Part 2: The Drama Triangle
This is part two of a three-part series on self-care and preventing practitioner burnout from faculty member Jennafer Vande Vegte, MSPT, BCB-PMD, PRPC. Part One is available here. Jennafer is the co-author and co-instructor of the along with Nari Clemons, PT, PRPC.
Augh, I was so frustrated with myself. I fell for it again. Here’s the scenario: a patient came in suffering excruciating pain. She had been to see a pelvic health professional as well as various medical professionals and was unable to get relief and answers for her rectal pain. She was desperate and called me “her last hope.” Phrases used included, “I need you! Fix me! I hear you are a miracle worker! If you can’t help me no one can!” And just like that I took on the role of Rescuer.
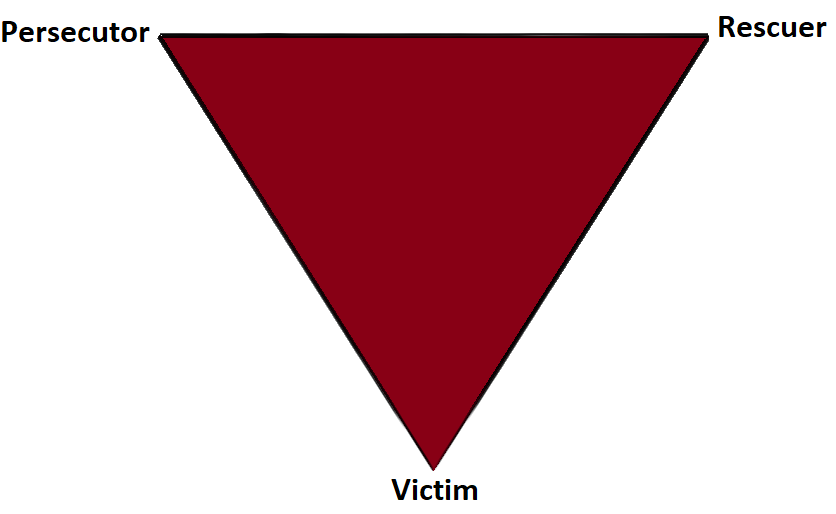
In 1968 a psychiatrist named Stephen Karpman developed a model of personal interaction that he called the Conflict Triangle. It has also become known as the Karpman Triangle, The Drama triangle or the Victim triangle. Per Wikipedia:
The Victim: The Victim's stance is "Poor me!" The Victim feels oppressed, helpless, hopeless, powerless and ashamed. They seem unable to make decisions, solve problems, take pleasure in life or achieve insight. The Victim, if not being persecuted, will seek out a Persecutor and also a Rescuer who may save the day, but may also perpetuate the Victim's negative feelings.
The Rescuer: The Rescuer's line is "Let me help you." A classic enabler, the Rescuer feels guilty if they don't rush to the rescue. Yet their rescuing has negative effects: It keeps the Victim dependent and gives the Victim permission to fail. The rewards derived from this rescue role are that the focus is taken off of the Rescuer. When they focus their energy on someone else, it enables them to ignore their own anxiety and issues. This rescue role is also pivotal because their actual primary interest is really an avoidance of their own problems disguised as concern for the victim’s needs.
The Persecutor: (a.k.a. Villain) The Persecutor insists, "It's your fault." The Persecutor is controlling, blaming, critical, oppressive, angry, authoritative, rigid, and superior.
 What is interesting about this triangle is that the roles are constantly shifting. In full rescuer mode, I gladly took on this patient, intent on solving her problems. Over time, I saw that my consistent coaching for lifestyle change and self-care was falling on deaf ears. My patient was not following through with anything I asked of her; therefore my treatment plan was not working. The patient began to get frustrated with me. I then cast myself as the victim. She became my persecutor! While perhaps in her mind, I had failed as the rescuer, she was still the victim and I had become her persecutor. At the time, I did not have the skills to know how to navigate this situation in a positive or helpful way. Finally I sought the advice of my supervisor and my therapist to draw up a contract with this patient. The contract outlined each of our responsibilities. If either of us didn’t fulfill our responsibilities, the consequence would be ending our professional relationship. When she persisted, unwilling to do her part, I discharged her per our agreement.
What is interesting about this triangle is that the roles are constantly shifting. In full rescuer mode, I gladly took on this patient, intent on solving her problems. Over time, I saw that my consistent coaching for lifestyle change and self-care was falling on deaf ears. My patient was not following through with anything I asked of her; therefore my treatment plan was not working. The patient began to get frustrated with me. I then cast myself as the victim. She became my persecutor! While perhaps in her mind, I had failed as the rescuer, she was still the victim and I had become her persecutor. At the time, I did not have the skills to know how to navigate this situation in a positive or helpful way. Finally I sought the advice of my supervisor and my therapist to draw up a contract with this patient. The contract outlined each of our responsibilities. If either of us didn’t fulfill our responsibilities, the consequence would be ending our professional relationship. When she persisted, unwilling to do her part, I discharged her per our agreement.
I learned so much from this experience. Here are some things that I have implemented and may be helpful in your practice if you have similar challenges.
- In an initial visit with a new patient I explain that the patient and I make a team and we each have a role to play in reaching the patient’s goals.
- If someone says, “Fix me!” I say, “Think of me as your coach, I can show you how to help your body heal, but it’s your job to do the work.”
- When I hear, “Everyone says you are a miracle worker.” I say, “That is so kind, but it doesn’t work that way. Healing is complicated and everyone has their own journey.”
- In this way, with baby steps, we can get OUT of the drama triangle and into healthy relationships with our patients and the people in our lives.
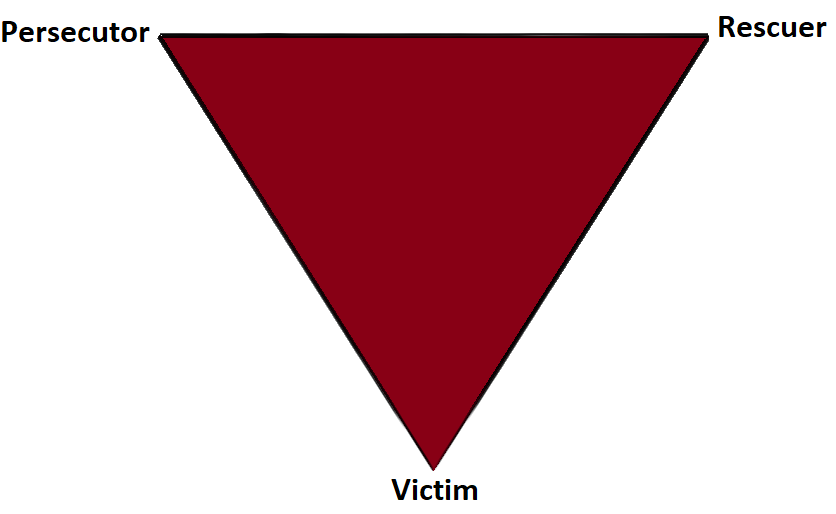
- Consider the Winner's Triangle published by Acey Choy in 1990.
In her blog NextMeCoaching, Jessica Vader coaches on turning Drama and Control into a Winning situation.
The three roles in the Winner’s Triangle.
Vulnerable – a victim should be encouraged to accept their vulnerability, problem solve, and be more self-aware.
Assertive – a persecutor should be encouraged to ask for what they want, be assertive, but not punishing.
Caring – a rescuer should be encouraged to show concern and be caring, but not over reach and problem solve for others.
If you struggle with professional and personal boundaries, you are not alone, and you can get support. Consider talking with your supervisor, a counselor, reading a good book on the subject, and or taking Boundaries, Mediation and Self Care, a course offering through Herman and Wallace that was designed to help pelvic health professionals stay healthy and inspired while equipping therapists with new tools to share with their patients.
We hope you will join us for Boundaries, Mediation and Self Care this November 9-11, 2019 in San Diego, CA.
Look forward to my next blog where saying no takes an unexpected turn.
The following is part three in a series documenting Deb Gulbrandson, PT, DPT's journey treating a 72 year old patient who has been living with multiple sclerosis (MS) since age 18. Catch up with Part One and Part Two of the patient case study on the Pelvic Rehab Report. Dr. Gulbrandson is a certified Osteoporosis Exercise Specialist and instructor of the Meeks Method, and she helps teach The Meeks Method for Osteoporosis course.
 On Maryanne’s third visit, after reviewing her home exercises I told her that today our focus was on alignment. “In dealing with osteoporosis we want the forces that act upon our bodies to line up as optimally as possible. We have gravity providing a downward force from above and we have ground reaction forces coming up from below. Remember back to your first visit when we did the Foot Press in sitting and talked about Newton’s 3rd Law? For every action there’s an opposite and equal reaction and, how by pressing your feet down it helped you to sit straighter and gave more support to your back?” She nodded in agreement.
On Maryanne’s third visit, after reviewing her home exercises I told her that today our focus was on alignment. “In dealing with osteoporosis we want the forces that act upon our bodies to line up as optimally as possible. We have gravity providing a downward force from above and we have ground reaction forces coming up from below. Remember back to your first visit when we did the Foot Press in sitting and talked about Newton’s 3rd Law? For every action there’s an opposite and equal reaction and, how by pressing your feet down it helped you to sit straighter and gave more support to your back?” She nodded in agreement.
“Well, there’s another important component to that- one that we call optimal alignment. When we sit or stand in a flexed posture, those two opposing forces do not line up well and can put undue stress and pressure on our body, particularly the vertebral bodies.” I showed her the spine again with an increased flexion (hyper-kyphosis) in the thoracic area. “It’s normal to have a kyphosis in the thoracic spine. What we don’t want is a hyper-kyphosis. We often see the apex of the increased curve around T-7, 8, 9 levels near the bra line. We also call it the “slouch line” because from the front, that’s where we slouch in sitting. A thoracic hyper-kyphosis can lead to hyper-lordosis in the lumbar spine as the body tries to counteract the flexion forces above with extension or arching in the low back. We know that Wolff’s Law states that bone in a healthy person will adapt to the loads under which it is placed.1 But we want those loads to be optimally transmitted; otherwise the adaptation can be problematic.”
With Maryanne sitting in a Perch Posture position on the side of the low mat table, I placed a 4 foot dowel rod alongside her back, touching her sacrum and apex of her thoracic curve. I instructed her to bring her occiput back toward the dowel without extending her neck. I wanted her to do more of a cervical retraction move. She was a good 3+ inches away. Previously I had measured her using the WOD (Wall to Occiput Distance).2 This helps patients understand when they are forward flexed in the upper thoracic and cervical area and becomes an exercise as well. Since Maryanne was not safe in a standing position, we used an armless chair against the wall. I turned it sideways so the side of the chair was snugged up to the wall and transferred her to the chair, sitting so that her sacrum was flush against the wall. “Bring your upper back against the wall without allowing your low back to arch forward”, I told her as I placed a folded towel behind her head. “Now you’re going to press the back of your head into the towel, just as you do when lying down in the Re-alignment routine. Before you perform the Head Press, inhale to prepare, start your exhale, then do the head press. Hold for 3 -5 seconds as you continue to exhale, then relax as you inhale. Do 3-5 reps.”
The Head Press in standing, (or in Maryanne’s case, sitting) is a convenient way to not only strengthen the back muscles isometrically, but also increase awareness of body in space and relationship of head to trunk positioning. For any individual who has developed a forward head position over a period of years, there is a loss of the proprioceptive feedback necessary to know when we’re not in alignment, even if we have the ROM to achieve it. And often a lack of strength and especially muscle endurance to maintain that optimally aligned position is problematic. Using the wall several times a day can assist in building strength and awareness. In Maryanne’s case we needed a folded towel behind her occiput to give her something to press into and prevented her from going into increased cervical extension.
“I still want you to do the Head Press in supine as part of the Re-alignment routine everyday”, I told her. “But also practice it in sitting against a wall, making sure your sacrum is right up against it. Do this several times a day for several minutes, holding 3-5 seconds each. And be sure to use your breath to maintain neutral alignment of your lumbar spine.”
And with that, our work for the day was done.
1. Wolff's Law and bone's structural adaptations to mechanical usage: an ... https://www.ncbi.nlm.nih.gov/pubmed/8060014
2. Concurrent Validity of Occiput-Wall Distance to Measure Kyphosis in Communities. Journal of Clinical Trials. May 18, 2012 Sawitree Wongsa1,4, Pipatana Amatachaya2,4, Jeamjit Saengsuwan3,4 and Sugalya Amatachaya1,4*
The following is part two in a series documenting Deb Gulbrandson, PT, DPT's journey treating a 72 year old patient who has been living with multiple sclerosis (MS) since age 18. Catch up with Part one of the patient case study on the Pelvic Rehab Report here. Dr. Gulbrandson is a certified Osteoporosis Exercise Specialist and instructor of the Meeks Method, and she helps teach The Meeks Method for Osteoporosis course.
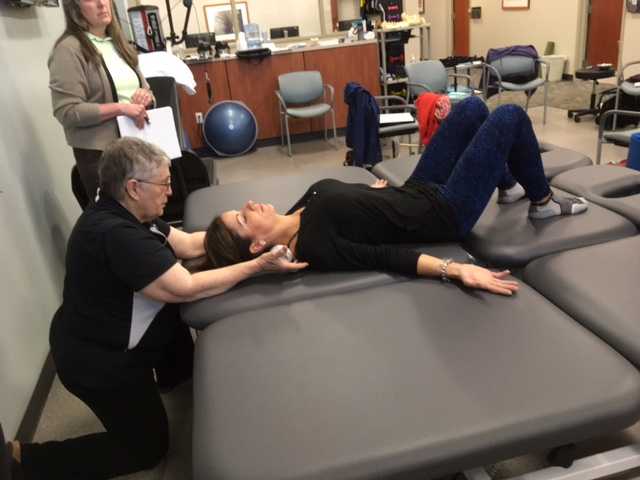
On Maryanne’s second visit, she reported she had been doing her “homework” and didn’t have any questions. Just to be sure, we reviewed them and I had her demonstrate. In Decompression position, she was lying supine with her hands on her abdomen, a common mistake I see. Usually this is due to tightness in pec minor with protracted scapulae. Patients unknowingly resort to the path of least resistance to take the strain off of the muscles. I explained to her that we want to use gravity to gently lengthen those muscles and “widen” the collarbones to allow for improved alignment. With her shoulders abducted to approximately 30 degrees and palms up, I propped a couple of small towels under her forearms which allowed her shoulders to relax into a more posterior and correct position.
“Today we begin the Re-alignment routine,” I said, “starting with the Shoulder Press.” I showed her how to gently press the back of her shoulders down into the mat without arching her lumbar spine. “As you press your shoulders down, exhale through your mouth as if you’re fogging a mirror. This will help activate your core muscles to keep your back in good alignment. Hold for 2-3 seconds, and then relax. Repeat 3 times.” Maryanne looked at me as if I’d lost my mind. “Did you say do 3 reps?” she asked. “I do 2 sets of 20 reps at the gym,” she said with obvious pride in her voice. “Yes, that’s where we start, and there are a couple of reasons. First, these are very site specific exercises which focus on the exact areas that need strengthening. Exercises done in a gym setting are often more general and usually involve compensation. We are minimizing any compensation such as allowing your low back to arch. There is probably weakness in those upper back muscles as well as the tightness seen in your anterior chest muscles and we need to go slowly. Also, we are simultaneously stretching while we strengthen. Our society is so forward biased (we work on computers, drive cars, make beds, eat- it’s all forward, forward, forward), that the anterior muscles get tight and the upper back muscles get overstretched and weak. We need to reverse that pattern. Take a look at our younger population and their texting postures. Yikes! We will be layering on more exercises as your technique improves so you’ll be doing more than just 3 reps, I promise.”
After the Shoulder Press we proceeded with the Head Press, Leg Lengthener and Arm Lengthener, spending time to make sure her cervical spine stayed in neutral as she pressed her head down into the mat. Head Press (cervical retraction) performed in supine allow patients to have something to press against and helps inhibit the tendency to move into cervical extension. It can also be done standing against the wall with a small pillow or folded towels between the occiput and the wall.
We ended with Maryanne in standing at the kitchen sink to promote functional activities and weight bearing positions. I reminded her to do the Foot Press through the floor using the Triangle of Foot Support visual. This helped to elongate her spine. “Imagine a bungie cord running from the top back of your head to the ceiling” I said which further increased her standing height. “Now I want you to imagine a shelf running straight out from your breastbone with a glass of some very expensive fine drink sitting on it. Do not spill your libation! Oh, and one last thing Maryanne. Breathe!!!” At which point she collapsed into laughter and our session was over. “Busted”, she said.
Today we pick up on Jennafer Vande Vegte's interview with her patient, "Ben", about his experience overcoming chronic pelvic pain syndrome. Ben's quality of life improved so much that he has returned to school in order to become a PTA, with a focus on pelvic rehabilitation!
Describe your physical therapy experience. Talk about your recovery process. Include the physical, mental and emotional components.
 For my initial visit, my therapist questioned and assessed my pain, then explained pelvic floor dysfunction. She made sure I understood that the evaluation and treatment process involved internal rectal work. After developing the condition and months of seeing doctors who didn’t listen, finally I found a physical therapist who was actually listening to me and determined to get to the bottom of what was going on. I could tell she already knew much about the mechanics (if not the exact cause) because she had treated other patients with the same issues. I immediately sensed a difference from any other health care professional in attitude, compassion, and knowledge. Of course, how do you know for sure? Well, you don’t. But after repeated visits and excellent results, you experience the difference. An important realization while going to Physical Therapy is learning to see the mind-body connection. In the back of my mind I sensed that my pain was being perpetuated by emotional trauma. This is not an intuitive way of thinking when you are in constant high-level, 5-alarm pain. I was obsessed with finding the cause of my pain, but chronic pain is extremely elusive and complicated.
For my initial visit, my therapist questioned and assessed my pain, then explained pelvic floor dysfunction. She made sure I understood that the evaluation and treatment process involved internal rectal work. After developing the condition and months of seeing doctors who didn’t listen, finally I found a physical therapist who was actually listening to me and determined to get to the bottom of what was going on. I could tell she already knew much about the mechanics (if not the exact cause) because she had treated other patients with the same issues. I immediately sensed a difference from any other health care professional in attitude, compassion, and knowledge. Of course, how do you know for sure? Well, you don’t. But after repeated visits and excellent results, you experience the difference. An important realization while going to Physical Therapy is learning to see the mind-body connection. In the back of my mind I sensed that my pain was being perpetuated by emotional trauma. This is not an intuitive way of thinking when you are in constant high-level, 5-alarm pain. I was obsessed with finding the cause of my pain, but chronic pain is extremely elusive and complicated.
Over the course of many months of PT though we couldn’t pinpoint what started the pain, we knew my nervous system was keeping it going. Sensory signals had somehow been rerouted through pain centers in the delicate and complicated highway interstate of the nervous system. It was as if the Fed Ex truck that was supposed to carry a package from Miami to Denver got rerouted to New York, stuck in traffic in Manhattan, flipped off by cab drivers, beaten up by gang members, contents of the truck shaken up by the driver trying to flee the city, and then finally finding the way out of New York to the true destination of Denver – with damaged goods, and shaking with anxiety. As to who the idiot dispatcher was who re-routed the truck to New York, well, he’s really good at keeping himself secret and innocent-looking. Jerk!
Physical therapy, over time, began to work for me. It released trigger points which are the first step in the long process of recovery. As we know, chronic tension must be addressed in tissues and nerves, and the mind must relearn how to remain in neutral. I found that as I gained periods of relief I could see that there truly was a mind-body connection beyond what I could imagine. My physical therapist and I both knew that nerves are the slowest recovering tissue in the body, and when you combine that with an anxious mind, you have a complicated puzzle to solve. There is definitely a closed circuit that develops with chronic pelvic pain. Pain causes anxiety, anxiety causes pain and circularly they feed one another.
During my physical therapy I joined a male pelvic pain message board online. I began understanding that most men who develop pelvic pain also have experienced traumatic emotional stress. And a large part of chronic pelvic pain is rooted in a mind-body dysfunction. I had to learn how to stop thinking catastrophically, especially during flare ups. I had to trust that my body would heal and think positively. I had to learn how to relax, take care of myself, eat well, stretch and exercise daily.
When I started physical therapy, I hoped to escape the pain. My first 5 month phase of physical therapy helped to loosen the chronically tightened pelvic sphincter muscles. However, I still had allodynia. In my second phase of physical therapy I began experiencing reduction of pain for a longer duration of time. After about a year of therapy, I finally got to a point where I could see there was significant improvement, even though some intermittent pain and anxious symptoms stubbornly persisted. In late spring of 2017, I finally felt like I had conquered the pain by 98%. Occasionally flares would still come, but they were brief and nothing like before physical therapy.
How has your experience with chronic pelvic pain changed you?
CPPS has profoundly changed me. I don’t take the little things for granted or sweat them anymore. I am grateful for not feeling that horrible, hellish sensation any longer. I appreciate having my mind pain and panic free. I speak my mind while respecting my own desires instead of belittling them. I am currently in school to become a Physical Therapy Assistant as through this process I learned that I’m actually much smarter than my middle school guidance counselor thought. I understand the mind is incredibly powerful, and fear rarely has the same power over me.
How do you handle flare ups?
I now handle brief flare ups with deep breaths, meditation, and/or just taking a step back and trying to zero in on what is really bothering me. At least now I can clearly think without debilitating pain and am able to function.
What would you like to say to other people who are struggling with chronic pelvic pain?
Oh, man. For the initial duration, I would say find a safe place where you can feel as comfortable as possible until the pain lessens. When it is bad, you sort of have to give in to it. However, part of this recovery is the physical mechanics of muscle and fascia. Physical Therapy is essential in the process of recovery to release this tension. I would tell them not to give up hope. You will not find many health professionals or websites that will tell you that you can beat this and recover 100%. But I will tell you, you can recover, 100%. You can. But for now, your full-time job is to work on recovery, and that includes lots of self-care, facing possible emotional pain, and physical therapy.
If you would like to learn more about addressing the mind body connection with patients please join us for Holistic Intervention and Meditation: Boundaries, Self-Care and Dialog in January. We will be exploring ways to help our patients heal to their fullest potential as well as keeping ourselves emotionally healthy in the process. Treating patients with persistent pain can be challenging for the best of us. Please come for this three-day course where you will leave feeling refreshed, renewed and reinvigorated to treat even your most complex patient.
Additional resources:
https://www.tamethebeast.org/#home
https://www.youtube.com/watch?v=jIsF8CXouk8
http://www.sciencedirect.com/science/article/pii/S1356689X11000737
http://www.noigroup.com/en/Home
https://bodyinmind.org/who-are-we/
Recently my coworkers and I celebrated a male patient’s recovery from a long and difficult journey with persistent pelvic pain. “Ben’s” case had many elements of what we normally see in our patients: chronic muscle holding, restricted fascia, allodynia, hyperalgesia, castrophizing and kenisiophobia. Ben was also very upfront about how his pain impacted his emotional well-being and vice versa. His healing process taught us a lot about the biopsychosocial aspects of treating persistent pain. Along his journey we dreamed of the day we could write a blog together and help other people learn from the experience. Ben also decided to make a career change entering school to become a PTA so that he could help others in pain. Here is my interview with this brave patient.
 1. Tell us about how your pain started
1. Tell us about how your pain started
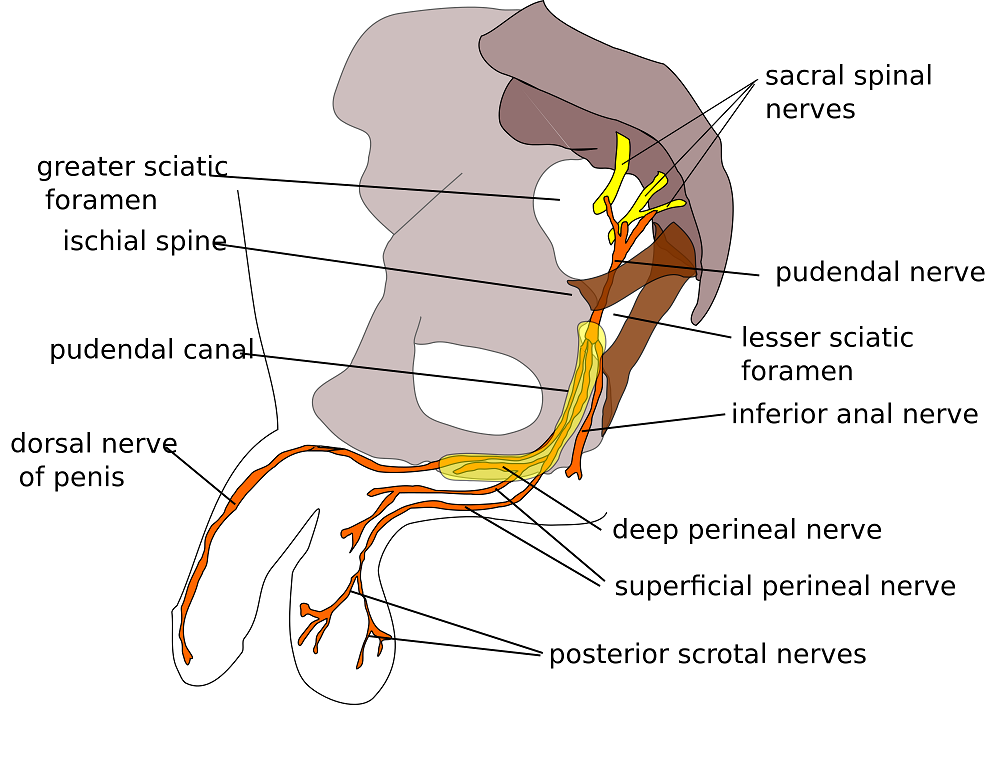
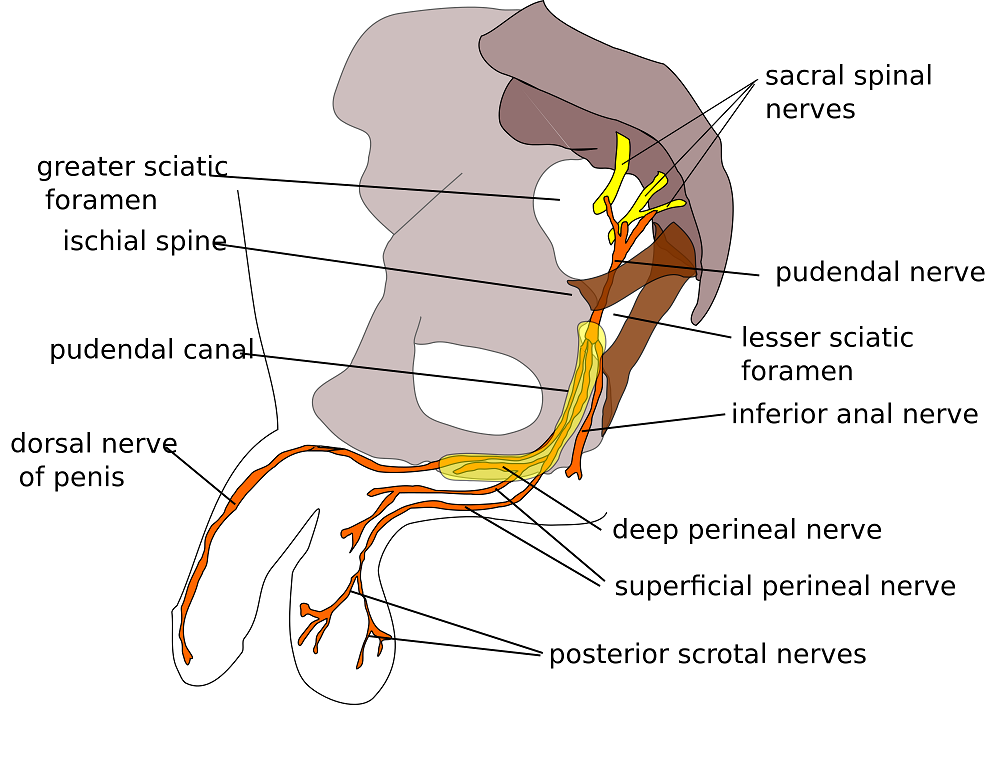
My pain started with urethral burning. Tests showed there was no infection. In retrospect, the cause of pain could have been the beginning of tension on pudendal nerve branches from extreme stress and a series of traumatic incidents that happened within weeks of each other. They included a very embarrassing and stressful summer of unemployment, a father who had heart failure and triple bypass in the fall, and a girlfriend who gave me an ultimatum when I was too stressed to get an erection.
2. What medical tests or treatments were done?
When the pain started, I first thought it was a basic urinary tract infection. I went to the med center and was prescribed an antibiotic. After 3 days without change, I went back in and although they still found no sign of infection, they prescribed an additional antibiotic. The urethral pain never stopped and seemed to get worse. Following a series of visits to numerous doctors and urologists, I repeated tests on the prostate fluid, blood tests, and more bacterial tests. No infection. My PCP also made a fairly large overture of testing me repeatedly for HIV. For five months I had a blood test every month, all came back negative. This was damaging to my psyche. For those months I was terrified my life was over. In retrospect, that doctor was out of line, I changed doctors.
3. What were your thoughts when your doctor suggested physical therapy?
When the doctor suggested pelvic floor physical therapy, I was a little skeptical because I was still convinced that something was wrong in a chemical or infectious way (as is typical for most men with pelvic floor dysfunction). However, desperate to take away the constant pain, I followed the advice.
Stay tuned for part two of our conversation with Ben, coming up in our next post on the Pelvic Rehab Report!
The following comes from a male patient who wanted to share his story about finding care for his pelvic floor dysfunction. His story highlights the important role pelvic rehab practitioners can play, and why we need to continue training more therapists in this field.
I’m 65 year old male and I developed pudendal neuralgia and pelvic floor issues as a result of an accident about four years ago. Shortly after my accident I started to experience pain in my testicles and perineum. At the time, I did not think that one had anything to do with the other. I made an appointment with my urologist who did an ultrasound and assured me that there was nothing physically wrong. I don’t think my testicles quite believe that but mentally I felt relieved. But the pain persisted and started to spread. Now it was also in my groin and penis. I was also having problems with chronic constipation, urinary retention and erectile dysfunction. Since I did have back surgery years ago I started to suspect my low back was causing the problem. I made an appointment with a well-respected orthopedic surgeon in New York. While he gave me his analysis with regards to my back problems he clearly avoided addressing the pelvic issues. I left there feeling lost. Suffice it to say that over the course of the next couple of years I saw several other specialists who either skirted around the issue or told me that nothing was wrong. A couple of years passed but the pelvic issues just continued to get worse and worse. I started seeing a new primary care physician who indicated that perhaps the source of the pelvic pain was coming from the pudendal nerve and felt that physical therapy might help. She gave me a prescription for physical therapy to evaluate for pudendal nerve.
 Well, I have a diagnosis now so I start researching pudendal neuralgia and land on the Pudendal Hope website. Wow! What an eye opener that was. I’m reading the information on the website and it was like I had an epiphany. I realized that I was not going crazy and that Pudendal Neuralgia and pelvic pain are very real issues.
Well, I have a diagnosis now so I start researching pudendal neuralgia and land on the Pudendal Hope website. Wow! What an eye opener that was. I’m reading the information on the website and it was like I had an epiphany. I realized that I was not going crazy and that Pudendal Neuralgia and pelvic pain are very real issues.
OK, so where do I go from here? With prescription in hand I’ll make an appointment with a physical therapist that deals with pudendal neuralgia. Ha, I thought getting a diagnosis was tough but finding a physical therapist that treats pudendal neuralgia and pelvic issues was no easy task. To make things even more challenging, finding a physical therapist who treats men was even harder. I made a few calls and kept looking online without much success. Desperate to find a physical therapist that treats men, I sent an email off to a therapist in California asking if by some chance she could recommend a physical therapist here in New Jersey. As luck would have it, I got both a response and a referral. With that, I called Michelle Dela Rosa at Connect Physical Therapy. I had to wait about six weeks for an appointment but finally the day arrived. OK, so now, I had set my expectations. I’ll go for a few weeks of physical therapy, the pain will go away and it will be back to a normal life. Well, not so much… the journey and education were just getting started.
There are days when I am in so much pain that I ask myself if the pelvic therapy is really doing me any good. But then I reflect back to how things were before I started the therapy. Funny thing about pain… often times it makes us forget how things were in the past and shift our focus to the here and now. That being said, I quickly realize how much I have truly progressed since starting therapy.
So what have I learned? Well, the first thing is to understand the anatomy and how all the pelvic muscle groups and nerves are integrated. After all you can’t fix what you don’t know is broken. Therapy has certainly helped educate me in that respect; I’ve learned the importance of proper breathing and strengthen the core muscles. I know that when I was in pain I would tighten up the pelvic muscles and hold my breath which would only make things worse, as the muscles would get into a knot, and make it even more difficult to get relief. I’ve learned a whole new set of exercises that I now have in my arsenal to help fight this battle. To help me deal with the chronic constipation I’ve learned how to massage my abdomen to help move things along. For those folks dealing with chronic constipation, well, we all know what happens when we push just a little too hard… flare time! I could go on and on. I learned to use tools, such as the TheraWand, to help break the tension for those internal pelvic muscles. Pelvic therapy has taught me the importance and benefits of the proper use of cold packs, glides, exercise, breathing, relaxing the pelvic floor and on and on and on.
I was a bit embarrassed getting started but the prospect of relieving some of the pelvic pain and the professionalism of my therapist quickly turned my embarrassment into a non-issue.
I want to express my thanks and gratitude to all those physical therapists who have the courage and vision to take on this problem. You are truly making a difference in the lives of the people you are helping.