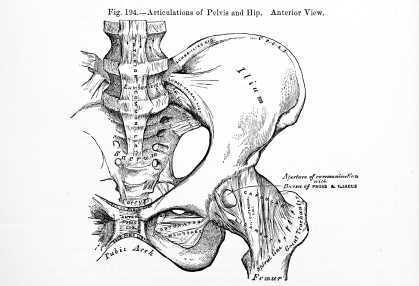
What structures may be implicated in posterior hip pain in the athlete? This question is addressed in a comprehensive article that can be accessed here. Complaints of posterior hip pain are increasingly common, and the differential diagnosis can include a variety of conditions and structures. The differential diagnosis of posterior hip pain may include hip extensor or hip rotator muscle strain, femoroacetabular impingement, proximal hamstring rupture, piriformis syndrome, and referral from the lumbar spine or sacroiliac joint, and systemic conditions such as cancer or infection, according to the article. To this list, could we add sciatic and other nerves in the buttock and pelvic floor, ischial injuries or ischial bursa irritation? With lists that include both systemic dysfunction and a variety of potential neuromusculoskeletal causes of posterior hip pain, the therapist must have a comprehensive ability to apply clinical reasoning, expert interview, and solid clinical examination and evaluation skills.
Posterior hip pain is only one type of hip pain, and one complaint within the world of pelvic pain. How does the therapist keep sharp tools for diagnosing musculoskeletal conditions, other connective tissue dysfunctions, as well as screen for disease conditions and other dysfunctions that can mimic hip or pelvic pain? Herman & Wallace has increased our offerings of courses towards differential diagnosis of hip and pelvic pain, including Biomechanical Assessment of the Hip & Pelvis, taught recently by Steve Dischiavi. (Stay tuned for Steve's upcoming course schedule!)
Another continuing education course that offers excellent opportunity to fine tune your skills in Differential Diagnosis of Pelvic Pain is coming up in October in Connecticut. The course is instructed by Peter Philip, who completed his Doctor of Science degree on the topic of Differential Diagnostics of Pelvic Pain. In addition to learning detailed anatomy and palpation skills, the participant can take away from the course a better understanding of embryology, the somatic and autonomic nervous system, and pelvic conditions that may be caused by or influenced by pelvic pain. The course will include both internal and external pelvic muscle examination techniques. With seven labs scheduled in this continuing education course, the participant will have abundant opportunities to practice instructed skills.

Insights in fascial mobility and dysfunctions are provided in this article by Gil Headley, and instructor who spends a significant amount of time working with anatomical dissections. Visceral fascia, according to Hedley, contains 3 layers: a fibrous outermost layer, a parietal serous layer, and a visceral serous layer. Fascial layers are, for the most part, designed to be able to slide over one another. Dysfunction can occur when there is a fixation in the connective tissues that prevents such sliding. A disruption in visceral fascial mobility may impair the necessary functional movement of the organs. Consider the mobility of the lungs and the heart when neuromuscular functions cause air or blood to expand and contract within the organ spaces. Bringing the concept to pelvic rehabilitation, what impairments are encountered when the bladder cannot easily fill or contract, or when movement of the bowels tugs on fascial restrictions? How are the tissues of the vaginal canal influenced by restrictions in tissues above, behind, or below the structure?
Examples of causes of adhesions may include (but not are limited to) inflammation from infections or disease, post-surgical scarring, dysfunctions caused by prior adhesion or limitation, and intentional therapeutic adhesions (think of a prolapse repair). While fibrous adhesions, once palpated, may be manually pulled apart, this is not the recommendation of the article author. Unfortunately, such an approach can result in further opportunity for inflammation and adhesions. One method of improving tissue mobility is to manually facilitate "…movement towards the normal range of motion of the fixed tissues with gentle traction…" timed with deep breathing. This technique may improve the ability of the organs and tissues to slide upon one another, and also may help in prevention of further movement restrictions. Would this type of intervention always require hands-on care? The author provides an example of a patient providing gentle traction by reaching to a pull-up bar, performing deep breathing and various trunk rotation positions following a thoracic surgery.
Visceral mobilization techniques may be a part of a patient's healing approach, and these techniques may be therapist-directed, patient-directed, or both. The Institute is pleased to offer two upcoming visceral mobilization continuing education courses next month instructed by faculty member Ramona Horton. Visceral Mobilization of the Reproductive System takes place in Boston, and Visceral Mobilization of the Urologic System is being hosted in Scottsdale.

What is the best reason to take a mindfulness or meditation course? Self-care! How many of us make choices in our daily lives that put our own health and wellness first? While we stay busy doing the important work of taking care of our patients, we can often forget to take care of ourselvs. Oftentimes, in addition to perhaps not learning to value self-care as we were growing up in our own families, we don't have strategies or the time-management skills to implement self-care. What is self-care? Self-care, as suggested by compassionfatigue.org, can include healthy lifestyle practices involving physical activity and healthy dietary habits, setting boundaries (saying "no"), having a healthy support system in place, organizing daily life to be proactive rather than reactive, reserving energy for worthy causes, and creating balance in life. (Check out this link for a prior blog post on compassion fatigue!)
The truth is, healthcare providers are stressed and burnout is common. So how does taking a course in mindfulness benefit the health care provider? Recent research including a university center based mindfulness-based stress reduction course was implemented with 93 providers including physicians, nurses, psychologists, and social workers. The training involved 8 weeks of 2.5 hour classes in addition to a seven hour retreat. Participants were instructed in mindfulness practices including a body scan, mindful movement, walking and sitting meditations, and were involved in discussions in how to apply mindfulness practices in the work setting. Outcomes included the Maslach Burnout Inventory and the SF-12. Results of the training, which was offered 11 times over a 6 year period, included improved scores relating to burnout and mental well-being.
But where can you take a course to learn valuable self-care tools? First up, there's the Meditation and Pain Neuroscience continuing education course happening at the beginning of next month. Then there is the Mindfulness-based Biopsychosocial Approach to the Treatment of Chronic Pain taking place in November in Seattle! Join us as we spread the word about how to not only take good care of your patients, but also of yourself.

While many of the Herman & Wallace Pelvic Rehabilitation continuing education courses focus on study of the pelvic floor muscles, the inclusion and consideration of the trunk, breathing, form and force closure, and posture are also needed to truly understand the pelvis. Our professional education does not prepare us well in regards to understanding the pelvic floor and pelvic girdle, and the foundational concepts that provide clinical meaningfulness come from a variety of research camps. If you feel that you were never provided this foundational information about the pelvic girdle and trunk, and wish to better apply practical concepts in movement and muscle facilitation (or inhibition), you might be looking for the Pelvic Floor/Pelvic Girdle continuing education course that is coming to Atlanta in late September.
The course covers interesting topics such as pelvic floor muscle activation patterns in health and in dysfunction, use of load transfer tests such as the active straight leg raise, orthopedic considerations of pelvic dysfunction, pelvic floor muscle (PFM) exercise cues, risk factors for pelvic dysfunction, and treatment of the coccyx. If you (or a friend you want to take a course with) is not quite sure about internal pelvic floor coursework at this time, the good news is that this course addresses pelvic dysfunction using an external approach. Experienced therapists can appreciate the research-based approach to muscle dysfunctions that can cause or perpetuate a variety of symptoms, and newer therapists have the chance to learn how to integrate pelvic floor/pelvic girdle concepts into current practice. A biofeedback lab introduces use of surface electromyography (sEMG) as well.
There is still time to sign up for the September course in Atlanta, the only remaining opportunity to take the Pelvic Floor/Pelvic Girdle continuing education course this year. Bring a friend, or a colleague, and work together to combine external and internal approaches to pelvic dysfunction.
In this study investigators tested the hypothesis that following hip arthroscopy, the number of patients who developed pudendal neuralgia would exceed 1%. Development of pudendal neuralgia symptoms following hip arthroscopy was assessed in 150 patients (female = 79, male = 71) who were operated on in one facility by a single surgeon. Indications for the surgery included post-trauma foreign-body, osteochondromatosis, and labral lesion resection. The Nantes criteria were utilized for diagnosis, which includes as "essential" criteria the following: pain in the region of the pudendal nerve; pain that is worsened by sitting, relieved by sitting on a toilet seat; pain does not interrupt sleep, pain with no objective sensory impairment and that is relieved by a pudendal nerve block.
The operated hip was placed in a position of 30 degrees of adduction, internal rotation and flexion. The hip was operated on with a single anterolateral approach in most cases, with a second anterolateral approach needed in eight cases. Study results include an incidence rate of 2% in the population of 150 patients. 3 of the patients (2 female, 1 male) were diagnosed with pudendal neuralgia presenting in all 3 as "pure sensory" with symptoms of perineal hypoesthesia and dysesthesia on the operated side. The 3 cases resolved spontaneously within 3 weeks to 6 months. Two cases of sciatica following hip arthroscopy were documented, and these cases resolved without intervention other than a short course of analgesics. The patients also presented with gluteus medius insertion tenderness.
Although the study also aimed to determine risk factors for development of pudendal neuralgia following hip scope, the small number of patients who developed symptoms made the analysis for risk factors difficult. The authors also point out that the one-way surgical technique (not the standard surgical technique) also may have created some bias in the study. In conclusion, although the cited study reported a low incidence of pudendal neuralgia onset following hip arthroscopy, larger numbers have appeared in the literature, and according to the authors, surgical risk factors for developing nerve complications following a hip scope include the amount of traction placed on the joint, the length of surgery, and appropriate pelvic support bilaterally. The take-home point for pelvic rehabilitation providers is that patients are at some risk for pelvic nerve dysfunction following hip arthroscopy, and we have a role in educating providers and in screening patients for such conditions.
The Herman & Wallace Pelvic Rehabilitation Institute offers many relevant courses regarding the hip and pelvis, and if you are interested in learning more about the pudendal nerve, hurry to sign up for the continuing education course "Pudendal Neuralgia Assessment, Treatment, and Differentials." You can also attend "Biomechanical Assessment of the Hip & Pelvis" continuing education course to learn all about testing, treatment, and diagnosis of the hip and pelvis.

The term "sports hernia" has been used over time to describe a variety of issues, and the medical and rehabilitation community has recently been provided with more clear definitions and descriptions of the condition. Sports hernia has referred to groin and pubic injuries and dysfunctions, as well as abdominal wall disruptions. Clinical diagnosis and treatment has often been challenging because of the inconsistency in definitions, recognition of signs, symptoms, and optimal treatment approaches. A clinical article update published last year states that the term "sports hernia" is a misnomer as there is no classical herniation of soft tissue. The article further describes how the term has become synonymous with sportsman's hernia, athletic pubalgia, and Gilmore's groin.
Improved terminology to describe a sports hernia may be an "inguinal disruption" as referenced in this website of Dr. William Brown. (His site, www.sportshernia.com also includes anatomy images and descriptions of a sports hernia.)The anatomy most often involved is the oblique muscles and accompanying aponeurotic fascia, the adductor attachments to the pubic bone, and occasionally the pubic bone itself. Sports medicine literature, and research involving hockey players in particular, has been rich with reports of players who have had a repair of the aponeurotic fascia and/or oblique muscles, followed by a short period of rehabilitation and a full return to sport. Other commonly involved athletes are those who participate in football, soccer, and tennis. Any sport that may include explosive stops and starts with twisting, turning, and lower extremity rotations can result in a sports hernia.
Institute faculty member Steve Dischiavi has been on the front line of treating athletes with abdominopelvic injuries, and he has prepared an outstanding continuing education course complete with many videos, assessment techniques and intervention strategies. To learn more about differential diagnosis and treatment of the lumbo-pelvic-hip complex, join Dr. Dischiavi this August in Arlington, VA for Biomechanical Assessment of the Hip & Pelvis.