Today The Pelvic Rehab Report is featuring two short interviews with instructor teams Alyson Lowrey & Tara Sulivan who teach Pain Science for the Chronic Pelvic Pain Population, and Sandra Gallagher & Caitlin Smigelski who teach Transgender Patients: Pelvic Health and Orthopedic Considerations.
The Pain Science for the Chronic Pelvic Pain Population instructors Alyson N Lowrey, PT, DPT, OCS &Tara Sullivan, PT, DPT, PRPC, WCS, IF answered the following two questions:
What Is Pain?
All pain occurs in the brain. Whether it is from acute tissue injury, nerve injury, or chronic pain, all pain has to be interpreted by the brain. How do you explain to a patient that their pain may not be from tissue damage, but from their brain interpreting something as painful that shouldn’t? While their pain may be in their brain, it is NOT in their head!
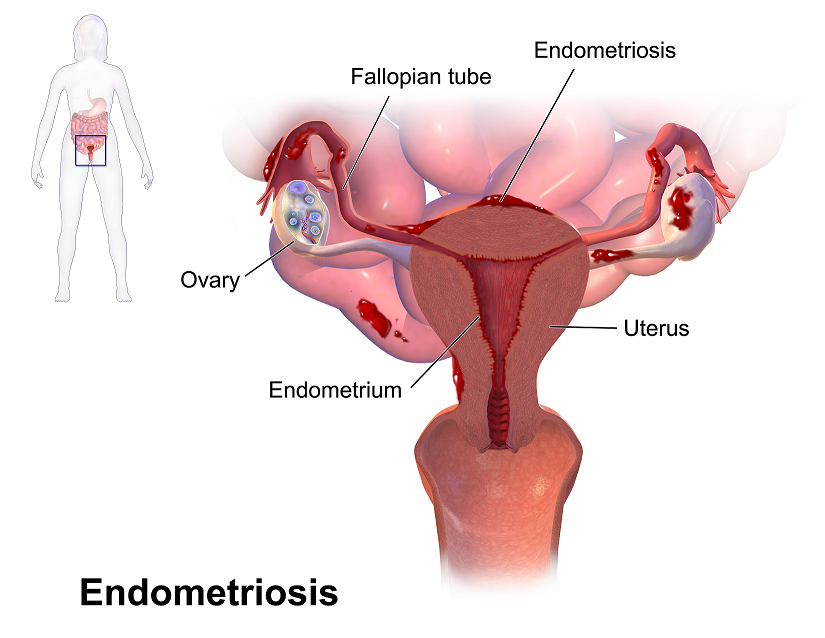
Pelvic pain is complicated because of a phenomenon called pelvic organ cross-talk. Your brain has a really hard time determining which pelvic organ or muscle is having pain or sensations, so signals can get crossed. Patients can present with uterine pain that can cause bowel or bladder pain and vice versa. We commonly see this with endometriosis and interstitial cystitis. Another example is the prostate and bladder. Prostatitis may present as an overactive bladder. This makes our jobs more difficult because we have to be able to determine the true source of a patient’s pain and understand that their pain may not be coming from an obvious source.
What is pain neuroscience education (PNE) and how can it be used?
Pain neuroscience education (PNE) is the explanation of the neurophysiological changes in the central nervous system to patients that have chronic pain. It is explaining pain, sensitization, and all the factors that can be contributing to their pain and abnormal sensations.
PNE typically decreases the threat value of pain, diminishes catastrophic thinking about pain, and facilitates a more active coping strategy. In the Pain Science for the Chronic Pelvic Pain Population, you will leave with the tools to combine pain science education with current interventions for a more effective treatment.
The Transgender Patients: Pelvic Health and Orthopedic Consideration instructors Sandra Gallagher, PT, DPT, WCS & Caitlin Smigelski, PT, DPT answered the following two questions:
What made you want to create this course?
We created this course on rehabilitation in gender-affirming care in 2018 because, at that time, nothing like it existed. We had learned so much from working with patients preparing for surgery and knew we need more information. Through attending conferences, we had opportunities to talk with experts in the field including surgeons, endocrinologists, primary care physicians, and social workers. Combined with researching additional topics, we made the course we wish we could have taken: a course that bridges physical rehabilitation considerations with medical and surgical information on transgender care.
Today, many brief courses and videos about gender-affirming care exist. You can now find courses and videos that address trauma-informed care, language aspects of gender-affirming care, and physicians and surgeons speaking on their procedures. We think this is great and encourage people to continue to seek out these learning opportunities! Our goal is to expand on the perspective of the rehab professional by offering a course that has both depth and breadth.
Our course has evolved to a hybrid format with pre-recorded self-paced lectures and live webinar content. We know that some participants are well versed in LGBTQ topics and are trained in providing trauma-informed care. For other participants, our course may be the first time they are exploring topics like sex, gender, sexuality, trauma-informed care, and gender-affirming language. The content in the pre-recorded lectures allows participants to work at their own pace, whether it is review or brand new information and allows everyone to have a similar foundation when we meet for the live portion.
What is your message to practitioners about gender-affirming care?
Our message to participants who are just starting their journey on gender-affirming care is to remember that gender is not genitals and that undergoing gender-affirming procedures is not strictly about sexual activity options. Sometimes people get so focused on the genital surgery or changes, that they forget the person. Every patient's path will be a bit different and there is more to gender-affirming care than peri-operative rehab.
Keep learning! Engage with professional organizations like WPATH, watch videos featuring gender diverse individuals, practice language with coworkers, and attend grand rounds. Many university hospitals now have virtual rounds that are available live or as recordings. There is so much information available if you search for it!
Pain Science for the Chronic Pelvic Pain Population
Course Date: October 8-9, 2022
Price:$400
Experience Level: Beginner
Contact Hours: 12
Description: This course is designed to expand the participant's knowledge, experience, and treatment in understanding and applying pain science to the chronic pelvic pain population including endometriosis, interstitial cystitis, irritable bowel syndrome, vaginismus, vestibulodynia, primary dysmenorrhea, and prostatitis. This course provides a thorough introduction to pain science concepts including classifications of pain mechanisms, peripheral pain generators, peripheral sensitization, and central sensitization in listed chronic pelvic pain conditions; as well as treatment strategies including therapeutic pain neuroscience education, therapeutic alliance, and the current rehab interventions' influence on central sensitization.
Lecture topics include the history of pain, pain physiology, central and peripheral sensitization, sensitization in chronic pelvic pain conditions, therapeutic alliance, pain science and trauma-informed care, therapeutic pain neuroscience education, the influence of rehab interventions on the CNS, and specific case examples for sensitization in CPP.
Transgender Patients: Pelvic Health and Orthopedic Considerations
Course Date: October 8,2022
Price: $500
Experience Level: Beginner
Contact Hours: 17
Description: This course is appropriate for any physical rehabilitation professional, regardless of their specialty area, who has an interest in better serving people who are gender diverse. There is specific content aimed at teaching pelvic health therapists how to expand their skills for working with people of all gender identities. There will be particular education regarding gender-affirming genital surgeries as well as discussion of other gender-affirming surgeries and medical interventions that people transitioning might choose.
Often times therapists think of genital surgeries and sexual function when contemplating work with transgender people. However, therapists have far more to offer transgender patients. For providing optimal care, knowledge of the intricacies of gender transition is essential. We provide that overview in this course. Topics covered include:
- Societal influence on gender transition including interactions with health care providers
- Recognizing difference between sex, sexuality, and gender
- Understand the complexities of the legal system for the person transitioning gender
- Tips and tools for a trauma-informed intake and examination
- Health effects of hormones for gender transition as related to differential diagnosis in rehabilitation
- Supporting healing after gender-affirming surgery
- Operative procedures for face and chest
- Operative procedures for masculinizing and feminizing genital surgery
- Pre-operative evaluation, treatment, and education issues
- Post-operative evaluation, treatment, education, and follow-up for genital surgeries
- Outcome measures with rehab focus for people undergoing gender-affirming surgeries
- Fertility and pregnancy in gender diverse people.
Alyson Lowrey, PT, DPT, OCS is the co-instructor for the H&W course Pain Science for the Chronic Pelvic Pain Population - Remote Course alongside Tara Sullivan, PT, DPT, PRPC, WCS, IF. Alyson treats the pelvic floor patient population through an orthopedic approach, working closely with pelvic floor specialists.
Pain neuroscience education (PNE) is the explanation of the neurophysiological changes in the central nervous system in patients with chronic pain. It includes how the nervous system functions and factors that influence its function such as social, psychological, and environmental factors. Pain neuroscience education aims to increase the patient’s knowledge about pain, decrease the threat of pain, and allow the patient to reconceptualize pain from a biopsychosocial perspective.
As a clinician seeing a patient with chronic and complex pain, it can be very daunting trying to determine how much education you should give the patient. Patients are generally very invested in improving their quality of life and therefore invested in learning how to treat their pain. Using techniques such as motivational interviewing is one way to determine if a patient is receptive to new information about pain and how to deliver that information. Education about pain needs to be varied and tailored to each patient based on their prior knowledge and perceptions, learning styles, their language, and their health literacy.
When a patient has an increased understanding of their pain and how their nervous system works, it can change their perspective about their pain by decreasing the threat value of their pain. PNE is the first step in the process of increasing a patient’s pain thresholds during exercise and functional activity. When patients no longer fear their pain as a sign of tissue damage, they can become empowered to re-educate their nervous system and pain processing centers in their brain. As providers, we are able to do this in several ways. We can do this by helping build new coping strategies and thought processes around their pain and dispelling misconceptions about their pain and physical ailments. We can suggest lifestyle and movement modifications that allow for more functional movement that doesn’t increase their pain activation centers. We can also adjust and modify our treatment plan around the patient's needs for success at each session. Consistently being a voice of encouragement, empowerment, and validation is also a very important component of PNE and our treatment as clinicians for our patients with chronic pain.
Pain Science for the Chronic Pelvic Pain Population - Remote Course
Course Date
October 8th-9th
Description
This course provides a thorough introduction to pain science concepts including classifications of pain mechanisms, peripheral pain generators, peripheral sensitization and central sensitization in listed chronic pelvic pain conditions; as well as treatment strategies including therapeutic pain neuroscience education, therapeutic alliance, and the current rehab interventions' influence on central sensitization. The rehab professionals who attend will be provided the understanding and tools needed to identify and treat patients with chronic pelvic pain from a pain science perspective. Lecture topics include the history of pain, pain physiology, central and peripheral sensitization, sensitization in chronic pelvic pain conditions, therapeutic alliance, pain science and trauma-informed care, therapeutic pain neuroscience education, the influence of rehab interventions on the CNS, and specific case examples for sensitization in CPP.
Herman & Wallace is excited to announce a collaboration with Dr. Michael Hibner, an international expert on pudendal neuralgia and chronic pelvic pain. Dr. Hibner is presenting a new remote course on January 9, 2022, titled Pudendal Dysfunction: The Physician's Perspective. Pudendal neuralgia is a painful, neuropathic condition involving the dermatome of the pudendal nerve. This condition is not widely known and often goes unrecognized by many practitioners. Dr. Hibner runs the Arizona Center for Chronic Pelvic Pain (AZCCPP), a comprehensive center for treating chronic pelvic pain, and places a heavy emphasis on working as part of a care team with physical therapists and other pelvic rehab providers.
In a recent publication by Dr. Hibner, he shares that “the International Pudendal Neuropathy Association estimates the incidence of this condition to be 1/100,000; however, most practitioners treating patients with this condition feel the actual rate of incidence may be significantly higher.” Many patients go an average of 10-15 years attempting to get a diagnosis for their pain. Diagnosis of this condition is heavily based on the utilization of Nantes Criteria in conjunction with clinical history and physical findings.
Dr. Hibner began his career as a urogynecologist. In the early 2000s, some of his patients presented with a vulvar burning pain that didn’t fit any known criteria. When he reviewed the histories of these patients, he found that the only thing in common between these patients was kickboxing. Further research then led him to pudendal neuralgia.
What are some of the typical patient characteristics/presentations and the time of diagnosis and referral?
If you think of chronic pelvic pain, it really spans multiple specialties. It spans urology, colorectal, gastrointestinal, and physiatry. A lot of it is musculoskeletal pain, so a lot of it is physical therapy, orthopedics, and neurosurgical. However, for pudendal neuralgia patients, there are three distinct groups of patients. The younger group, 20-year-olds, are mostly injured in some type of athletic activity (skiers, gymnasts, cyclists, workout, etc.). The second group is slightly older, approximately mid-30s. Their most common cause of PN is traumatic vaginal childbirth. The older group often has had a mesh procedure (such as for prolapse) with the older kind of meshes.
What is your standard approach to PN patient complaints?
My protocol is that every patient that comes in gets a pelvic MRI before being seen (while doing Kegels and Valsalva). Even if seeing a physical therapist, I would have them see one associated with my practice so that the PT could take part in the patient meeting. I have my fellow take the patient history. Then we meet in my office, myself, the physical therapist, and my fellow, with MRI results, before seeing the patient. Then I meet the patient and can offer options.
How do I diagnose and treat PN?
I used to believe that the Nantes Criteria is what you had to use when diagnosing pudendal neuralgia. I recently retranslated the criteria for a textbook that is coming out soon. Patients should meet some of these criteria but don’t need to meet all of them. It just means that your pain is in the area of the pudendal nerve, but it doesn’t tell you that the nerve is entrapped. More pain with sitting is an important criterion. Having no pain at night is not true all the time, as it depends on the origin. However, this is not true with mesh origination PN.
The second part of it is the MRI. I have had very high hopes for the MRI in relation to diagnosing PN. This is not the answer for all of it. It is important, but the resolution of the PN is smaller than the MRI so that you can see the vascularization. A lot of times, you find other things than the compression of the nerve. It is a very good test to make sure that there is nothing else you are missing.
When talking about the MRI, what other diagnostic tests are helpful?
The warm threshold test, PN modern terminal latency test (you need to know the length of the nerve so it is not effective as that cannot be determined). The Pinprick test - not useful or accurate. What works best by far is the patient history, just talking to the patient. The [patient's] history is the key. What happened? The nerve can’t become entrapped on its own. If you see enough patients over the years, you can learn through experience. The MRI is valuable to make sure there is nothing else.
A pelvic exam by a qualified pelvic rehab therapist is important because it helps to rule out pelvic muscle spasms. The pain from the PN and the Obturator Levator muscle may be very similar and difficult to differentiate. Does the amount of spasms correlate with the number of symptoms/pain that they have?
You can’t treat the PN without addressing the pelvic floor. What I tell patients is this. The number one thing for repetitive injury is to stop what you’re doing. The number two thing is to choose physical therapy over anything else. By far the majority of patients are helped by appropriate pelvic floor physical therapy.
Pudendal Dysfunction: The Physician's Perspective is scheduled for January 9, 2022. Course topics include pathoanatomy and clinical presentations, basics of surgical techniques, and terminology. The latter half of the course focuses on the physician and the rehab therapist working together and features case studies and clinical pearls from Dr. Hibner, a pioneer, and leader in the field.
The interview excerpts are taken from Dr. Hibner's interview with Holly Tanner and Jessica Reale for the H&W Pelvic Floor Level 2A course pre-recorded lectures.

This blog contains an interview with Alyson N Lowrey, PT, DPT, OCS. Alyson treats the pelvic floor patient population through an orthopedic approach, working closely with pelvic floor specialists. Alyson’s clinical interests include evaluation/treatment of chronic pain, lumbar and cervical spine disorders, foot and ankle disorders, pelvic pain, and clinical instruction. Alyson is the co-instructor for the new H&W course, Pain Science for the Chronic Pelvic Pain Population - Remote Course scheduled for July 17-18, 2021.
Q: Who are you? Describe your clinical practice.
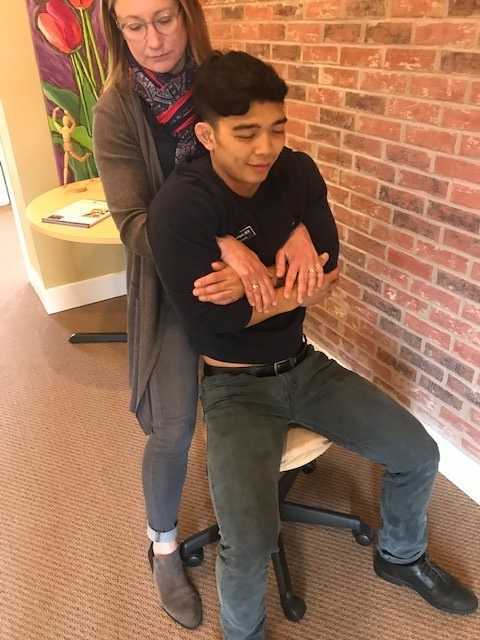
A: I work in an outpatient hospital-based clinic where I am able to provide true 1:1 care to patients of all ages and orthopedic conditions. Since pelvic floor therapy came to our clinic, I have developed strong clinical and personal relationships with pelvic floor therapists. We have been able to successfully combine our respective expertise into a wholistic approach for improving patient’s functional outcomes. My knowledge and relationships with pelvic floor therapy have allowed me as an ortho clinician to recognize when a patient’s dysfunction may have a pelvic floor component and refer appropriately. I am also in a unique opportunity where my pelvic floor colleagues will co-treat or transition care of a patient to me to continue to improve their overall function by providing functional strengthening and neuromuscular re-education to the pelvic floor musculature and other supportive muscular systems. This relationship also allows us to treat comorbid orthopedic conditions and pelvic dysfunctions such as low back pain or SIJ dysfunction as well.
Q: How did you get involved in the pelvic rehabilitation field?
A: I became involved with pelvic rehabilitation through working in a clinic with Tara Sullivan. Her knowledge is immense and our working relationship has shaped and changed how I assess patients. My practice has expanded drastically knowing so much more about pelvic floor dysfunction. I also have personal struggles with pelvic pain, which has given me a patient’s perspective as well on how important pelvic rehabilitation is.
Q: If you could get a message out to other clinicians about pelvic rehab what would it be?
A: I would encourage all ortho clinicians to educate themselves on pelvic rehab. Pelvic rehab is not yet fully integrated into our DPT curriculums and is often treated as a very separate area of dysfunction. Integrating pelvic floor function and dysfunction into my ortho world has drastically changed how I see and treat many patients.
Q: What made you want to create this course, Pain Science for the Chronic Pelvic Pain Population?
A: Tara and I wanted to create this course to help other clinicians become more proficient at treating chronic pain. A large portion of our caseloads is chronic pain both generally and with pelvic conditions. Patients with these conditions are often overlooked and not treated appropriately by the medical system at large. They are often dismissed or mislead that they have something drastically wrong with them, or worse, nothing wrong with them at all. This population often has the most functional deficits and the worst clinical outcomes. We want to change that.
Q: What need does your course fill in the field of pelvic rehabilitation?
A: There is a need in rehabilitation and medicine to understand pain from a biopsychosocial approach and to treat chronic pain conditions from that perspective. Pain is complex, and treatment is complex. Chronic pelvic pain is a subdivision of prevalent chronic pain that is not talked about or treated often enough.
Q: Who, what demographic, would benefit from your course?
A: Any clinician who treats chronic pain conditions can benefit from this course.
If you would like to learn more about chronic pelvic pain, you can join Alyson at Pain Science for the Chronic Pelvic Pain Population - Remote Course scheduled for July 17-18, 2021.
In the United States, estimated direct medical costs for outpatient visits for chronic pelvic pain (CPP) is more than $2.8 billion per year.1 In a 2017 study in the Clinical Journal of Pain by Sanses et al, a detailed musculoskeletal exam of clients with CPP can assist both physicians as well as physical therapists in differential diagnosis and appropriate referrals for this population.
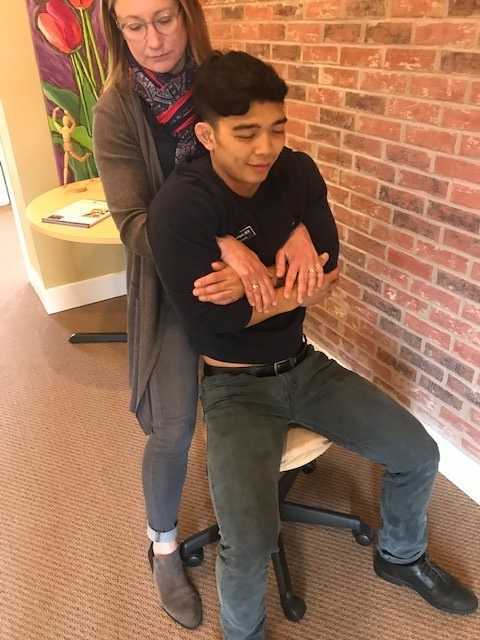
Evaluating a client with pelvic pain requires a skill set that includes direct pelvic floor as well as musculoskeletal test item clusters. The prioritization of which depends upon many factors including clinician discipline, experience, specialty vs. general setting, as well as client history, presentation and goals. In addition to the direct pelvic floor assessment, there are additional key musculoskeletal screening tests that are an essential part of a pelvic pain assessment. New this year, my course Finding the Driver in Pelvic Pain will incorporate the use of Real Time Ultrasound in neuromuscular assessment and re-education of the pelvic floor and abdominal wall during the Sunday morning lab session.
Peery et al (2012) noted that abdominal pain was one of the most common presenting reasons for an outpatient physician visit in the United States. Abdominal pain is one of the many complaints that our clients may report requiring differential diagnosis including urogynecologic, colorectal, musculoskeletal, visceral or neurogenic causes. Lower abdominal quadrant pain may denote serious emergent pathology. Clinical findings, physical exam and client symptoms in addition to smart differential diagnosis must be used to determine if the abdominal pain is musculoskeletal in nature. Direct access requires physical therapists to perform a skilled initial screening for abdominal pain in order to determine if it is abdominal wall versus a visceral origin. Physicians are fluent in ruling out emergent pathology but may not be familiar with musculoskeletal tests for non-emergent pathology. Assessment of bowel and bladder function and habits are essential to perform. This blog specifically addresses three physical exam tests that can be performed as part of abdominal wall pain screening. According to Cartwright et al, the location of the abdominal pain should drive the evaluation.
Carnett’s test is a simple clinical test that assesses abdominal pain response when a client tenses their abdominal muscles. A positive Carnett’s sign denotes the origin of symptoms within the abdominal wall with a negative tests suggesting intra-abdominal pathology. The test is performed in supine, the clinician gently palpating the area of abdominal pain and has the client lift their head and shoulders off the table. Conditions such as myofascial trigger points, scar and muscular pain would be flared with palpation of the contractile tissue with activation of the abdominal wall muscles. If the pain is due to visceral origin, appendicitis for example, the pain would remain unchanged with palpation with head lift. Although some perform Carnett’s test by lifting both legs off the table, this method may cause unnecessary pain in clients with poor lumbopelvic control. (Figure 1) The head and shoulder lift option is felt to be comparable method of performing Carnett’s test.
Blumberg’s sign is most commonly used to rule in appendicitis, peritonitis or a visceral driver of right lower quadrant pain. The test is performed by the clinician applying deep pressure over McBurney’s point (Figure 2) with an abrupt and rapid release of pressure. Although there are anatomical variations in appendix location, pain reproduction is consistent with a positive test and immediate referral to the ER is indicated.
Thoracic dysfunction, including disc herniation, can result in abdominal pain.2 In thoracic discogenic driven abdominal pain, symptoms would likely be exacerbated by coughing, sneezing, spinal flexion and activities that would increase spinal loading. A simple screening for this is seated thoracic traction. If the client reports reduction or resolution of symptoms with traction, further musculoskeletal tests including regional movement and PIVM testing could be implemented to rule in or rule out need for diagnostic imaging.
In the Herman Wallace course “Finding the Driver in Pelvic Pain” participants learn a comprehensive musculoskeletal screen including abdominal, neural mobility and conductivity, pelvic ring, pelvic floor and biomechanical contributing factors to pelvic pain. Evidence based test item clusters are defined, along with their diagnostic accuracy, for all associated systems in order to outline a comprehensive screen for pelvic pain clients. To learn more about musculoskeletal screening for pelvic pain, check out faculty member Elizabeth Hampton PT, DPT, WCS, PRPC, BCB-PMD’s course Finding the Driver of Pelvic Pain, which is next offered Jun 28, 2019 - Jun 30, 2019 in Columbus, Ohio. We are fortunate to have Dick Poore, President of The Prometheus Group present on Sunday June 30th for technical support for the Real Time Ultrasound portion of the course.
1. Sanses et al. "The Pelvis and Beyond: Musculoskeletal Tender Points in Women with Chronic Pelvic Pain". Clin. J. Pain. 2016 Aug. doi: 10.1097/AJP.0000000000000307
2. Papadakos et al. "Thoracic Disc Prolapse Presenting with Abdominal Pain: Case Report and Review of the Literature". Ann. R. Coll. Surg. Engl. 20019 Jul. doi: 10.1308/147870809X401038
Recent data suggests that there are about 4 million American women diagnosed with endometriosis, but that 6/10 are not diagnosed. Currently, using the gold standard for diagnosis there are potentially 6 million American woman that may experience the sequelae of endometriosis without having appropriate management or understanding the cause of their symptoms.
The gold standard for endometriosis is laparoscopy either with or without histologic verification of endometrial tissue outside of the uterus. However, there is a poor correlation between disease severity and symptoms. The Agarwal et al study suggests a shift to focus on the patient rather than the lesion and that endometriosis may better be defined as “menstrual cycle dependent, chronic, inflammatory, systemic disease that commonly presents as pelvic pain”. There is often a long delay in symptom appreciation and diagnosis that can range from 4-11 years. The side effects of this delay are to the detriment of the patient; persistent symptoms and effect of quality of life, development of central sensitization, negative effects on patient-physician relationship. If this disease continues to go untreated it may affect fertility and contribute to persistent pelvic pain.
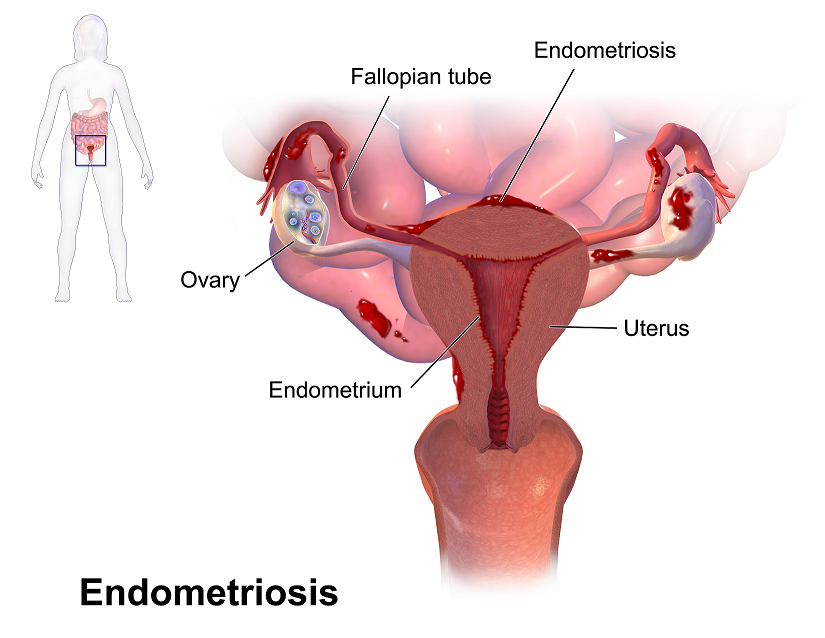 The authors suggest a clinical diagnosis with transvaginal ultrasound for patients presenting with persistent or cyclic pelvic pain, patient history, have symptoms consistent with endometriosis, or other findings suggestive of endometriosis. The intention of using transvaginal ultrasound is to make diagnosis more accessible and limit under diagnosis. It is not intended to minimize laparoscopy as a diagnostic tool or treatment option.
The authors suggest a clinical diagnosis with transvaginal ultrasound for patients presenting with persistent or cyclic pelvic pain, patient history, have symptoms consistent with endometriosis, or other findings suggestive of endometriosis. The intention of using transvaginal ultrasound is to make diagnosis more accessible and limit under diagnosis. It is not intended to minimize laparoscopy as a diagnostic tool or treatment option.
The algorithm for a clinical diagnosis evaluates patient presentation of the following:
- Symptoms including persistent or cyclic pelvic pain, dysmenorrhea or painful menstruation cramps, deep dyspareunia or pain with deep vaginal penetration, cyclic dyschezia or straining for soft stools, cyclic dysuria or pain with urination, cyclic catamenial symptoms located in other systems such as acne or vomiting.
- Assessment of patient history including infertility, current chronic pelvic pain, or painful periods as an adolescent, previous laparoscopy with diagnosis, painful periods that are not responsive to NSAIDS, and a family history.
- Physical exam physicians assess for nodules in cul de sac, retroverted uterus, mass consistent with endometriosis, visible or obvious external endometrioma. Imaging should be ordered or performed.
- Clinical signs would consist of endometrioma with US, presence of soft markers (sliding sign) this is where the fundus of the uterus is compared to its neighboring structures and can indicate the immobility of those structures, and nodules or masses.
Of course, there are differential diagnosis for endometriosis, and those are symptoms of non-cyclical patterns of pain and bladder/bowel dysfunction that would indicate IBS, UTI, IC/PBS. A history of post-operative nerve entrapment of adhesions. Examination positive for pelvic floor spasm, severe allodynia in vulva and pelvic floor, masses such as fibroids. It is important to note that these other diagnoses can coexist with endometriosis and do not rule out possible endometriosis diagnosis.
Hopefully, diagnosing individuals earlier and possibly at a younger age would limit the disease severity and symptoms. This would allow this population to limit the possibility of central sensitization and pain persistence that can affect so much of daily life. Earlier diagnosis may affect infertility and allow this population to make informed decisions about family and career from a place of empowerment.
Agarwal SK, Chapron C, Giudice LC, Laufer MR, Leyland N, Missmer SA,Singh SS, Taylor HS, "Clinical diagnosis of endometriosis: a call to action", American Journal of Obstetrics and Gynecology (2019), doi: https://doi.org/10.1016/j.ajog.2018.12.039.
Exciting news! Carolyn McManus, Herman & Wallace instructor of Mindfulness-Based Pain Treatment, will be a presenter in programming at the International Association for the Study of Pain (IASP) World Congress on Pain in to be held in Boston, September 11 - 16. This conference brings together experts from around the globe practicing in multiple disciplines to share new developments in pain research, treatment and education. Participants from over 130 countries are expected to attend. The last time it was held in the U.S. was 2002, so it presents an especially exciting opportunity for those interested in pain to have this international program taking place in the U.S. Carolyn will present a workshop on mindfulness in a Satellite Symposia, Pain, Mind and Movement: Applying Science to the Clinic.
 Carolyn has been a leader in bringing mindfulness into healthcare throughout her over-30 year career. She recognized early on in her practice how stress amplified patients’ symptoms and, as she had seen the benefits of mindfulness in her own life, it was a natural progression to integrate mindful principles and practices into her patient care. An instructor for Herman and Wallace since 2014, she has developed two popular courses, Mindfulness-Based Pain Treatment and Mindfulness for Rehabilitation Professionals, enabling her to share her clinical and research experiences with her colleagues.
Carolyn has been a leader in bringing mindfulness into healthcare throughout her over-30 year career. She recognized early on in her practice how stress amplified patients’ symptoms and, as she had seen the benefits of mindfulness in her own life, it was a natural progression to integrate mindful principles and practices into her patient care. An instructor for Herman and Wallace since 2014, she has developed two popular courses, Mindfulness-Based Pain Treatment and Mindfulness for Rehabilitation Professionals, enabling her to share her clinical and research experiences with her colleagues.
For many patients, pain is not linearly related to tissue damage and interventions based on structural impairment alone are inadequate to provide full symptom relief. Mindfulness training can offer a key ingredient necessary for a patient to make additional progress in treatment. By learning therapeutic strategies to build body awareness and calm an over-active sympathetic nervous system, patients can mitigate or prevent stress-induced symptom escalation. They can learn to move with trust and confidence rather than fear and hesitation.
A growing body of research in mindfulness-based therapies demonstrates multiples benefits for patients suffering with pain conditions. Research suggests that mindfulness training can be helpful to women preparing for childbirth and patients suffering from fibromyalgia, pelvic pain, IBS and low back pain. In addition, for patients with anxiety, mindfulness training may contribute to reductions in anxiety and in adrenocorticopropic hormone and proinflammatory cytokine release in response to stress. Authors of this study conclude that these large reductions in stress biomarkers provide evidence that mindfulness training may enhance resilience to stress in patients with anxiety disorders.
In addition to her presentation at the IASP World Congress Satellite Symposia, Carolyn will be sharing a more in-depth examination and practice of mindfulness in her upcoming course Mindfulness-Based Pain Treatment, August 4 and 5 at Virginia Hospital Center, Arlington VA, and again November 3 and 4 at Pacific Medical Center in Seattle, WA. Please join an internationally-recognized expert for 2 days of innovative training in mindfulness that will both improve your patient outcomes and enhance your own well-being!
Duncan LG, Cohn MA, Chao MT, et al. Benefits of preparing for childbirth with mindfulness training: A randomized controlled trial. BMC Pregnancy Childbirth 2017 May 12;17(1):140.
Fox SD, Flynn E, Allen RH. Mindfulness meditation for women with chronic pelvic pain: a pilot study. J Reprod Med.2011;56(3-4):158-62.
Garland EL, Gaylord SA, Paisson O. Therapeutic mechanisms of a mindfulness-based treatment for IBS: effects on visceral sensitivity, catastrophizing and affective processing of pain sensations. J Behav Med. 2012;35(6):591-602.
Cherkin DC, Sherman KJ, Balderson BH, et al. Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized Clinical Trial. JAMA. 2016;315(12):1240-9.
Hoge EA, Bui E, Palitz SA, et al. The effect of mindfulness meditation training on biological acute stress responses in generalized anxiety disorder. Psychiatry Res. 2018;262:328-332.
“Keep Calm and Treat Pain” is perhaps an affirmation for therapists when encountering patients suffering from pain, whether acute or chronic. The reality is this: treating pain is complicated. Treating pain has brought many a health care provider to his or her proverbial knees. It has also led us as a nation into the depths of the opioid epidemic which claimed over 165,000 lives between the years of 1999 and 2014 (Dowell & Haegerich, 2016). That number has swollen to over 200,000 in up-to-date calculations and according to the CDC, 42,000 human beings, not statistics, were killed by opioids in 2016 - a record.
 So why has treating pain eluded us as a nation? The answers are as complicated as treating pain itself. Which is why we as health care providers must seek out not simply alternatives, but the truth in the matter. Why are so many suffering? Why has chronic pain become the enormous beast that it has become? What might we do differently, collectively, and how might we examine this issue through a holistic mindset?
So why has treating pain eluded us as a nation? The answers are as complicated as treating pain itself. Which is why we as health care providers must seek out not simply alternatives, but the truth in the matter. Why are so many suffering? Why has chronic pain become the enormous beast that it has become? What might we do differently, collectively, and how might we examine this issue through a holistic mindset?
In just a few weeks, I have the privilege of teaching amongst 10 physical therapy professionals and one physician from around the nation who with coordinated efforts created a landmark pre-conference course at CSM in New Orleans through the Orthopaedic Section of the APTA. Included in the 11 are myself and another Herman & Wallace instructor Carolyn McManus, PT, MS, MA who teaches “Mindfulness Based Pain Treatment” through the Institute.
The CSM pre-conference course title is “Keep Calm and Treat Pain” representing a necessary effort to provide the clinician with ideas and inspiration for helping the profession as a whole treat pain with an integrative approach.
“Pain and Nutrition: Building Resilience Through Nourishment” is the section I look forward to sharing. It will introduce concepts we can leverage to allow us confidence in seeking alternate ways of taming this beast which is chronic pain - ways which can enhance health and well-being of our clients in pelvic rehabilitation. We must not be passive observers of the opioid epidemic. We must come to terms with the fact that our nations go-to tool for treating pain unfortunately causes side-effects which can and does include loss of life. We can do better. And we will.
While the CSM pre-conference course will give you a taste of the nutrition concepts available to you, it is a mere tip of the nourishment iceberg. I continue my passion and mission with the two-day course titled “Nutrition Perspectives for the Pelvic Rehab Therapist”, an experience that can elevate your conversations with clients. It will pave a path of understanding for the provider, allowing us to share options, understanding, and hope. “Nutrition Perspectives for the Pelvic Rehab Therapist is coming next to Maywood, IL March 3 & 4, 2018. I welcome you to join me.
APTA CSM: https://apta.expoplanner.com/index.cfm?do=expomap.sess&event_id=27&session_id=13763. Accessed January 8, 2018.
CDC: https://www.cdc.gov/drugoverdose/index.html. Accessed January 8, 2018.
Dowell, D., & Haegerich, T. M. (2016). Using the CDC Guideline and Tools for Opioid Prescribing in Patients with Chronic Pain. Am Fam Physician, 93(12), 970-972.
Lerner, A., Neidhofer, S., & Matthias, T. (2017). The Gut Microbiome Feelings of the Brain: A Perspective for Non-Microbiologists. Microorganisms, 5(4). doi:10.3390/microorganisms5040066
Murthy, V. H. (2016). Ending the Opioid Epidemic - A Call to Action. N Engl J Med, 375(25), 2413-2415. doi:10.1056/NEJMp1612578
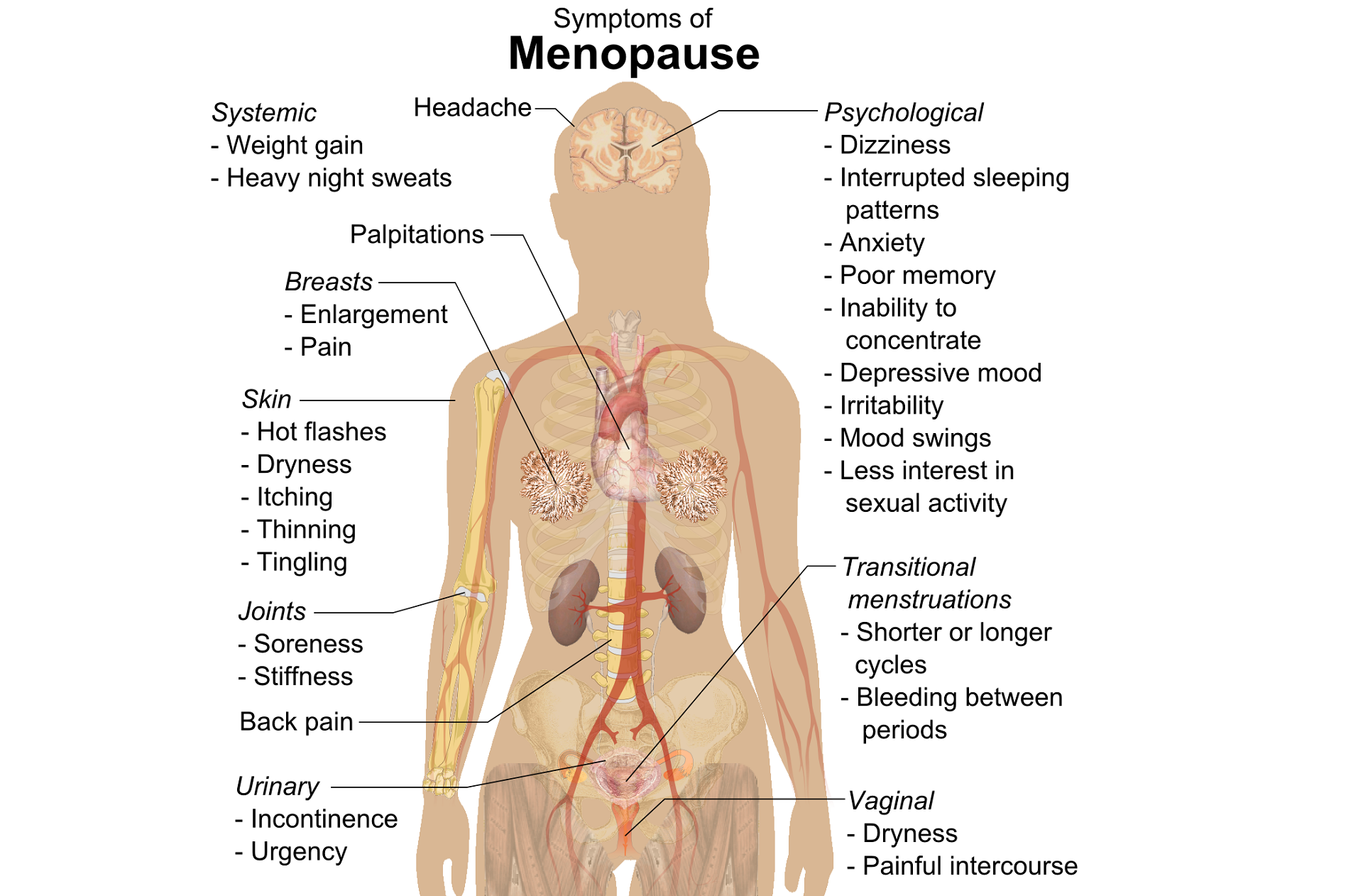
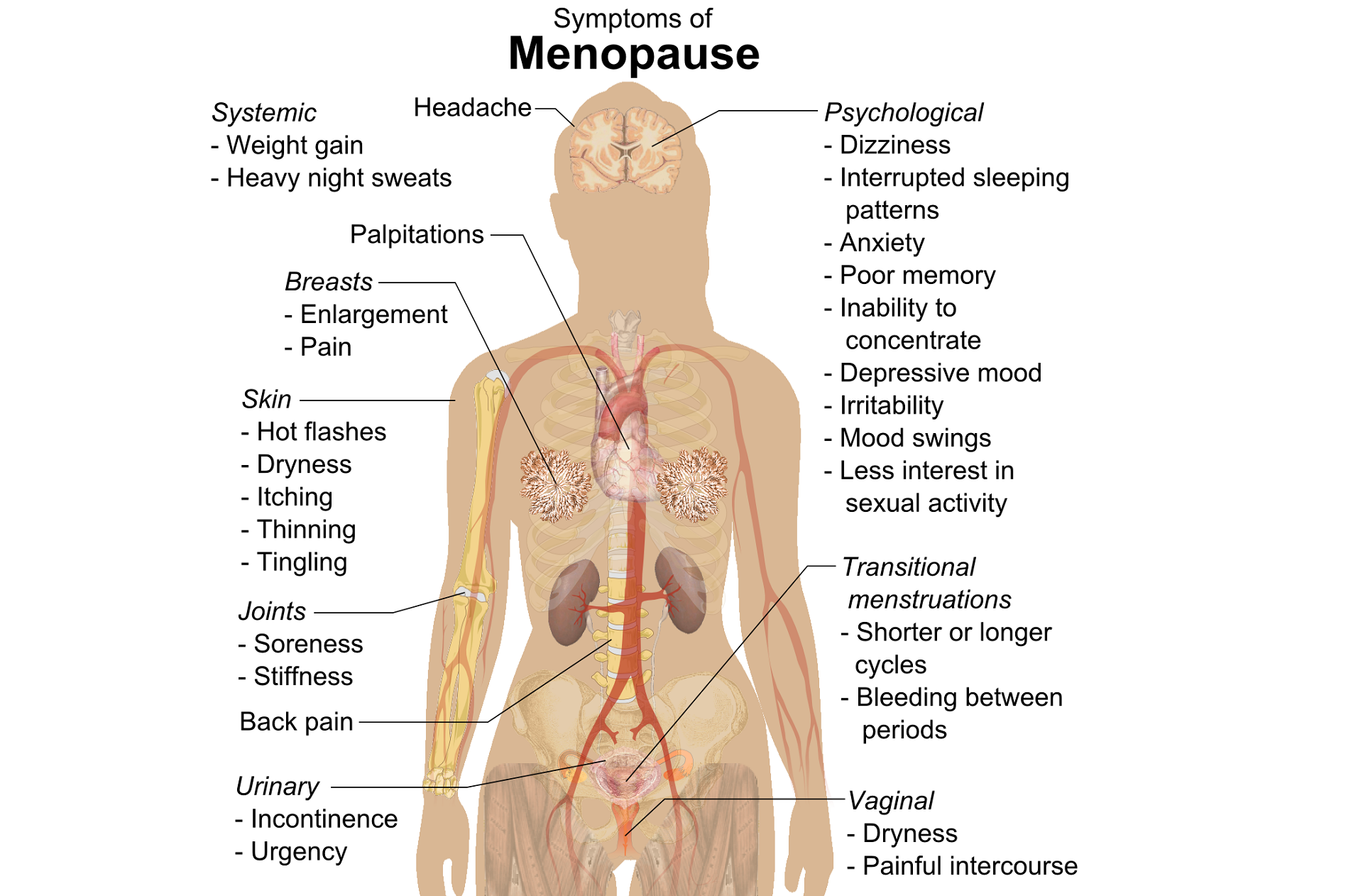
Perimenopausal pelvic health issues are, for many of us, some of the most common issues that we see in the women that we work with. Urinary incontinence is one of the most important issues for peri- and postmenopausal women. In Melville’s study1 of U.S. women, half of the participants between the ages of 50 and 90 experienced urine leakage every month. Zhu’s 2008 study2 looked at the risk factors for SUI - Multiple vaginal deliveries, Age/postmenopausal status, Chronic pelvic pain, Obesity, lack of exercise, constipation, and hypertension. But what is not often (enough) looked at in the research, is the link between urinary dysfunction and sexual dysfunction – usually because questions aren’t asked or assumptions are made. In Mestre et al’s 2015 paper3, they write ‘…Integrating sexual health in clinical practice is important. In women with pelvic floor disorders, the evaluation of the anatomical defects, lower urinary tract function and the anorectal function often receives more attention than sexual function.’
 But are they linked?
But are they linked?
In Moller’s exploration of this topic, they report that lower urinary tract symptoms (LUTS) have a profound impact on women’s physical, social, and sexual wellbeing. Unsurprisingly (to pelvic rehab specialists at least!), they found that the LUTS are likely to affect sexual activity. Conversely, sexual activity may affect the occurrence of LUTS. The aims of the Moller study were to elucidate to which extent LUTS affect sexual function and to which extent sexual function affect LUTS in an unselected population of middle-aged women in 1 year. A questionnaire was sent to 4,000 unselected women aged 40–60 years. Compared to women having sexual relationship, a statistically significant 3 to 6 fold higher prevalence of LUTS was observed in women with no sexual relationship. In women who ceased sexual relationship an increase in the de novo occurrence of most LUTS was observed. In women who resumed sexual relationship a decrease in LUTS was observed. In women whose sexual activity was unchanged no change in the occurrence of LUTS. So they rightfully concluded ‘…sexual inactivity may lead to LUTS and vice versa.’
In my Menopause course, we will explore the range of perimenopausal pelvic health issues that many women face and their inter-related nature – not just with each other but also how orthopaedic, endocrine and gastro-intestinal health issues influence pelvic health and wellness. Interested in learning more? Come and join the conversation in California in February 2018!
1. Melville JL, et al. Urinary incontinence in US women: a population-based study. Arch Intern Med 2005;165(5):537-42 - See more at: http://www.nursingcenter.com/lnc/JournalArticle?Article_ID=698029#sthash.cm8A90tS.dpuf
2. Zhu L1, Lang J, Wang H, Han S, Huang J. Menopause. 2008 May-Jun;15(3):566-9. The prevalence of and potential risk factors for female urinary incontinence in Beijing, China
3. Mestre M, Lleberia J, Pubill J, Espuña-Pons M Actas Urol Esp. 2015 Apr;39(3):175-82. Epub 2014 Aug 28. Questionnaires in the assessment of sexual function in women with urinary incontinence and pelvic organ prolapse.
Today we pick up on Jennafer Vande Vegte's interview with her patient, "Ben", about his experience overcoming chronic pelvic pain syndrome. Ben's quality of life improved so much that he has returned to school in order to become a PTA, with a focus on pelvic rehabilitation!
Describe your physical therapy experience. Talk about your recovery process. Include the physical, mental and emotional components.
 For my initial visit, my therapist questioned and assessed my pain, then explained pelvic floor dysfunction. She made sure I understood that the evaluation and treatment process involved internal rectal work. After developing the condition and months of seeing doctors who didn’t listen, finally I found a physical therapist who was actually listening to me and determined to get to the bottom of what was going on. I could tell she already knew much about the mechanics (if not the exact cause) because she had treated other patients with the same issues. I immediately sensed a difference from any other health care professional in attitude, compassion, and knowledge. Of course, how do you know for sure? Well, you don’t. But after repeated visits and excellent results, you experience the difference. An important realization while going to Physical Therapy is learning to see the mind-body connection. In the back of my mind I sensed that my pain was being perpetuated by emotional trauma. This is not an intuitive way of thinking when you are in constant high-level, 5-alarm pain. I was obsessed with finding the cause of my pain, but chronic pain is extremely elusive and complicated.
For my initial visit, my therapist questioned and assessed my pain, then explained pelvic floor dysfunction. She made sure I understood that the evaluation and treatment process involved internal rectal work. After developing the condition and months of seeing doctors who didn’t listen, finally I found a physical therapist who was actually listening to me and determined to get to the bottom of what was going on. I could tell she already knew much about the mechanics (if not the exact cause) because she had treated other patients with the same issues. I immediately sensed a difference from any other health care professional in attitude, compassion, and knowledge. Of course, how do you know for sure? Well, you don’t. But after repeated visits and excellent results, you experience the difference. An important realization while going to Physical Therapy is learning to see the mind-body connection. In the back of my mind I sensed that my pain was being perpetuated by emotional trauma. This is not an intuitive way of thinking when you are in constant high-level, 5-alarm pain. I was obsessed with finding the cause of my pain, but chronic pain is extremely elusive and complicated.
Over the course of many months of PT though we couldn’t pinpoint what started the pain, we knew my nervous system was keeping it going. Sensory signals had somehow been rerouted through pain centers in the delicate and complicated highway interstate of the nervous system. It was as if the Fed Ex truck that was supposed to carry a package from Miami to Denver got rerouted to New York, stuck in traffic in Manhattan, flipped off by cab drivers, beaten up by gang members, contents of the truck shaken up by the driver trying to flee the city, and then finally finding the way out of New York to the true destination of Denver – with damaged goods, and shaking with anxiety. As to who the idiot dispatcher was who re-routed the truck to New York, well, he’s really good at keeping himself secret and innocent-looking. Jerk!
Physical therapy, over time, began to work for me. It released trigger points which are the first step in the long process of recovery. As we know, chronic tension must be addressed in tissues and nerves, and the mind must relearn how to remain in neutral. I found that as I gained periods of relief I could see that there truly was a mind-body connection beyond what I could imagine. My physical therapist and I both knew that nerves are the slowest recovering tissue in the body, and when you combine that with an anxious mind, you have a complicated puzzle to solve. There is definitely a closed circuit that develops with chronic pelvic pain. Pain causes anxiety, anxiety causes pain and circularly they feed one another.
During my physical therapy I joined a male pelvic pain message board online. I began understanding that most men who develop pelvic pain also have experienced traumatic emotional stress. And a large part of chronic pelvic pain is rooted in a mind-body dysfunction. I had to learn how to stop thinking catastrophically, especially during flare ups. I had to trust that my body would heal and think positively. I had to learn how to relax, take care of myself, eat well, stretch and exercise daily.
When I started physical therapy, I hoped to escape the pain. My first 5 month phase of physical therapy helped to loosen the chronically tightened pelvic sphincter muscles. However, I still had allodynia. In my second phase of physical therapy I began experiencing reduction of pain for a longer duration of time. After about a year of therapy, I finally got to a point where I could see there was significant improvement, even though some intermittent pain and anxious symptoms stubbornly persisted. In late spring of 2017, I finally felt like I had conquered the pain by 98%. Occasionally flares would still come, but they were brief and nothing like before physical therapy.
How has your experience with chronic pelvic pain changed you?
CPPS has profoundly changed me. I don’t take the little things for granted or sweat them anymore. I am grateful for not feeling that horrible, hellish sensation any longer. I appreciate having my mind pain and panic free. I speak my mind while respecting my own desires instead of belittling them. I am currently in school to become a Physical Therapy Assistant as through this process I learned that I’m actually much smarter than my middle school guidance counselor thought. I understand the mind is incredibly powerful, and fear rarely has the same power over me.
How do you handle flare ups?
I now handle brief flare ups with deep breaths, meditation, and/or just taking a step back and trying to zero in on what is really bothering me. At least now I can clearly think without debilitating pain and am able to function.
What would you like to say to other people who are struggling with chronic pelvic pain?
Oh, man. For the initial duration, I would say find a safe place where you can feel as comfortable as possible until the pain lessens. When it is bad, you sort of have to give in to it. However, part of this recovery is the physical mechanics of muscle and fascia. Physical Therapy is essential in the process of recovery to release this tension. I would tell them not to give up hope. You will not find many health professionals or websites that will tell you that you can beat this and recover 100%. But I will tell you, you can recover, 100%. You can. But for now, your full-time job is to work on recovery, and that includes lots of self-care, facing possible emotional pain, and physical therapy.
If you would like to learn more about addressing the mind body connection with patients please join us for Holistic Intervention and Meditation: Boundaries, Self-Care and Dialog in January. We will be exploring ways to help our patients heal to their fullest potential as well as keeping ourselves emotionally healthy in the process. Treating patients with persistent pain can be challenging for the best of us. Please come for this three-day course where you will leave feeling refreshed, renewed and reinvigorated to treat even your most complex patient.
Additional resources:
https://www.tamethebeast.org/#home
https://www.youtube.com/watch?v=jIsF8CXouk8
http://www.sciencedirect.com/science/article/pii/S1356689X11000737
http://www.noigroup.com/en/Home
https://bodyinmind.org/who-are-we/