Darla Cathcart, PT, DPT, Ph.D., WCS, CLT graduated from Louisiana State University (Shreveport, LA) with her physical therapy degree, performed residency training in Women’s Health PT at Duke University, and received her Ph.D. from the University of Arkansas Medical Sciences. Her dissertation research focus was on using non-invasive brain stimulation to augment behavioral interventions for women with lifelong vaginismus, and her ongoing line of research will continue to center around pain with intercourse. Darla is part of Herman & Wallace's core faculty and recently launched her own course Vaginismus and Vulvovaginal Dyspareunia. She sat down with the Pelvic Rehab Report to discuss working with vaginismus and vulvovaginal dyspareunia patients.
I believe one of the most important things that we as pelvic therapists can do for patients experiencing vaginismus and vulvovaginal dyspareunia is to offer HOPE!
These patients often arrive at therapy with a belief that something is uniquely wrong with them. Often, they have been to more than a handful of other doctors and care providers who are unfamiliar with pelvic floor problems causing pain with sex (which is substantiated by the research) who have maybe given them messages of "I can't find anything wrong with you" and "You just need to relax."
If I had a dollar for every time a patient told me that another care provider told them to "Just drink a glass of wine before sex to help you relax" (palm to forehead!)...These messages often cause these patients to feel as if their pain with sex is made up in their heads, or that a scary diagnosis is being overlooked.
Unfortunately, unless they have found a provider who can quickly identify that the patient has a musculoskeletal problem with the pelvic floor that needs a pelvic therapy referral, then the patient has often gone for many months, years, or even a decade or more without being properly heard or getting the right help.
When I sit down with a patient, after hearing a bit of that person's story, I typically start the conversation with "Thank you for sharing your story. I want you to know that you are not alone - a big percentage of my patients have pain with sex. I also want you to know that based on what you are telling me, you will likely get better as most of them have done."
Patients often express relief, sometimes disbelief, or both, mixed with some hope - a bit of "Ah, this person hears me and knows what I'm talking about, and says I can get better!" The belief of being able to get better, even if mixed with some doubt, is an extremely valuable start on their healing journeys.
There are many factors that the pelvic therapist could consider to facilitate conversations around pain with sex.
As with all of our patients seeking pelvic rehab, communication requires non-judgment and respecting a patient's boundaries. Asking a patient "Have you been sexually abused or had sexual trauma in the past?" can feel unnerving and alarming for a patient who is not ready to have that conversation with their pelvic therapist. However, asking a patient "Have you had any negative sexual experiences that you would like to share, that you feel may be impacting your symptoms?" allows the patient to decline until they feel ready to engage in such a conversation.
This softer approach lets the patient know that the therapist is open to a conversation about impactful events and respects that patient's autonomy in sharing that history. Putting the patient in the driver's seat is also critical. For instance, consider a patient who, theoretically, would benefit greatly from using vaginal trainers (dilators) but declines to use them. An approach of "but using trainers will be the only way to get better" may result in the patient quitting therapy, or worse, feeling traumatized from the therapy experience. Alternatively, affirming to patients that the treatments chosen are their prerogative keeps the path for ongoing healing and provider trust.
A statement of "Not using vaginal trainers is your choice, but we can always consider them again in the future if you change your mind. Let me talk you through the alternative treatments, and how their effects will differ from that of the vaginal trainer use" leaves the door open to return to that treatment down the road if the patient chooses, and also respects the choice of the patient in the moment. The key is to not be pushy about pursuing the undesired treatment down the road! It could be mentioned again, but use judgment and caution in the approach.
A final highlight is being sure to give patients space to share their story, as often they have not been heard by previous providers or their symptoms have been discounted.
My course Vaginismus and Vulvovaginal Dyspareunia, is scheduled for March 3rd and September 14th this year and takes a deep dive into the detail of how to make the rubber meet the road to not only get treatment started but to really help progress a patient into a satisfying sex life. This course was developed so that the participant could leave this course and understand how to really approach the examination, history taking, and step-by-step procedures in instructing and using vaginal trainers and other tools for patients having painful intercourse. Additionally, this course should increase the practitioner's confidence in incorporating instructions and education related to a patient's concerns about the female sexual cycle and response (arousal, desire, orgasm), sexual positioning, lubrication, and partner integration.
Darla Cathcart, PT, DPT, WCS, CLT graduated from Louisiana State University (Shreveport, LA) with her physical therapy degree, performed residency training in Women’s Health PT at Duke University, and received her Ph.D. from the University of Arkansas Medical Sciences. Her dissertation research focus was on using non-invasive brain stimulation to augment behavioral interventions for women with lifelong vaginismus, and her ongoing line of research will continue to center around pain with intercourse. Darla is part of Herman & Wallace's core faculty and instructs Pelvic Floor Level 1, Level 2A, and Level 2B, the Pregnancy & Postpartum Series, and recently launched her own course Vaginismus and Vulvovaginal Dyspareunia.
How is this class different from the information in Pelvic Floor 2B?
The main difference is in the questions that these two courses answer: "what treatments can I use" versus "how can I use those treatments effectively?" In Pelvic Floor Level 2B, participants are told about various methods for addressing pain with intercourse (such as using vaginal trainers/dilators and manual therapy techniques), with brief descriptions of how to use some of these tools. In this Vaginismus and Vulvovaginal Dyspareunia course, we go into depth on how to use these treatments specifically based on a patient's examination findings and goals.
What are the top 5 takeaways a practitioner could hope to gain from this class?
1. Vaginal Trainers (dilators) can be more effective when going beyond "just sticking them in."Traditionally, patients have been taught to just insert "dilators" to a point of stretching and discomfort, and to hold that stretch, maybe even distract themselves from the activity by watching TV or reading a book. As with other areas of the body, using active methods to increase tissue flexibility, such as incorporating contract-relax and breathing techniques, can really enhance the treatment! During the labs in this 100% remote course (a combination of self-paced preview videos and live online instruction), participants will be guided through step-by-step instructions for using and progressing through vaginal trainers and other treatments (the same step-by-step instructions you can use with your patients on Monday morning!). Additionally, as in other areas of the body, focusing on the body part that is being worked on is beneficial for increasing motor control, which is also desirable for addressing pelvic floor muscles that have too much tone and tenderness or pain with attempts at insertion. Participants will also be walked through activities that increase the brain's connection with and control of the pelvic floor and genitals, thus tapping into contemporary pain science concepts as well. And speaking of pain science . . .
2. As a practitioner, you likely already know that our words, verbiage for questions and instruction, and analogies and stories matter! Throughout the course, we will talk about why some words or terms can be harmful or less helpful, and how to replace them with healing or more neutral terms. For instance, we will talk about how the traditional term "dilator" can be a bit scary and anxiety-provoking for someone who has had lifelong vaginismus; but the term "trainer" suggests that the muscles are being taught and retrained on how to function. We will also walk through examples of approaching and discussing sexual abuse and trauma, general sexual history and activity, and patient goals. We will review some basics about contemporary pain science, and analogies that we can share with our patients to help decrease their fear and anxiety surrounding treatment for and engaging in sexual function. Participants should leave the course feeling more confident in talking about sex with their patients!
3. How do we incorporate the female sexual cycle/response (arousal, desire, orgasm), sexual positioning, and sexual assist devices and props into helping our patients? These are topics that will be tackled and broken down in both the preview material, with key concepts being reviewed or covered during the live remote portion of the course. We will talk about using the timing of sexual responses to a patient's advantage with transitioning to sexual function.
4. When should a patient move from vaginal trainers to the bedroom? Should the patient's partner(s) be involved? How do I answer questions about specific sexual positions? How do I answer my patient's questions about libido concerns? These are all concepts that will be tackled, with both specific examples and cases and also with general guidelines for applying the information to your individual patients.
5. You will have the opportunity to practice or follow along with the very things you will teach your patients during the live remote lab portion of the course, from the privacy of your own home or private treatment room in your office. I believe a great advantage that rehabilitation professionals have in treating patients is that we have experienced many of the examination and treatment techniques while practicing them in a class, course, or another setting. Personally testing out these techniques gives you, as a practitioner, a strong advantage in knowing how to best describe the nuances of applying treatments to aid in your patient's understanding. It also gives you a good dose of empathy for being the person on the table!
What special interest do you have in this topic?
As a pelvic health therapist for over 20 years, working with patients who have lifelong vaginismus, acquired vaginismus, and dyspareunia has been one of my primary passions. In completing a Ph.D. in 2020, my line of research began with a clinical randomized controlled trial working with patients with lifelong vaginismus and vaginal trainers, using neuroscience and pain science concepts to incorporate contract-relax and breathing techniques to enhance treatment. I never tire of having a patient return to the clinic excited that they finally had pain-free intercourse! I am passionate about teaching other therapists, healthcare providers, patients, and their partners about the concepts I've learned in my many years of practice.
Who is the audience for this class?
This course is for any pelvic health rehabilitation or health care provider who is a novice or wants to enhance their skills for working with patients with vaginismus and vulvovaginal dyspareunia.
Why was it needed and developed?
This course, Vaginismus and Vulvovaginal Dyspareunia, is needed to move beyond the basic concepts about what we can do to help patients having pain with intercourse. This course takes a deep dive into the detail of how to make the rubber meet the road to not only get treatment started but to really help progress a patient into a satisfying sex life. This course was developed so that the participant could leave this course and understand how to really approach the examination, history taking, and step-by-step procedures in instructing and using vaginal trainers and other tools for patients having painful intercourse. Additionally, this course should increase the practitioner's confidence in incorporating instructions and education related to a patient's concerns about the female sexual cycle and response (arousal, desire, orgasm), sexual positioning, lubrication, and partner integration.
Vaginismus and Vulvovaginal Dyspareunia
Course Date:
February 4
Price: $375
Experience Level: Beginner
Contact Hours: 15
Description: This course is for the pelvic health practitioner who is new to treating patients with vaginismus/vulvovaginal dyspareunia or to vaginal trainer(dilator) use or pelvic health rehabilitation; or for the experienced practitioner who has found that patients with vaginismus/vulvovaginal dyspareunia plateau with vaginal trainers or other treatments. In this course, pelvic health rehabilitation providers will learn about the different types of vaginismus and dyspareunia. Definitions and history of terminology will be explained related to pain with sexual activity and intercourse, including Genito-Pelvic Pain/Penetration Disorder, Lifelong or Primary Vaginismus, Acquired or Secondary Vaginismus, Dyspareunia, Vulvodynia, and others.
From a pain-science viewpoint, verbiage and terminology to reduce patient fear and anxiety will be discussed and incorporated throughout the course. Evidence for focalized dystonia as a component of lifelong vaginismus and how that impacts treatment will be reviewed. Causes for acquired vaginismus (such as postpartum healing or hormonal changes) will be addressed. Treatment approaches for reducing patient fear and anxiety, addressing medical and/or sexual trauma/abuse history, and promoting patient empowerment will be covered. The remote live portion of the course will also focus on rehabilitation treatments, including walking the participant through the functional use of vaginal trainers (commonly known as dilators), and methods for progressing their use. Clinical cases will be provided to illustrate a variety of treatment approaches based on different patients’ treatment goals, history, examination findings, and sexual pain diagnosis.
I recently assisted at a Pelvic Floor Level 2B course which has been updated with recent research, new sections, and less repetition from Pelvic Floor Level 1. In the course they mentioned this article which sparked a lively discussion and I had to learn more. It is rare to see a study with a large number of participants in pelvic health and especially with a vaginismus diagnosis.
Vaginismus is defined as a genito-pelvic pain/penetration disorder along with dyspareunia under the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders; Fifth Edition) in which penetration is often impossible due to pain and fear. Vaginismus is both a physical and psychological disorder as it exhibits both muscle spasms and fear/anxiety of penetration. Symptoms vary by severity. Common presentation is an inability or discomfort to insert/remove a tampon, pain with penetration, and complaints of “hitting a wall” in attempted penetration; and inability to participate in gynecological exams.
 The authors of this study evaluated the severity of vaginismus. The penetrative history was used in addition to presentation at pelvic exam, and then given a level. There are 2 grading systems, Lamont and Pacik, that indicate the level of fear and anxiety about being touched. They found that those with severe vaginismus were Lamont levels 3 and 4, and Pacik level 5. For example, a Pacik Level 5 includes Lamont grade 4 “generalized retreat: buttocks lift up; thighs close, patient retreats” plus a visceral reaction such as “palpitations, hyperventilation, sweating, severe trembling, uncontrollable shaking, screaming, hysteria, wanting to jump off the table, a feeling of going unconscious, nausea, vomiting and even a desire to attack the doctor”.
The authors of this study evaluated the severity of vaginismus. The penetrative history was used in addition to presentation at pelvic exam, and then given a level. There are 2 grading systems, Lamont and Pacik, that indicate the level of fear and anxiety about being touched. They found that those with severe vaginismus were Lamont levels 3 and 4, and Pacik level 5. For example, a Pacik Level 5 includes Lamont grade 4 “generalized retreat: buttocks lift up; thighs close, patient retreats” plus a visceral reaction such as “palpitations, hyperventilation, sweating, severe trembling, uncontrollable shaking, screaming, hysteria, wanting to jump off the table, a feeling of going unconscious, nausea, vomiting and even a desire to attack the doctor”.
241 patients participated in this study, with a mean duration of 7.8 years. 70% of participants were a Lamont level 4 or Pacik level 5 at baseline. The authors looked at previous treatments tried and coping strategies; 74% had tried lube, 73% had tried dilators, 50% had tried Kegels, 28% had tried physical therapy, 3% had tried a surgical vestibulectomy. The full table 2 is in the article. Most participants had a mean of at least 4 failed treatments.
The aim was to help these women to achieve pain free intercourse after treatment. In order to tolerate the treatment, many were sedated with midazolam before the Q-tip test, and more sedation given as needed. The treatment lasted for about 30 minutes and consisted of:
- Q-tip test with as minimal sedation as possible to rule out vulvodynia and provoked vestibulodynia
- Digital exam of tolerance in order to assess the level of spasm in introitus. Graded 0 (no spasm) to 4 (severe spasm where digital insertion was difficult)
- Botox 50 U injections to right and left submucosal space near the bulbospongiosus muscle administered with a pediatric speculum placed. Additional Botox was injected submucosally into levator ani muscles if also in spasm/tight
- Injections 0.25% bupivacaine (a numbing agent) 1 mL increments along right and left lateral vaginal walls (9 mL per side) from cervix to introitus
- Progressive dilation; circumference 3 inches (#4), 4 inches (#5), 5 inches (#6)
- Reassessed with digital examination
- Re-insert #5 or #6 dilator and patient was awakened and taken to recovery
If the patient consented, her partner could be present during the procedure and was allowed to palpate the level of spasm with gloved digit and was educated on dilator insertion. The authors noted that many partners had a ‘profound’ experience.
A nurse worked with the couple for about two hours in the recovery room to help them be more comfortable moving the dilator in and out with minimal-to-no pain as the numbing agent lasts 6-8 hours. Three participants were treated each time and consented to meet each other. Patients were discharged with #4 dilator in place and asked to keep in until the next day. They were given Ibuprofen and sleeping aids as needed.
Day 1
Participants return with partners and progress up to larger sizes (#5 and #6). They participate in group counseling with the primary researcher Dr. Pacik. This lasted about 5 hours; and consisted of education of dilator progression, returning to intercourse and lubricants. If participants wished to have private counseling instead that was granted. Many exchanged contact information. They were encouraged to continue seeing their healthcare clinicians as indicated; sex therapists, physical therapists, psychologists.
Dilator Progression
Month 1
- 2 hours of dilator per day. Either in 1 sitting or 1 hour of dilator work x2 per day
- Progress to bigger sizes until #5 or #6 is comfortable
Month 2
- 1 hour of dilator use per day and continue toward larger sizes
Month 3
- 15-30 minutes of dilator use per day
Months 4-12
- 10-15 minutes of dilator use per day or every other day
During the counseling session post-procedure, the recommendations for returning to intercourse included:
- Delaying intercourse until #5 dilator was able to be easily inserted
- It is helpful to do 1 hour of dilator work before attempting intercourse for the first time
- If partner’s penis is larger progress to larger dilators (#7 - 6 inch circumference or #8 7 inch circumference)
- Goal of the first few attempts is to insert tip of dilator only
- Once tip can be inserted easily then progress to full penetration; restrain from thrusting
- Try “spooning position” if ‘leg lock’ occurs
- Try different positions with dilator work and intercourse to see what works best
71% of participants achieved pain-free coitus 5 weeks after the procedure. 2.5% could not achieve coitus within one-year period although they could use #5 or #6 dilators. The participants were given a validated outcome tool, the Female Sexual Function Index (FSFI), before and after the procedure and at 1-month, 3-months, 6-months, and 1-year; with significant improvement at each interval. The patients were followed for one year, and often remained in contact with the authors for much longer ranging from 16-months to 9-years.
The authors propose that use of dilators at the time of botox and post procedure counseling and support help participants ‘break through’, whereas previous treatment may not be as multidimensional and limit efficacy. Botox lasts 2-4 months and allowed for dilation progression.
Initially after reading this article the treatment seemed a little drastic to me, but then I considered the women with this level of vaginismus are often not coming into my clinic. They may need this level of structure, consistently, and multidimensional treatment as half measures have failed them. I am so glad they were persistent and found the help they needed.
Pacik, P., Geletta, S. Vaginismus Treatment: Clinical Trials Follow Up 241 Patients. Sex Med 2017;5:e114-e123
In this post, we want to give a high-level overview of interstitial cystitis and an introduction to other resources if you’d like to dive deeper into treatment the condition. There’s a printable, patient-friendly version of this overview if you’d like to use it in describing the condition with patients. In addition, you may want to review the 8 Myths of Interstitial Cystitis series and the AUA Guidelines for Interstitial Cystitis.
Definition
Interstitial cystitis is defined as pain or pressure perceived to be related to the urinary bladder, associated with lower urinary tract symptoms of more than six weeks duration, in the absence of infection or other identifiable causes.
Unfortunately, for physicians, pelvic floor dysfunction falls under category of ‘unidentifiable cause.’ Interstitial cystitis is really more of a description of symptoms, rather than a discrete diagnosis, and the condition presents in many different ways.

Symptoms
The hallmarks of interstitial cystitis are pelvic pain, often in the suprapubic area or inner thighs, and urinary urgency and frequency. Other common symptoms include pain with intercourse, nocturia, low back pain, constipation, and urinary retention.
Many patients are surprised to realize that symptoms like painful intercourse, low back pain, and constipation are related to their IC diagnosis. This challenges the misconception that issues are arising solely from the bladder, and is a good way to help patients (and their physicians) understand that IC is about more than just the bladder.
Diagnosis
Interstitial cystitis is fundamentally a diagnosis of exclusion. Most patients suspect a urinary tract infection (UTI) when their symptoms first present. It’s actually common for symptoms to start as the result of a UTI, and simply not resolve once the infection has cleared. Patients are often treated with multiple rounds of antibiotics for these ‘phantom’ UTIs, where cultures have come back negative, before an IC diagnosis is considered.
It’s important for us as physical therapists to be able to share with patients that no testing is required to confirm an IC diagnosis, it can be diagnosed clinically. In practice, a urologist will likely want to conduct a cystoscopy, which can rule out more serious issues like bladder cancer as well as check for Hunner’s lesions (wounds in the bladder that are present in about 10% of IC patients). However, after that, no additional testing is needed. The potassium sensitivity test (PST) was formerly used by some urologists, but it has been shown to be useless diagnostically and extremely painful for patients and is not recommended by the American Urological Association. Urodynamic testing is also often conducted, but again is not necessary to establish an IC diagnosis.
Physical Therapy for IC
According to the American Urological Association, physical therapy is the most proven treatment for interstitial cystitis. It’s given an evidence grade of ‘A’ (the only treatment with that grade) and recommended in the first line of medical treatment.
In controlled clinical trials, manual physical therapy has been shown to benefit up to 85% of both men and women. These trials reported benefits after ten visits of one-hour treatment sessions.
In a study conducted at our clinic , PelvicSanity, we found that physical therapy was able to reduce pain for IC patients from an average of 7.6 (out of 10) before treatment to 2.6 following physical therapy. Similarly, how much their symptoms bothered patients fell from 8.3 to 2.8. More than half of patients reported improvements within the first three visits.
Unfortunately, many patients still aren’t referred to pelvic physical therapy by their physician. More than half of the patients in the study had seen more than 5 physicians before finding pelvic PT, and only 7% of patients felt they had been referred to physical therapy at the appropriate time by their doctor.
Multi-Disciplinary Approach
Patients with interstitial cystitis or pelvic pain always benefit from a multidisciplinary approach to treatment.This can include:
- Stress relief to downregulate the nervous system can decrease symptoms and reduce flares. Gentle exercise, meditation, yoga, deep breathing, or working with a psychologist can all provide benefits for patients.
- Diet and nutrition are important when working with IC patients. There is no formal ‘IC Diet’, but most patients are sensitive to at least a few trigger foods. The gold standard of treatment is an elimination diet, where the common culprits are completely removed from the diet and then added back in one at a time. This identifies which foods are triggers for patients. With nutrition for IC, patients should avoid their personal trigger foods and eat healthy – it doesn’t have to be any more restrictive or complicated.
- Alternative treatments like acupuncture have been shown to reduce pelvic pain in patients, and several supplements have shown benefits in trials or anecdotally among patients.
- Bladder treatments include instillations and nerve stimulation. Some patients may benefit from bladder instillations, but many others find that the process of the instillation actually causes additional symptoms. If instillations are beneficial, patients should be encouraged to address the underlying issues during the reprieve that instillations bring. Percutaneous tibial nerve stimulation or an implanted nerve stimulation device can both be possible treatment options.
- Oral medications can also reduce symptoms, but do not address the underlying cause of symptoms in patients. Medication that dampens the nervous system, often an anti-depressant or similar medication, can reduce pain and hypersensitivity. Anti-inflammatories may be beneficial in lowering inflammation and helping break the cycle of dysfunction-inflammation-pain. Most patients are started on Elmiron®, the only FDA-approved medication for IC; unfortunately, in the most recent clinical trial research Elmiron has been shown to be no more effective than a placebo. If it is effective, it only is beneficial for about one-third of patients, and many won’t be compliant with the drug due to cost and side effects.
 Nicole Cozean, PT, DPT, WCS (www.pelvicsanity.com/about-nicole) is the founder of PelvicSanity physical therapy in Southern California. Name the 2017 PT of the Year by the ICN, she’s the first physical therapist to serve on the Interstitial Cystitis Association’s Board of Directors and the author of the award-winning book The IC Solution (www.pelvicsanity.com/the-ic-solution). She teaches at her alma mater, Chapman University, as well as continuing education through Herman & Wallace. Nicole also founded the Pelvic PT Huddle (www.facebook.com/groups/pelvicpthuddle), an online Facebook group for pelvic PTs to collaborate.
Nicole Cozean, PT, DPT, WCS (www.pelvicsanity.com/about-nicole) is the founder of PelvicSanity physical therapy in Southern California. Name the 2017 PT of the Year by the ICN, she’s the first physical therapist to serve on the Interstitial Cystitis Association’s Board of Directors and the author of the award-winning book The IC Solution (www.pelvicsanity.com/the-ic-solution). She teaches at her alma mater, Chapman University, as well as continuing education through Herman & Wallace. Nicole also founded the Pelvic PT Huddle (www.facebook.com/groups/pelvicpthuddle), an online Facebook group for pelvic PTs to collaborate.
Interstitial Cystitis Course
In our upcoming course for physical therapists in treating interstitial cystitis (April 6-7, 2019 in Princeton, New Jersey), we’ll focus on the most important physical therapy techniques for IC, home stretching and self-care programs, and information to guide patients in creating a holistic treatment plan. The course will delve into how to handle complex IC presentations. It’s a deep dive into the condition, focusing not just on manual treatment techniques but also how to successfully manage an IC patient from beginning to resolution of symptoms.
Additional Resources
- Interstitial Cystitis Overview (printable)
- The Interstitial Cystitis Solution
- Patient groups include the Interstitial Cystitis Association (ICA) (www.ic-help.org) and the IC Network (www.ic-network.com), which both have fantastic resources for patients.
- The AUA Guidelines for IC
- IC Flare-Busting Plan
Myofascial release (MFR) can be one of your greatest treatment tools as a pelvic rehabilitation practitioner. Just in case you don’t think about fascia often here are a couple helpful things to remember. Fascia is the irregular connective tissue that covers the entire body, and it is the largest sensory system in the body, making it highly innervated. The mobilizing effect of MFR techniques occurs by stimulating various mechanoreceptors within the fascia (not by the actual force applied). MFR techniques can help to reduce tissue tension, relax hypertonic muscles, decrease pain, reduce localized edema, and improve circulation just to name a few physiological effects.
 An interesting case report published in 2015 by the Journal of Women’s Health Physical Therapy1 offers a wonderful example of how a physical therapist used specific MFR techniques for a patient with clitoral phimosis and dyspareunia. The specific MFR techniques used helped to provide relief and restore mobility to the pelvic tissues for this patient.
An interesting case report published in 2015 by the Journal of Women’s Health Physical Therapy1 offers a wonderful example of how a physical therapist used specific MFR techniques for a patient with clitoral phimosis and dyspareunia. The specific MFR techniques used helped to provide relief and restore mobility to the pelvic tissues for this patient.
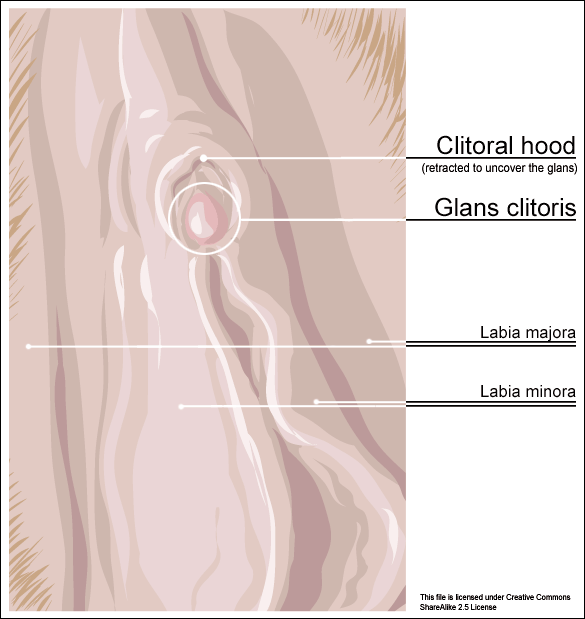
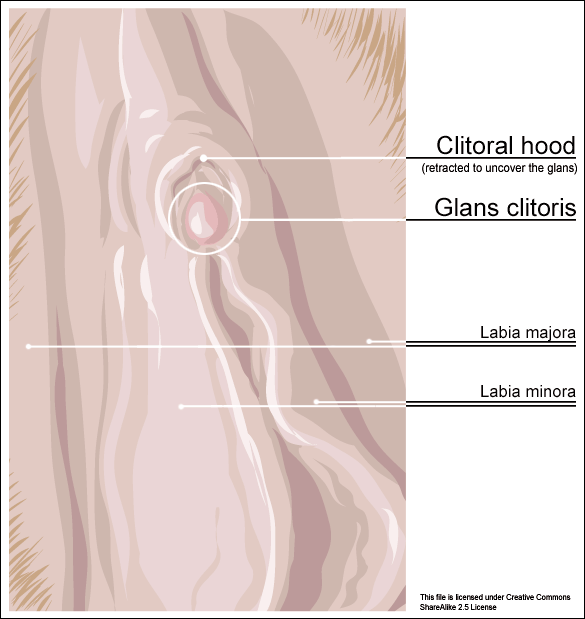
Clitoral phimosis is adherence between the clitoral prepuce (also known as the clitoral hood) and the glans. This condition can be the result of blunt trauma, chronic infection, inflammatory dermatoses, and poor hygiene. In this case report, the 41-year-old female patient had sustained a blunt trauma injury to the vulva (when her toddler son charged, contacting his head forcibly into her pubic region). She presented to physical therapy with complaints of dyspareunia, low back pain, a bruised sensation of her pubic region, vulvar pain provoked by sexual arousal, decreased clitoral sensitivity, and anorgasmia. The physical therapist completed an orthopedic assessment for the lower quarter (including spine and extremities), as well as a thorough pelvic floor muscle assessment.
Treatment for this patient addressed not only the pelvic complaints, but the lower quarter complaints as well. A detailed treatment summary for each visit is outlined in the case report. The clitoral MFR and stretching was performed by applying a small amount of topical lubricant to the clitoral prepuce. Then, a gloved finger or a cotton swab was used to stabilize the clitoris, a prolonged MFR or sustained stretch was applied in the direction away from the fixated clitoris by the therapist’s other finger. The therapist applied this technique along the entire length of the prepuce. The other physical therapy interventions this patient was treated with were stretching, joint mobilization, muscle energy techniques, transvaginal pelvic floor muscle massage, clitoral prepuce MFR techniques, biofeedback, Integrative Manual Therapy (IMT) techniques, nerve mobilization, and therapeutic and motor control exercises. Additionally, between the physical therapy evaluation and the second visit the patient did use topical Clobetasol 0.05% cream (commonly prescribed for vulvar dermatitis issues such as Lichen Sclerosis) for 30 days with no change to her clitoral phimosis.
After 11 sessions, the patient had resolution of dyspareunia, vulvar pain, pubic pain, and reduced low back pain. Also, the patient had 100% restored mobility of the clitoral prepuce, as well as normalized clitoral sensitivity and clitoral orgasm. The patient felt these improvements were still present at her 6-month follow-up interview over the phone. Current medical management for clitoral phimosis is surgical release or topical/injectable corticosteroids. Having a conservative treatment option, such as MFR, for this condition can be helpful for patients. As with most evolving treatment techniques, more research and studies are appropriate.
Not one health care professional had ever assessed the fascial mobility of the clitoris until this physical therapist did. This case report is an example of how MFR techniques can be effective treatment tools for your patients with pelvic disorders and a good reminder to check the fascial mobility of the pelvic tissues.
Morrison, P., Spadt, S. K., & Goldstein, A. (2015). The Use of Specific Myofascial Release Techniques by a Physical Therapist to Treat Clitoral Phimosis and Dyspareunia. Journal of Women’s Health Physical Therapy, 39(1), 17-28.
My job as a pelvic floor therapist is rewarding and challenging in so many ways. I have to say that one of my favorite "job duties" is differential diagnosis. Some days I feel like a detective, hunting down and piecing together important clues that join like the pieces of a puzzle and reveal the mystery of the root of a particular patient's problem. When I can accurately pinpoint the cause of someone's pain, then I can both offer hope and plan a road to healing.
 Recently a lovely young woman came into my office with the diagnosis of dyspareunia. As you may know dyspareunia means painful penetration and is somewhat akin to getting a script that says "lower back pain." As a therapist you still have to use your skills to determine the cause of the pain and develop an appropriate treatment plan.
Recently a lovely young woman came into my office with the diagnosis of dyspareunia. As you may know dyspareunia means painful penetration and is somewhat akin to getting a script that says "lower back pain." As a therapist you still have to use your skills to determine the cause of the pain and develop an appropriate treatment plan.
My patient relayed that she was 6 months post partum with her first child. She was nursing. Her labor and delivery were unremarkable but she tore a bit during the delivery. She had tried to have intercourse with her husband a few times. It was painful and she thought she needed more time to heal but the pain was not changing. She was a 0 on the Marinoff scare. She was convinced that her scar was restricted. "Oh Goodie," I thought. "I love working with scars!" But I said to her, "Well, we will certainly check your scar mobility but we will also look at the nerves and muscles and skin in that area and test each as a potential pain source, while also completing a musculoskeletal assessment of the rest of you."
Her "external" exam was unremarkable except for adductor and abdominal muscle overactivity. Her internal exam actually revealed excellent scar healing and mobility. There was significant erythemia around the vestibule and a cotton swab test was positive for pain in several areas. There was also significant muscle overactivity in the bulbospongiosis, urethrovaginal sphincter and pubococcygeus muscles. Also her vaginal pH was a 7 (it should normally be a 4, this could indicate low vaginal estrogen). I gave her the diagnosis of provoked vestibulodynia with vaginismus. Her scar was not the problem after all.
Initially for homework she removed all vulvar irritants, talked to her doctor about trying a small amount of vaginal estrogen cream, and worked on awareness of her tendency to clench her abdominal, adductor, and pelvic floor muscles followed by focused relaxation and deep breathing. In the clinic I performed biofeedback for down training, manual therapy to the involved muscles, and instructed her in a dilator program for home. This particular patient did beautifully and her symptoms resolved quite quickly. She sent me a very satisfied email from a weekend holiday with her husband and daughter.
Although this case was fairly straightforward, it is a great example of how differential diagnosis is imperative to deciding and implementing an effective treatment plan for our patients. In Herman & Wallace courses you will gain confidence in your evaluation skills and learn evidence based treatment processes that will enable you to be more confident in your care of both straightforward and complex pelvic pain cases. Hope to see you in class!
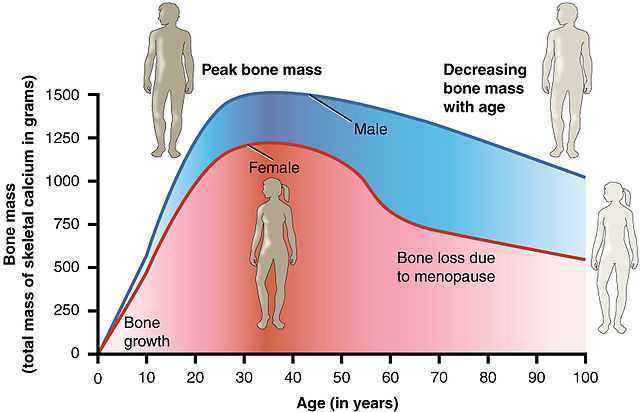
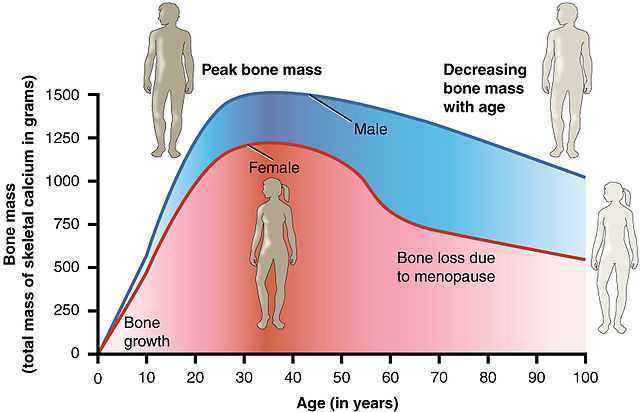
After menopause, more than half of women may have vulvovaginal symptoms that can impact their lifestyle, emotional well-being and sexual health. What's more, the symptoms tend to co-exist with issues such as prolapse, urinary and/or bowel problems. But unfortunately many women aren't getting the help they need, despite a growing body of evidence that skilled pelvic rehab interventions are effective in the management of bladder/bowel dysfunctions, POP, sexual health issues and pelvic pain.
 Vaginal dryness, hot flashes, night sweats, disrupted sleep, and weight gain have been listed as the top five symptoms experienced by postmenopausal women in North America and Europe, according to a study by Minkin et al 2015, and they also concluded ‘The impact of postmenopausal symptoms on relationships is greater in women from countries where symptoms are more prevalent.’
Vaginal dryness, hot flashes, night sweats, disrupted sleep, and weight gain have been listed as the top five symptoms experienced by postmenopausal women in North America and Europe, according to a study by Minkin et al 2015, and they also concluded ‘The impact of postmenopausal symptoms on relationships is greater in women from countries where symptoms are more prevalent.’
Between 17% and 45% of postmenopausal women say they find sex painful, a condition referred to medically as dyspareunia. Vaginal thinning and dryness are the most common cause of dyspareunia in women over age 50. However pain during sex can also result from vulvodynia (chronic pain in the vulva, or external genitals) and a number of other causes not specifically associated with menopause or aging, particularly orthopaedic dysfunction, which the pelvic physical therapist is in an ideal position to screen for.
According to the North America Menopause Society, ‘…beyond the immediate effects of the pain itself, pain during sex (or simply fear or anticipation of pain during sex) can trigger performance anxiety or future arousal problems in some women. Worry over whether pain will come back can diminish lubrication or cause involuntary—and painful—tightening of the vaginal muscles, called vaginismus. The result can be a vicious circle, again highlighting how intertwined sexual problems can become.’
The research has demonstrated that the optimal strategy for post-menopausal stress incontinence is a combination of local hormonal treatment and pelvic floor muscle training – the strategy of combining the two approaches has been shown to be superior to either approach used individually (Castellani et al 2015, Capobianco et al 2012) and similar conclusions can be drawn for promoting sexual health peri- and post-menopausally.
The pelvic rehab specialist may be called upon to screen for orthopaedic dysfunction in the spine, hips or pelvis, to discuss sexual ergonomics such as positioning or the use of lubricant as well as providing information and education about sexual health before, during and after menopause.
To learn more about sexual health and pelvic floor function/dysfunction at menopause, join me in Atlanta in March for Menopause: A Rehab Approach!
Prevalence of postmenopausal symptoms in North America and Europe, Minkin, Mary Jane MD, NCMP1; Reiter, Suzanne RNC, NP, MM, MSN2; Maamari, Ricardo MD, NCMP3, Menopause:November 2015 - Volume 22 - Issue 11 - p 1231–1238
Low-Dose Intravaginal Estriol and Pelvic Floor Rehabilitation in Post-Menopausal Stress Urinary Incontinence, Castellani D. · Saldutto P. · Galica V. · Pace G. · Biferi D. · Paradiso Galatioto G. · Vicentini C., Urol Int 2015;95:417-421
After menopause, more than half of women may have vulvovaginal symptoms that can impact their lifestyle, emotional well being and sexual health. What's more, the symptoms tend to co-exist with issues such as prolapse, urinary and/or bowel problems. But unfortunately many women aren't getting the help they need, despite a growing body of evidence that skilled pelvic rehab interventions are effective in the management of bladder/bowel dysfunctions, POP, sexual health issues and pelvic pain.
 Vaginal dryness, hot flashes, night sweats, disrupted sleep, and weight gain have been listed as the top five symptoms experienced by postmenopausal women in North America and Europe, according to a study by Minkin et al 2015, and they also concluded ‘The impact of postmenopausal symptoms on relationships is greater in women from countries where symptoms are more prevalent.’ Between 17% and 45% of postmenopausal women say they find sex painful, a condition referred to medically as dyspareunia. Vaginal thinning and dryness are the most common cause of dyspareunia in women over age 50. However pain during sex can also result from vulvodynia (chronic pain in the vulva, or external genitals) and a number of other causes not specifically associated with menopause or aging, particularly orthopaedic dysfunction, which the pelvic physical therapist is in an ideal position to screen for.
Vaginal dryness, hot flashes, night sweats, disrupted sleep, and weight gain have been listed as the top five symptoms experienced by postmenopausal women in North America and Europe, according to a study by Minkin et al 2015, and they also concluded ‘The impact of postmenopausal symptoms on relationships is greater in women from countries where symptoms are more prevalent.’ Between 17% and 45% of postmenopausal women say they find sex painful, a condition referred to medically as dyspareunia. Vaginal thinning and dryness are the most common cause of dyspareunia in women over age 50. However pain during sex can also result from vulvodynia (chronic pain in the vulva, or external genitals) and a number of other causes not specifically associated with menopause or aging, particularly orthopaedic dysfunction, which the pelvic physical therapist is in an ideal position to screen for.
According to the North America Menopause Society, ‘…beyond the immediate effects of the pain itself, pain during sex (or simply fear or anticipation of pain during sex) can trigger performance anxiety or future arousal problems in some women. Worry over whether pain will come back can diminish lubrication or cause involuntary—and painful—tightening of the vaginal muscles, called vaginismus. The result can be a vicious circle, again highlighting how intertwined sexual problems can become.’
The research has demonstrated that the optimal strategy for post-menopausal stress incontinence is a combination of local hormonal treatment and pelvic floor muscle training – the strategy of combining the two approaches has been shown to be superior to either approach used individually (Castellani et al 2015, Capobianco et al 2012) and similar conclusions can be drawn for promoting sexual health peri- and post-menopausally.
The pelvic rehab specialist may be called upon to screen for orthopaedic dysfunction in the spine, hips or pelvis, to discuss sexual ergonomics such as positioning or the use of lubricant as well as providing information and education about sexual health before, during and after menopause.
To learn more about sexual health and pelvic floor function/dysfunction at menopause, join me in Atlanta in March for Menopause: A Rehab Approach.
Prevalence of postmenopausal symptoms in North America and Europe, Minkin, Mary Jane MD, NCMP1; Reiter, Suzanne RNC, NP, MM, MSN2; Maamari, Ricardo MD, NCMP3, Menopause:November 2015 - Volume 22 - Issue 11 - p 1231–1238
Low-Dose Intravaginal Estriol and Pelvic Floor Rehabilitation in Post-Menopausal Stress Urinary Incontinence, Castellani D. · Saldutto P. · Galica V. · Pace G. · Biferi D. · Paradiso Galatioto G. · Vicentini C., Urol Int 2015;95:417-421