Chronic non-cancer pain (CNCP), defined as pain persisting for more than three months, affects approximately 20% of adults worldwide, with a higher prevalence among vulnerable populations such as the elderly and those from diverse cultural backgrounds. The economic burden of CNCP is substantial, exceeding that of heart disease, diabetes, and cancer in countries like the United States. Beyond the financial implications, CNCP significantly impacts individuals' quality of life, leading to absenteeism, loss of productivity, and increased healthcare utilization.
Traditionally, CNCP management has focused on pharmacological interventions and physical therapies. However, emerging evidence underscores the importance of a holistic, person-centered approach that addresses various lifestyle factors, including nutrition. Healthy eating patterns are associated with reduced systemic inflammation, as well as lower risk and severity of chronic non-cancer pain and associated comorbidities.
Persisting low-grade systemic inflammation is associated with CNCP and multiple comorbid chronic health conditions. Diet plays a complex role in modulating systemic inflammation. Knowledge is expanding rapidly in this area and multiple links between diet and inflammation have been identified. Metabolic mechanisms associated with postprandial hyperglycemia and frequent and prolonged rises in plasma insulin levels, influenced by dietary intake, can produce systemic inflammation.
Nutritional Strategies for Pain Management
Evidence from a number of recent systematic reviews shows that optimizing diet quality and incorporating foods containing anti-inflammatory nutrients such as fruits, vegetables, long-chain and monounsaturated fats, antioxidants, and fiber leads to a reduction in pain severity and interference.
Non-nutritive bioactive compounds such as polyphenols mitigate oxidative stress and inflammation, as well as modulate pain experiences. One such mechanism operates through the inhibition of COX-2 in neuromodulating pathways. Polyphenols are found in a range of foods such as fruits, vegetables, whole grains, cocoa, tea, coffee, and red wine.
Incorporating anti-inflammatory foods into one's diet can be a practical approach to managing CNCP. Emphasizing the consumption of fruits, vegetables, whole grains, and healthy fats, while reducing the intake of processed foods and sugars, can help modulate inflammation and alleviate pain. Additionally, maintaining a balanced diet supports overall health, which is crucial for individuals dealing with chronic pain.
Adopting a healthy, anti-inflammatory diet can reduce systemic inflammation and alleviate pain severity, contributing to improved quality of life for individuals with CNCP. As research in this field continues to evolve, healthcare providers should consider incorporating nutritional strategies into comprehensive, person-centered pain management plans.
To learn more about essential digestion concepts, nourishment strategies, and the interconnected nature of physical and emotional health across the lifespan join Megan Prybil in her upcoming course, Nutrition Perspectives for the Pelvic Rehab Therapist on February 23-24, 2025. Whether at the beginning of your journey or well on your way down the path of integrative care, this continually updated and relevant course is a unique, not-to-be-missed opportunity.
Resources:
- Brain K, Burrows TL, Bruggink L, Malfliet A, Hayes C, Hodson FJ, Collins CE. Diet and Chronic Non-Cancer Pain: The State of the Art and Future Directions. J Clin Med. 2021 Nov 8;10(21):5203. doi: 10.3390/jcm10215203. PMID: 34768723; PMCID: PMC8584994.
- Nijs J, Malfliet A, Roose E, Lahousse A, Van Bogaert W, Johansson E, Runge N, Goossens Z, Labie C, Bilterys T, Van Campenhout J, Polli A, Wyns A, Hendrix J, Xiong HY, Ahmed I, De Baets L, Huysmans E. Personalized Multimodal Lifestyle Intervention as the Best-Evidenced Treatment for Chronic Pain: State-of-the-Art Clinical Perspective. J Clin Med. 2024 Jan 23;13(3):644. doi: 10.3390/jcm13030644. PMID: 38337338; PMCID: PMC10855981.
- Elma Ö, Brain K, Dong HJ. The Importance of Nutrition as a Lifestyle Factor in Chronic Pain Management: A Narrative Review. J Clin Med. 2022 Oct 9;11(19):5950. doi: 10.3390/jcm11195950. PMID: 36233817; PMCID: PMC9571356.
- Lahousse A, Roose E, Leysen L, Yilmaz ST, Mostaqim K, Reis F, Rheel E, Beckwée D, Nijs J. Lifestyle and Pain following Cancer: State-of-the-Art and Future Directions. J Clin Med. 2021 Dec 30;11(1):195. doi: 10.3390/jcm11010195. PMID: 35011937; PMCID: PMC8745758.
- Nijs J, Reis F. The Key Role of Lifestyle Factors in Perpetuating Chronic Pain: Towards Precision Pain Medicine. J Clin Med. 2022 May 12;11(10):2732. doi: 10.3390/jcm11102732. PMID: 35628859; PMCID: PMC9145084.

The year was 1998 - my fellow classmates and I converged upon our journey in graduate school to become physical therapists. In our first semester, we shouldered a heavy load of coursework and were memorably immersed in a battle between courses taught by our anatomy and histology professors. Both professors claimed stake to the title of teaching the “most important course in the curriculum.” The connection between anatomy and physical therapy was clear and specific. But there were moments when the connection between histology and physical therapy seemed less relevant and the demands from our histology professor obtuse. The battle between courses played out in both the cadaver lab and the histology slide viewing rooms. My classmates and I found ourselves compelled to pour over both anatomy and histology with focused intensity; the figurative competition became a grind.
We shared in collective moans and groans surrounding the challenge of having a histology professor who thought so highly of cellular structure and function and insisted our appreciation of the topic should equal that of learning anatomy. This professor made exceedingly clear to each of us: “You MUST know what a normal cell looks like to understand basic anatomy and physiology. If you don’t know what normal looks like, then you’ll never know what abnormal looks like.” We studied muscle slides, fibrocartilage slides, hyaline cartilage slides, endothelium slides, neuron slides, bone slides, tendon slides….and on and on and on. We counted mitochondria. We compared normal and abnormal. Over and over again.
Little did I know - our future understanding of health would literally hinge upon such things. Normal and abnormal cellular health. Intra- and Inter-cellular (mis)communication. Inter-cellular barrier integrity. Mitochondrial (dys)function.
In September 2024, Dr. Casey Means shined a spotlight on our country’s health crises by participating in a non-partisan roundtable discussion titled “American Health and Nutrition – a Second Opinion” – elucidating in a national forum the stark reality of the dismal nutrition situation that plagues our country resulting in equally dismal national health statistics. We are all witnesses to this health catastrophe. She also recently published “Good Energy,” a call-to-action she co-authored with her brother Cally Means. In the roundtable discussion and in the book, Dr. Means eloquently describes the driver of all health and disease states - the status of cellular function – and that this is foundationally driven by nutrition or lack thereof. Based on the overwhelming evidence in the literature I’ve read through the years, and compiled to create “Nutrition Perspectives in Pelvic Rehab,” I couldn’t agree with her more.
And I guess this is where I admit our histology professor was on to something.
As rehab professionals, we absolutely care about what cells look like, act like, move like, and feel like. We may not realize it, but cellular health or dysfunction can dictate if our patients have low energy, metabolic dysregulation (diabetes, obesity, fatty liver disease), neurodegenerative diseases like Parkinson’s, Alzheimer’s, dementia & peripheral neuropathy (Qiao et.al., 2024; Sabui et.al., 2022), neurocognitive changes, (Shatalina et.al., 2024) cancer, chronic pain, or even dysregulation of the gut-brain axis (found in conditions such as IBS). Cellular dysfunction is at the foundation of all of these conditions and their sequelae. We also may not realize it, but when we palpate tissue that is painful, inflamed, tense, tight, dyscoordinated, or find joints to be irritated (Seewald et.al. 2023) cellular dysfunction may be making itself manifest. Sarcopenia, muscle degeneration and weakness, also has underpinnings in metabolic and thus cellular dysregulation (Daily &Park, 2022; Xie & Huang, 2024). Chronic systemic inflammation is by definition cellular dysregulation. (Kharrazian, 2022)
And finally, we also may not fully realize the decidedly negative impact our standard American diet has on each and every condition just listed, or more precisely, on our cellular health. Without normal cellular function our bodies will devolve into chaos - otherwise known as disease states.
As rehab professionals, we need to know all we can about anatomy, biomechanics, and therapeutic intervention. In my journey, it was the requisite histological training combined with my studies in nutritional sciences that allowed me to see how the “peripheral” topics of nutrition, health, and cellular function intersected in vivid clarity early in my career. This fueled my long-standing passion to share this information with other healthcare providers through the creation of “Nutrition Perspectives.”
This intersection should inform our intention as we steer towards solutions to the overarching American health crisis while helping our clients – one conversation at a time. “Nutrition Perspectives in Pelvic Rehab” (NPPR) provides practical steps to navigate a path forward to improve digestive health, gut health, and overall health. First, we must bravely confront the magnitude and complexity of the problem as we equip ourselves with working knowledge of functional nutrition as shared in NPPR.
Optimizing cellular health can positively influence everything we care about as rehab providers. I might argue in this context – that learning about functional nutrition may be equivalent in importance to anatomy and histology! More fairly – the intersection of anatomy, histology & nutrition will be the foundation upon which the future of health and wellness, and hopefully healthcare will eventually be built.
Nutrition Perspectives in Pelvic Rehab is nearing its 10th anniversary– 10 years of sharing profoundly important nutritional concepts that impact each one of us and the clients we serve. As the body of evidence explodes, the essence of the message within NPPR is unwavering and may just become your “most important course in the curriculum.” Nutrition matters deeply – all the way down to the cellular level.
Come learn the hows and whys in an upcoming offering of Nutrition Perspectives in Pelvic Rehab – available in remote format on the following dates: Dec 7-8, 2024; Feb 22-23, 2025; June 7-8, 2025; Oct 11-12, 2025 & Dec 6-7, 2025.
Resources:
- American Health and Nutrition – A Second Opinion. https://rumble.com/v5fy7bv-american-health-and-nutrition-a-second-opinion.html
- Daily JW, Park S. Sarcopenia Is a Cause and Consequence of Metabolic Dysregulation in Aging Humans: Effects of Gut Dysbiosis, Glucose Dysregulation, Diet and Lifestyle. Cells. 2022 Jan 20;11(3):338. doi: 10.3390/cells11030338. PMID: 35159148; PMCID: PMC8834403.
- Kharrazian D. Functional Medicine Approaches to Neurodegeneration. Phys Med Rehabil Clin N Am. 2022 Aug;33(3):733-743. doi: 10.1016/j.pmr.2022.04.011. PMID: 35989061.
- Means, C; Means, C. Good Energy – the Surprising Connection between Metabolism and Limitless Health. Avery. May 2024.
- Qiao L, Yang G, Wang P, Xu C. The Potential Role of Mitochondria in the Microbiota-Gut-Brain Axis: Implications for Brain Health. Pharmacol Res. 2024 Sep 25:107434. doi: 10.1016/j.phrs.2024.107434. Epub ahead of print. PMID: 39332752.
- Sabui A, Biswas M, Somvanshi PR, Kandagiri P, Gorla M, Mohammed F, Tammineni P. Decreased anterograde transport coupled with sustained retrograde transport contributes to reduced axonal mitochondrial density in tauopathy neurons. Front Mol Neurosci. 2022 Sep 30;15:927195. doi: 10.3389/fnmol.2022.927195. PMID: 36245925; PMCID: PMC9561864.
- Seewald LA, Sabino IG, Montney KL, Delco ML. Synovial fluid mitochondrial DNA concentration reflects the degree of cartilage damage after naturally occurring articular injury. Osteoarthritis Cartilage. 2023 Aug;31(8):1056-1065. doi: 10.1016/j.joca.2023.03.013. Epub 2023 Apr 6. PMID: 37028640; PMCID: PMC10524327.
- Shatalina E, Whitehurst TS, Onwordi EC, Gilbert BJ, Rizzo G, Whittington A, Mansur A, Tsukada H, Marques TR, Natesan S, Rabiner EA, Wall MB, Howes OD. Mitochondrial complex I density is associated with IQ and cognition in cognitively healthy adults: an in vivo [18F]BCPP-EF PET study. EJNMMI Res. 2024 Apr 17;14(1):41. doi: 10.1186/s13550-024-01099-1. PMID: 38632153; PMCID: PMC11024075.
- Xie X, Huang C. Role of the gut-muscle axis in mitochondrial function of aging muscle under different exercise modes. Ageing Res Rev. 2024 Jul;98:102316. doi: 10.1016/j.arr.2024.102316. Epub 2024 May 3. PMID: 38703951.
AUTHOR BIO
Megan Pribyl, PT, CMPT, CMTPT/DN, PCES

Megan Pribyl, PT, CMPT, CMTPT/DN, PCES (she/her) is a mastery-level physical therapist at the University of Kansas Health System in Olathe, KS treating a diverse outpatient population in orthopedics including pelvic health, pregnancy, and postpartum rehabilitation – all with integration of health and wellness. She began her PT career in 2000 after graduating from the University of Colorado Health Sciences Center with her Master of Science in Physical Therapy. Prior, she earned her dual degree in Nutrition and Exercise Sciences (B.S. Foods & Nutrition, B.S. Kinesiology) in 1998 from Kansas State University. Later, she obtained her CMPT from the North American Institute of Orthopedic Manual Therapy and became certified in dry needling in 2019. Since 2015, she has been a faculty member of Herman & Wallace Pelvic Rehab Institute and enjoys both teaching and developing content. She created and instructs Nutrition Perspectives for the Pelvic Rehab Therapist offered remotely through Herman & Wallace. She also teaches Pelvic Function – Level 1, Pregnancy Rehabilitation and Postpartum Rehabilitation. She brings many years of experience and insight to all courses. As a content developer, Megan has also contributed to the Herman & Wallace Oncology Series, Pelvic Function Level 2A, as well as the Pelvic Function Series Capstone Course.
Megan’s longstanding passion for both nutritional sciences and manual therapy culminated in her creating Nutrition Perspectives for the Pelvic Rehab Therapist designed to propel understanding of human physiology as it relates to pelvic conditions, pain, healing, and therapeutic response. She harnesses her passion to integrate ancient and traditional practices with cutting-edge discoveries creating a unique experience sure to elevate your level of appreciation for the complex and fascinating nature of clinical presentations in orthopedic manual therapy and pelvic rehabilitation. Clinicians will come away from this course with both simple and practical integrative tools that can be immediately utilized to help clients and providers alike - along their path of healing.
Megan enjoys her many fulfilling roles as an instructor, clinician, wife, and mom to two active teenagers and owner of two rambunctious golden retrievers. She loves to read, cook, be in the great outdoors, travel, and spend time with her family and friends. She has a passion for both the mountains and the beach, exploring scientific literature, and learning all she can about the power of using nature, nurture, and nutrition to heal and sustain health.

Megan Pribyl, PT, CMPT is a practicing physical therapist at the Olathe Medical Center in Olathe, KS treating a diverse outpatient population in orthopedics including pelvic rehabilitation. Megan’s longstanding passion for both nutritional sciences and manual therapy has culminated in the creation of her remote course, Nutrition Perspectives for the Pelvic Rehab Therapist, designed to propel understanding of human physiology as it relates to pelvic conditions, pain, healing, and therapeutic response.
She harnesses her passion to continually update this course with cutting-edge discoveries creating a unique experience sure to elevate your level of appreciation for the complex and fascinating nature of clinical presentations in orthopedic manual therapy and pelvic rehabilitation.
Indulgences over the holiday season lead many to experience symptoms of indigestion, part of the discomfort that fuels our renewed January focus on exercise and “eating right”.
With this in mind, let’s discuss how we as a nation handle GI distress or GERD (gastroesophageal reflux disease) symptoms. Typically here in the US, there are 2 methods we typically use:
- The quick way - by popping a Tums or Rolaids or
- The prolonged way - by taking PPI’s (proton pump inhibitors) or H-2 blockers on a regular basis (eg. Pepcid AC).
Both are reliable ways to efficiently feel a little less GI distress.
The quick relief strategy neutralizes the acid that is already in the stomach whereas the longer-acting PPI’s and H-2 blockers actually block or suppress acid production in the stomach. And even though these “longer term” drugs are designed for short-term use, the more I inquire about their use with my patients, the more a troublesome pattern emerges. Many of my patients struggling with complex symptom constellations (eg. a non-relaxing pelvic floor, constipation, perineal skin issues, gut issues, anxiety, depressive symptoms, etc.) describe that they have taken these “digestive aides” continually for years. YEARS.
So, this approach is fine, yes? We know acid reflux can lead to esophageal irritation, not to mention pain and nagging discomfort. It can lead to disordered sleep and its associated sequelae. In extreme cases, esophageal irritation could even progress to esophageal cancer. Therein lies the justification for using drugs that suppress or block acid production in the stomach over the long term. Even though long-term safe use of these drugs has never been established.
Hmmm. I hope this is cause for pause. It’s true we don’t want GERD or indigestion, yet it remains ubiquitous. The prevalence of at least weekly GERD symptoms in the US is approximately 20% (El-Serag et al., 2014) with an overall prevalence estimated up to 30% in the US (Eusebi et al., 2017). This prevalence of GERD is deemed “exceedingly common”, ranking as the most frequent gastrointestinal diagnosis associated with outpatient clinic visits in the US (Richter, 2018). For as frequently as I see these drugs listed on patient intake forms - or forgotten to be listed since it is such a part of one’s routine - I feel strongly that we are dealing with an epidemic I call “indigestion nation”.
Instead of blaming our stomach acid, it’s time for us to look at the other side of the issue and ask why. Why are so many struggling with digestion? And is there a better way to get a handle on this under-appreciated situation?
Next question: how often is nutrition or food digestibility considered in scenarios involving GERD symptoms, GI upset, or indigestion?
When I ask my patients about this, the standard answer prevails: they try their best to avoid known triggers including fried and spicy foods. Beyond that, there is little forward thinking in terms of where our collective indigestion originates.
Further, how many healthcare providers or patients contemplate what long-term acid suppression might look like?
- Isn’t our stomach SUPPOSED to be acidic? (Answer: it is)
- What happens if it isn’t? (Answer: lots of undesirable things)
- From there, we begin connecting the dots to find points of clarity.
In order to digest proteins, our stomach has to be acidic. The acid in the stomach also kills or deactivates harmful viruses and bacteria that could otherwise gain access to the rest of our system via the intestinal barrier. And our standard American diet does not include foods that contain important bioactive compounds and enzymes that take some of the burden of digestion off our plate – or rather our stomach, intestines, and accessory digestive organs. These are not frequently discussed principles of digestion.
We are conditioned to seek the quick fixes to our digestive woes. Woes that have increased in prevalence in North America by approximately 50%, relative to the baseline prevalence in the early to middle 1990s (Richter, 2018). Our go-to quick (Tums and Rolaids) and long-term strategies (Pepcid AC) are not without consequences. And I’m not even referring to the recently elucidated serious issue of the H-2 blocker ranitidine (generic Zantac) containing N-nitrosodimethylamine (NDMA)….a probable human carcinogen (Mahase, 2019).
Facts like these will sometimes get us to take notice. However, the more pervasive problem is this: components of our diets have become so difficult to digest, so physiologically incompatible with us, that we forget to examine this issue through such a simple lens. If our diet consists of foods that are difficult to break down or contain substances that can be disruptive to our digestive processes, it’s no surprise our body may reject them or be unable to digest them fully.
However, if our diet consists of foods that are designed for nourishment, naturally pre-digested and ready to assimilate or use by the body for building blocks and fuel, our body will know how to break them down and utilize them fully…..miraculously reducing the digestive burden and improving symptoms of GI distress including GERD and indigestion.
It sounds simple enough.
But in this day and age, the savvy healthcare provider will do well to learn and appreciate the breadth and depth of this concept and what it means to you as both a consumer of food and one who cares for others who consume food - all of us. This understanding - especially for a pelvic rehab provider- is critical to harness.
From simple but nuanced concepts, one can help prompt remarkable changes. I’ve seen it firsthand innumerable times.
I invite each of you to learn more about this fascinating topic and how it interrelates with so many facets of our health. Take advantage of the multiple remote-course offerings of Nutrition Perspectives for the Pelvic Rehab Therapist in 2024 - February 24-25, April 27-28, June 8-9, and December 7-8.
References:
- Richter, J. E., & Rubenstein, J. H. (2018). Presentation and Epidemiology of Gastroesophageal Reflux Disease. Gastroenterology, 154(2), 267-276. doi:10.1053/j.gastro.2017.07.045
- Eusebi LH, Ratnakumaran R, Yuan Y, et al. Global prevalence of, and risk factors for, gastro- oesophageal reflux symptoms: a meta-analysis. Gut. 2017
- El-Serag HB, Sweet S, Winchester CC, et al. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2014; 63(6):871– [PubMed: 23853213]
- Mahase, E. (2019). FDA recalls ranitidine medicines over potential cancer causing impurity. BMJ, 367, l5832. doi:10.1136/bmj.l5832

Megan Pribyl, PT, CMPT is a practicing physical therapist at the Olathe Medical Center in Olathe, KS treating a diverse outpatient population in orthopedics including pelvic rehabilitation. Megan’s longstanding passion for both nutritional sciences and manual therapy has culminated in the creation of her remote course, Nutrition Perspectives for the Pelvic Rehab Therapist, designed to propel understanding of human physiology as it relates to pelvic conditions, pain, healing, and therapeutic response. She harnesses her passion to continually update this course with cutting-edge discoveries creating a unique experience sure to elevate your level of appreciation for the complex and fascinating nature of clinical presentations in orthopedic manual therapy and pelvic rehabilitation.
It has been nearly 8 years since I taught my first in-person rendition of “Nutrition Perspectives for the Pelvic Rehab Therapist” in Seattle, WA through Herman & Wallace – and over a decade since I began writing the course in earnest. Creating and teaching this course has been an honor for me and truly a full-circle opportunity to share my passion for nutrition with other clinicians. The mission of the course is to create a ripple effect from one person to the next. But if there’s anything the last couple of years has taught me, it’s that we still have a long way to travel to reach the destination of fully integrated care centered on the whole person. As a guide, I tap the growing body of literature on nutrition and health to help show us the way.
I recall having taught this course on 11 occasions in-person between June 2015 and October 2019 at gracious site host clinics nationwide. I enjoyed each and every one of these experiences. Since the 2020 pivot to remote format, I have taught Nutrition Perspectives via Zoom 18 times - after we were faced with restrictions on traveling and gathering.
Having taught Nutrition Perspectives in both formats, I’d like to share with you first why I love teaching this course, and second why I love teaching it in its remote format. It truly is a class perfectly suited to this mode of delivery.
First, why I love teaching this course:
It is my passion to share nutrition information with peers in pelvic rehab. Before becoming a PT, I studied nutrition as an undergrad. After becoming a PT, and more specifically a pelvic PT, it became crystal clear that we needed to incorporate the essence of nutritional sciences into pelvic rehab– and even into general clinical practice. Nutrition Perspectives became my answer to the burning and urgent questions I had about how we could blend the worlds of rehabilitation and nutrition. I scoured the literature to find answers – and what I found was astonishing. Paradigm shifting. Compelling.
Early in my career, I would only sporadically encounter patients who would experience what I would now describe as “functional gastro-intestinal disorders with extra-intestinal manifestations”. Fast-forwarding to today, it is rare to see a patient who does not experience any conditions such as GERD, constipation, gas/abdominal pain/bloating/discomfort, anxiety, depression, and complex or chronic pain conditions. Because of this reality, it has become essential for healthcare providers to have a basic working knowledge of functional nutrition. Especially providers in pelvic rehabilitation. Having a working knowledge of these conditions and potential nutritional underpinnings can help us better understand and serve our clients.
Not only does nutrition have significant relevance to our patients – it is relevant to each of us as human beings! But be aware – the realm of nutrition appears chock-full of confusing contradictions. And our patients are now – more than ever – asking us for our thoughts on nutrition-related topics. They’re listening to podcasts. They’re reading social media posts and blogs. They’re watching short video clips to find quick answers to complex questions. And they want to run some of their questions by you – their trusted health professional ally. You want to feel confident and competent in what you’re sharing. My mission is to make evidence-informed information accessible and relevant to you, the practicing clinician so then you can, in turn, share with confidence and competence.

Now, on to why I love teaching this course remotely:
Don’t get me wrong – I love to travel. But imagine traveling alone to new cities -not as a free-spirited adventure solo traveler – but instead as an idealistic instructor who doesn’t want to be without any supplies needed for teaching a course far from home! This translates to a very heavy suitcase filled with visual aids and lab supplies. This humongous check-in bag contains items necessary to conduct the course descriptively – books, empty product containers, glass jars (yes, GLASS), carefully packaged kefir grains, a SCOBY, bowls, spoons, kitchen towels, and those hard-to-find food items that one can’t be certain to find in an unfamiliar city. And a tablecloth. Because when we’re talking about food with guests, presentation is important!
Now imagine navigating travel challenges with said heavy, giant suitcase; chucking it on and off a rental car bus during a cold rainstorm for example.. Imagine pushing it down a carpeted hotel hallway that is so plush, it prohibits the wheels from functioning properly. Imagine repacking in 15 minutes what took 3 hours to initially pack in order to catch a return flight home.
This was the reality of logistics I eagerly and enthusiastically took on to be able to teach this class. But that giant suitcase couldn’t hold even close to everything I wanted to share, and it actually was a bit cumbersome to manage. Maybe a lot cumbersome. Always plastered with the bright orange “HEAVY” sticker warning – there was a limit to what I could bring along to live course events.
When we first transitioned this course to remote format, it was a quick response to begin offering CEUs when lockdown mode began. The silver lining, we discovered, was that the remote format for this course was in fact – much better than the live event format.
Now, all the necessary supplies are right where I need them to best instruct. Plus, predictable kitchen and lecture spaces create a seamless experience for the participants. Teaching from home has been life-changing as an instructor. I can practice what I preach about nourishing the nervous system and mitigating stress with lifestyle choices. It is nourishing to be able to sleep well at home the nights before I teach. Adequate rest is a superpower that allows me to give my best well-rested self to the participants.
The remote format is not just nourishing to me, but also to the participants who can attend from the comfort of home or familiarity of a clinic. Wherever you are, you can take the course. No airports, no suitcases, nor carpeted hotel hallways. That’s accessibility. That’s getting this information into the hands and minds of providers in locations all around this country and beyond. We need this accessibility if we ever hope to reach our destination of fully integrative care of the whole person – for all.
For these reasons, Nutrition Perspectives for the Pelvic Rehab Therapist will remain in this remote format – even as our lives begin to involve travel and in-person events again. All good things. But I do hope you enjoy taking Nutrition Perspectives as much as I enjoy teaching it. I invite you to join me on the journey toward implementing more integrative care as standard practice. It’s not always an easy road, nor the popular road. And sometimes it feels as hard as dragging a giant, heavy suitcase behind you. But it’s a path worth taking – one that will be fruitful for both you and the clients you serve. Let’s travel it together.
Nutrition Perspectives for the Pelvic Rehab Therapist will be offered quarterly in 2023: January 21-22, June 10-11, September 16-17, and December 2-3.
Nutrition Perspectives for the Pelvic Rehab Therapist

Course Dates:
January 21-22, June 10-11, September 16-17, and December 2-3
Price: $525
Experience Level: Beginner
Contact Hours: 17.75
Description: Participants will be introduced to the latest research in nutrition through immersive lectures and hands-on labs. The course will cover essential digestion concepts, nourishment strategies, and the interconnected nature of physical and emotional health across the lifespan. Further, clinicians will delve into nutritional relevancies in bowel and bladder dysfunction, pelvic health, pain, and healing. Labs throughout include insightful demonstrations and breakout sessions. The course participant will acquire new, readily applicable tools for patient empowerment, engagement, and self-management utilizing presented principles.

As 2022 has gotten underway, it has already brought many of us to a place where we simply need to hear something lighthearted. The start of a new year also gives us a chance to examine priorities and make room for what matters most. “What matters most” can look different for each of us; for me, it’s my family – including two dogs – Stella and Sadie. Of course, the dogs fall in line behind my human nuclear and extended families, however, they are such a part of my daily life and contribute to my quality of life, it seems only natural to share this story with a wider audience -especially because this story revolves around one of my favorite topics – intentional nourishment!
Let me begin by telling you about our 5-year-old Golden Retriever named Stella. She came to us as one of only three puppies in a litter; a pleasantly plump pup, she was well developed, well-fed, and well-loved. According to everyone who has had the opportunity to meet her, she is the happiest dog they’ve ever met. When we brought her home at eight weeks, she topped the scale at 21 lbs.
Stella's fur was shiny, her disposition sunny; she emanated maturity and wisdom. She slept through the night with such efficiency, we hardly remember having to let her out at night as a puppy. She was content; the perfect combination of calm and energetic. She was a breeze to housetrain, has an impeccable record of only two accidents in the house, and nary an indoor fecal incontinence episode. Stella brought us so much joy that we decided on a whim to add a second puppy to the milieu.
The second puppy is our ~16-week-old Golden Retriever puppy named Sadie. This past October – by coincidence – my family learned about some surprise Goldens needing homes – 17 to be exact – and we wondered if we might be interested in one. Two weeks later, sweet Sadie came home with us.
Weighing in at only 13 lbs 6 oz at eight weeks, she was miniature compared to Stella at the same age. It didn’t take us long to figure out that not only was she smaller, but her digestive tract and elimination systems were not like Stella’s either. Sadie pooped often - what seemed like every hour – including sometimes in the house. Her bottom was sore and irritated, and she seemed frustrated and uncomfortable. My husband and I looked at each other more than once thinking the same thought: WHAT did we get ourselves into?!?
Sadie tested negative for parasites, and the vet said she was just working on adjusting to her new home and to give it time. He also suggested we might be feeding her too much. So, we fed her less - but that didn’t help. We tried adding pumpkin, that didn’t help either. Then we upped her food amount again, tried timing her foods differently, tried feeding her more often, then less often. None of these approaches helped. The messes continued.
We began to feel exasperated. I was reluctant to try adding new foods for fear of upsetting her GI tract further.
This puppy was pooping nonstop – much of it type 6 & 7 applying the Bristol Scale to dogs (1). She barely came in at 16 lbs. week 10 and alarmingly, she still weighed 16 lbs. at week 12. The vet confirmed our concerns – she was too thin and needed to put on weight.
Now I started to worry. With all the bowel troubles she had, how could she thrive? We weren’t getting any continuous hours of sleep at night which meant she wasn’t either. It was an exhausting few weeks.
Given what we had tried – with no success – we had no choice but to begin what we called “Operation Nourishment” for this little puppy. We put worries aside about adding new foods and applied what we understand about functional nutrition to help our sweet Sadie.
“Operation Nourishment” consisted of following several basic digestive principles:
- Make her food more digestible
- Feed her nutrient-dense options (dog appropriate, of course)
- Practice puppy-version mindfulness at mealtime
- Help support her puppy microbiome
#1: Make her food more digestible: Without changing the kibble she was eating, we soaked it with a bit of water before ingestion to soften it. This helped make her food easier to break down in her digestive tract and also helped S L O W D O W N her tendency to inhale food. Prior, she was definitely not chewing her food thoroughly which can result in undigested food reaching the colon and causing irritation. The softened food facilitated just the slightest bit of chewing and tripled the time it took her to finish a meal, giving her GI tract less of a shock.
#2: Feed her nutrient-dense options: We began adding an organic egg (3,4) softly cooked in a tiny bit of coconut oil (2) to her breakfast. The egg adds a whole food-based protein-containing cholesterol, vitamins, and minerals -all important for building her gut lining and nervous system. Coming from such a large litter in a somewhat stressful/chaotic environment, her gut and nervous system may not have been at their healthiest and needed extra support (4).
#3: Practice mindfulness at mealtime: The egg at breakfast has quickly become the highlight of her day.
The anticipation while watching us cook it calms her. She intently follows as the pan comes out of the cupboard and onto the stove. She watches more intently as we slowly cook the egg. Then she must wait even longer while it sits in her bowl to cool up on the countertop.
I presume this has taught her mindfulness and presence before eating – essential for thorough digestion!
#4: Help support her puppy microbiome: We gradually began to add a dollop of kefir (5) to her breakfast and dinner – knowing that even dogs have a microbiome and that cultured foods can help normalize gut flora which can help normalize stool consistency. A healthy gut helps us extract nutrients from the food we eat. It can also, fascinatingly, modulate our stress responses.
“Operation Nourishment” began to take effect almost immediately. She jumped from 16 to 24 lbs. in 3 weeks! We were so proud! She finally began to have a soft, healthy belly - and the vet was thrilled, “whatever you’re doing, keep it up!”. She began to sleep through the night – and WE were thrilled. She also began to sprout her golden retriever fur patterns and take on more shine. Brilliantly, her stools became formed – a perfect 4 on the Bristol Stool Scale (1) and had significantly less urgency which led to the elimination of accidents. We were shocked at how quickly her body adapted to a diet higher in nutrient density and digestibility– one that was safe and appropriate for puppies.
Upping her nutrient density and digestibility helped unlock her potential so she could become the best sweet version of herself. Once more deeply nourished, she happily settled into her calm, gentle nature. She and Stella have become quite the pair. And we – her humans - are finally, gratefully sleeping again (most nights), which makes us adore her even more.
How might A Tale of Two Goldens provide us with insight relevant to pelvic rehabilitation?
We acknowledge that no two people come into this world in exactly the same circumstance and that we each arrive with a certain level of built-in resiliency. Some of us come into this world with our tails wagging, ready to greet everything that comes our way. Many of us and those we serve– let’s face it –are figuratively more like Sadie. We have the potential waiting inside of us to become the best version of ourselves.
Sometimes reaching that potential takes just a little tweaking, a little coaxing, a little know-how. Maybe that tweaking, coaxing, and know-how could include principles of “Operation Nourishment” for ourselves and those we serve in the form of nourishment-focused guidance. With a little patience, time, and intentional action, we may be surprised to see how a few small changes have an enormous impact on what matters most to each of us and those we serve.
Nourishment knowledge – now more than ever – is vital.
Join us in 2022 for Nutrition Perspectives for the Pelvic Rehab Therapist to learn more about these principles and beyond. Upcoming 2022 remote offerings include Feb 26-27, April 29-30, July 23-24, August 27-28, Sept 23-24, Oct 22-23, and Nov 11-12. We welcome you to join us.
References:
- https://www.bladderandbowel.org/wp-content/uploads/2017/05/BBC002_Bristol-Stool-Chart-Jan-2016.pdf Accessed January 11, 2022.
- Alves DVS, Sousa MSB, Tavares MGB, Batista-de-Oliveira Hornsby M, Amancio-Dos-Santos A . Coconut oil supplementation during development reduces brain excitability in adult rats nourished and overnourished in lactation. Food Funct. 2021 Apr 7;12(7):3096-3103. doi: 10.1039/d1fo00086a. Epub 2021 Mar 15. PMID: 33720258.
- Avirineni BS, Singh A, Zapata RC, Phillips CD, Chelikani PK. Dietary whey and egg proteins interact with inulin fiber to modulate energy balance and gut microbiota in obese rats. J Nutr Biochem. 2022 Jan;99:108860. doi: 10.1016/j.jnutbio.2021.108860. Epub 2021 Sep 11. PMID: 34520853.
- Choi, M., Lee, J. H., Lee, Y. J., Paik, H. D., & Park, E. (2022). Egg Yolk Protein Water Extracts Modulate the Immune Response in BALB/c Mice with Immune Dysfunction Caused by Forced Swimming. Foods, 11(1). doi:10.3390/foods11010121
- Vieira CP, Rosario AILS, Lelis CA, Rekowsky BSS, Carvalho APA, Rosário DKA, Elias TA, Costa MP, Foguel D, Conte-Junior CA. Bioactive Compounds from Kefir and Their Potential Benefits on Health: A Systematic Review and Meta-Analysis. Oxid Med Cell Longev. 2021 Oct 27;2021:9081738. doi: 10.1155/2021/9081738. PMID: 34745425; PMCID: PMC8566050.
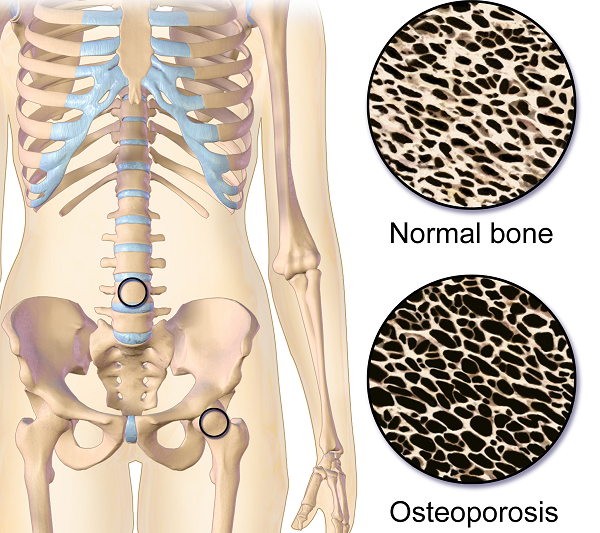
Osteoporosis or low bone mass is much more common than most people realize. Approximately 1 in 2 women over the age of 50 will suffer a fragility fracture in their lifetime. A fragility fracture is identified as a fracture due to a fall from a standing height. According to the US Census Bureau there are 72 million baby boomers (age 51-72) in 2019. Currently over 10 million Americans have osteoporosis and 44 million have low bone mass.
Many myths abound regarding osteoporosis. Answer these 5 questions below to test your Osteoporosis IQ. 1
1. “Men don’t get osteoporosis.”
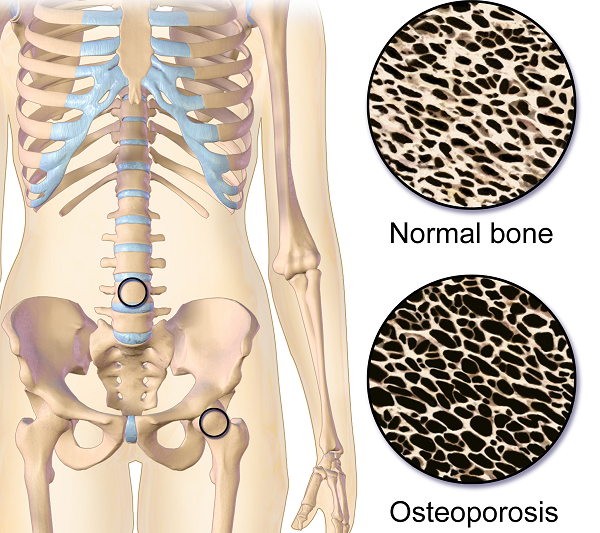 Fact: In addition to the statistic above regarding the incidence of fractures in women, up to 1 in 4 men over the age of 50 will suffer a fragility fracture.
Fact: In addition to the statistic above regarding the incidence of fractures in women, up to 1 in 4 men over the age of 50 will suffer a fragility fracture.
2. “Osteoporosis is a natural part of aging.”
Fact: Although we do lose bone density as we age, osteopenia or osteoporosis is a much more significant loss than seen in normal aging. DXA (dual energy x-ray absorptiometry) is the gold standard for measuring bone density and the test shows whether an individual’s numbers fall into the normal, osteopenia, or osteoporosis range based on his or her age.
3. “I don’t need to worry about osteoporosis until I’m older.”
Fact: Osteoporosis has been called a “pediatric condition which manifests itself in old age.” Up until the age of 30 we build bone faster than it breaks down. This includes the growth phase of infants and adolescents and is also the time to build as much bone density as possible. By the age of 30, called our Peak Bone Mass, we have accumulated as much bone density as we will ever have. Proper nutrition, osteoporosis specific exercises, and good body mechanics in our formative years can all play a role in reducing the effects of low bone mass later on.
4. “I exercise regularly (including sit ups and crunches for my core). I would know if I had a fracture.”
Fact: Two myths here. Flexion based exercises such as sit-ups, crunches, and toe touches are contraindicated for osteoporosis. A landmark study done by Dr. Sinaki from Mayo clinic showed women with osteoporosis had an 89% re-fracture rate after performing flexion based exercises. 2
Fact: Secondly, only 30% of vertebral compression fractures (VCF) are symptomatic meaning many individuals fracture without knowing it. This can lead to a fracture cascade as individuals continue performing movements and exercises that are contraindicated.
5. “Tests for osteoporosis are painful and expose you to a lot of radiation.”
Fact: The DXA is a simple and painless test which lasts 5-10 minutes. You lay on your back and the machine scans over you with an open arm- no enclosed spaces. There is very little radiation. Your exposure is 10-15 times more when flying from New York to San Francisco.
How did you do? Feel free to share these myths with your patients, many of whom may have osteoporosis in addition to the primary diagnosis for which they are being treated. To learn more about treating patients with low bone density/osteoporosis, consider attending a Meeks Method for Osteoporosis course!
1. www.nof.org
2. https://www.ncbi.nlm.nih.gov/pubmed/6487063
3. https://www.aafp.org/afp/2016/0701/p44.html
A recent article in the Washington Post Health & Science section explored the wonders of dietary fibre in an article called ‘Fiber has surprising anti-aging benefits, but most people don’t eat enough of it’ The article discussed how ‘…Fiber gets well-deserved credit for keeping the digestive system in good working order — but it does plenty more. In fact, it’s a major player in so many of your body’s systems that getting enough can actually help keep you youthful. Older people who ate fiber-rich diets were 80 percent more likely to live longer and stay healthier than those who didn’t, according to a recent study in the Journals of Gerontology’
But what is fiber and why does it matter?
Before we jump in there, let me answer the perennial questions that arise when we, as pelvic rehab clinicians, talk about fiber…’Is it in our scope of practice to talk about food?!’ I think it is fundamental that if we are placing ourselves as experts in bladder and bowel dysfunction, that we also remember that we can’t focus on problems at one end of ‘the tube’ without thinking about what happens at the other end. Furthermore, let me quote the APTA RC 12-15: The Role of the Physical Therapist in Diet and Nutrition. (June 2015): “as diet and nutrition are key components of primary, secondary, and tertiary prevention of many conditions managed by physical therapists, it is the role of the physical therapist to evaluate for and provide information on diet and nutritional issues to patient, clients, and the community within the scope of physical therapist practice. This includes appropriate referrals to nutrition and dietary medical professionals when the required advice and education lie outside the education level of the physical therapist’’
Fiber plays a huge role in so many of the health issues that we as clinicians face daily – constipation is regarded as a scourge of a modern sedentary society, perhaps over-reliant on processed convenience food – this is borne out when we gaze upon the rows of constipation remedies and laxatives in our pharmacies and supermarkets.
Let's take a look at the effects of fiber on breast cancer recovery – what does the research say?
There is growing interest and evidence to suggest that making different food choices can help control symptoms of breast cancer treatment and improve recovery markers – avoiding food with added sugar, hydrating well and focusing primarily on plant based food. Fiber is of course beneficial for bowel health, but may also have added benefits for heart health, managing insulin resistance, preventing excess weight gain and actually helping the body to excrete excess estrogen, which is often a driver for hormonally sensitive cancers. Fiber may be Insoluble (whole grains, vegetables) or Soluble (oats, rice, beans, fruit) but both are essential and variety is best.
In their paper ‘Diets and Hormonal levels in Post menopausal women with or without Breast Cancer’ Aubertin – Leheudre et al (2011) stated that ‘…Women eating a vegetarian diet may have lower breast cancer because of improved elimination of excess estrogen’, but even prior to that, in ‘Estrogen excretion patterns and plasma levels in vegetarian and omnivorous women.’ Golden et al (1982) concluded that ‘…that vegetarian women have an increased fecal output, which leads to increased fecal excretion of estrogen and a decreased plasma concentration of estrogen.’
Fiber may also be beneficial in the management of colorectal cancer, which is on the rise in younger women and men. A recent report by the World Cancer Research Fund International/American Institute for Cancer Research found that eating 90 grams of fiber-rich whole grains daily could lower colorectal cancer risk by 17 percent…and the side effects? A happier healthy digestive system, improved cardiovascular health and a lower risk of Type 2 Diabetes.
Your mother was right – eat your vegetables!
For more information on colorectal function and dysfunction, take Pelvic Floor Level 2A or for a deeper dive on the role of nutrition and pelvic health, why not take Megan Pribyl’s excellent course, Nutrition Perspectives for the Pelvic Rehab Therapist? Physical Therapy Treatment for the Breast Oncology Patient is also an excellent opportunity to learn about chemotherapy, radiation and pharmaceutical side effects of breast cancer treatment, as well as expected outcomes in order for the therapist to determine appropriate therapeutic parameters.
https://www.washingtonpost.com/national/health-science/fiber-has-surprising-anti-aging-benefits-but-most-people-dont-eat-enough-of-it/2018/04/27/c5ffd8c0-4706-11e8-827e-190efaf1f1ee_story.html?fbclid=IwAR0b-9VFUOCyUOgwe2BqV7-ahqwGzWs9rNpd1mscT75KNOGqnHm4ooFAu74&utm_term=.4d2784974ddc
Estrogen excretion patterns and plasma levels in vegetarian and omnivorous women. Goldin BR, Adlercreutz H, Gorbach SL, Warram JH, Dwyer JT, Swenson L, Woods MN. N Engl J Med. 1982 Dec 16;307(25):1542-7.
Diets and hormonal levels in postmenopausal women with or without breast cancer. Aubertin-Leheudre M1, Hämäläinen E, Adlercreutz H. Nutr Cancer. 2011;63(4):514-24. doi: 10.1080/01635581.2011.538487.
Nutrition Perspectives for the Pelvic Rehab Therapist
There are moments when I pause and realize how far we’ve come in a short period of time, and then others when I’m acutely reminded how far we have yet to go. Our destination is an integrative health care system which addresses nourishment first and early versus last, not at all, or only when all else fails. My mission is to support the concept of nourishment first and early though sharing of “Nutrition Perspectives for the Pelvic Rehab Therapist” through the Herman & Wallace Pelvic Rehab Institute.
 After each weekend I teach Nutrition Perspectives for the Pelvic Rehab Therapist, I feel affirmed that this class, this information is vital and at times life-changing for practicing clinicians. And every time I teach, participants share that they take away much more than they expected. It’s a course that makes accessible complex concepts to entry level participants while offering timely and cutting edge integrative instruction to the advanced clinician eager to incorporate this knowledge into their practice. Supportive literature is woven throughout the tapestry of the course.
After each weekend I teach Nutrition Perspectives for the Pelvic Rehab Therapist, I feel affirmed that this class, this information is vital and at times life-changing for practicing clinicians. And every time I teach, participants share that they take away much more than they expected. It’s a course that makes accessible complex concepts to entry level participants while offering timely and cutting edge integrative instruction to the advanced clinician eager to incorporate this knowledge into their practice. Supportive literature is woven throughout the tapestry of the course.
After the most recent live course event, a participant shared with me a letter she received from a patient in 2016 who mentions the lack of nutritional attention during her cancer treatment. I want to share with you the essence of this letter:
“In October 2015, I was diagnosed with cancer. The following December I started treatments of radiation and chemotherapy. I really appreciate all the fine employees who helped me through care and treatments. Every clinician I came across, whether a doctor, nurse, phlebotomist, radiation and chemo teams, and my PT, were all exceptional in showing care, concern and knowledge.
However, one area I felt was lacking in was nutrition. I was frequently offered a standard hospital-issue protein drink. When offered, I explained that I would not take it due to it containing high fructose corn syrup (HFCS). I asked if they knew that HFCS was like putting and accelerant on a fire? I received a smile and a nod of head as to say they understood.
I was also offered soda pop to wash down bad tasting medicines/ liquids I was to take. I opted to just down the medication without chasing it as I didn’t want to exacerbate my condition. While taking chemotherapy, I was offered snacks containing HFCS and other non-nutritive so-called foods.
I was also offered limited entree choices, but there were plenty of pies, cakes, jellies, and other non-nutritive foods to choose from. All Items I would not consider for a cancer diet or even a healthy diet. I finally took a picture of the menu selection sheet as I thought no one would believe such a thing could happen.
I received excellent care throughout your system with the exception of nutrition . I would ask that you take a look at making menus with truly healthy options as well as giving patients options that do not contain ingredients that feed the cancer.”
While this letter addresses an inpatient issue at one regional health system, it correspondingly brings into focus the irony present in the vast majority of health care settings across the nation from inpatient to outpatient settings: there is a profound lack of clarity about what it means to be nourished, especially when we are at our most vulnerable.
I cannot claim “Nutrition Perspectives” will solve our nation-wide problem, however, I am certainly encouraging a movement towards a collective understanding of the imperative fact that food is medicine - powerful medicine - and we must as front-line practitioners harness what this understanding can offer. Pelvic rehab practitioners are uniquely positioned to process this information and begin immediately sharing it in clinical practice.
Like many providers, this same participant shared with me that upon receipt of this letter two years ago, she struggled to make progress with what and how to offer nutritional information - mainly because of the overwhelming nature of the subject, and also because of the conflicting and oftentimes confusing information traditionally shared with the public. After attending Nutrition Perspectives, she said “I cannot even begin to describe how much your course has met ALL my hopes for helping clients!….I had struggled to put something together and here it all is - so unbelievably grateful.”
And that’s what this course is all about - empowering you as you broaden your scope of knowledge in a way that teaches you not facts, but deep understanding. Once that foundational understanding is laid, this grass-roots effort will progress like putting an accelerant on the integrative movement. Soon we’ll see the inclusion of nourishment information as first-line practice, and the lives impacted in a positive way will continue to grow.
Please join me at the next opportunity to share in this live experience with other like-minded clinicians. Nutrition Perspectives for the Pelvic Rehab Therapist will be coming to Denver, CO September 15 & 16, 2018!
Advancing Understanding of Nutrition’s Role in…..Well….Everything
Gratitude filled my heart after being able to take part in the pre-conference course sponsored by the APTA Orthopedic Section’s Pain Management Special Interest Group this past February. For two days, participants heard from leaders in the field of progressive pain management with integrative topics including neuroscience, cognitive behavioral therapy, motivational interviewing, sleep, yoga, and mindfulness to name a few. It’s exciting to witness and participate in the evolution of integrative thinking in physical therapy. When it was my turn to deliver the presentation, I had prepared about nutrition and pain, I could hardly contain my passion. While so much of our pain-related focus is placed on the brain, I realized acutely the stone yet unturned is the involvement of the enteric nervous system (aka the gut) on pain and….well…everything.
Much appreciation is due to those on the forefront of pain sciences for their research, their insight, their tireless work to fill our tool boxes with pain education concepts. Neuroscience has made tremendous leaps and bounds as has corresponding digital media to help explain pain to our patients. One such brilliant 5-minute tool can be found on the Live Active YouTube channel.
What I love about this video is how intelligently (and artistically!) it puts into accessible language some incredibly complex processes. It even mentions lifestyle and nutrition as playing a role in what is commonly referred to as a maladaptive central nervous system.
"Maladaptive central nervous system"
Ok. I’ll admit, I struggle with the implications of this term. However, what doesn’t sit right with me is the concept of chronic or persistent pain being entirely in the brain as though the brain is a static entity. We know the brain to be plastic but often do not identify just how this is so.
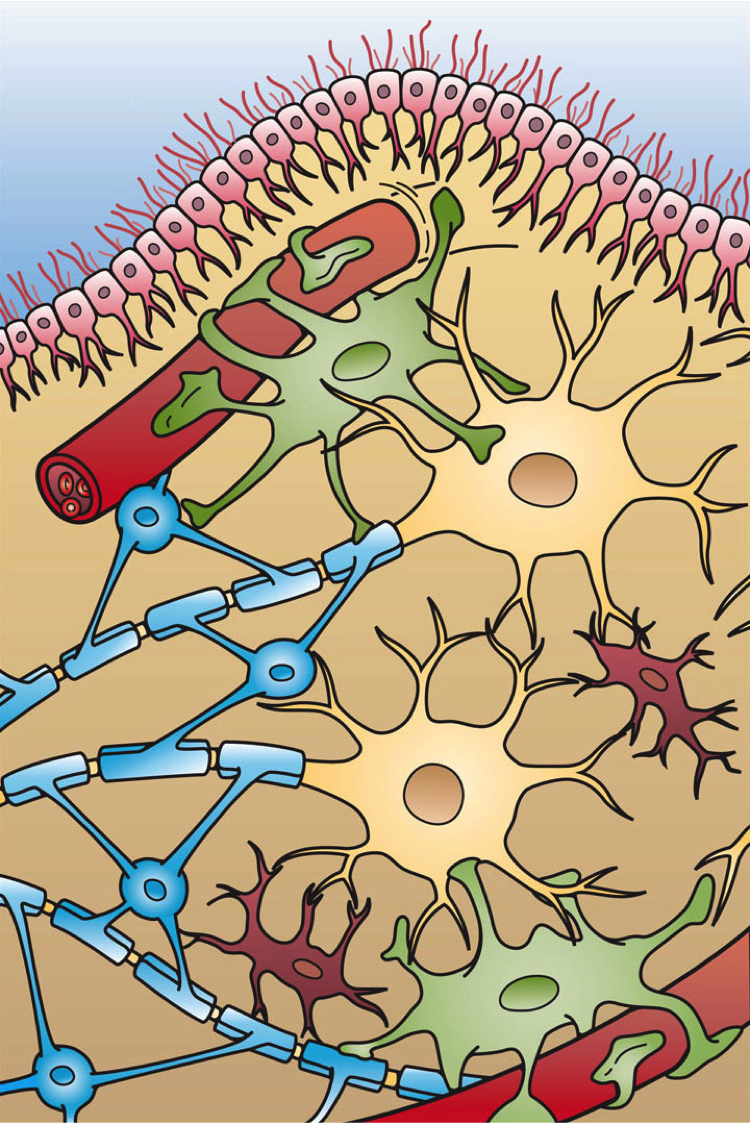 What about the role of our second brain…. the one with 200-600 million neurons that live in that middle part of our body (right next to / inside our pelvis)? Termed the enteric nervous system, this second brain both stores and produces neurotransmittersTurna, et.al., 2016, serves as the scaffolding of interplay between the ENS, SNS, and CNS. This ENS is home to the interface of “bugs, gut, and glial” which are “not only in anatomical proximity, but also influence and regulate each other…interconnected for mutual homeostasis.”Lerner, et.al., 2017 In fact, part of this process then directly impacts the brain. “Healthy brain function and modulation are dependent upon the microbiota’s [gut bugs] activity of the vagus nerve.”Turna, et.al., 2016. Further, “by direct routes or indirectly, through the gut mucosal system and its local immune system, microbial factors, cytokines, and gut hormones find their ways to the brain, thus impacting cognition, emotion, mood, stress resilience, recovery, appetite, metabolic balance, interoception and PAIN.”Lerner, et.al., 2017
What about the role of our second brain…. the one with 200-600 million neurons that live in that middle part of our body (right next to / inside our pelvis)? Termed the enteric nervous system, this second brain both stores and produces neurotransmittersTurna, et.al., 2016, serves as the scaffolding of interplay between the ENS, SNS, and CNS. This ENS is home to the interface of “bugs, gut, and glial” which are “not only in anatomical proximity, but also influence and regulate each other…interconnected for mutual homeostasis.”Lerner, et.al., 2017 In fact, part of this process then directly impacts the brain. “Healthy brain function and modulation are dependent upon the microbiota’s [gut bugs] activity of the vagus nerve.”Turna, et.al., 2016. Further, “by direct routes or indirectly, through the gut mucosal system and its local immune system, microbial factors, cytokines, and gut hormones find their ways to the brain, thus impacting cognition, emotion, mood, stress resilience, recovery, appetite, metabolic balance, interoception and PAIN.”Lerner, et.al., 2017
So, by process of logic, it requires little convincing to conclude that the food we eat or fail to eat directly impacts the health or dysfunction of this magnificently orchestrated system. One that directly and profoundly impacts our brain, our body, our being. And it’s a concept that our patients, our clients, ourselves, know in our gut to be true.
And it’s thanks to all the hard work of those who have come before us that we can share in the advancing understanding for the benefit of thousands who need your help, expertise and guidance. Please join me for Nutrition Perspectives for the Pelvic Rehab Therapist. The next course will be in Springfield, MO on June 23-24, 2018. Vital and clarifying information awaits you!
Live Active. (2013, Jan) Understanding Pain in less than 5 minutes, and what to do about it! https://www.youtube.com/watch?v=C_3phB93rvI Retrieved March 28, 2018.
Lerner, A., Neidhofer, S., & Matthias, T. (2017). The Gut Microbiome Feelings of the Brain: A Perspective for Non-Microbiologists. Microorganisms, 5(4). doi:10.3390/microorganisms5040066
Turna, J., Grosman Kaplan, K., Anglin, R., & Van Ameringen, M. (2016). "What's Bugging the Gut in Ocd?" a Review of the Gut Microbiome in Obsessive-Compulsive Disorder. Depress Anxiety, 33(3), 171-178. doi:10.1002/da.22454
I love adding flax seed to my recipes when I bake. I even hide it in yogurt with crushed graham crackers for my kids. It is a powerful nutrient that can be consumed without knowing it! Although the specific mechanism for its efficacy on prostate health continues to be researched, studies over the last several years applaud flax seed for its benefits and encourage me to keep sneaking it in my family’s diet.
 In 2008, Denmark-Wahnefried et al. performed a study to see if flax seed supplementation alone (rather than in combination with restricting dietary fat) could decrease the proliferation rate of prostate cancer prior to surgery. Basically, flax seed is a potent source of lignan, which is a phytoestrogen that acts like an antioxidant and can reduce testosterone and its conversion to dihydrotestosterone. It is also rich in plant-based omega-3 fatty acids. In this study, 161 prostate cancer patients, at least 3 weeks prior to prostatectomy, were divided into 4 groups: 1) normal diet (control); 2) 30g/day of flax seed supplementation; 3) low-fat diet; and 4) flax seed supplementation combined with low-fat diet. Results showed the rate of tumor proliferation was significantly lower in the flax seed supplemented group. The low-fat diet was proven to reduce serum lipids, consistent with previous research for cardiovascular health. The authors concluded, considering limitations in their study, flax seed is at least safe and cost-effective and warrants further research on its protective role in prostate cancer.
In 2008, Denmark-Wahnefried et al. performed a study to see if flax seed supplementation alone (rather than in combination with restricting dietary fat) could decrease the proliferation rate of prostate cancer prior to surgery. Basically, flax seed is a potent source of lignan, which is a phytoestrogen that acts like an antioxidant and can reduce testosterone and its conversion to dihydrotestosterone. It is also rich in plant-based omega-3 fatty acids. In this study, 161 prostate cancer patients, at least 3 weeks prior to prostatectomy, were divided into 4 groups: 1) normal diet (control); 2) 30g/day of flax seed supplementation; 3) low-fat diet; and 4) flax seed supplementation combined with low-fat diet. Results showed the rate of tumor proliferation was significantly lower in the flax seed supplemented group. The low-fat diet was proven to reduce serum lipids, consistent with previous research for cardiovascular health. The authors concluded, considering limitations in their study, flax seed is at least safe and cost-effective and warrants further research on its protective role in prostate cancer.
In 2017, de Amorim et al. investigated the effect of flax seed on epithelial proliferation in rats with induced benign prostatic hyperplasia (BPH). The 4 experimental groups consisting of 10 Wistar (outbred albino rats) rats each were as follows: 1) control group of healthy rats fed a casein-based diet (protein in milk); 2) healthy rats fed a flax seed-based diet; 3) hyperplasia-induced rats fed a casein diet; and 4) hyperplasia-induced rats fed a flax seed diet. Silicone pellets full of testosterone propionate were implanted subcutaneously in the rats to induce hyperplasia. Once euthanized at 20 weeks, the prostate tissue was examined for thickness and area of epithelium, individual luminal area, and total prostatic alveoli area. Results showed the hyperplasia induced rats fed a flax seed-based diet had smaller epithelial thickness as well as a reduced proportion of papillary projections found in the prostatic alveoli. These authors determined flax seed exhibits a protective role for the epithelium of the prostate in animals induced with BPH.
Bisson, Hidalgo, Simons, and Verbruggen2014 hypothesized a lignan-fortified diet could decrease the risk of BPH. The authors used an extract rich in lignan obtained from flax seed hulls. Four groups of 12 Wistar rats were used, with 1 negative control group and 3 groups with testosterone propionate (TP)-induced BPH (1 positive control, and 2 with diets containing 0.5% or 1.0% of the extract). Over a 5 week period, the 2 BPH-induced groups consuming the lignan extract starting 2 weeks prior to the BPH induction demonstrated a significant inhibition of prostate growth from the TP compared to the positive control group. These authors concluded the lignan-rich flax seed hull extract prevented BPH induction.
From BPH to prostate cancer, flax seed has proven a noteworthy supplement for preventative health. A tablespoon of flax seed in a muffin recipe is likely not a life-changing dose, but it’s a start. Nutrition Perspectives for the Pelvic Rehab Therapist enlightens practitioners with even more healthy choices, and Post-Prostatectomy Patient Rehabilitation gives you the necessary tools to help patients recover from prostate cancer.
Demark-Wahnefried, W., Polascik, T. J., George, S. L., Switzer, B. R., Madden, J. F., Ruffin, M. T., … Vollmer, R. T. (2008). Flax seed Supplementation (not Dietary Fat Restriction) Reduces Prostate Cancer Proliferation Rates in Men Presurgery. Cancer Epidemiology, Biomarkers & Prevention : A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology, 17(12), 3577–3587. http://doi.org/10.1158/1055-9965.EPI-08-0008
de Amorim Ribeiro, I.C., da Costa, C.A.S., da Silva, V.A.P. et al. (2017). Flax seed reduces epithelial proliferation but does not affect basal cells in induced benign prostatic hyperplasia in rats. European Journal of Nutrition. 56: 1201. https://doi.org/10.1007/s00394-016-1169-1
Bisson JF, Hidalgo S, Simons R, Verbruggen M. 2014. Preventive effects of lignan extract from flax hulls on experimentally induced benign prostate hyperplasia. Journal of Medicinal Food. 17(6): 650-656. http://doi.org/10.1089/jmf.2013.0046