H&W is proud to be able to present a new remote course on ethics from new faculty member, and Sr. TA, Mora Pluchino, PT, DPT, PRPC. Mora is a graduate of Stockton University with a BS in Biology (2007) and Doctorate of Physical Therapy (2009). She has been working at Bacharach Institute for Rehabilitation ever since graduation and has experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training.
Mora began treating Pelvic Health patients in 2016 and has experience treating women, men, and children with a variety of Pelvic Health dysfunction. In 2020, she opened her own "after hours" virtual practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients and has been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules and has been a TA with Herman & Wallace since 2020 with over 150 hours of lab instruction experience. Mora authored and instructs Ethical Concerns for Pelvic Health Professionals.
● You are a new graduate, and your employer sends you to Pelvic Floor Level 1 and expects you to start up a Pelvic Health Program at the facility. Your first scheduled patient is a diagnosis you didn’t learn about and don’t feel comfortable treating, but your student loan payments have started, and you need this job.
● The word has gotten out and referrals are flowing into your clinic after hearing what a life-changing service your Pelvic Health program provides. You have a 6 month long waiting list and your front desk person asks you how to organize the list. Options include prioritizing based on the severity of issues, first come/ first serve, based on past history with the facility, etc.
Put yourself in these situations and reflect. How would you feel? What would you do? All of the situations above have a common theme. They present Ethical Concerns for Pelvic Health Professionals. Ethical situations are very common in day-to-day practice for any health care professional. Treating in the pelvic region can add additional complications due to the level of intimacy and vulnerability in this care.
Ethics by definition is “the division of philosophy concerned with how a person should behave in a matter that is considered morally correct or good” that gives us standards, virtues, and rules (Boone, 2017). The professional code of ethics for each professional category and is grounded in virtue ethics. Virtue ethics includes four main concepts including balance of harms and benefits, doing no harm, justice, and autonomy (Kirsch, 2005)
Whether a practitioner is a physical therapist/ physical therapist assistant, occupational therapist, psychologist, social worker, nurse, doctor, or physician’s assistant, their governing professional organization will have a code of ethics and conduct to help guide these practitioners in good decision making. There are many ethical decision-making models to help guide an individual through the process of identifying, defining, examining, and then problem solving any ethical occurrence.
The RIPS Model, originally presented by Arlanian, Swisher & Davis in 2005, presents an ethical framework to help guide practitioners through the steps needed to address ethical concerns. The world of ethical decision-making is typically one of many options, typically being more “gray area” than simply “black” and “white.” Ethical Concerns for Pelvic Health Professionals is designed to help make these decisions easier to define, examine, discuss, and address so we can have these tough conversations!
Ethical Concerns for Pelvic Health Professionals is a one-day remote course that covers ethical considerations for professionals working in the area of Pelvic Health. In general, Health Care Professionals have many day-to-day ethical considerations to “do no harm.” This includes basic decisions for billing, patient care, safety, and compliance. The purpose of this class is to explore the ethical challenges Pelvic Health practitioners may experience including consent, managing trauma and abuse, and preventing misconduct. To learn more join us in Ethical Concerns for Pelvic Health Professionals on June 18, 2022!
Research:
Boone, B. (2017). Ethics 101: From altruism and utilitarianism to bioethics and political ethics, an exploration of the concepts of right and wrong. Adams Media.
Kirsch, N. (2005). Ethics in Physical Therapy: A Case-Based Approach. McGraw Hill Publications. American Physical Therapy Association.

Elena Teare, the Communications Lead from Open Arms Perinatal Services sat down with The Pelvic Rehab Report to discuss their organization and annual fundraiser Labor of Love.
For our practitioners who are not familiar with Open Arms, can you tell me the organization?
Open Arms is the leading independent, community-based program in Washington State providing wraparound perinatal services to low-income families. We serve nearly 300 families every year and our award-winning program is not hospital-directed or based. Our trusted, community-centered approach always prioritizes the unique cultural, linguistic, and emotional needs of each client free of charge.
We provide services across four program areas: birth doulas, community-based outreach doulas (who provide in-home support up to two years of age), family support services, and lactation support peer counseling. We also train emerging birth workers to serve families in their own communities.
Our communities of focus are Black/African American, Somali, Latinx, and American Indian/Alaska Native communities of King, Snohomish, and Pierce counties. 87% of our clients are of color.

Can you share a success story?
In 2019, Asha was experiencing homelessness when pregnant with her second child. She heard about Open Arms through her shelter and soon was matched with Suad Farole, a Community-Based Outreach Doula. Originally from Somaliher through pregnancy, birth, and her daughter for two years. When Asha became pregnant with her son in late 2020, she knew she wanted Suad to be with her. In Asha’s words, “When I first decided to get a doula, I didn’t expect what I received. Suad was a true gift that not only oversaw the safety of my child as she came into this world, but she truly cared for my well-being and helped me to become the mother that I am now.”
What is the importance of the yearly Labor of Love event?
Labor of Love is our most important fundraising event of the year! It is a chance for us to engage our community and highlight the extraordinary outcomes our families achieve. When community members invest in the work that we do, they provide Open Arms with the flexibility to allocate dollars to any part of the organization that needs extra support. Given the uncertainty in today’s world, it’s important that we have the ability to respond quickly to the changing circumstances of our client families.

What makes you, the staff, volunteers, and the community passionate about this organization?
Our approach is evidence-informed, culturally appropriate, and community-centered and is effective in reducing medical interventions and the costs of perinatal care. By prioritizing the emotional needs of birthing people, our staff and volunteers set the stage for new mothers and parents to be strong and confident advocates for their children and families. By removing the cultural barriers to perinatal care by providing culturally competent care, we facilitate better community linkage to the health care system.
Our doulas and lactation consultants, as well as community of midwives, are committed to improving the health outcomes for birthing people and children of systematically underserved communities. Our families’ outcomes exceed those of Washington state and the country. As of 2021, 95% of our families give birth at full term and healthy birth weight, 85% avoid unplanned cesareans, and 82% are still breast/chestfeeding at six months.[i]
How do persons in need find your organization and what partnerships do you have?
Many of our families are referred from other organizations and service providers, and others find us through word of mouth in the community. Through our Perinatal and Lactation Support Collaborative, we have strong partnerships with the organizations like the Center for Indigenous Midwifery, Generations Midwifery Services, Global Midwifery Services, The Pacific Islander Health Board of Washington, and Rainier Valley Midwives. Additionally, the Program for Early Parenting Support (PEPS) and the Tubman Center for Health and Freedom are additional partnerships we have.

What is the awareness level in the community of Open Arms?
Open Arms clients are referred from other community partners and agencies who trust us to provide the best possible, culturally sensitive care. Over 30% of our referrals are from previous clients who seek our services again or refer friends and family.
How can people who are interested in supporting Open Arms donate or support the organization?
Interested supporters can make a gift to Open Arms online at https://www.openarmsps.org/get-involved/donate/make-gift-today/. To make an even bigger difference in the lives of the families we serve, community members can join our Baby Whisperers Monthly Giving Circle with a sustaining monthly gift. We also value gifts of time and welcome volunteers to assist with some of the behind-the-scenes logistics of the organization. People can stay up to date with our work and opportunities to get involved by heading to our site and subscribing to our newsletter or following our social media channels.

[i] Compared to King county’s rates: 91% of people give birth at full term; 93% are at a healthy birth weight, and 39% are breast/chestfeeding at six months.
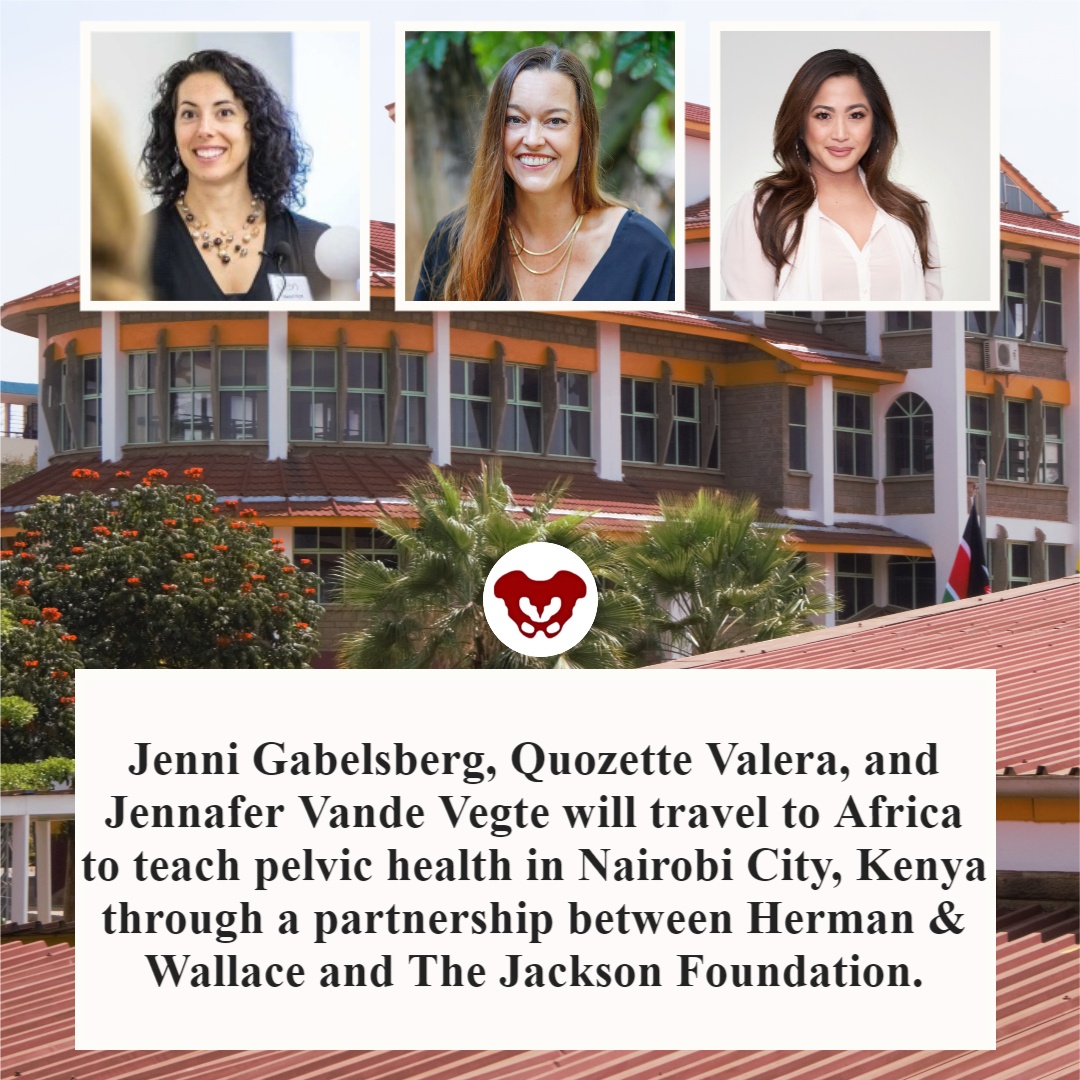
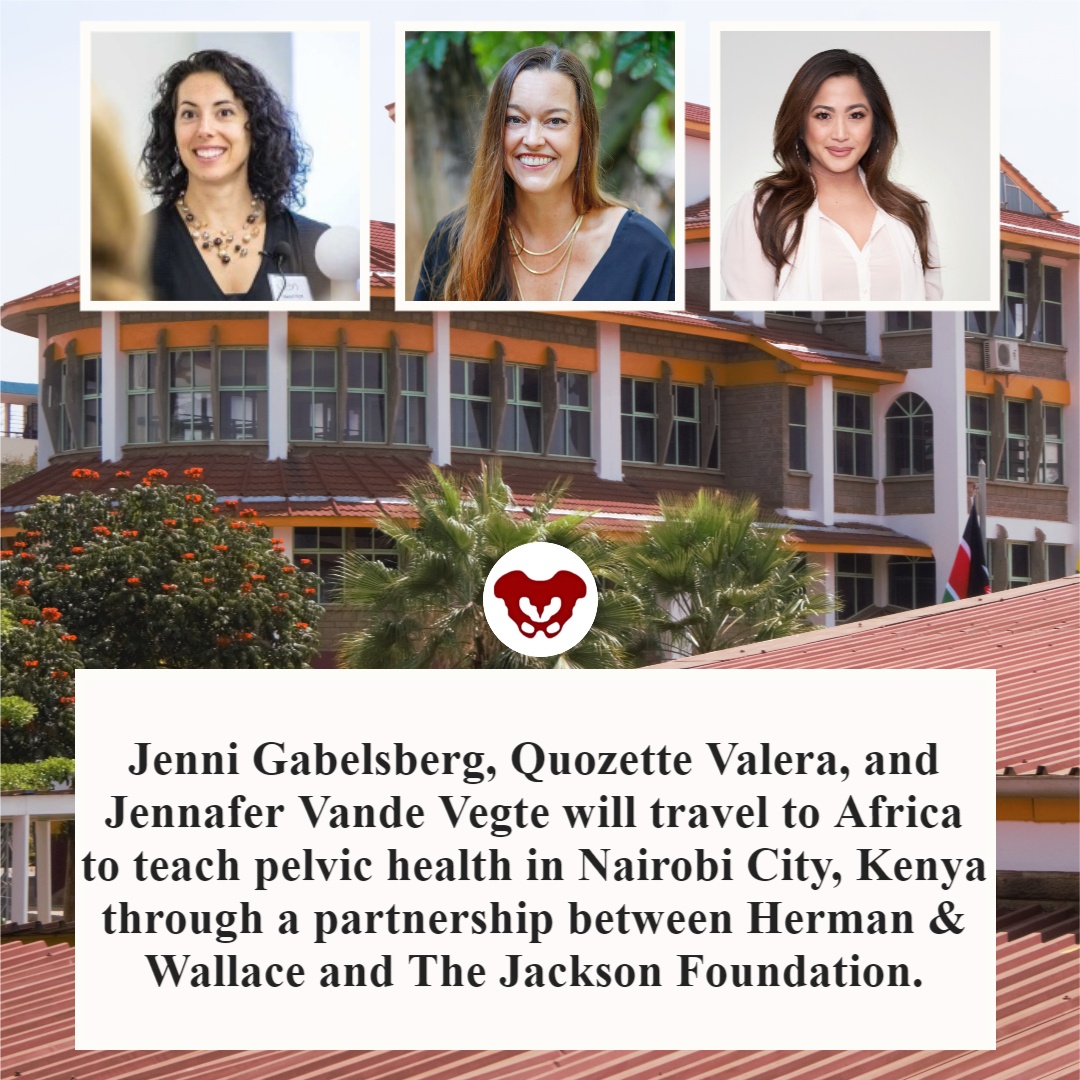
Faculty members Jenni Gabelsberg DPT, WCS, MSc, MTC and Jennafer Vande Vegte, PT, BCB-PMD, PRPC along with senior Teaching Assistant Quozette Valera PT, DPT will travel to Africa to teach pelvic health in Nairobi City, Kenya through a partnership between Herman & Wallace and The Jackson Foundation. These instructors will be teaching two modules of comprehensive pelvic health training with the goal of creating a self-sustaining, continuous education program taught and offered locally. In addition to training a cohort of physiotherapists in assessing and treating the pelvic floor, these American faculty members will be mentoring local Kenyan therapists to teach these courses in an ongoing manner. We at the Institute are proud and thrilled to be a part of spreading this knowledge and skillset in this currently-underserved region.
The courses offered will comprise H&W's Pelvic Floor Series, with the addition of content relevant to Kenya, including obstetric fistula and female genital mutilation. According to the Worldwide Fistula Fund, there are ~ 2 million women and girls suffering from fistulas. Estimates range from 30 to 100 thousand new cases developing each year; 3-5 cases/1000 pregnancies in low-income countries. A woman may suffer for 1-9 years before seeking treatment. For women who develop fistula in their first pregnancy, 70% end up with no living children.
Have you ever had a dream hidden so deep in your heart you never even spoke it aloud?
The dream for me, to someday teach internationally will come to fruition in February 2022. Jenni Gabelsberg DPT, WCS, MSc, MTC; Quozette Valera PT, DPT; and I will travel to Africa to teach pelvic health in Nairobi City, Kenya through a partnership between Herman & Wallace and The Jackson Foundation.
Richard Jackson, a prominent clinician, educator, and businessman himself (The Jackson Clinics, Richard Jackson Seminars, and The Jackson Foundation), had his own dream to build the quality of physical therapy in Africa by educating and empowering clinicians through an evidence-based curriculum developed by Richard and taught by his staff. Richard served two years in the Peace Corps in Kenya in the late 70s. He taught PT at Kenya Medical Training College. In 2010 a former colleague of his moved from the US back to Ethiopia to address and equip PT education and educators in the country. This led to a partnership where Richard helped develop the first DPT program in Africa. “We were in Ethiopia for seven years. We started a residency program that turned into a doctoral program in physical therapy. In December 2017, we graduated 17 DPTs and now we are out. It is sustainable. It’s up to them to carry on and they have the curriculum and the skills,” said Richard in this article.
In 2012 the program Richard stated reproduced and blossomed in Nairobi, Kenya. Let’s talk for a second about what the field of PT is like in Kenya. In a country of almost 54 million people, there are about 2,000 PTs. Thirty-five percent (700) are women, as reported by the Kenya Society of Physiotherapists. The degree is a diploma that takes 3 years to earn, and there are 9 programs available.
There is a women’s health section along with other specialty sections. Medical care has both private and public facilities which can have a wide variation in amenities. After offering specialty training in orthopedics and neurology, Richard recognized the need to expand training to pelvic health. Thus, a partnership between Herman & Wallace, The Pelvic Health and Rehab Center, and The Jackson Foundation was born. In 2019 three cohorts of teachers: Nancy Cullinane PT, MHS, WCS, Kathy Golic PT, and Terri Lannigan PT, DPT, OCS taught module one; Kathy Golic, Casie Danenhauer, and Sherine Aubert fielded a second module; and then educated and equipped the first class of 35 pelvic health graduates. The foundation of the Kenyan Pelvic Health Program thus laid; the future looked bright!
Then…covid brought everything to a screaming halt.
Almost three years later, the program will eagerly resume in Nairobi City.
One can imagine in a country with so few therapists, so few female therapists, and even fewer (think under 50!) pelvic health therapists, the desperate need for pelvic health training and treatment is difficult to fathom. Add to that the strain of a rather patriarchal society where women's health may not be readily accepted or addressed.
In her blog about her experience in Kenya, Sherine Aubert reflects, “To me, this two-week course was way beyond teaching pelvic floor physical therapy - it was truly empowering women to speak up for themselves and each other in the medical community. It provided a voice for anyone suffering from pelvic floor issues to seek help.”
As for Jenni, Quozette, and I, we are beyond humbled and excited to be a part of this experience. Per Richard, "Everyone has come back from these experiences profoundly changed."
If you would like to support this program, we are open to your ideas, expertise, and connections. You can also make a tax-deductible donation to The Jackson Foundation here.
If you have connections to help us bring donations of pelvic health supplies, please contact one of us at jennafermi@gmail.com or jgablesPT@gmail.com
For further information:
Read about Richard Jackson.
- https://www.middleburglife.com/world-class-care-at-the-jackson-clinics/
- https://www.orthopt.org/uploads/content_files/files/Jackson.pdf
- https://www.teachandtreat.org/
Read about the 2019 pelvic health training in Kenya:
- https://hermanwallace.com/blog/pelvic-floor-level-1-is-heading-to-kenya
- https://hermanwallace.com/blog/week-one-at-kenya-medical-training-college-in-nairobi-kenya
- https://hermanwallace.com/blog/the-second-course-module-in-nairobi-kenya
Read more about PT in Kenya:

Another circle around the sun.
Another covid pandemic run.
Courses scheduled all year round.
Remote Courses. Live Events, and Satellites abound.
From Oncology and the Pelvic Floor Level 1and Pregnancy Rehabilitation.
To Pain Science for the Chronic Pelvic Pain Population.
Instructors are ready.
With TAs aplenty.
Prove your advanced expertise
And sit for the PRPC.
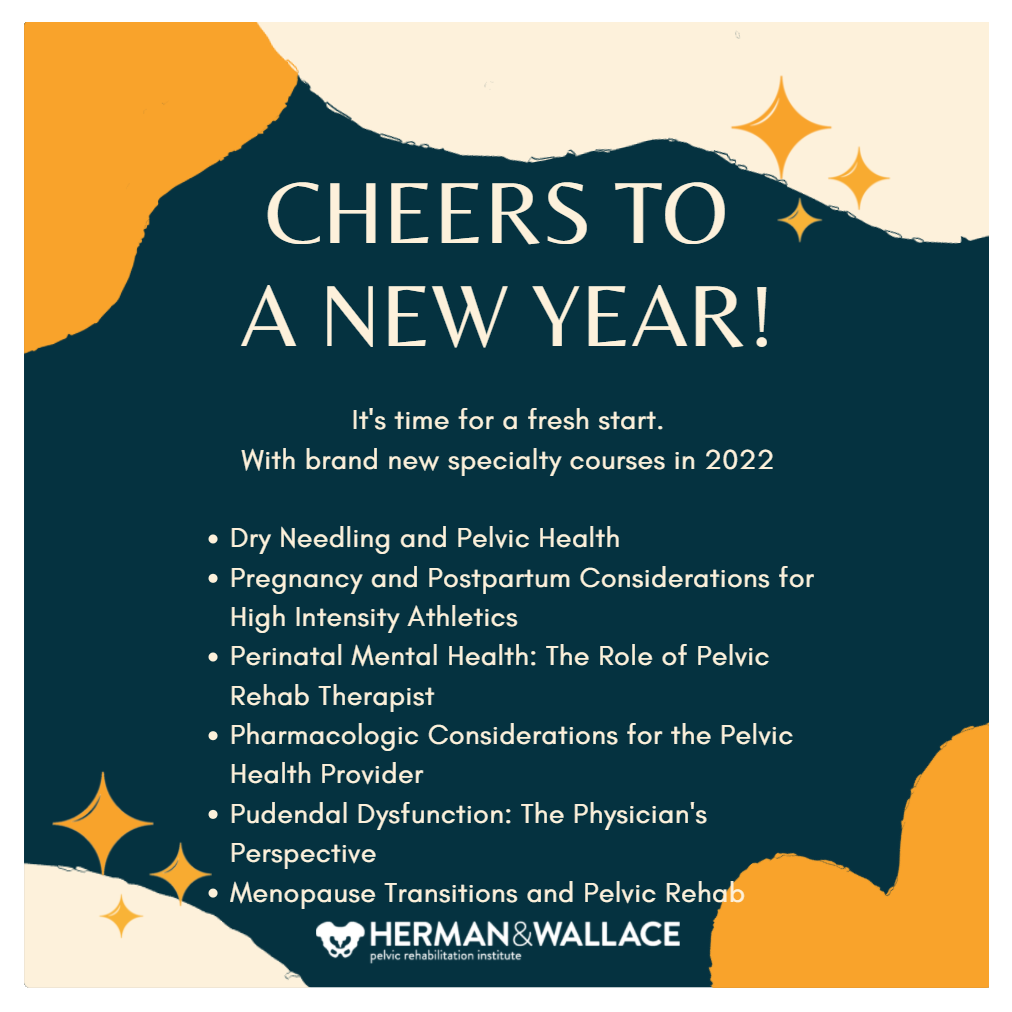
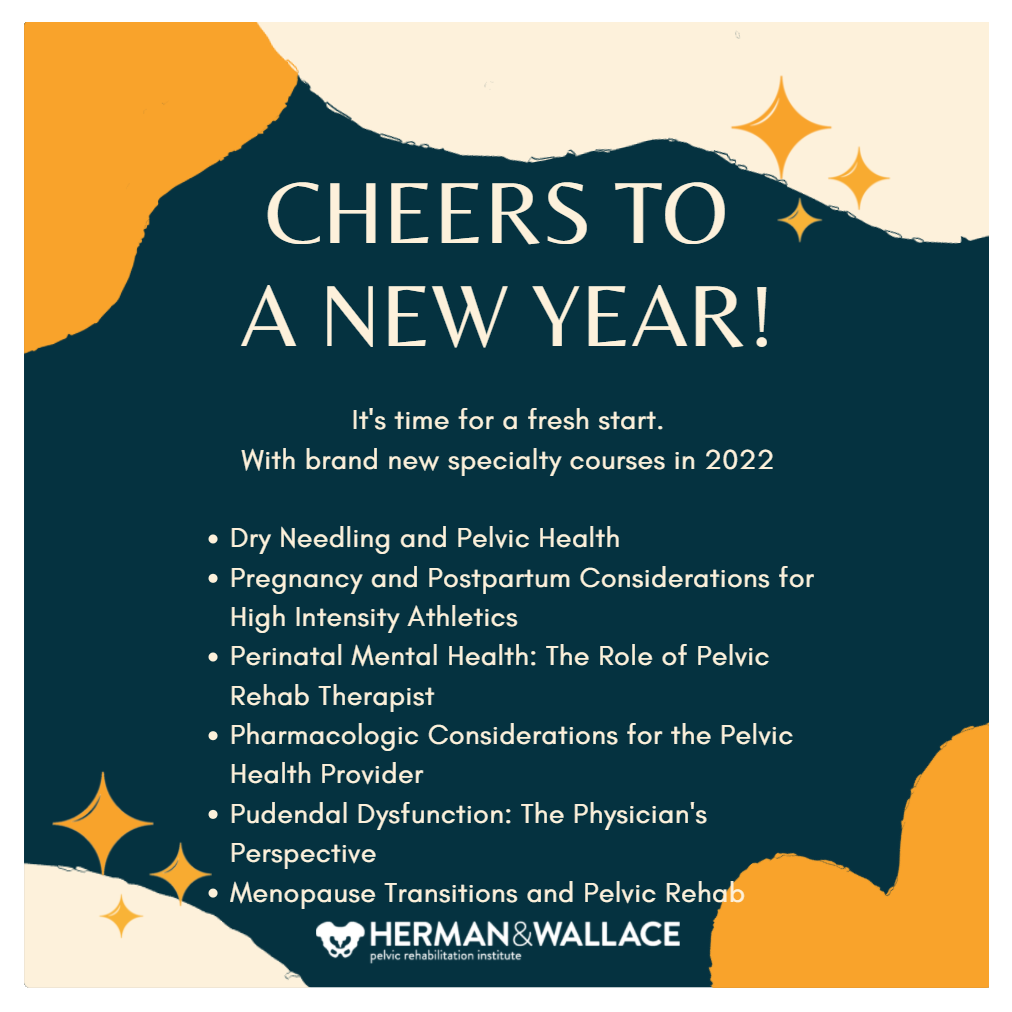
Our resolution here at Herman & Wallace is to provide even more course content for you! Our plan is to have a total of 22 new courses from 2021-2022 available and over 400 course events/satellites scheduled! In addition, we at H&W want to take the time to let our faculty, teaching assistants, hosts, and students know how much we appreciate you! As the pandemic continues into 2022, know that we see you. We appreciate all that you do and the efforts that you go to.
The best way to make an attainable New Year's Resolution is to use SMART goals. Most of us have seen SMART goals used for work and business decisions. Keep the specific, measurable, and time-specific aspects of goal setting while making sure they are attainable and realistic.
Did you set any New Year's Resolutions yet? If not, then here are 5 suggestions!
- Learn something new. Have fun while challenging yourself to take the next step in your pelvic rehab journey. H&W offers courses that are beginner, intermediate, and advanced levels.
- Build your confidence. Whether it is in gaining confidence in internal exams, or in treating the lumbar nerve H&W has a course for you.
- Meditate & Practice Mindfulness in your personal life and practice. H&W recommends joining Restorative Yoga for Physical Therapists or Boundaries, Self-Care and Meditation.
- Try something that scares you. Push yourself to try things that are out of your comfort zone. Take a new course for a different patient demographic to incorporate into your daily practice such as Bowel Pathology and Function or Transgender Patients: Pelvic Health and Orthopedic Considerations
- Volunteer. Give back to the Pelvic Rehab Community by TA'ing for a satellite course.
Herman & Wallace wishes you a fresh start with renewed energy and confidence throughout the New Year. Happy 2022!
Herman & Wallace has more than 55 different courses with over 200 individual course events scheduled throughout the year to choose from. Our course catalog is growing all the time with new courses, new instructors, more course dates, and even more satellite locations!
In 2022 there are already six BRAND NEW courses available, with more to be planned. H&W is kicking off the new year strong with Dr. Michael Hibner on January 9th with Pudendal Dysfunction: The Physician's Perspective. Kristina Koch is back in 2022 with her newly updated and reformated course, Pharmacologic Considerations for the Pelvic Health Provider which is scheduled for April 10, July 9, and November 19th.
Do you live near Salt Lake City, Utah? Our first live, in-person course since the pandemic will be there on March 12-13, 2022: Dry Needling and Pelvic Health.
- Disclaimer: Due to the nature of this course content, it will be delivered in the traditional "in-person" manner. This means the course instructors will be teaching at a single location, and it will not be possible to join the course remotely via video conference. As with all Herman & Wallace courses, this course content is only intended for practitioners who are licensed appropriately, and for whom dry needling is within their scope of practice. It is the responsibility of every course registrant to check with their state boards to ensure that the content of a Herman & Wallace course that they attend is within their state-specific scope of practice.
Interested in women's health? There are 3 new courses appearing this year:
- Perinatal Mental Health: The Role of Pelvic Rehab Therapist - February 5, 2022
- Menopause Transitions and Pelvic Rehab - March 5-6, 2022
- Pregnancy and Postpartum Considerations for High-Intensity Athletics - May 21, 2022
Are you thinking about taking a course, but not sure if it is for you? H&W courses are for licensed practitioners interested in the field of pelvic rehabilitation. The most common registrants that we see in our courses include:
- Doctor of Osteopathic Medicine (DO)
- Doctor of Chiropractic (DC)
- Nurse-Midwives (CNM)
- Nurse Practitioners (ARNP)
- Occupational Therapists (OT)
- Occupational Therapists Assistants (OTA)
- Physical Therapists (PT)
- Physical Therapists Assistants (PTA)
- Doctor of Medicine (MD)
- Physicians Assistants (PA)
- Registered Nurses (RN)
H&W courses are classified as Beginner (no prerequisites), Intermediate (one prerequisite), or Advanced (two or more prerequisites). A Beginner course can be taken by a licensed practitioner without prior coursework requisites. Therapists interested in registering for an Intermediate or Advanced course must review the prerequisites on the course description and honestly assess/report their fulfillment of the published prerequisites.
For example, courses that have Pelvic Floor Level 1 as a prerequisite require a working knowledge of performing internal assessments. It is never recommended that a participant skip this introduction without prior training or experience performing an internal exam. Some courses are part of a series and it is not recommended that they be taken out of order. On the Continuing Education Courses page, you can click the Experience Level tab to see courses organized by level of difficulty.
Clinical experience or alternative coursework may be a substitute for the published course requirements, and it is recommended that a therapist considering opting out of a published prereq review the objectives of the required course and assert that said objectives have been met. Review the Course Overview and Objectives on each course page and ask yourself what your treatment goals (in both the long and short term) are and what patient population you are targeting. All courses list the learning objectives, which will give you a lot of information about what you'll be learning at a given course.
If you would like additional guidance on which course offering best fits your goals and target patient population, please contact us! We are here to guide you into an event that best suits your needs.
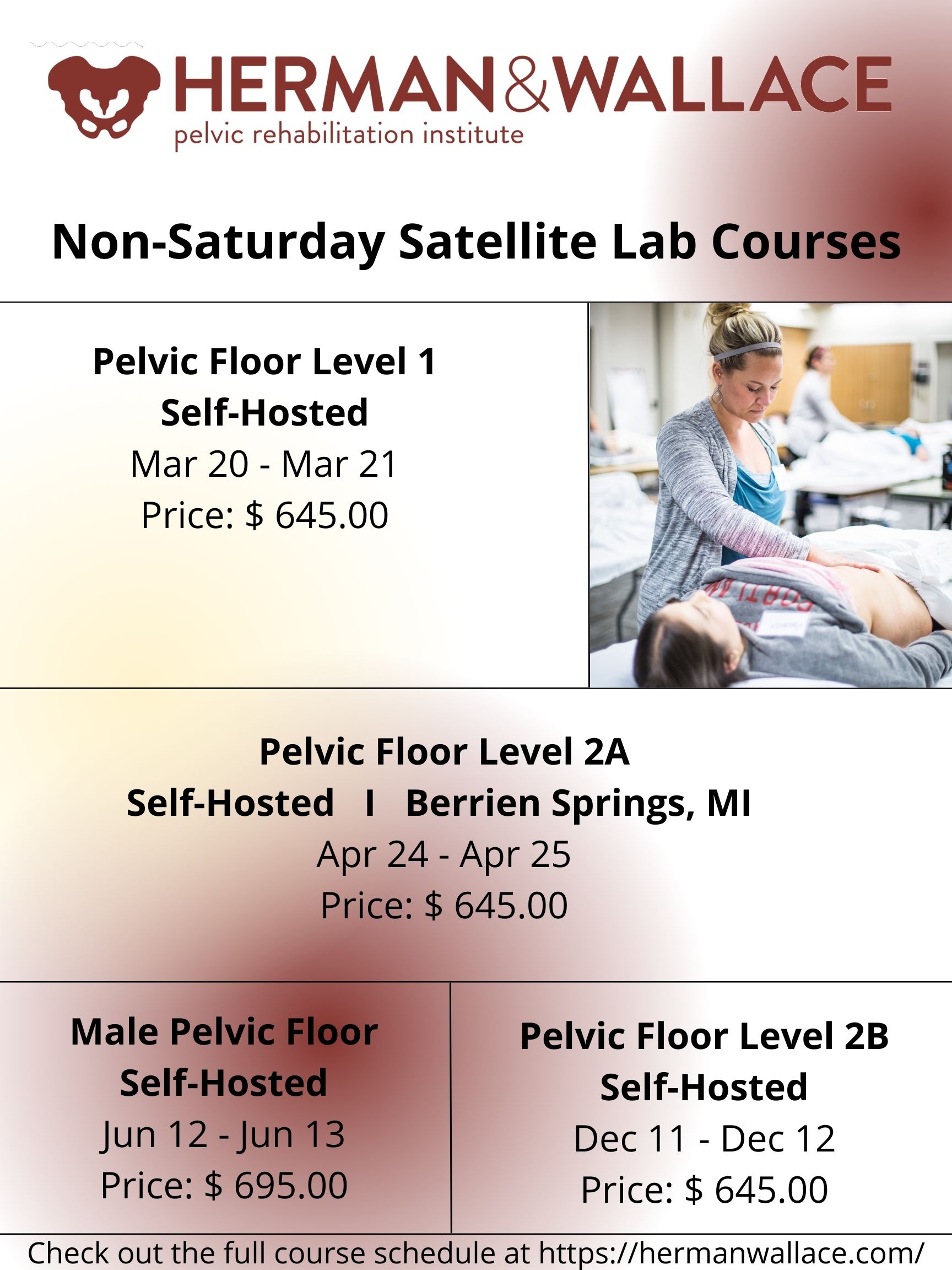
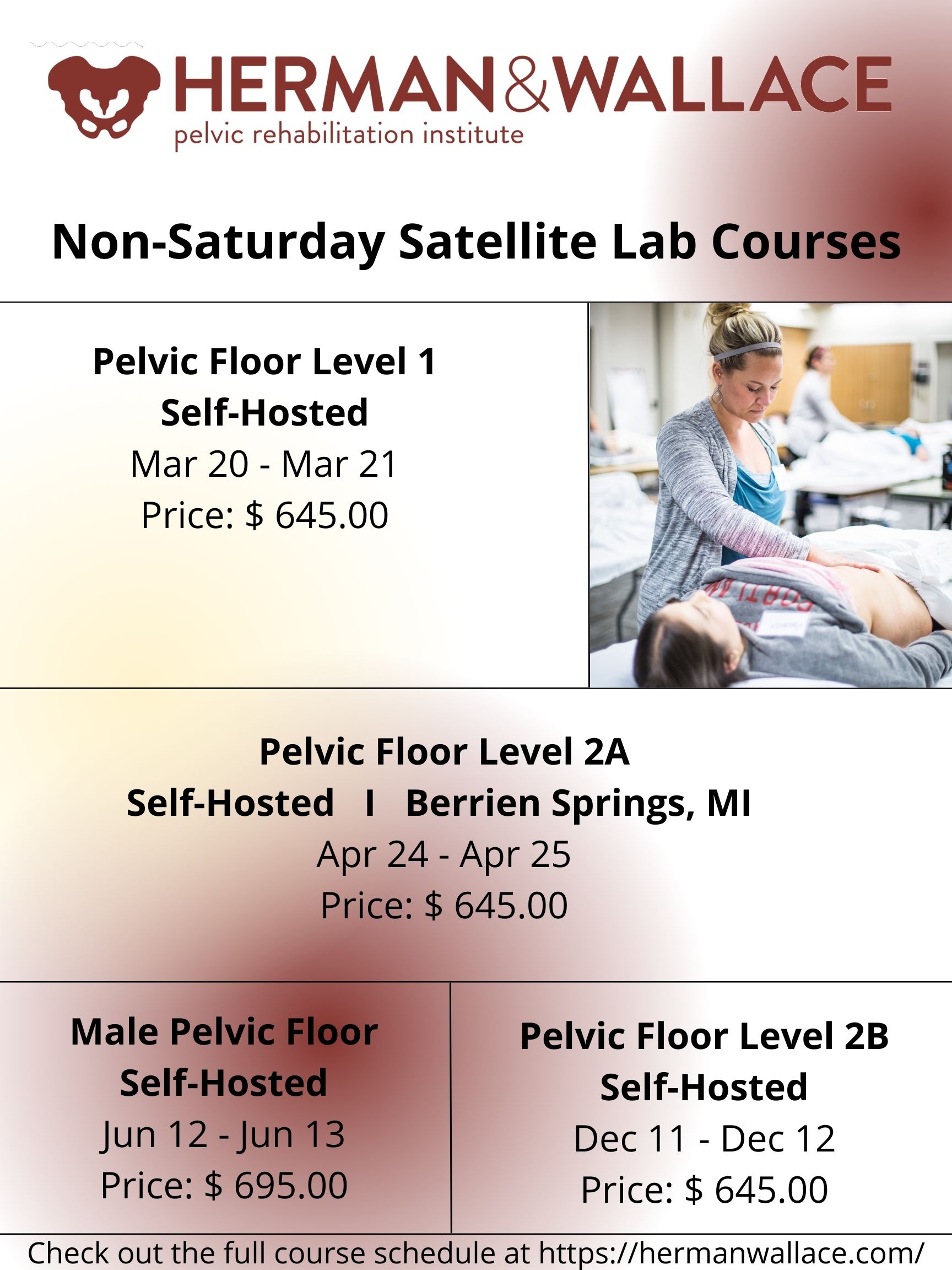
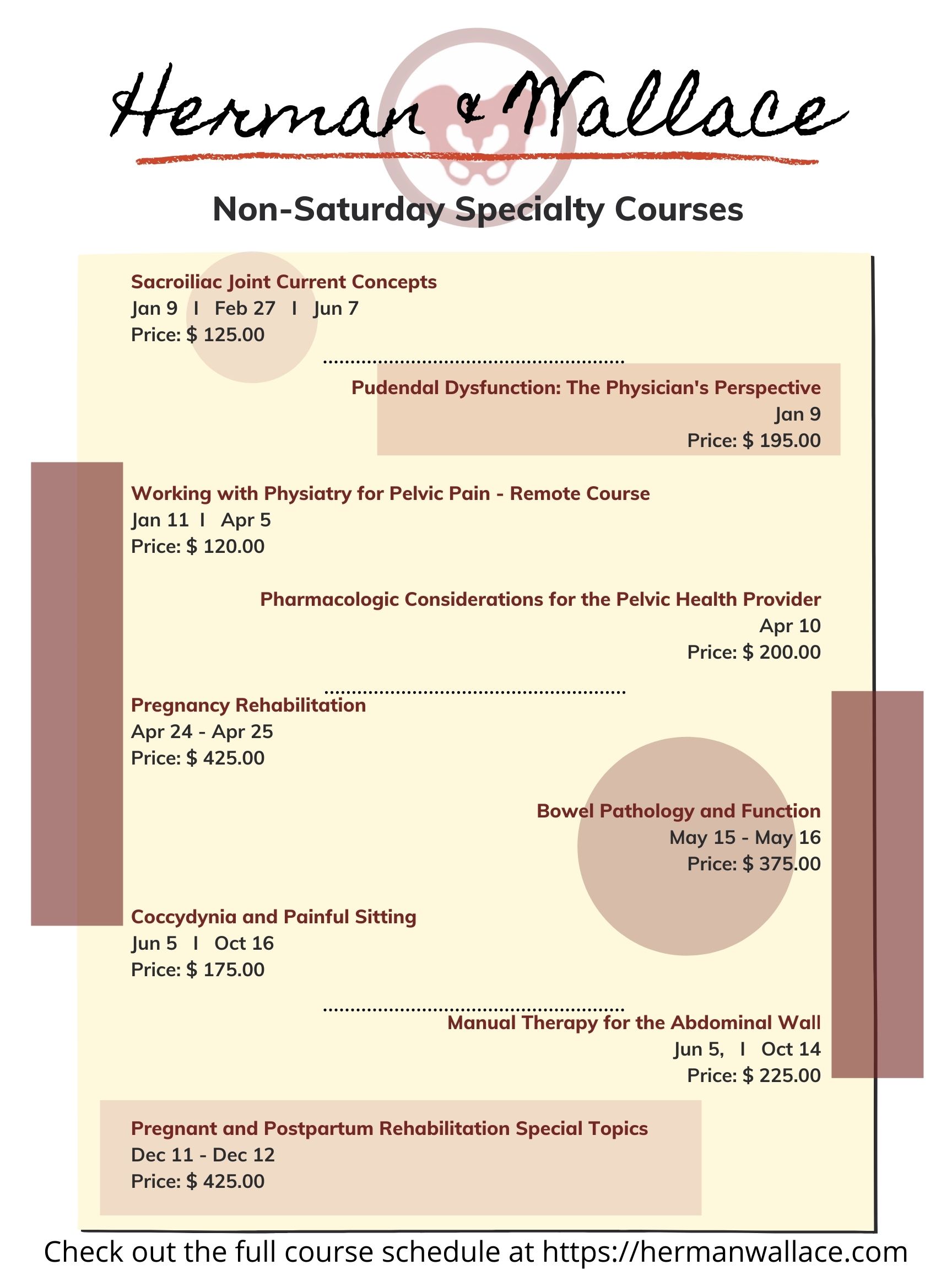
Did you know that Herman & Wallace provides continuing education courses for other weekdays than Saturday?
There is a wide selection of courses that fall on other weekdays. From Pelvic Floor Level 1 scheduled March 20-21, 2022 on Sunday and Monday to our specialty courses such as Working with Physiatry for Pelvic Pain scheduled for Tuesday, January 11, 2022.
Are you interested in attending a satellite lab course, but don't see a satellite available? Do you know a clinic that would be able to host? Feel free to reach out to us through the Host A Course form online.
Generally, H&W is looking for locations to host that have the following:
- Room for about 10-14 therapists to gather (with social distancing)
- Space for folks to sit six feet apart during lecture
- Roughly one lab table for every two participants (5 tables for a 10 person group)
- The following AV equipment:
- LCD projector and table for projector
-
- Laptop with Zoom downloaded - plugs into the projector and plays the instructor teaching live on Zoom
- Projection screen
- Speakers - Bluetooth or plug into the laptop. These do not have to be fancy, but they need to be loud enough that everyone can hear
We look forward to seeing you in one of our courses in the upcoming year!
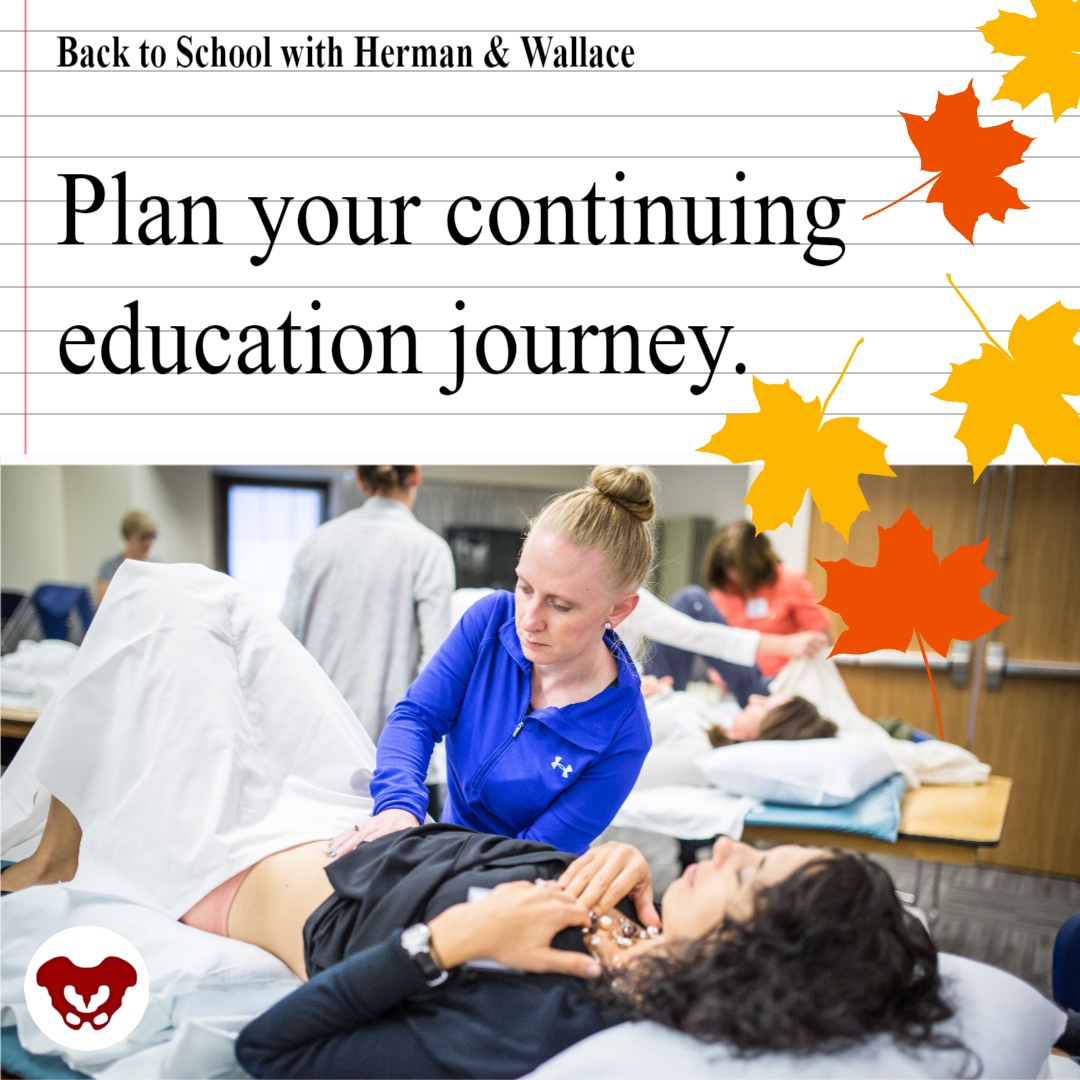
It’s back-to-school time for Herman & Wallace! H&W courses are provided in one of two formats: remote courses, and satellite lab courses.
Our team here at H&W has been working hard to schedule courses throughout the rest of this year and into 2022. If you are looking for the perfect course, then check the course catalog. We are adding course events to the schedule every week. There are several brand new course options on the schedule.
New Satellite Lab Courses:
Satellite lab courses allow participants and teaching assistants to gather in small groups to view lectures and practice hands-on labs. The satellite lab course also has an option where you can register with a partner and attend remotely together as a Self-Hosted Satellite.
- Rehabilitative Ultrasound Imaging - Orthopedic Topics November 12-13, 2021
- Rehabilitative Ultrasound Imaging - Women's Health and Orthopedic Topics November 12—14, 2021
- Biofeedback for Pelvic Muscle Dysfunction December 4-5, 2021
New Remote Courses:
Remote courses allow registrants to attend entirely from home or another safe location. Registrants in remote courses can often attend the course "solo" and do not need to find a partner or small group. In terms of COVID-19, remote courses are our safest option for those who want to eliminate their potential exposure to other registrants.
- Shockwave Treatment: Therapeutic Interventions in Pelvic Health & Demystifying the Research September 12, 2021
- Oncology of the Pelvic Floor Level 2A October 2-3, 2021
- Weightlifting and Functional Fitness Athletes October 16, 2021
- Transgender Patients: Pelvic Health and Orthopedic Considerations October 30, 2021
- Fertility Considerations for the Pelvic Therapist November 7, 2021
- Doula Services and Pelvic Rehab Therapy December 4, 2021
- Pudendal Dysfunction: The Physician's Perspective January 9, 2022
- Perinatal Mental Health: The Role of Pelvic Rehab Therapist February 5, 2022
Don't see the course you are looking for? Check out the full course list on the Herman & Wallace Continuing Education Courses page.
The following post comes from Dawn Sandalcidi PT, RCMT, BCB-PMD author and instructor of the Pediatric Incontinence and Pelvic Floor Dysfunction course, and the more recent follow-up course, Pediatric Functional Gastrointestinal Disorders. Dawn has developed a pediatric dysfunctional voiding treatment program in which she lectures on nationally. She has further studied pediatric conditions in post graduate work at Regis University. Dawn has published articles in the Journal of Urologic Nursing, the Journal of Manual and Manipulative Therapy, and the Journal of Women’s Health Physical Therapy.
Growing up, I was blessed to be around children with Cerebral Palsy (CP), which stimulated my desire to become a physical therapist, a career that I love more now than when I started nearly 38 years ago!
Did you know….
The incidence of Cerebral Palsy in Nepal is estimated to be over 60,000. The Self -Help Group for CP estimate that 80% of children (and adults) also present with bowel and bladder leakage which significantly affects their quality of life and leads to infections and other medical complications. Additionally, a recent pilot study revealed an incidence of urinary leakage in school children aged 10-16 years at 73%, as compared to 6-13% in developed countries. This has shown me a clear and meaningful need to help CP kids in Nepal who are tragically affected.


Pictures from http://www.cpnepal.org/about.html
Through a partnership with the University in Nepal, I will be training Nepali Physical Therapists how to treat children with bowel and bladder issues. Nepal currently does not have any trained providers - this training will provide sustainability as these providers will be able to treat multiples of children with bowel bladder issues, in addition to strategies for prevention. The plan is also to visit several villages with a Self-Help Group for Cerebral Palsy children to educate families and caregivers how to manage incontinence and constipation in these children.
I need your help to accomplish this!
I will be donating a 3-day training for PT’s and several caregiver trainings for this project. With your help I can secure needed supplies, bring physical therapists from remote villages to the course and help with travel expenses.
The Prometheus Group has generously donated an entire biofeedback system with pediatric animation to the hospital, but additional lead wires and electrodes are needed to run the system.
What’s needed?

- Supplies for treatments
- Electrodes for 1 child $4.60 x 100 =$460
- Additional lead wires and adaptors - $340 per set – 2 sets per year= $680.00
- Airfare and Travel Expenses (Hotel, etc.) to help offset the costs of - $3,750.00
My goal is to raise approximately $6,000 to help improve the quality of life for these children.
Your Support Will Make a Great Impact:
- $50 will help pay for electrodes for 10 children
- $150 will bring a physical therapist from a remote region to the course
- Any $ amount will help me educate the therapists in Nepal to sustain the program and treat thousands of children = PRICELESS
A donation of any size will make a difference and will be tremendously appreciated. Please consider donating an amount that feels comfortable to you and know that you are impacting the health, well-being and quality of life for Nepalese children.
This is a personal mission - I’m asking for a personal donation (which unfortunately is not tax-deductible) to help me make a difference in the lives of these children. My hope is to train the physical therapists in Nepal who will in turn continue to train others. Training the trainers is the most sustainable way for me to begin this grass-roots process.
I need to be funded by February 29!
3 Options for donations
1. Venmo @Dawn-Sandalcidi- no fees
2. https://fundly.com/nepal-2020-1 (fees apply)
3. Mail a check directly (no fees) to:
3989 E. Arapahoe Rd #120
Centennial, CO 80122
Thank you so much for your consideration!
Dawn Sandalcidi
Update: Please note that this course is now only offered online through the instructor's website. For more information visit https://pelvicpainrelief.com/laser/
Herman & Wallace is announcing a new course on laser therapy for pelvic pain! The Pelvic Rehab Report caught up with the instructor, Isa Herrera.
Laser Therapy For Female Pelvic Pain was developed by Isa Herrera MSPT, CSCS for Herman and Wallace specifically for women’s health clinicians. Ms. Herrera is the author of 4 books, including the breakthrough book, Ending Female Pain, A Woman’s Manual, now in its 2nd Edition. Ms. Herrera has appeared on several national TV and radios shows including on MTV True Life, The Regis and Kelly Show and NBC’s Today Show. She lectures nationally on the topic of women’s health and has been a passionate advocate about pelvic health for over 10 years.
Can you describe the clinical/treatment approach/techniques covered in this continuing education course?
Laser Therapy For Female Pelvic Pain Conditions (LTFPP) is a two-day intensive course that provides the clinician with hands-on experience and treatment protocols using low level laser for the relief female chronic pain conditions that include vestibulodynia, vaginismus, bladder, coccyx and scar pain.
“This class is one in which pelvic floor therapists bring their foundational knowledge of anatomy, neurology and previous training and learn to apply it to laser therapy. “ says Ms. Herrera. “In this class I will share with you my treatment protocols that I have used at my healing center for the last ten years. These treatment protocols are safe and help provide pain relief, reducing injury damage and loss of function. Your patients will oftentimes see immediate results,” she continued.
What inspired you to create this course?
“Clinicians deal with female chronic pain on a daily basis that can be problematic to treat and manage. There is an arsenal of tools, exercises and techniques at their disposal, but many times using a proven modality can help to accelerate the pain-relieving process for the patient. I created this course not only to help the women out there who suffer everyday with debilitating pain, but also to help clinicians achieve even more success with their treatments.”
What resources and research were used when writing this course?
- Atlas Of Clinical Anatomy-Frank Netters
- Grays Anatomy
- Ending Female Pain, 2nd edition, Isa Herrera
- Herman and Wallace PF 1, PF2, PF3
- V Book by Elizabeth G. Stewart and Paula Spencer
- Travell and Simmons Volume 2. Myofascial Pain and Dysfunction: The Trigger Point Manual. The Lower Extremities
- Current Research Articles on Low Level Laser Therapy
Why should a therapist take this course? How can these skill sets benefit his/ her practice?
“This class is for the clinician that is working in the field of women’s health and who typically treats female chronic pain conditions. Clinicians looking for a non-invasive modality, one that is easy to operate and provides reliable and effective treatment options, will see great value in this course. This course provides the clinician with protocols and applicable information on the safe usage of low level laser therapy for female pelvic pain,” says Herrera.
We are thrilled to announce that Herman and Wallace instructor, Carolyn McManus, MPT, will co-present an educational session with internationally recognized pain researcher Etienne Vachon-Pressseau, PhD at APTA’s NEXT meeting in Chicago on June 13. Dr. Vachon-Presseau is an assistant professor at the Alan Edwards Centre for Research on Pain at McGill University and has led pioneering research into stress-associated brain changes in patients with persistent pain.
 In a presentation entitled, When Stress Complicates Care for Your Patient in Pain: Evidence-Based Mechanisms and Treatment, Dr. Vachon-Presseau will discuss the latest research and theory illuminating the role of stress in the maladaptive neuroplastic brain changes observed in patients with chronic pain. Carolyn will discuss direct clinical applications of this marterial and highlight research on the role of mindfulness in the self-regulation of stress and pain. She will share a practical model for integrating mindfulness into physical therapy for the treatment of persistent pain conditions.
In a presentation entitled, When Stress Complicates Care for Your Patient in Pain: Evidence-Based Mechanisms and Treatment, Dr. Vachon-Presseau will discuss the latest research and theory illuminating the role of stress in the maladaptive neuroplastic brain changes observed in patients with chronic pain. Carolyn will discuss direct clinical applications of this marterial and highlight research on the role of mindfulness in the self-regulation of stress and pain. She will share a practical model for integrating mindfulness into physical therapy for the treatment of persistent pain conditions.
We are excited that Carolyn has been offered this honor to co-present at NEXT with a world renown researcher in the field of pain and contribute her insights from an over 30-year career specializing in mindfulness and pain. She will offer her popular course, Mindfulness-Based Pain Treatment, in Portland OR, July 27 and 28 and in Houston TX, October 26 and 27. We recommend these unique opportunities to train with Carolyn, a nationally recognized leader trailblazing the successful applications of mindfulness into the field of physical therapy. Hope to see you there!