Pamela A. Downey, PT, DPT, WCS, BCB-PMD, PRPC is Senior Faculty with Herman & Wallace and is instructing the upcoming Pudendal Neuralgia and Nerve Entrapment scheduled for January 27, 2024. She is the owner of Partnership in Therapy, a private practice in Coral Gables, Florida where she treats women and men with pelvic floor dysfunction, related urogynecological and colorectal issues, spine dysfunction, osteoporosis, and complaints associated with pregnancy and the postpartum period. Her mission is to educate and integrate healthy lifestyles for patients on the road to wellness. Pam sat down with the Pelvic Rehab to discuss her upcoming course.
What makes pudendal neuralgia such a difficult diagnosis to treat?
I think people often see the content in Pelvic Function Level 1 - Introduction to Pelvic Health and it's like a tidy little box. Then you get the patient and as the practitioner you're like I don't know what to do with this person. We need to show that pudendal skills are needed in differential diagnosis. Even though this course is called Pudendal Neuralgia and Nerve Entrapment, it is about differential diagnosis for a lot of pelvic pain. When you feel more secure in knowing what you're treating and have a systematic way of looking at it, then you can be more productive in your patient care.
I think some ortho therapists treat in a linear fashion, and they go from week one to week eight through a protocol and things generally go well because it's a predictable course when you're rehabbing a total knee replacement, or you have an elbow tendonitis, and you expect these structures to follow a path. But then when you come into the nerve side of things, nerves can be unpredictable. They're influenced by lots of factors. It could be your mood. It could be the range of motion around a joint. It could be a previous history of another neurologic problem feeding it, such as disc pathology. It can be something around a postural habit, and it could be a straight up other dysfunction that then affects the pudendal distribution. And if you don't treat the cause of the initial, you will never improve the latter, which is the neurological presentation in pudendal.
I love that it's more about figuring out the differential diagnosis for pelvic pain and going from that angle into pudendal dysfunction, entrapment, neuralgia, and everything that goes with that. For example, you're going to get a patient with an order for pudendal neuralgia, or even worse entrapment. When they get an order for pudendal neuralgia, then they'll kind of forget that the person may not have pudendal neuralgia. They have problems in the pudendal distribution, but that's basically everything we treat. So as a pelvic rehab practitioner they have to tease it out.
When I look at a script I always say, “that's nice.” The referring doctor may have written it as pudendal neuralgia so that the patient could get reimbursement for the therapy with the diagnosis code. But then we get to add our diagnosis codes on top of that and drive a treatment plan.
So, I think that is a big hangup. Practitioners run when they usually see this diagnosis. You don't want a pudendal patient. Especially if you do not have a lot of skills, because you are going to be like, well, what can I do for this patient? If they sit, they have pain. If they exercise, they have pain. They don't have like a whole repertoire. In the pudendal neuralgia course, we talk about how to figure out if the driver is the spine, the hip, the nerve itself, if it's the pelvic floor musculature, or if it's biomechanical. There are so many facets.
How often do these scripts come in for patients that have pudendal neuralgia?
In pelvic pain they're probably coming in a high percentage, like I would say three-quarters. In practice, depending on who's referring into the person's practice, it's going to be a significant amount of walk-in traffic and referred traffic. Because every levator syndrome patient could have a pudendal issue driving the levators, and long-standing levator pain can end up being pudendal.
It's kind of like are you treating the chicken or the egg? I think giving the person skills to do test and retest and having a way to keep falling back on to this and then to also be able to transmit the idea that this isn't a fix -it problem. You know, we just don't put a band aid on it and you're done. Other folks who are more newish, who expect this linear event, they're going to struggle because there's going to be setbacks and sometimes doing more is the exact opposite of what needs to be done. Less is more.
When you look at the H&W course catalog, where would you recommend that practitioners take the Pudendal Neuralgia course?
The sweet spot for taking the pudendal neuralgia course would be practitioners who have taken PF1 and Pelvic Function Level 2A - Colorectal Pelvic Health, Pudendal Neuralgia, and Coccyx Pain, because they learn the rectal canal and PF2A. Practitioners who focus specifically on treating the male pelvic patient would benefit from this course because it is a good thinking course for how to treat men. It could pair well with Pelvic Function Level 2C - Men’s Pelvic Health and Rehabilitation (formerly Male Pelvic Floor). In my practice I get a lot of men coming in because they look on the internet and decide that they got pudenda neuralgia.
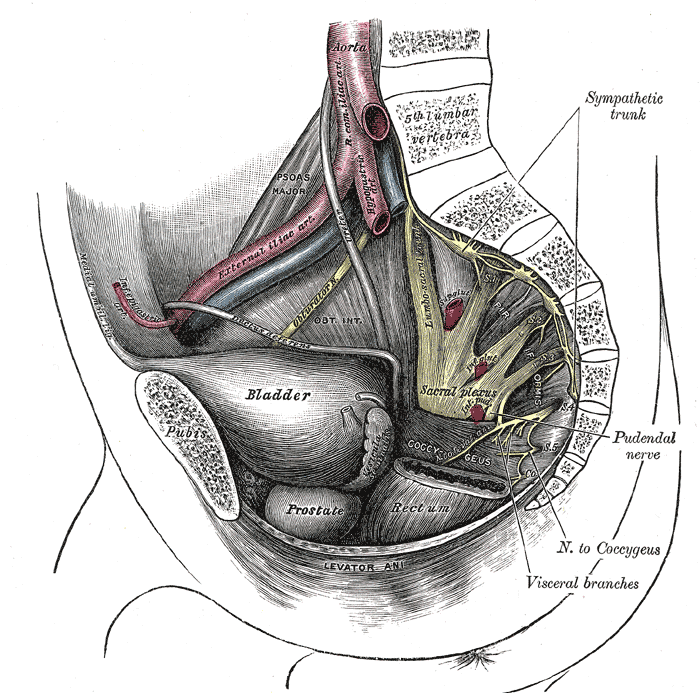
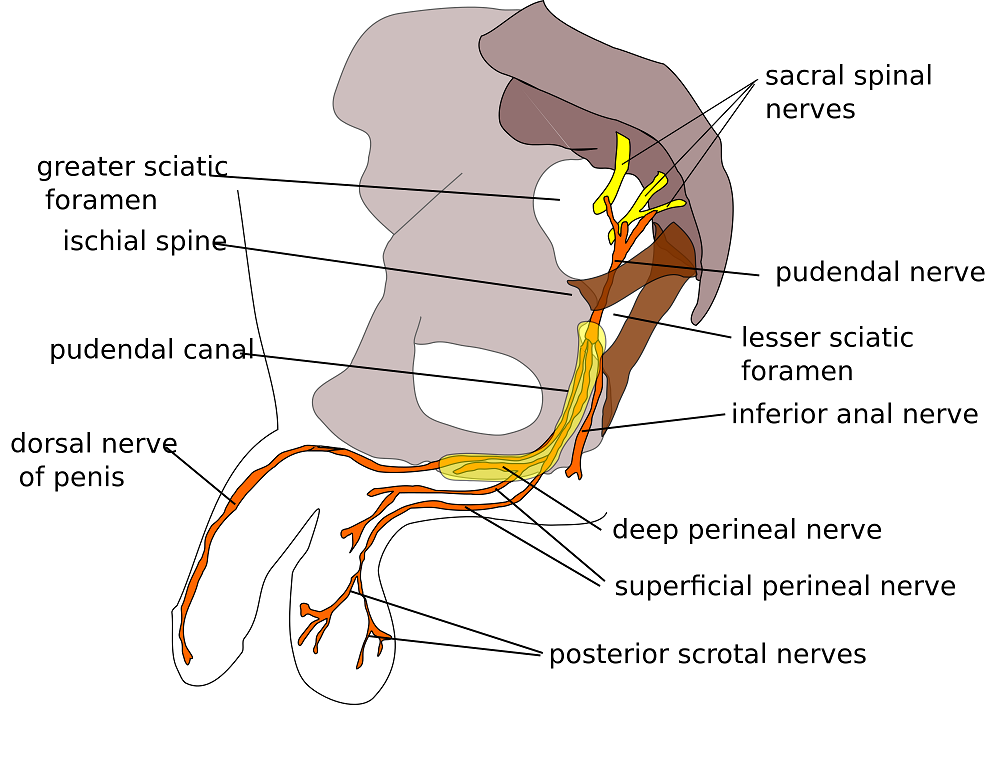
If you understand differential diagnosis you can touch on is this a sciatic nerve problem? Is this a genitofemoral problem? We look at the lumbo-sacral plexus in a decision tree, and then we then focus on pudendal and then how people manage them from a medical standpoint and from a therapy standpoint. I talk about using a rule-out method - this could be genital femoral, this could be pudendal nerve. And then you prove what the problem is by doing test and retest.
There's also a lot of pain neuroscience, so practitioners who have taken Pain Science for the Chronic Pelvic Pain Population would benefit from this course. The pudendal neuralgia course goes really well with this course because the practitioners who have taken the pain science course already know that there's going to be ups and downs. Also Nari Clemon’s nerve courses, Lumbar Nerve Manual Assessment and Treatment and Sacral Nerve Manual Assessment and Treatment, are definitely lab -oriented courses and this could be a backgrounder even going into her series, because she's going to talk about a lot of nerve techniques that can be then applied to the pudendal. Nari's courses give solid hands-on skills to deal with nerves, palpation, and finding them. Then this course shows you how to treat them. Not necessarily Pudendal, but all the nerve things. These courses enhance each other. It's like a decision tree where pudendal is on there and you can pass through it and go into Nari’s stuff where you can get a good idea and then use your myofascial, your orthopedic, your neuro skills.
Dr. Michael Hibner is an international expert on pudendal neuralgia and chronic pelvic pain. Dr. Hibner joins Holly Tanner to discuss his new exclusive course with H&W titled Pudendal Dysfunction: The Physician's Perspective.
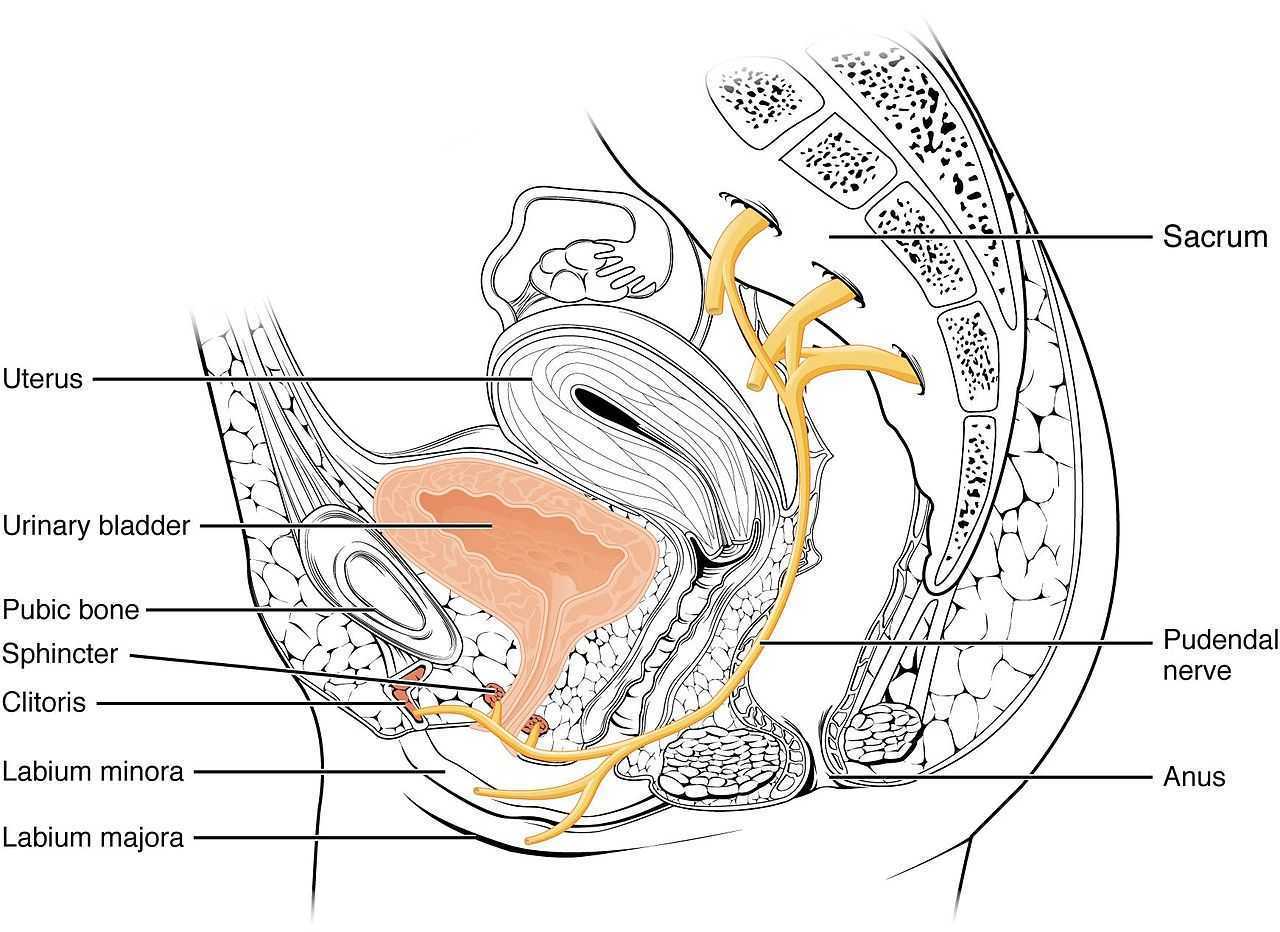
Pudendal neuralgia is a painful, neuropathic condition involving the dermatome of the pudendal nerve. This condition is not widely known and often goes unrecognized by many practitioners. Dr. Hibner runs The Arizona Center for Chronic Pelvic Pain (AZCCPP), a comprehensive center for treating chronic pelvic pain, and places a heavy emphasis on working as part of a care team with physical therapists and other pelvic rehab providers.
In this interview Dr. Hibner discusses how he treats pudendal neuralgia, “I treat patients with all reasons for pelvic pain but mostly pudendal neuralgia or patients with mesh injury or had an injury caused by pelvic mesh… I work very closely with physical therapists and I am a great, great believer in physical therapy. I am very happy that you are allowing me to share my perspective on Pudendal Neuralgia, and my perspective on physicians working with physical therapists.”
If I had pudendal neuralgia and I had a choice between surgery, injections, physical therapy, or medication. I would for sure have chosen physical therapy every time…there is no doubt in my mind. You can’t treat the PN without addressing the pelvic floor. What I tell patients is this. The number one thing for repetitive injury is to stop what you’re doing. The number two thing is to choose physical therapy over anything else. By far the majority of patients are helped by appropriate pelvic floor physical therapy.
Pudendal Dysfunction: The Physician's Perspective is scheduled for January 9, 2022. Course topics include pathoanatomy and clinical presentations, basics of surgical techniques, and terminology. The latter half of the course focuses on the physician and the rehab therapist working together and features case studies and clinical pearls from Dr. Hibner, a pioneer, and leader in the field.
Herman & Wallace is excited to announce a collaboration with Dr. Michael Hibner, an international expert on pudendal neuralgia and chronic pelvic pain. Dr. Hibner is presenting a new remote course on January 9, 2022, titled Pudendal Dysfunction: The Physician's Perspective. Pudendal neuralgia is a painful, neuropathic condition involving the dermatome of the pudendal nerve. This condition is not widely known and often goes unrecognized by many practitioners. Dr. Hibner runs the Arizona Center for Chronic Pelvic Pain (AZCCPP), a comprehensive center for treating chronic pelvic pain, and places a heavy emphasis on working as part of a care team with physical therapists and other pelvic rehab providers.
In a recent publication by Dr. Hibner, he shares that “the International Pudendal Neuropathy Association estimates the incidence of this condition to be 1/100,000; however, most practitioners treating patients with this condition feel the actual rate of incidence may be significantly higher.” Many patients go an average of 10-15 years attempting to get a diagnosis for their pain. Diagnosis of this condition is heavily based on the utilization of Nantes Criteria in conjunction with clinical history and physical findings.
Dr. Hibner began his career as a urogynecologist. In the early 2000s, some of his patients presented with a vulvar burning pain that didn’t fit any known criteria. When he reviewed the histories of these patients, he found that the only thing in common between these patients was kickboxing. Further research then led him to pudendal neuralgia.
What are some of the typical patient characteristics/presentations and the time of diagnosis and referral?
If you think of chronic pelvic pain, it really spans multiple specialties. It spans urology, colorectal, gastrointestinal, and physiatry. A lot of it is musculoskeletal pain, so a lot of it is physical therapy, orthopedics, and neurosurgical. However, for pudendal neuralgia patients, there are three distinct groups of patients. The younger group, 20-year-olds, are mostly injured in some type of athletic activity (skiers, gymnasts, cyclists, workout, etc.). The second group is slightly older, approximately mid-30s. Their most common cause of PN is traumatic vaginal childbirth. The older group often has had a mesh procedure (such as for prolapse) with the older kind of meshes.
What is your standard approach to PN patient complaints?
My protocol is that every patient that comes in gets a pelvic MRI before being seen (while doing Kegels and Valsalva). Even if seeing a physical therapist, I would have them see one associated with my practice so that the PT could take part in the patient meeting. I have my fellow take the patient history. Then we meet in my office, myself, the physical therapist, and my fellow, with MRI results, before seeing the patient. Then I meet the patient and can offer options.
How do I diagnose and treat PN?
I used to believe that the Nantes Criteria is what you had to use when diagnosing pudendal neuralgia. I recently retranslated the criteria for a textbook that is coming out soon. Patients should meet some of these criteria but don’t need to meet all of them. It just means that your pain is in the area of the pudendal nerve, but it doesn’t tell you that the nerve is entrapped. More pain with sitting is an important criterion. Having no pain at night is not true all the time, as it depends on the origin. However, this is not true with mesh origination PN.
The second part of it is the MRI. I have had very high hopes for the MRI in relation to diagnosing PN. This is not the answer for all of it. It is important, but the resolution of the PN is smaller than the MRI so that you can see the vascularization. A lot of times, you find other things than the compression of the nerve. It is a very good test to make sure that there is nothing else you are missing.
When talking about the MRI, what other diagnostic tests are helpful?
The warm threshold test, PN modern terminal latency test (you need to know the length of the nerve so it is not effective as that cannot be determined). The Pinprick test - not useful or accurate. What works best by far is the patient history, just talking to the patient. The [patient's] history is the key. What happened? The nerve can’t become entrapped on its own. If you see enough patients over the years, you can learn through experience. The MRI is valuable to make sure there is nothing else.
A pelvic exam by a qualified pelvic rehab therapist is important because it helps to rule out pelvic muscle spasms. The pain from the PN and the Obturator Levator muscle may be very similar and difficult to differentiate. Does the amount of spasms correlate with the number of symptoms/pain that they have?
You can’t treat the PN without addressing the pelvic floor. What I tell patients is this. The number one thing for repetitive injury is to stop what you’re doing. The number two thing is to choose physical therapy over anything else. By far the majority of patients are helped by appropriate pelvic floor physical therapy.
Pudendal Dysfunction: The Physician's Perspective is scheduled for January 9, 2022. Course topics include pathoanatomy and clinical presentations, basics of surgical techniques, and terminology. The latter half of the course focuses on the physician and the rehab therapist working together and features case studies and clinical pearls from Dr. Hibner, a pioneer, and leader in the field.
The interview excerpts are taken from Dr. Hibner's interview with Holly Tanner and Jessica Reale for the H&W Pelvic Floor Level 2A course pre-recorded lectures.
My 6 year old girl (going on 13) asks “Alexa” to play the Descendants II soundtrack over and over again. So the song, “Space Between,” was lingering in my head while reading the most recent articles on pudendal neuralgia, particularly when pudendal entrapment is to blame. After all, entrapment, by medical standards, describes a peripheral nerve basically being caught in between two surrounding anatomical structures.
 Ploteau et al., (2016) presented 2 case studies highlighting the warning signs when pudendal nerve entrapment does not follow the Nantes criteria. A brief summary of those 5 criteria follows:
Ploteau et al., (2016) presented 2 case studies highlighting the warning signs when pudendal nerve entrapment does not follow the Nantes criteria. A brief summary of those 5 criteria follows:
- Pain in the region of the pudendal nerve innervation from anus to penis or clitoris.
- Pain most predominant while sitting.
- The patient does not wake at night from the pain.
- No sensory impairment can be objectively identified.
- Diagnostic pudendal nerve block relieves the pain.
The case studies of a 31 and a 68 year old female revealed endometrial stromal sarcoma and adenoid cystic carcinoma in the ischiorectal fossa, with night pain was noted in both patients, as well as no pain with sitting or defecation, respectively. Clinicians must always be mindful to resolve red flags in patients.
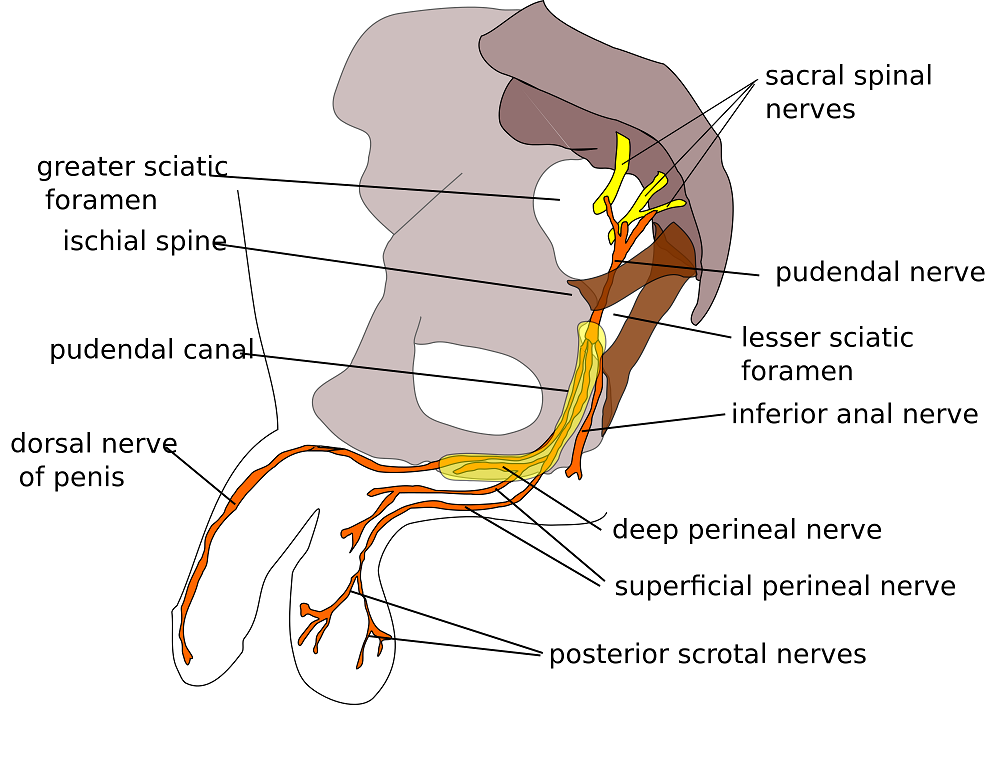
In 2016, Florian-Rodriguez, et al., studied cadavers to determine the nerves associated with the sacrospinous ligament, focusing on the inferior gluteal nerve. Fourteen cadavers were observed, noting the distance from various nerves to the sacrospinous ligament (from a pelvic approach) and to the ischial spine (from a gluteal approach). The S3 nerve was closest to the sacrospinous ligament, and the pudendal nerve was the closest to the ischial spine. In 85% of subjects, 1 to 3 branches from S3/S4 nerves pierced or ran anterior to the sacrotuberous ligament and pierced the inferior part of the gluteus maximus muscle. The authors concluded the inferior gluteal nerve was less likely to be the source of postoperative gluteal pain after sacrospinous ligament fixation; however, as the pudendal nerve branches from S2-4, it was more likely to be implicated in postoperative gluteal pain.
A study by Ploteau et al. (2017) explored the anatomical position of the pudendal nerve in people with pudendal neuralgia. In 100 patients who met the Nantes criteria, 145 pudendal nerves were surgically decompressed via a transgluteal approach. At least one segment of the pudendal nerve was compressed in 95 of the patients, either in the infrapiriform foramen, ischial spine, or Alcock’s canal. In 74% of patients, nerve entrapment was between the sacrospinous ligament and the sacrotuberous ligament. Anatomical variants were found in 13% of patients, often with a transligamentous course of the nerve.
When the pudendal nerve is caught in the narrow space between ligaments in the pelvis, diagnosing the source of pain is paramount. Research supports a gluteal approach in releasing the entrapped nerve. Post-surgical care falls into the hands of pelvic floor therapists, so taking “Pudendal Neuralgia and Nerve Entrapment: Evaluation and Treatment” may be something to consider in order to provide optimal care.
Ploteau, S, Cardaillac, C, Perrouin-Verbe, MA, Riant, T, Labat, JJ. (2016). Pudendal Neuralgia Due to Pudendal Nerve Entrapment: Warning Signs Observed in Two Cases and Review of the Literature. Pain Physician. 19(3):E449-54
Florian-Rodriguez, ME, Hare, A, Chin, K, Phelan, JN, Ripperda, CM, Corton, MM. (2016). Inferior gluteal and other nerves associated with sacrospinous ligament: a cadaver study. American Journal of Obstetrics and Gynecology. 215(5):646.e1-646.e6. doi: 10.1016/j.ajog.2016.06.025
Ploteau, S, Perrouin-Verbe, MA, Labat, JJ, Riant, T, Levesque, A, Robert, R. (2017). Anatomical Variants of the Pudendal Nerve Observed during a Transgluteal Surgical Approach in a Population of Patients with Pudendal Neuralgia. Pain Physician. 20(1):E137-E143
In the comedy, Kindergarten Cop, Detective John Kimble may only have had a headache, not a tumor, but sometimes our patients do have a tumor. One of my patients was actually just diagnosed with a brain tumor after responding poorly to a cortisone injection for her neck pain. Tumors in other areas of the body, even in the pelvis, can be the source of symptoms that may seem like a nerve entrapment. This is a serious consideration to be given when diagnosing pudendal neuralgia.
 In 2008, Labat et al. published the “Diagnostic Criteria for Pudendal Neuralgia by Pudendal Nerve Entrapment” in Neurourology and Urodynamics . A group in Nantes, France, established criteria in 2006, since the diagnosis is primarily clinical in nature. The results of this paper concluded the five essential diagnostic criteria (Nantes criteria) are as follows:
In 2008, Labat et al. published the “Diagnostic Criteria for Pudendal Neuralgia by Pudendal Nerve Entrapment” in Neurourology and Urodynamics . A group in Nantes, France, established criteria in 2006, since the diagnosis is primarily clinical in nature. The results of this paper concluded the five essential diagnostic criteria (Nantes criteria) are as follows:
- Pain located in the anatomical region of the pudendal nerve.
- Pain worsened with sitting.
- Pain does NOT awaken the patient at night.
- Negative sensory loss upon clinical exam.
- Pain is relieved with an anesthetic pudendal nerve block.
A recent study by Waxweiler, Dobos, Thill, & Bruyninx explored the Nantes criteria as related to choosing surgical candidates for pudendal neuralgia from nerve entrapment. They looked at how a patient’s response to the anesthetic block corresponded to appropriate selection of patients for a successful surgical outcome. Six of 34 patients in the study had a negative anesthetic pudendal nerve block, and 100% of those patients had no symptom relief after surgery. In contrast, 64% of the patients who met all five of the Nantes criteria responded positively to surgery. The authors concluded confirmation of the 5th criteria as essential for predicting success of surgery for pudendal neuralgia by pudendal nerve entrapment.
In Pain Physician in 2016, Ploteau et al. present two case studies where consideration of the Nantes criteria helped diagnose rare tumors in patients who demonstrated red flags during examination. Warning signs such as nocturnal awakening, point-specific pain, pain of a neuropathic nature, and neurological deficits cannot be overlooked when a patient presents with pudendal neuralgia. In the case studies presented, the 31 year old woman did not have pain exacerbated with sitting and woke at night with pain, and the 62 year old woman was awakened at night with pain. Each patient had magnetic resonance imaging performed, and rare diagnoses of endometrial stromal sarcoma and adenoid cystic carcinoma were made, respectively. The tumors arose in the ischiorectal fossa and compressed the pudendal nerve, presenting as pudendal neuralgia in atypical forms requiring careful clinical examination and referral for MRI for accurate diagnosis.
Although a tumor rarely exists, it is our duty to recognize signs and symptoms that do not follow established criteria. Paying attention to what your patients say just may be lifesaving. Proper diagnosis of pudendal neuralgia is essential and sometimes falls in our hands.
Labat, JJ., Riant, T., Robert, R., Amarenco, G., Lefaucheur, JP., Rigaud, J. (2008). Diagnostic criteria for pudendal neuralgia by pudendal nerve entrapment (Nantes criteria). Neurourology and Urodynamics. 27(4):306-10. doi: 10.1002/nau.20505.
Waxweiler, C., Dobos, S., Thill, V., Bruyninx, L. (2016). Selection criteria for surgical treatment of pudendal neuralgia. Neurourology and Urodynamics. doi:10.1002/nau.22988.
Ploteau, S., Cardaillac, C., Perrouin-Verbe, M. , Riant, T., & Labat, J. (2016). Pudendal Neuralgia Due to Pudendal Nerve Entrapment: Warning Signs Observed in Two Cases and Review of the Literature. Pain Physician. 19:E449-E454.
One of my dear patients was recently diagnosed with Ehlers-Danlos sydrome (EDS). The diagnosis brought a sense of relief for sweet Katie who for years struggled with numerous health problems and was often misunderstood and under cared for by the medical community. Katie was referred to me 2 years ago at 28 for pelvic pain, endometriosis and IC. Upon exam we also discovered a significant elimination disorder and paradoxical elimination. Katie regularly timed her elimination and was spending at times up to 2 hours trying to empty her bowels. As we worked together we uncovered bilateral hip dysplasia, left hip labral tear, ilioinguinal and pudendal neruralgia and POTS (Postural Orthostatic Hypotension Syndrome). Katie already had a history of anxiety and depression but managed well with good family and friend support. When the diagnosis of EDS came, she finally felt like she had an explanation for why her body is like it is. This brought great relief as well as the knowledge that her condition was genetic and her conditions needed to be managed as best as possible to give her the most function, but would likely never be fully resolved.
 In her book "A Guide to Living with Ehler's Danlos Syndrome" Isobel Knight does a beautiful job outlining the various genetic subtypes of Ehlers Danlos but also highlighting the fact that EDS hypermobility type (Type III) does not just affect the connective tissue in the musculoskeletal sytem leading to joint instability and hypermoblity, muscle tears, dislocations, subluxations, hip dysplasia and flat feet. EDS can also affect the body's systemic collagen leading to increased risk for endometriosis, POTS, Renauds, bladder problems, fibromyalgia, headaches, restless legs, ashtma, consitpation, bloatedness, prolapse, IBS symptoms, anxiety, depression and learning difficulties. She notes that some people have only a few of these systemic symptoms while others may be more affected. Per Isobel: "it is important that all symptoms are treated seriously and not ridiculed and that the appropriate medical support is given to them when necessary."
In her book "A Guide to Living with Ehler's Danlos Syndrome" Isobel Knight does a beautiful job outlining the various genetic subtypes of Ehlers Danlos but also highlighting the fact that EDS hypermobility type (Type III) does not just affect the connective tissue in the musculoskeletal sytem leading to joint instability and hypermoblity, muscle tears, dislocations, subluxations, hip dysplasia and flat feet. EDS can also affect the body's systemic collagen leading to increased risk for endometriosis, POTS, Renauds, bladder problems, fibromyalgia, headaches, restless legs, ashtma, consitpation, bloatedness, prolapse, IBS symptoms, anxiety, depression and learning difficulties. She notes that some people have only a few of these systemic symptoms while others may be more affected. Per Isobel: "it is important that all symptoms are treated seriously and not ridiculed and that the appropriate medical support is given to them when necessary."
It seems that EDS is becoming more widely recognized. As rehabilitation specialists we should be alert to problems stemming from joint hypermobility when we notice how our patients position themselves. Often legs are curled up or double crossed. Upon questioning we might find that the patient has a history of being "double jointed" or was able to do "party tricks" with their bodies. The Bighton scale is a test of joint hypermobility which we should all be familiar with. It is also important to note that a patient may have hypermobility without having EDS, and that EDS is usually associated with pain. A rheumatologist, or in Katie's case a geneticist, can help confirm a suspected EDS diagnosis.
If you have a patient with hypermobliiy or with EDS, know that their ability to know where their body is in space is limited as their joints have much more range of motion than normal. The proprioceptors do not fire well at mid range and the patient will have to be trained to become accustomed to neutral joint positions. This was really painful for Katie and it took a huge mental and physical effort. She is getting stronger now and it is becoming easier to achieve. Stretching and soft tissue massage can feel really good when your muscles have to work so hard to maintain your joints in healthy positions. Patients should be instructed to not stretch into end range and also not "hang out" on their ligaments. Some patients may have to begin just with isometrics. I used Sara Meeks' program for safe and effective floor exercise with Katie. The floor gave her support while she strengthened her core muscles. Then she was able to progress to seated and seated on a ball as well as standing exercises. She loves the body blade! Yoga, Pilates, exercise in water can be effective for strength, propriception and movement reeducation. Mirrors are helpful for increasing position sense.
It is also helpful to note that even patients with EDS may be hypermobile in some joints and hypomobile in others. Isobel reports that her SI joints were extremely unstable while her thoracic spine was very rigid to the point that her lung capacity was affected. Having her therapist work on the hypomobility and doing breath work was life changing.
As pelvic health therapists and rehabilitation providers we may be the first professional to suspect EDS in a patient. There is a great deal that we and the greater medical and holistic community can do to help patients with EDS lead lives with less pain and dysfunction.
Herman & Wallace are pleased to announce a new course! Pudendal Neuralgia and Nerve Entrapment will be presented by Michelle Lyons in Freehold, NJ on June 17/18, 2017. We chatted with Michelle about this new course to hear her thoughts and get an overview of the contents
 There are a number of courses which I teach for Herman & Wallace including Pelvic Floor Level 2A, my Male Oncology and Female Oncology and the The Athlete and the Pelvic Floor courses. They all have sections on pudendal dysfunction and it’s an area that participants always want more information on. There’s no other nerve that elicits the same interest, discussion and confusion! Nobody really talks about iliohypogastric or ulnar neuralgia with the same intensity as pudendal neuralgia, and no other nerve dysfunction provokes the same amount of controversy and mystery.
There are a number of courses which I teach for Herman & Wallace including Pelvic Floor Level 2A, my Male Oncology and Female Oncology and the The Athlete and the Pelvic Floor courses. They all have sections on pudendal dysfunction and it’s an area that participants always want more information on. There’s no other nerve that elicits the same interest, discussion and confusion! Nobody really talks about iliohypogastric or ulnar neuralgia with the same intensity as pudendal neuralgia, and no other nerve dysfunction provokes the same amount of controversy and mystery.
When I was approached about developing this course for the Institute, I jumped at the opportunity. For those who don’t know me, I really like to bring an integrative approach to my work, both clinically and educationally. I have experience and training in nutrition, coaching, yoga, Pilates and mindfulness as a therapeutic intervention and I think these fit really well alongside traditional pelvic rehab approaches. Manual therapy and bespoke exercise prescription will always be the bedrock of my approach, but sometimes our patients, especially those with chronic pain, need some extra support. I’m also a bit of an anatomy nerd, so the chance to delve deep into pelvic neuroanatomy and neurodynamics was too much to resist!
I think this is a Golden Age in pelvic health – there are so many great learning opportunities and resources available to us to help serve our patients better. Another area that I find fascinating to explore is the huge leap we have made in understanding neuroscience and the role of pain education when it comes to chronic pelvic pain. I’m a big fan of the work done by Moseley and Butler in Australia, and I love how authors like Hilton, Vandyken and Louw have transferred that to the world of pelvic pain in their book "Why Pelvic Pain Hurts". The language that we use is very important when discussing how the brain responds to chronic pain and the changes that occur with central sensitization. We never want our patients to feel as if we think their pain is ‘all in their heads’ but at the same time, we need to be able to incorporate strategies such as motor imagery and graded exposure and to demonstrate to our patients that"…it is important to acknowledge that chronic pain need not involve any structural pathology" (Aronoff 2016).
Those are some of the discussions we’ll be having in Freehold, NJ next June – I hope you’ll come and join the conversation!
"What Do We Know About the Pathophysiology of Chronic Pain? Implications for Treatment Considerations" Aronoff, GM Med Clin North Am. 2016 Jan;100(1):31-42
"Why Pelvic Pain Hurts: Neuroscience Education for Patients with Pelvic Pain" Hilton, Vandyken, Louw, International Spine and Pain Institute (May 28, 2014)
The following comes from a male patient who wanted to share his story about finding care for his pelvic floor dysfunction. His story highlights the important role pelvic rehab practitioners can play, and why we need to continue training more therapists in this field.
I’m 65 year old male and I developed pudendal neuralgia and pelvic floor issues as a result of an accident about four years ago. Shortly after my accident I started to experience pain in my testicles and perineum. At the time, I did not think that one had anything to do with the other. I made an appointment with my urologist who did an ultrasound and assured me that there was nothing physically wrong. I don’t think my testicles quite believe that but mentally I felt relieved. But the pain persisted and started to spread. Now it was also in my groin and penis. I was also having problems with chronic constipation, urinary retention and erectile dysfunction. Since I did have back surgery years ago I started to suspect my low back was causing the problem. I made an appointment with a well-respected orthopedic surgeon in New York. While he gave me his analysis with regards to my back problems he clearly avoided addressing the pelvic issues. I left there feeling lost. Suffice it to say that over the course of the next couple of years I saw several other specialists who either skirted around the issue or told me that nothing was wrong. A couple of years passed but the pelvic issues just continued to get worse and worse. I started seeing a new primary care physician who indicated that perhaps the source of the pelvic pain was coming from the pudendal nerve and felt that physical therapy might help. She gave me a prescription for physical therapy to evaluate for pudendal nerve.
 Well, I have a diagnosis now so I start researching pudendal neuralgia and land on the Pudendal Hope website. Wow! What an eye opener that was. I’m reading the information on the website and it was like I had an epiphany. I realized that I was not going crazy and that Pudendal Neuralgia and pelvic pain are very real issues.
Well, I have a diagnosis now so I start researching pudendal neuralgia and land on the Pudendal Hope website. Wow! What an eye opener that was. I’m reading the information on the website and it was like I had an epiphany. I realized that I was not going crazy and that Pudendal Neuralgia and pelvic pain are very real issues.
OK, so where do I go from here? With prescription in hand I’ll make an appointment with a physical therapist that deals with pudendal neuralgia. Ha, I thought getting a diagnosis was tough but finding a physical therapist that treats pudendal neuralgia and pelvic issues was no easy task. To make things even more challenging, finding a physical therapist who treats men was even harder. I made a few calls and kept looking online without much success. Desperate to find a physical therapist that treats men, I sent an email off to a therapist in California asking if by some chance she could recommend a physical therapist here in New Jersey. As luck would have it, I got both a response and a referral. With that, I called Michelle Dela Rosa at Connect Physical Therapy. I had to wait about six weeks for an appointment but finally the day arrived. OK, so now, I had set my expectations. I’ll go for a few weeks of physical therapy, the pain will go away and it will be back to a normal life. Well, not so much… the journey and education were just getting started.
There are days when I am in so much pain that I ask myself if the pelvic therapy is really doing me any good. But then I reflect back to how things were before I started the therapy. Funny thing about pain… often times it makes us forget how things were in the past and shift our focus to the here and now. That being said, I quickly realize how much I have truly progressed since starting therapy.
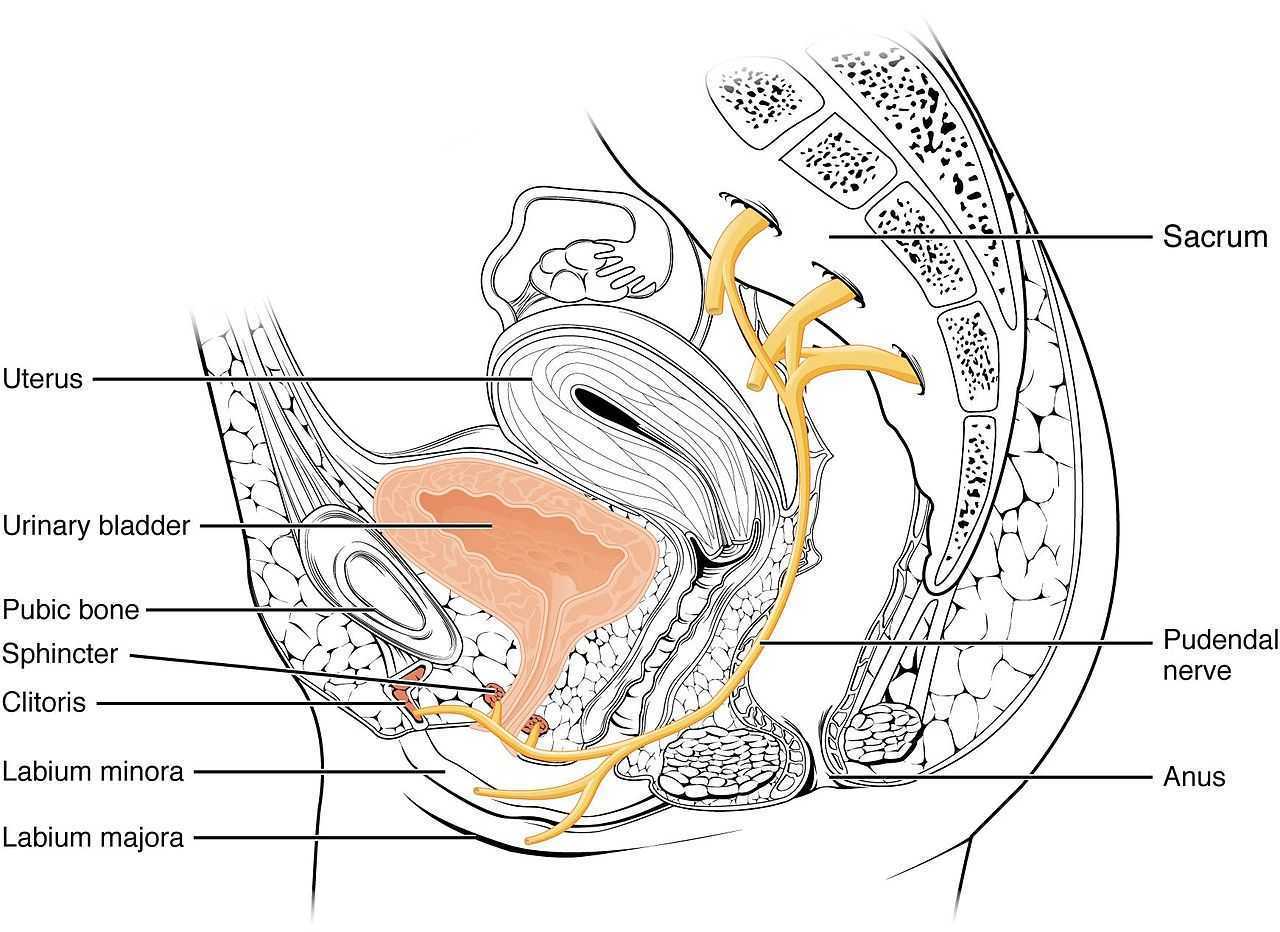
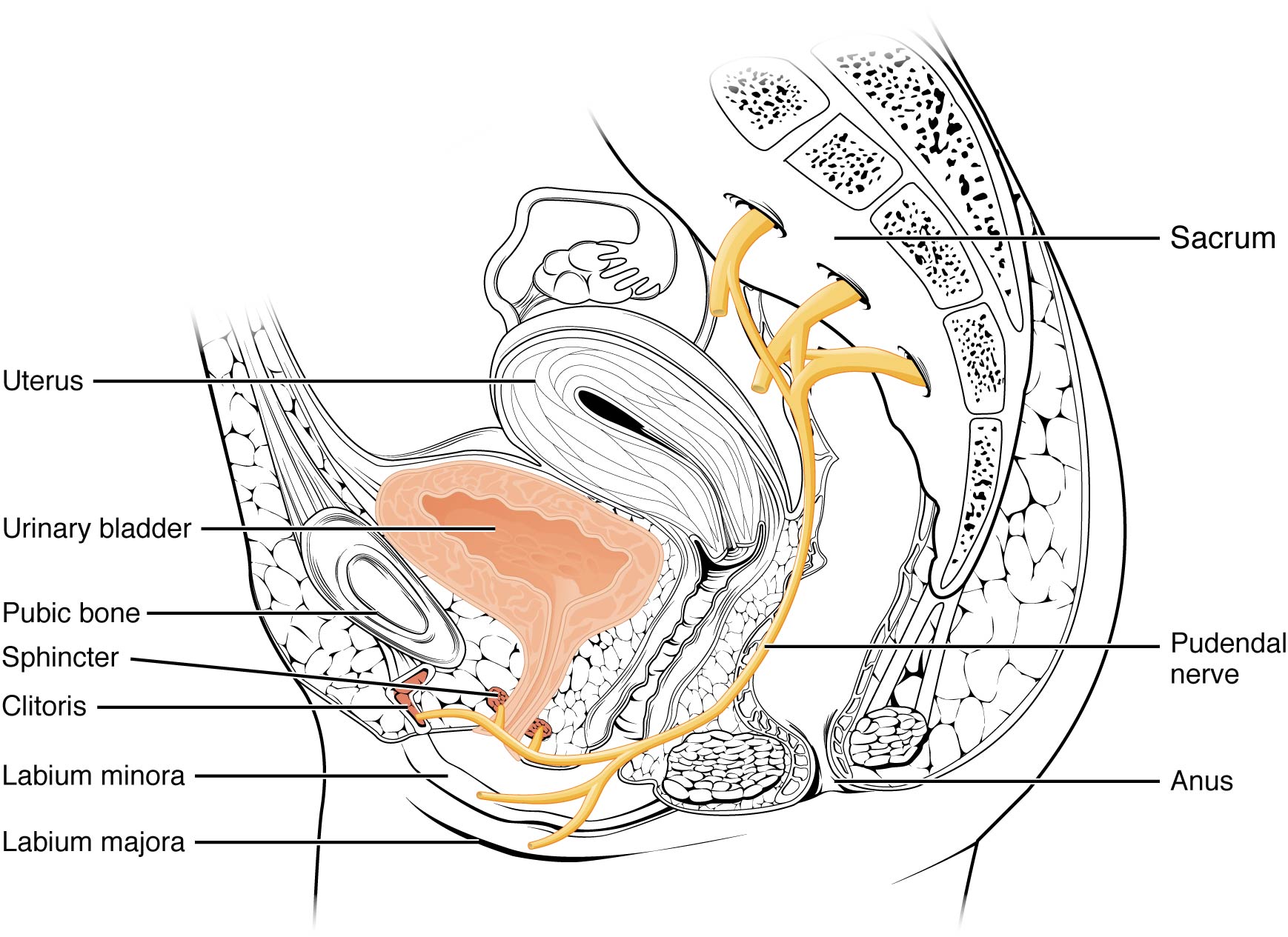
So what have I learned? Well, the first thing is to understand the anatomy and how all the pelvic muscle groups and nerves are integrated. After all you can’t fix what you don’t know is broken. Therapy has certainly helped educate me in that respect; I’ve learned the importance of proper breathing and strengthen the core muscles. I know that when I was in pain I would tighten up the pelvic muscles and hold my breath which would only make things worse, as the muscles would get into a knot, and make it even more difficult to get relief. I’ve learned a whole new set of exercises that I now have in my arsenal to help fight this battle. To help me deal with the chronic constipation I’ve learned how to massage my abdomen to help move things along. For those folks dealing with chronic constipation, well, we all know what happens when we push just a little too hard… flare time! I could go on and on. I learned to use tools, such as the TheraWand, to help break the tension for those internal pelvic muscles. Pelvic therapy has taught me the importance and benefits of the proper use of cold packs, glides, exercise, breathing, relaxing the pelvic floor and on and on and on.
I was a bit embarrassed getting started but the prospect of relieving some of the pelvic pain and the professionalism of my therapist quickly turned my embarrassment into a non-issue.
I want to express my thanks and gratitude to all those physical therapists who have the courage and vision to take on this problem. You are truly making a difference in the lives of the people you are helping.

A US study published in the International Society for Sexual Medicine last year reports on the available evidence linking cycling to female sexual dysfunction. In the article, some of the study results are summarized in the left column of the chart below. On the right side of the column, we can consider ideas about how to potentially address these issues.
| Examples of Research Cited |
Ideas for Addressing Potential for Harm |
| dropped handlebar position increases pressure on the perineum and can decrease genital sensation | encourage cyclists to take breaks from dropped position, either by standing up or by moving out of drops temporarily |
| chronic trauma can cause clitoral injury | encourage cyclists to wear appropriately padded clothing, to apply cooling to decrease inflammation, and to use quality shocks or move out of the saddle when going over rough roads/terrain when able |
| saddle loading differs between men and women | women should consider specific fit for bike saddles |
| women have greater anterior pelvic tilt motion | is pelvic motion on bike demonstrating adequate stability of pelvis or is there a lot of extra motion and rocking occurring? |
| lymphatics can be harmed from frequent infections and from groin compression | patients should be instructed in positions of relief from compression and in self-lymphatic drainage |
| pressure in the perineal area is affected by saddle design, shape | female cyclists with concerns about perineal health should work with a therapist or bike expert who is knowledgeable about a variety of products and fit issues |
| unilateral vulvar enlargement can occur from biomechanics factors | therapists should evaluate vulvar area for size, swelling, and evidence of imbalances in the tissues from side to side, and evaluate bike fit and mechanics, encouraging women to create more symmetry of limb use |
| genital sensation is frequently affected in cyclists, indicating dysfunction in pudendal nerve | therapists should evaluate female cyclists for sensory or motor loss, establishing a baseline for re-evaluation |
Because women tend to be more comfortable in an upright position, the authors recommend that a recreational (more upright) versus a competitive (more aerodynamic and forward leaning) position may be helpful for women when appropriate. Although saddles with nose cut-outs and other adaptations such as gel padding in seats are discussed in the article, the authors caution against making any distinct recommendations due to the paucity of literature that is available. The paper concludes that more research is needed, and particularly for considering the varied populations of riders ranging from recreational to racing.
Within a pelvic rehabilitation setting, applying all orthopedic and specific pelvic rehabilitation skills is necessary for women cyclists who present with pelvic dysfunction. Because injury to the perineal area including the pudendal nerve can have negative impact on function such as bowel, bladder, or sexual health, skills in helping a patient heal from compressive or traumatic cycling injuries is very valuable. To learn more about pudendal nerve health and dysfunction, the Institute offers a 2-day course titled Pudendal Neuralgia Assessment, Treatment and Differentials: A Brain/Pain Approach. This course is offered next in Salt Lake City in April, so sign up soon!