Have you ever gambled with what you thought was gas, only to find out that it was not? When my son was little, he asked me one day, “Mom did you ever try to fart, but it wasn’t really a fart?” At the time, I told him it was called a “shart.” Of course, being a little boy, he thought that was funny. However, being an adult and thinking you are passing gas, and it not be only gas can be mortifying. Think about how that could affect your quality of life and ability to go out in public. If you can’t trust your anal sphincters and anal canal to not know what you are letting go, it can be stressful!
What can lead to confusion and issues with sensation in this area? There are many different reasons that this area may not function ideally and be able to identify what is within the anal canal. These reasons can range from surgery in the area, radiation therapy, more minor procedures such as hemorrhoid treatment, and even chronically ignoring the urge to defecate. When sensation changes, the function of the sampling response and rectoanal inhibitory reflex (RAIR) or sampling response is changed.
The sampling response is when a small amount of fecal matter accumulates in the rectum, and a stretch occurs in the area. This then triggers a relaxation of the internal anal sphincter, and a contraction of the external anal sphincter that allows a small amount of the fecal matter to drop down into the anal canal. The contents of fecal matter are sampled, and it is determined if it is solid, liquid, or gas. If it is gas, then we can select to expel it; if it is liquid we usually respond with a stronger contraction of the external anal sphincter to hold it in. If it is solid, we can determine whether or not it is a good time to go. If it is, then we head to the restroom; if it is not, we engage the rectoanal inhibitory reflex and hold the stool until we decide there is a better time. You can see, if this sampling and identifying of the contents is off and not functioning properly, then we can have some issues arise and situations with “sharts” that would not be ideal!
We as pelvic rehab clinicians are the perfect people to help people when their sensation is not optimal, and they may have some issues with fecal and flatulence incontinence. Using rectal balloon catheters has been a game changer in my practice when working with these patients that have issues with sensation in their anal canal. The balloon retraining helps with retraining sensation in this area. I use it along with strengthening the pelvic floor and external anal sphincter; along with any manual therapy that may be needed, and defecation training. The addition of the balloons allows me to address sensation. The use of adding or removing small amounts of air in an inflated balloon allows the patient to learn what changes in sensation in the area feel like, which improves sensation and awareness of the contents within the anal canal. If you think about it, there isn’t another way to treat sensation inside of the anal canal. If we can retrain sensation, then we can make it less likely for a patient to think they are safe with expelling gas but be surprised when more comes out!
Join me for the May 17th course offering of Anorectal Balloon Catheters- Intro and Practical Applications. In this short course, you will learn how to use balloon catheters and even practice a lab using balloons. The purchase of a balloon is needed before the course so that you can participate in the labs. This course can change how you treat your patients who may suffer from fecal incontinence and constipation.
AUTHOR BIO
Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC
 Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC (she/her) has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health, including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC (she/her) has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health, including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
In 2009, Allison collaborated with the Primal Pictures team for the release of the Pelvic Floor Disorders program. Allison's publications include “The Use of Transabdominal Ultrasound Imaging in Retraining the Pelvic-Floor Muscles of a Woman Postpartum.” Physical Therapy. Vol. 88, No. 10, October 2008, pp 1208-1217. (PMID: 18772276), “Beyond the Abstract” for Urotoday.com in October 2008, “Posters to Go” from APTA combined section meeting poster presentation in February 2009 and 2013. In 2016, Allison co-authored a chapter in “Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies.”
Allison works in the Denver metro area in her practice, Inspire Physical Therapy and Wellness, where she works in a more holistic setting than traditional therapy clinics. In addition to instructing Herman and Wallace on pelvic floor-related topics, Allison lectures nationally on lymphedema, cancer-related changes to the pelvic floor, and the sacroiliac joint. Allison serves as a consultant to medical companies and physicians.
Outside of work, Allison enjoys spending time with her family, caring for her animals, reading, traveling, and most importantly of all, being a mom! She lives in the Denver metro area with her family.
Lila Abbate PT, DPT, OCS, WCS, PRPC is the creator and instructor of Bowel Pathology Function & Dysfunction and the Pelvic Floor, a course which instructs in comprehensive evaluation and treatment techniques for bowel pathologies and dysfunctions, including fecal incontinence, chronic constipation, and the relationship between constipation and rectal and/or abdominal pain. Join Dr. Abbate in one of five events taking place in 2020!
Bowel dysfunction can be very rewarding to treat. Most pelvic health physical therapists are nervous about diving into bowel treatment. When I was training with my mentor, Elise Stettner, PT she used to remind me that “any PT can treat urinary symptoms. The patients who are really suffering are those bowel dysfunctions.” That statement really stuck with me and mentoring with her and treating those patients created a passion for treating patients who suffer from bowel dysfunction.
 Within the term bowel dysfunction, fecal urgency, is a common symptom and is under-researched. In 2019, Similis, et al published A Systemic Review and Network Meta-Analysis Comparing Treatments for Faecal Incontinence, doesn’t even mention physical therapy and pelvic floor muscle rehabilitation as an intervention for fecal incontinence and fecal urgency treatment.
Within the term bowel dysfunction, fecal urgency, is a common symptom and is under-researched. In 2019, Similis, et al published A Systemic Review and Network Meta-Analysis Comparing Treatments for Faecal Incontinence, doesn’t even mention physical therapy and pelvic floor muscle rehabilitation as an intervention for fecal incontinence and fecal urgency treatment.
Anecdotally, I have a lot of pelvic health patients and even generalized orthopedic patients who report that having bowel urgency is a more apparent symptom in their life after having a back or hip surgery. What started as a once-in-a-while problem, fecal urgency has crept up and become the new normal in their lives. They have subliminally re-routed their day to accommodate their bowel movements in order avoid incidences and accidents whether its waiting to eat breakfast until they get to work, waiting to drink a favorite drink until they are near a toilet or taking supplements before bed to empty their bowels before they start their day in order to avoid accidents during their day. Learning to treat bowel urgency can tremendously help patients regain control and abolish their symptoms.
Bowel urgency has many parallels to urinary urgency. The colon is giving the signal too soon, potentially at an inappropriate time, and the muscles need to be strong enough to hold the urge of defecation back in order to postpone. The failure occurs when one part of the continence mechanism fails. Bowel Pathology Function & Dysfunction and the Pelvic Floor course helps you to learn how to treat and guide your patients and conquer all types of bowel dysfunction.
Similis et al, A systematic review and network meta-analysis comparing treatments for faecal incontinence. Int J Surg. 2019 Jun;66:37-47. doi: 10.1016/j.ijsu.2019.04.007. Epub 2019 Apr 22.
For over 25 years my practice has had a focus on children suffering from bloating, gas, abdominal pain, fecal incontinence and constipation. Functional Gastrointestinal Disorders (FGID) are disorders of the brain -gut interaction causing motility disturbance, visceral hypersensitivity, altered immune function, gut microbiota and CNS processing. (Hyams et al 2016). Did you know that children who experience chronic constipation that do not get treated have a 50% chance of having issues for life?
 The entire GI system is as amazing as it is and complicated. Its connection to the nervous system is fascinating, making it a very sensitive system. In her book GUT, Giulia Enders talks about Ninety percent of the serotonin we need comes from our gut! The psychological ramifications of ignoring the problem are too great (Chase et el 2018). Last year an 18-year-old patient of mine had to decline a scholarship to an Ivy League University because she needed to live at home due to her bowel management problem.
The entire GI system is as amazing as it is and complicated. Its connection to the nervous system is fascinating, making it a very sensitive system. In her book GUT, Giulia Enders talks about Ninety percent of the serotonin we need comes from our gut! The psychological ramifications of ignoring the problem are too great (Chase et el 2018). Last year an 18-year-old patient of mine had to decline a scholarship to an Ivy League University because she needed to live at home due to her bowel management problem.
Unfortunately, FGID conditions can lead to suicide and death. Over 15 years ago my children’s pediatrician told me about an 11-year-old boy who hung himself because he had encopresis. In 2016 a 16-year-old girl suffered a cardiac arrest and died because of constipation.
The problems with children are different than for adults and need to be addressed with a unique approach.
How do physical therapists treat pediatric FGID?
- Have a solid foundation in the gastrointestinal system
- Coordinate muscle functions from top to bottom!
- Identify common childhood patterns
- Learn treatment techniques and strategies to address the issues specifically
Study and understand gastrointestinal anatomy, physiology, function and examination techniques. The entire GI system is as amazing as it is complicated. Its connection to the nervous system is fascinating, making it a very sensitive system. Ninety percent of the serotonin we need comes from our gut! The psychological ramifications of ignoring the problem are too great.
What do the Pelvic Floor Muscles (PFM) have to do with it?
Encopresis leads to a weak internal/external anal sphincter and pelvic floor muscles and constipation leads to pelvic floor muscles that can’t relax. Confused? When the Rectal Anal Inhibitory Reflex or RAIR fails from bypass diarrhea the sphincter muscles relax, and feces leaks out. This constant leakage leads to weak sphincter and pelvic floor muscles. When it happens on a regular basis most children don’t feel it, however their peers smell it and life changes.
My course, Pediatric Functional Gastrointestinal Disorders, teaches how to coordinate the muscle function based on the tasks required.
How did this start?
One painful bowel movement can lead to withholding for the next due to fear of the pain happening again. The muscles of the pelvic floor then tighten to hold the poop in. This actually does not make the muscle strong but instead makes it confused. The muscle then is controlled by the consistency of poop being too hard and painful to let out or too loose and not able to hold in.
Managing functional GI disorders is a process. It takes the bowel a long time to re-train and it requires patience and skill to know how to do it. Many therapists and patients themselves get frustrated and compliance fails. This is mostly due to lack of knowing how to titrate medications and give the bowel what it needs (other than proper nutrition that is!) It's like retraining a person to walk after a stroke, the brain needs to relearn normal bowel sensations.
Most families don’t realize how severe constipation can be. It is an insidious problem that gets ignored until it is too late.
Typically, what I hear from parents is their child was diagnosed with constipation and was advised to take a daily laxative. So, which one is the best one? How do they all work? Once leakage occurs again the laxative is discontinued as we think the bowel must be empty and this medication is causing the leaks which is counterproductive. Now the frustrating cycle of backing up or being constipated begins again. The constipation returns, the laxative is restarted, the loose stool leaks out and the laxative is stopped and that is the REVOLVING DOOR or what I refer to as children riding the “Constipation Carousel”. The bowel is an amazingly beautiful, smart but also sensitive organ that does not like this back and forth and therefore will not learn how to be normal. In the meantime, they experience distended abdomens and dysmorphia ending up in eating disorder clinics. I had an 11-year-old girl taking Amitriptyline for abdominal pain all because of a pressure problem in the gut not knowing how to work the pelvic floor with the diaphragm and her core.
No two children are the same and no two colons are the same. Laxatives need to be titrated to the specific needs of your child’s colon and motility of their colon not their age or body weight.
The success in getting children to have regular bowel movements of normal consistency without any fecal leaks is based not only teaching how to titrate laxatives but also how to sense urge, become aware of the pelvic floor muscles and learn how NOT to strain to defecate, retrain the core and diaphragm with the ribcage and integrate developmental strategies for function. Teaching Interoception- what my body feels like when I have an urge- is an important part of this course. This is especially important for those children born with anorectal malformations or congenital problems such as imperforate anus or Hirschsprung’s Disease.
In this class we use visceral techniques, manual therapy techniques, sensory techniques and neuromuscular reeducation and coordination to retrain the entire system.
Come and explore the amazing gut with me and learn how to improve the health and well-being of your patients, in Pediatric Functional Gastrointestinal Disorders!
1. Hyams, JS, et al. Childhood Functional Gastrointestinal Disorders: Child/Adolescent. Gastroenterology volume 150, 2016;1456-1468.
2. Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features and rome IV. Gastroenterology 2016;150:1262-1279
3. Robin SG, Keller C, Zwiener R, et al. Prevalence of Pediatric Functional Gastrointestinal Disorders Utilizing the Rome IV Criteria. J Pediatr 2018; 195:134.
4. Koppen IJN, Vriesman MH, Saps M, Rajindrajith S, Shi X, van Etten-Jamaludin FS, Di Lorenzo C, Benninga MA, Tabbers MM. Prevalence of Functional Defecation Disorders in Children: A Systematic Review and Meta-Analysis. J Pediatr. 2018 Jul;198:121-130.e6. doi: 10.1016/j.jpeds.2018.02.029. Epub 2018 Apr 12.
5. Zar-Kessler C, Kuo B, Cole E, Benedix A, Belkind-Gerson, J. Benefit of pelvic floor physical therapy in pediatric patients with dyssynergic defecation constipation. 2019 Dig Dis https://doi.org/10.1159/000500121/
6. Chase J, Bower W, Susan Gibb S. et al. Diagnostic scores, questionnaires, quality of life, and outcome measures in pediatric continence: A review of available tools from the International Children’s Continence Society. J Ped Urol (2018) 14, 98e107
After completing an intake on a patient and learning that her history of constipation started about 3 years ago with insidious onset, the story wasn’t really making any sense of how or why this started. Yes, she was menopausal. Yes, she seemed to be eating fiber and drinking water. Yes, she got a bowel movement urge daily, but her bowel movements felt incomplete. Yes, she was a little older, using Estrace cream, and her mobility had slowed down, but nothing seemed to make sense in the story that was leading me to believe it was an emptying problem or a stool consistency issue. She had a bowel movement urge, she could empty, but it was incomplete.
 So, after explaining about physical therapy, the muscle problems involved and what we do here, it led us to the physical examination portion. I explained that we check both the vaginal and rectal pelvic floor muscle compartments to determine rectal fullness internally, check for a rectocele, check for muscle lengthening (excursion) and shortening (contraction). She was on board and desperate to find an answer. She was eager for me to help her find an answer to her emptying problem that she had for the last 3 years.
So, after explaining about physical therapy, the muscle problems involved and what we do here, it led us to the physical examination portion. I explained that we check both the vaginal and rectal pelvic floor muscle compartments to determine rectal fullness internally, check for a rectocele, check for muscle lengthening (excursion) and shortening (contraction). She was on board and desperate to find an answer. She was eager for me to help her find an answer to her emptying problem that she had for the last 3 years.
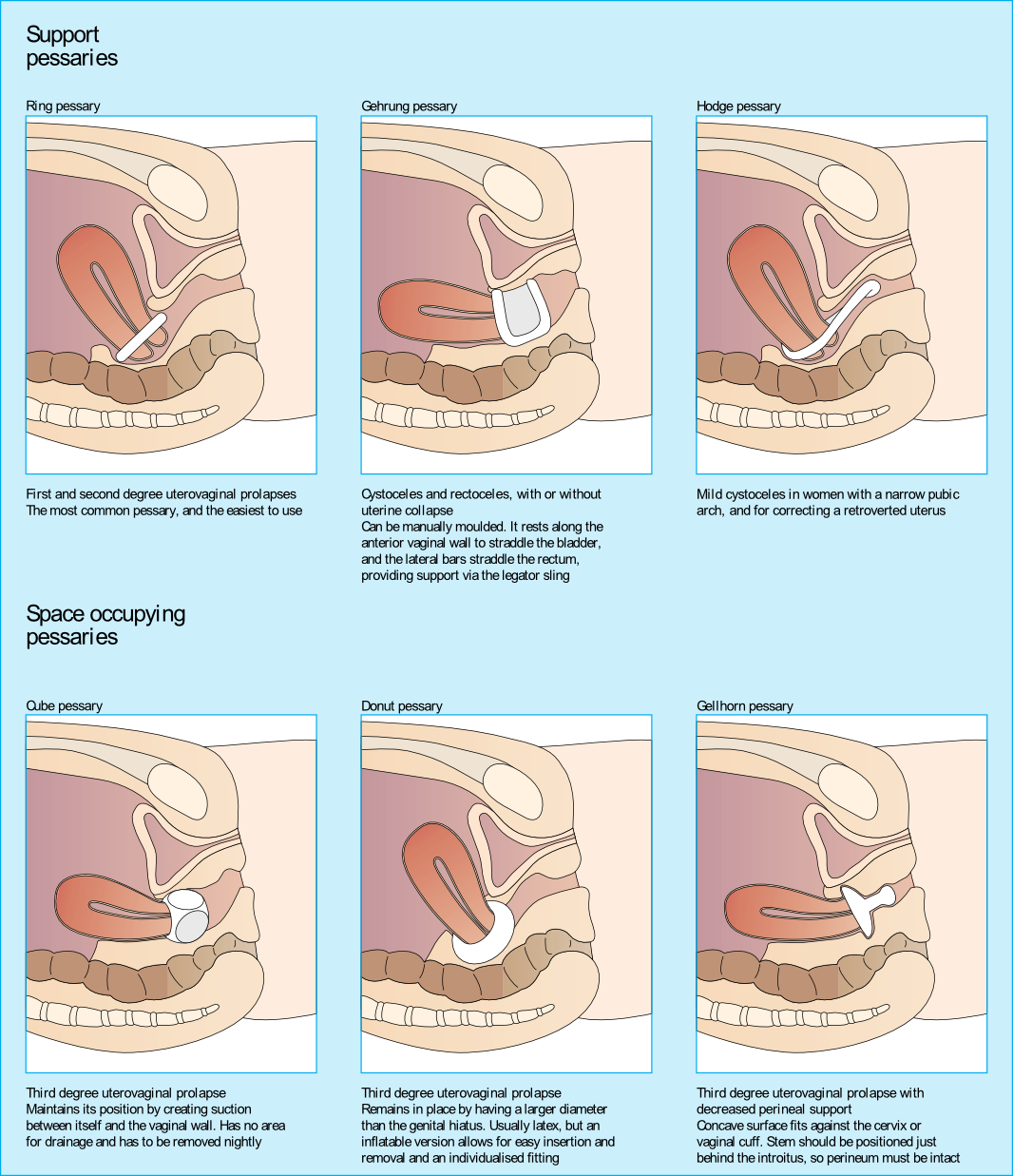
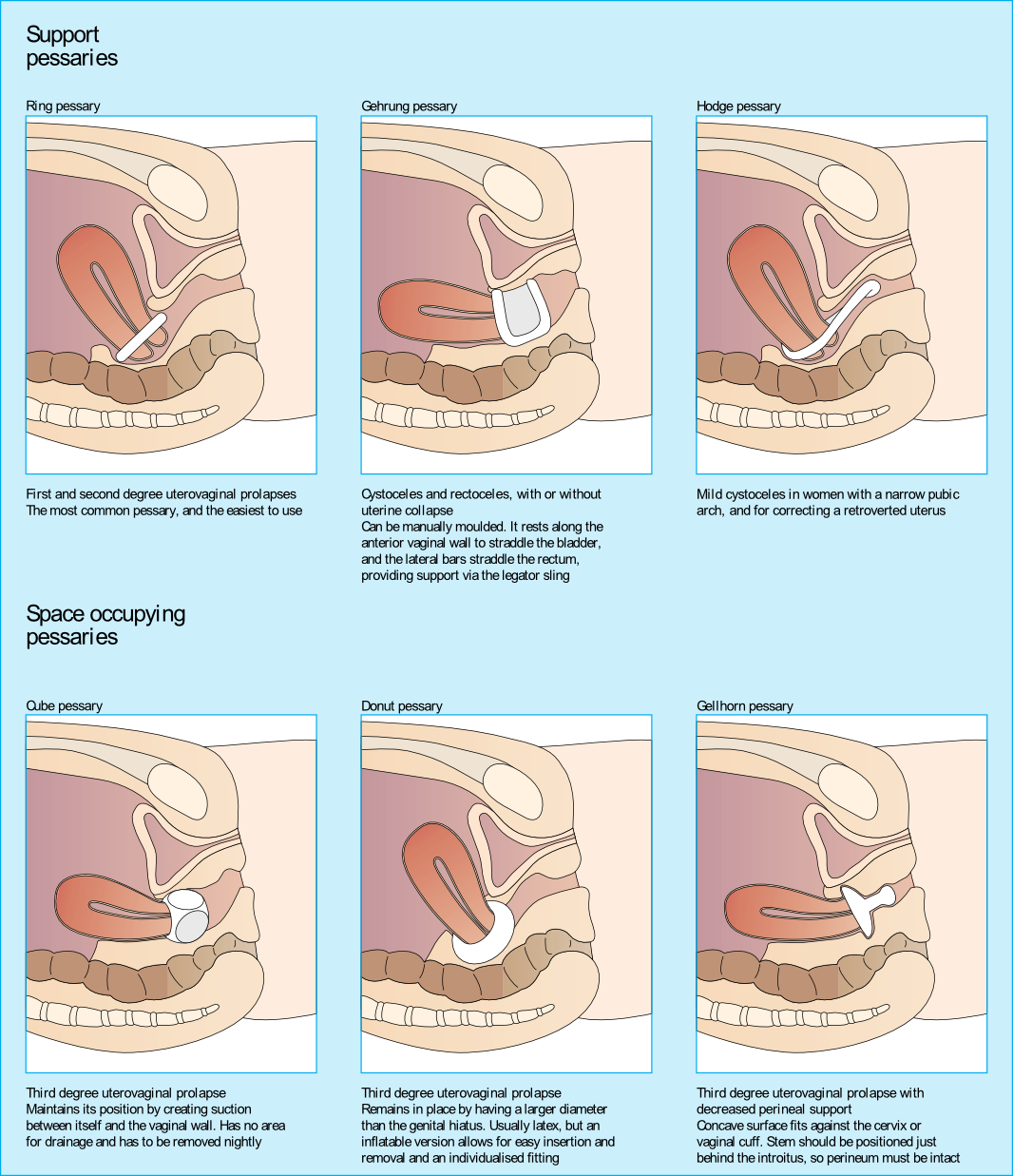
Upon entering her vaginal canal slowly, I start to move around and felt a ring of plastic. “Are you wearing a pessary?” I asked. “Pessary? Oh, yes, I forgot to tell you about that!”, she exclaimed. “How long have you been using it?” I asked. “About 3 years…” she answered.
I sent her back to the urogynecologist to get fit for another type of pessary as her muscle examination proved to be negative. Since that time, I have added the question “Do you wear a pessary?” as part of the constipation intake questions. Pessary use creates the ability for a patient to forgo or to extend their time for a surgical intervention due to pelvic organ prolapse.
Looking at the dynamics of the pessary, it may block bowel movement emptying. The recent study by Dengle, et al, published in the October 2018 in the International Urogynecological Journal confirms this anecdotal, clinical finding. The article, Defecatory Dysfunction and Other Clinical Variables Are Predictors of Pessary Discontinuation, looked at reasons for discontinuation of pessary use from April 2014 to January 2017 and did a retrospective chart review on a selected 1071 women. Incomplete defecation had the largest association with pessary discontinuation.
While there are over 20 sizes of pessaries on the market, patients will discontinue use without having a better conversation with their practitioner. From a PT perspective, when the patient comes in with bowel emptying issues, if no muscle dysfunction is found, it needs to be brought to the provider’s attention. Our role in educating the patient on the options that are available and creating this dialogue can prove to be very helpful in those suffering from pelvic organ prolapse and defecatory dysfunction.
Dengler, EG et al. "Defecatory dysfunction and other clinical variables are predictors of pessary discontinuation." Int Urogynecol J. 2018 Oct 20. doi: 10.1007/s00192-018-3777-1. https://www.ncbi.nlm.nih.gov/pubmed/30343377
When I bring up the topic of pelvic floor dysfunction in athletes, stress urinary incontinence (SUI) is usually the first aspect of pelvic health that springs to mind – and rightly so, as professional sport is one of the risk factors for stress urinary incontinence Poswiata et al 2014. The majority of studies show that the average prevalence of urinary incontinence across all sports is 50%, with SUI being the most common lower urinary tract symptom. Athletes are constantly subject to repeated sudden & considerable rises in intra-abdominal pressure: e.g. heel striking, jumping, landing, dismounting and racquet loading.
What’s less often discussed is the topic of gastrointestinal dysfunction in athletes. Anal incontinence in athletes is not well documented, although a study from Vitton et al in 2011 found a higher prevalence than in age matched controls (conversely a study by Bo & Braekken in 2007 found no incidence). More recently, Nygaard reported earlier this year (2016) that young women participating in high-intensity activity are more likely to report anal incontinence than less active women.
A presentation by Colleen Fitzgerald, MD at the American Urogynecologic Society meeting in 2014 highlighted the multifaceted nature of pelvic floor dysfunction in female athletes, specifically in this case, triathletes. The study found that one in three female triathletes suffers from a pelvic floor disorder such as urinary incontinence, bowel incontinence and pelvic organ prolapse. One in four had one component of the "female athlete triad", a condition characterized by decreased energy, menstrual irregularities and abnormal bone density from excessive exercise and inadequate nutrition. Researchers surveyed 311 women for this study with a median age range of 35 – 44. These women were involved with triathlete groups and most (82 percent) were training for a triathlon at the time of the survey. On average, survey participants ran 3.7 days a week, biked 2.9 days a week and swam 2.4 days a week.
Of those who reported pelvic floor disorder symptoms, 16% had urgency urinary incontinence, 37.4% had stress urinary incontinence, 28% had bowel incontinence and 5% had pelvic organ prolapse. Training mileage and intensity were not associated with pelvic floor disorder symptoms. 22% of those surveyed screened positive for disordered eating, 24% had menstrual irregularities and 29% demonstrated abnormal bone strength. With direct access becoming a reality for many of us, we must acknowledge the need for specific questioning when it comes to pelvic health issues, as well as the ability to recognise signs and symptoms of the female athlete triad in our patients.
Want to learn more about pelvic health for athletes? Join me in beautiful Arlington this November 5-6 at The Athlete and the Pelvic Floor!
J Hum Kinet. 2014 Dec 9; 44: 91–96 Published online 2014 Dec 30. doi:10.2478/hukin-2014-0114 PMCID: PMC4327384. Prevalence of Stress Urinary Incontinence in Elite Female Endurance Athlete Anna Poświata, Teresa Socha and Józef Opara1
J Womens Health (Larchmt). 2011 May;20(5):757-63. doi: 10.1089/jwh.2010.2454. Epub 2011 Apr 18. Impact of high-level sport practice on anal incontinence in a healthy young female population. Vitton V, Baumstarck-Barrau K, Brardjanian S, Caballe I, Bouvier M, Grimaud JC.
Am J Obstet Gynecol. 2016 Feb;214(2):164-71. doi: 10.1016/j.ajog.2015.08.067. Epub 2015 Sep 6. Physical activity and the pelvic floor. Nygaard IE, Shaw JM.
Appropriate sun exposure and/or daily supplements provide our bodies with sufficient amounts of Vitamin D. I would venture to guess almost every one of the patients I treated in Seattle had a deficiency of Vitamin D if they were not taking a supplement. Running outside year round has always kept my skin slightly tan and my levels of Vitamin D healthy; however, when I was pregnant in the Pacific Northwest, I had to supplement my diet with Vitamin D, which was a first for this East Coast beach girl. The benefit of Vitamin D has spread beyond just bone health, with studies showing its impact on pelvic floor function.
Parker-Autry et al., (2012) published a study discerning the Vitamin D levels in women who already presented with pelvic floor dysfunction versus “normal” gynecological patients. The retrospective study involved a chart review of 394 women who completed the Colorectal Anal Distress Inventory (CRADI)-8 and the Incontinence Impact Questionnaire (IIQ-7). These women all had a total serum 25-hydroxy Vitamin D [25(OH)D] drawn within one year of their gynecological visit. The authors defined a serum 25(OH)D of <15ng/ml as Vitamin D deficient, between 15-29ng/ml as Vitamin D insufficient, and >30ng/ml as Vitamin D sufficient. In the pelvic floor disorder group comprised of 268 women, 51% were found Vitamin D insufficient, 13% of whom were deficient. The CRADI-8 and IIQ-7 scores were noted as higher among the Vitamin D insufficient women. Overall, the mean 25(OH)D levels in the women without pelvic floor issues were higher than those who presented with pelvic floor disorder symptoms.
Another case-control study in 2014 by Parker-Autry et al., focused on the association between Vitamin D deficiency and fecal incontinence. They considered 31 women with fecal incontinence versus a control group of 81 women without any pelvic floor symptoms, looking at serum Vitamin D levels. The women with fecal incontinence had a mean serum Vitamin D level of 29.2±12.3 ng/ml (insufficient/deficient), while the control group had a higher mean level of 35±14.1 ng/ml (sufficient). The women completed the Modified Manchester Health Questionnaire and the Fecal Incontinence Severity Index, and women with deficient Vitamin D scored higher on the questionnaire, indicating fecal incontinence as a burden on quality of life. The severity scores were higher for Vitamin D deficient women, but there was not a statistically significant difference between the groups. Once again, the pelvic floor disorder and Vitamin D deficiency correlation prevailed in this study.
An even more recent study looked at postmenopausal women and Vitamin D deficiency (Navaneethan et al., 2015). This prospective case control study involved 120 postmenopausal women, 51 of whom had pelvic floor disorders. The serum 25-hydroxy Vitamin D levels were obtained, and the results revealed a deficiency in those women with pelvic floor dysfunction. Vitamin D levels were found to be significantly lower in women who were 5 years or more into menopause. Overall, Vitamin D was deemed a worthy factor to consider in the pelvic floor disorder population as well as in postmenopausal women.
Taking time to talk to patients about their lifestyle, daily supplements, and diet can often shed light on their ability to benefit from our treatments. If a Vitamin D deficiency sounds possible, discuss current research with them and suggest they get their serum Vitamin D levels checked. Don’t underestimate the power of a little sunshine – it just might have a positive impact on pelvic floor health.
Parker-Autry, C. Y., Markland, A. D., Ballard, A. C., Downs-Gunn, D., & Richter, H. E. (2012). Vitamin D Status in Women with Pelvic Floor Disorder Symptoms. International Urogynecology Journal, 23(12), 1699–1705. http://doi.org/10.1007/s00192-012-1700-8
Parker-Autry, C. Y., Gleason, J. L., Griffin, R. L., Markland, A., & Richter, H. E. (2014). VITAMIN D DEFICIENCY IS ASSOCIATED WITH INCREASED FECAL INCONTINENCE SYMPTOMS. International Urogynecology Journal, 25(11), 1483–1489. http://doi.org/10.1007/s00192-014-2389-7
Navaneethan, P. R., Kekre, A., Jacob, K. S., & Varghese, L. (2015). Vitamin D deficiency in postmenopausal women with pelvic floor disorders. Journal of Mid-Life Health, 6(2), 66–69. http://doi.org/10.4103/0976-7800.158948