This post is a follow-up to the February 20th post written by Nancy Cullinane, "Pelvic Floor One is Heading to Kenya"
By the time folks are reading this, Nancy Cullinane, PT, MHS, WCS, Terri Lannigan, PT, DPT, OCS, and I will likely be in a warm, crowded classroom in Nairobi, Kenya helping 30+ “physios” navigate the world of misbehaving bladders, detailed anatomy description, and their first internal lab experiences. No doubt it will be both challenging and extremely rewarding. We are so grateful to the Herman & Wallace Pelvic Rehab Institute for sharing their curriculum in partnership with the Jackson Clinics Foundation to allow us to offer their valuable curriculum in order to affect positive health care changes.
I personally am humbled and honored to get to play a small but key role in the development of foundational knowledge and skills for these women PT’s who will no doubt change the lives of countless Kenyan women, and, consequently, their families.
My adventure truly began when I offered to write lectures on the topics of Fistula and FGM/C (female genital mutilation/cutting) and I began the process of crash course learning about these topics. The quest has taken me on a deep dive into professional journals, NGO websites, surgical procedure videos and insightful interviews with some of the pioneers working for years including “in the field” to help women in Africa and in countries where these issues are prevalent.
Before I began my research on the topic of fistula, I pretty much thought of a fistula as a hole between two structures in the body where it doesn’t belong, and narrowly thought of in terms of anal fistulas, acknowledging how lucky we are that there are skilled colorectal surgeons who can fix them. But after more research, my world view changed. (Operative word here being “world”).
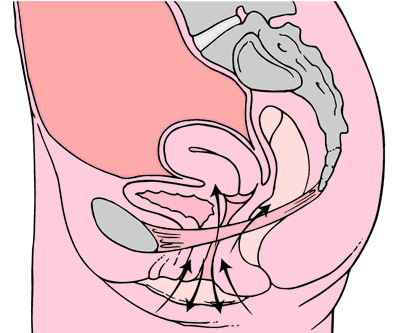
A fistula is an abnormal or surgically made passage between a hollow or tubular organ and the body surface, or between two hollow or tubular organs. For our purposes here today, I am referring to an abnormal hole or passage between the vagina and the bladder, or rectum, or both. When the fistula forms, urine and/or stool passes through the vagina. The results are that the woman becomes incontinent and cannot control the leakage because the vagina is not designed to control these types of body fluids.
According to the Worldwide Fistula Fund, there are ~ 2 million women and girls suffering from fistulas. Estimates range from 30 to 100 thousand new cases developing each year; 3-5 cases/1000 pregnancies in low-income countries. A woman may suffer for 1-9 years before seeking treatment. For women who develop fistula in their first pregnancy, 70% end up with no living children.
Vesicovaginal fistulas (VVF) can involve the bladder, ureters, urethra, and a small or large portion of the vaginal wall. Women with VVF will complain of constant urine leakage throughout the day and night, and because the bladder never fills enough to trigger the urge to void, they may stop using the toilet altogether. During the exam there may be pooling of urine in the vagina.
Rectovaginal Fistula is less common, and accounts for ~ 10% of the cases. Women with RVF complain of fecal incontinence and may report presence of stool in the vagina. These women often will also have VVF.
In Kenya, most fistulas are obstetric fistulas, which occur as a result of prolonged obstetric labor (POL). These are also called gynecologic, genital, or pelvic fistulas. Traumatic fistulas account for 17-24 % of the cases and are caused by rape, sexual or other trauma, and sometimes even from FGM/C. The other type of fistula by cause is iatrogenic, meaning unintentionally caused by a health care provider during procedures such as during a C-section, hysterectomy, or other pelvic surgery. Most fistulas seen in the US are of this type.
Prolonged Obstructed Labor most often occurs when the infant’s head descends into the pelvis, but cannot pass though because of cephalo-pelvic disproportion (mismatch between fetus head and mother’s pelvis) thus creating sustained pressure on the tissues separating the tissues of the vagina and bladder or rectum, (or both) leading to a lack of blood flow and ultimately to necrosis of the tissue, and the development of the fistula. Those who develop this type of fistula spend an average of 3.8 days in labor (start of uterine contractions), some up to a week. In these cases, family members or traditional birth attendants may not recognize this is occurring, and even if they do, they may not have the instrumentation, the facilities or the skills necessary to handle the situation with an instrumental delivery or a C-section. And many of these women are in remote locations without transportation to appropriate facilities or lack the money to pay for procedures.
There are many adverse events and medical consequences that can result as a result of untreated obstetrical fistulas including the death of the baby in 90% of the cases. Physical effects besides the incontinence previously mentioned can include lower extremity nerve damage, which can be disabling for these women, along with a host of other physical and systemic health issues. The social isolation, ostracization by community, divorce, and loss of employment can lead to depression, premature lifespan, and sometimes suicide.
The good news is there are several great organizations making a difference.
In most cases, surgery is needed to repair the fistula. Sometimes, however, if the fistula is identified very early, it may be treated by placing a catheter into the bladder and allowing the tissues to heal and close on their own, and this is more viable in high-income countries after iatrogenic fistulas, but unfortunately, most women in the low-income countries have to wait for months or years before they receive any medical care.
There is an 80-90% cure rate depending on the severity, but according to the Worldwide Fistula Fund, 90% are left untreated, as the treatment capacity is only around 15,000 per year for the 100,00 new patients requiring it. Prevention is vital.
Despite successful repair of vesicovaginal fistulas, research shows that 15-35% of women report post-op incontinence at the time of discharge from the hospital, and that 45-100% of women may become incontinent in the years following their repair. Studies suggest that scar tissue-fibrosis of the abdominal wall and pelvis, and vaginal stenosis are strongly associated with post-operative incontinence.
According to research by Castille, Y-J et al in Int. J Gynecology Obstet 2014, there can be improved outcome of surgery both in terms of successful closure of vesicovaginal fistula and reduced risk of persistent urinary incontinence if women are taught a correct pelvic floor muscle contraction and advised to practice PFM exercise. Other studies have shown a positive effect from pre and post op PT in both post op urinary incontinence and PFM strength and endurance with a reduction of incontinence in more than 70% of treated patients, with improvements maintained at the 1year follow up. SO, THIS IS ONE REASON WE ARE SO EXCITED TO BE GOING TO KENYA!
I inquired about the use of dilators via email communication with surgeon Rachel Pope , MD MPH who has done extensive work in Malawi with women who have suffered from fistula, including the use of dilators, and her response was: “in women who have had obstetric fistula the dilators seem only marginally helpful after standard fistula repairs. The key is to have a good vaginal reconstructive surgery where skin flaps that still maintain their blood supply replace the area in the vagina previously covered by scar tissue. The dilators work exceedingly well when there is healthy tissue in place, and I think the overall outcomes are better for women in those scenarios compared to the cement-like scar we often see in women with fistulas.”
In the US, there are specialist surgeons who provide surgical repairs. While genitourinary fistulas can occur because of obstructed labor and operative deliveries in high income countries, they can also occur in a variety of pelvic surgeries, post pelvic radiation, as well as in cases of cancer, infections, with stones, and as well etiology includes instrumentations such as D&Cs, catheters, endoscopic trauma, and pessaries, and as well in cases of foreign bodies, accidental trauma, and for congenital reasons. As pelvic therapists it is important to know your patients’ surgical and medical history and to pay special attention to the patient’s history regarding their incontinence description and onset and be mindful during exam to notice possible pooling of urine in the vagina. Though rare in terms of occurrence, we should be aware of the possibility and may play a role in referring the patient to a physician who can do further diagnostic testing
In conclusion, I want to thank UK physiotherapist Gill Brook MCSP (DSA) CSP MSC, president of the IOPTWH who shared with me by interview her knowledge of fistula and experiences with the Addis Ababa Fistula Hospital in Ethiopia, which she has been visiting for 10 years, as well as Seattle’s Dr. Julie LaCombe MD FACOG who has performed fistula surgeries in Uganda and Bangladesh and met with me personally to share about obstetrical trauma and fistula surgery and management.
Nancy, Terri and I will look forward to sharing photos and more about our journey and experiences, upon our return. In the meantime, check out the Campaign to End Fistula and join the campaign.
Andrea Wood, PT, DPT, WCS, PRPC is a pelvic health specialist at the University of Miami downtown location. She is a board certified women’s health clinical specialist (WCS) and a certified pelvic rehabilitation practitioner (PRPC). She is passionate about orthopedics and pelvic health. In her spare time, you can find her enjoying the south Florida outdoors.
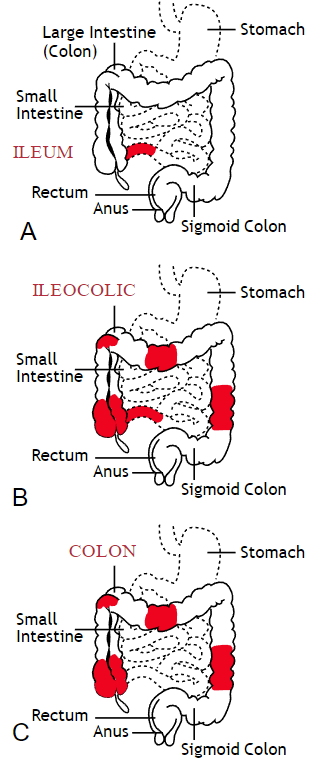
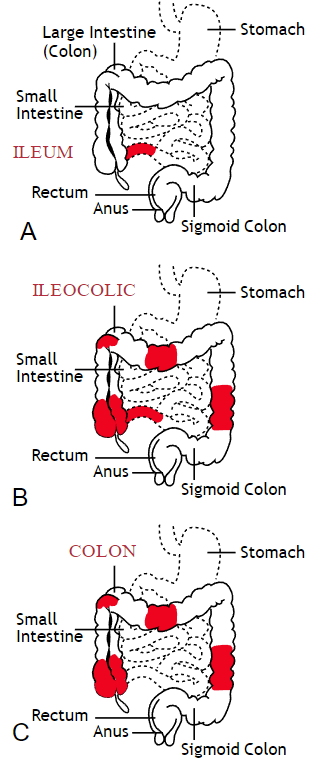
Inflammatory bowel disease (IBD) includes the two diagnosis of Crohn’s Disease and Ulcerative Colitis. While both can cause similar health effects, the differences of the disease pathologies are listed below:1
| Ulcerative Colitis | Crohn’s Disease | |
| Affected Area |
|
|
| Pattern of Damage |
|
|
Common complications experienced by patients with IBD include fecal incontinence, fecal urgency, night time soiling, urinary incontinence, abdominal pain, hip and core weakness, pelvic pain, fatigue, osteoporosis, and sarcopenia. In a sample of 1,092 patients with Crohn’s Disease, Ulcerative Colitis, or unclassified IBD, 57% reported fecal incontinence. Fecal incontinence was reported not only during periods of flare ups, but also during remission periods.2 One common factor affecting fecal incontinence is external anal sphincter fatigue. External anal sphincter fatigue has also been shown to be present in IBD patients who are not experiencing fecal incontinence or fecal urgency. IBD patients have been shown in studies to have similar baseline pressures versus healthy matched controls, thus indicating the possibility that deficits in endurance versus strength can play a larger role in fecal incontinence.3 Other factors contributing to fecal incontinence include post inflammatory changes that may alter anorectal sensitivity, anorectal compliance, neuromuscular coordination, and cause visceral hypersensitivity. Visceral hypersensitivity may be caused by continuous release of inflammatory mediators found in patients with IBD. It is also important to screen properly for incomplete bowel emptying and stool consistency to rule out overflow diarrhea or fecal impaction. Reports of need to splint digitally for full evacuation may indicate incomplete bowel emptying and defaectory disorders such as paradoxical contraction of the puborectalis muscle or rectocele. Anorectal manometry testing may be highly useful in identifying patients likely to improve from biofeedback therapy.4
Urinary incontinence can also be another secondary consequence to IBD. In a sample of 4,827 patients with IBD, 1/3 of responders reported urinary incontinence that was strongly associated with the presence of fecal incontinence. Frequent toilet visits for defecation may stimulate overactive bladder. Women were more likely to experience fecal incontinence versus men. One possible mechanism for increased fecal incontinence in women is men often have a longer and more complete anal sphincter that may be protective of fecal incontinence.5
Physical activity has been shown to be lower in patients with IBD versus healthy controls. 6, 7 Guiding IBD patients in proper exercises programs can have great benefits. Exercise may reduce inflammation in the gut and maintain the integrity of the intestines, reducing inflammatory bowel disease risk.8 It can also help increase bone mass density, an important factor in IBD patients who are at greater risk for osteoporosis. It has also been shown to help general fatigue in IBD patients. Patients with Crohn’s disease who participate in higher exercise levels may be less likely to develop active disease at 6 months. Treadmill training at 60% VO2 max and running three times a week has not been shown to evoke gastrointestinal symptoms in IBD patients. An increase of BMI predicts poorer outcomes and shorter time to first surgery in patients with Crohn’s disease.6
Conservative physical therapy interventions for treating IBD symptoms can include the following:
| Symptoms resulting from IBD | Physical Therapy Interventions |
| Fecal Incontinence (FI) |
|
| Urinary urgency |
|
| Sarcopenia |
|
| Fatigue |
|
| Pelvic Pain |
|
Surgical interventions for IBD are dependent upon what type of disease the patient has and what areas of the intestines are affected the most. Surgery may be considered once the disease has become non responsive to medication therapy and quality of life continues to decline. A colectomy involves removing the colon while a proctocolectomy involves both removal of the colon and rectum. For ulcerative colitis patients, options include total proctocolectomy with end ileostomy or a restorative proctocolectomy with ileal pouch anal anastomosis. Restorative proctocolectomy eliminates the need for an ostomy bag making it the preferred surgery of choice if possible and gold standard for ulcerative colitis patients.10 For patients with Crohn’s disease, options include resection of part of the intestines followed by an anastomosis of the remaining healthy ends of the intestines, widening of the narrowed intestine in a procedure called a strictureplasty, colectomy or proctocolectomy, fistula repair, and removal of abscesses if needed.11
1. Crohn’s and Colitis Foundation. 2019. What is Crohn’s Disease. Retrieved from: http://www.crohnscolitisfoundation.org/what-are-crohns-and-colitis/what-is-crohns-disease/
2. Vollebregt PF, van Bodegraven A, Markus-de Kwaadsteniet T, et al. Impacts on perianal disease and faecal incontinence on quality of life and employment in 1092 patients with inflammatory bowel disease. Ailment Pharmacol Ther. 2018; 47: 1253-1260
3. Athanasios A, Kostantinos H, Tatsioni A et al. Increased fatigability of external anal sphincter in inflammatory bowel disease: significance in fecal urgency and incontinence. J Crohns Colitis (2010) 4: 553-560.
4. Nigam G, Limdi J, Vasant D. Current perspectives on the diagnosis and management of functional anorectal disorders in patients with inflammatory bowel disease. Therap Adv Gastroenterol. 2018 Dec 6: doi: 10.1177/1756284818816956
5. Norton C, Dibley L, Basset P. Faecal incontinence in inflammatory bowel disease: Associations and effect on quality of life. J Crohn’s Colitis. (2013) 7, e302-e311.
6. Biliski J, Mazur-Bialy A, Brzozowski B et al. Can exercise affect the course of inflammatory bowel disease? Experimental and clinical evidence. Pharmacological Reports. 2016 (68): 827-836.
7. Tew G, Jones K, Mikocka-Walus A. Physical activity habits, limitations, and preditors in people with inflammatory bowel disease: a large cross-sectional online survey. Inflamm Bowel Dis. 2016; 22(12): 2933-2942.
8. Vincenzo M, Villano I, Messina A. Exercise modifies the gut microbiota with positive health effects. Oxidative Medicine and Cellular Longevitiy. 2017: Article ID 3831972.
9. Cramer H, Schafer M, Schols M. Randomised clinical trial: yoga vs written self care advice for ulcerative colitis. Aliment Pharmacol Ther. 2017; 45: 1379-1389.
10. Cornish J, Wooding K, Tan E, et al. Study of sexual, urinary, and fecal function in females following restorative proctocolectomy. Inflamm Bowel Dis. 18 (9) 2012. 1601-160
11. Crohn’s and Colitis Foundation. 2019. Surgery Options. Retrieved from: http://www.crohnscolitisfoundation.org/what-are-crohns-and-colitis/what-is-crohns-disease/surgery-options.html
Today's guest post comes from Kelsea Cannon, PT, DPT, a pelvic health practitioner in Seattle, WA. Kelsea graduated from Des Moines University in 2010 and practices at Elizabeth Rogers Pilates and Physical Therapy.
Many studies done on pelvic floor muscle training largely have subjects who are Caucasian, moderately well educated, and receive one-on-one individualized care with consistent interventions. This led a group of researchers to investigate the occurrence of pelvic floor dysfunction, specifically pelvic organ prolapse (POP), in parous Nepali women. These women are known to have high incidences of POP and associated symptomology. Another impetus to perform this research: the discovery that there was a major lack of proper pelvic floor education for postpartum women. These women were commonly encouraged to engage their pelvic floor muscles via performing supine double leg lifts, sucking in their tummies/holding their breath/counting to ten, and squeezing their glutes. These exercises would be on a list of no-no’s here in the United States. In 2017, Delena Caagbay and her team of researchers discovered that in Nepal, no one really knew the correct way to teach proper pelvic floor muscle contractions, preventing the opportunity for women to better understand their pelvic floors. The team then set out to investigate the needs of this population, with the eventual goal of providing effective pelvic floor education for Nepali women.
 Caagbay and her team first wanted to know what baseline muscle activity the Nepali women had in their pelvic girdle. Physical examinations and internal pelvic floor muscle strength assessments revealed that surprisingly there was a low prevalence of pelvic floor muscle defects, such as levator avulsions and anal sphincter trauma. Uterine prolapses were most common while rectoceles were comparatively less common. Their muscles were also strong and well-functioning, often averaging a 3/5 on the Modified Oxford Scale. It was hypothesized that these women had low prevalence of muscle injury because instruments were not commonly used during childbirth, they had lower birth weight babies, and the women were typically younger when giving birth (closer to 20-21 years old). But they had a high prevalence of POP even with good muscle tone? Researchers suggested that their incidence of POP is likely stemming from their sociocultural lifestyle requirements, as women are left to do most of the daily household chores and caregiving tasks while men often travelled away from the home to perform paid labor. Physical responsibilities for these women commonly begin at younger ages and while it helps promote good muscle tone, the heavier loading places pressure on the connective tissue and fascia that support the pelvic organs. Because of the demands of their lifestyles, Nepali women are often forced to return to their physically active state within a couple weeks after giving birth.
Caagbay and her team first wanted to know what baseline muscle activity the Nepali women had in their pelvic girdle. Physical examinations and internal pelvic floor muscle strength assessments revealed that surprisingly there was a low prevalence of pelvic floor muscle defects, such as levator avulsions and anal sphincter trauma. Uterine prolapses were most common while rectoceles were comparatively less common. Their muscles were also strong and well-functioning, often averaging a 3/5 on the Modified Oxford Scale. It was hypothesized that these women had low prevalence of muscle injury because instruments were not commonly used during childbirth, they had lower birth weight babies, and the women were typically younger when giving birth (closer to 20-21 years old). But they had a high prevalence of POP even with good muscle tone? Researchers suggested that their incidence of POP is likely stemming from their sociocultural lifestyle requirements, as women are left to do most of the daily household chores and caregiving tasks while men often travelled away from the home to perform paid labor. Physical responsibilities for these women commonly begin at younger ages and while it helps promote good muscle tone, the heavier loading places pressure on the connective tissue and fascia that support the pelvic organs. Because of the demands of their lifestyles, Nepali women are often forced to return to their physically active state within a couple weeks after giving birth.
After assessing the current needs, cultural norms, and prevalence of POP in Nepali women, Caagbay et al created an illustrative pamphlet on how to contract pelvic floor muscles as well as provided verbal instruction on pelvic floor muscle activation. Transabdominal real time ultrasound was applied to assess the muscle contraction of 15 women after they received this education. Unfortunately, even after being taught how to engage their pelvic floor muscles, only 4 of 15 correctly contracted their pelvic floors.
This study highlighted that brief verbal instruction plus an illustrative pamphlet was not sufficient in teaching Nepali women how to correctly contract their pelvic floor muscles. Although there was a small sample size, these results can likely be extrapolated to the larger population. Further research is needed to determine how to effectively teach correct pelvic floor muscle awareness to women with low literacy and/or who reside in resource limited areas. Lastly, it is important to consider the significance of fascial and connective tissue integrity within the pelvic floor when addressing pelvic organ prolapse.
1 Can a leaflet with brief verbal instruction teach Napali women how to correctly contract their pelvic floor muscles? DM Caagbay, K Black, G Dangal, C Rayes-Greenow. Journal of Nepal Health Research Council 15 (2), 105-109.
https://www.nepjol.info/index.php/JNHRC/article/viewFile/18160/14771
2 Pelvic Health Podcast. Lori Forner. Pelvic organ prolapse in Nepali women with Delena Caagbay. May 31, 2018.
3 The prevalence of pelvic organ prolapse in a Nepali gynecology clinic. (2017) F. Turel, D. Caagbay, H.P. Dietz. Department of Obstetrics and Gynecology, Sydney Medical School Napean, University of Sydney.
4 The prevalence of major birth trauma in Nepali women. (2017) F. Turel, D. Caagbay, H.P. Dietz. Department of Obstetrics and Gynecology, Sydney Medical School Nepean, University of Sydney.
The following is a guest submission from Alysson Striner, PT, DPT, PRPC. Dr. Striner became a Certified Pelvic Rehabilitation Practitioner (PRPC) in May of 2018. She specializes in pelvic rehabilitation, general outpatient orthopedics, and aquatics and treats at Carondelet St Joesph’s Hospital in the Speciality Rehab Clinic located in Tucson, Arizona.
Recently, I had a patient present with Complex Regional Pain Syndrome (CRPS) on his right foot. He stated that the pain had started about 10 days after his prostatectomy when someone had fallen onto his right foot. He reported a bunionectomy on that foot 7 years prior and noted an episode of plantar facilities before his prostatectomy. CRPS is defined as “chronic neurologic condition involving the limbs characterized by severe pain along with sensory, autonomic, motor, and trophic impairments” in a 2017 article "Complex regional pain syndrome; a recent update" by Goh, En Lin. The article goes on to discuss how CRPS can set off a cascade of problems including altered cutaneous innervation, central and peripheral sensitization, altered sympathetic nervous system function, circulating catecholamines, changes in autoimmunity, and neuroplasticity.
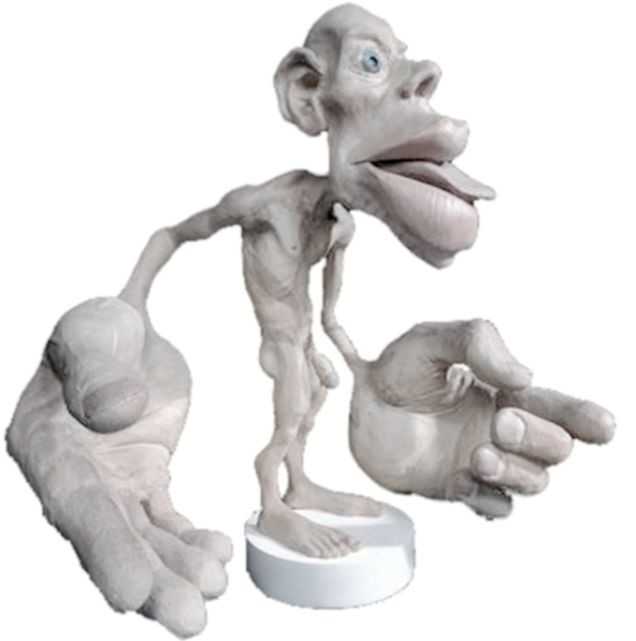
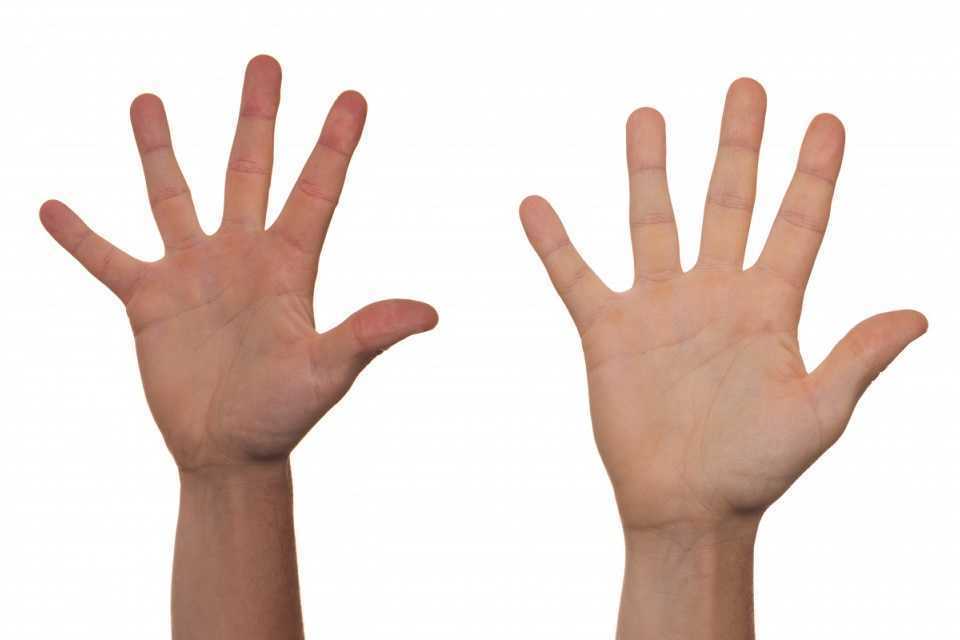
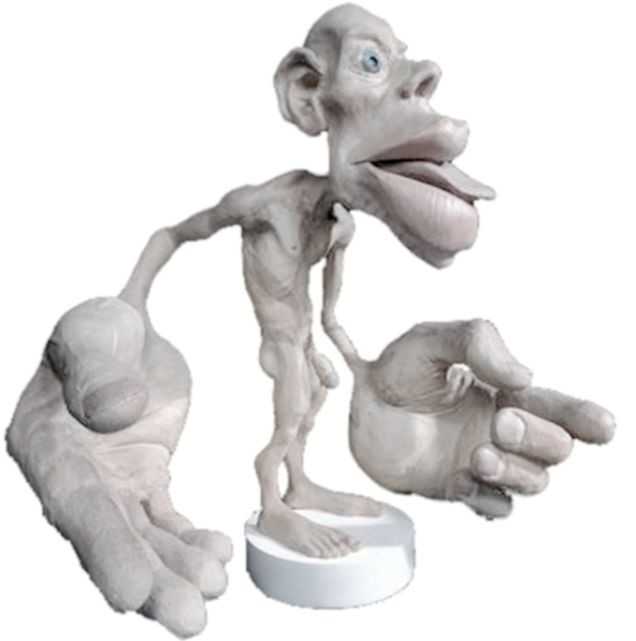 A recent persistent pain theory to explain the relationship between pelvic floor and his foot could be overflow or ‘smudging’ in his homunculus. The homunculus is the map of our physical body in our brain where the feet are located next to the genitals. Possibly when one has pain, there can be ‘smudging’ of our mental body map from one area into another. I have heard this explained as though a chalk or charcoal drawing has been swipes their hand through the picture. A recent study by Schrabrun, SM et al “Smudging of the Motor Cortex is Related to the Severity of Low Back Pain” found that people with chronic low back pain had a loss of cortical organization which and that this loss was associated with the severity and location of LBP.
A recent persistent pain theory to explain the relationship between pelvic floor and his foot could be overflow or ‘smudging’ in his homunculus. The homunculus is the map of our physical body in our brain where the feet are located next to the genitals. Possibly when one has pain, there can be ‘smudging’ of our mental body map from one area into another. I have heard this explained as though a chalk or charcoal drawing has been swipes their hand through the picture. A recent study by Schrabrun, SM et al “Smudging of the Motor Cortex is Related to the Severity of Low Back Pain” found that people with chronic low back pain had a loss of cortical organization which and that this loss was associated with the severity and location of LBP.
There are many ways to improve the organization of the homunculus and create neuroplasticity. One such way was suggested is with Transcutaneous electrical nerve stimulation (TENS) to the bottom of the foot to affect bladder spasms and pain. In recent study, “Transcutaneous electrical stimulation of somatic afferent nerves of the foot relieved symptoms related to postoperative bladder spasms,". Zhang, C et al. 2017 found that participates that had either a bladder surgery or a prostate surgery had improvement in bladder spasm symptoms and VAS scores on day two and three. Their protocol was to use two electrodes over the bottom of the foot at 5 Hz with 0.2 millisecond pulse width until a muscle twitch was achieved and was increased, but still comfortable for an hour (there is a picture of electrode placement in the article). The authors note that this neuromodulation of the foot sensory nerves may inhibit interactions between the somatic peripheral neuropathway and autonomic micturition reflex to calm the bladder and pain.
No matter what we do to help calm nervous systems from the top down; pain neuroscience education, mindful based relaxation, graded motor imagery, or from the bottom up; de-sensitization, biofeedback, or good old-fashioned TENS. The result is the same; a cortical organization and happier patients.
En Lin Goh†, Swathikan Chidambaram† and Daqing Ma. "Complex regional pain syndrome: a recent update". Burns & Trauma 2017 5:2.https://doi.org/10.1186/s41038-016-0066-4"
Schabrun SM, Elgueta-Cancino EL, Hodges PW. "Smudging of the Motor Cortex Is Related to the Severity of Low Back Pain." Spine (Phila Pa 1976). 2017 Aug 1;42(15):1172-1178. doi: 10.1097/BRS.0000000000000938
Chanjuan Zhang, et al. "Transcutaneous electrical stimulation of somatic afferent nerves in the foot relieved symptoms related to postoperative bladder spasms". BMC Urol. 2017; 17: 58. doi: 10.1186/s12894-017-0248-9
Kelly Feddema, PT, PRPC returns in a guest post on Pregnancy Associated Ligamentous Laxity. Kelly practices pelvic floor physical therapy in the Mayo Clinic Health System in Mankato, MN, and she became a Certified Pelvic Rehabilitation Practitioner in February of 2014. See her post on diastasis recti abdominis on the pelvic rehab report, and learn more about evaluating and treating pregnant patients by attending Care of the Pregnant Patient!
 Pregnancy associated ligamentous laxity is something that we, as therapists, are fairly well aware of and see the ramifications of quite often in the clinic. We know the female body is changing to allow the mother to prepare for the growth and birth of the tiny (or sometimes not so tiny) human she is carrying. We also know that the body continues to evolve after the birth to eventually return to a post-partum state of hormonal balance. Do we think much about what this ligamentous laxity can mean during the actual delivery? Does laxity predispose women to other obstetric injury?
Pregnancy associated ligamentous laxity is something that we, as therapists, are fairly well aware of and see the ramifications of quite often in the clinic. We know the female body is changing to allow the mother to prepare for the growth and birth of the tiny (or sometimes not so tiny) human she is carrying. We also know that the body continues to evolve after the birth to eventually return to a post-partum state of hormonal balance. Do we think much about what this ligamentous laxity can mean during the actual delivery? Does laxity predispose women to other obstetric injury?
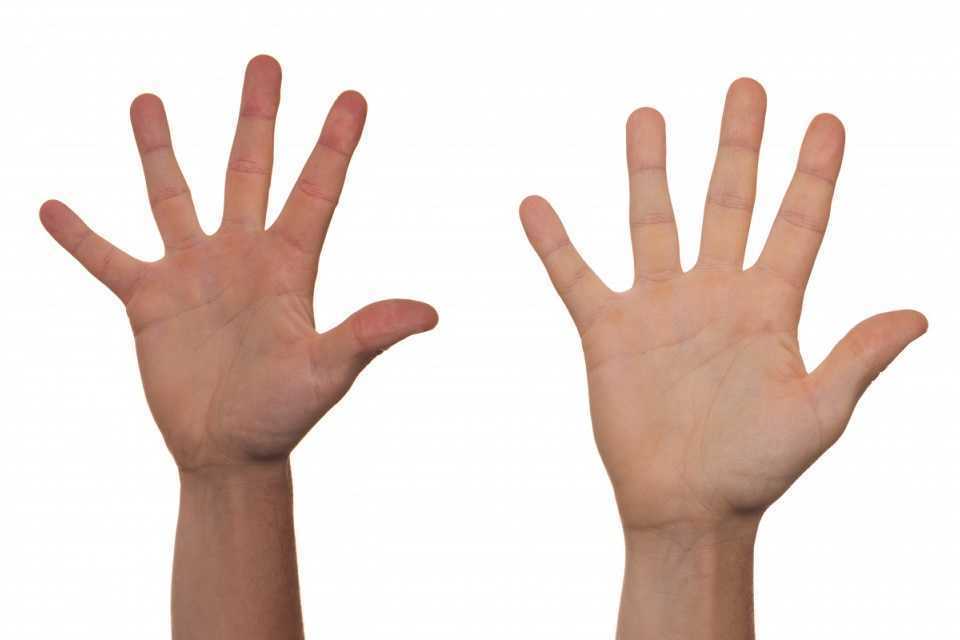
A recent study in the International Urogynecology Journal assessed ligamentous laxity from the 36th week of pregnancy to the onset of labor by measuring the passive extension of the non-dominant index finger with a torque applied to the second metacarpal phalangeal joint. They collected the occurrence and classification of perineal tears in 272 out of 300 women who ended up with vaginal deliveries and looked for a predictive level of second metacarpophalangeal joint (MCP) laxity for obstetric anal sphincter injury (OASI). They concluded that the increased ligamentous laxity did seem associated with OASI occurrence which was opposite of their initial idea that more lax ligaments would be at less of a risk of OASI.
In another study from the same journal published in 2017, researchers studied if levator hiatus distension was associated with peripheral ligamentous laxity during pregnancy. This was a small study but they concluded that levator hiatus distension and ligamentous laxity were significantly associated during pregnancy. They did admit the relationship was weak and results would have to be confirmed with a larger study and more specific study methods. However, the likelihood of major levator trauma more than triples during the reproductive years from under 15% at age 20 to over 50% at age 40(University of Sydney) so it seems that these issues warrant continued study with the continued trend toward delayed child bearing in Western cultures.
Gachon, B., Desgranges, M., Fradet, L. et al. Int Urogynecol J (2018). https://doi.org/10.1007/s00192-018-3598-2
Gachon, B., Fritel, X., Fradet, L. et al. Int Urogynecol J (2017) 28: 1223. https://doi.org/10.1007/s00192-016-3252-9
University of Sydney. "Levator Trauma" sydney.edu.au. Accessed 25 April 2018.
The Institute has welcomed occupational therapists since our founding in 2006. In addition, three OTs: Richard Sabel, MA, MPH, OTR, GCFP, Erica Vitek, MOT, OTR, BCB-PMD, PRPC, and Tiffany Ellsworth Lee MA, OTR, BCB-PMD all teach courses as members of our faculty. (Erica Vitek is also one of several OTs who holds certification as a Pelvic Rehabilitation Practitioner through H&W).
Recently, the Institute was contacted by an Occupational Therapist who has attended many of our courses, regarding a challenge she was experiencing obtaining CEUs in her state (Oregon) for courses on Pelvic Rehab and Biofeedback. In light of this, the Institute has been discussing with some of the occupational therapists on our faculty, as well as representatives of the BCIA and Marquette University, and how to spread awareness about and recognition of OT’s roles in pelvic rehab. Below, we’ve asked faculty member Erica to share a bit more about her journey and the role of the pelvic rehab occupational therapist.
 As an OT student, I had a professor who brought in practicing clinicians to discuss their unique roles out in the field. Pelvic health happened to be one of the topics of the day. I was completely intrigued by the clinician, who had such passion about the role of OT in pelvic health. It became clear that helping people with impaired basic bodily functions was imperative to fulfilling life roles and participation; it was OT. I knew from that moment that I wanted to help people deal with these challenging, private issues.
As an OT student, I had a professor who brought in practicing clinicians to discuss their unique roles out in the field. Pelvic health happened to be one of the topics of the day. I was completely intrigued by the clinician, who had such passion about the role of OT in pelvic health. It became clear that helping people with impaired basic bodily functions was imperative to fulfilling life roles and participation; it was OT. I knew from that moment that I wanted to help people deal with these challenging, private issues.
In my journey, I did not immediately start out in pelvic health, but instead in an acute care hospital that had a women’s health program with a strong interest in pelvic health. A very experienced OT and her team of 2 additional OTs were doing great work in that department already. The window of opportunity opened for me to mentor with that group and I eventually was able to begin to get my own referrals and develop a robust hospital-based outpatient practice. At that time, ALL of my experience had been with OTs doing this work and I was naïve to the fact that outside of my world, most of the clinicians doing this type of work were physical therapists (PT). I asked to join a highly trained and skilled group within my health system of all women’s health PTs. Overtime, I was able to demonstrate my level of competency within the group of PTs and contribute valuable things to our organization. Herman and Wallace Rehabilitation Institute was instrumental in my quest to demonstrate competency as they allowed OTs a clear pathway for enrollment in their coursework and application for the Pelvic Rehabilitation Practitioner Certification examination. I can be proud to have those credentials to my name.
My challenges in the area of pelvic health practice have thankfully been minimal, nearly nonexistent, and it has come to my awareness in recent weeks that this is not the case for OTs around the country trying to develop themselves as pelvic health practitioners. My original OT mentors reassured me with the AOTA’s published document titled Occupational Therapy Practice Framework: Domain & Process, detailed a clear place in the role of pelvic health. This document has gone through 3 revisions over the course of its first publication in 2002. The 2nd edition was published in 2008 and the 3rd edition in 2014. I’d like to cite a few important areas of the document that I find to be helpful in an OT’s quest to demonstrate our role in pelvic health rehabilitation.
I’d first like to quote the definition occupational therapy according to the 3rd edition, “occupational therapy is defined as the therapeutic use of everyday life activities (occupations) with individuals or groups for the purpose of enhancing or enabling participation in roles, habits, and routines in home, school, workplace, community, and other settings. Occupational therapy practitioners use their knowledge of the transactional relationship among the person, his or her engagement in valuable occupations, and the context to design occupation-based intervention plans that facilitate change or growth in client factors (body functions, body structures, values, beliefs, and spirituality) and skills (motor, process, and social interaction) needed for successful participation. Occupational therapy practitioners are concerned with the end result of participation and thus enable engagement through adaptations and modifications to the environment or objects within the environment when needed. Occupational therapy services are provided for habilitation, rehabilitation, and promotion of health and wellness for clients with disability- and non-disability-related needs. These services include acquisition and preservation of occupational identity for those who have or are at risk for developing an illness, injury, disease, disorder, condition, impairment, disability, activity limitation, or participation restriction. “
As we look closer at the framework and the definition of OT, there is clear evidence that the occupational therapist (OT) has a role in the treatment of pelvic health conditions. Importantly, occupations are defined by this document as “…various kinds of life activities in which individuals, groups, or populations engage, including activities of daily living (ADL), instrumental activities of daily living (IADLs), rest and sleep, education, work, play, leisure, and social participation.” The clearest examples of the OT’s role in pelvic health occupations within this section include: 1) ADL section: toileting and hygiene (continence needs, intentional control of bowel movements and urination) and sexual activity. 2) IADLs section: sleep participation (sustaining sleep without disruption, performing nighttime care of toileting needs). 3) Achieving full participation in work, play, leisure, and social activities, requires one to be able to maintain continence in a socially acceptable manner in which they can feel confident and comfortable to fulfill their roles and duties.
Client factors as defined in this document are “Specific capacities, characteristics, or beliefs that reside within the person and that influence performance in occupations. Client factors include values, beliefs, and spirituality; body functions; and body structures.” Client factors are further identified as affecting the performance skills and participation of the clients we work with. OT’s role per definition is to “facilitate change and growth in client factors”. In order to fully enhance our client’s performance skills/participation related to change and growth in client factors, OT’s have to examine the whole person, including pelvic health impairments, which have a negative influence on performance. Within client factors, the document defines body structures as, “Anatomical parts of the body, such as organs, limbs, and their components that support body function.” Within this category, one can refer to multiple items named that relate to the care that OTs provide in pelvic health rehabilitation, including but not limited to, structures related to the digestive, metabolic, and endocrine systems and structures related to the genitourinary and reproductive systems.
Since the first email from this individual in Oregon, we have been reached by several other OTs asking about similar challenges and questions about scope of practice. Because of our commitment to honoring the AOTA’s Practice Framework, and because we believe that the great patient need that exists can be better served by having trained OTs able to treat pelvic health conditions, the Institute is working with members of our faculty and professional network to advocate for recognition of OTs in pelvic rehab and resolve confusion about scope of practice. For those interested in further resources, please check out:
- Pelvic Floor Biofeedback
- The Women’s Health 4 OT Facebook Group
- The OTs for Pelvic Health Facebook Group
- Occupation Therapy in Postpartum Care Facebook Group
- Womens Health Occupational Therapy Australia Facebook Group
American Occupational Therapy Association. (2002). Occupational therapy practice framework: Domain and process. American Journal of Occupational Therapy, 56, 609-639.
American Occupational Therapy Association. (2008). Occupational therapy practice framework: Domain and process (2nd ed.). American Journal of Occupational Therapy, 62, 625-683.
American Occupational Therapy Association. (2014). Occupational therapy practice framework: Domain and process. American Journal of Occupational Therapy, 68, S1-S48.
Today's guest post comes to us from Kelly Feddema, PT, PRPC. Kelly practices pelvic floor physical therapy in the Mayo Clinic Health System in Mankato, MN, and she became a Certified Pelvic Rehabilitation Practitioner in February of 2014. To learn more about diastasis recti abdominis, consider attending Care of the Postpartum Patient!
It can be a struggle to treat patients with diastasis recti if they don't seek treatment early after giving birth. Many therapists may often find themselves thinking “if I only could have started them sooner.” Why does this condition often get missed at postpartum examinations? I personally deal with symptoms from an undiagnosed diastasis, and I'm a therapist! I didn’t really pay attention to it until I started down the road of becoming a pelvic floor therapist.
 Diastasis recti can be a difficult diagnosis to treat, as the patient may come to us when they are already one year postpartum, and not everyone agrees on the what are the best treatments. To crunch or not crunch? To use a brace or not to brace? It would be great if we had a similar healthcare system to France, where the norm is to have 10-20 postpartum rehabilitation visits with women after child birth. While therapy is available in the United States, women must ask for it.
Diastasis recti can be a difficult diagnosis to treat, as the patient may come to us when they are already one year postpartum, and not everyone agrees on the what are the best treatments. To crunch or not crunch? To use a brace or not to brace? It would be great if we had a similar healthcare system to France, where the norm is to have 10-20 postpartum rehabilitation visits with women after child birth. While therapy is available in the United States, women must ask for it.
There are many programs out there from the more well-known Tupler Technique and Mutu programs to others that come up when searching for exercise ideas. The American Physical Therapy Association (APTA) has a basic program to work on isolating the transverse abdominis (TrA) muscle and then progressing movements in the legs while keeping the TrA activated.
Some research by Paul Hodges and Diane Lee from 2016 in the Journal of Orthopedic Sports Physical Therapy indicates that narrowing the inter-rectus distance with a TrA contraction might improve force transfer between the sides of the abdominals and in turn, improve abdominal mechanics.
Another study in Physiotherapy from December of 2014 by AG Pascoal, et.al. utilized ultrasound to determine the effect of isometric contraction of the abdominal muscles on inter-rectus distance in postpartum women. They found that the while the inter-rectus distance in postpartum women was understandably higher than controls, it significantly lowered during an isometric contraction of the abdominal muscles.
One year later, a study in the same journal by MF Sancho, et.al. had similar findings when studying women who had a vaginal delivery and women who had Cesarean deliveries. They found that abdominal crunch exercises were successful in reducing inter-rectus distance, but drawing-in exercises were not.
As with a lot of research, the findings lead to more questions and ideas to explore. I think it is safe to say that starting safe re-education of the muscles as early as possible is going to provide women the most benefit in reducing diastasis recti, and that will help to prevent further issues in the abdominal and pelvic region.
Sagira Vora, PT, MPT, WCS, PRPC practices in Bellevue, WA at the Overlake Hospital Medical Center, and she played a pivotal role in creating the Pelvic Rehabilitation Practitioner Certification examination. Today's post is part one of a multi-part series on pelvic rehabilitation and sexual health. Stay tuned for part two!
“Have mind-blowing sex: learn how to do your Kegels.” “Amazing orgasms, ladies do your Kegels!” These were just some of the headlines that greeted me as I researched what was being said in the popular media regarding pelvic floor exercises and improving sexual function in women. Some other wisdom from popular women’s magazines included advice on, “stopping the flow of urine,” to do your Kegels. We know how much we pelvic floor therapists love hearing that phrase!

I found a few recent and past studies that have tried to study pelvic floor exercises and sexual function in women.
In 1984, Chambless et.al. studied a small group of women who were able to achieve orgasm through intercourse less than 30% of time. Strength gains in the pubococcygeus muscles were noted in the exercise group but neither the exercise nor control group achieved increased orgasmic frequency.
In a more recent study, Lara et. al. studied 32 sexually active post-menopausal women, who had the ability to contract their pelvic floor muscles, tested the hypothesis that 3 months of physical exercises including pelvic floor muscle training with biweekly physical therapy visits and exercise performed at home three times a week, would enhance sexual function. Pelvic floor muscle strength was significantly improved post-test, but this study found no effect on sexual function.
Forty years after Dr. Kegel’s assertion about sexual arousal enhancing properties of pubococcygeus muscle exercises, Messe and Geer tested Kegel’s hypothesis in their psychophysiological study, in which they asked women to perform vaginal contractions while engaging in sexual fantasy. A second group was asked to engage in sexual fantasy without the contractions, and yet a third group was given the task of vaginal contractions but no sexual fantasy. The results indicated that performing vaginal contractions with sexual fantasy improved arousal and orgasmic ability. Initially, this group made better gains than vaginal contractions alone and fantasizing alone. However, with a second test session one week later, no further gains were noted in the ability of this group to improve sexual arousal or orgasm. Messe and Geer speculated that increased muscle tone may result in increased stimulation of stretch and pressure receptors during intercourse, leading to enhanced arousal and orgasmic potential.
The most interesting finding was reported by an older study done by Roughan, who reported no differences in the groups he studied. Roughan et. al. expected women with orgasm difficulties to improve after 12-week period of pelvic floor strengthening exercises, compared to a group that practiced relaxation and an attention control group. No difference was found between the orgasmic ability of the two groups.
The majority of women studied here had no reported pelvic floor dysfunction. Perhaps, contrary to popular opinion and against the advice of women’s magazines, women with healthy pelvic floors may not benefit from pelvic floor exercises any more than they would from relaxation training, or mindful attention to sexual stimuli.
So, what then, will increase our mojo in bed, you ask? Stay tuned for the next blogs…
Chambless D, Sultan FE, Stern TE, O’Neill C, Garrison S. Jackson A. Effect of pubococcygeal exercise on coital orgasm in women. J Consult Clin Psychol. 1984; 52:114-8
Laan E. Rellini AH. Can we treat anorgasmia in women? The challenge to experiencing pleasure: Sex Relation Ther. 2011:26:329-41
Messe MR, Geer JH. Voluntary vaginal musculature contractions as an enhancer of sexual arousal. Arch Sex Behav. 1985; 14:13-28
Padoa, Anna. Rosenbaum, Talli. 1st edition. 2016. The Overactive Pelvic Floor.
Roughan PA, Kunst L. Do pelvic floor exercises really improve orgasmic potential? J Sex Marital Ther. 1984;7:223-9
Jason Hardage is a physical therapist who practices in Alameda, CA. He recently attended the Mindfulness-Based Pain Treatment course which is written and instructed by faculty member Carolyn McManus, PT, MS, MA. Dr. Hardage was kind enough to send in the following review in order to help spread the good word about this powerful course. Your next opportunity to learn how to apply mindfulness practices in your clinic will be in Boston, MA on March 4-5, 2017.
Carolyn McManus' 2-day course, Mindfulness-Based Pain Treatment, was truly outstanding. In my opinion, the integration of mindfulness into healthcare is a paradigm shift and in that sense Carolyn is a visionary who is ahead of her time, as she has been practicing in this arena for many years. Her expertise is clear (as is her joy in teaching).
 In this course, she introduces the basic terminology, concepts, and mindfulness practices in a way that is experiential, practical, and accessible, with many tools and techniques to integrate into clinical practice. She thoroughly reviews the evidence in a way that is skillful and compelling and provides the theory as to how mindfulness works, then provides case studies from her own clinical practice. She also provides a brief survey of other tools and approaches that are complementary, such as yoga, loving kindness meditation, and motivational interviewing, then shows how to put it all together, including suggestions for documentation and billing. She is generous in sharing resources, including patient education materials and four open-access guided relaxation and meditation sessions from her Web site, as well as resources for continued study. Furthermore, she presents ways for the healthcare practitioner to use mindfulness for self care, to help combat the burnout that can come with serving those with complex needs in a demanding healthcare environment.
In this course, she introduces the basic terminology, concepts, and mindfulness practices in a way that is experiential, practical, and accessible, with many tools and techniques to integrate into clinical practice. She thoroughly reviews the evidence in a way that is skillful and compelling and provides the theory as to how mindfulness works, then provides case studies from her own clinical practice. She also provides a brief survey of other tools and approaches that are complementary, such as yoga, loving kindness meditation, and motivational interviewing, then shows how to put it all together, including suggestions for documentation and billing. She is generous in sharing resources, including patient education materials and four open-access guided relaxation and meditation sessions from her Web site, as well as resources for continued study. Furthermore, she presents ways for the healthcare practitioner to use mindfulness for self care, to help combat the burnout that can come with serving those with complex needs in a demanding healthcare environment.
This is certainly one of the best courses that I've taken in over 17 years as a physical therapist. While it's easy to see how the content of the course is applicable to people with chronic pain, in my opinion, this approach is broadly applicable across patient populations. It's exciting to know that we have a physical therapist who is an expert, long-time practitioner and teacher of mindfulness from whom to learn. I highly recommend this course! At the same time, it left me wanting more and I'd love to see Carolyn develop other ways to deliver content--such as a blog and online video content--that would allow her to connect with a wider audience and also to stay connected to those who have taken her course.**
Sincerely,
Jason Hardage, PT, DPT, DScPT, GCS, NCS
Alameda, CA
Editor's note: Since publication of this review, Carolyn has began to publish a blog on mindfulness! See more at The Mindfulness in Healthcare Blog
The following comes from a male patient who wanted to share his story about finding care for his pelvic floor dysfunction. His story highlights the important role pelvic rehab practitioners can play, and why we need to continue training more therapists in this field.
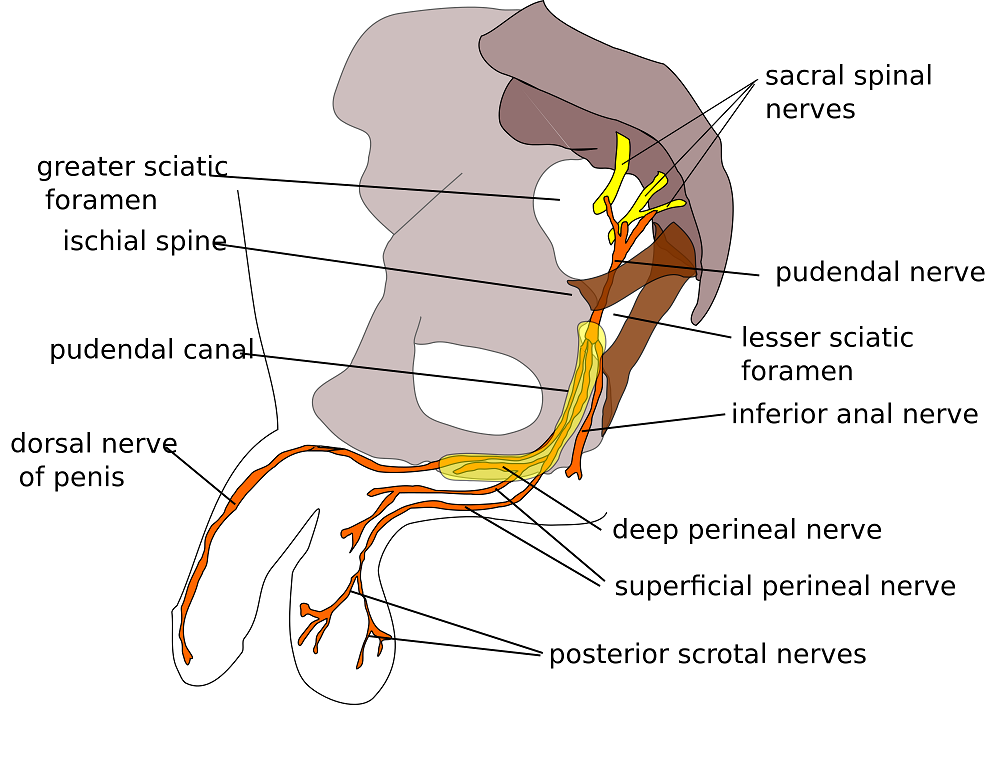
I’m 65 year old male and I developed pudendal neuralgia and pelvic floor issues as a result of an accident about four years ago. Shortly after my accident I started to experience pain in my testicles and perineum. At the time, I did not think that one had anything to do with the other. I made an appointment with my urologist who did an ultrasound and assured me that there was nothing physically wrong. I don’t think my testicles quite believe that but mentally I felt relieved. But the pain persisted and started to spread. Now it was also in my groin and penis. I was also having problems with chronic constipation, urinary retention and erectile dysfunction. Since I did have back surgery years ago I started to suspect my low back was causing the problem. I made an appointment with a well-respected orthopedic surgeon in New York. While he gave me his analysis with regards to my back problems he clearly avoided addressing the pelvic issues. I left there feeling lost. Suffice it to say that over the course of the next couple of years I saw several other specialists who either skirted around the issue or told me that nothing was wrong. A couple of years passed but the pelvic issues just continued to get worse and worse. I started seeing a new primary care physician who indicated that perhaps the source of the pelvic pain was coming from the pudendal nerve and felt that physical therapy might help. She gave me a prescription for physical therapy to evaluate for pudendal nerve.
 Well, I have a diagnosis now so I start researching pudendal neuralgia and land on the Pudendal Hope website. Wow! What an eye opener that was. I’m reading the information on the website and it was like I had an epiphany. I realized that I was not going crazy and that Pudendal Neuralgia and pelvic pain are very real issues.
Well, I have a diagnosis now so I start researching pudendal neuralgia and land on the Pudendal Hope website. Wow! What an eye opener that was. I’m reading the information on the website and it was like I had an epiphany. I realized that I was not going crazy and that Pudendal Neuralgia and pelvic pain are very real issues.
OK, so where do I go from here? With prescription in hand I’ll make an appointment with a physical therapist that deals with pudendal neuralgia. Ha, I thought getting a diagnosis was tough but finding a physical therapist that treats pudendal neuralgia and pelvic issues was no easy task. To make things even more challenging, finding a physical therapist who treats men was even harder. I made a few calls and kept looking online without much success. Desperate to find a physical therapist that treats men, I sent an email off to a therapist in California asking if by some chance she could recommend a physical therapist here in New Jersey. As luck would have it, I got both a response and a referral. With that, I called Michelle Dela Rosa at Connect Physical Therapy. I had to wait about six weeks for an appointment but finally the day arrived. OK, so now, I had set my expectations. I’ll go for a few weeks of physical therapy, the pain will go away and it will be back to a normal life. Well, not so much… the journey and education were just getting started.
There are days when I am in so much pain that I ask myself if the pelvic therapy is really doing me any good. But then I reflect back to how things were before I started the therapy. Funny thing about pain… often times it makes us forget how things were in the past and shift our focus to the here and now. That being said, I quickly realize how much I have truly progressed since starting therapy.
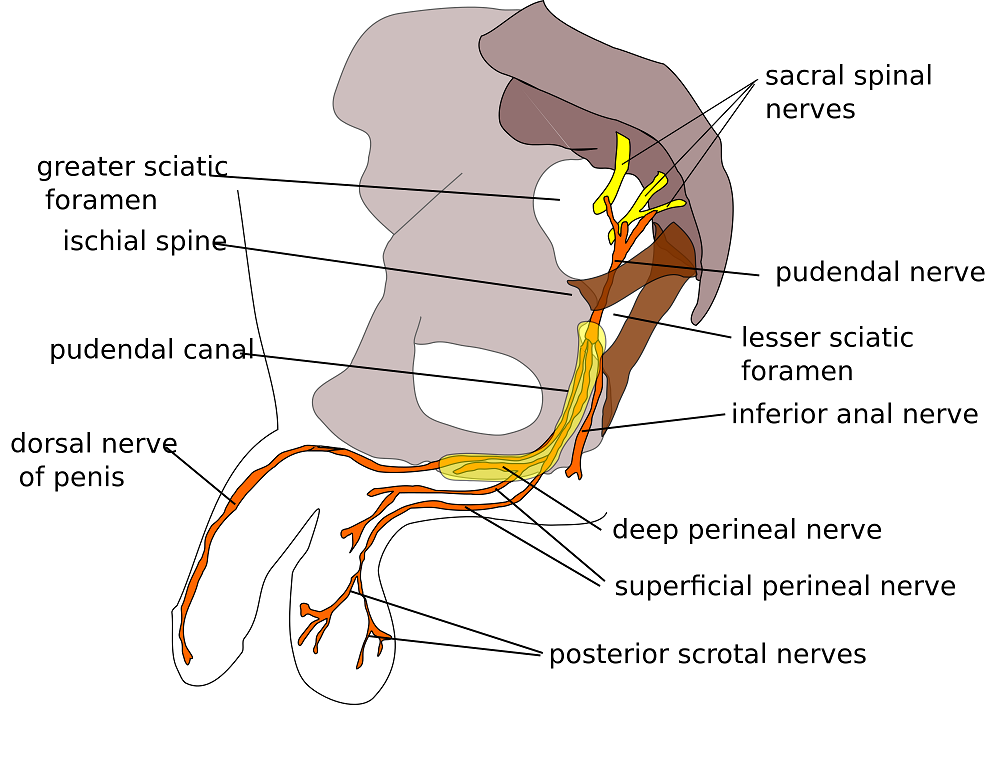
So what have I learned? Well, the first thing is to understand the anatomy and how all the pelvic muscle groups and nerves are integrated. After all you can’t fix what you don’t know is broken. Therapy has certainly helped educate me in that respect; I’ve learned the importance of proper breathing and strengthen the core muscles. I know that when I was in pain I would tighten up the pelvic muscles and hold my breath which would only make things worse, as the muscles would get into a knot, and make it even more difficult to get relief. I’ve learned a whole new set of exercises that I now have in my arsenal to help fight this battle. To help me deal with the chronic constipation I’ve learned how to massage my abdomen to help move things along. For those folks dealing with chronic constipation, well, we all know what happens when we push just a little too hard… flare time! I could go on and on. I learned to use tools, such as the TheraWand, to help break the tension for those internal pelvic muscles. Pelvic therapy has taught me the importance and benefits of the proper use of cold packs, glides, exercise, breathing, relaxing the pelvic floor and on and on and on.
I was a bit embarrassed getting started but the prospect of relieving some of the pelvic pain and the professionalism of my therapist quickly turned my embarrassment into a non-issue.
I want to express my thanks and gratitude to all those physical therapists who have the courage and vision to take on this problem. You are truly making a difference in the lives of the people you are helping.