
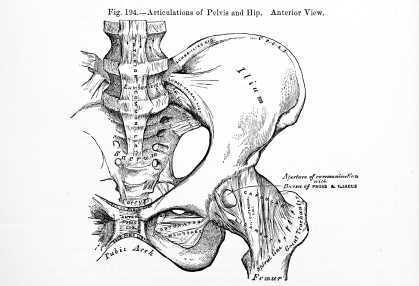
What are the roles of hip labrum innervation in both nociception and proprioception? Canadian researchers tackled this question by studying hip joints that were harvested during total hip replacement or hip resurfacing surgery. Twenty labrums were harvested and the structures in the labrum were divided into four quadrants including antero-superior (AS), postero-superior (PS), antero-inferior (AI), and postero-inferior (PI). The mean age of the subjects was near 60. The authors reported the following:
•Labral innervation is from a branch of the nerve to the quadratus femoris and the obturator nerve.
•All labrum samples had abundant free nerve endings according to the authors. These nerve endings are responsible for nociception transmission.
•Three different types of nerve end organs were noted: Vater-Pacini, Golgi-Mazonian, and Ruffini corpuscles. These nerve end organs operate to provide proprioception through their roles in pressure, deep sensation, and temperature.
•The free nerve endings and nerve end organs were observed more often in the AS and PS zones.
•The nerve endings were noted to be abundant in the superficial zones of the acetabular labrum which were for the most part avascular.
•The antero-superior zone of the labrum has abundant free nerve endings, a fact that correlates with the location of common labral tears and that also fits with the pain produced using a maneuver to test impingement in the hip (flexion, adduction, internal rotation).
•No significant differences in age was noted with respect to the innervation.
The study further states that a labral debridement may ease pain with removal of the free nerve endings, yet the labral repair may best allow for proprioceptive abilities and higher function in the injured hip. The authors also describe the findings that there are abundant myofibroblasts in the labrum that may account for the labrum's ability to heal. To learn more about healing labrums and getting patients moving, check out faculty member Ginger Garner's continuing education course on Extra-Articular Pelvic and Hip Labrum Injury: Differential Diagnosis and Integrative Management. The next opportunity to take the course is in March in Houston.
How long do hot flashes last in a woman's life? One recent study asked this question by following 255 women from premenopause to natural menopause. The authors found that moderate to severe symptoms of hot flashes continued on average 5 years after the date of the woman's last period. Unfortunately, up to 1/3 of the women continued to report hot flashes 10 or more years after menopause. Results also found that risks for hot flashes were higher in women who were African-American or in obese, white women. Higher education level was found to be protective against hot flashes.
The Mayo clinic states that while the exact cause of hot flashes is not known, there are several factors that may influence their occurrence. Changes in reproductive hormones in addition to hypothalamic shifts create a sensitivity to even slight changes in temperature. Women can experience a wide range of menopausal symptoms, with hot flashes ranging from sudden feelings of warmth that occur a couple times per day to profuse sweating that can occur up to one time per hour.
Menopause.org is a helpful resource for our patients, and lifestyle changes are offered such as avoiding stress, breathing techniques, and creating strategies to maintain body temperature within a limited range. Hormonal treatment and non-hormonal options are also described on this site, and while certain hormonal options may be contraindicated for some patients, there are therapies such as sleeping medications that may improve quality of life for a woman who is suffering significant sleep disruption. Decisions to utilize hormonal drug therapy may depend on many factors, such as benefits to risk ratios, if the patient has her uterus, and age of the patient. Many nonprescription options are also available, with conflicting or little evidence to support many of the claims. Regardless of the remedy that a patient may take for her menopausal symptoms, keep in mind that all medications or supplements should be reported to the physician and/or pharmacist so that drug interactions can be screened. Even herbal supplements can have a negative impact on other drugs that a woman is taking, so she should always fully disclose her medications, supplements (including teas!), creams, and other natural remedies.
If you are working with more women in the perimenopausal period, you may have questions about the hormonal changes and effects on rehabilitation. Faculty member Michelle Lyons will offer her new continuing education course called Menopause: A Rehabilitation Approach. At this course she will systemic changes in menopause, bone health, perimenopausal pelvic floor issues, sexual health, weight management, and procedures such as hysterectomy. The next opportunity to take this course is in February in Orlando - what a great time to head to the sunshine!
This November, Herman & Wallace is thrilled to be offering a brand-new course instructed by Carolyn McManus, PT, MS, MA, called Mindfulness-Based Biopsychosocial Approach to Chronic Pain. This course will be offered November 15-16, 2014 in Seattle, WA. We sat down with Carolyn to learn more about her course.

The constant flood of information in today’s interconnected, wired world trains the mind in distraction and away from the immediate experience of life. Many people spend hours gazing down at quickly changing images on the small frame of an electronic device and only notice the body when it has its aches and pains! Mindful awareness offers us a skillful way to pay attention, build body awareness, touch life fully and provides a healing antidote to information overload.
Mindful awareness invites us to rest the mind in the present moment with openness, friendliness and curiosity. This is not our natural tendency and requires training. Often we are caught in a struggle with the present moment, perceive it as flawed, find fault with ourselves and constantly drive ourselves to run, do and achieve. When mindful, we still have our plans, goals and to-do list, but this is not an obstacle to resting the mind here and now. We can stop the struggle with the present moment, touch life fully and open to the potential for ease and insight in the midst of things just as they are. New perceptions and an experience of aliveness can occur that can never happen when we are lost in distraction. Danna Faulds expresses this beautifully in her poem "Walk Slowly":
It only takes a reminder to breathe,
a moment to be still, and just like that,
something in me settles, softens, makes
space for imperfection. The harsh voice
of judgment drops to a whisper and I
remember again that life isn’t a relay
race; that we all will cross the finish
fine; that waking up to life is what we
were born for. As many times as I forget to catch myself charging forward
without even knowing where I am going,
that many times I can make the choice
to stop, to breathe, and be, and walk
slowly into the mystery.
I began practicing mindfulness meditation to help manage stress and heal from a back injury. I found the practice easily translated to patient care and helped my patients build body awareness, detach from maladaptive thinking habits and experience inner calm and relaxation. They gained insight into the reactions, behaviors and situations that escalated and de-escalated their symptoms. Research shows that mindfulness improves attention regulation and executive function, body awareness and emotional regulation. (1) I am excited to share with my colleagues what I have learned through the practice of mindfulness and its applications to both self-care and patient care in my November course.
Learn more about Carolyn's course and join her this November in Seattle to attend her Mindfulness course!
1. Holzel BK, Lazar SW, Guard T, et al. How Does Mindfulness Meditation Work? Proposing Mechanisms of Action From a Conceptual and Neural Perspective. Perspect Psychol Science. 2011;6: 537–559.
Avulsion fractures refer to a forcible separation, or tearing away of bone due to a sudden and powerful contraction of muscle. This injury is most common in adolescents, with the as yet developing growth plates being a likely location of avulsion. A systematic review of the literature published in 2011 describes the pathology of pelvic avulsion fractures as "highly prevalent" among adolescent athletes. Additionally, patients who have mature skeletons and who have a history of prior surgical interventions to the bones are also at risk for pelvic avulsion fractures.
Avulsion fractures appear to occur most commonly during the eccentric phase of muscle activity during sporting activities. Pre-existing pain in hip or pelvis may be present, but is not a reliable predictive sign of subsequent fracture. Included in this review article were 48 case reports and case series of which 88% related to physical activity and the remaining 12% related to previous surgical procedures. Within the cases related to physical activity, the mean age of fracture in subjects was 16.8, with 84% being male. Activities in which subjects were involved involved included soccer, gymnastics, and running sports. In the cases related to surgery, mean age of fracture was 56.4, and 100% were female. All of the surgery-related cases presented in the literature were treated with conservative measures. Conservative care described included a period of bed rest for 3 days progressing to walking with crutches until the patient was able to walk without significant pain.
Symptoms reported by patients who have suffered an avulsion fracture of the pelvis may include reporting a popping sensation, local pain, and difficulty walking. Having had a bone harvest from the iliac crest may also predispose a patient to a subsequent avulsion fracture. The authors state that surgery may be considered when there is greater than 2 centimeters of displacement of the avulsion or if the ischial tuberosity is involved.
Rehabilitation therapists should be alert to the age, activity levels, and histories of patients who present with pelvic and hip pain, as an avulsion fracture may be the source of pain. Radiographic imaging will provide further information upon which a plan of care can be made. If you would like to learn more about diagnosing pelvic pain, join your colleagues at one of our courses aimed towards identifying sources of pelvic pain. Peter Philip's continuing education course titled Differential Diagnostics of Chronic Pelvic Pain will next be offered in July of next year in Arlington, VA. Another popular course called Finding the Driver in Pelvic Pain was created by faculty member Elizabeth Hampton and will be offered in April in Milwaukee, WI.

Do women who participate in yoga during pregnancy feel more optimistic, more powerful, and more well? Yes! This is the reply from a study involving 21 women who enrolled in a yoga class for six weeks. While twelve of the women had previously practiced yoga, none were currently practicing. The format of the class involved the following components: checking in (sharing the prior week's experiences), centering (visualization and breathing exercises), warm-up (neck rolls, shoulder exercises, and side stretches), yoga flow (yoga standing positions such as sun salutation), standing postures (balance, wall positions), mat work (seated postures and hip exercises), Savasana (modified to left side lying), and meditation.
Outcomes tools utilized in this study included the Life Orientation Test-Revised for measuring optimism, the Power as Knowing Participation in Change Tool version II for measuring sense of power, the Short-Form 12 Version 2.0, and the Well-being Picture Scale. Participants in the study were also given a journal to document time spent practicing yoga, and how they felt after practicing yoga, both physically and emotionally. The authors conclude that yoga as a self-care practice can be used to promote self-care and well-being in women who are pregnant.
Why are feelings of power, well-being, and optimism valuable for women who are pregnant? The authors discuss the literature which has suggested higher levels of adaptive coping in women with high-risk pregnancies, and the concept that optimism is associated with physical health. Previous studies about using yoga during pregnancy have proposed benefits to the mother both during her pregnancy as well as during labor and delivery. The authors of the study also describe power within the perspective of Rogers' science of unitary human beings, with sharing of interesting philosophical concepts such as resonancy, integrality, and diversity of the human-environmental field.
Because yoga is a popular activity with pregnant women, the study adds to the growing body of research about yoga in the peripartum period. If you are interested in learning how to apply yoga concepts for patients who are pregnant, come to Ginger Garner's continuing education course Yoga As Medicine for Pregnancy and the next opportunity to take this course is next month in New York!
Earlier this year, the Food and Drug Administration issued a warning about serious side effects of laxatives if not used according to the label or when used in the presence of certain comorbities. Sodium phosphate laxatives, according to the label, are to be taken as a single daily dose, and for no more than three days. In addition to the warning to contact a physician if the patient has kidney disease, cardiac conditions, or dehydration, the FDA advises patients to ask their physician before taking the drug with age older than 55, or when taking certain medications. These medications include: diuretics, angiotensin-converting (ACE) inhibitors, angiotensin receptor blockers (ARBs), and nonsteroidal anti-inflammatory drugs (NSAIDs).
Laxatives are grouped into different classes and have varied effects on a person's gastrointestinal system. The following is adapted from the Mayo Clinic's website and describes the main types of laxatives.
| Laxative Type
|
Action
|
Brand Example |
| Oral osmotics | Draw water into the colon to improve passage of stool | Miralax |
| Oral bulk formers | Absorb water to form soft, bulky stool | Metamucil |
| Oral stool softeners | Add moisture to stool | Surfak |
| Oral stimulants | Trigger rhythmic contractions of intestinal wall | Senekot |
| Rectal stimulants | Trigger rhythmic contractions of intestinal wall | Dulcolax |
Because laxatives can interact with medications, asking about medication lists (including supplements and herbals) is important for pelvic rehabilitation providers. Even the teas available at the grocery store that are marketed to help with digestion and specifically, constipation, may work well and may interact with a patient's medications. If you are interested in learning more about laxatives, constipation, and promotion of bowel health with rehabilitation techniques, sign up for the Bowel Pathology and Function continuing education course. This course, written by faculty member Lila Abbate, has been well-received and aims to further the knowledge of therapists who are treating patients with bowel dysfunction. The next course is coming up next month in California!

What are the spontaneous mental images that women who have chronic pelvic pain report, and how might the positive or negative mental images relate to chronic pelvic pain? These questions are the focus of research published by authors from the UK in the journal Pain Medicine. Mental images are distinguished in this study from thoughts, or thinking in words, as mental images are "cognitions with sensory-perceptual qualities." These qualities are often visual, and may also be related to smell, touch, taste, and hearing. Ten women were interviewed, 8 of whom had a diagnosis of endometriosis or adenomyosis. The researchers explained that they wanted to learn more about the women's thoughts when in pain, and asked about any images that popped into their heads when in pain. Researchers asked other questions about images related to specific categories, while attempting to avoid offering any leading words during their interview. The patients' most significant mental image (chose by the patient) was then explored for content, triggers, related emotion, meaningfulness, activity impairment, and related behavioral changes.
Other data collected included the Brief Pain Inventory short form, the Pain Catastrophizing Scale, the Spontaneous Use of Imagery Scale, the Hospital Anxiety and Depression Score, and the Mini-International Neuropsychiatric Interview. The range of pain duration in the subjects was 3-20 years, with a mean age of 36.2. While every one of the ten women reported that pain was a trigger, other triggers for a negative mental image included movement, social gatherings, exercise, babies, anxiety, sex, sleep, talking about pain, and reminders of surgery or menstruation- in other words, common daily activities or experiences. The content of the most significant mental images included being raped, having "malicious demons" playing around the pelvis, bright lights in an operating room, being terrorized, feeling sad, helpless, anxious, angry, panicky, guilty, disgusted, horrified, and revulsed. The associated meanings were usually also quite negative in nature. The women reported active avoidance of the triggers when able, limiting activities such as social outings or physical activity. Positive or "coping" images were also reported, with images such as putting the pain into a box, mentally "rubbing pain" medication on the body, or imagining a loved one.
What does this information have to do with pelvic rehabilitation? This study utilized a cognitive-behavioral (CBT) framework, and aspects of CBT are tools that rehabilitation professionals utilize in daily practice. Simply put, a cognitive-behavioral approach addresses how a person's thoughts and feelings affect behavior. In rehabilitation, research studies have described how CBT is utilized in the physical therapy setting, and how therapists can be trained to use skills in CBT to help patients . We can engage patients in conversations about what negative images may be impacting movement, and what positive images may be utilized as healthy coping strategies. For more information about the mind and patient education, join us at Carolyn McManus's continuing education course Mindfulness-Based Biopsychosocial Approach to the Treatment of Chronic Pain which takes place next month in Seattle.
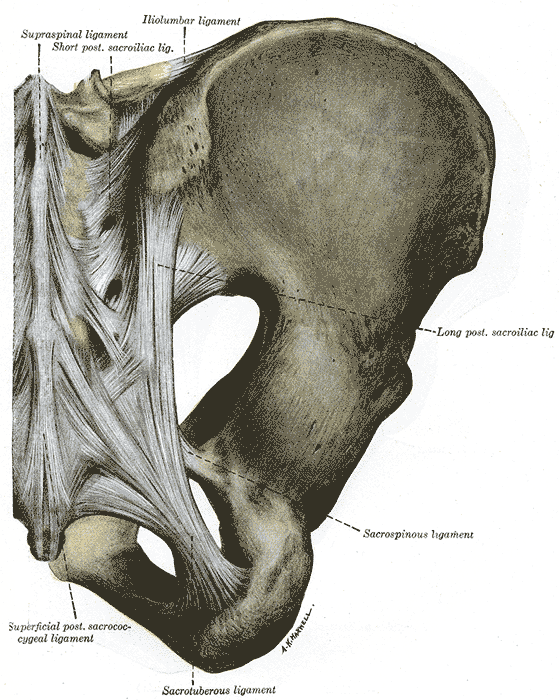
Several researchers have contributed to foundational literature in trunk control including Richardson, Snijders, and Hull. One study of interest completed by these authors and other colleagues assessed sacroiliac joint stability with contraction of the transversus abdominis muscles compared to contraction of all the lateral trunk muscles.
In this experiment, 13 healthy subjects without a history of low back pain participated in the tests. Eight men and five women with a mean age of 26 and who were able to complete the required muscle activations participated in the study. The subjects were positioned in prone, and electromyographic recordings as well as ultrasound imaging were used to verify the muscle activation patterns. To measure sacroiliac joint stiffness or laxity, Doppler imaging of vibrations was utilized. The theory of using vibration to measure joint stiffness includes that a transfer of vibration across a joint is best when the joint is more stiff, according to the authors.
The results of the study include a decrease in laxity (or an increase in stiffness) in the sacroiliac joint when either muscle patterns were used, however, when the transversus only was activated, laxity was decreased more than during a more global contraction.
Research in trunk and pelvic control has typically divided the muscles into local or global muscles, with inclusion of the the more superficial, larger muscles that control trunk movement grouped into the global muscles. Local muscles in this study describe the deeper, smaller muscles more apt to act as stabilizers of the lumbar spine and sacrum such as the transversus abdominis and multifidus. While this description is not inclusive of all or of more recent models, for the purposes of this study, these descriptions may be found useful.
The authors acknowledge that the role of the pelvic floor in creating sacroiliac joint stiffness, having not been measured, is not known in this study. The research does support the body of work that describes use of specific training for treating patients with low back pain, rather than global exercises without an emphasis on local muscle activation.
Many of you are aware of the various "camps" and beliefs about trunk and pelvic rehabilitation and activation, and more than likely, as with most issues in life, the truth lies in the middle. Do some patients simply need to correct their breathing patterns, trunk alignment, or gait patterns? Sure, and other patients may require a focus on inhibiting a very painful muscle, bringing awareness to that area, and learning how to "turn on" the muscle and incorporate the muscle pattern into routine activities. Herein we find, in my opinion, the art of rehabilitation. Researchers and therapists will continue to work towards clinical prediction rules and guidelines for best practice, yet we are left with understanding the theories and tools that drive the research and clinical practice so that we can apply individual plans of care for patients. If you find yourself "stuck" with the same "core" exercises and feel that you would like to improve your skills in sacroiliac rehabilitation, therapists have been raving about Peter Philip's sacroiliac joint course, where you can learn very specific palpation, testing, and rehabilitation principles. The next opportunity to take this course is in January!
The Herman & Wallace Pelvic Rehabilitation Institute is excited to offer continuing education courses this year in mindfulness and in meditation, which are not necessarily one in the same. However, each has a relationship with the other, and may be combined into lovely practices. More importantly, you may be wondering, "How does mindfulness fit into pelvic rehab?" Mindfulness or meditation has been applied to many pain diagnoses, and even to pelvic rehab conditions such as bowel or bladder dysfunction, and pelvic pain. (For some interesting reading about mindfulness and meditation, check out the National Center for Complementary and Alternative Medicine's website by clicking here.
In this Canadian study, 14 women participated in four sessions of mindfulness and cognitive behavioral therapy tailored to women with provoked vulvodynia (PVD). The sessions were spaced 2 weeks apart, and each session was 2 hours in length. The program included education in PVD and in pain neurophysiology, cognitive behavioral skills ("identifying problematic thoughts"), progressive muscle relaxation (contract-relax), and mindfulness exercises. The mindfulness exercises included eating meditation, mindfulness of breath, body scan and mindfulness of thoughts. The goal of this particular research article was to describe the women's thoughts about participation in the study activities. The authors report on six major themes from the study:
1)Feeling more normal and part of a community in the group setting
2)Positive psychological outcomes
3)Impact of relationship (supportive versus unsupportive partner)
4)Feeling of gratitude for group facilitators
5)Concern about barriers to continuing their mindfulness practice
6)Feelings of self-efficacy in being able to exert control over their pain
One of the major themes expressed by the participants in this study is that of feeling more "normal" through finding out that other women have the same symptoms and knowing that there are a myriad of symptoms associated with vestibulodynia. By participating in the study, women reported having improvements in self-esteem and feeling more optimistic about their challenges with physical activities such as sexual relationships. Carloyn McManus, who has degrees in both physical therapy and psychology, shares her expertise in our new course: Mindfulness-based Biopsychosocial Approach to the Treatment of Chronic Pain. The next opportunity to take this mindfulness continuing education course, and learn skills that you can immediately apply in mindfulness is this November in Seattle.
Consider how many times we have worked with a patient who refuses to participate in rehabilitation or cancels an appointment because of constipation. Also recall the high number of patients we treat who are in chronic pain and who are also likely taking an opioid medication for pain management. A well-known side effect of opioids is constipation, which can create a viscous cycle: taking the medication can mean having to strain to pass stool, or being bloated which can aggravate an already painful state. Not taking pain medications can increase pain levels, potentially decreasing physical activity levels, another cause for poor bowel function. A recent research article sheds light on this problem, pointing out that, despite a failure of medications in positively treating their constipation, patients are willing to continue on the current course of treatment.
The on-going longitudinal study in the USA, Canada, Germany, and the UK aims to assess the burden of opioid-induced constipation (OIC) in patients who have chronic pain that is not cancer-related. Patients were using at least 30 mg of opioids per day for more than four weeks and had self-reported opioid-induced constipation. For the 493 patients who met the inclusion criteria, retrospective chart reviews, on-line patient surveys, and physician surveys were utilized. Outcomes tools included the Patient Assessment of Constipation-Symptoms, Work Productivity and Activity Impairment Questionnaire-Specific Health Problem, EuroQOL 5 Dimensions, and Global Assessment of Treatment Benefit, Satisfaction, and Willingness to Continue. 62% of the patients were female, mean age in males and females was 52.6.
Patients complained of bowel dysfunction including abdominal pain and bloating, painful straining to defecate and having flatulence, rectal pain and bleeding, headaches, and having hard stools that were difficult to pass. Most of the patients (83%) wanted to have at least one bowel movement (BM) per day, yet the mean reported BM was 1.4 per week without use of laxatives, and 3.7 BM with use of laxatives. Natural or behavioral therapies were used by 84%, and 60% of the patients used at least 1 over-the-counter (OTC) laxative, 24% used 2 or more OTC laxatives, and 19% used one or more prescription laxatives. Unfortunately, 94% of the patients reported inadequate response to laxative use.
Current employment rates for the sample population was 27%, and of these patients, the average reports of missed work due to constipation issues was 4.6±11.9 hours of work over the past 7 days. Even worse, from a pain-management perspective, 49% of the patients reported "…moderate to complete interference with pain management resulting from their constipation." The authors conclude the following: "The prevalence of these symptoms suggests that patients may be undertreating their OIC and/or that the currently utilized therapies for the treatment of OIC may be lacking in efficacy and tolerability." Can we conclude that the under-treatment applies to a lack of pelvic rehabilitation intervention? Granted, opioid-induced constipation by nature of its effects on the gut will in turn affect peristalsis and hydration of stool. However, if a patient learns techniques to stimulate bowel activity, how to manage abdominal bloating and pain, and how to affect the nervous system in a positive way, perhaps less work (and leisure) time would be lost.
If you are interested in learning more about constipation, we have one opening in the PF2A St. Louis course taking place in early October. If you have already taken PF2A, and want to expand your knowledge and your skill set, join faculty member Lila Abbate in her Bowel Pathology and Function continuing education course in California in early November. Course topics include over-the-counter products and medications affecting bowel health, constipation and fecal incontinence, internal vaginal and rectal muscle mapping, and a balloon-manometry lab- a lab that therapists are thrilled to have offered in an Institute course!
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/









































