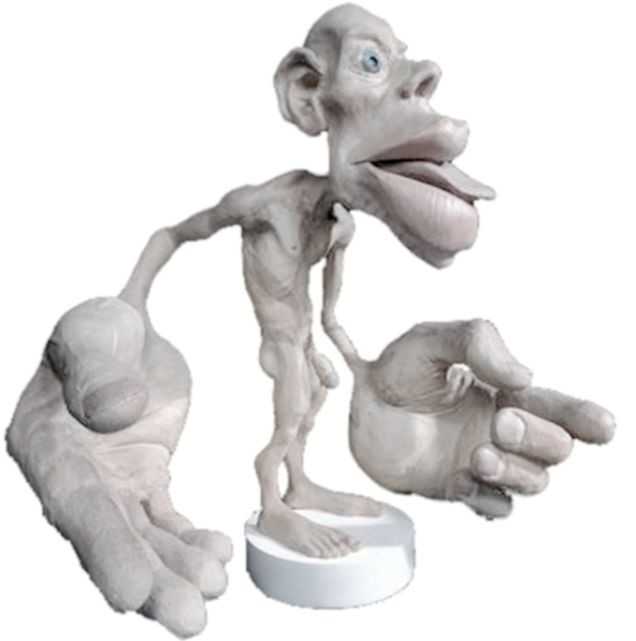
In the 16th century, a theory called Preformationism claimed that sperm contained a preformed, exceedingly minute body referred to as a homunculus, which eventually became a person. This idea of a tiny man had staying power, as today the homunculus is a “body map” based on how much of the cerebral cortex is devoted to sensing each part of the body. Although the idea of a 16th alchemist placing little bodies into a flask conjures a variety of tantalizing images, our program focuses on the mundane, contemporary version of the homunculus. So…what does this have to do with a course that addresses pelvic floor dysfunction? Everything.
 Emerging evidence indicates that therapies that include work to enhance body awareness/kinesthetic sense are potent and effective. Our professional training unfortunately, tends to over-emphasize a structural approach. The good news is that manual therapy, to some degree, enhances a client’s body awareness; but when we have more “tools” to capitalize on this synergy between manual therapy and improved body awareness, we have a potent “elixir” to promote change. To quote Deane Juhan, “touching hands are not like pharmaceuticals or scalpels…they are like flashlights in a darkened room.” By using the “flashlight”, we not only contribute to structural change, but neurological change – meaning the more we pay attention to a particular part of our body, the more “real estate” the brain devotes to that part of the body. Increasing the pelvic floor’s “footprint” on the brain can enhance function of the pelvic floor dramatically and quickly. Therefore, rehabilitation to address pelvic floor dysfunction benefits from weaving orthopedic, neurologic and mindfulness practices together.
Emerging evidence indicates that therapies that include work to enhance body awareness/kinesthetic sense are potent and effective. Our professional training unfortunately, tends to over-emphasize a structural approach. The good news is that manual therapy, to some degree, enhances a client’s body awareness; but when we have more “tools” to capitalize on this synergy between manual therapy and improved body awareness, we have a potent “elixir” to promote change. To quote Deane Juhan, “touching hands are not like pharmaceuticals or scalpels…they are like flashlights in a darkened room.” By using the “flashlight”, we not only contribute to structural change, but neurological change – meaning the more we pay attention to a particular part of our body, the more “real estate” the brain devotes to that part of the body. Increasing the pelvic floor’s “footprint” on the brain can enhance function of the pelvic floor dramatically and quickly. Therefore, rehabilitation to address pelvic floor dysfunction benefits from weaving orthopedic, neurologic and mindfulness practices together.
This program is designed to add a new dimension for the skilled pelvic floor practitioner and to also serve practitioners new to this area of practice. There is no internal manual work; rather we draw from our deep knowledge of Yoga, Tai Chi, along with other Chinese internal martial arts (that put lots of emphasis on the pelvic floor for performance) and Feldenkrais to address pelvic floor dysfunction. Some lessons focus directly on the pelvic region and others on integrating the pelvic floor with full body movement. Ultimately, our goal is to help you connect the dots between structural, functional movement and mindfulness practices, as this powerful triad offers practitioners a comprehensive, approach for treating pelvic floor dysfunction.
We hope you’ll come join in New York City on September 18th & 19th. If you do, wear comfortable clothes as the workshop is designed to provide participants opportunities to embody the work…emphasis is placed on labs more than lecture.
Don’t hesitate to contact us if you have any questions.
Bill@EastWestRehab.com
SabelNYC@Aol.com
In manual therapy training, we do not learn just one position to mobilize a joint, so why should pelvic floor muscle training be limited by the standard training methods? There is almost always at least one patient in the clinic that fails to respond to the “normal” treatment and requires a twist on conventional therapy to get over a dysfunction. Thankfully, classes like “Integrative Techniques for Pelvic Floor and Core Function” provide clinicians with the extra tools that might help even just one patient with lingering symptoms.
 In 2014, Tenfelde and Janusek considered yoga as a treatment for urge urinary incontinence in women, referring to it as a “biobehavioral approach.” The article reviews the benefits of yoga as it relates to improving the quality of life of women with urge urinary incontinence. Yoga may improve sympatho-vagal balance, which would lower inflammation and possibly psychological stress; therefore, the authors suggested yoga can reduce the severity and distress of urge UI symptoms and their effect on daily living. Since patho-physiologic inflammation within the bladder is commonly found, being able to minimize that inflammation through yoga techniques that activate the efferent vagus nerve (which releases acetylcholine) could help decrease urge UI symptoms. The breathing aspect of yoga can reduce UI symptoms as it modulates neuro-endocrine stress response symptoms, thus reducing activation of psychological and physiologic stress and inflammation associated with stress. The authors concluded the mind-body approach of yoga still requires systematic evaluation regarding its effect on pelvic floor dysfunction but offers a promising method for affecting inflammatory pathways.
In 2014, Tenfelde and Janusek considered yoga as a treatment for urge urinary incontinence in women, referring to it as a “biobehavioral approach.” The article reviews the benefits of yoga as it relates to improving the quality of life of women with urge urinary incontinence. Yoga may improve sympatho-vagal balance, which would lower inflammation and possibly psychological stress; therefore, the authors suggested yoga can reduce the severity and distress of urge UI symptoms and their effect on daily living. Since patho-physiologic inflammation within the bladder is commonly found, being able to minimize that inflammation through yoga techniques that activate the efferent vagus nerve (which releases acetylcholine) could help decrease urge UI symptoms. The breathing aspect of yoga can reduce UI symptoms as it modulates neuro-endocrine stress response symptoms, thus reducing activation of psychological and physiologic stress and inflammation associated with stress. The authors concluded the mind-body approach of yoga still requires systematic evaluation regarding its effect on pelvic floor dysfunction but offers a promising method for affecting inflammatory pathways.
Pang and Ali (2015) focused on complementary and alternative medicine (CAM) treatments for interstitial cystitis (IC) and bladder pain syndrome (BPS). Since conventional therapy has not been definitely determined for the IC/BPS population, CAM has been increasingly used as an optional treatment. Two of the treatments under the CAM umbrella include yoga (mind-body therapy) and Qigong (an energy therapy). Yoga can contribute to IC/BPS symptom relief via mechanisms that relax the pelvic floor muscle. Actual yoga poses of benefit include frog pose, fish pose, half-shoulder stand and alternate nostril breathing. According to a systematic review, Qigong and Tai Chi can improve function, immunity, stress, and quality of life. Qigong has been effective in managing chronic pain, although not specifically evidenced with IC/BPS groups. Qigong has also been shown to reduce stress and anxiety and activate the brain region that suppresses pain. The CAM gives a multimodal approach for treating IC/BPS, and this has been recommended by the International Consultation on Incontinence Research Society.
Evidence is emerging in every area of treatment these days, so it is only a matter of time before randomized controlled trials regarding alternative treatment methods for the pelvic floor begin to fill pages of our professional journals. Yoga, Qigong, Tai Chi, biologically based therapies, manipulative and body-based approaches, and whole medical systems all offer safe, effective treatment options for the IC/BPS and urinary incontinence patient populations. The more we use these extra treatment tools and document the results, the more likely we will see clinical trials proving their efficacy.
Tenfelde, S and Janusek, L. (2014). Yoga: A Biobehavioral Approach to Reduce Symptom Distress in Women with Urge Urinary Incontinence. THE JOURNAL OF ALTERNATIVE AND COMPLEMENTARY MEDICINE. 20 (10), 737–742. http://doi.org/10.1089/acm.2013.0308
Pang, R., & Ali, A. (2015). The Chinese approach to complementary and alternative medicine treatment for interstitial cystitis/bladder pain syndrome.Translational Andrology and Urology, 4(6), 653–661. http://doi.org/10.3978/j.issn.2223-4683.2015.08.10
Yoga offers a compelling mind-body approach to maternal care that is forward thinking and aligns with the World Health Organization and Institute of Medicine’s recommendations for patient-centered care. But let’s take a look at WHY postpartum care MUST change in order to establish need for the entry of yoga into postpartum care.
Maternal Health Track Record
The United States and similarly developed countries have a very poor track record for postpartum care. The record is so poor that the problem in the US has been labeled a “human rights failure.”1
 On its own, the US has the worst track record for not only postpartum care, but for maternal and infant mortality and first-day infant death rate in the developed world (Save the Children 2013). Between 1999-2008, global mortality rates decreased by 34% while the US’s rates doubled for mothers.1
On its own, the US has the worst track record for not only postpartum care, but for maternal and infant mortality and first-day infant death rate in the developed world (Save the Children 2013). Between 1999-2008, global mortality rates decreased by 34% while the US’s rates doubled for mothers.1
Patient satisfaction also suffers under the current model of care, with many more mothers experiencing postpartum depression, a significant risk factor for both mother and baby during and after pregnancy.
The increase in mortality and poor outcomes can, in part, be attributed not to underuse, but overuse of medical intervention during pregnancy and birth. 2,3,4 Countries that have “access to woman-centered care have fewer deaths and lower health care costs”; and, hospital system reviews in the US show that reducing medical interventions are both reducing cost and improving outcomes.1,4,5
The notorious lack of accountability (reporting system) in maternal health care also plagues the US and suggests that maternal deaths are even higher than currently reported, leading to Coeytaux’s conclusion that the “United States is backsliding.”1
Improving Postpartum Outcomes with Integrated Physical Therapy Care
In After the Baby’s Birth, maternal health advocate Robin Lim writes,
"All too often, the only postpartum care an American woman can count on is one fifteen minute appointment with her doctor, six weeks after she has given birth. This six-week marker ends an arbitrary period within which she is supposed to have worked out most postpartum questions for herself. This neglect of postpartum women is not just poor healthcare, it is abusive, particularly to women suffering from painful physical and/or psychological disorders following childbirth."
Physical therapists can be instrumental change agents in improving current postpartum care, especially through the integration of contemplative sciences like yoga. Yoga can be the cornerstone of holistically-driven, person-centered care, especially in comorbid conditions such as pelvic pain and depression, where pharmacological side effects, stigma, can severely diminish adherence to biomedical interventions.6 Coeytaux, as well as other authors, clearly correlate the reduction of maternal mortality with improved postpartum care. The World Health Organization recommends that postpartum checkups should include screening for:
- Back pain
- Incontinence (stress)
- Hemorrhoids
- Constipation
- Fatigue
- Breast pain
- Perineal pain
- Depression
- Painful or difficult intercourse
- Headaches
- Bowel problems
- Dizziness or fainting
 A physical therapist is a vital team member in not only screening for many of the
A physical therapist is a vital team member in not only screening for many of the
listed problems above, but in managing them. It is important to note that other countries, like France, deliver high quality postpartum rehab care plus in-home visits, all while spending far less than the US on maternal care.
The World Health Organization, however, clarifies the vital importance of postpartum care delivery by making a significant recommendation for a paradigm shift in biomedical care.7
Yoga as a “Best Care Practice” for Postpartum Care
The WHO recommends the use of a biopsychosocial model of care, which yoga is ideally suited to provide via its ancient, multi-faceted person-centered philosophy. Medical Therapeutic Yoga is a unique method of combining evidence-based rehabilitation with yoga to emerge with a new paradigm of practice. MTY:
- Addresses the mother as a person, not as a condition or diagnosis.
- Empowers mothers with self-care strategies for systems-based, not just musculoskeletal or neuromuscular, change.
- Addresses all domains of biopsychosocial impairment.
- Teaches interdisciplinary partnership-based theory, which is integral to creative collaborative discourse and innovation in postpartum care.
- Equips clinicians with business service, website development, practice paradigm, and social media campaign tools to fully develop the new clinical niche of Professional Yoga Therapy practice.
- Promotes patient advocacy, health promotion, and public health education via mainstreaming yoga into rehabilitative and medical services.
- Provides the gender context for prescription that traditional yoga is lacking.
- Evolves yoga for use in prenatal and postpartum care.
Physical therapy screening and intervention in the postpartum is vital, but the addition of yoga can optimize postpartum care and has enormous potential to be a “Best Care Practice” for postpartum care in rehabilitation.
As a mind-body intervention, yoga during pregnancy can increase birth weight, shorten labor, decrease pre-term birth, decrease instrument-assisted birth, reduce perceived pain, stress, anxiety sleep disturbances, and general pregnancy-related discomfort and quality of life physical domains.8-9
In addition to the typical physical therapy intervention for postpartum physical therapy, the MTY paradigm provides:
- self-care strategies for psychoemotional health and social engagement, increasing self-efficacy, confidence, and self-worth,
- a concise container for clinical-decision through its algorithmic programming,
- psychoemotional and neuroendocrine intervention,
- nutritional counseling and resource utilization,
- energetic adjunct therapies steeped in Ayurvedic science,
- executive functioning and cognitive support,
- epigenetic effect, and
- inter- and intrarelational development.
Postpartum integrated physical therapy care can provide more comprehensive care than rehab alone because of its multi-faceted biopsychosocial structure and systems-based model of care. Ginger’s course, Yoga as Medicine for Labor, Delivery, and Postpartum provides evidence-based methodology for prenatal and postpartum practice that streamlines clinical decision-making and intervention through introduction of a yogic model of assessment.
To learn more about Ginger’s course, visit Yoga as Medicine for Labor, Delivery, and Postpartum
Coeytauz et al., Maternal Mortality in the US: A Human Rights Failure. Contraception Editorial, March 2011. http://www.arhp.org/publications-and-resources/contraception-journal/march-2011
Kuklina E, Meikle S, Jamieson D, et al. Severe obstetric morbidity in the US, 1998–2005. Obstet Gynecol. 2009;113:293–299.
Tita ATN, Landon MB, Spong CY, et al. Timing of elective cesarean delivery at term and neonatal outcomes. NEJM. 2009;360:111–120.
Clark SL, Belfort MA, Byrum SL, Meyers JA, Perlin JB. Improved outcomes, fewer cesarean deliveries, and reduced litigation: results of a new paradigm in patient safety. Am J Obstet Gynecol. 2008;199:e1–105.e7.Abstract | Full Text | Full-Text PDF (100 KB)
Oshiro BT. Decreasing elective deliveries before 39 weeks of gestation in an integrated health care system. Obstet Gynecol. 2009;113:804–811.
Buttner, M. M., Brock, R. L., O'Hara, M. W., & Stuart, S. (2015). Efficacy of yoga for depressed postpartum women: A randomized controlled trial. Complementary Therapies in Clinical Practice, 21(2), 94-100. doi:10.1016/j.ctcp.2015.03.003 [doi]
WORLD HEALTH ORGANIZATION., 2002. Towards a common language for functioning, disability and health : ICF. Geneva: World Health Organisation.
Curtis, K., Weinrib, A., & Katz, J. (2012). Systematic review of yoga for pregnant women: Current status and future directions. Evidence-Based Complementary and Alternative Medicine : ECAM, 2012, 715942. doi:10.1155/2012/715942 [doi]
Sharma, M., & Branscum, P. (2015). Yoga interventions in pregnancy: A qualitative review. Journal of Alternative and Complementary Medicine (New York, N.Y.), 21(4), 208-216. doi:10.1089/acm.2014.0033 [doi]
I lived in Seattle during my pregnancies, where practicing yoga is almost as common as drinking coffee. I never accepted my friends’ invitations to partake in a perinatal yoga classes, mostly because I do not know how to do it, and I simply ran instead. My friends reaped the benefits of the meditation and strengthening involved when it came to delivering their babies. Researchers have been trying to measure the physical benefits from performing yoga during pregnancy, both for the mother and the fetus, and scientifically support the efficacy of participating in peripartum yoga.
 In a systematic review of studies regarding yoga for pregnant women, Curtis, Weinrib, and Katz (2012) explored the literature on yoga for pregnancy. Six studies were included in the review, only 3 of which were randomized controlled trials. The aspects of yoga included in the trials were postures, breathing practices, meditation, deep relaxation, counseling on lifestyle change, and chanting and anatomy information. The programs in the trials began either between 18-20 weeks gestation or between 26-28 weeks. The yoga was practiced either 3 times per week for 30-60 minutes or 60 minutes daily. Control groups included walking, standard prenatal exercise, or general nursing care. The literature review suggested improvements were noted regarding quality of life and self-efficacy, discomfort and pain during labor, and birth weight and preterm births. Due to the limited number of trials, only a general positive commendation of yoga during pregnancy could be made from this research.
In a systematic review of studies regarding yoga for pregnant women, Curtis, Weinrib, and Katz (2012) explored the literature on yoga for pregnancy. Six studies were included in the review, only 3 of which were randomized controlled trials. The aspects of yoga included in the trials were postures, breathing practices, meditation, deep relaxation, counseling on lifestyle change, and chanting and anatomy information. The programs in the trials began either between 18-20 weeks gestation or between 26-28 weeks. The yoga was practiced either 3 times per week for 30-60 minutes or 60 minutes daily. Control groups included walking, standard prenatal exercise, or general nursing care. The literature review suggested improvements were noted regarding quality of life and self-efficacy, discomfort and pain during labor, and birth weight and preterm births. Due to the limited number of trials, only a general positive commendation of yoga during pregnancy could be made from this research.
In 2015, Jiang et al. looked at 10 randomized controlled trials from 2004 to 2014 regarding yoga and pregnancy. The authors found consistent evidence showing a positive correlation between yoga intervention and lower incidence of prenatal disorders and small gestational age. Lower levels of stress and pain as well as higher relationship scores were noted with yoga. The studies showed yoga to be a safe and effective means of exercise during pregnancy, but the authors agreed further randomized controlled studies still need to be performed.
A 2015 randomized control trial by Rakhshani et al. examined the effect of yoga on utero-fetal-placental circulation during pregnancy considered high-risk. The yoga group consisted of 27 women who received standard care plus 60 minute yoga sessions 3 times per week and practice at home. The control group included 32 women who received standard care and walked 30 minutes in the morning and evening. The intervention began at the 13th week of gestation and concluded at the end of the 28th week. Yoga intervention involved yoga postures, relaxation and breathing exercises, and visualization with guided imagery. The authors conceded larger studies need to be performed to confirm the results of their randomized controlled trial; however, they concluded yoga visualization and guided imagery can significantly improve uteroplacental and fetoplacental circulation.
Although further studies are needed to make evidence-based claims regarding yoga during pregnancy, the general consensus deems yoga appropriate and safe. As with any exercise program, a tailored approach for each individual is prudent. Yoga includes many components, and current trials consistently indicate the visualization/imagery aspect is safe and beneficial during pregnancy, even when high risk. In retrospect, when I had placenta previa, perhaps I should’ve traded my running shorts for yoga pants!
Curtis, K., Weinrib, A., & Katz, J. (2012). Systematic Review of Yoga for Pregnant Women: Current Status and Future Directions. Evidence-Based Complementary and Alternative Medicine : eCAM, 2012, 715942.
Jiang Q, Wu Z, Zhou L, Dunlop J, Chen P. (2015). Effects of yoga intervention during pregnancy: a review for current status. American Journal of Perinatology. 32(6):503-14..
Rakhshani, A., Nagarathna, R., Mhaskar, R., Mhaskar, A., Thomas, A., & Gunasheela, S. (2015). Effects of Yoga on Utero-Fetal-Placental Circulation in High-Risk Pregnancy: A Randomized Controlled Trial. Advances in Preventive Medicine, 2015, 373041.
Faculty member, Ginger Garner PT, L/ATC, PYT will be giving 2 lectures at this year’s annual Montreal International Symposium for Therapeutic Yoga, or MISTY for short, in Montreal, Quebec. The first is a 2-hour lecture titled, Vocal Liberation, and the second is a 4-hour lecture titled, Hip Preservation: Yoga Reconsidered, Visit http://www.homyogaevents.com to learn more.
 Yoga is, unarguably, a popular contemplative science, enjoying 36.7 million practitioners in the US alone, up from 20.4 million in 2012.1 A 16 billion dollar industry, yoga is one of the most widely utilized methods of complementary and integrative medicine in America today. In 2008, the editor of Yoga Journal declared “yoga as medicine” as the next great wave. That was right in the middle of the Great Recession, when the last thing on the collective healthcare industry’s mind was yoga.
Yoga is, unarguably, a popular contemplative science, enjoying 36.7 million practitioners in the US alone, up from 20.4 million in 2012.1 A 16 billion dollar industry, yoga is one of the most widely utilized methods of complementary and integrative medicine in America today. In 2008, the editor of Yoga Journal declared “yoga as medicine” as the next great wave. That was right in the middle of the Great Recession, when the last thing on the collective healthcare industry’s mind was yoga.
What happened during the same time frame as the interest in yoga surged?
Our expanded knowledge of hip anatomy, physiology, and pathophysiology exploded onto the medical scene, providing more information than ever about how to address, preserve, and otherwise attend to the hip joint. Prior to this new age of research, the hip was relegated to a joint worthy of no more than a tendonitis, bursitis, or osteoarthritis diagnosis. A person was simply a hip replacement candidate or not. There was no other option once a hip joint had prematurely degenerated. Now, that has all changed, thanks to technological advances in diagnostic testing and investigation.
Yet, the worlds of hip preservation and rehabilitation and yoga have yet to join hands. Many of my patients and colleagues have suffered from unnecessary hip injuries, from labral tears, all types of impingement, and compounding secondary diagnoses such as torn hamstrings, sports hernias, gluteal tendinopathy, to pelvic pain, all due to yoga practice. Some suffered injuries in yoga class during a single traumatic injury, and some injuries were drawn out over years of accumulated microinjury to capsuloligamentous, bony, or cartilaginous structures.
Hip labral injuries (HLI) have vastly increased over the last 10 years, perhaps making HLI the newest orthopaedic diagnosis of the 21st century. This discovery also makes surgical and conservative management of HLI uncharted territory. Conservative therapy includes nonsurgical and post-surgical rehabilitation, and since the average time from injury to diagnosis is 2.5 years, there are many people with hip, pelvic, back, or sacroiliac joint pain that have undiagnosed hip labral tears.
I should make myself quite clear, however. I am not out to demonize yoga or fear-monger the practice of yoga or how it may wreck a person’s body (to use recently controversial language).
My purpose is two-fold: To clarify 1) “what” and “how” yoga can be a safe, effective form or physical therapy and rehabilitation for the hip and pelvis, as well as to 2) underscore the areas where yoga posture practice should be evolved to prevent injury.
To that end, I have written and will be presenting a new 4-hour workshop entitled, Hip Preservation: Yoga Reconsidered, at the Montreal International Symposium on Therapeutic Yoga (MISTY) this weekend in Canada. The lecture is relevant for yoga teachers, yoga enthusiasts, yoga therapists, and health care professionals who are interested in learning how to prevent hip injury in yoga practice.
The workshop will introduce identification of imbalances that could contribute to HLI, as well as understand the common mistakes made in yoga practice that could increase HLI or hip impingement. Understanding the pain patterns that surround HLI are also critical to safe and therapeutic yoga practice and will be discussed. Discussion of structure, function, ability and “dis”ability of the hip, including their major substrates, will help identify the “red flags” in yoga practice, identifying high risk populations and those who need postural modification(s) and/or outside referral to physical therapy.
I am looking forward to instructing a high energy, action-packed hands-on learning session at MISTY on March 19-20, along with my presenting a 2-hour lecture on maximizing public speaking impact through Vocal Liberation: The Voice as Therapy.
- The Voice as a Linking Science for Clinical and Business Efficacy
- Hip Preservation: Yoga Reconsidered
- Ginger’s lecture overview - Montreal International Symposium for Therapeutic Yoga
Want to learn more?
Bring Ginger’s 16 hour continuing education course, Differential Diagnosis for Hip Labral Injuries to your facility in 2017 through Herman & Wallace Pelvic Rehabilitation Institute.
Yoga in America 2016 Survey. Yoga Alliance and Yoga Journal. January 2016.
Depression and anxiety can limit ability to care for one’s self, limit ability to care for a new baby or developing fetus, and can cause mood swings, impaired concentration, and sleep disturbance. Disorders of depression and anxiety are common in the perinatal period (immediately before and after birth) with depression rates around 20% and perinatal anxiety present in about 10% of women. These mood disorders greatly diminish quality of life for mother and baby. Medication may be effective, however, side effects are often unknown, and potentially adverse for the perinatal patient. Many women worry that using medication to treat these disorders may harm the fetus, negatively affect mother child bonding, and poorly influence child development. As health care providers, being aware of alternative treatments for depression and anxiety is essential. Having alternative treatments can allow our patients to combat these common perinatal problems which will improve quality of life, improve bonding between baby and mother and improve the overall perinatal experience. In the general population, positive mental and physical health benefits have been continually demonstrated by yoga participants in current research. Can yoga be an effective, alternative treatment to help perinatal patients improve mental health and well-being?
 A recent 2015 systematic literature review published in the Journal of Holistic Nursing reviewed 13 studies to examine existing empirical literature on yoga interventions and yoga’s effects on pregnant women’s health and well-being. The conclusion of the review found that yoga interventions were generally effective at reducing depression and anxiety in perinatal women and the decrease in depression and anxiety was noted regardless of the type of outcome measure used and results were optimized when the study was 7 weeks or longer. Other positive secondary findings noted with the regular yoga participation in the perinatal participants were: improvements in pain, anger, stress, gestational age at birth, birth weight, maternal-infant attachment, power, optimism, and well-being. What is yoga and what form of it may help battle perinatal depression and anxiety?
A recent 2015 systematic literature review published in the Journal of Holistic Nursing reviewed 13 studies to examine existing empirical literature on yoga interventions and yoga’s effects on pregnant women’s health and well-being. The conclusion of the review found that yoga interventions were generally effective at reducing depression and anxiety in perinatal women and the decrease in depression and anxiety was noted regardless of the type of outcome measure used and results were optimized when the study was 7 weeks or longer. Other positive secondary findings noted with the regular yoga participation in the perinatal participants were: improvements in pain, anger, stress, gestational age at birth, birth weight, maternal-infant attachment, power, optimism, and well-being. What is yoga and what form of it may help battle perinatal depression and anxiety?
Yoga by definition is a Hindu philosophy that teaches a person to experience inner peace by controlling the mind and body. Merriam-Webster defines yoga as a system of exercises for attaining bodily or mental control and well-being. All styles of yoga include some combination of physical poses, breathing techniques, and meditation-relaxation techniques. Hatha yoga is the most common form completed in the United States and consists modernly of various postures, breathing, and meditation. In the 13 reviewed studies, all interventions consisted of different forms of yoga and the overall conclusion of the systematic review was the decrease in depression and anxiety was significant no matter the form of yoga completed. Physical and emotional issues such as hormonal changes, sleep deprivation, inability to handle new tasks, self-worth, and body issues, during the perinatal period can contribute to increased anxiety and depression. As health care providers we need to have alternative treatments to help our perinatal patients’ battle depression and anxiety. Yoga is a promising alternative to medication to help decrease depression and anxiety. Additionally it may be helpful for management of pain, anger, stress, gestational age at birth, birth weight, maternal-infant attachment, power, optimism, and well-being.
Interested in learning more about how you can apply therapeutic yoga in your practice? Check out "Yoga as Medicine for Pregnancy this April in Washington, DC!
Sheffield, K. M., & Woods-Giscombé, C. L. (2015). Efficacy, Feasibility, and Acceptability of Perinatal Yoga on Women’s Mental Health and Well-Being A Systematic Literature Review. Journal of Holistic Nursing, 0898010115577976.
Herman & Wallace Pelvic Rehabilitation Institute faculty member, Ginger Garner PT, L/ATC, PYT, will be giving 2 lectures at this year’s annual Montreal International Symposium for Therapeutic Yoga, or MISTY for short, in Montreal, Quebec. The first is a 2-hour lecture titled, Vocal Liberation, and the second is a 4-hour lecture titled, Hip Preservation: Yoga Reconsidered, Visit http://www.homyogaevents.com to learn more. Read below as Ginger shares why the voice is a linking science.
The Voice as a Linking Science for Clinical and Business Efficacy
 Your voice can be the key to your success. Forbes magazine’s #3 habit in an article, Five Habits of Highly Effective Communicators, is “Find your own voice.” London’s think tank Tomorrow’s Company declares in a recent report on efficacy in business leadership, “Having a voice really matters for employees today.” The director of the Involvement and Participation Association (IPA) and vice-chair of the London-based MadLeod Review on employee engagement says, “Voice is extremely important because there are many changing business concepts and one of the essential ones is trust. Our voice is one of the things we really need to change old management paradigms and build trust in an organization.”
Your voice can be the key to your success. Forbes magazine’s #3 habit in an article, Five Habits of Highly Effective Communicators, is “Find your own voice.” London’s think tank Tomorrow’s Company declares in a recent report on efficacy in business leadership, “Having a voice really matters for employees today.” The director of the Involvement and Participation Association (IPA) and vice-chair of the London-based MadLeod Review on employee engagement says, “Voice is extremely important because there are many changing business concepts and one of the essential ones is trust. Our voice is one of the things we really need to change old management paradigms and build trust in an organization.”
If you are an instructor, teacher, educator, therapist, or all four, having a voice is synonymous with having a job. You can’t do your job without a voice. And yet, we don’t spend much time thinking about vocal physiology, much less how to maintain and even improve it.
The most powerful change agent or therapeutic modality you have - is your voice. Yet, the voice is often overlooked as a therapeutic tool. Think of how important it is for someone giving a TED talk to have good vocal quality, for example. Now consider how important it is for others, like you, who may have to speak for hours on end each day. The vocal folds must be cared for just like we attend to the mind and body during postural yoga practice or movement therapy.
What were the other findings of the report?
- Voice is the foundation of sustainable business success. It increases employee engagement, enables effective decision-making and drives innovation.
- Finding your voice involves both cultural and structural pursuit. First, we need to be culturally competent and sensitive. Only then can we provide the right process through which our voice can be heard.
The power of the voice cannot be ignored, particularly for those who have allergies, respiratory issues, or struggle to make a powerful impact or to establish themselves as an effective team member or thought leader. Oftentimes, the voice is the single variable that holds us back from making the success we are seeking in our work. US News World and Report states,
“Whether you are an aspiring leader or in a support role, developing your communication skills can impact your success. First, let’s take a look at the complexities of communication. It's more than the words you use. It's how and when you choose to share information. It's your body language and the tone and quality of your voice.”
Psychology Today and National Public Radio have recently reported on the relationship between vocal quality and job success and effectiveness. Both agree that speech rate, tone of voice, facial expression, and diction have a great deal of power to make or break effective communication. If tone doesn’t match facial expression, for example, neural dissonance occurs, which erodes trust, increase skepticism, and cooperation.1 In fact, warm vocal tone is a sign of transformational leadership, which generates “more satisfaction, commitment, and cooperation between team members”.2 Changing pitch increases therapeutic potential and improves the chances of your being understood by colleagues, especially when diction is congruent with emotion.1 Additionally, training mindfulness during public speaking can improve prefrontal cortex activity, which allows for improved social awareness, mood-regulation, decision-making, and empathy.4 Vocal awareness and training can slow your pace of speaking, which is shown to deepen others’ respect for you and simultaneously calm anxiety, traits which are bridge-building and healing for all relationships, business and personal.
About MISTY
MISTY is a not-for-profit organization and event dedicated to teaching others about therapeutic yoga.
Ginger’s workshop, “Vocal Liberation,” will introduce techniques for developing and preserving the voice, including projection, quality, longevity, and therapeutic impact through fusion of nada yoga and ENT physiology, which Ginger has developed over her career in public speaking and vocal performance. Want to learn about therapeutic yoga at MISTY? There’s still time to join Ginger and a host of other talented speakers and therapists. Learn more and register at http://www.homyogaevents.com.
Use of affective prosody by young and older adults. Dupuis K, Pichora-Fuller MK. Psychol Aging. 2010 Mar;25(1):16-29.
Leadership = Communication? The Relations of Leaders' Communication Styles with Leadership Styles, Knowledge Sharing and Leadership Outcomes. de Vries RE, Bakker-Pieper A, Oostenveld W. J Bus Psychol. 2010 Sep;25(3):367-380.
Short-term meditation training improves attention and self-regulation. Tang YY, Ma Y, Wang J, Fan Y, Feng S, Lu Q, Yu Q, Sui D, Rothbart MK, Fan M, Posner MI. Proc Natl Acad Sci U S A. 2007 Oct 23;104(43):17152-6.
 We know that many of our patients who struggle with severe pelvic pain need rehabilitation efforts directed towards quieting of the nervous system. In general, activation of the parasympathetic system is a goal, with targeted physiologic improvements in heart rate, respiration, and blood pressure, for example. Many providers are teaching patients physiologic quieting techniques such as breathing, mindfulness strategies, visualization, meditation, and encouraging activities like yoga. Does yoga really affect the nervous system? To assess the ability of yoga to increase cardiac parasympathetic nervous system modulation, a study published in Evidence-Based Complementary and Alternative Medicine examined the effects of yoga practice on physiologic variables.
We know that many of our patients who struggle with severe pelvic pain need rehabilitation efforts directed towards quieting of the nervous system. In general, activation of the parasympathetic system is a goal, with targeted physiologic improvements in heart rate, respiration, and blood pressure, for example. Many providers are teaching patients physiologic quieting techniques such as breathing, mindfulness strategies, visualization, meditation, and encouraging activities like yoga. Does yoga really affect the nervous system? To assess the ability of yoga to increase cardiac parasympathetic nervous system modulation, a study published in Evidence-Based Complementary and Alternative Medicine examined the effects of yoga practice on physiologic variables.
Cardiac vagal modulation was the primary variable assessed in this study; ambulatory 24-hour Holter monitoring, with heart rate variability (HRV) identified hourly by a blinded observer, was the method used to collect data. (The authors explain that this is an established tool to measure HRV, and that HRV can be used as a predictor of cardiac mortality and sudden cardiac death.) Eleven healthy yoga practitioners (4 men and 7 women) completed 5 sessions of training. All of the subjects had at least 3 years of experience practicing Iyengar yoga, and some of the subjects were certified Iyengar instructors. During 2 of the sessions, subjects were trained for 90 minutes, once per week, for 5 weeks. During 2 of these sessions, the subjects practiced a yoga session developed by B.K.S. Iyengar for cardiac patients, and during the other 3 sessions, they practiced a placebo relaxation session. The yoga program started with 15 minutes of resting poses, 60 minutes of standing poses, backbends, inverted poses, and ended with 15 minutes of resting poses. (The yoga sequence is listed in the linked article.) The yoga practitioners were matched to a healthy group of volunteers not practicing any relaxation techniques and instead participating in a placebo program. The placebo program included 15 minutes of resting on the floor, 60 minutes walking in a park, followed by another 15 minutes resting on the floor.
Results of the monitoring indicated that heart rate variability was significantly higher during the yoga intervention. The authors conclude that “…relaxation by yoga training is associated with a significant increase of cardiac vagal modulation.” Recommended as an easy-to-apply, no side effects intervention for cardiac rehabilitation programs, it seems that yoga could be beneficial for many patients with different conditions and in various practice settings. The yoga applications can be modified with props and by sequence of yoga postures to account for patient’s level of health. Finding yoga instructors who are capable of adapting yoga to a patient’s specific needs is also important, and if you would like to learn more about yoga applications in rehabilitation, the Institute has several courses that you may find helpful.
Herman & Wallace has several courses available for practitioners who want to start implementing these tools into their practice. Yoga for Pelvic Pain discusses the positive effects of yoga on interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia, and it includes the instruction of many poses/techniques. The next opportunity to take this course is next month, September 12-13 in Boston, MA.
Michelle Lyons is instructor of "Oncology and the Female Pelvic Floor: Female Reproductive and Gynecologic Cancers", among other Herman & Wallace courses. We thought you might like to hear her expert analysis of current research going on in the field of gynecologic oncology, and the benefits therapeutic yoga can have on patient rehabilitation. Take it away, Michelle!

More than 65,000 women are diagnosed with gynecologic cancers (vulvar, vaginal, cervical, ovarian, endometrial) in the United States each year (Sohl et al 2012). Treatment options for these women include surgery, chemotherapy, radiation and hormone therapy – all of which have the potential to have local, regional and global effects on a woman’s body. The pelvic rehab specialist is in a unique position to hugely improve quality of life issues for these women – dealing with issues directly associated with pelvic health (urinary, sexual and bowel function and dysfunction) as well as more global issues such as bone health, peripheral neuropathies and musculoskeletal dysfunctions.
Yoga has enormous potential as a therapeutic tool for gynecologic cancer survivors and as exercise prescription experts, we can add yoga as a multi-purpose tool to our skill-set.
Empirical research on therapeutic yoga has been ongoing for several decades, including several recent studies conducted with cancer patients and survivors. Although most of the research looking at the benefits of yoga for cancer survivors has been done in the context of breast and prostate cancers, we can safely extrapolate many of the benefits associated with oncology rehab yoga, including its immediately obvious ability to improve flexibility, strength, balance, but also the impact yoga can have on decreasing inflammation, improving sleep and raising quality of life scores in pelvic cancer survivors.
Recent papers by Dewhirst et al showed how moderate exercise can improve the efficacy of chemotherapy and radiation by decreasing tumour hypoxia – they also discovered that this may limit metastatic aggression.
We also know that exercise can be potent medicine when it comes to dealing with the effects of cancer treatments, especially fatigue, bone health and cardiovascular function, which may disrupt return to exercise (Kerry et al 2005). But pelvic cancer patients may face extra barriers when it comes to returning to exercise, such as pelvic pain and concerns about continence, as well as diminished flexibility, balance and strength. But as Blaney et al concluded in their 2013 paper ‘…however, the main barriers reported were those that had the potential to be alleviated by exercise.’ And in my opinion, this can be achieved by integrating yoga into our pelvic oncology rehab programs.
These recent and exciting research findings have encouraged me to add a therapeutic yoga lab session to my Oncology & the Pelvic Floor course, which I will be teaching in NY next month. This is the last chance to catch this course stateside this year so I hope you will join me in White Plains to explore the many ways we can make a serious impact on pelvic cancer survivorship (Bring your yoga mat!)
References:
Psychooncology. 2013 Jan;22(1):186-94.
Cancer survivors' exercise barriers, facilitators and preferences in the context of fatigue, quality of life and physical activity participation: a questionnaire-survey. Blaney JM1, Lowe-Strong A, Rankin-Watt J, Campbell A, Gracey JH.
Annals of Behavioral Medicine
April 2005, Volume 29, Issue 2, pp 147-153
A Longitudinal Study of Exercise Barriers in Colorectal Cancer Survivors Participating in a Randomized Controlled Trial
Kerry S. Courneya Ph.D., Christine M. Friedenreich Ph.D., H. Arthur Quinney Ph.D., Anthony L. A. Fields M.D., Lee W. Jones Ph.D., Jeffrey K. H. Vallance M.A., Adrian S. Fairey M.Sc.
JNCI J Natl Canc
Allison S. Betof, Christopher D. Lascola, Douglas H. Weitzel, Chelsea D. Landon, Peter M. Scarbrough, Gayathri R. Devi, Gregory M. Palmer, Lee W. Jones, and Mark W. Dewhirst
Modulation of Murine Breast Tumor Vascularity, Hypoxia, and Chemotherapeutic Response by Exercise
Today we are fortunate to hear from Barbara S. Rabin MSPT ATC PYTc, owner and practitioner at Holistic Physical Therapy in Gates Mills, OH. Barbara has more than 20 years of experience in orthopedic rehabilitation. Her perspective as an athletic trainer and orthopedic therapist highlights the many approaches practitioners can take when working with pelvic rehabilitation patients.
"We were reminded how all the muscles of the hip are intricately integrated into the pelvic floor and one can’t ignore the influence and interaction they have on each other."
My physical therapy career has been in the world of outpatient orthopedics and sports medicine. While in physical therapy graduate school I became a nationally certified athletic trainer, and most of my post graduate CEU’s have been in the orthopedic and sports medicine arena.
Stepping Outside the Comfort Zone
As an orthopedic PT, it was “safe” to study the pelvic girdle when I took Richard Jackson’s continuing education course in 1994 because it focused on muscles, ligaments, bones and nerves. However, I was leaving “safe territory” when I took Janet Hulme’s course, “Beyond Kegels: Evaluation and Treatment of Pelvic Muscle Dysfunction and Incontinence” in 1998. Long ago, back in gross anatomy lab in physical therapy school, we barely looked at the pelvic floor contents. Yes, we identified the digestive system but basically ignored all of the rest. Our mission was mostly to learn the muscles, ligaments, bones and nerves. After Janet Hulme’s course, I tried to offer incontinence rehabilitation at my place of employment at the time, but the idea was quickly dismissed. However, I am very glad to say that pelvic floor rehab is now commonly offered at most major hospitals and many clinics.
I continued my education of the pelvis and hip in several other courses and especially enjoyed one I attended last year called, "Extra-Articular Pelvic and Hip Labrum Injury: Differential Diagnosis and Integrative Management" by the Herman & Wallace Pelvic Rehabilitation Institute and taught by Ginger Garner PT ATC PYT. We were reminded how all the muscles of the hip are intricately integrated into the pelvic floor and one can’t ignore the influence and interaction they have on each other.
I was intrigued and wanted to learn more about the pelvic floor. I got another opportunity when I most recently attended an intimidating course for an “orthopedic sports medicine physical therapist” called, “Mobilization of Visceral Fascia for the Treatment of Pelvic Dysfunction - Level 1: The Urinary System” taught by Ramona Horton, MPT. I learned that externally mobilizing the bladder can often increase hip extension. Here was a combining of the fascial, pelvic floor, and orthopedic worlds!
Myofascial Release and Other Manual Therapy
I learned several manual therapy techniques in courses, and I took the best out of many but never specialized. As of late, I have been gladly drawn into the world of John F Barnes myofasical release. Studying and working with the fascia coincides with my holistic approach of rehabilitation, since the fascia is intricately woven throughout our body. The fascia was another thing we ignored in gross anatomy lab in physical therapy school. It was cut to move it out of the way so we could “get to the important stuff.” Even in that dead and embalmed state, the fascia was fascinating. It was strong and flexible at the same time. Now, with the advent of micro discography of the fascia by Dr. Jean-Claude Guimberteau (http://www.guimberteau-jc-md.com/en/biographie.php) we can view fascia in its live state and we can really see the phenomenal structure that it truly is.
Incorporating Yoga into Rehabilitation Practices
About eight years ago I took my first yoga class. I thought I was a conditioned athlete as a lifelong runner but I was humbled as I could not even balance on one leg for a minute. I noticed the physical and emotional benefits in myself and wanted to include yoga in the treatment of my patients. I had a patient who had physical issues from an eating disorder and needed supervision to exercise. I thought to myself that what she needed was not physical therapy but possibly meditation and relaxation. Even though I didn’t learn those techniques in PT school, I felt that I should be able to offer them to my patients. With one yoga class under my belt, in 2007, I entered into a 200 hour teacher training with Marni Task studying her combination of Jivamukti and Anusara yoga. I further continued my yoga training in 2011 with Ginger Garner PT, ATC, PYT of Professional Yoga Therapy Studies (http://proyogatherapy.org). Her school of medical yoga training, was just what I was looking for to merge my worlds of physical therapy and yoga.
Instead of looking at our patients as “pieces and parts,” referring to them as “the knee or the shoulder patient,” it is so important to see them as a whole. As an orthopedic PT I need to recognize that patients have not only a physical side of muscles, ligaments, bones and nerves, but other parts too that make them a whole person. Most likely I won’t specialize in pelvic pain or woman’s health but it is so important for me to be knowledgeable about this field to be the most effective therapist. In addition, it’s important to also go beyond the physical aspect and recognize patient’s psycho-emotional-social, spiritual, energetic, and intellectual aspects of their beings. Optimal health is achieved by recognizing and addressing all aspects of a patient.
And on that note, I’m going to continue merging all of my worlds of fascia, pelvic floor, orthopedics, and yoga, to address all the components of well-being, as I attend an upcoming course offered by Herman and Wallace called, Yoga for Pelvic Pain this month in Cleveland, Ohio.