In a recent article entitled “Physiotherapy Approaches in Individuals with Functional Defecation Disorders: Literature Review,” published in the Journal of Health Sciences in August of 2025, the use of surface EMG biofeedback (sEMG) was recommended as a first-step treatment for functional defecation disorders. It was concluded that biofeedback applications were superior to standard treatment and effective in improving patients’ quality of life. Both the American Neurogastroenterology and Motility Society and the American College of Gastroenterology recommend biofeedback as first-line therapy for dyssynergic defecation.
Surface electromyography (sEMG) biofeedback has emerged as one of the most effective conservative interventions for treating dyssynergic defecation, also known as pelvic floor dyssynergia. This condition is characterized by the paradoxical contraction or inadequate relaxation of the pelvic floor muscles and external anal sphincter during attempted defecation, resulting in functional outlet obstruction and chronic constipation. Dyssynergia affects many of our clients with chronic constipation and is a prevalent referral diagnosis in pelvic floor rehabilitation. For pelvic health therapists, sEMG biofeedback provides a valuable therapeutic tool that directly retrains neuromuscular coordination, corrects maladaptive defecation mechanics, and improves patient outcomes without the risks associated with pharmacologic or surgical interventions.
How Surface EMG Biofeedback Works
Biofeedback therapy addresses the underlying pathophysiology of dyssynergia by helping patients learn to modulate pelvic floor muscle activity during simulated defecation. Surface EMG biofeedback uses external perianal or intrarectal sensors to record muscle activation patterns, visually displaying motor unit firing in real time on a monitor. When patients attempt defecation, those with dyssynergia often engage in compensatory or dysfunctional mechanics such as breath-holding, strain maneuver without pelvic floor relaxation, or tightening of the external anal sphincter and puborectalis muscle. Biofeedback enables patients to see these abnormalities and receive immediate coaching to correct them. This learning model aligns with the principles of motor relearning and neuroplasticity and is particularly effective for reeducating muscles involved in autonomic and habitual reflex responses, including those of the pelvic floor.
A key benefit of surface EMG biofeedback is its ability to correct maladaptive motor patterns rather than merely provide symptomatic relief. Unlike laxatives, which simply soften stool or increase motility, biofeedback teaches coordinated defecation by training patients to relax the anal sphincter, lengthen the pelvic floor, and generate appropriate intra-abdominal pressure. Many patients demonstrate dyssynergic patterns such as Type I dyssynergia, where the pelvic floor contracts during attempted evacuation, or Type III, where inadequate abdominal force is generated. Biofeedback helps individualize treatment, as therapists can use EMG data to identify specific coordination deficits and modify training accordingly. In addition, EMG signals provide objective progress markers, reinforcing patient engagement and compliance.
Another important clinical advantage of biofeedback is that it is non-invasive, safe, and well-tolerated across patient populations. It is appropriate for adults, older adults, and even motivated pediatric patients. Side effects are minimal, especially with surface EMG sensors that eliminate the need for internal probes when preferred clinically. This makes EMG biofeedback a valuable option for patients who may not tolerate rectal balloon training or invasive anorectal procedures due to pain, anxiety, or trauma history.
Integrating Biofeedback into Pelvic Rehabilitation
Biofeedback therapy integrates well within holistic pelvic rehabilitation programs. Treatment typically includes coordination training, diaphragmatic breathing, colonic massage instruction, toileting posture education, bowel mechanics retraining, and behavioral strategies to restore normal recto-anal sensory reflexes. Surface EMG enhances the effectiveness of behavioral training by improving patients’ proprioceptive awareness of their pelvic floor, a region in which neuromuscular awareness is typically poor. Additionally, EMG biofeedback can incorporate downtraining techniques to reduce high resting pelvic floor tone.
Despite its proven benefits, access to biofeedback therapy can be inconsistent due to limited awareness among healthcare providers and insufficient training opportunities for therapists. However, pelvic health therapists are uniquely positioned to deliver this intervention effectively due to their expertise in neuromuscular reeducation, movement analysis, and behavioral coaching. Incorporating sEMG biofeedback into a pelvic rehabilitation practice not only aligns with evidence-based care but also enhances clinical credibility and expands therapeutic capabilities, especially for patients with chronic functional bowel disorders.
Surface EMG biofeedback offers substantial therapeutic benefits for the treatment of pelvic floor dyssynergia. It is superior to standard medical therapy, targets the root cause of dyssynergia through neuromuscular retraining, promotes long-term bowel function normalization, and empowers patients to take an active role in their recovery. With growing clinical validation and patient demand for non-pharmacologic treatments, sEMG biofeedback should be considered an essential component of pelvic floor therapy practice. For pelvic health therapists seeking to deliver advanced, evidence-based care, biofeedback represents a powerful and effective intervention with lasting results.

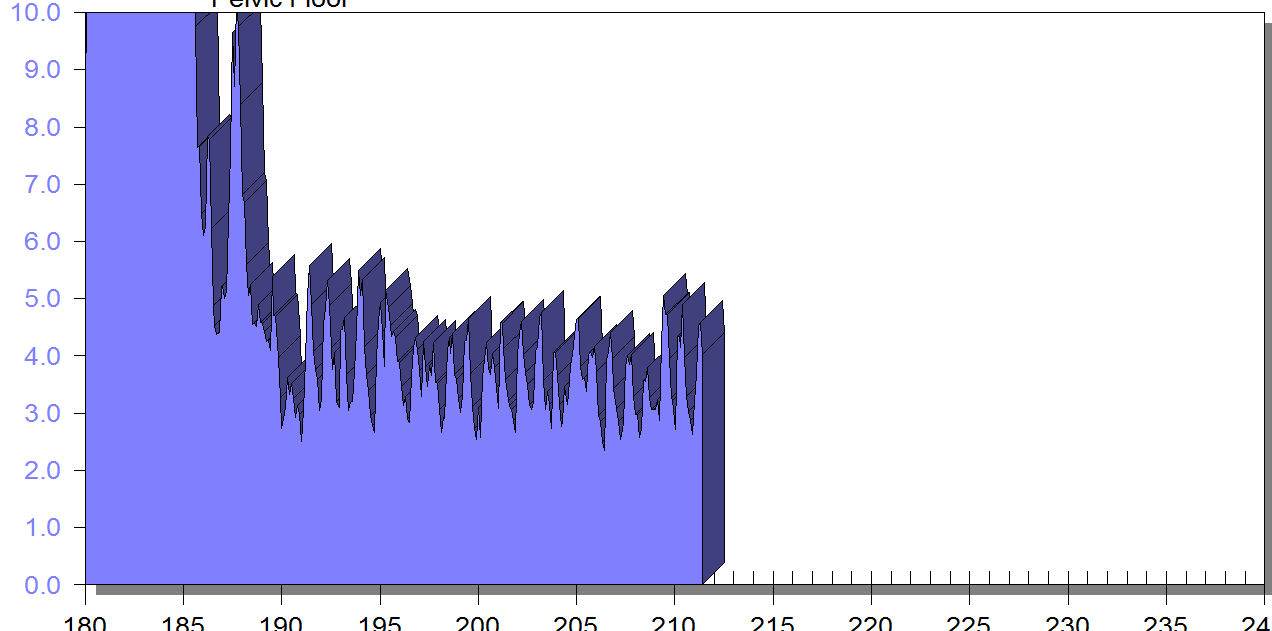
Excessive pelvic floor activity during attempts at bowel evacuation creates a mechanical barrier to evacuation and demonstrates dyssynergia (incoordination). When a patient “bears down” the abdominals (blue) should increase, and the pelvic floor (green) should relax.

Correct pattern: Pelvic floor muscles relax and abdominal muscles contract to increase intra-abdominal pressure for proper bowel movement coordination.
Conclusion
A long history of scientific evidence supports the use of sEMG biofeedback for managing incontinence or pain symptoms. As a noninvasive, cost-effective, and powerful treatment modality, healthcare providers should consider this tool when managing pelvic floor dysfunction. Providers should be adequately educated in this valuable modality to make the most of the skills and knowledge gained through this intervention. For more information regarding courses and certification, please visit www.pelvicfloorbiofeedback.com.
Biofeedback for Pelvic Muscle Dysfunction is available in satellite and self-hosted formats.
Biofeedback for Pelvic Muscle Dysfunction, scheduled for December 13, 2025, is led by board-certified Instructors Jane Kaufman and Tiffany Lee, who introduce participants to the use of biofeedback in the treatment of bladder, bowel, and pelvic floor disorders. In this course, participants learn about surface EMG biofeedback by using the equipment on themselves to experience dynamic muscle assessment in supine, sitting, and standing positions. This dynamic course also includes behavioral strategies to relearn proper muscle control and improve pelvic floor function.
If you attend this course at a scheduled hosted location (NOT self-hosted), then the equipment will be supplied by our biofeedback vendor, Current Medical Technologies. Satellite Locations for December 13th are:
Self-hosted participants do not need partners and can treat themselves using the equipment. Equipment used in this course, and required for all self-hosted registrants, is as follows (all items can be purchased on www.cmtmedical.com):- A 2-channel sEMG biofeedback hand-held unit with software on a laptop or computer is required. The instructors will teach biofeedback with the Prometheus Telesis software. Participants can use MR-20, MR-25, EMYO, CTS 1500, or CTS 2000.
- The participants who are self-hosting will need a vaginal or rectal sensor and abdominal leads. Alternatively, participants can use external perianal electrodes.
- To use the disposable external electrodes, participants will need a Pathway Velcro adapter (PG-3660), 1 Pathway External Adapter (PG-7100), and Vermed sEMG disposable lead wire set (VM-A10057-S).
- Another option for external electrodes are the Pre-gelled sEMG Biofeedback Electrodes (DE-301) with a 24-inch external lead wire set (PG-5328).
References:
- Büyüktaş, N., & Bakar, Y. (2025). Physiotherapy Approaches in Individuals with Functional Defecation Disorders: Literature Review. Fenerbahçe University Journal of Health Sciences, 5(2), 281-291.
- Kaufman, J., Stanton, K., & Lee, T. E. (2021). Pelvic Floor Biofeedback for the Treatment of Urinary Incontinence and Fecal Incontinence. Biofeedback, 49(3), 71-76.
- Rao, S. S., Benninga, M. A., Bharucha, A. E., Chiarioni, G., Di Lorenzo, C., & Whitehead, W. E. (2015). ANMS‐ESNM position paper and consensus guidelines on biofeedback therapy for anorectal disorders.Neurogastroenterology & Motility, 27(5), 594-609.
- Shelly, Beth & Kaufman, Jane (2023). Foundations of Pelvic Floor Muscle Assessment Using Surface Electromyography. APTA Academy of Pelvic Health Physical Therapy.
AUTHOR BIO
Tiffany Lee, OTR, OTD, MA, BCB-PMD, PRPC
 Tiffany Lee holds a BS in OT from UTMB Galveston (1996), an MA in Health Services Management, and a post-professional OTD from Texas Tech University Health Sciences Center. In 2004, she received her board certification in Pelvic Muscle Dysfunction from the Biofeedback Certification International Alliance. She is a Herman and Wallace Pelvic Rehab Institute faculty member and teaches biofeedback courses. She has been treating pelvic health patients for 25 out of her 30-year career. Her private practice in San Marcos, Texas, is exclusively dedicated to treating urinary and fecal incontinence and pelvic floor disorders. Her continuing education company, Biofeedback Training & Incontinence Solutions, offers clinical consultation and training workshops. She also enjoys mentoring healthcare professionals working toward their BCIA certification.
Tiffany Lee holds a BS in OT from UTMB Galveston (1996), an MA in Health Services Management, and a post-professional OTD from Texas Tech University Health Sciences Center. In 2004, she received her board certification in Pelvic Muscle Dysfunction from the Biofeedback Certification International Alliance. She is a Herman and Wallace Pelvic Rehab Institute faculty member and teaches biofeedback courses. She has been treating pelvic health patients for 25 out of her 30-year career. Her private practice in San Marcos, Texas, is exclusively dedicated to treating urinary and fecal incontinence and pelvic floor disorders. Her continuing education company, Biofeedback Training & Incontinence Solutions, offers clinical consultation and training workshops. She also enjoys mentoring healthcare professionals working toward their BCIA certification.
This article is contributed by faculty members Tiffany Lee and Jane Kaufman. Their course, Biofeedback for Pelvic Floor Muscle Dysfunction, is scheduled for December 4-5, 2021 provides a safe space for clinicians to learn and practice this valuable tool.
Rarely do practitioners see a topic so argued in pelvic rehabilitation as the use of surface EMG biofeedback. There are practitioners who boldly state they are for or against it on their social media accounts and clinic pages. Therapists are not questioning the use of biofeedback with neurologic or orthopedic applications, so why is it such a polarizing topic in pelvic health? The Pelvic Rehab Report sits down with faculty members Tiffany Lee and Jane Kaufman to discuss the tool they love. This month they published a Special Issue article in the Biofeedback Journal for the Association for Applied Psychophysiology and Biofeedback. These two instructors have over 50 years of combined experience using biofeedback.(*)
Biofeedback provides visual and auditory feedback of muscle activity and is a non-invasive technique that allows patients to adjust muscle function, strength, and behaviors to improve pelvic floor function. The small electrical signal (EMG) provides information about an unconscious process and is presented visually on a computer screen, giving the patient immediate knowledge of muscle function, enabling the patient to learn how to alter the physiological process through verbal and visual cues. Jane Kaufman explains that "many patients gain knowledge and awareness of the pelvic floor muscle through tactile feedback, but the visual representation is what helps patients to hone in on body awareness and connect all the dots." Muscle evaluation through digital exam offers strength but does not appropriately address electrical activity such as resting tone, ability to recruit or release tone in the muscle. The use of biofeedback addresses the specificity of muscle contraction and release offering an additional view of muscle function.
In a 2020 research study by Pilkar et al, clinicians reported sEMG barriers of use which included limited time and resources, clinically inapplicable sEMG system features, and the majority of clinicians' lack of training and/or confidence in utilization of sEMG technology. This research also noted technical challenges including the limited transfer of ever-evolving sEMG research into the off-the-shelf EMG systems, nonuser-friendly intuitive interfaces, and the need for a multidisciplinary approach for accurate handling and interpretation of data. (1)
To break this down into layman terms, one contraindication may be the price of a biofeedback unit. Tiffany Lee recommends using a 2-channel sEMG biofeedback hand-held unit with the software on a laptop or computer. In fact, to become board certified in pelvic floor biofeedback, the Biofeedback Certification International Alliance (BCIA) requires that you have a 2 channel EMG system with software. If you are using a hand-held one channel unit, the patient will have a difficult time seeing the muscle activity and the coordination between the abdominals and pelvic floor. This prevents meaningful treatment with this treatment tool as the patient cannot understand or interpret the LED bars on the machine (and often the therapist cannot understand either). In truth, the benefits outweigh the cost of the equipment and within a few treatments, you can cover the cost of the unit with the appropriate software to offer the proper visualization of muscle function.
Training is another issue, to start utilizing biofeedback in your clinical setting you need to have proper training in the modality. Most therapists have never been properly trained and if they take a course where the instructor doesn’t believe in the benefits of biofeedback, they feel negatively toward a tool they have never personally explored. Biofeedback relies on a skilled clinician to interact with the patient, give verbal cues, ensure that the proper muscles are contracting and relaxing, and must be used in conjunction with their other skills and knowledge.
Think of sEMG biofeedback as a tool in your toolbox. Tiffany shares, "in a study by Aysun Ozlu MD, et al., the authors conclude that biofeedback-assisted pelvic floor muscle training, in addition to a home exercise program, improves stress urinary incontinence rates more than home exercise program alone." She continues, "Biofeedback is a powerful tool that can benefit your patient population and add to your skill-set."(2)
Essentially, the acceptance of sEMG biofeedback in rehabilitation requires a unit (with software and sensors), training, and a multidisciplinary approach. Used correctly, it can positively impact patient performance and care in the clinic. Keep in mind sEMG is a non-invasive technique. It has already shown great promise in the field of neuro-rehabilitation and has been a widely-utilized tool to assess neuromuscular outcomes in research. Jane Kaufman concludes that "In short, biofeedback treatment/training using the proper instrumentation provides the precise information necessary to change behaviors." This gives the patient the opportunity to recognize that ‘yes, they are in charge of this muscle and that they can achieve success in overpowering the symptoms.’ Biofeedback routinely allows the patient to understand that they are empowered to heal themselves with the tools you offer. They are in charge of their bodies and the outcome of treatment.
There is a long history of scientific evidence to support the use of sEMG biofeedback in the management of incontinence symptoms or pain symptoms. As a non-invasive, cost-effective, and powerful treatment modality, healthcare providers should consider this treatment tool when managing patients with pelvic floor dysfunction. Providers should be educated in the proper use of this valuable modality to gain the most out of the skills and knowledge that can be achieved through this intervention. For more information regarding courses and certification please visit www.BCIA.org.
Tiffany asked several PTs and OTs that have been to the board certification courses what they love about biofeedback. Here are a few answers:
- “Biofeedback empowers my patients and gives them the confidence that they are actually doing their exercises and/or relaxing correctly! I’ve had nothing but positive feedback from patients and it’s such a great tool to have as a pelvic floor therapist.”
- “My patients really love it, and they ask for it. I especially see the value for dyssynergia work on bearing down and learning eccentric abdominals and relaxed pelvic floor muscles. For men, I work on relaxing in standing and postures if they can’t empty their bladder. Ultimately the treatment needs to be meaningful to the patient. Biofeedback can complement other treatments. Their needs come before ours.”
- “After ONE session with a 5-year-old with constipation, mom called me in sheer excitement, screaming over the phone that he pooped on the potty!!! Something he has NEVER done before. Biofeedback helped him find and coordinate the potty muscles and tummy muscles and this made a huge difference for him!”
- “Becoming certified in biofeedback has only been positive for me. My patients feel that the initial sEMG evaluation sets the stage for my plan of care, and my reassessment at discharge is a tangible reflection of their progress. Not to mention its strength as a marketing tool.”
The Satellite Lab Course, Biofeedback for Pelvic Floor Muscle Dysfunction, scheduled for December 4-5, 2021 provides a safe space for clinicians to learn and practice this valuable tool. Registrants will gain knowledge about the benefits of using this modality in their clinical practice. Participants will learn how to administer biofeedback assessments, analyze and interpret sEMG signals, conduct treatment sessions, and role-playing patient instruction/education for each diagnosis presented during the many hands-on lab experiences.
Special Issue article in the Biofeedback Journal for the Association for Applied Psychophysiology and Biofeedback
- * Pelvic Floor Biofeedback for the Treatment of Urinary Incontinence and Fecal Incontinence. Jane Kaufman, PT, MEd BDB-PMD; Kathryn Stanton, PT, DPT; Tiffany Ellsworth Lee, MA, OTR BCB-PMD, PRPC. Biofeedback (2021) 49 (3): 71–76. https://doi.org/10.5298/1081-5937-49.3.01.
References:
- Use of Surface EMG in Clinical Rehabilitation of Individuals With SCI: Barriers and Future Considerations. Rakesh Pilkar, Kamyar Momeni, Arvind Ramanujam, Manikandan Ravi, Erica Garbarini, Gail F. Forrest. Front Neurol. 2020; 11: 578559. Published online 2020 Dec 18. doi: 10.3389/fneur.2020.578559 PMCID: PMC7780850
- Comparison of the efficacy of perineal and intravaginal biofeedback assisted pelvic floor muscle exercises in women with urodynamic stress urinary incontinence. Aysun Ozlu MD, Neemettin Yildiz MD, Ozer Oztekin MD. Neurourol Urodyn. 2017 Nov;36(8):2132-2141. Epub 2017 Mar 27. doi: 10.1002/nau.23257 PMID: 28345778.
- The basics of surface electromyography. R. Cram, G. S. Kasman. In E. Criswell (Ed.). Cram’s introduction to surface electromyography (2nd ed., pp. 3–7.) Jones and Bartlett. 2011
Using sEMG biofeedback to get real-time results
Tiffany Lee, MA, OTR, BCB-PMD and Jane Kaufman, PT, BCB-PMD are internationally board-certified clinicians in the treatment of pelvic floor muscle dysfunction through the Biofeedback Certification International Alliance. Combined, they have over fifty years of treatment experience using sEMG biofeedback. Their new course, “Biofeedback for Pelvic Floor Muscle Dysfunction”, will provide the nuts and bolts of this powerful tool so that clinicians can return to the clinic after this course with another component to their toolbox of treatment strategies.
 As a clinician treating patients with pelvic floor muscle dysfunction, have you gone away from a treatment session and asked yourself ‘what else can I do for this patient?’. Have you considered adding surface EMG, often referred to as biofeedback, to your treatment plan, but aren’t sure how to go about it correctly or effectively? Perhaps you think you can’t use the sensor because the patient has pain. Maybe you think biofeedback only helps with up-training or strengthening.
As a clinician treating patients with pelvic floor muscle dysfunction, have you gone away from a treatment session and asked yourself ‘what else can I do for this patient?’. Have you considered adding surface EMG, often referred to as biofeedback, to your treatment plan, but aren’t sure how to go about it correctly or effectively? Perhaps you think you can’t use the sensor because the patient has pain. Maybe you think biofeedback only helps with up-training or strengthening.
So exactly what is biofeedback? Why should I consider this modality? Biofeedback provides a non-invasive opportunity for patients to see muscle function visualized on a computer screen in a way that allows for immediate feedback, simple representation of muscle function, and allows the patient and the clinician the opportunity to alter the physiological process of the muscle through basic learning strategies and skilled cues. Many patients gain knowledge and awareness of the pelvic floor muscle through tactile feedback, but the visual representation is what helps patients really hone in on body awareness and connect all the dots. Here are a few comments that our patients have made; “I can now pay attention to my muscle while at work thanks to the visual of my muscle when sitting and standing”; “I needed to see my muscle to fully understand how to release the tension in it “; “I totally get what I need to do now that I have a clear picture of what you want”; “Seeing is believing”.
A 2017 study by Moretti, E., et al. is a great article that helps support the concept that measuring the pelvic floor electrical activity through a standard vaginal sensor is not always an option. For many patients, use of surface electrodes with peri-anal electrodes will provide the same reading and offer a more comfortable alternative for those patients who cannot use an internal sensor. This allows the clinician more opportunities to use this treatment modality with ease and assurance that the patient can learn from the visual representation of the muscle without fear of penetration from a sensor, and get great results!
In another study by Aysun Ozlu MD, et al. the authors conclude that biofeedback assisted pelvic floor muscle training, in addition to a home exercise program, improves stress urinary incontinence rates more than home exercise program alone.
Herman & Wallace is offering a course for clinicians in Alexandria, Virginia this June that will answer all of your questions and concerns about this fabulous treatment tool: biofeedback! This course enables the clinician to learn and practice this valuable tool and gain knowledge about the benefits of this modality, so that treatment can begin immediately with ample opportunity for patient’s positive feedback and awareness of muscle function. Participants will experience being a biofeedback practitioner and patient (using a self-inserted vaginal or rectal sensor). Participants will be administering biofeedback assessments, analyzing and interpreting sEMG signals, conducting treatment sessions, and role-playing patient instruction/education for each diagnosis presented during the many hands-on lab experiences. Biofeedback is a powerful tool that can benefit your patient population, and add to your skill-set.
Moretti, E., Galvao de moura Filho, A., Correia de Almedia, J., Araaujo, C., Lemos, C. “Electromyographic assessment of women’s pelvic floor: What is the best place for a superficial sensor?” Neurology and Urodynamics; 2017; 9999:1-7.;
Aysun Ozlu MD, Neemettin Yildiz MD, Ozer Oztekin MD, “Comparison of the efficacy of perineal and intravaginal biofeedback assisted pelvic floor muscle exercises in women with urodynamic stress urinary incontinence”
Influencing pelvic floor EMG activity through hip joint mobilization and positioning
EMG is a helpful tool to observe pelvic floor muscle activity and how it is influenced by everything from regional musculoskeletal factors and mucosal health, to client motor control, awareness, and comfort.
In this post I will discuss the case of one client who was referred for dyspareunia treatment, and whose SEMG findings are outlined in Figures 1-3. She had validated test item clusters for right hip labral tear as well as femoral acetabular impingement, in addition to right sided pelvic floor muscle overactivity and sensitivity with less than 3 ounces of palpation pressure.
The figures below demonstrate peri-anal SEMG response of pelvic floor muscles within a single treatment session, which included sacral unloading in supine as well as hip joint mobilization to demonstrate the relationship between her pelvic floor and her hips. Our focus for this SEMG downtraining treatment was to enable her to understand the connection between her pelvic floor muscle holding patterns and her body’s preferences to remain out of ranges of motion that impinged and irritated her hip.
By creating a clear understanding of how the client could 'listen" to her muscle activity via SEMG (as well as her kinesthetic awareness of her own comfort), she began to understand the difference between body and hip position, her pelvic floor muscle activity, and her pain during intercourse.
Pelvic floor motor control with normalized respiration, orthopedic considerations of sexual activity, and other physical therapy as well as multidisciplinary treatments were integrated into her ability to resume intercourse. The lens of SEMG, however, was a powerful tool to help her make the connection between her hip and its influence on her pelvic floor overactivity and symptoms.
Musculoskeletal co-morbidities in pelvic pain are common, requiring the clinician to have a set of test item clusters to scan and clear key structures, as well as the ability to convey this information without creating distress to the client when positive findings are discovered. For example, labral tears and subchondral cysts are common findings in asymptomatic clients and physical therapy plays a key role in reducing client fear, avoiding symptom provocation, reducing regional muscle overactivity, as well as facilitating movement and strengthening in painfree ROM.
Although this case example describes intraarticular hip dysfunction as a driver of this clients PFM overactivity, Finding the Driver in Pelvic Pain is a course that is designed to cover comprehensive key test item clusters for a fundamental pelvic pain scan exam of intrapelvic as well as extrapelvic drivers, to ensure the clinician understands the contributing factors that can influence or be influenced by the pelvic floor. This course is best suited for physical therapists and physical therapist assistants who are looking to create an organized approach to their scan exam for pelvic pain. For non-physical therapists, this can be a powerful introduction to the skill set and vocabulary needed to create a multidisciplinary team with a PT in the treatment of these clients.
FIGURE 1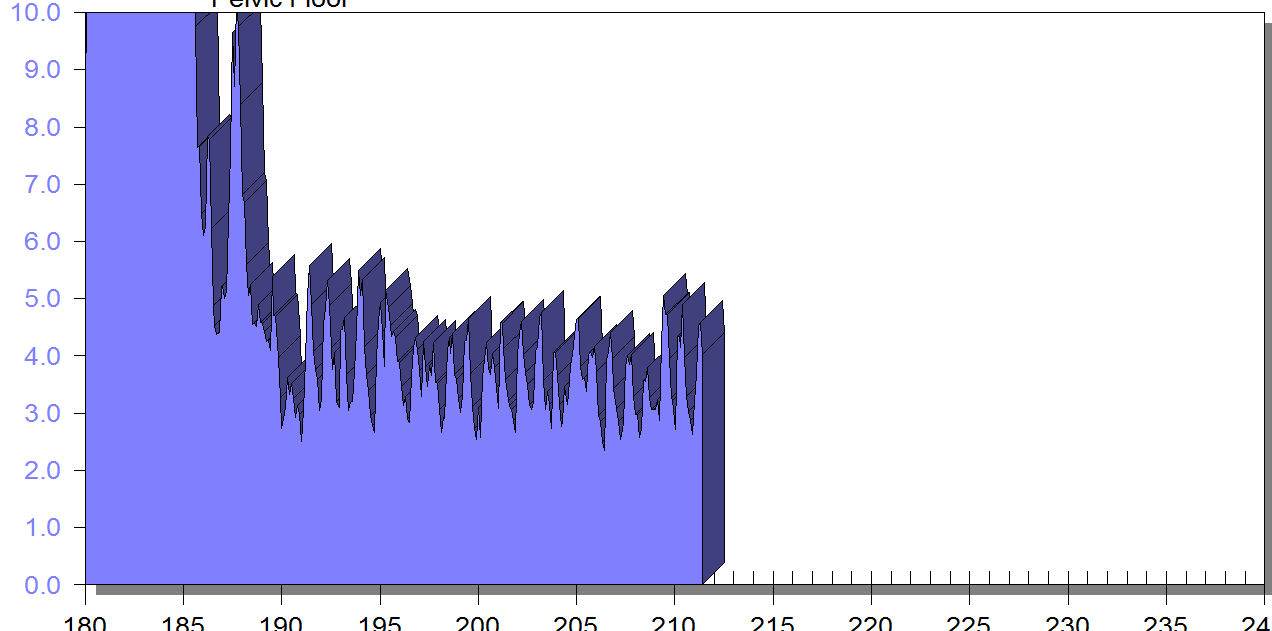
PFM EMG at rest in supine, knees bent, feet on table (peri-anal SEMG electrode placement)
FIGURE 2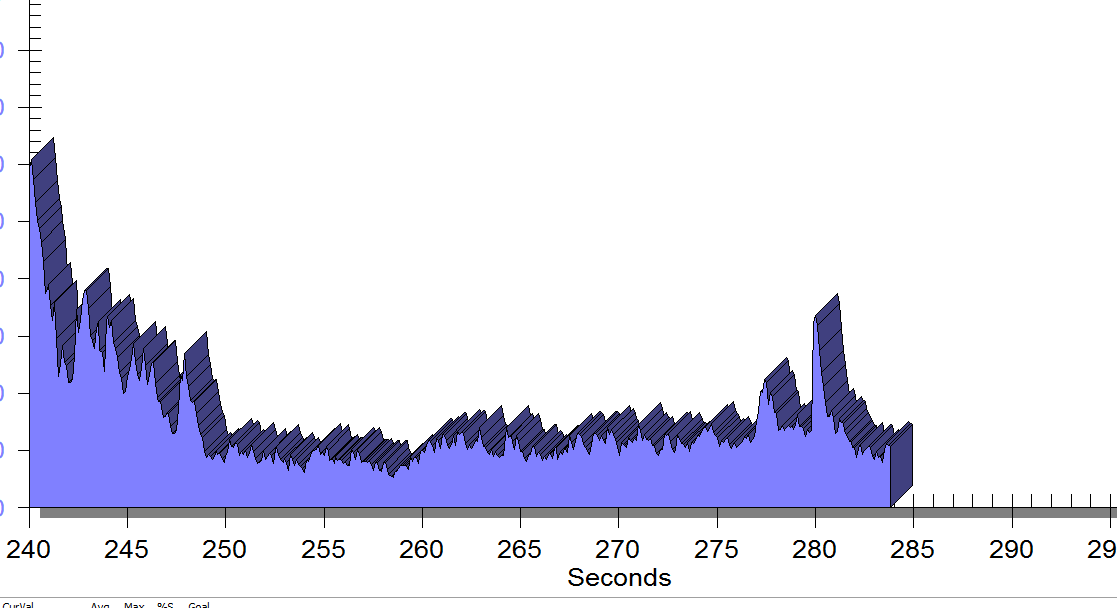
Same position, only with sacral unweighting by placing folded towels on either side of sacrum, unweighting all pressure from sacrum. Immediate report of increased comfort in buttocks, hips and pelvis.
Figure 3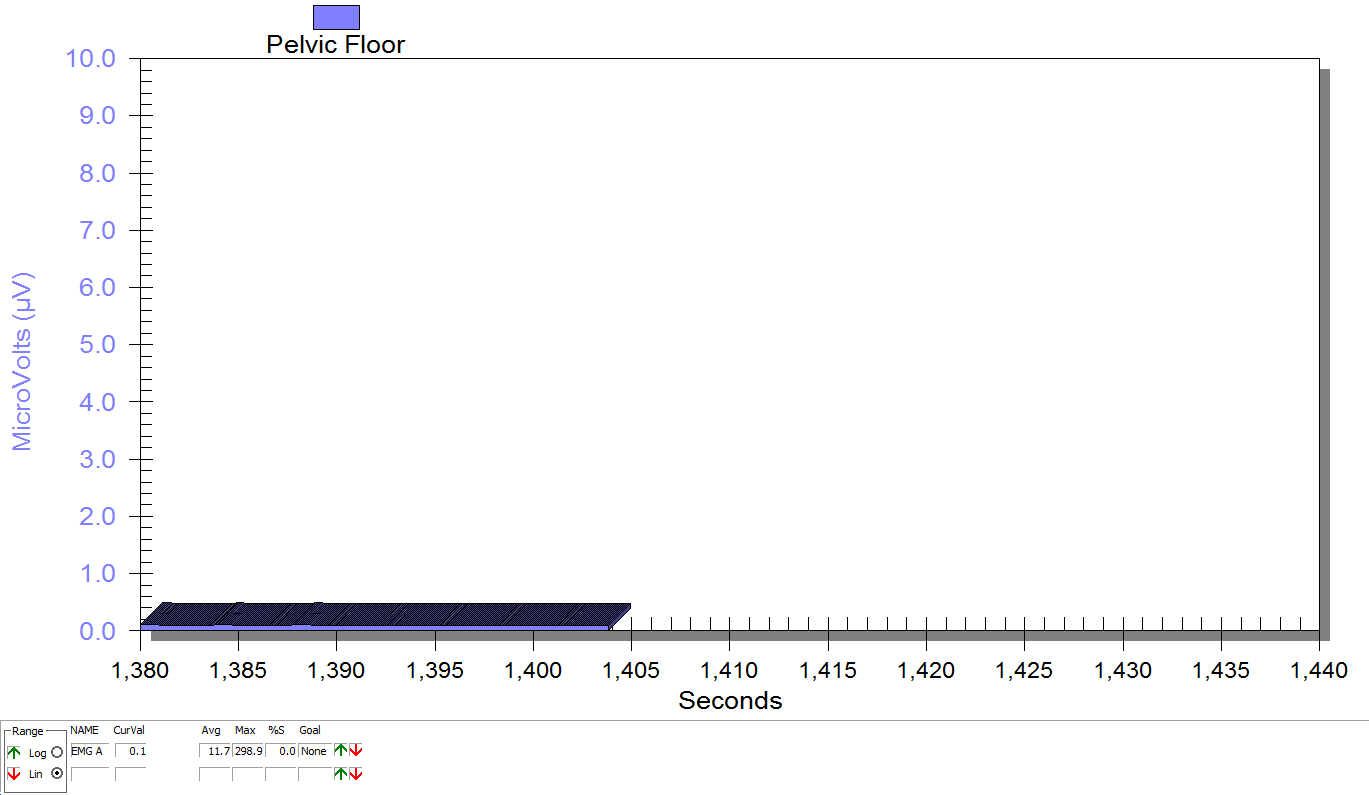
Supine, sacrum unweighted as in figure 2, after multidirecitonal hip joint mobilizaiton.
Groh, Herrera. A comprehensive review of hip labral tears. Curr Rev Musculoskelet Med. 2009 Jun; 2(2): 105–117. Published online 2009 Apr 7. doi: 10.1007/s12178-009-9052-9
Yosef, et al. Multifactorial contributors to the severity of chronic pelvic pain in women. Am J Obstet Gynecol. 2016 Dec;215(6):760.e1-760.e14. doi: 10.1016/j.ajog.2016.07.023. Epub 2016 Jul 18.