Vestibulodynia is defined as pain at the vestibule, which is the area around the opening of the vagina (introitus). Being diagnosed with vestibulodynia can leave patients feeling frustrated because it doesn’t explain WHY they have pain at the vestibule. There are several types of vestibulodynia including infection, inflammation, neoplastic, neurologic, trauma, and hormonal deficiencies.
The most common type of vestibulodynia is caused by hormonal deficiencies known as Hormonally-Mediated Vestibulodynia. This type is caused by hormonal changes including taking birth control, breast feeding, postpartum, estrogen blockers, and peri or post menopause.
The most common cause of Hormonally-Mediated vestibulodynia in younger women (under the age of 25) is systemic birth control (i.e. oral contraceptive pills (OCPs), depo-shot, NuvaRing). Side effects of birth control (BC) such as breakthrough bleeding, nausea, headaches, increased risk of stroke, and abdominal cramping are more commonly discussed among doctors and patients.
However, what is NOT often discussed with patients prior to starting birth control, especially OCPs, is that systemic BC use causes vestibulodynia, decrease vaginal lubrication, decrease thickness of labia minora, and decreased vaginal introitus size, all leading to dyspareunia (painful sex). These changes can occur as early as 90 days after starting OCPs or with long-term use.
Unfortunately, if the onset of birth control was before the age of 17, there’s even a higher risk of developing hormonally associated vestibulodynia.1
So, WHY and HOW, does this happen?
 Systemic birth control gets processed through the liver which INCREASES a protein called the Sex Hormone Binding Globulin (SHBG). SHBG binds to the free testosterone in the blood, so even if your body is making testosterone, high levels of SHBG (from the BC) DECREASE the testosterone in your body. This inhibits testosterone from getting to the tissue that needs it to be healthy—–the vestibule. The vestibule is rich with androgen receptors! If those receptors aren’t getting the testosterone (and estrogen) they need because of the increased SHBG then the vestibular tissue can become painful (vestibulodynia)!
Systemic birth control gets processed through the liver which INCREASES a protein called the Sex Hormone Binding Globulin (SHBG). SHBG binds to the free testosterone in the blood, so even if your body is making testosterone, high levels of SHBG (from the BC) DECREASE the testosterone in your body. This inhibits testosterone from getting to the tissue that needs it to be healthy—–the vestibule. The vestibule is rich with androgen receptors! If those receptors aren’t getting the testosterone (and estrogen) they need because of the increased SHBG then the vestibular tissue can become painful (vestibulodynia)!
Most commonly patients will complain about pain at the opening upon entry, dryness, friction, feeling of tearing, and actual tissue tearing resulting in bleeding, or inability to tolerate penetration at all.
Vestibulodynia can also lead to pelvic floor muscle overactivity which contributes to even more pain! Join the Sexual Medicine in Pelvic Rehab class on the weekend of June 15th-16th to learn how to identify, treat, and differentially diagnose different causes of sexual dysfunctions to get your patients better faster!
Reference:
- Goldstein, A, Burrows L, and Goldstein I. Can oral contraceptives cause vestibulodynia? J Sex Med 2010; 7: 1585-1587
AUTHOR BIO
Tara Sullivan, PT, PRPC, WCS, IF

Dr. Tara Sullivan, PT, PRPC, WCS, IF started in the healthcare field as a massage therapist practicing for over ten years, including three years of teaching massage and anatomy & physiology. During that time, she attended college at Oregon State University earning her Bachelor of Science degree in Exercise and Sport Science, and she continued to earn her Masters of Science in Human Movement and Doctorate in Physical Therapy from A.T. Still University. Dr. Tara has specialized in Pelvic Floor Dysfunction (PFD) treating bowel, bladder, sexual dysfunctions, and pelvic pain exclusively since 2012. She has earned her Pelvic Rehabilitation Practitioner Certification (PRPC) deeming her an expert in the field of pelvic rehabilitation, treating men, women, and children. Dr. Sullivan is also a board-certified clinical specialist in women’s health (WCS) through the APTA and a Fellow of the International Society for the Study of Women's Sexual Health (IF).
Dr. Tara established the pelvic health program at HonorHealth in Scottsdale and expanded the practice to 12 locations across the valley. She continues treating patients with her hands-on individualized approach, taking the time to listen and educate them, empowering them to return to a healthy and improved quality of life. Dr. Tara has developed and taught several pelvic health courses and lectures at local universities in Arizona including Northern Arizona University, Franklin Pierce University, and Midwestern University. In 2019, she joined the faculty team at Herman and Wallace teaching continuing education courses for rehab therapists and other health care providers interested in the pelvic health specialty, including a course she authored-Sexual Medicine in Pelvic Rehab, and co-author of Pain Science for the Chronic Pelvic Pain Population. Dr. Tara is very passionate about creating awareness of Pelvic Floor Dysfunction and launched her website pelvicfloorspecialist.com to continue educating the public and other healthcare professionals.
In March 2024, Dr. Tara left HonorHealth and founded her company Mind to Body Healing (M2B) to continue spreading awareness on pelvic health, mentor other healthcare providers, and incorporate sexual counseling into her pelvic floor physical therapy practice. She has partnered with Co-Owner, Dr. Kylee Austin, PT.
We are preparing for a busy second half of the year, and are seeking hosts for our satellite and in-person course offerings. If you'd like to cut down on travel and earn a free course registration, consider hosting a course with us this year! Satellites require a minimum space for 16 attendees, and in-person courses need to be able to accommodate 30+.
We always want to hear from those interested in hosting our courses. We work with healthcare organizations of all types, sizes, and locations. Please, Contact us about hosting Pelvic Function Level 1 or any other course!
There are two formats of course which you can host, and they are described below.
Satellite Lab Courses (such as those in the Pelvic Function Series)
This is when the instructor presents lectures remotely via Zoom to several satellites at once for a scheduled course date while on-site teaching assistants guide participants at each given location with questions and labs.
Satellite lab events can be great for clinics that have space for 16+ participants, and the following equipment:
- One lab table for every two participants (minimum eight)
- One chair for each participant to use during the lectures
- Either an LCD projector and projection screen OR a large television (minimum of 52" screen)
- Laptop with Zoom downloaded and up-to-date, and any necessary cables to connect the laptop to the projector/TV
- Speakers that are loud enough for the full room to clearly hear the instructor. We DO NOT recommend Bluetooth speakers.
In-Person Courses (such as Modalities and Pelvic Function)
At in-person courses, registrants, teaching assistants, and instructors gather at a single location for lectures and labs. In-person hosts who are located in densely populated areas are prioritized and who have a demonstrated history of successfully hosting courses.
In-person courses can be great for clinics that have space for 30+ participants, including one instructor and 2-3 teaching assistants, and the following equipment:
- One lab table for every two participants (minimum eight)
- One chair for each participant to use during the lectures
- A lapel microphone for the instructor to use during lecture
- Speakers that are loud enough for the full room to clearly hear the instructor. We DO NOT recommend Bluetooth speakers.
Remote Courses
Remote courses take place entirely on Zoom and do not gather in lab groups. However, if there is enough interest in taking a course, it is possible to host one of these courses as an in-person course.
Find out more and submit your hosting interest form today at https://www.hermanwallace.com/host-a-course.
Did you know that you could access and regulate the Vagus nerve through Acupressure points in the ear?
 At HWConnect last year, I had the pleasure of meeting the amazing Ramona Horton. Ramona introduced us to Acupressure points in the outer ear that can directly stimulate the Auricular branch of the Vagus nerve and here you can see us both practicing Auricular Acupressure.
At HWConnect last year, I had the pleasure of meeting the amazing Ramona Horton. Ramona introduced us to Acupressure points in the outer ear that can directly stimulate the Auricular branch of the Vagus nerve and here you can see us both practicing Auricular Acupressure.
Auricular therapy includes Acupuncture and Acupressure in the auricle. The ear is innervated by cranial and spinal nerves, which are separated into motor and sensory areas. The motor area includes the facial nerve, which controls the outer ear muscles. The sensory area is composed of Auricular branches of the Vagus nerve1.
The Auricular branch of the Vagus nerve innervates multiple areas of the ear. The three main areas are the Concha, Cymba Concha, and the Inner Tragus. The miraculous Vagus nerve plays an important role in maintaining physiological homeostasis and autonomic self-regulation across multiple systems in the body. Stimulation of the Vagus nerve through auricular Acupressure can provide Vagal regulation impacting both the autonomic and central nervous systems. The measurement of vagal tone in humans has become one index of stress vulnerability2.
In addition to the acupressure points in the ear, there are several Acupressure points like Central Vessel 17 ( CV 17 ), Yintang ( EX HN3 ), Heart 7, and Pericardium 6 that can be used for calming and self-regulation. Key potent points in the Kidney, Bladder, Spleen, Stomach, Pericardium, and Heart meridians play a vital role in emotional regulation as well as addressing a host of bowel and bladder dysfunctions.
Acupressure is widely considered to be a powerful Complementary & Alternative Medicine (CAM) therapy and is gaining acceptance within the medical community as part of an Integrative medicine approach. It draws its roots from Acupuncture which is part of Traditional Chinese Medicine (TCM) believed to be over 3000 years old. Acupressure involves the application of pressure to points located along the energy meridians of the body which are connected to the visceral functions of vital organ systems.
 Emerging research shows that these Acupoints are embedded in a three-dimensional fascial network throughout the body and have a high electrical conductivity on the surface of the skin. Histological studies show a high density of A and C afferent fibers at these points. Through a vast network of interstitial connective tissue, these Acupoints connect the peripheral nervous system to the central viscera.
Emerging research shows that these Acupoints are embedded in a three-dimensional fascial network throughout the body and have a high electrical conductivity on the surface of the skin. Histological studies show a high density of A and C afferent fibers at these points. Through a vast network of interstitial connective tissue, these Acupoints connect the peripheral nervous system to the central viscera.
Acupressure is a non-invasive, low-cost, and efficient CAM therapy approach and can be used as an adjunct to traditional rehabilitation interventions. Research shows that tapping on Acupressure points has been used as part of Emotional Freedom Techniques (EFT) as well as for the treatment of urinary incontinence, dysmenorrhea, menstrual issues, constipation, anxiety, and a host of other conditions.
The course Acupressure for Optimal Pelvic Health is next offered on June 1st -2nd and explores Acupressure as an evidence-based modality for the management of a host of pelvic health conditions and as a self-regulation modality for the management of anxiety, stress, pain, and symptom management. The course covers two patient home exercise programs with specific potent points for Anxiety and for Daily Wellness and introduces Yin Yoga as a complementary practice to Acupressure.
This course is curated and taught by Rachna Mehta PT, DPT, CIMT, PRPC, RYT 200. Rachna has integrated Acupressure as part of her rehabilitation toolbox for several years now bringing holistic healing and wellness to her patients.
References
- Hou PW, Hsu HC, Lin YW, Tang NY, Cheng CY, Hsieh CL. The History, Mechanism, and Clinical Application of Auricular Therapy in Traditional Chinese Medicine. Evid Based Complement Alternat Med. 2015;2015:495684. doi:10.1155/2015/495684
- Oleson T. Application of Polyvagal Theory to Auricular Acupuncture. Med Acupunct. 2018;30(3):123-125. doi:10.1089/acu.2018.29085.tol
- Monson E, Arney D, Benham B, et al. Beyond Pills: Acupressure Impact on Self-Rated Pain and Anxiety Scores. J Altern Complement Med. 2019;25(5):517-521.
- Au DW, Tsang HW, Ling PP, Leung CH, Ip PK, Cheung WM. Effects of acupressure on anxiety: a systematic review and meta-analysis. Acupunct Med. 2015;33(5):353-359. doi:10.1136/acupmed-2014-010720
- Son CG. Clinical application of single acupoint (HT7). Integr Med Res. 2019;8(4):227-228.
- Kwon CY, Lee B. Acupuncture or Acupressure on Yintang (EX-HN 3) for Anxiety: A Preliminary Review. Med Acupunct. 2018;30(2):73-79.
AUTHOR BIO:
Rachna Mehta PT, DPT, CIMT, PRPC, RYT 200
 Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 graduated from Columbia University, New York with a Doctor of Physical Therapy degree. Rachna has been working in outpatient hospital and private practice settings for over 15 years with a dual focus on Orthopedics and Pelvic Health. She was instrumental in starting one of the first Women’s Health Programs in an outpatient orthopedic clinic setting in Mercer County, New Jersey in 2009. She has authored articles on pelvic health for many publications. She is a Certified Integrated Manual Therapist through Great Lakes Seminars, is Board-certified in Orthopedics, is a certified Pelvic Rehab Practitioner, and is also a registered yoga teacher through Yoga Alliance. Rachna has trained in both Hatha Yoga and Yin Yoga traditions and brings the essence of Yoga to her clinical practice.
Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 graduated from Columbia University, New York with a Doctor of Physical Therapy degree. Rachna has been working in outpatient hospital and private practice settings for over 15 years with a dual focus on Orthopedics and Pelvic Health. She was instrumental in starting one of the first Women’s Health Programs in an outpatient orthopedic clinic setting in Mercer County, New Jersey in 2009. She has authored articles on pelvic health for many publications. She is a Certified Integrated Manual Therapist through Great Lakes Seminars, is Board-certified in Orthopedics, is a certified Pelvic Rehab Practitioner, and is also a registered yoga teacher through Yoga Alliance. Rachna has trained in both Hatha Yoga and Yin Yoga traditions and brings the essence of Yoga to her clinical practice.
Rachna currently practices in an outpatient setting. The majority of her clinical orthopedic practice has focused on treating musculoskeletal, neurological, pre- and post-operative surgical conditions to name a few. She specializes in working with pelvic health patients who have bowel & bladder issues with high pelvic pain which sparked her interest in Eastern holistic healing traditions and complementary medicine. She has spent many hours training in holistic healing workshops with teachers based worldwide. She is a member of the American Physical Therapy Association and a member of APTA’s Academy of Orthopaedic Physical Therapy and the Academy of Pelvic Health Physical Therapy.
Rachna also owns TeachPhysio, a PT education and management consulting company. Her course Acupressure for Optimal Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional, and energy body.

Do you listen to any podcasts? What about podcasts that are focused on pelvic issues and aimed toward the pelvic health practitioner? Here at Herman & Wallace, many of us listen to these and we all have our favorites. Recently HW was lucky enough to work with The Pelvic Service Announcement when Callie and Rachel interviewed Holly Tanner for the episode “Stay Curious and Stay Open” which is available on streaming platforms today.
Who are Callie Teel and Rachel Fritz?
 Callie and Rachel are two physical therapists whose passion for women’s health and commitment to education are changing the way people think about this important field.
Callie and Rachel are two physical therapists whose passion for women’s health and commitment to education are changing the way people think about this important field.
Callie and Rachel first crossed paths at Texas Tech University Health Sciences Center, where they both graduated from physical therapy school in 2021. Following their graduation, the duo began their careers at Optimal Physical Therapy in Amarillo, Texas. It didn't take long for them to realize that there was a significant gap in the public's understanding of pelvic health and the role of pelvic floor physical therapy.
As Callie and Rachel embarked on their new careers, they frequently encountered patients who were unaware of the benefits and importance of pelvic health. Many of these patients were women dealing with postpartum recovery, incontinence, pelvic pain, and other issues that affect quality of life. Callie and Rachel saw an opportunity to make a difference—not just in their clinic but also in the wider community.
Pelvic Service Announcement Podcast
 Determined to bridge the gap in knowledge, Callie and Rachel decided to share their expertise with the public in a way that was both accessible and engaging. This led to the creation of the "Pelvic Service Announcement Podcast," or PSA for short. Through their podcast, they aim to demystify pelvic health, answer common questions, and offer practical advice for anyone interested in learning more about the subject.
Determined to bridge the gap in knowledge, Callie and Rachel decided to share their expertise with the public in a way that was both accessible and engaging. This led to the creation of the "Pelvic Service Announcement Podcast," or PSA for short. Through their podcast, they aim to demystify pelvic health, answer common questions, and offer practical advice for anyone interested in learning more about the subject.
Since launching the PSA podcast, Callie and Rachel have gained a devoted following, with listeners appreciating their down-to-earth approach and willingness to tackle topics that are often considered taboo. They cover a wide range of issues, from pregnancy and childbirth to pelvic pain and sexual health, always with a focus on empowering their audience with knowledge and resources.
For those interested in learning more, the PSA podcast is available on all major streaming platforms. Tune in to hear Callie and Rachel discuss the latest in pelvic health and share valuable insights that you won't want to miss.
Stay Curious and Stay Open Episode Description
Get ready for one of the most exciting guests ever to be featured on The Pelvic Service Announcement. This week, the PSA girls were honored to host Holly Tanner, PT, DPT, MA, OCS, WCS, PRPC, LMP, BCB-PMD, CCI for the first-ever Herman & Wallace podcast collaboration. Holly is the Director of Education for the Herman & Wallace Pelvic Rehabilitation Institute and shared some valuable insights into the world of pelvic health education, managing complicated cases, and navigating interpersonal relationships in the clinic. Whether you're a patient, clinician, or just someone with a love for pelvic health, this is an episode you don't want to miss.
Have you ever heard the phrase “In one ear and out the other?” I sure have, I have vivid memories of my grandmother scolding me for just that. She could never understand how when she said things to me, particularly a list of tasks to do, I could never seem to remember. Funnily enough, my grandfather’s nickname for me was “rabbit ears” because he swore I could pick up on a conversation from anywhere in close proximity so it wasn’t my hearing. Pretty conflicting and confusing, right? I had trouble processing things I heard or remembering them long enough to do them. Years of Catholic school helped to give me structure and tools to keep myself and my fun little brain organized and on task, and I ended up being able to keep up with the rest of my class.
The older and more self-aware I got, the more I realized my brain doesn’t work the way everyone else’s does. The more I worked with kiddos with autism and ADHD, the more I realized my brain worked similarly to theirs. When I first heard the term “neurodivergent” I felt immediately like I had found the answer to a question I didn’t even know existed for myself. This was why I wasn’t the same as other people in processing all things! This is why I had to touch everything to learn about it. This is why I had to rewrite all my notes from professors instead of just being able to absorb what they said. This is why I needed mnemonics, stories, acronyms, and other little “hacks” to learn things.
There are many different ways people can learn. The most common forms of learning consider if a person learns best through visual, aural/ auditory, reading/writing, or kinesthetic movement. Individuals can be any combination of these, which can vary as they grow through life. Someone may start out learning better kinesthetically and learn to process information better visually as they age. In our COVID era, a new format of teaching became more prevalent, bringing “at distance” learning in to save the day in many instances.

The prevalence of distance learning via forums such as Google Meet or Zoom brought up some questions about how well students could learn. Did students learn as well virtually? Did different types of learners have different results? Did how students felt they learned correlate with the outcome measures of learning? Distance education provides the ability for some populations to get education they would not be able to attain otherwise. In a study by Wakahiu & Kangethe, 2014, “participants described learning experiences with profound statements that endorsed online learning as an excellent strategy for fulfilling their dreams to acquire an education.”
Distance learning has many benefits including the ability to learn new materials and achieve new intellectual goals in most locations on a flexible time schedule. Another benefit is the access to visual resources and the potential to be able to rewatch. The decreased cost of transport and the safety (and hopefully less stress) of staying home were also huge benefits. Some disadvantages include not being able to guarantee effective learning, the ability to stay attentive, or be successful with materials. There can be connection and technological problems as well as some students not having the best learning environment in their home (Masalimova et al, 2022). When I think of learning and pelvic health, I think not having face-to-face interaction, accountability, and reinforcement of practicing the skills can hinder some student’s learning ability.
A report by the U.S. Department of Education compared the exam grades for online and face-to-face versions of the same course from 1996 to 2008 and concluded that “online learning could produce learning outcomes equivalent to or better than face-to-face learning (Zheng, 2021).” Cacault et al., 2021 also assessed the effects of online lectures finding that having access to a live-streamed lecture in addition to an in-person option “improves the achievement of high-ability students, but lowers the achievement of low-ability students.”
How does this apply to Herman and Wallace? The pelvic institute has a variety of ways to learn including online courses, self-hosted options, satellite in-person classes with TAs, and in-person classes with instructors. They have made sure to account for different scenarios in order to make pelvic health learning accessible for all they can. The newest addition to the categories of “in person” and “with instructors” is Modalities and Pelvic Function. I had the pleasure of being on the curriculum team for this class and also being one of the instructors for the first run.
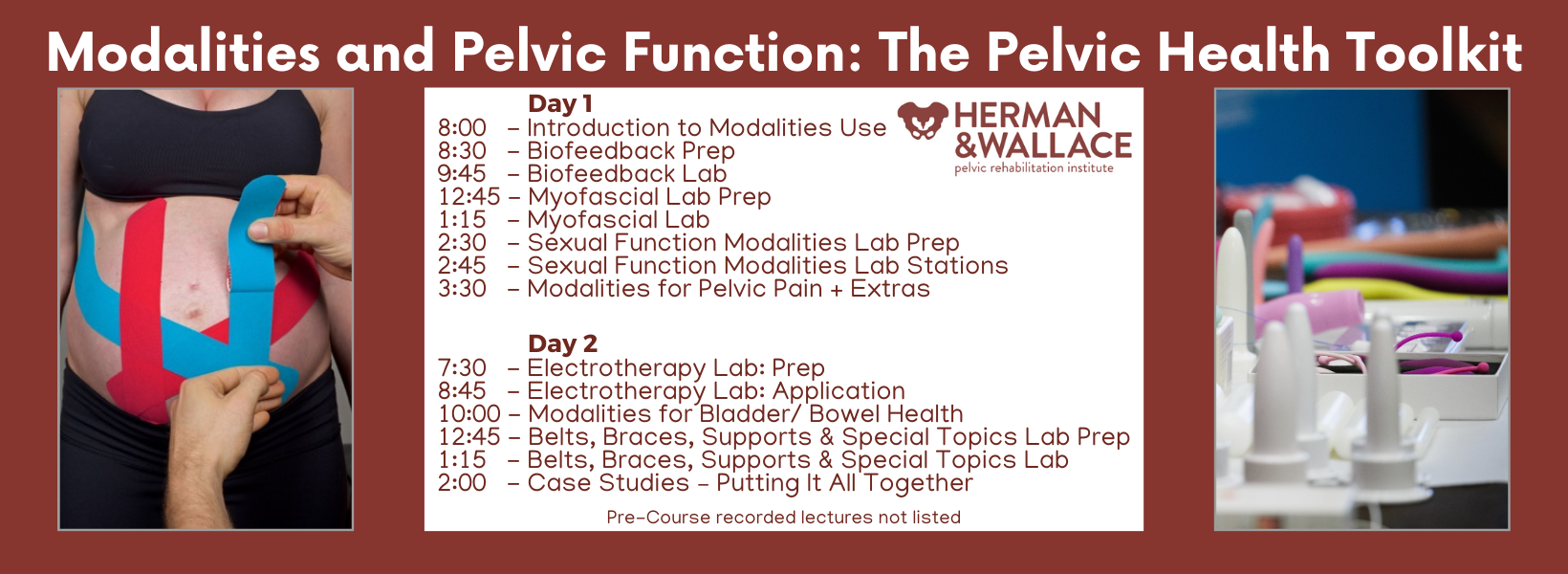
I thought people would like the stuff. I thought they would be excited to try biofeedback and electrical stimulation. I thought they would be pleasantly surprised by prizes and goodie bags full of awesome takeaways. I knew it would be a novel learning experience.
What I did not expect was the overwhelming feedback from participants stating things like“this course was one of the best I have met for my learning style.” The curious part is that when they were asked what their preferred learning style was, they were all different! Some liked to see, some needed to hear it, and some just were there to touch and feel and touch again. Varied practitioners, varied experience levels, varied treatment settings and population and one very consistent point of feedback…”This class just gets me.”
If you’re on the hunt for a class that “puts it all together” when it comes to the tools and toys that can be used for the pelvic floor, check out Modalities and Pelvic Function. Not only are there SO MANY samples (think three shipping crates full - sorry UPS) BUT this class shows you how much is out there to treat pelvic health patients, the pros/cons, the indications, contraindications, and relative precautions as well as the language on how to educate your patient on the use of these items in the clinic or as part of their home self-care routine. Join me this summer either in Raleigh NC on July 13-14 or in Manchester NH on August 24-25!

Don’t believe me…here are two testimonials from our inaugural class!
“Of all of the pelvic floor courses I have taken up to date, this is by far the most enjoyable one! not only did it include how to efficiently treat patients, but it was well organized, exciting content, and everyone was lovely! the instructors were so personable and taught in a way to benefit any learning style. I will be recommending this to all of my fellow PF PTs!” - Rachel Biek, PT, DPT
“I loved the in-person portion of this class! The instructors (Mora and Jenna) were perfect in their roles, we were relaxed and had so much fun exploring the variety of tools to use. The feel of the class was supportive and intimate, and we had adequate time to explore everything. Mora and Jenna did an excellent job, hard to believe this was their first time teaching this class!” - Allison M. Gannon, PT, DPT
REFERENCES:
- Cacault, Christian Hildebrand, Jérémy Laurent-Lucchetti, Michele Pellizzari, Distance Learning in Higher Education: Evidence from a Randomized Experiment, Journal of the European Economic Association, Volume 19, Issue 4, August 2021, Pages 2322–2372, https://doi.org/10.1093/jeea/jvaa060
- Masalimova, A. R., Khvatova, M. A., Chikileva, L. S., Zvyagintseva, E. P., Stepanova, V. V., & Melnik, M. V. (2022, March). Distance learning in higher education during COVID-19. In Frontiers in Education (Vol. 7, p. 822958). Frontiers Media SA.
- Wakahiu, J., & Kangethe, S. (2014). Efficacy of online distance learning: Lessons from the Higher Education for Sisters in Africa Program. European Journal of Research and Reflection in Educational Sciences, 2(1), 1-25.
- Zheng, M., Bender, D. & Lyon, C. Online learning during COVID-19 produced equivalent or better student course performance as compared with pre-pandemic: empirical evidence from a school-wide comparative study. BMC Med Educ 21, 495 (2021). https://doi.org/10.1186/s12909-021-02909-z
AUTHOR BIO:
Mora Pluchino, PT, DPT, PRPC

I am a graduate from Stockton University with my BS in Biology (2007) and Doctorate of Physical Therapy (2009). I have experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. I began treating Pelvic Health patients in 2016 and now have experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much I have not treated since beginning this journey and I am always happy to further my education to better help my patients meet their goals.
I strive to help all of my patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at the present time. In 2020, I opened my own practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. I have been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. I have also been a TA with Herman and Wallace since 2020 and have over 150 hours of lab instruction experience.
Yoga is a common term in our current society. We can find it in a variety of settings from dedicated studios, gyms, inside corporations, online, on Zoom, at home, and on retreat. The basic structure of a typical yoga class is a series of flowing or non-flowing postures, some requiring balance, some requiring going upside down, and many requiring significant mobility to achieve a certain shape. At the end of these classes is a pose called savasana, corpse pose (or sometimes translated for comfort as final resting pose). In this pose, which is often a treat for students after working through class, students lie on the ground, eyes closed, possibly supported by props and rest. It is perhaps the only other time in the day that that person is instructed to lie on the floor in between sleep cycles.
Savasana is one of many restorative yoga postures. In the work created, and popularized by Judith Hanson Lasater, PT, PhD1, restorative yoga has taken a turn away from the active physical postures, breath manipulations, and meditations that are commonplace in how we think of yoga. She has focused on rest and the need for rest in our current climate of productivity, poor self-care, and difficulty managing stress and pain.
In a dedicated restorative yoga class (not a fusion of exercise then rest, or stretch then rest…which are really lovely and have their own benefits), a student comes to class, gathers a number of props, and is instructed through 3 to 5 postures, all held for long durations to complete an hour or longer class. Consider what it would look like to do 3 things over 1 hour with the intent of resting. It is quite a counterculture. Students have various experiences with this type of practice, but over time many begin to feel the need for rest (or restorative practice) in an equivalent way that one feels thirsty or hungry.
We know the benefits of rest: being able to access the ventral vagal aspect of the parasympathetic nervous system is what Dr. Stephen Porges2 suggests supports health, growth, and restoration. There is an impact on the ventral vagal complex in the brainstem that regulates the heart, the muscles of the face and head, as well as the tone of the airway. To heal, we need access to this pathway. To manage stress, we need to access this pathway. To be able to choose our actions rather than be reactionary, we need to access this pathway. Restorative yoga is an accessible method that may be a new tool in a patient’s toolbox to help manage their nervous systems.
Learn how to incorporate restorative yoga in your daily practice and clinic - join Kate Bailey in Restorative Yoga for Physical Therapists on June 15th. You don't have to be a PT to join, all clinicians are welcome!
References:
- Relax and Renew: Restful Yoga for Stressful Times by Judith Hanson Lasater PT, PhD
- Polyvagal Theory by Stephen W Porges PhD
AUTHOR BIO:
Kate Bailey, PT, DPT, MS

Kate Bailey received her Doctorate in Physical Therapy and Master of Science in Anatomy from the University of Delaware. Her physical therapy practice is focused on pelvic health for all genders and ages. Kate brings over 15 years of teaching movement experience to her physical therapy practice with specialties in Pilates and yoga with a focus on alignment and embodiment. Kate’s Pilates background was unusual as it followed a multi-lineage price apprenticeship model that included the study of complementary movement methodologies such as the Franklin Method, Feldenkrais, and Gyrotonics®. Building on her Pilates teaching experience, Kate began an in-depth study of yoga, training with renowned teachers of the vinyasa and Iyengar traditions. She held a private practice teaching
Did you know that the Pelvic Rehabilitation Practitioner Certification (PRPC) is celebrating its 10th anniversary? That's right, the first PRPC examination was administered in 2014 and since then, over 700 practitioners from all over the world have earned their certification.
Are you ready to join the ranks of these proficient professionals? Becoming PRPC certified allows you to proudly display the designation "PRPC" after your name, establishing you as an expert in pelvic rehabilitation.
Not sure if you qualify to sit for the PRPC examination? Don't worry, here are some frequently asked questions that may help clarify your eligibility.
What is the PRPC?
The certification available through the Institute is called the Pelvic Rehabilitation Practitioner Certification (PRPC). Earning the PRPC Certification is a professional achievement that demonstrates your dedication and expertise in the field. Through a specialized exam, you'll validate your knowledge and join an exclusive community of respected practitioners.
The PRPC was the first-ever certification exam for therapists seeking distinction for treating pelvic dysfunction in all genders throughout the life cycle.
Who can sit for the exam? Do I have to be a physical therapist?
While a license to practice skills in pelvic rehabilitation is required for the PRPC exam, you don't have to be a physical therapist to apply. In fact, HW welcomes a diverse group of professionals including Physical Therapists (PTs), Physical Therapist Assistants (PTAs), Physicians (MDs), Registered Nurses (RNs), Occupational Therapists (OTs), Occupational Therapist Assistants (OTAs), Doctors of Osteopathic Medicine (DOs), Doctors of Chiropractic Medicine (DCs), Advanced Registered Nurse Practitioners (ARNPs), Nurse Midwives (CNMs), Doctors of Naturopathic Medicine (NDs), and Physician Assistants (PA-Cs) with an active state-board license.
Do I have to take certain Herman & Wallace courses?
There are no course prerequisites for taking the PRPC exam. A valid certification exam tests demonstrable knowledge and skills, which can be gained from a combination of coursework, clinical experience, professional mentorship, etc.
Therapists considering applying should have a comprehensive skill set, which is often gained through several beginner, intermediate, and advanced courses in pelvic function and dysfunction. These can include the Pelvic Function Series, from Level 1 to Capstone, as well as specialized courses for bowel, bladder, sexual, and pelvic pain dysfunctions, depending on your interests and patient demographics.
Pricing for PRPC is discounted for those who have completed at least one course through Herman & Wallace.
How much pelvic rehabilitation experience do I need?
To be eligible to sit for the exam, all applicants must have completed a minimum of 2000 hours of direct pelvic patient care within the past 8 years, with at least 500 of those hours completed in the last 2 years. It's important to note that these patient care hours must come from a licensed clinician and cannot include any hours spent before becoming licensed.
A general guideline for what qualifies as direct pelvic patient care is any time spent directly impacting the care of a specific patient. These activities include (but are not limited to) examination, evaluation, diagnoses, treatment plans, and intervention for conditions related in whole or in part, to the health and function of pelvic structures and the pelvic floor. This includes seeing patients for pelvic pain, pelvic girdle dysfunction, and conditions of bowel, bladder, and sexual dysfunction and includes the care for pediatric, adolescent, adult, and aged patients of any gender.
Where can I find more information?
All the details of the PRPC can be found on our website through the Certification Tab. You can find sample questions, pricing information, and even some study resources!
Are you ready to take your clinical practice to the next level?
Don’t miss this opportunity to become PRPC Certified! Remember - this is the only certification that encompasses pelvic rehabilitation for ALL people across the lifespan. The next testing administration is November 1-15, 2024. The registration cut-off date is October 1st, and the sooner you get your application approved, the faster you can be connected to like-minded practitioners who want to study with you for the exam!
While the exam itself may not be "fun" (let's be honest), the studying process is where you truly elevate your expertise. Immerse yourself in a wealth of knowledge, expand your skills, and refine your techniques - all while preparing for the exam. Good luck on your journey to becoming a certified expert in pelvic rehabilitation!
A testimonial from Erika Darbro, PT, DPT, PRPC
"As a perpetual learner, I recognize the importance of staying up to date with the latest advancements in the field. Each year, I actively participate in numerous continuing education courses, a practice that reflects my dedication to providing the highest quality of care. It was a natural next step to take my commitment a step further by pursuing the Pelvic Rehabilitation Practitioner Certification (PRPC) in 2020.
"Choosing to become certified was not a decision made lightly. The PRPC certification stood out as the perfect fit for my clinical ethos – to treat all genders. Unlike some certifications that focus solely on women's health, the PRPC encompasses pelvic health topics for all populations. This alignment with my values was a driving force behind my choice, emphasizing my dedication to being an inclusive pelvic health practitioner.
"Obtaining the PRPC certification was not just about acquiring a credential; it was a statement of my commitment to being an expert in the pelvic health field. It serves as a recognition of my passion for treating the pelvic health population and reinforces the idea that I don't merely dabble in pelvic health.
"The pursuit of certification was also a personal challenge. It pushed me to elevate my skills, deepen my knowledge, and continually evolve as a practitioner. By challenging myself, I hope to inspire other healthcare professionals to embrace continuous learning and strive for excellence in their field."
Cancer and oncology treatments have several common side effects like fatigue, changes in appetite, and pain. However, patients who have bladder or gynecological cancers can also experience side effects that affect the bladder, bowel, and sexual functioning. The pelvic floor muscles of these patients can be negatively impacted by many things including surgery, radiation, and in some cases, the tumor itself. Pelvic rehab programs can play a crucial role in improving pelvic floor function and overall quality of life for patients who have been diagnosed or treated for these cancers. Don't underestimate the impact of pelvic rehab on regaining both the quality and satisfaction of life after treatment.
Radiation for gynecological cancers, for instance, has been reported to cause vaginal stenosis resulting in generalized pelvic pain and dyspareunia.1 Surgical options including tumor debulking, hysterectomy, and salpingo-oophorectomy can result in scar tissue that can cause tissues or muscles to shift. As pelvic rehab professionals, it is our privilege to offer an evidence-based and solution-focused approach for the often overlooked pelvic health issues faced by people undergoing treatment for pelvic cancers. Our role is crucial in providing much-needed support and care for these patients.
Pelvic rehab therapy can improve and sometimes even prevent the detrimental impacts on the pelvic and abdominal area that negatively impact the patient’s quality of life. Some of the most common therapy options to help improve your patient's pelvic functioning are:
- Soft tissue mobilization and stretching of tight muscles.
- Exercises to strengthen the core and pelvic floor muscles.
- Recommending dietary changes such as avoiding alcohol or caffeinated beverages and other dietary irritants.
- Relaxation and deep breathing to relax the muscles.
- Postural corrections.
- Biofeedback techniques.
- Vaginal dilators or anal dilators for pain during intercourse.
As Michelle Lyons shared in a past blog with the Pelvic Rehab Report, “Whether it is advice on managing anal fissures (skin protection, down-training overactive pelvic floor muscles, achieving good stool consistency, teaching defecatory techniques) or dealing with dyspareunia (dilator or vibrator selection, choosing and using an appropriate lubricant, dealing with the ergonomic or orthopedic challenges that can be a barrier to returning to sexual function and enjoyment), pelvic rehab practitioners are probably the best clinicians for optimizing a return to both pelvic and global health during and after treatment for pelvic cancers.”2
If you work with patients facing pelvic or abdominal issues from a cancer diagnosis or treatment regime, join Herman & Wallace in Oncology of the Pelvic Floor Level 2B scheduled for May 4-5, 2024. This course covers topics on bladder and gynecological cancers including diagnoses, medical treatments, and ways a pelvic rehab professional can help these patients recover. Learn how to help your patients, not just survive, but thrive after treatment. Pelvic therapy interventions from urinary continence to sexual function can offer valuable tools for your patient's long-term well-being.
Resources:
- Damast S, Jeffery DD, Son CH, Hasan Y, Carter J, Lindau ST, Jhingran A. Literature Review of Vaginal Stenosis and Dilator Use in Radiation Oncology. Pract Radiat Oncol. 2019 Nov;9(6):479-491. doi: 10.1016/j.prro.2019.07.001. Epub 2019 Jul 11. PMID: 31302301; PMCID: PMC7944435. https://pubmed.ncbi.nlm.nih.gov/31302301/
- Lyons, Michelle. “Rehabilitating Pelvic Floor Muscles after Cancer Treatment.” The Pelvic Rehab Report, Herman & Wallace. February 13, 2017. https://hermanwallace.com/blog/rehabilitating-pelvic-floor-muscles-after-cancer-treatment.
This article has been reviewed for accuracy by Allison Ariail.
So often as “pelvic floor therapists”, our name and scope of manual treatment can seem to center around stretching or strengthening pelvic floor muscles. But, if you have been practicing for a while, maybe you want to go deeper.
We talk in the Pelvic Function Series about “zooming out” (considering postural, musculoskeletal, breathing, autonomics, and pressure systems). We also have noticed in our field an increased emphasis on the nervous system for regulating the system.
We also talk about “zooming in”, bringing our focus inside the pelvis. That could be pelvic floor muscles, but if we want to zoom in even deeper, we may start to look at peripheral nerves, supportive ligaments, and the interplay between bones, ligaments, fascia, and muscles that could be keeping pain, dysfunction, over-activity, or tension syndromes alive.
The sacrospinous and sacrotuberous ligaments are incredible structures we often don’t give enough attention to. Both the SS and ST ligaments have coccyx attachments and can affect coccyx pain, position, and create tension in the coccygeal nerves.
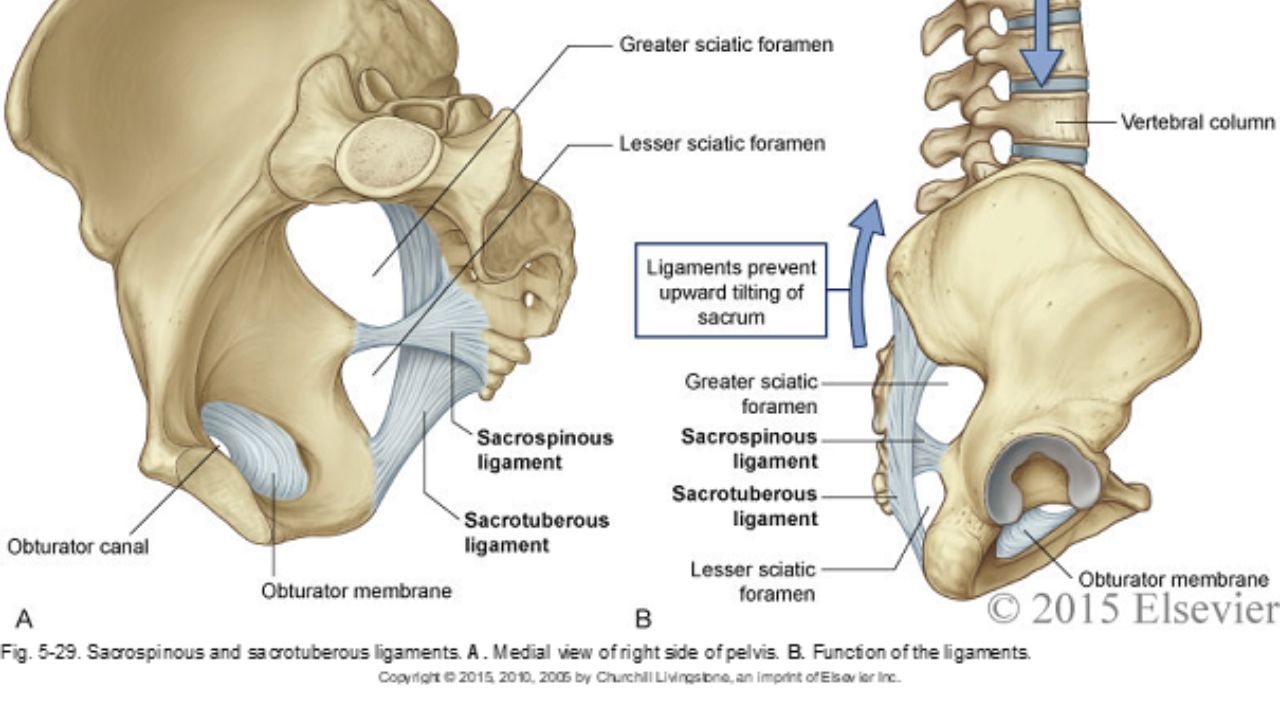
The entire support and structure of the posterior-lateral pelvic bowl is constructed from these two ligaments (with the posterior longitudinal SI ligament). They can become tight and rigid from bearing the burden of stabilizing. The SS ligament may even hold the support for the vaginal canal after hysterectomy. These two ligaments create the greater and lesser sciatic foramen and the nerves of the sacral plexus (pudendal, sciatic, gluteal nerves, and posterior femoral cutaneous nerves) all have intimate relationships and are affected by the tension in these ligaments.
In the Sacral Nerve Manual Assessment and Treatment Class, we learn techniques to deeply release these ligaments (without stressing our hands), external fascial techniques for the coccyx fascia and ligaments, releases for the deep hip muscles that these nerves run through, and how to individually do neuro-lymphatic work to decrease perineural thickening and swelling within the nerve that prevents pain-free gliding. We use differential diagnosis, manual technique, home program, and intricate anatomy study to learn how to get closer to the root of dysfunction in the pelvic floor and posterior gluteals, saddle region, and leg. Come join us on May 11&12 to add depth to your toolbox and understanding of the anatomy of the pelvic nerves.
*Images used with permission from Elsevier 2015.
AUTHOR BIO:
Nari Clemons, PT, PRPC

Nari Clemons was born and raised in the Midwest before moving to Portland, Oregon. At Herman & Wallace, Nari teaches the Pelvic Function Series (PF1, 2A, 2B, and PF Capstone). She was one of three co-authors. Her passion is taking difficult concepts and techniques and simplifying them so that participants can leave courses with confidence, enthusiasm, and feeling empowered in their clinical practice.
Nari graduated from the Medical College of Ohio in consortium with the University of Toledo, with a degree in physical therapy. She owns a private practice, Portland Pelvic Therapy, where she focuses on pelvic, abdominal, and neural issues. Nari has studied visceral and neural manipulation extensively, traveling as far as France to take courses from Jean Pierre Barral. She is also a registered yoga teacher, having trained at the Yoga Center of Seattle and It’s Yoga. Additionally, she has accumulated months of time at intensive meditation retreats. Nari’s approach to the body is holistic and eclectic while being well-rooted in research.

Over the last five years, there has been a groundswell in the recognition that healthcare for those in the LGBTQ+ community has been, at best, incredibly lacking & the world of physical therapy is no exception. Fortunately, this growing awareness is being followed by tangible efforts to improve the quality of care provided to this population as evidenced by the formation of PT Proud, a Catalyst Group in the APTA, & a growing body of research to address the unique needs of LGBTQ+ patients. Hermann & Wallace is even offering its first-ever 2-day course solely focused on treating patients who are gender diverse!
However, it is not uncommon for people to feel overwhelmed by all of the changing terminology & fear of accidentally offending someone. Thus, despite good intentions, many providers find themselves avoiding education & discussion of this topic altogether. The problem with this is that every clinician will inevitably encounter someone who is LGBTQ+ & merely “treating everyone the same '' may inadvertently end up causing harm. This is especially pertinent to pelvic health practitioners as we work on highly personal & vulnerable areas of the body. There are countless reasons why it is a worthwhile endeavor to share your knowledge on this topic which is discussed more thoroughly in a blog post I wrote a few years ago (here), but this post will focus more on practical takeaways that you can implement in your practice.
As mentioned earlier, the terminology can be intimidating; let's break them below into two categories: gender and sexual minorities:
- Sex - biological characteristics of chromosomes & anatomy (ie. male, female, intersex)
- Gender - societal & cultural catego
- rization based on one’s sex (ie. man, woman, non-binary)
- Cisgender - one who identifies with the gender assigned to them at birth
- Intersex- someone born with aspects of both male & female anatomy (i.e. external vulva & internal testes)
- Transgender - one whose gender does not match the sex they were born with (maybe abbreviated trans; this includes people who are non-binary)
- AFAB- assigned female at birth
- AMAB- assigned male at birth
- Transwoman/MTF - assigned male at birth & identifies female
- Transman/FTM - assigned female at birth & identifies male
- Non-binary- one who identifies as neither male nor female; may use gender-neutral pronouns (they/them)
- Top surgery - breast removal (typically FTM) or augmentation (typically MTF)*
- Bottom surgery - reassigning one’s genitalia to the anatomy they identify with
- Gender identity - the gender that someone associates with internally
- Gender expression - the external gender that someone conveys through appearance & behavior
- *Non-binary folks may also undergo various gender affirmation surgeries & /or take hormones.
- Sexual orientation - the gender(s) that one is attracted to. (Transgender is not a sexual orientation.)
- Lesbian- a woman attracted to other women
- Gay- a man attracted to other men
- Bisexual- a person attracted to both men and women
- Pansexual- someone attracted to people regardless of their gender identity
- Asexual- a person who is not sexually attracted to others; may still experience romantic attraction
- Queer- an umbrella term that applies to all LGBTQ+ people; used as a sexual orientation when other labels are not accurate; may be perceived as a derogatory slur, especially among older individuals
There can be many combinations of the terms above. Someone could identify internally as male but live outwardly as a woman for a variety of reasons including safety, cost of transition, etc. Also, gender & sexual orientation do not always pair up in a heteronormative fashion. A person could be cisgender & bisexual (a woman AFAB attracted to both men & women) or transgender & lesbian (a transwoman AMAB attracted to women). Furthermore, not all people who are transgender have surgery or undergo hormone therapy, but this does not change their gender identity. Some helpful visuals to understand these ideas are the Gender Unicorn (here) & the Genderbread Person (here).
Now that you have some context to work with, what else can you do to put patients at ease?
- Consider having a rainbow flag in the waiting room to let patients know they are in a safe space
- Wear a small pin indicating that you are an ally.
- Have inclusive intake forms with a blank space to enter gender rather than a checkbox for male or female.
- If applicable, know where gender-neutral bathrooms are located & inform patients.
Ultimately, the best method to provide compassionate and competent care is to minimize your assumptions. There are many things you can do in your day-to-day interactions with patients to convey that you are trying to open up your worldview. For example, if you find yourself assuming someone’s gender identity based on their name or appearance, I’d challenge you to practice using the gender-neutral they/them pronoun until you learn how they identify. If you are unsure, it is okay to privately ask them! This is far less triggering than misgendering someone. Another common microaggression is assuming a patient’s partner’s gender based on heteronormative values. Try using the terms “spouse” or “partner” when talking to a patient about their loved one(s). It may seem banal to you, but your LGBTQ+ patients will notice.
Disclaimer: I can only represent the part of the community that I identify with. The views expressed are my informed opinions & may not be generalizable to all LGBTQ+ persons. I am thankful to be given a platform to address a topic that is so rarely discussed, but if I have made any errors or misrepresentations, please correct me!
My course will provide a safe space to ask all the questions about caring for LGBTQ+ patients and practicing the skills needed to help advance your practice. Join me for Inclusive Care for Gender and Sexual Minorities next scheduled for June 8th.
AUTHOR BIO:
Brianna Durand, PT, DPT
 Brianna Durand, PT, DPT earned her Doctor of Physical Therapy at Texas Woman’s University in Houston, TX. During graduate school, she led and co-founded PT Proud, a Catalyst Group within the Health Policy and Administration Section of the APTA, to improve the education, equity, and inclusion of LGBTQ+ patients, students, and clinicians.
Brianna Durand, PT, DPT earned her Doctor of Physical Therapy at Texas Woman’s University in Houston, TX. During graduate school, she led and co-founded PT Proud, a Catalyst Group within the Health Policy and Administration Section of the APTA, to improve the education, equity, and inclusion of LGBTQ+ patients, students, and clinicians.
Brianna owns and operates Empower Physiotherapy, a private practice in Seattle. As a competitive powerlifter, Brianna enjoys working with strength athletes who experience pelvic floor dysfunction, especially stress incontinence. She is passionate about providing care to individuals in the LGBTQ+ community, including those undergoing hormonal/surgical transition. Additional clinical interests of hers include prenatal/postpartum care for trans and gender-nonconforming folx and pelvic floor care for patients that are intersex. In her spare time, Brianna enjoys playing board games, lifting heavy, and watching stand-up comedy.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/









































