Allison Ariail, PT, DPT, CLT-LAANA, BCB-PMD is one of the creators of the Herman & Wallace Oncology of the Pelvic Floor Course Series. Allison Ariail is a physical therapist who started working in oncology in 2007 when she became certified as a lymphatic therapist. She worked with breast cancer, lymphedema patients, head and neck cancer patients, and the overall oncology team to work with the whole patient to help them get better. When writing these courses, Allison was part of a knowledgeable team that included Amy Sides and Nicole Dugan among others.
As pelvic rehab professionals, we know the importance of the microbiome of the digestive tract and how this can influence issues our bowel patients may experience. You also may know that the GI microbiome can influence immune function as well as mental health. Did you know that the urinary bladder has its own microbiome? Recent developments in next-generation sequencing and bioinformatic platforms have allowed for the detection of microbial DNA in the urinary tract.(1) This could be a game changer for those who suffer from chronic urinary tract infections. However, it could be even more important as a way to prevent bladder cancer. May is Bladder Cancer Awareness Month. In honor of this month, let’s further discuss how the urinary microbiome may influence the development of bladder cancer.
Dysbiosis of the urinary microbiome could be related to bladder cancer through chronic inflammation in the urothelial microenvironment. Chronic inflammation is a hallmark of genomic instability and the development of cancer. A study in 2021 compared the urinary microbiome of patients with muscle-invasive and non-muscle-invasive bladder cancer. They found the microbial profiles differed in patients with cancer compared to healthy individuals. They also found that there were different microbial profiles from the less invasive non-muscle invasive versus the more invasive types of bladder cancer.(2)
The urinary microbiome is a growing area of research and I would expect to see more information come out on this, what influences the urinary microbiome, as well as how modulating this can prevent and fight urothelial cell carcinoma. I would anticipate more treatment options including some new immunotherapy agents to emerge that can help to fight bladder cancer.
If you do not know much about bladder cancer and would like to learn more, Oncology of the Pelvic Floor Level 2B covers topics on bladder cancer and gynecological cancers. Join us to learn more about these diagnoses, medical treatments, and ways a pelvic rehab professional can help these patients recover.
Resources:
1. Neugent ML, Hulyalkar NV, Nguyen VH, Zimmern PE, and De Nisco NJ. Advances in understanding the human urinary microbiome and its potential role in urinary tract infection. mBio. 2020; 11(2): e00218-20.
2. Hussein AA, Elsayed AS, Durrani M, et al. Investigating the association between the urinary microbiome and bladder cancer: an exploratory study. Urol Oncol. 2021; 39(6): 370.e9-370e19.

*Certified Lymphatic Therapists may skip Oncology of the Pelvic Floor Level 1 and move on to the Level 2A and Level 2B courses.*
Oncology of the Pelvic Floor Level 1 - no partner needed for registration
Price: $550.00 Experience Level: Beginner Contact Hours: 17.5 hours
Description: The course will address issues that are commonly seen in a patient who has been diagnosed with cancer such as cardiotoxicity, peripheral neuropathy, and radiation fibrosis. Some holistic medicine topics, including yoga and mindfulness, will be discussed in order to fully prepare the participant to be able to competently work with cancer survivors.
The basics of the lymphatic system will be covered, as well as when to refer the patient to a lymphatic specialist for further treatment. Red flags and warning symptoms will be discussed so the participant feels comfortable with knowing when to refer the patient back to their medical provider for further assessment.
This introductory course is aimed to get the participant comfortable with working with oncology patients and as part of an interdisciplinary oncology team.
Course Dates: July 8-9 and December 2-3
Oncology of the Pelvic Floor Level 2B - partner needed for registration
Price: $600.00 Experience Level: Intermediate Contact Hours: 19.25 hours
This course was designed to build on the information that was presented in Oncology of the Pelvic Floor Level 1.
Description: Information will be provided focusing on gynecological and bladder cancers including risk factors, diagnosis, and prognosis. The participant will also understand the sequelae of the medical treatment of cancer and how this can impact a patient’s body and quality of life. Other topics include rehabilitation and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy.
Course Dates: December 9-10
Megan Pribyl, PT, CMPT is a physical therapist at the Olathe Medical Center in Olathe, KS treating a diverse outpatient population in orthopedics including pelvic rehabilitation. Megan’s longstanding passion for both nutritional sciences and manual therapy has culminated in the creation of her remote course, Nutrition Perspectives for the Pelvic Rehab Therapist, designed to propel understanding of human physiology as it relates to pelvic conditions, pain, healing, and therapeutic response.
I have always viewed resultant health as the sum total of nutrition, exercise, lifestyle factors, environmental/toxicant & chemical exposure, genetics, and spiritual confluences. In balance, health and vitality flourish. Out of balance, health struggles manifest. If we take a look around, we bear witness to modern culture’s harmful effects upon our physiology – and specifically on our blood-brain barrier (BBB). Health struggles affecting the brain and impacted by BBB dysfunction are diverse and can include anxiety, depression, chronic pain, and neurodevelopmental disorders. Other disorders linked to a compromised BBB include Alzheimer’s disease, dementia, Parkinson’s Disease, and MS. So we ought to care a lot about our BBB – yet most of us don’t make conscious lifestyle choices based on protecting this vital gatekeeping system. Perhaps if we examine one specific angle of this issue - that diet and short-chain fatty acids influence the integrity of the blood-brain barrier – we might decide to care a lot more about protecting our brain – like we mean it.
For starters, it helps to acknowledge that our entire body IS an immune system – one that is constantly surveying potential threats to our existence. It is very well established that 70% of our immune system resides in our gut. This placement makes sense because the very act of eating exposes our inner workings to whatever “food” passes through the alimentary canal. Our digestive tract is a frontline sorting station that decides what can pass through the intestinal barrier and what cannot. Having a strong intestinal barrier is critical to maintain health as evidenced by a wealth of both animal and human studies.
Most of us also don’t constantly think about our intestinal barrier – but science contends that we should. Because what happens there impacts our entire body and all systems – including our nervous system. A recent study even describes a “Gut Spinal Cord Immune Axis” wherein the health of our spinal cord itself is dependent on immune factors regulated by the gut microbiota. (3) That’s how far your gut health influence goes.
So, let’s talk about one way our gut, a.k.a. microbiome, keeps us healthy. The microbes in our large intestine should be numerous and diverse. These microbes thrive in the presence of prebiotic fiber components (sources of prebiotic fiber are diverse, from the plant world and include things like Jerusalem artichoke, bananas, onions, berries, garlic, and other herbs and spices) which arrive in the colon because they are consumed by the host – us. When your microbes feast on the prebiotic fibers, they produce a by-product, and this byproduct is SCFA’s or short-chain fatty acids. It is well established that these SCFAs play a powerful immunomodulatory role both locally (in the intestine) and distantly (e.g. at the blood-brain barrier). This is the best way to create healthy short-chain fatty acids so they can do what they do best in our system – modulate inflammation.
But what happens if we don’t have richness (as in ample number) or diversity (as in different health-promoting species) of microbes in our large intestine? We can’t produce as many SCFAs.
What happens if we don’t consume the food (eg. prebiotic fiber) our microbes like to eat? Or if we aren’t eating foods that contain microbes (eg. cultured foods)? We can’t produce as many SCFAs.
What happens if we are deficient in healthy SCFAs? We may end up with undesirable physiological sequelae such as systemic inflammation. Which can include blood-brain barrier inflammation. (2)
Remember that we have nerves everywhere in our body – centrally and peripherally. If any of the nerves in our body (peripheral nerves), brain (CNS), or gut (ENS) are inflamed, this can be termed neuroinflammation. Neuroinflammation in the CNS leads to blood-brain barrier inflammation resulting in increased permeability – this ultimately allows substances to reach the brain that shouldn’t.
Neuroinflammation is at the root of many of the health sequelae we currently see in non-communicable conditions. (5) Maybe in your patient it manifests as chronic pain. Maybe in your friend, it’s anxiety and depression. Maybe in your aunt it’s MS, your uncle it’s Alzheimer’s. Maybe in your neighbor it’s fibromyalgia. Neuroinflammation has many faces.
When we look at factors that contribute to blood-brain barrier dysfunction, many can be traced to the cumulative effects of a standard American diet and lack of nutrient density. Further, and more ubiquitous – is our unseen exposure to toxicants such as herbicides and pesticides as well as a multitude of other potential cell health disruptors. (1, 4)
Because of the massive implications of human disease states, we need to pay attention to what the literature is telling us about the interconnected nature of health and lifestyle. We must stop polluting our human physiology and we must start feeding ourselves food that isn’t paradoxically decimating our microbiome. It’s that simple. And complicated. At the same time.
Taking a deep breath is the first step. A crucial second step is staring down the truth of our country’s health care and agricultural realities. The third is gaining perspective on what actions each of us can take today – wherever we live, whatever our socioeconomic status, and whatever our current health status. There is much work to do.
I invite you to an opportunity to learn about many actions we can take today and examine nutritional concerns in depth that have implications not only for the population you treat as a pelvic rehab therapist but for yourself, your friends, and your extended human family.
We must prioritize protective health choices. We must care for our gut, propagate healthy short-chain fatty acids, and therefore care for our blood-brain barrier. And subsequently, protect our brain - like we mean it. Because our modern culture will not do that for us. Solving our nation’s health crises will take each of us collectively to make a difference. The health status of our nation can improve – one protected brain at a time.
Join us for our next offering of Nutrition Perspectives for the Pelvic Rehab Therapist scheduled for June 10-11, 2023.
References:
- Abou Diwan M, Lahimer M, Bach V, Gosselet F, Khorsi-Cauet H, Candela P. Impact of Pesticide Residues on the Gut-Microbiota-Blood-Brain Barrier Axis: A Narrative Review. Int J Mol Sci. 2023 Mar 24;24(7):6147. doi: 10.3390/ijms24076147. PMID: 37047120; PMCID: PMC10094680.
- Fock E, Parnova R. Mechanisms of Blood-Brain Barrier Protection by Microbiota-Derived Short-Chain Fatty Acids. Cells. 2023 Feb 18;12(4):657. doi: 10.3390/cells12040657. PMID: 36831324; PMCID: PMC9954192.
- Raue KD, David BT, Fessler RG. Spinal Cord-Gut-Immune Axis and its Implications Regarding Therapeutic Development for Spinal Cord Injury. J Neurotrauma. 2023 Mar 10. doi: 10.1089/neu.2022.0264. Epub ahead of print. PMID: 36509451.
- Sharma T, Sirpu Natesh N, Pothuraju R, Batra SK, Rachagani S. Gut microbiota: a non-target victim of pesticide-induced toxicity. Gut Microbes. 2023 Jan-Dec;15(1):2187578. doi: 10.1080/19490976.2023.2187578. PMID: 36919486; PMCID: PMC10026936.
- Takata F, Nakagawa S, Matsumoto J, Dohgu S. Blood-Brain Barrier Dysfunction Amplifies the Development of Neuroinflammation: Understanding of Cellular Events in Brain Microvascular Endothelial Cells for Prevention and Treatment of BBB Dysfunction. Front Cell Neurosci. 2021 Sep 13;15:661838. doi: 10.3389/fncel.2021.661838. PMID: 34588955; PMCID: PMC8475767.
Nutrition Perspectives for the Pelvic Rehab Therapist

Price: $525.00 Experience Level: Beginner Contact Hours: 17.5 hours
Course Dates: June 10-11, September 16-17, and December 2-3
Description: Participants will be introduced to the latest research in nutrition through immersive lectures and hands-on labs. The course will cover essential digestion concepts, nourishment strategies, and the interconnected nature of physical and emotional health across the lifespan. Further, clinicians will delve into nutritional relevancies in bowel and bladder dysfunction, pelvic health, pain, and healing. Labs throughout include insightful demonstrations and breakout sessions. The course participant will acquire new, readily applicable tools for patient empowerment, engagement, and self-management utilizing presented principles.
Aparna Rajagopal, PT, MHS, WCS, PRPC, Capp-OB Certified is the lead therapist at Henry Ford Macomb Hospital's pelvic dysfunction program, where she treats pelvic rehab patients and consults with the sports therapy team. Her interest in treating peripartum patients and athletes allowed her to recognize the role that breathing plays in pelvic dysfunction.
Leeann Taptich DPT, SCS, MTC, CSCS leads the Sports Physical Therapy team at Henry Ford Macomb Hospital where she mentors a team of therapists. She also works very closely with the pelvic team at the hospital which gives her a very unique perspective of the athlete.
Aparna and Leeann co-authored the course, Breathing and the Diaphragm: Pelvic and Orthopedic Therapists, which helps clinicians understand breathing mechanics and their relationship to the pelvic floor.
Abdominal bloating and distension are two very commonly reported GI symptoms in the pelvic practice setting. However, these symptoms are not commonly recognized in other physical therapy settings. While many people experience occasional bloating/discomfort it does not necessitate medical intervention, but repeated and long-standing bloating/distention can impact the quality of life.
One diagnosis which is associated with these symptoms is Abdomino-Phrenic dyssynergia where patients develop a paradoxical abdomino-phrenic response. Normally, as a response to an increase in intraluminal gas, the diaphragm relaxes, and the abdominal musculature contracts. When dyssynergia is present, the opposite happens and the diaphragm contracts, and the abdominals relax. Abnormal pelvic floor function is also associated with this diagnosis. Treatments typically used are biofeedback therapy and breathing techniques.
Where Leeann and I work, we are seeing patients increasingly referred with this diagnosis. Recently we treated a 72-year-old female patient with a long-standing history of troublesome bloating and distention, with the diagnosis of Abdomino phrenic dyssynergia.
- The patient had complaints of bloating and abdominal distension all day long, worsening toward evening
- She reported limiting her food intake in the evenings on account of the discomfort and "tightness" in the abdomen
- She rated the discomfort as 3-5/10 in the morning time with an increase to 8/10 by late evening
- She also reported poor sleep because of how "hard and tight" the abdomen felt by bedtime
Upon examination, amongst other findings, the patient demonstrated:
- Significant tightness in her posterior chain and her erector spinae in both thoracic and lumbar regions
- Decreased thoracic rotation/mobility
- Increased connective tissue restrictions in both upper abdominal quadrants, especially in the epigastric area and inferior to the rib cage
- Decreased lower rib cage mobility
- Poor ability to prolong exhale or to exhale strongly
- Decreased ability to relax the pelvic floor musculature after a contraction
In addition to biofeedback and visceral mobilizations, treatment techniques included joint mobility techniques inclusive of simple rib and thoracic spine mobilizations, soft tissue mobility techniques including gentle diaphragm releases, breath training, and breathing techniques to aid in pelvic floor relaxation.
The patient received 9 treatment sessions and a home maintenance program which she followed with good compliance. She reported a 70% overall improvement and was now able to sleep through the night and eat in the evenings without discomfort.
In our course, Breathing and the Diaphragm: Pelvic and Orthopedic Therapists, you will learn:
- Explain normal diaphragmatic breathing and the role of the internal and external oblique musculature.
- Assess and treat dysfunctional breathing patterns including but not limited to chest, abdominal, and paradoxical breathing patterns.
- Understand the concept of Intra-Abdominal Pressure (IAP) and the control and use of IAP with the diaphragm in a lowered position as a stabilizing mechanism for the spine.
- Understand the concept of regional interdependence and its application in the treatment of back or pelvic pain patients.
- Recognize the effects of postural patterns and the linkage to the diaphragm and pelvic floor.
- Understand the muscles and myofascial components involved in dysfunctional breathing and techniques to effectively treat the same.
- Understand and demonstrate mobilizations of the rib and thoracic spine and develop a comprehensive treatment program.
- Develop an exercise progression for dysfunctional breathing for use in the clinic and in-home programs.
- Integrate diaphragmatic breathing and mobility in the athletic clientele
Course Dates: April 22-23
Price: $450
Experience Level: Beginner
Contact Hours: 14
Description: This remote course is an integrated approach where participants will learn how the diaphragm, breathing, and the abdominals can affect core and postural stability through intra-abdominal pressure changes while looking at structures from the glottis and the cervical region to the pelvic floor.
This course includes assessment and treatment of the barriers by addressing thoracic spine articulation and rib cage abnormalities in the fascial system of muscles related to breathing and the diaphragm. Instructed techniques are applicable to patients who present with Diastasis Rectus Abdominis, pelvic pain, incontinence, and prolapse, as well as cervical, thoracic, scapular, and lumbar pain.
Allison Ariail, PT, DPT, CLT-LAANA, BCB-PMD is one of the creators of the Herman & Wallace Oncology of the Pelvic Floor Course Series. Allison Ariail is a physical therapist who started working in oncology in 2007 when she became certified as a lymphatic therapist. She worked with breast cancer, lymphedema patients, head and neck cancer patients, and the overall oncology team to work with the whole patient to help them get better. When writing these courses, Allison was part of a knowledgeable team that included Amy Sides and Nicole Dugan among others.
March is Colorectal Cancer Awareness Month. Did you know that the incidence rate of colorectal cancers is increasing? According to the International Agency for Research on Cancer, 1.9 million new cases of colorectal cancer were identified worldwide in 2020. This number is expected to grow even more. It is predicted that by 2040 the number of new cases of colorectal cancer will rise to 3.2 million new cases a year, and 1.6 million annual deaths worldwide. Additionally, did you know due to the fact that the incidence rate is increasing and it is being diagnosed in younger individuals, the age for screening for colorectal cancer has lowered to 45? At age 45 individuals should begin regular screening for colorectal cancer either via stool-based testing or visual-based screening via a colonoscopy. If someone has risk factors they may need to begin screening at a younger age.
Colorectal cancer can often be preventable through modifiable risk factors. Changing some of these risk factors, alongside the detection and removal of precancerous lesions can lower someone's risks. However, if a diagnosis is made, treatment can help to prolong the life of the patient. The treatment can include various surgeries, chemotherapy, and radiation. All of these treatments can cause changes to a patient's body. A rehab professional that has knowledge about both the body and how the medical treatment of cancer causes changes, can make all the difference in the world for that patient returning to activities that they enjoy and love after treatment.
There are not many opportunities for rehab professionals to learn about these changes and how we can help these patients. However, Herman & Wallace has a series focused on helping oncology patients. In this series, techniques are learned that can help colorectal cancer patients recover from their diagnosis and the medical treatment they go through. The oncology series is online and offered several times a year. You can attend the upcoming oncology courses on: Oncology of the Pelvic Floor Level 1 scheduled for July 8-9 and December 2-3, Level 2A scheduled for May 20--21, and Level 2B scheduled for December 9-10.
Reference:
Morgan E, Arnold M, Gini A, et al. Global burden of colorectal cancer in 2020 and 2040: incidence and mortality estimates from GLOBOCAN. Colon. 2023; 72(2).
*Certified Lymphatic Therapists may skip Oncology of the Pelvic Floor Level 1 and move on to the Level 2A and Level 2B courses.*

Oncology of the Pelvic Floor Level 1 - no partner needed for registration
Price: $550.00 Experience Level: Beginner Contact Hours: 17.5 hours
The basics of the lymphatic system will be covered, as well as when to refer the patient to a lymphatic specialist for further treatment. Red flags and warning symptoms will be discussed so the participant feels comfortable with knowing when to refer the patient back to their medical provider for further assessment.
This introductory course is aimed to get the participant comfortable with working with oncology patients and as part of an interdisciplinary oncology team.
Course Dates: July 8-9 and December 2-3
Oncology of the Pelvic Floor Level 2A - partner needed for registration
Price: $495.00 Experience Level: Intermediate Contact Hours: 17.25 hours
This course was designed to build on the information that was presented in Oncology of the Pelvic Floor Level 1.
Information will be provided focusing on male pelvic cancers, colorectal cancer, and anal cancer including risk factors, diagnosis, and prognosis. The participant will also understand the sequelae of the medical treatment of cancer and how this can impact a patient's body and quality of life. Other topics include rehabilitation and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy.
Course Dates: May 20--21
Oncology of the Pelvic Floor Level 2B - partner needed for registration
Price: $600.00 Experience Level: Intermediate Contact Hours: 19.25 hours
This course was designed to build on the information that was presented in Oncology of the Pelvic Floor Level 1.
Information will be provided focusing on gynecological and bladder cancers including risk factors, diagnosis, and prognosis. The participant will also understand the sequelae of the medical treatment of cancer and how this can impact a patient’s body and quality of life. Other topics include rehabilitation and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy.
Course Dates: December 9-10
Rachna Mehta, PT, DPT, CIMT, OCS, PRPC, RTY 200 is the author and instructor of the Acupressure for Optimal Pelvic Health course. Rachna brings a wealth of experience to her physical therapy practice and has a personal interest in various eastern holistic healing traditions.
As I walked into the room to greet a new patient, I quickly glanced at the prescription for Pelvic Floor Physical Therapy in her chart. The words “urinary retention” caught my attention. As I gathered her history, I learned that this patient had a history of high anxiety and had been to the ER twice within a few weeks with symptoms of urinary retention. She was now taught to self-catheterize herself to manage her symptoms. After comprehensive testing by her urologist ruled out obstructive and neurological causes, she was referred to pelvic floor therapy with a diagnosis of pelvic floor muscle tension and inability to relax her pelvic floor muscles.
Urinary retention, or the inability to voluntarily void urine, is one of the most prevalent presenting urologic complaints in the emergency department. Voluntary urination requires close coordination between muscles of the pelvic floor, bladder, and urethra, as well as the nerves innervating them.
Female urinary retention is either acute or chronic and can be categorized according to the International Continence Society as:
- Complete (full retention) or partial (high post-void residuals)
- Acute or chronic
- Symptomatic or asymptomatic
- Mechanism (obstructive or non-obstructive)
Two of the most common causes of chronic urinary retention in women are bladder muscle dysfunction and obstruction. The condition is important as it can lead to significant clinical problems if left untreated, such as bladder decompensation, hydronephrosis, renal failure, vesicoureteral reflux, nephrolithiasis, and urinary tract infections, as well as symptoms including suprapubic pain, feelings of incomplete emptying, weak urinary stream, urgency, and incontinence1.
The patient was anxious and worried and could not step out more than an hour away from her home as she feared she would need to return home to void. She could only void at her own home and her social life was extremely limited due to these voiding restrictions. Given her high anxiety, I initiated Acupressure points for Anxiety in her program as an evidence-based holistic practice.
Acupressure is widely considered to be a powerful Complementary & Alternative Medicine (CAM) therapy and is gaining acceptance within the medical community as part of an Integrative medicine approach. It draws its roots from Acupuncture which is part of Traditional Chinese Medicine (TCM) believed to be over 3000 years old. TCM is based on Meridian theory where key Acupressure points (or Acupoints ) lie along specific meridian lines and are connected to the visceral functions of vital organ systems.
Research shows that Acupressure points have been used with Emotional Freedom Techniques (EFT) as well as for the management of pain, anxiety, nausea, fatigue, urinary incontinence, constipation, and symptom management. Studies over the past few decades have found that Acupressure points transmit energy or the vital Qi (life force energy ) through interstitial connective tissue with potentially powerful integrative applications through multiple systems.
Acupressure has demonstrated the ability to improve heart rate variability, and thus decrease sympathetic nervous system activity. By decreasing sympathetic nervous system stimulation, the release of stress hormones such as epinephrine and cortisol is decreased, and the relaxation response can be augmented, which may correlate with decreasing levels of pain, stress, and anxiety2.
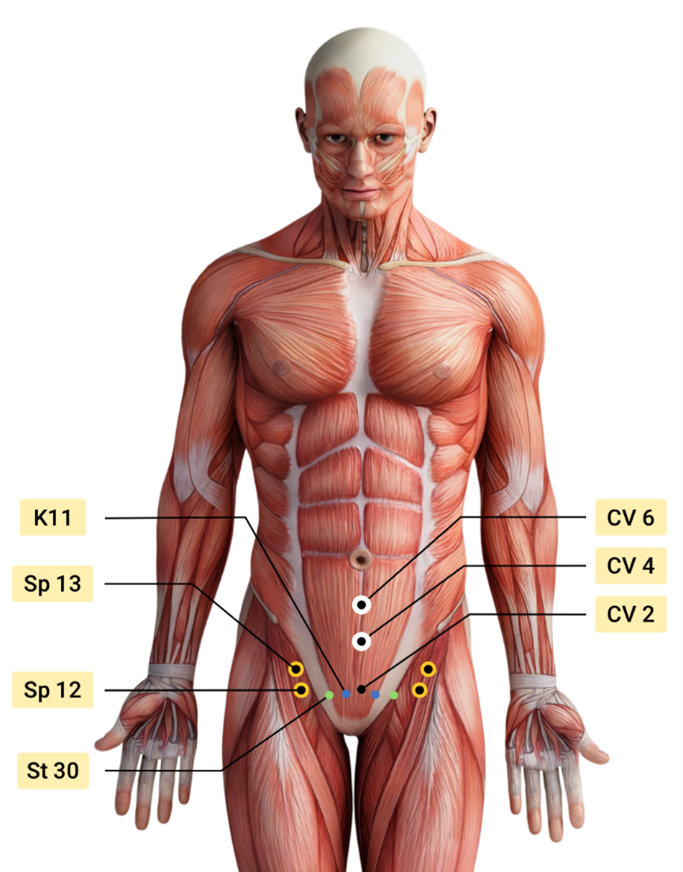
Over the next few weeks, the patient was treated by a multidisciplinary team including her Primary Care Physician, Psychologist, Acupuncturist, and Pelvic floor Physical Therapist. Integrating Acupressure along with manual therapy, behavioral modifications, exercises, breath work and stretching, key potent points in the Central Channel, Kidney, Stomach, Spleen, and Bladder meridians were utilized to down-regulate her nervous system and improve the physiological functioning of her vital organs.
The patient was also taught to use perineal acupressure points for the management of intermittent constipation. The patient learned and practiced daily an Acupressure Anxiety points regimen along with traditional rehabilitation exercises, and became calmer and more mindful with complete resolution of urinary retention symptoms. She could now step outside her home and use public bathrooms which socially was a big achievement for her.
The course Acupressure for Optimal Pelvic Health next offered on Feb 4th -5th 2023 explores Acupressure as an evidence-based modality for the management of Anxiety, Stress, Pain, and Symptom management. The course also teaches two programs with specific potent points for Anxiety and for Daily Wellness and introduces Yin Yoga as a complementary practice to Acupressure. This course is curated and taught by Rachna Mehta PT, DPT, CIMT, PRPC, RYT 200. Rachna has integrated Acupressure as part of her rehabilitation toolbox for several years now bringing holistic healing and wellness to her patients.
References
- Leslie SW, Rawla P, Dougherty JM. Female Urinary Retention. [Updated 2022 Nov 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538497/
- Monson E, Arney D, Benham B, et al. Beyond Pills: Acupressure Impact on Self-Rated Pain and Anxiety Scores. J Altern Complement Med. 2019;25(5):517-521.
- Au DW, Tsang HW, Ling PP, Leung CH, Ip PK, Cheung WM. Effects of acupressure on anxiety: a systematic review and meta-analysis. Acupunct Med. 2015;33(5):353-359. doi:10.1136/acupmed-2014-010720
- Son CG. Clinical application of single acupoint (HT7). Integr Med Res. 2019;8(4):227-228.
- Kwon CY, Lee B. Acupuncture or Acupressure on Yintang (EX-HN 3) for Anxiety: A Preliminary Review. Med Acupunct. 2018;30(2):73-79.
- Abbott, R., Ayres, I., Hui, E. et al. Effect of Perineal Self-Acupressure on Constipation: A Randomized Controlled Trial. J GEN INTERN MED30, 434–439 (2015).
Acupressure for Optimal Pelvic Health
Course Dates:
February 4-5, June 3-4, October 14-15
Price: $450
Experience Level: Beginner
Contact Hours: 12.50
Description: This continuing education course is a two-day seminar that offers participants an evidence-based perspective on the application of Acupressure for evaluating and treating a host of pelvic health conditions including bowel, bladder, and pelvic pain issues. The course explores a brief history of Acupressure, its roots in Acupuncture and Traditional Chinese Medicine (TCM), and presents current evidence that supports the use of complementary and alternative medicine as an adjunct to western medicine. TCM concepts of Meridian theory and energy channels are presented with scientific evidence of Acupoints transmitting energy through interstitial connective tissue with potentially powerful integrative applications through multiple systems.
Lectures will present evidence on the use of potent Acupressure points and combinations of points for treating a variety of pelvic health conditions including chronic pelvic pain, dysmenorrhea, constipation, digestive disturbances, and urinary dysfunctions to name a few. Key acupoints for decreasing anxiety, stress, and bringing the body back to a state of physiological balance are integrated throughout the course.
Participants will be instructed through live lectures and demonstrations on the anatomic location and mapping of acupressure points along five major meridians including the spleen, stomach, kidney, urinary bladder, and gall bladder meridians. Key associated points in the pericardium, large intestine, small intestine, lung, and liver meridians as well as the governing and conception vessels will also be introduced. The course offers a brief introduction to Yin yoga and explores Yin poses within each meridian to channelize energy through neurodynamic pathways to promote healing across multiple systems. Participants will learn how to create home programs and exercise sequences and will be able to integrate acupressure and Yin yoga into their orthopedic and pelvic health interventions.
Mora Pluchino, PT, DPT, PRPC (Faculty member, and Sr. TA) is a graduate of Stockton University with a BS in Biology (2007) and a Doctorate of Physical Therapy (2009). Mora authored and instructs Ethical Concerns for Pelvic Health Professionals and Ethical Considerations from a Legal Lens.
When I used to hear the word “ethics requirement,” I would wrinkle my nose and find the cheapest, quickest course to fulfill my New Jersey requirement. I would sit through it and count down the hours. It was not out of a lack of respect for the continuing educator or the importance of the material. I just felt, no matter how the material was presented it was just dry and did not feel like it applied to my more niched areas of practice.
As I dove deeper into pelvic floor treatment and the pelvic floor community, I realized there was such a need for us to have these conversations on the topic of ethics. A lot of questions posted on social media forums and groups have an underlying ethical component and practitioners are not necessarily aware. The more I researched, the more I realized these topics are so complex and can be very interesting when applied to the daily life of a pelvic health provider
Let’s talk about how you can know if something has an ethical component or concern. There are a variety of tests and measures to assess ethical situations and we review these in the class Ethical Concerns for the Pelvic Health Professional. If you are wondering if some of the clinical questions you have are actually founded in ethics you may find yourself asking questions like the following.
One of my favorite ways to assess an ethical question is by using the Kidder’s Ethical Decision Making Model. The fourth step of this model includes four checkpoints that can be helpful for quick clinical questions. These give us an idea of ways to recognize right versus wrong in scenarios and how we can correct or act accordingly. The four tests proposed by kidder are “The Legal Test,” “The Stench Test,” “The Front Page Test” and “The Mom Test” (Ferrier, 2021). If an ethical concern does not pass one of these tests, it does not have merit as an ethical course of action. If something doesn’t pass these tests, the right versus wrong aspect is a moral temptation and a person has to decide which option they would like to choose. We all have different moral compasses and backgrounds and so each person’s comfort level with these decisions may be different.
If a scenario arises, we start with “The Legal Test.” This is where we think about whether an action (or inaction) is legal or not. This may require some research or consultation if we do not know the answers. “The Stench Test” tests a person’s inner moral intuition. How does it feel with how you have been raised and when referenced against your moral foundation? “The Front Page Test” encourages a person to theorize how they would feel if the ethical situation they are thinking about were to be on the front page of a newspaper. It is a publicity test, do you want that to be how the world sees you, your clinic, your practice, your skills, etc? “The Mom Test” makes us reference all those who have been moral examples or might pass judgment on decisions we make (Ferrier, 2021).
Knowing these tests, look at the scenarios at the end of this blog. Imagine how you might run through the four Kidder Tests clinically. This can be great practice for clinical decision making. Like any skill, the more we practice, the more confident we are in the skill and the easier it is to do the task.
Ultimately with ethical decision making, there is a lot more “grey area” and “it depends” answers than there are clear cut scenarios. We can be much more comfortable with the decisions we make based on how we have examined the information and considered all options and outcomes. One of the positives of this class, Ethical Concerns for the Pelvic Health Professional - January 29, 2023, is having an audience of peers to talk through real clinical concerns and situations to problem solve and get input on things that may be weighing on a provider.
Scenario 1: Your patient comes in and tells you that their partner yells at them on a regular basis and controls how they can spend their money.
- The Legal Test: What are your legal abilities and obligations here?
- The Stench Test: How do you feel about this?
- The Front Page Test: If someone posted the story “Therapist told about XYZ and does ABC” how would you feel?
- The Mom Test: How would your parent/ caregiver feel about your decision on this scenario?
Scenario 2: A patient tells you that their practitioner forced them to have a pelvic examination without explaining the procedure and continued after the patient asked them to stop.
- The Legal Test: Is what this practitioner did legal?
- The Stench Test: What is your gut feeling in this scenario?
- The Front Page Test: If someone wrote a review about your practice and included this story, would it be a positive for your practice?
- The Mom Test: How would your favorite clinical instructor have felt about this situation?
Scenario 3: You have been invited to an affiliate program with a popular medical device company. You have the opportunity to make $15 for every patient care item you can sell in your clinic.
- The Legal Test: Are there any legal implications?
- The Stench Test: How do you feel with a quick “right versus wrong” decision here?
- The Front Page Test: How could you advertise this for your clinic in a way that is positive?
- The Mom Test: If someone posted this situation in a Facebook Pelvic Support Group, what would the response be?
Resource:
Ferrier, Patricia. Applying Kidder's ethical decision making model - in this article, the author uses a model of. Studocu. (2021). Retrieved December 26, 2022, from https://www.studocu.com/en-us/document/florida-institute-of-technology/introduction-to-behavior-analysis/applying-kidders-ethical-decision-making-model/20045486
Ethical Concerns for Pelvic Health Professionals

Course Dates:
January 29, September 16
Price: $175
Experience Level: Beginner
Contact Hours: 6
Description: The purpose of this class is to explore the ethical challenges Pelvic Health Practitioners may experience including consent, managing trauma and abuse, and preventing misconduct. This includes basic decisions for billing, patient care, safety, and compliance. Pelvic Rehabilitation comes with additional layers of vulnerability and ethical challenges due to the anatomical areas being treated, topics being discussed, and intimacy of sessions

Megan Pribyl, PT, CMPT is a practicing physical therapist at the Olathe Medical Center in Olathe, KS treating a diverse outpatient population in orthopedics including pelvic rehabilitation. Megan’s longstanding passion for both nutritional sciences and manual therapy has culminated in the creation of her remote course, Nutrition Perspectives for the Pelvic Rehab Therapist, designed to propel understanding of human physiology as it relates to pelvic conditions, pain, healing, and therapeutic response. She harnesses her passion to continually update this course with cutting-edge discoveries creating a unique experience sure to elevate your level of appreciation for the complex and fascinating nature of clinical presentations in orthopedic manual therapy and pelvic rehabilitation.
It has been nearly 8 years since I taught my first in-person rendition of “Nutrition Perspectives for the Pelvic Rehab Therapist” in Seattle, WA through Herman & Wallace – and over a decade since I began writing the course in earnest. Creating and teaching this course has been an honor for me and truly a full-circle opportunity to share my passion for nutrition with other clinicians. The mission of the course is to create a ripple effect from one person to the next. But if there’s anything the last couple of years has taught me, it’s that we still have a long way to travel to reach the destination of fully integrated care centered on the whole person. As a guide, I tap the growing body of literature on nutrition and health to help show us the way.
I recall having taught this course on 11 occasions in-person between June 2015 and October 2019 at gracious site host clinics nationwide. I enjoyed each and every one of these experiences. Since the 2020 pivot to remote format, I have taught Nutrition Perspectives via Zoom 18 times - after we were faced with restrictions on traveling and gathering.
Having taught Nutrition Perspectives in both formats, I’d like to share with you first why I love teaching this course, and second why I love teaching it in its remote format. It truly is a class perfectly suited to this mode of delivery.
First, why I love teaching this course:
It is my passion to share nutrition information with peers in pelvic rehab. Before becoming a PT, I studied nutrition as an undergrad. After becoming a PT, and more specifically a pelvic PT, it became crystal clear that we needed to incorporate the essence of nutritional sciences into pelvic rehab– and even into general clinical practice. Nutrition Perspectives became my answer to the burning and urgent questions I had about how we could blend the worlds of rehabilitation and nutrition. I scoured the literature to find answers – and what I found was astonishing. Paradigm shifting. Compelling.
Early in my career, I would only sporadically encounter patients who would experience what I would now describe as “functional gastro-intestinal disorders with extra-intestinal manifestations”. Fast-forwarding to today, it is rare to see a patient who does not experience any conditions such as GERD, constipation, gas/abdominal pain/bloating/discomfort, anxiety, depression, and complex or chronic pain conditions. Because of this reality, it has become essential for healthcare providers to have a basic working knowledge of functional nutrition. Especially providers in pelvic rehabilitation. Having a working knowledge of these conditions and potential nutritional underpinnings can help us better understand and serve our clients.
Not only does nutrition have significant relevance to our patients – it is relevant to each of us as human beings! But be aware – the realm of nutrition appears chock-full of confusing contradictions. And our patients are now – more than ever – asking us for our thoughts on nutrition-related topics. They’re listening to podcasts. They’re reading social media posts and blogs. They’re watching short video clips to find quick answers to complex questions. And they want to run some of their questions by you – their trusted health professional ally. You want to feel confident and competent in what you’re sharing. My mission is to make evidence-informed information accessible and relevant to you, the practicing clinician so then you can, in turn, share with confidence and competence.

Now, on to why I love teaching this course remotely:
Don’t get me wrong – I love to travel. But imagine traveling alone to new cities -not as a free-spirited adventure solo traveler – but instead as an idealistic instructor who doesn’t want to be without any supplies needed for teaching a course far from home! This translates to a very heavy suitcase filled with visual aids and lab supplies. This humongous check-in bag contains items necessary to conduct the course descriptively – books, empty product containers, glass jars (yes, GLASS), carefully packaged kefir grains, a SCOBY, bowls, spoons, kitchen towels, and those hard-to-find food items that one can’t be certain to find in an unfamiliar city. And a tablecloth. Because when we’re talking about food with guests, presentation is important!
Now imagine navigating travel challenges with said heavy, giant suitcase; chucking it on and off a rental car bus during a cold rainstorm for example.. Imagine pushing it down a carpeted hotel hallway that is so plush, it prohibits the wheels from functioning properly. Imagine repacking in 15 minutes what took 3 hours to initially pack in order to catch a return flight home.
This was the reality of logistics I eagerly and enthusiastically took on to be able to teach this class. But that giant suitcase couldn’t hold even close to everything I wanted to share, and it actually was a bit cumbersome to manage. Maybe a lot cumbersome. Always plastered with the bright orange “HEAVY” sticker warning – there was a limit to what I could bring along to live course events.
When we first transitioned this course to remote format, it was a quick response to begin offering CEUs when lockdown mode began. The silver lining, we discovered, was that the remote format for this course was in fact – much better than the live event format.
Now, all the necessary supplies are right where I need them to best instruct. Plus, predictable kitchen and lecture spaces create a seamless experience for the participants. Teaching from home has been life-changing as an instructor. I can practice what I preach about nourishing the nervous system and mitigating stress with lifestyle choices. It is nourishing to be able to sleep well at home the nights before I teach. Adequate rest is a superpower that allows me to give my best well-rested self to the participants.
The remote format is not just nourishing to me, but also to the participants who can attend from the comfort of home or familiarity of a clinic. Wherever you are, you can take the course. No airports, no suitcases, nor carpeted hotel hallways. That’s accessibility. That’s getting this information into the hands and minds of providers in locations all around this country and beyond. We need this accessibility if we ever hope to reach our destination of fully integrative care of the whole person – for all.
For these reasons, Nutrition Perspectives for the Pelvic Rehab Therapist will remain in this remote format – even as our lives begin to involve travel and in-person events again. All good things. But I do hope you enjoy taking Nutrition Perspectives as much as I enjoy teaching it. I invite you to join me on the journey toward implementing more integrative care as standard practice. It’s not always an easy road, nor the popular road. And sometimes it feels as hard as dragging a giant, heavy suitcase behind you. But it’s a path worth taking – one that will be fruitful for both you and the clients you serve. Let’s travel it together.
Nutrition Perspectives for the Pelvic Rehab Therapist will be offered quarterly in 2023: January 21-22, June 10-11, September 16-17, and December 2-3.
Nutrition Perspectives for the Pelvic Rehab Therapist

Course Dates:
January 21-22, June 10-11, September 16-17, and December 2-3
Price: $525
Experience Level: Beginner
Contact Hours: 17.75
Description: Participants will be introduced to the latest research in nutrition through immersive lectures and hands-on labs. The course will cover essential digestion concepts, nourishment strategies, and the interconnected nature of physical and emotional health across the lifespan. Further, clinicians will delve into nutritional relevancies in bowel and bladder dysfunction, pelvic health, pain, and healing. Labs throughout include insightful demonstrations and breakout sessions. The course participant will acquire new, readily applicable tools for patient empowerment, engagement, and self-management utilizing presented principles.
Faculty member, and Sr. TA, Mora Pluchino, PT, DPT, PRPC is a graduate of Stockton University with a BS in Biology (2007) and a Doctorate of Physical Therapy (2009). Mora authored and instructs Ethical Concerns for Pelvic Health Professionals and Ethical Considerations from a Legal Lens.
- "I want to start my own practice but I'm not sure if I need to hire a lawyer to help!"
- "I have a problematic patient that I want to discontinue seeing, but don't want to be guilty of abandonment of care."
- "I am so confused by the types of clinical insurance that I am required to have!"
- "I want to hire an employee and include a non-compete clause in their employment contract!"
- "I want to start my own cash-based practice and need help with this process!"
- "I plan to market my practice for THIS population, is it legal to exclude THAT group of people?"
With the end of 2022 approaching, now is the perfect time to take a pelvic health-focused ethics class. For many states, licensed professionals have to fulfill an ethics continuing education requirement, including physical therapists, occupational therapists, mental health, and many other healthcare providers.
I started writing this series a year ago. I struggled to find a class to meet my biannual ethics requirement for New Jersey that was related to my practice in pelvic health. I soon realized that as a pelvic health provider and educator, the most popular questions that come up for practitioners, secondary only to specific treatment interventions, are ethical in nature.
- "Is ________ ok?"
- "What happens if ________ happens?"
- "Can a patient sue me for ______?"
- "How do I do ________ legally?"
Providers want to know that they are providing services that are legal and ethical. Even if you have never considered yourself as being overly concerned with the topic of ethics, you have probably had these thoughts. That was certainly the case for me! The further I fell down the rabbit hole of ethics, the more I realized it affects our day-to-day clinical life minute by minute. Ethics is the study of right versus wrong and how we make those personal qualifying decisions. So this covers everything from cleaning procedures, scheduling, patient care, and more!
Practitioners want to know that they will not be open to any legal action for the care and services provided. This usually requires more awareness and knowledge than just purchasing an annual liability insurance policy. Each provider and clinical environment has their own ethos, policies, and procedures, but there are also larger existing rules and laws to help guide providers to provide the best possible care.
In Ethical Concerns for the Pelvic Health Professional, we discuss the basics of doing no harm to our patients, obtaining informed consent, and decision-making based on different ethical models. The goal here is to send you to work immediately following this class feeling more confident in ethical labeling and decision-making. This class is a more global and essential look at the concept of ethics as applied to pelvic health.
The sole purpose of Ethical Considerations from a Legal Lens is to explore the ethical challenges pelvic health practitioners may experience from a health law perspective. This course is for any pelvic health professional looking to build skills for ethical evaluation, problem-solving, and derivation of solutions with a specific focus on legalities and related concepts.
This series of ethics-related classes is meant to build your clinical character and problem-solving abilities in what feels like "sticky" situations and help to guide you to clinical and business decisions that make you feel comfortable at the end of a work day.
To sweeten up this class series, each offering has an expert join the discussion on certain topics and case studies, to offer additional perspectives and points of view to the discussion.
I am looking forward to having an open discussion about the ethical and legal considerations for our profession at the next offered class on December 10th, 2022!
Ethical Considerations from a Legal Lens
Course Dates:
December 10, 2022
June 3, 2023
November 12, 2023
Price: $175
Experience Level: Beginner
Contact Hours: 6
Description: This one-day remote course covers ethical considerations from a legal lens for professionals working in the area of Pelvic Health. In general, Health Care Professionals have many day-to-day ethical considerations to “do no harm.” This includes basic decisions for billing, patient care, safety, and compliance. Pelvic Rehabilitation comes with additional layers of vulnerability and ethical challenges, and the legalities of pelvic health can add further complications for patient care, business, and clinical practice decisions.
The purpose of this class is to explore the ethical challenges Pelvic Health Practitioners may experience from a health law perspective. This course is for any Pelvic Health Professional looking to build skills for ethical evaluation, problem-solving, and derivation of solutions with a specific focus on the legalities and related concepts. Prior to the live aspect of this course, participants will be asked to review the ethical framework and definitions via pre-recorded lecture and take Core Values Self Assessment. Live instruction will review applicable health laws and legal terms that converge with the pelvic health world. This will be followed by case study discussion in small groups, followed by a large group discussion with input from the instructor and a legal expert/ educator. The remainder of this course is meant to be a guided discussion through the legal and ethical struggles of the pelvic health practitioner.
Ethical Concerns for Pelvic Health Professionals - Remote Course
Course Dates:
January 29, 2023
September 16,2023
Price: $175
Experience Level: Beginner
Contact Hours: 6
Description: This course is for any Pelvic Health Professional looking to build skills for ethical evaluation, problem-solving, and derivation of solutions, and explores the ethical challenges practitioners may experience including consent, managing trauma and abuse, and preventing misconduct. Prior to the live aspect of this course, participants will be asked to review the ethical framework and definitions via pre-recorded lecture and take Core Values Self Assessment. Live instruction will review the ways in which patients and practitioners can be vulnerable in the pelvic health treatment setting and how to address this. This will be followed by case study discussion in small groups, followed by large group discussion with input from the instructor and an ethics expert/ educator. The remainder of this course is meant to be a guided discussion through the ethical struggles of the pelvic health practitioner
Kelly Sammis, PT, OCS, CLT, AFDN-S is a physical therapist, educator of dry needling and all things pelvic, Pilates instructor, wife, and mama living and working in Parker, Colorado. She specializes in the treatment of male and female pelvic floor dysfunction, athletic injury/return to sport, sports performance, and persistent pain. Her formal education took place at Ohio University (2007) and The University of St Augustine for Health Sciences (2010). Kelly serves as the lead faculty developing and teaching dry needling and pelvic health courses nationwide. Kelly co-instructs the Herman & Wallace Dry Needling courses along with site fellow faculty member Tina Anderson, MS PT.
Urinary incontinence (UI) is defined as ‘any complaint of involuntary leakage or urine’ that has several different subtypes based on when this leakage occurs1. UI is a common and relevant condition that has a profound influence on well-being and quality of life of many patients worldwide. Millions of men and women throughout the world are affected. According to our body of evidence, UI can affect anywhere between 5-70% of the female population2-4 and 11-32% of the male population5,6, contributing to decreased participation in preferred daily, work and recreational activities alongside an immense economic burden for some of those affected.1-7These symptoms have not only been shown to have a significant impact on a person’s quality of life, but also on their mental health status.7
While UI is both common and very bothersome, it is also very treatable. I would love nothing more than to see our society and healthcare continuum recognize that UI is something that is ABNORMAL versus the typical categorization that it is a normal part of the aging, postpartum or postoperative experience.
Common, not normal. Common, but treatable.
UI can be treated with lifestyle and behavioral interventions, bladder training, electrical stimulation, pelvic floor muscle training (PFMT) with or without biofeedback, physical therapy, neuromodulation, periurethral injections and, in some cases, surgical intervention. 5,8
Understanding the continence mechanism
In a well-functioning pelvic floor, the connective tissue of the ligaments and fascia act together with the pelvic floor musculature to counteract the impact of any increase in intra-abdominal pressure and ground reaction forces, helping to maintain our continence.8-10 This is an automatic function, requiring no need to think about voluntary contraction of the pelvic floor musculature. 8 When this mechanism is not working adequately, which can undoubtedly be multifactorial, urinary incontinence may occur.
The external urethral sphincter mechanism is a complex system of striated muscle which includes fiber blends from the urogenital triangle musculature and the anterior muscle bundle of the levator ani. 11 The good news here is that we, as rehabilitative clinicians, have many different tissue targets for treatment of UI.
Dry Needling and UI
Dry needling (DN) encompasses the insertion of solid filament, non-injectate needles into, alongside or around muscles, nerves or connective tissues with or without mechanical and/or electrical stimulation for the management of pain and dysfunction in neuromusculoskeletal conditions. DN is both effective and efficient in modulating the central and peripheral nervous systems as well as the somatic tissues, including the pelvic floor.
There is a growing body of evidence that has provided us with an understanding on how to best utilize this technique in our clinical practice as it relates to UI.12-17 With the external urethral sphincter and associated tissues being a main player in our urinary continence mechanism, it provides a road map on how we can utilize DN to treat UI. This boils down to two things: (1) tissue specificity and (2) utilization of electrical stimulation. DN provides us with an avenue to directly influence a specific tissue as we are able to use an indwelling needle electrode placed strategically into a muscular or perineural tissue target. Using that tactically placed indwelling electrode we can then precisely deliver electrical stimulation, essentially speaking the language of the neuromotor system, making this technique one of the most effective tools we have as rehabilitative clinicians to treat UI.
Ultimately, we are able to stimulate the pudendal nerve alongside the targeted tissues. This can help to improve electric activation, proprioception and coordination in pelvic floor contraction during situations that contribute to UI.18,19,22 Additionally, the pudendal nerve is an efferent nerve for the external urethral sphincter, so this treatment is capable of increasing the pressure of urethral closure, improving UI. Another important factor is that electrical stimulation has been shown to increase blood flow to the urethra and pelvic floor musculature, lending towards improvements in neuromuscular connections, muscle fiber function and genital atrophy, all leading to improvements in the mechanism of urethral closure. 19-22
The power of the tissue reset that DN provides has changed clinical outcomes for the better. It has, and will continue to, positively impact and change the lives of many patients through facilitating a more balanced homeostatic baseline within the tissues, healthier motor recruitment patterns and optimal neuromuscular utility to re-establish function. Want to add this tool to your clinical practice? Check out our Dry Needling course offerings with Herman & Wallace!
References:
- Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/ International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26
- Milson I and Gyhagen M. The prevalence of urinary incontinence. Climacteric. 2019;22(3):217-222
- Carryer, J, Weststrate, J, Yeung, P et al. Prevalence of key care indicators of pressure injuries, incontinence, malnutrition, and falls among older adults living in nursing homes in New Zealand. Research In nursing & Health. 2017;40(6):555–563
- Damian, J, Pastor-Barriuso, R, Garcia Lopez, FJ et al. Urinary incontinence and mortality among older adults residing in care homes. Journal of Advanced Nursing. 2017;73(3):688–699
- Gacci M, Sakalis VI, Karavitakis M et al. European Association of Urology guidelines on male urinary incontinence. European Urology. 2022;82:387-398
- Cao C, Zhang C, Sriskandarajah C et al. Trends and racial disparities in the prevalence of urinary incontinence among men in the USA, 2001-2020. European Urology Focus. 2022; https://doi.org/10.1016/j.euf.2022.04.015
- Krhut J, Gartner M, Mokris J et al. Effect of severity of urinary incontinence on quality of life in women. Neurourol Urodyn. 2018;37:1925–1930
- Bo K. Physiotherapy management of urinary incontinence in females. Journal of Physiotherapy. 2020;
- Ashton-Miller J, DeLancey JOL. Functional anatomy of the female pelvic floor. In: Bø K, Berghmans B, Van Kampen M, Mørkved S, eds. Evidence based physical therapy for the pelvic floor. Bridging science and clinical practice. Chapter 3. Edinburgh: Elsevier; 2015:19–34
- DeLancey JOL, Low LK, Miller JM et al. Graphic integration of causal factors of pelvic floor disorders: an integrated life span model. Am J Obstet Gynecol. 2008;199:610.e1–610.e5
- Suriyut J, Muro S, Baramee P et al. Various significant connections of the male pelvic floor muscles with special reference to the anal and urethral sphincter muscles. Anatomincal Science Internatiional. 2020;95:305-312
- Feng X, Lv J, Li M et al. Short-term efficacy and mechanism of electric pudendal nerve stimulation versus pelvic floor muscle training plus transanal electrical stimulation in treating post-radical prostatectomy urinary incontinence. Oncology. 2022;160:168-175
- Wang S, Zhang S. Simultaneous perineal ultrasound and vaginal pressure measurement prove the action of electrical pudendal nerve stimulation in treating female stress incontinence. BJU Int. 2012;110:1338–1343
- Wang S, Lv J, Feng X, Wang G, Lv T. Efficacy of electrical pudendal nerve stimulation in treating female stress incontinence. Urology. 2016;91:64–69
- Wang S, Lv J, Feng X, Lv T. Efficacy of electrical pudendal nerve stimulation versus transvaginal electrical stimulation in treating female idiopathic urgency urinary incontinence. J Urology. 2017;197:1496–1501
- Wang S, Zhang S, Zhao L. Long-term efficacy of electric pudendal nerve stimulation for urgency-frequency syndrome in women. International Urogynecology Journal. 2014;25:397-402.
- Li T, Feng X, Lv J et al. Short-term clinical efficacy of electric pudendal nerve stimulation of neurogenic lower urinary tract disease: a pilot research. Urology. 2018;112:69-73
- Monga AK, Tracey MR, Subbaroyan J. A systematic review of clinical studies of electrical stimulation for treatment of lower urinary tract dysfunction. Int Urogynecol J. 2002;23:993–1005
- Chai TC, Steers WD. Neurophysiology of micturition and continence in women. Int Urogynecol Urol. 1997;8:85–97
- Spruijt J, Vierhout M, Verstraeten R, et al. Vaginal electrical stimulation of the pelvic floor: a randomized feasibility study in urinary incontinent elderly women. Acta Obstet Gynecol Scand. 2003;82:1043–8
- Balcom AH, Wiatrak M, Biefeld T et al. Initial experience with home therapeutic electrical stimulation for continence in myelomenin-gocele population. J Urol. 1997;158:1272–6
- Correia GN, Pereira VS, Hirakawa HS et al. Effects of surface and intravaginal electrical stimulation in the treatment of women with stress urinary incontinence: randomized controlled trial. Euro J of Ob & Gyn and Reproductive Bio. 2014;173:113-118
Dry Needling and Pelvic Health - Live Course
Course Dates:
Worcester, MA - November 12-13, 2022
Katy, TX - January 21-22, 2023
Birmingham, AL - September 16-17, 2023
Price: $995
Experience Level: Beginner
Contact Hours: 26
Description: This is the foundational dry needling course in our three course pelvic health series. Practitioners will learn an innovative approach to treating clients with pelvic floor and neuromusculoskeletal dysfunction commonly associated with lumbopelvic pain, incontinence, voiding dysfunction and/or sexual pain or dysfunction. This foundational dry needling course will instruct participants in the application of dry needling to female pelvic floor musculature and associated neuroanatomical structures including the lumbosacral spine, abdomen, pelvis, and hip joint complex. This course will provide a comprehensive review of anatomy, a strong emphasis on safety and precautions, ample lab time to optimize dry needling techniques, as well as dialogue surrounding clinical integration and relevant evidence.
Dry Needling and Pelvic Health: Advanced Concepts and Neuromodulation - Live Course
Course Dates:
Salt Lake City, UT - November 5-6, 2022
Price: $995
Experience Level: Advanced
Contact Hours: 26
Description: Dry Needling and Pelvic Health: Advanced Concepts and Neuromodulation is a lab intensive, hybrid course designed with the pelvic health practitioner in mind. This course is an innovative approach to treating clients with pelvic floor dysfunction commonly associated with pelvic pain, incontinence, voiding dysfunction and/or sexual pain or dysfunction. This advanced dry needling course will instruct participants in the application of dry needling to female and male pelvic floor musculature and associated neuroanatomical structures including the thoracolumbar spine, trunk, abdomen, pelvis and hip joint complex. This course will also discuss and integrate the concept of and techniques associated with neuromodulation. Additionally, there will be a comprehensive review of anatomy, a strong emphasis on safety and precautions, ample lab time to optimize dry needling techniques, as well as dialogue surrounding clinical integration and relevant evidence.
Dawn Sandalcidi, PT, RCMT, BCB-PMD can be found online at https://kidsbowelbladder.com/. Dawn is a long time instructor with Herman & Wallace and has generously shared her recent blog with The Pelvic Rehab Report. "Stool Withholding And Core Activation" can be found in its original post on her website here: https://kidsbowelbladder.com/stool-withholding-and-core-activation/.
What do they have in common?
About 9-12% of children suffer from functional constipation, which is the vicious cycle of retained stool causing rectal distention and subsequent loss of sensation and urge to defecate, which results in further stool retention. The exact physiologic causes for functional constipation are not completely understood.
We know the bowel absorbs water constantly. The longer stool sits in the rectum, the harder it becomes. For some children, this leads to very large stools that are uncomfortable or difficult to eliminate. In turn, these children may practice something called stool withholding (which may be the reason stool was sitting in the rectum too long in the first place).
There are many other reasons a child may withhold their stools beside the standard issues that functional constipation presents. Some other reasons for stool withholding include:
- Inability to generate intraabdominal pressure
- Availability, likes, and dislikes of the toilet
- Fear of having a bowel movement
- Perineal sensation issues
- Psychological concerns
- Pain with defecation
- Dietary contribution
- Illness or infection
- Medications
- And more
No matter how or why a child began withholding stools, it’s vital to treat the problem as soon as possible. When withholding and constipation go untreated, they can cause lifelong issues. In this article, we will explore the relationship between constipation and core control, specifically the child’s ability to generate intraabdominal pressure.
What are the Symptoms a Child May have When Practicing Stool Withholding?
Normally, when enough stool enters the rectum and it’s time for a bowel movement, the rectum will send messages to the brain to make you aware that it’s time to have a poop. Ideally, when you receive this message and become aware of your body’s need to defecate, you find a toilet and do so.
When a child regularly withholds stools, the stool may become retained in the rectum and cause rectal distention and a subsequent loss of sensation. Because the rectum isn’t able to sense its fullness, the messages are never sent to the brain, and the sense of urge to poop disappears.
Although children who withhold stools may not have the urge to poop, they can have other physical symptoms if their stool withholding causes stool retention.
Physical symptoms of stool retention include:
- Abdominal pain
- Offensive body odor
- Stools that clog the toilet
- Decreased appetite
- Urinary incontinence or frequency
- And more
Children who withhold stools do not always have retention, however, and sometimes will simply withhold stools due to their environment (such as being at school during the day), and poop as soon as they get home.
How Might Core Strength Relate to Stool Withholding?
I treated a 6-year-old child once who had a bowel movement every single day, but only after he fell asleep in his parents' arms. His parents hadn’t been able to transition him out of diapers because of this. His bowel movements were so predictable that his parents would wait for him to poop, then clean him up and put him back to bed.
This child was also autistic and did have issues with low tone. I discovered during examination of the child that he had a difficult time voluntarily contracting his core muscles. Rotational and balance activities were difficult for him to perform as well due to his lack of core control.
You may be wondering what the core has to do with constipation, or stool withholding specifically. For starters, you need adequate core strength in order to sit upright on the toilet. Without proper core control, children may develop poor toileting postures which can lead to difficulty with defecation.
Correct toileting posture involves first being able to have enough hip extension, back extension, and side-to-side control to balance in a seated position on the toilet seat. Seats of differing heights add to the complexity of good toileting posture.

Proper Body Position for Toileting
Ideally, your feet should be supported, not dangling (which is a common occurrence for our children using adult-sized toilets). Forearms should be resting on the thighs, and the hips should be bent to at least 90 degrees of flexion. The spine should be in a neutral position (no posterior pelvic tilt).
This position allows for the pelvic floor muscles to relax appropriately, and for the core muscles to activate enough in order to produce appropriate intraabdominal pressure.
Without appropriate intraabdominal pressure generation, it will be difficult for a child to push out their poop. This is precisely what we discovered with my patient who was withholding until she got into bed. When in her parents' arms she was flexed, it was easier for her to generate enough intraabdominal pressure to poop, and so she did!
Knowing the reason for his withholding allowed us to target treatment planning where he needed it the most.
How to Address Core Strength in Children who Withhold Stools
Once you’ve determined that core activation is a root issue, you’ll need to address it in order to see any change with your patient’s bowel habits. Parents are usually at their wit’s end and are looking to you for answers. Your physical exam is your best tool in identifying root causes of stool withholding.
Many children attending physical and/or occupational therapy do suffer from low tone. As we’ve learned, this can compound constipation issues and even lead to stool withholding.
With the child above, we worked on core activation exercises first in supine, then in prone on an incline, and gradually added challenge to his exercises until she was able to generate enough intraabdominal pressure to poop on the toilet independently.
Even if your patient does not suffer from low tone, core activation and training may still be indicated. Some children have difficulty with coordinating or timing appropriate muscle contraction and relaxation. Be sure to evaluate the core when treating patients who suffer from constipation and stool withholding.
These children may have difficulty crossing midline as well. Age-appropriate exercises to engage the core while also incorporating diagonal and midline-crossing motions will be beneficial for those patients.
Additionally, you’ll want to assess the rib cage. Oftentimes I find children who have difficulty with core control also have a wider rib angle and hence need upper abdominal engagement exercises.
Lastly, many of the children you’ll treat will need help with rotation. This is a common finding during examination and without addressing rotation, you’ll see much slower progress.

Treating Stool Withholding and Core Issues is Possible
So many children with constipation will not receive appropriate treatment during childhood and their problems will persist into adulthood. It’s our job as pediatric therapists to identify children in need of help. Many children with bowel and bladder problems will be seen in your clinics for other issues, and unfortunately never even bring up the bowel or bladder concerns.
I put together a list of 5 Screening Questions you can ask your patients to determine whether they might be suffering from bowel or bladder issues and not even know it. This is a quick and easy way to identify patients in need of pediatric pelvic floor therapy.
It’s a great idea to get in touch with your local pediatric pelvic floor specialist to be able to easily refer these patients. You can also become a pediatric pelvic floor therapist yourself by taking my online courses! I believe this patient population is severely underserved and have made it easier than ever to learn how to best support these children.
My courses are held live in various locations around the world throughout the year, but I also offer online options for you to be able to work at your own pace from the comfort of home. Inside my online courses, there is space in every module to leave comments or ask questions and they go directly to me.
Sign Up For the Pediatric Functional Gastrointestinal Disorders Remote Course.
I’ve also created a group online where those who have taken my courses can collaborate, receive my mentorship, and discuss any issues that come up along their pediatric pelvic floor therapy journey. The group is called KBB Professional Village.
Learn More about KBB Professional Village.
Pediatric Functional Gastrointestinal Disorders
Course Dates:
November 12-13, 2022
May 20-21, 2023
November 4-5, 2023
Price: $600
Experience Level: Intermediate
Contact Hours: 15
Description: This two-day, remote course is offered on Zoom and is the next step for therapists who focus on the pediatric pelvic floor patient population. It is designed to expand your knowledge of the development of normal bowel patterns in children, introduce the new Rome IV criteria (Zeevenhoovenet al. 2017), and review the anatomy and physiology of the GI system with emphasis on Pediatric Functional Gastrointestinal Disorders (FGID).
This course will delve into the most common types of functional constipation and the tests and measures used to assess it. Special emphasis on constipation with the coexistence of fecal incontinence (Nurko, Scott. 2011) and the psychological effects of these disorders will also be presented. Additionally, participants who have not yet been trained will learn external and internal anorectal PFM evaluation of the pediatric perineum. Indications for rectal balloon training and determining the appropriate patient will be instructed with lab. Functional defecatory positions for breathing and PFM relaxation, manual therapy techniques of the abdominal wall and viscera will be taught.