Men who present with chronic pelvic pain frequently have symptoms referred along the penis and into the tip of the penis, or glans. Symptoms may include numbness, tingling, aching, pain, or other sensitivity and discomfort. The tip of the penis, or glans, is a sensory structure, which allows for sexual stimulation and appreciation. This same capacity for valuable sensation can create severe discomfort when signals related to the glans are overactive or irritating. One of the most common complaints with this symptom is a level of annoyance and distraction, with level of bother worsening when a person is less active or not as mentally engaged with tasks. Wearing clothing that touches the tip of the penis (such as underwear, jock straps, jeans, or snug pants) may be limited and may worsen symptoms. When uncovering from where the symptoms originate, the culprit is often the dorsal nerve of the penis, which is sensible given that the glans is innervated by this branch of the pudendal nerve. If we consider this possibility (because certainly there are other potential causes) we find that there are many potential sites of pudendal nerve irritation to consider. First, let’s visualize the anatomy of the nerve.
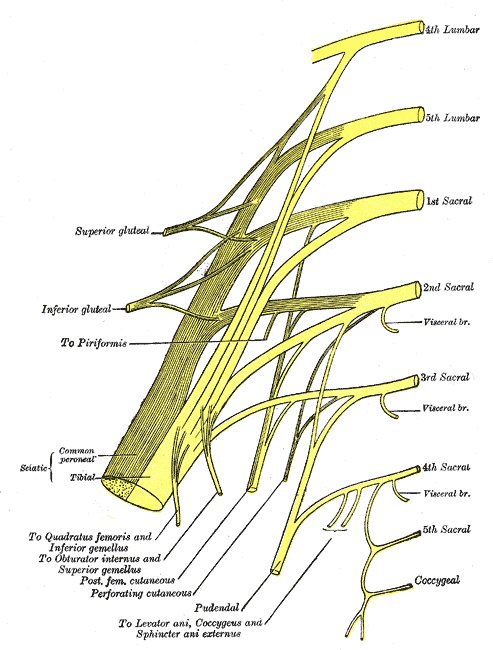
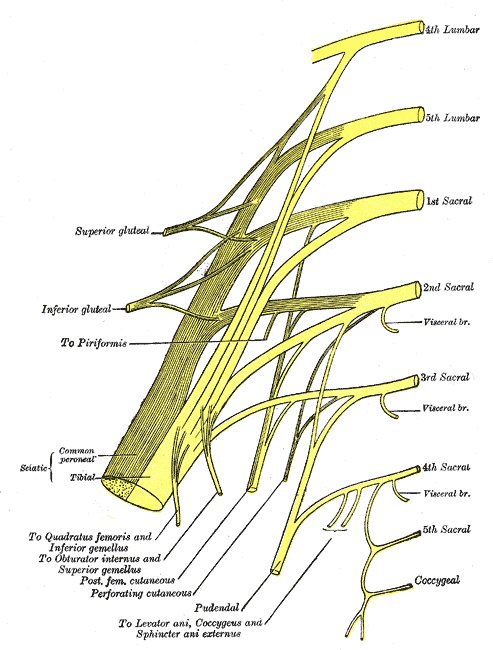
Following the usually accepted descriptions of the dorsal nerve, we know that it is a terminal branch of the pudendal nerve that primarily is created from the mid-sacral nerves. This can lead us to include the lumbosacral region in our examination and treatment, yet in my clinical experience, there are other sites that more often reproduce pain in the glans. As the dorsal nerve branches off of the pudendal, usually after the location of the sacrotuberous ligament, it passes through and among the urogenital triangle layers of fascia where compression or irritation may generate symptoms.
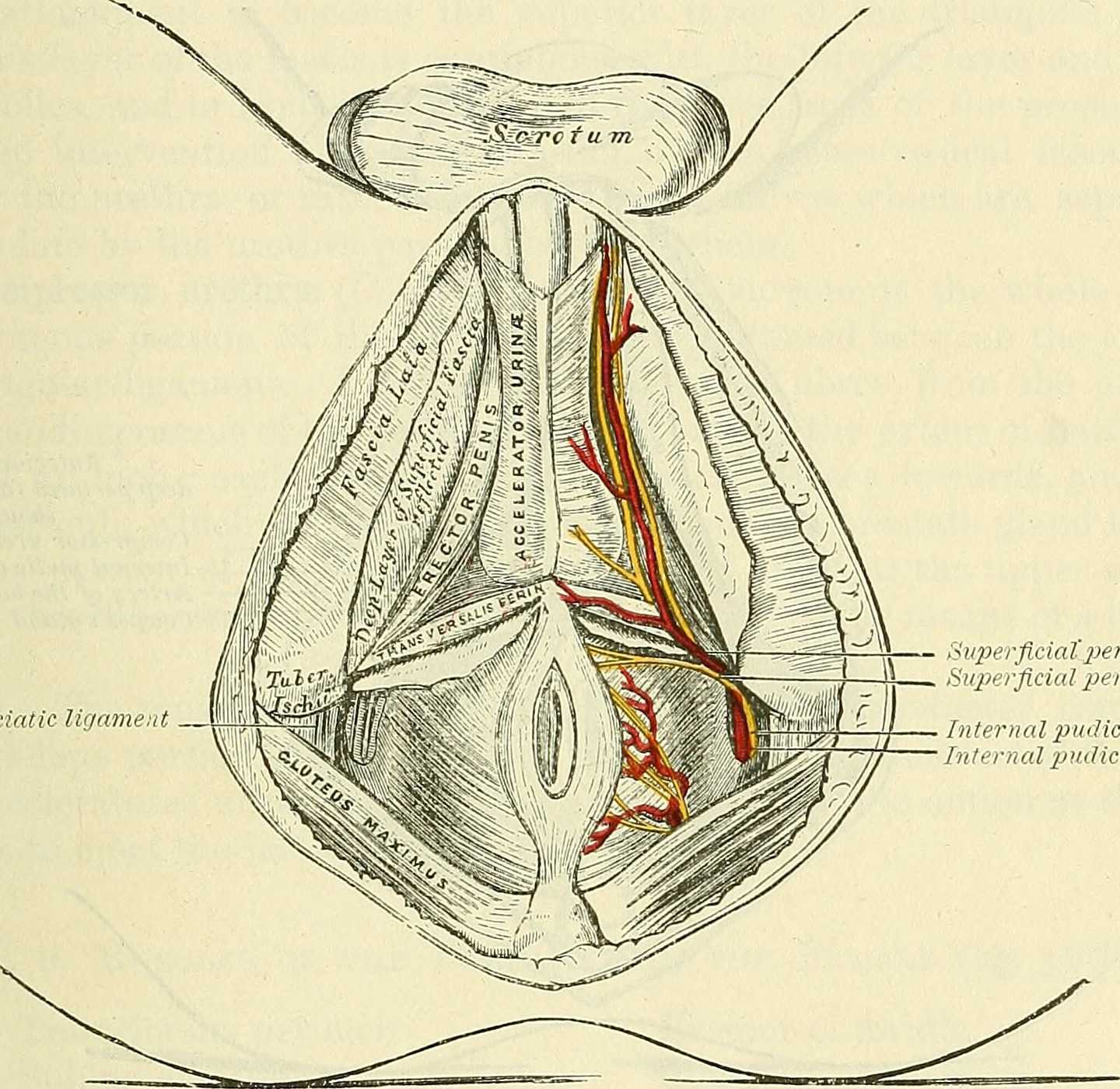
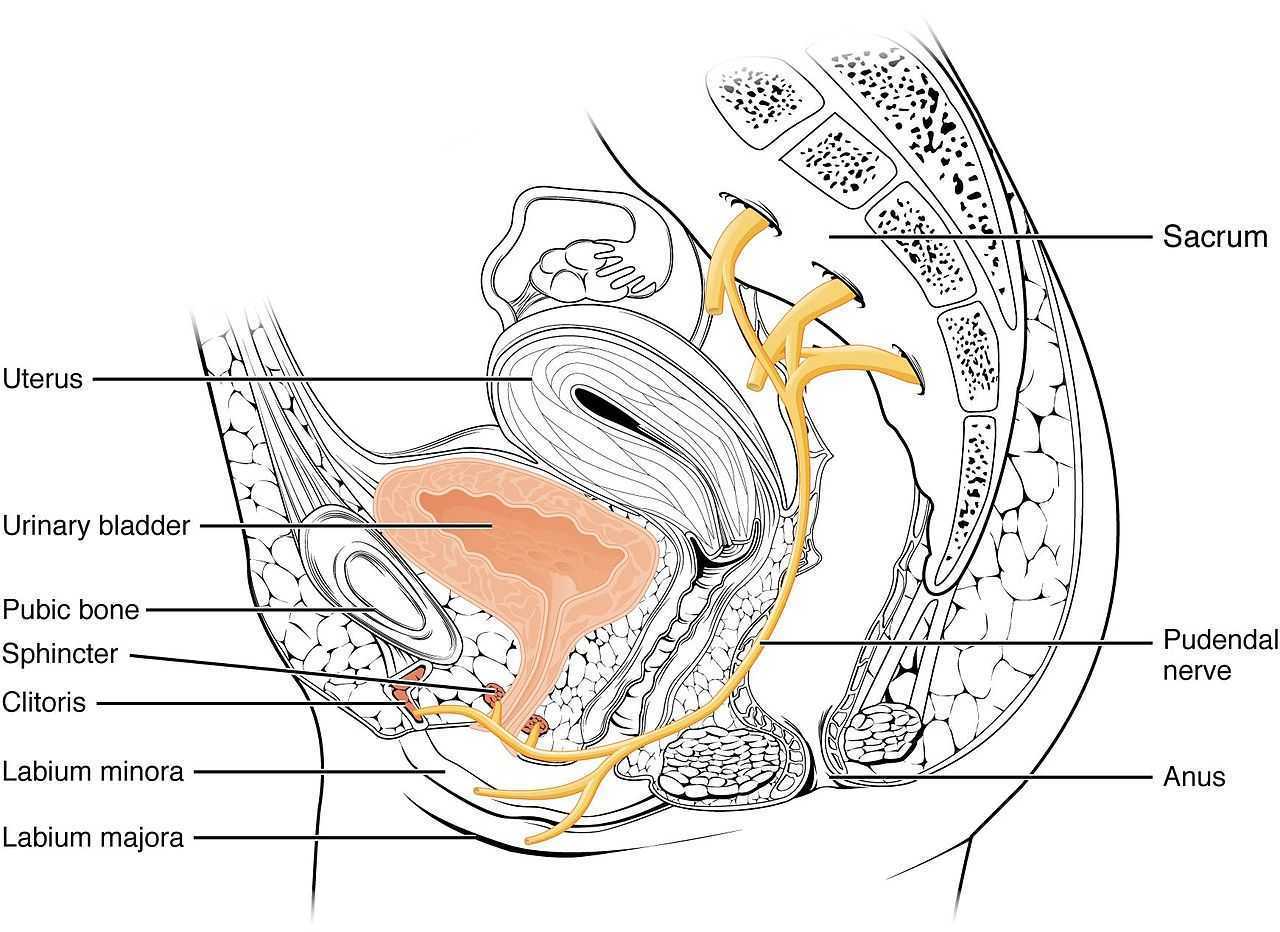
As the nerve travels towards the pubic bone, it will pass inferior to the pubic bone, a location where suspensory ligaments of the penis can be found as well as pudendal vessels and fascia. This is also a site of potential compression and irritation, and palpation to this region may provide information about tissue health. Below is a cross-section of the proximal penis, allowing us to see where the pudendal nerve and vessels would travel inferior to the pubic bone.
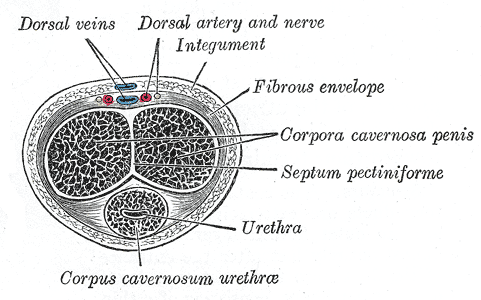
As the dorsal nerve extends along either side of the penis, giving smaller branches along its path towards the glans, the nerve may also be experiencing soft tissue irritation along the length of the penis or even locally at the termination in the glans.
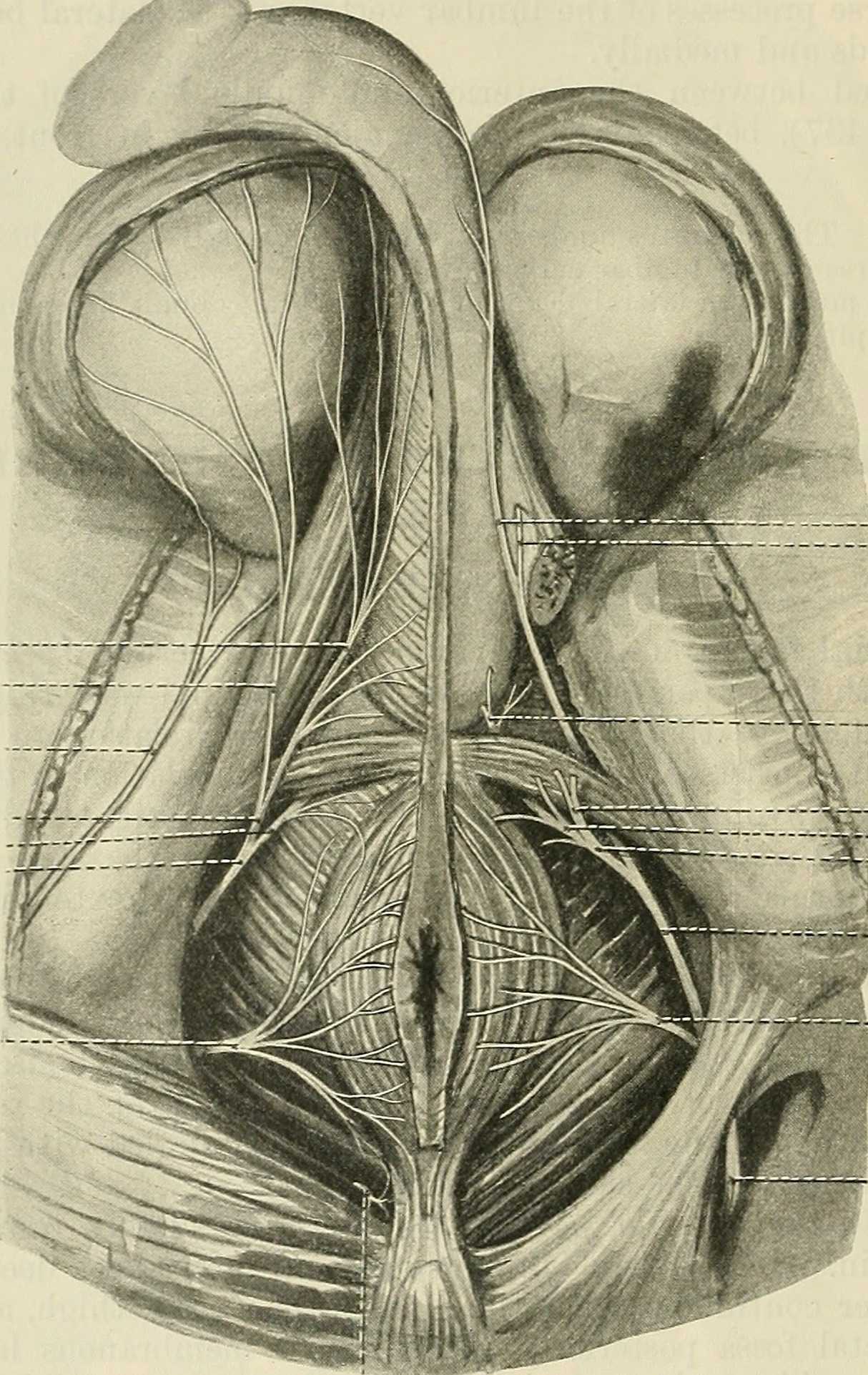
Palpation internally (via rectum) or externally may be a part of the assessment as well as treatment of this condition. Oftentimes, tip of the penis pain can be reproduced with palpation internally and directed towards the anterior levator ani and the connective tissues just inferior to the pubic bone. It may be difficult to know if the muscle is providing referred pain, or if the nerve is being tensioned and reproducing symptoms, however gentle soft tissue work applied to this area is often successful in reducing or resolving symptoms regardless of the tissue involved. In my experience, these symptoms of referred pain at the tip of the penis is often one of the last to resolve, and the use of topical lidocaine may be helpful in managing symptoms while healing takes place. Home program self-care including scar massage if needed, nerve mobilizations, trunk and pelvic mobility and strengthening, and advice for returning to meaningful activities can play a large role in resolution of pain in the glans.
If you would like to learn more about treating genital pain in men, consider joining me in Male Pelvic Floor: Function, Dysfunction, & Treatment. The 2018 courses will be in Freehold, NJ this June, and Houston, TX in September.
Erica Vitek, MOT, OTR, BCB-PMD, PRPC is the author and instructor of Neurologic Conditions and Pelvic Floor Rehab, a new course coming to Grand Rapids, MI and Philadelphia, PA. This post is the next in her series on creating a course about neurologic conditions and pelvic rehabilititation.
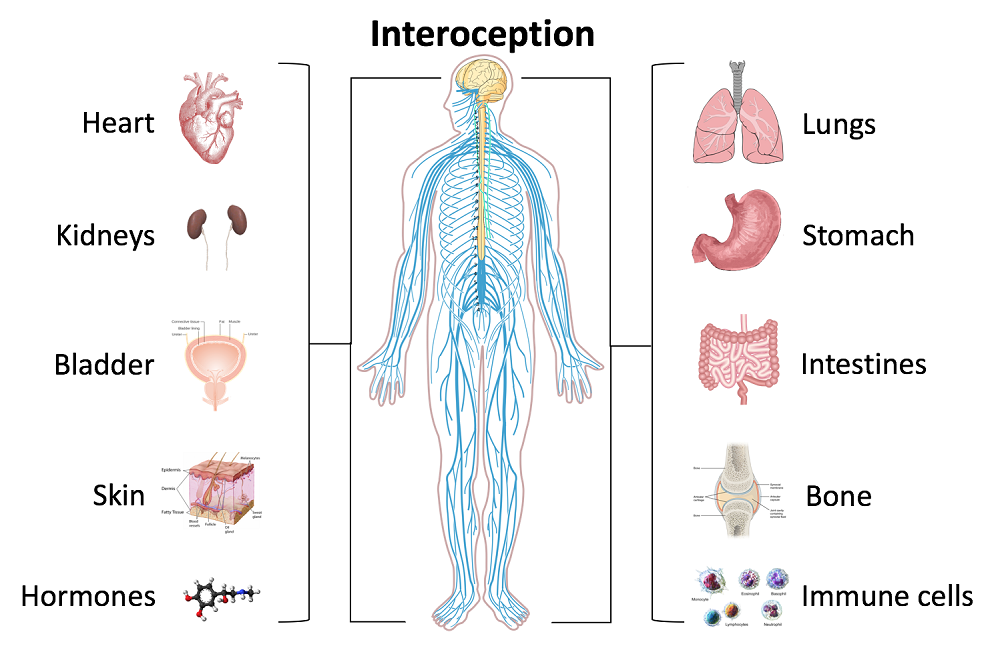
Being a clinician, as we evaluate and treat people with pelvic health conditions, we typically take all systems of the body into account. We take the problem presented to us by the client and we examine, from all angles, how we might go about advice and treatment to best achieve their goals in alleviating the problem. We do a full review of medical history and pharmacology. We examine our client in-depth from a musculoskeletal perspective. We look at psychological contributions to the problem they are facing. We can look at their lifestyle and have them make a detailed diary to help us analyze their bladder, bowel, fluid intake and dietary habits. Do we also always include a look at the neurological components? Do we know what we are looking for? What are the best tools we can have in our toolbox as clinicians to look at our client’s problem through a “neuro brain”?
 In writing each lecture of this course, I have had to step back each time I am developing a new concept and look at it with in-depth thought and contemplation about how I will use this in the clinic to assess my client’s concerns using a neuro-based approach. Taking the concepts and facts about the musculoskeletal system that we know well and then taking a look at the neurological systems contributions and relationship to that dysfunction can be challenging. The main reason for this challenge is that neuro system dysfunction is many times hard explain, presents with inconsistent or changing symptoms, may have motor or sensory deficits together or by themselves, may radiate to different locations than where the true dysfunction is located, and may have developed into central sensitization causing a hypervigilance to typically non-painful stimuli.
In writing each lecture of this course, I have had to step back each time I am developing a new concept and look at it with in-depth thought and contemplation about how I will use this in the clinic to assess my client’s concerns using a neuro-based approach. Taking the concepts and facts about the musculoskeletal system that we know well and then taking a look at the neurological systems contributions and relationship to that dysfunction can be challenging. The main reason for this challenge is that neuro system dysfunction is many times hard explain, presents with inconsistent or changing symptoms, may have motor or sensory deficits together or by themselves, may radiate to different locations than where the true dysfunction is located, and may have developed into central sensitization causing a hypervigilance to typically non-painful stimuli.
In brain storming our ideas for course creation, much was said about thinking back to college or other continuing education courses and “learning a little about a lot of things neuro” but not the in-depth knowledge one might want to have when focusing their attention on specific neurodegenerative conditions such as Parkinson disease, demyelinating diseases such as Multiple Sclerosis, injury to the brain due to cerebral vascular accident or incomplete or complete spinal cord injury.
As I progress deep into the development of this course, I have my “neuro brain” on and a persistent focus set on providing clinicians with as much in-depth information on neurological contributions to pelvic floor function and dysfunction. I want clinicians to walk away from this course feeling confident that through evaluation of a client that has been diagnosed with Parkinson disease, Multiple Sclerosis or suffered a spinal cord injury, they would have the tools to develop an in-depth treatment plan that would provide these clients with the best results possible to improve their quality of life. I also want clinicians to have the confidence to market themselves to their local neurologists. This is an entirely new avenue for developing a referral base in pelvic health work. Many times for clients who have chronic neurological conditions, the problem list is long and bladder, bowel and sexual health concerns might not even be broached within the very short physician appointment times. We can give our neurologists new treatments to be confident in and excited about to improve their patient’s quality of life!
My 6 year old girl (going on 13) asks “Alexa” to play the Descendants II soundtrack over and over again. So the song, “Space Between,” was lingering in my head while reading the most recent articles on pudendal neuralgia, particularly when pudendal entrapment is to blame. After all, entrapment, by medical standards, describes a peripheral nerve basically being caught in between two surrounding anatomical structures.
 Ploteau et al., (2016) presented 2 case studies highlighting the warning signs when pudendal nerve entrapment does not follow the Nantes criteria. A brief summary of those 5 criteria follows:
Ploteau et al., (2016) presented 2 case studies highlighting the warning signs when pudendal nerve entrapment does not follow the Nantes criteria. A brief summary of those 5 criteria follows:
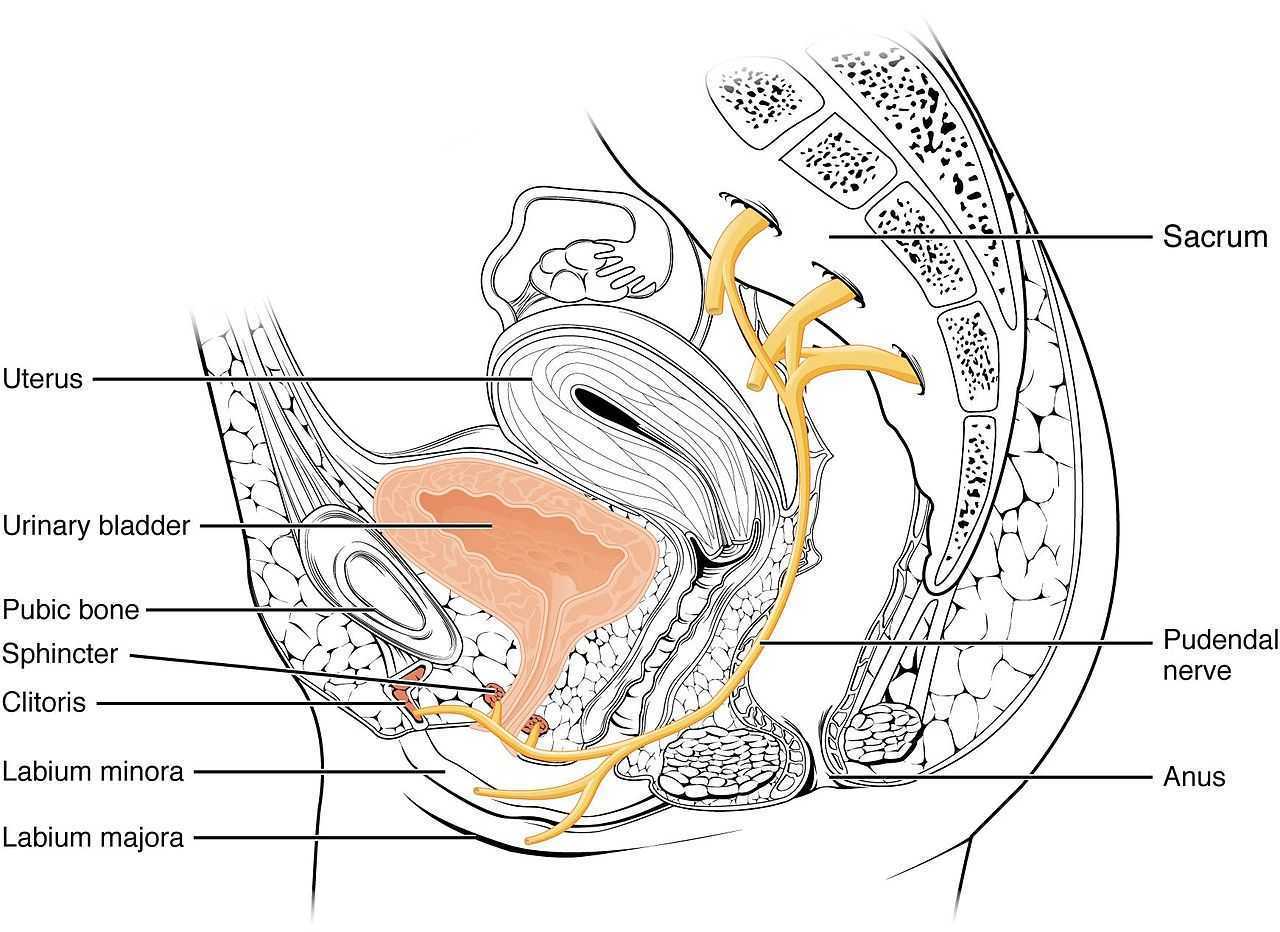
- Pain in the region of the pudendal nerve innervation from anus to penis or clitoris.
- Pain most predominant while sitting.
- The patient does not wake at night from the pain.
- No sensory impairment can be objectively identified.
- Diagnostic pudendal nerve block relieves the pain.
The case studies of a 31 and a 68 year old female revealed endometrial stromal sarcoma and adenoid cystic carcinoma in the ischiorectal fossa, with night pain was noted in both patients, as well as no pain with sitting or defecation, respectively. Clinicians must always be mindful to resolve red flags in patients.
In 2016, Florian-Rodriguez, et al., studied cadavers to determine the nerves associated with the sacrospinous ligament, focusing on the inferior gluteal nerve. Fourteen cadavers were observed, noting the distance from various nerves to the sacrospinous ligament (from a pelvic approach) and to the ischial spine (from a gluteal approach). The S3 nerve was closest to the sacrospinous ligament, and the pudendal nerve was the closest to the ischial spine. In 85% of subjects, 1 to 3 branches from S3/S4 nerves pierced or ran anterior to the sacrotuberous ligament and pierced the inferior part of the gluteus maximus muscle. The authors concluded the inferior gluteal nerve was less likely to be the source of postoperative gluteal pain after sacrospinous ligament fixation; however, as the pudendal nerve branches from S2-4, it was more likely to be implicated in postoperative gluteal pain.
A study by Ploteau et al. (2017) explored the anatomical position of the pudendal nerve in people with pudendal neuralgia. In 100 patients who met the Nantes criteria, 145 pudendal nerves were surgically decompressed via a transgluteal approach. At least one segment of the pudendal nerve was compressed in 95 of the patients, either in the infrapiriform foramen, ischial spine, or Alcock’s canal. In 74% of patients, nerve entrapment was between the sacrospinous ligament and the sacrotuberous ligament. Anatomical variants were found in 13% of patients, often with a transligamentous course of the nerve.
When the pudendal nerve is caught in the narrow space between ligaments in the pelvis, diagnosing the source of pain is paramount. Research supports a gluteal approach in releasing the entrapped nerve. Post-surgical care falls into the hands of pelvic floor therapists, so taking “Pudendal Neuralgia and Nerve Entrapment: Evaluation and Treatment” may be something to consider in order to provide optimal care.
Ploteau, S, Cardaillac, C, Perrouin-Verbe, MA, Riant, T, Labat, JJ. (2016). Pudendal Neuralgia Due to Pudendal Nerve Entrapment: Warning Signs Observed in Two Cases and Review of the Literature. Pain Physician. 19(3):E449-54
Florian-Rodriguez, ME, Hare, A, Chin, K, Phelan, JN, Ripperda, CM, Corton, MM. (2016). Inferior gluteal and other nerves associated with sacrospinous ligament: a cadaver study. American Journal of Obstetrics and Gynecology. 215(5):646.e1-646.e6. doi: 10.1016/j.ajog.2016.06.025
Ploteau, S, Perrouin-Verbe, MA, Labat, JJ, Riant, T, Levesque, A, Robert, R. (2017). Anatomical Variants of the Pudendal Nerve Observed during a Transgluteal Surgical Approach in a Population of Patients with Pudendal Neuralgia. Pain Physician. 20(1):E137-E143
In an effort to provide the best possible educational experience for clinical rehabilitation application of neuroanatomy, I was on a mission. Having a core, base knowledge review of the nervous system is essential when leading into talking about dysfunction and disease of that system. I went on a search for anatomical depictions that could clearly identify the structures and processes I was trying to portray. New books from the library and books I own from when I was in college serve as great resources when trying to get back into studying the specifics, but do not offer the opportunity to easily get these images into a powerpoint. Online resources are also challenging. I am learning how time consuming the process can be to determine who owns the online image, if it is free to copy, save and utilize for my own teaching purposes, or if I need to go through the process of requesting permissions for use.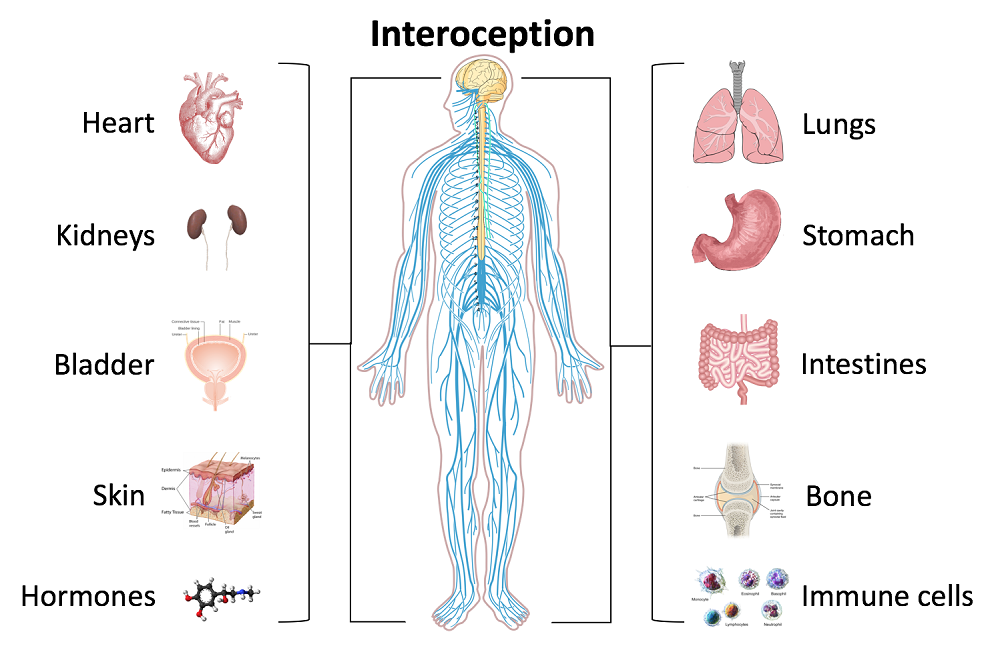
Through my employer, where I treat patients in the clinic, I have access to a program called Primal Pictures. I had used this in the past for clinic related marketing presentations and educational materials for patients and other clinicians I have mentored. Looking into the product further, I came to find out that there is a newer version of the program which offered so many more options. A truly unlimited amount of images which can be manipulated into an optimal position depicting the most clear neuroanatomical views I have ever been able to find. Not only does it provide me with the images I need in order to depict the treacherous pathways of the nerves in our body, but it also provides some amazing depictions of the physiological processes that occur within our nervous system to allow for healthy day to day functioning and protection of our bodies.
I also came across the title of a journal article that I was sure would provide some excellent depictions of neuroanatomy. The article titled, Sectional Neuroanatomy of the Pelvic Floor, provides cross sectional views of both the male and female pelvises. I obtained the article which has an excellent color-coded system, each nerve colored the same as the muscles and skin surface it innervates, going from superior to inferior cross sections. This makes for a clear understanding of each structures anatomical position. It is a great reference when looking at the anatomical relationships to adjacent structures and can help guide palpation skills. The article was more specifically written for physicians to best direct needle procedures/injections in the most accurate location possible when targeting nerves and structures. Neuroanatomy and physiology can be essential to understanding certain patient populations we encounter as we practice pelvic floor rehabilitation. Having clear depictions to refer to can help you provide the best possible base knowledge to your patients as you help them understand the challenges they face and how to overcome them.
Kass, J. S., Chiou-Tan, F. Y., Harrell, J. S., Zhang, H., & Taber, K. H. (2010). Sectional neuroanatomy of the pelvic floor. Journal of computer assisted tomography, 34(3), 473-477.