Surface EMG is the only modality that can isolate the active component of tone and is, therefore, a very valuable tool in the assessment of patients with altered tone conditions. However, it is the most misunderstood modality in pelvic health therapy. Rarely do practitioners see a topic so argued in pelvic rehabilitation as surface EMG biofeedback. Some practitioners boldly state they are for or against it on their social media accounts and clinic pages. Therapists are not questioning the use of biofeedback with neurologic or orthopedic applications, so why is it such a polarizing topic in pelvic health? The Pelvic Rehab Report sits down with faculty members Tiffany Lee and Jane Kaufman to discuss the tool they love. These two instructors have over 50 years of combined experience using biofeedback and have been teaching biofeedback board certification courses together for the past 16 years.
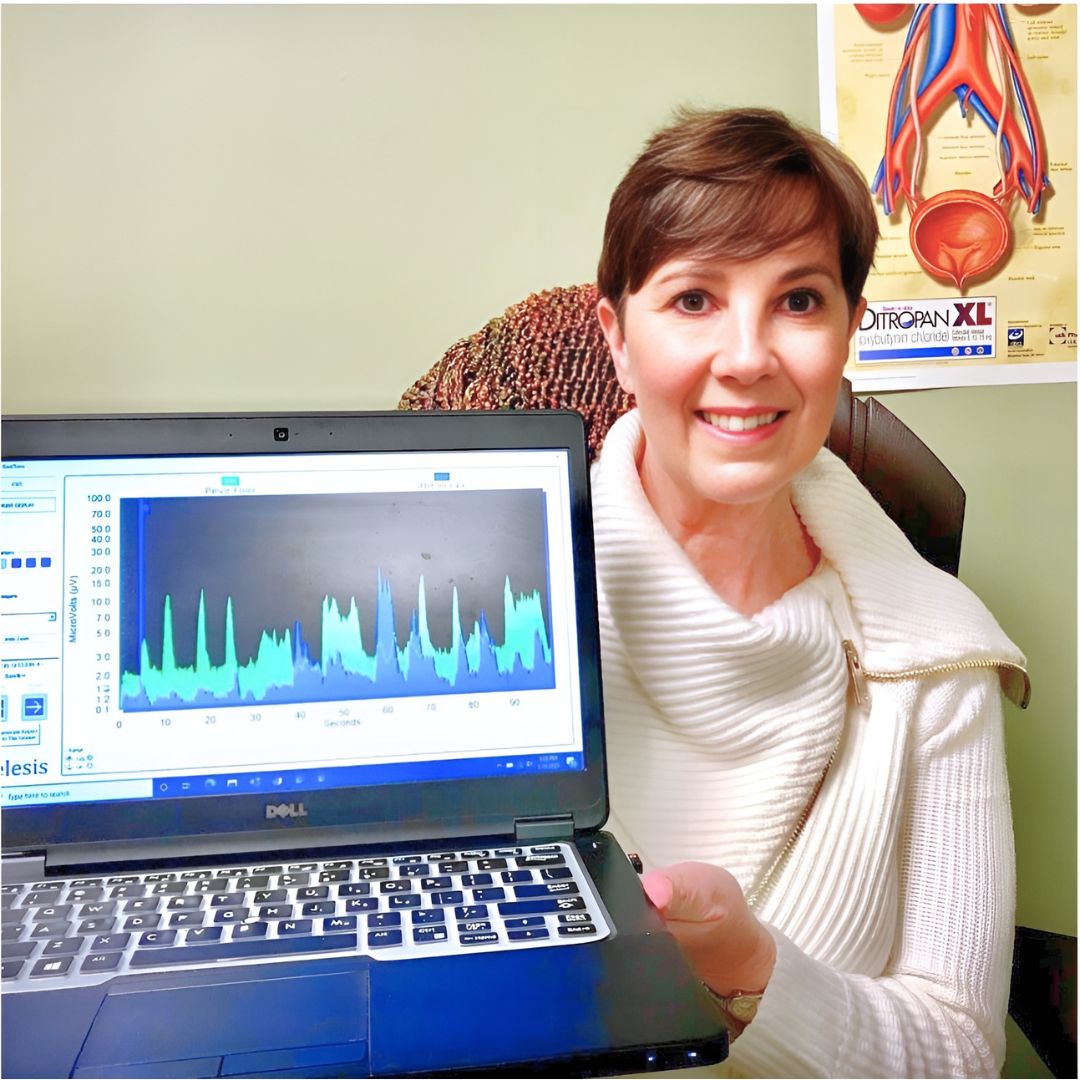
Biofeedback provides visual and auditory feedback of muscle activity and is a non-invasive technique that allows patients to adjust muscle function, strength, and behaviors to improve pelvic floor function. The small electrical signal (EMG) provides information about an unconscious process and is presented visually on a computer screen, giving the patient immediate knowledge of muscle function and enabling the patient to learn how to alter the physiological process through verbal and visual cues. Jane Kaufman explains “Many patients gain knowledge and awareness of the pelvic floor muscle through tactile feedback, but the visual representation helps patients hone in on body awareness and connect all the dots." Muscle evaluation through digital exam offers strength but does not appropriately address electrical activity such as resting tone and the ability to recruit or release tone in the muscle. The use of biofeedback addresses the specificity of muscle contraction and release, offering an additional view of muscle function.
In a 2020 research study by Pilkar et al., clinicians reported sEMG barriers of use, which included limited time and resources, clinically inapplicable sEMG system features, and the majority of clinicians' lack of training and/or confidence in the utilization of sEMG technology. This research also noted technical challenges, including the limited transfer of ever-evolving sEMG research into off-the-shelf EMG systems, nonuser-friendly intuitive interfaces, and the need for a multidisciplinary approach to accurately handling and interpreting data.
One barrier may be the price of a biofeedback unit. Tiffany Lee recommends using a 2-channel sEMG biofeedback hand-held unit with the software on a laptop or computer. In fact, to become board-certified in pelvic floor biofeedback, the Biofeedback Certification International Alliance (BCIA) requires a 2-channel EMG system with software. If you use a hand-held one-channel unit, the patient will have difficulty seeing the muscle activity and the coordination between the abdominals and pelvic floor. This prevents meaningful treatment as the patient cannot understand or interpret the LED bars on the machine (and often, the therapist cannot understand either). In truth, the benefits outweigh the cost of the equipment. You can cover the unit's cost and software to visualize muscle function and tone within a few treatments. Training is another issue; you need proper training in the modality to start utilizing biofeedback in your clinical setting. Most therapists have never been adequately trained. If they take a course where the instructor doesn’t believe in the benefits of biofeedback, they feel negatively toward a modality they have never personally explored. Biofeedback relies on a skilled clinician to interact with the patient, give verbal cues, ensure that the proper muscles are contracting and relaxing, and must be used in conjunction with their other skills and knowledge.
Think of sEMG biofeedback as one tool in your toolbox. Tiffany shares, "In a study by Aysun Ozlu MD et al., the authors conclude that biofeedback-assisted pelvic floor muscle training, in addition to a home exercise program, improves stress urinary incontinence rates more than a home exercise program alone." She continues, "Biofeedback is a powerful tool that can benefit your patient population and add to your skill set.
The acceptance of sEMG biofeedback in rehabilitation requires a unit (with software and sensors), training, and a multidisciplinary approach. Used correctly, it can positively impact patient performance and care in the clinic. Keep in mind that sEMG is a non-invasive technique. It has already shown great promise in neurorehabilitation and has been a widely utilized tool to assess neuromuscular outcomes in research. Jane Kaufman concludes, "Biofeedback treatment/training using the proper instrumentation provides the precise information necessary to change behaviors." This allows the patient to recognize that ‘yes, they are in charge of this muscle and that they can achieve success in overpowering the symptoms.’ Biofeedback routinely allows patients to understand that they are empowered to heal themselves with the tools you offer. They are in charge of their bodies and the outcome of treatment. It is also an important tool to use with patients who have experienced trauma and who are not ready to participate in manual therapy, and it is valuable for the pediatric population as well. Tiffany adds, “This modality can bring new business to your clinic. My local GI and colorectal providers often refer up to 5 new patients a week to my practice.
There is a long history of scientific evidence supporting the use of sEMG biofeedback in managing incontinence or pain symptoms. As a noninvasive, cost-effective, and powerful treatment modality, healthcare providers should consider this tool when managing pelvic floor dysfunction patients. Providers should be educated in the proper use of this valuable modality to gain the most out of the skills and knowledge that can be achieved through this intervention. For more information regarding courses and certification, please visit www.pelvicfloorbiofeedback.com.
Tiffany asked several PTs and OTs who have been to the board certification courses what they love about biofeedback. Here are a few answers
- “Biofeedback empowers my patients and gives them the confidence that they are actually doing their exercises and relaxing correctly! I’ve had nothing but positive feedback from patients, and it’s such a great tool to have as a pelvic floor therapist.”
- “My patients really love it, and they ask for it. I especially see the value for dyssynergia work on bearing down and learning eccentric abdominals and relaxed pelvic floor muscles. For men, I work on relaxing in standing and toileting postures if they can’t empty their bladder.”
- “Ultimately, the treatment needs to be meaningful to the patient. Biofeedback can complement other treatments. Their needs come before ours. We should offer all of our patients the ability to control their own muscles and SEE how to do it.”
- “After ONE session with a 5-year-old with constipation, mom called me in sheer excitement, screaming over the phone that he pooped on the potty!!! Something he has NEVER done before. Biofeedback helped him find and coordinate the potty muscles and tummy muscles, and this made a huge difference for him!”
- “Becoming certified in biofeedback has only been positive for me. My patients feel that the initial sEMG evaluation sets the stage for my care plan, and my discharge reassessment is a tangible reflection of their progress. Not to mention its strength as a marketing tool.”
Jane Kaufman adds “Biofeedback in treatment has been a game changer. Using this tool as a foundation for treatment in my clinic allowed my practice to grow, thrive, and achieve great acclaim in our region and beyond. It is not unusual for patients to travel several hours to seek treatment because of the empowering effect the biofeedback visual had on their understanding of their dysfunction.”
Biofeedback for Pelvic Floor Muscle Dysfunction is scheduled for July 28th and December 7th, 2024, and provides a safe space for clinicians to learn and practice this valuable tool. Registrants will need equipment to participate in this online course and will learn about the benefits of using this modality in their clinical practice.
In this course, Tiffany and Jane guide participants through learning to administer biofeedback assessments, analyze and interpret sEMG signals, conduct treatment sessions, and role-play patient instruction/education for each diagnosis presented during the many hands-on lab experiences.
References:
- Use of Surface EMG in Clinical Rehabilitation of Individuals With SCI: Barriers and Future Considerations Rakesh Pilkar, Kamyar Momeni, Arvind Ramanujam, Manikandan Ravi, Erica Garbarini, Gail F. Forrest. Front Neurol. 2020; 11: 578559. Published online 2020 Dec 18. doi: 10.3389/fneur.2020.578559 PMCID: PMC7780850
- Comparison of the efficacy of perineal and intravaginal biofeedback-assisted pelvic floor muscle exercises in women with urodynamic stress urinary incontinence. Aysun Ozlu MD, Neemettin Yildiz MD, Ozer Oztekin MD. Neurourol Urodyn. 2017 Nov;36(8):2132-2141. Epub 2017 Mar 27. doi: 10.1002/nau.23257 PMID: 28345778.
- Cram, J. R., & Kasman, G. S. (2011). The basics of surface electromyography. In E. Criswell (Ed.). Cram’s introduction to surface electromyography (2nd ed., pp. 3–7.) Jones and Bartlett.
- Kaufman, J., Stanton, K., & Lee, T. E. (2021). Pelvic Floor Biofeedback for the Treatment of Urinary Incontinence and Fecal Incontinence. Biofeedback, 49(3), 71-76.
- Shelly, Beth & Kaufman, Jane (2023). Foundations of Pelvic Floor Muscle Assessment Using Surface Electromyography. APTA Academy of Pelvic Health Physical Therapy.
AUTHOR BIOS
Tiffany Lee, OTR, OTD, MA, BCB-PMD, PRPC

Tiffany Lee holds a BS in OT from UTMB Galveston (1996), an MA in Health Services Management, and a post-professional OTD from Texas Tech University Health Sciences Center. In 2004, she received her board certification in Pelvic Muscle Dysfunction from the Biofeedback Certification International Alliance. She is a Herman & Wallace Pelvic Rehab Institute faculty member and teaches biofeedback courses. She has been treating pelvic health patients for 25 out of her 30-year career. Her private practice in San Marcos, Texas, is exclusively dedicated to treating urinary and fecal incontinence and pelvic floor disorders. Her continuing education company, Biofeedback Training & Incontinence Solutions, offers clinical consultation and training workshops. She also enjoys mentoring healthcare professionals working toward their BCIA certification.
Jane Kaufman, PT, M.Ed, BCB-PMD
Jane has been practicing PT for more than fifty years. She is a graduate of the Ithaca College Physical Therapy program and earned her master’s degree at the University of Vermont. In her early career, she practiced in outpatient settings, skilled nursing, and acute rehabilitation. Jane’s career began at Columbia Presbyterian Medical Center and progressed to the University of Vermont Health Network where she supervised the Department of Physical Therapy’s outpatient services. In the late 1990s, Jane became intrigued with pelvic floor muscle dysfunction, evolving to a quarter-century career in this highly specialized field.
In 2001 she began her career as a sole practitioner in pelvic floor muscle dysfunction and in 2003 established Phoenix Physical Therapy, PLC with a staff of clinicians specializing in the treatment of pelvic floor dysfunction, incontinence, and pelvic pain for all genders and all ages. In 2005, Jane became certified in the use of surface EMG biofeedback for pelvic floor muscle dysfunction (BCB-PMD ) from the Biofeedback Certification International Alliance. She sold her practice in 2022, having established a renowned reputation in Vermont, upstate New York, regionally, nationally, and internationally. Post Phoenix, Jane continues to offer workshops for other healthcare providers in the use of biofeedback for pelvic muscle dysfunction, and mentors healthcare professionals around the world toward certification in this field through the Biofeedback Certification International Alliance. Jane teams with Tiffany Lee, OTR, OTD through Biofeedback Training and Incontinence Solutions (www.pelvicfloorbiofeedback.com).
Jane has recently begun a consulting practice helping adults with pelvic floor muscle dysfunction issues and has continued helping children/teens through her new practice, PottyTime Physical Therapy (www.pottytimephysicaltherapy.com). In addition to her practice and teaching, Jane has participated in research through the University of Vermont Health Network on pelvic organ prolapse, incontinence, and sexual dysfunction. She has authored an article published in the online international journal Biofeedback and was a co-author in the APTA self-study manual for Foundations in Pelvic Floor Muscle Assessment using Surface Electromyography with Dr. Beth Shelley, PT, DPT, WCS, BCB-PMD. She is a Herman & Wallace Pelvic Rehabilitation Institute faculty member and teaches biofeedback courses through this company. Jane may be reached by email at: jkaufmanpt@comcast.net

Did you know that chronic pain affects an estimated 51.6 million adults in the United States alone? That's almost 21% of the population (1). It's a debilitating condition that can disrupt daily life and limit one's ability to function. But what about those with hypermobility? Often individuals with hypermobility are even more susceptible to chronic pain and their treatment may require a unique approach.
There are many variables that make a person more susceptible to developing chronic pain. Some of these include genetics, prior trauma, culture, and health history. Patients with hypermobility are more likely to develop chronic pain and may also need to be treated with a different lens than the rest of the population.
What is Hypermobility
Hypermobility spectrum disorder (HSD) includes joint hypermobility syndrome (JHS) as one of its conditions and is a connective tissue disorder characterized by chronic musculoskeletal pain due to joint hyperextensibility and is a common cause of chronic pain, fatigue, headaches, anxiety, orthostasis, and abdominal pain. Hypermobility spectrum disorder (HSD) is sometimes considered a milder variant of hypermobile EDS (hEDS) and is seen in up to 3% of the general population, with a prevalence rivaling fibromyalgia, gout, and rheumatoid arthritis (2).
Joint hypermobility implies a range of motion of a joint that exceeds the documented “norm.” Norms for each joint are determined by the specific joint anatomy, the person’s age, sex, and ethnicity. Hypermobility is typically scored using the Beighton scale requiring at least a 5 to be classified as systemically hypermobile. The Beighton score is determined by 9 points awarded for each described condition met. The conditions include (3,4):
- Elbow hyperextension of at least 10 degrees (one for each elbow)
- Knee hyperextension of at least 10 degrees (one for each knee)
- Ability to passively extend the pinky finger to 90 degrees or more (one for each hand)
- Ability to touch the thumb to the forearm with wrist flexion (one for each hand)
- Ability to forward flex the trunk at the hips and place both palms on the floor with knees extended.

Hypermobility as a problematic condition occurs on a spectrum and ranges from Hypermobility Spectrum Disorder (HSD) to genetic connective tissue disorders such as hypermobile EDS (hEDS). Patients with connective tissue disorders often have other symptoms associated with the syndrome such as fragile blood vessels or cardiac arrhythmias (3). Those with generalized joint hypermobility are less likely to have other associated comorbidities.
Hypermobility and Rehab
A patient with hypermobility must have their hypermobility considered in their treatment plan as their tissues, and force tolerance of tissues, differ from the rest of the population. Patients with hypermobility may present with decreased strength overall and require more strength than typical to perform activities. This is likely due to the extensibility of the tendons and ligaments, changing the force a muscle can produce. Patients with hypermobility also often have decreased proprioception, as their tissue laxity cannot provide as much awareness to the brain. These variables can lead to a higher incidence of injury, with dislocation common for those with hEDS (4).
Hypermobility is also correlated with pelvic pain and dysfunction, especially in female patients. They are more prone to pelvic organ prolapse but also may present with pelvic floor muscle overactivity (3) creating a difficult case to treat, especially if they have chronic pain in addition. This patient will often benefit from rehabilitation to address the prolapse, muscle overactivity, and then coordination of core and pelvic stabilizers. Knowing that the patient has hypermobility can be vital to the successful treatment plan for this presentation. When treating patients with hypermobility, they often have decreased functional tolerances for loading, not only at the joints but also systemically. hEDS especially, is highly associated with autonomic dysfunction such as postural orthostatic tachycardia syndrome (POTS), which may affect your treatment plan as well. A portable pulse oximeter and slow positional changes may be helpful in decreasing and monitoring symptoms (3,4).
 Pain Patterns and Hypermobility (3)
Pain Patterns and Hypermobility (3)
Pain patterns for the hypermobile patient include all 3 subtypes of pain.
- Nociceptive Acute Pain
- Neuropathic Pain
- Nociplastic Pain
Nociceptive acute pain will occur at localized injury sites with frequent dislocations, strains, and sprains. These recurrent injuries can then lead to chronic musculoskeletal changes of the joint that affect function and gait.
Neuropathic pain can also become problematic for this population. Due to the increased laxity of their vertebrae, they may suffer from higher incidences of spinal cord compression and peripheral nerve compression. It is also becoming more common to evaluate this population with a dermal biopsy for small fiber neuropathy. As the patient experiences continued nociceptive and neuropathic pain inputs over and over, their nervous system may also sensitize causing both peripheral and central sensitization with nociplastic pain.
Nociplastic pain may then transform into widespread generalized pain. As their pain patterns progress, they may start to experience more fear avoidance behaviors and may become deconditioned. Deconditioning in turn can lead to more injuries and continues a recurrent cycle for these patients.
Conclusion
Knowing that patients with hypermobility are more susceptible to chronic pain allows us to treat this population more effectively. As rehab practitioners, we can educate the patient, improve strength, improve stability, improve proprioception, and work to desensitize the nervous system. A sensitive nervous system may be the initial hurdle with the hypermobile patient.
Pain neuroscience education is the first step to educate the patient on how their nervous system functions and to decrease fear they may have around pain. After education, there are several physical interventions we can use for the nervous system including dry needling, spinal mobilization, manual therapy, and exercise.
Ready to Learn More?
Expand your knowledge, experience, and treatment in understanding and applying pain science to the chronic pelvic pain population with Alyson Lowrey and Tara Sullivan in their upcoming course Pain Science for the Chronic Pelvic Pain Population on August 17-18, 2024.
This course is not specific to the patient who is hypermobile. However, there are portions of the course that address this population. This course provides a thorough introduction to pain science concepts including classifications of pain mechanisms, peripheral pain generators, peripheral sensitization, and central sensitization in listed chronic pelvic pain conditions; as well as treatment strategies including therapeutic pain neuroscience education, therapeutic alliance, and the current rehab interventions' influence on central sensitization.
Pain Science for the Chronic Pelvic Pain Population is a remote course that will provide you with the understanding and tools needed to identify and treat patients with chronic pelvic pain from a pain science perspective. Lecture topics include the history of pain, pain physiology, central and peripheral sensitization, sensitization in chronic pelvic pain conditions, therapeutic alliance, pain science and trauma-informed care, therapeutic pain neuroscience education, the influence of rehab interventions on the CNS, and specific case examples for sensitization in CPP.
References:
- Rikard, S. Michaela, et al. “Chronic pain among adults — United States, 2019–2021.” Morbidity and Mortality Weekly Report, vol. 72, no. 15, 14 Apr. 2023, pp. 379–385, DOI: https://doi.org/10.15585/mmwr.mm7215a1.
- Kumar, Bharat, and Petar Lenert. “Joint hypermobility syndrome: Recognizing a commonly overlooked cause of chronic pain.” The American Journal of Medicine, vol. 130, no. 6, June 2017, pp. 640–647, DOI: https://doi.org/10.1016/j.amjmed.2017.02.013.
- Syx D, De Wandele I, Rombaut L, Malfait F. Hypermobility, the Ehlers-Danlos syndromes and chronic pain. PubMed. 2017;35 Suppl 107(5):116-122.
- Scheper M, De Vries JE, Verbunt J, Engelbert RHH. Chronic pain in hypermobility syndrome and Ehlers-Danlos syndrome (hypermobility type): it is a challenge. Journal of Pain Research. August 1, 2015:591-601
AUTHOR BIO
Alyson Lowrey, PT, DPT, OCS
Dr. Lowrey attended the University of New Mexico where she received a BA degree in Psychology in 2011. She then attended the University of New Mexico School of Medicine to earn her Doctor of Physical Therapy degree in 2014. Following graduation from UNM, Alyson completed the HonorHealth Orthopaedic Residency program in 2015 and became a board-certified orthopedic specialist (OCS) in 2016. She is now the director of that residency program and lectures about pain and pelvic dysfunction in the curriculum. Alyson treats the pelvic floor patient population through an orthopedic approach, working closely with pelvic floor specialists. This allows for a wholistic style addressing the entire patient from a functional perspective. Alyson’s clinical interests include the evaluation and treatment of chronic pain, lumbar and cervical spine disorders, foot and ankle disorders, pelvic pain, and clinical instruction. She is certified in dry needling and an APTA-certified clinical instructor, regularly taking students from several PT schools. She participates in Creighton’s and Midwestern University’s Doctor of Physical Therapy programs as adjunct faculty assisting in lab and lecturing in Biomechanics, Kinesiology, and Musculoskeletal courses. Outside of the clinic, she enjoys being active, doing yoga, crafting, and spending time with her husband and cats.

Most of us spend our day sitting and do not think about the position of our ilia, sacrum, or coccyx during the change from standing to sitting. Weight-bearing through a tripod of bilateral ischial tuberosities and a sacrum that should have normalized form closure should be easy and pain-free.
The coccyx typically has minimal weight bearing in sitting, about 10%, just like the fibula, however, it can be a major pain generator, if the biomechanics of the ilia, sacrum, and femoral head positions are not quite right. A lot of patients will state “My pain is worse with sitting” which can mean thoracic pain, low back/sacral pain, and even lower extremity radicular pain.
Scanning the literature for coccyx treatment does not always yield the best results for physical or occupational therapists. Most literature states what the medical interventions can be, and physical therapy is never at the forefront. However, as we are musculoskeletal and neuromuscular specialists, this is no different in our thinking patterns relating to coccyx pain or painful sitting.
During sitting, the coccyx has normal flexion and extension moments that will change or become dysfunctional once mechanics above and below that joint change. A simple ankle sprain from 2 years ago can result in chronic knee and sacroiliac pain that can lead to coccyx pain over time. Even the patient who has long-standing TMJ (temporomandibular joint) and cervical dysfunction, now has a thoracic rotation and your correction of their coccyx deviation cannot maintain correction.
Coccydynia and Painful Sitting is a course that provides a spark for your orthopedic mindset and encourages clinicians to evaluate the coccyx more holistically.
- What are the joints doing?
- How does it change from sitting to standing?
- Standing to sitting?
- What is the difference from sitting upright to slump activities?
Working through the basics and the obvious with failed results takes you to the next step of critical thinking within this course. How does the patient present? What seems to be lacking and how to correct them biomechanically to achieve pain-free sitting? Related coccyx musculature and nerve dysfunction can seem like the easiest to treat, but what happens when those techniques fail?
In Coccydynia and Painful Sitting, we look at the entire body, from the cranium to the feet, to determine the driver of coccyx pain and dysfunction. A better understanding of ilial motion, with accompanied spring tests (Hesch Method) normalizing spinal mechanics and lower extremity function is highlighted in this course. Internal vaginal and rectal release of pelvic floor muscles can lead to normalized coccyx muscle tension that is supported via coccyx taping.
To learn more, join Lila Abatte in her next Coccydynia remote course scheduled for July 13, 2024.
AUTHOR BIO
Lila Abbate, PT, DPT, OCS, WCS, PRPC

Lila Abbate, PT, DPT, MS, OCS, WCS, PRPC is the Director/Owner of New Dimensions Physical Therapy with locations in Roslyn, Long Island, and the Noho Section of New York City. Dr. Abbate graduated from Touro College in Dix Hills, NY with a Bachelor of Science (BS) in Health Sciences and a Master of Arts (MA) in Physical Therapy in 1997. She completed her Advanced Masters in Manual Orthopedic Physical Therapy (MS) at Touro College, Bayshore, NY in 2003 and continued to pursue her Doctor of Physical Therapy (DPT) at Touro in 2005. Dr. Abbate is a Board-Certified Specialist by the American Physical Therapy Association in Orthopedics (OCS) 2004 and Women’s Health (WCS) 2011. She obtained the Certified Pelvic Rehabilitation Practitioner (PRPC) from the Herman & Wallace Institute in 2014. She is a Diane Lee/LJ Lee, Integrated Systems Model (ISM) graduate and completed the New York series in 2012.
Dr. Abbate has been an educator for most of her physical therapy career. She has experience as a full-time faculty at Touro College, Manhattan Campus from 2002 to 2006 teaching the biomechanical approach to orthopedic dysfunction and therapeutic exercise as well as massage/soft tissue work that highlighted trigger point work, scar management, and myofascial release.
She is currently on faculty as a Lecturer at Columbia University teaching the private practice section Business & Management course (since 2016) along with the Pelvic Health elective (since 2012). She teaches nationally and internationally with the Herman & Wallace Pelvic Rehabilitation Institute teaching advanced courses of her own intellectual property: Orthopedic Assessment for the Pelvic Health Therapist, Bowel Pathology Function, Dysfunction and the Pelvic Floor, Coccydynia & Painful Sitting: Orthopedic Implications. She was a co-writer for the Pudendal Neuralgia course and teaches the Pelvic Function Series and the Pregnancy and Postpartum Rehabilitation courses. She has written two book chapters in 2016: Pelvic Pain Management by Valvoska and Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies by Chughtai.
She is a member of the American Physical Therapy Association, the National Vulvodynia Association, the American Urogynecology Association, and the International Pelvic Pain Society. Dr. Abbate is also a Senior Physical Therapy consultant for SI Bone, a sacroiliac joint instrumentation company.

This specialty kind of fell into my lap after years of “kicking and screaming,” well, not really, just saying no a lot.
In March of 2018, I attended a continuing education course at Springfield College with a student of mine at the time (who had just completed his final clinical affiliation for split outpatient ortho and acute care in a small community hospital in Connecticut) on pelvic floor therapy. Each year I looked at the offerings for clinical instructors and nothing really excited me, but this time was different. When it was time to choose I sat down with my student and asked him what he was going to and we chose to go to the pelvic health course as he was going into outpatient orthopedics and knew he might come in contact with pregnant or postpartum patients that might need the education on pelvic health. I was excited to learn more about the pelvic floor and what that really entailed. Every time this pelvic floor physical therapist spoke about patients and the conditions she treated and how they exuded confidence going on vacation, going to an event, or even being more intimate with their partners I thought “This might be for me.” I was intrigued and excited to learn, for probably the first time, in at least 2 years.
The next day I was approached by my manager about starting a pelvic health program at our local hospital together as a team; and when I say approached, I mean there was a note on my desk that read “Please see me” and she signed her first initial. My first instinct was, “Oh no, what did I do now?” I had been skeptical for approximately 2 years as the topic came up about every other month at our staff meetings, however, without a doubt or skip in my breath I said “Sure, why not?!” At this point, I thought what do I have to lose? I was getting reimbursed to take these continuing education classes, I was getting to travel, and I was learning alongside a colleague. I went home that night and told my parents what I was going to do and they thought I was joking. My friends and boyfriend said, “You’re going to do what?” Within 1 week we were signed up for our first pelvic floor series courses through Herman & Wallace starting with Pelvic Floor 1 (now Pelvic Function 1) in Virginia Beach, VA. I began seeing patients within 3 months of taking PF1 after developing the history sheet and marketing with local OBGYN/midwife offices. Fast forward to August 2018, we took PF2A and in October 2018, I took PF2B, both in Boston, MA.
As a new pelvic floor therapist, the initial diagnoses included urinary dysfunction, prolapse, pelvic pain, and the postpartum population. Over time and taking more courses I began to treat more complex pelvic pain diagnoses. This allowed me to use more of my manual therapy skills and some more medical skills as these types of patients required an in-depth treatment approach. I took Capstone in October 2019 in Houston, TX and then we all know what happened next. After meeting patient after patient who experienced medical gaslighting, experienced pain for decades, and had run out of doctors to see, I decided to take a deeper dive into chronic and complex pelvic pain diagnoses, ie: vaginismus, vulvodynia, vestibulodynia, endometriosis, adenomyosis and so much more. I love treating each and every patient who comes through the door and into my treatment room, however, I hold a special place in my heart for those who have been told that there is no other treatment for them, or they’ve exhausted all of their outcomes. Since 2018, I haven’t met a patient I haven’t been able to help, even a little bit.
Prior to treating any pelvic floor diagnoses, I took 2-3 doctor of physical therapy (DPT) students each year, some of them shared with another acute care PT. I couldn’t fathom not taking students as I was diving into this much-needed area of physical therapy. I took my first pelvic floor-focused student in January 2020. I developed my own system as there wasn’t any standard of practice that I could find amongst other pelvic floor therapists regarding clinical education. I developed a system that taught a very basic PF1 if the student had not taken it yet that included learning the muscles, nerves, basic diagnoses, treatments, and integration into function. In order to teach a student how to do an internal vaginal assessment, I first conduct an internal assessment on the student, and then I have them perform one on me. When I tell other therapists what my structure and strategy are in order to get students ready for seeing their own caseload I always get a look of “Oh really?” and an eyebrow raise. At the end of the day, how do I know they will be competent enough to perform an internal vaginal assessment on a patient if I don’t know if their pressure is adequate or if they are palpating the correct structures?
I was starting to take more courses and follow more and more groups on social media. I always felt like an outlier as I never felt like I had to force a student who was interested in pelvic health to take PF1 unless they knew downright they wanted to go straight into pelvic health prior to starting their affiliation. They signed up for this affiliation and there is an agreement that I guide them and enhance their learning. We practice until they feel confident and competent and then choose a patient who is willing and gives consent to the student performing the internal vaginal assessment, of course with me in the room, until I feel the student is 100% independent. Since 2020 I have taken 6 DPT students who were interested in pelvic health, with another one scheduled for October 2024. I am beyond happy to say that each student has taken a job with a pelvic health focus after completing their clinical affiliation with me so I have to think I’m doing all the right things!
In January 2021, I was approached by the teaching assistant (TA) coordinator for Herman & Wallace as they were in desperate need of a TA in Danbury, CT for PF1 and I thought “What the heck? I do this day in a day out, I’d be a great TA” and jumped on that opportunity. Through my opportunities as a TA, I have been able to learn from so many amazing pelvic floor therapists all over the country, guide new therapists in their pelvic floor journey, and embark on this new journey for myself as a leader in pelvic health. I have been so lucky to have been able to TA so many courses local to my home in Connecticut over the last 3 years, which has allowed me to form professional connections and network with local to CT physical and occupational therapists, as well as the ability take over a dozen additional courses through H&W ranging from Bowel Pathology & Function to Pharmacology for the Pelvic Floor Therapist to Dry Needling without having to pay out of my own pocket. I am halfway into year 4 of my TA journey with H&W, became a lead TA in October 2023, and I truly look forward to each, and every, course I choose to TA. I love this journey I have created for myself and I am so passionate to share it with anyone and everyone willing to listen.
I am proud of the pelvic floor therapist I’ve blossomed into over the last 6 years. I honestly couldn’t have done any of this without the support of my family, boyfriend, friends, and coworkers who have listened to me talk endlessly about all of the different avenues the pelvic floor can be affected and how to begin to address those issues. My story into the pelvic health world is not like anyone else’s and that’s what makes each and every one of our journeys unique!
AUTHOR BIO
Alyssa Itzkowitz, PT, DPT, PCES, PRPC
 Alyssa is always taking new clients at Rockville General Hospital located in Vernon, CT. Ahe treats all genders and ages 15+ (anything younger than that is on a case-by-case basis). Evaluations are 90 minutes and follow-up treatment sessions are based on the needs of the patient and are either 30 or 60 minutes.
Alyssa is always taking new clients at Rockville General Hospital located in Vernon, CT. Ahe treats all genders and ages 15+ (anything younger than that is on a case-by-case basis). Evaluations are 90 minutes and follow-up treatment sessions are based on the needs of the patient and are either 30 or 60 minutes.
You can find our contact information on our hospital website: www.echn.org/services/rehabilitation or email Alyssa to discuss scheduling further: aitzowitz@echn.org.

So many physiological changes occur to the body during pregnancy, it is no wonder that during pregnancy people have back and lower extremity aches and pains. It is common to experience hormonal changes, weight gain, and reduced abdominal strength during this time, not to mention the anterior shift in their center of mass.
These physiological changes result in altered spinal and pelvic alignment, and increased joint laxity. Also, many individuals report increases in size of their feet and a tendency to have flatter arches during and after pregnancy. Alignment changes may influence pain, and altered alignment could change the physical stresses placed upon different tissues of the body, which that specific tissue was not adapted to, therefore, causing pain or injury to that tissue.
A study published in 2016, in the Journal of Women’s Health Physical Therapy1, investigated if there may be a relationship between anthropometric changes of the foot that occur with pregnancy and pregnancy-related musculoskeletal pain of the lower extremity. The study included 15 primigravid women and 14 weight-matched controls. This study was a repeated-measurements design study, where the investigators measured foot length, foot width, arch height index, arch rigidity index (ARI), arch drop (AD), rear foot angle, and pelvic obliquity during the second and third trimesters and post-partum. The subjects were surveyed on pain in the lower back, hips/buttocks, and foot/ankle.
The author’s findings were that measures of arch flexibility (ARI and AD) correlated with pain in the lower back and the foot and ankle and that medial longitudinal arch flexibility may be related to pain in the lower back and foot. The more flexible arches were associated with more pain in the study participants. They reported the participants in their study did not have very high pain levels in general and recommended further studies to compare pregnant individuals who experience severe pain with those who do not while comparing their alignment factors.
This article is a good reminder for physical therapists to consider the changes that occur to the foot including changes in arch height, arch flexibility, and foot size, and how that influences the pelvis and lower extremity for prevention and treatment of musculoskeletal pain during pregnancy.
Educating our pregnant patients on shoe wear seems even more important now. Making recommendations, unique to each patient based on their objective data, foot type, and arch flexibility status seems like an appropriate addition to a well-rounded treatment plan.
Doesn’t it seem prudent to wear shoes that provide some arch support to hopefully reduce musculoskeletal pain associated with pregnancy changes?
I have observed some patients who are pregnant arrive at their physical therapy appointment wearing unsupportive flip-flops and other poor shoe-wear choices. I understand there are barriers for pregnant patients, I remember from when I was pregnant that reaching your feet to put shoes on can be very difficult, and sometimes your feet are swelling so it may be near impossible to physically get shoes on your feet. You might even need a new pair of shoes, as your shoes may no longer fit.
However, an article such as this one seems like something I could easily share with a patient to help persuade them of the importance of good shoe wear or at least proper arch support. Being able to discuss a recent scientific study with a patient can be powerful and motivating to a patient.
Additionally, an article such as this reminds a practitioner of specific objective data to monitor such as arch height and flexibility as it changes throughout the patient’s pregnancy.
- How does the patient’s changing arch height and flexibility influence their specific pelvic, hip, knee, and ankle alignment?
- How does swelling play a part in the patients’ foot anthropometrics day to day, trimester to trimester?
- Ask more questions about their daily activities, are they ‘barefoot and pregnant’?
- Could something as simple as having them wear appropriate, arch-supportive shoes while in the home reduce their lower extremity or back pain?"
Join us at the next Pregnancy Rehabilitation course scheduled for July 20-21 to learn more about pregnancy-related topics.
Reference:
- Harrison, K. D., Mancinelli, C., Thomas, K., Meszaros, P., & McCrory, J. L. (2016). The Relationship Between Lower Extremity Alignment and Low Back, Hip, and Foot Pain During Pregnancy: A Longitudinal Study of Primigravid Women Versus Nulliparous Controls. Journal of Women’s Health Physical Therapy, 40(3), 139-146.
AUTHOR BIO
Rachel Kilgore, DPT, OCS, COMT, PRPC, PPCES
Rachel Kilgore, DPT, OCS, COMT, PRPC, PPCES graduated from Central Washington University with a Bachelor of Science (BS) in exercise science and a minor in nutrition in 2004 where she also captained the collegiate soccer team. Rachel completed her Doctor of Physical Therapy (DPT) at University of Washington in 2007. She has worked in out patient orthopedics and pelvic health since 2007. She furthered her physical therapy training earning Certified Orthopedic Manual Therapist (COMT), Physical Therapy Board-Certified Specialist in Orthopedics (OCS), and Pelvic Rehabilitation Practitioner Certification (PRPC). She is a member of the American Physical Therapy Association (APTA), Section of Orthopedics and Section of Women’s Health, and the Physical Therapy Association of Washington (PTWA).
Currently, Rachel practices in Seattle at Flow Rehab in the Freemont Neighborhood with Holly Tanner and Jake Bartholomy. Her patient care focuses on orthopedics, female athletes, and women’s health conditions for bladder & bowel dysfunctions, pelvic, pain, pregnancy and post-partum issues.

I arrived to Pelvic Health Physical Therapy by fruitful exposure and a professional demand to fulfill a new employer’s needs. 10 years later, I am all-in serving women and men with bladder, bowel, sexual dysfunction, and abdominopelvic pain to optimally live their lives well more comfortably.
Throughout my PT education at Washington University in St. Louis, I envisioned specializing in Orthopedics using a Movement Systems Impairment (MSI) diagnostic and treatment approach. While a student in my final 3-month clinical experience at a hospital-based Outpatient Orthopedic Clinic, I had the good fortune to be paired with a clinical instructor who was largely Orthopedic-based but treated Pelvic Health 1 day per week as the sole Pelvic Health PT Provider (shoutout Barb Davis!). The setting was a large community-based safety-net institution, Denver Health, which served Denver residents including underserved populations. Patients presented with chronic pain, complex socioeconomic dynamics, and diverse ethnic backgrounds with Denver historically being a migrant and refugee-welcoming city. My pelvic patients were interesting, and my Pelvic Health interest was sparked.
As a new graduate seeking employment, I secured a job at a hospital-based Outpatient Orthopedic Clinic in San Diego, CA at Scripps Health. My new position was created for an Orthopedic PT who was interested in being mentored in Pelvic Health PT due to a growing need to support Pelvic Health patients and providers in North County San Diego. I was offered mentorship and financial support to pursue continuing education to set a foundation in Pelvic Health. I had an interest, there was a clinical need, I seized the opportunity, ran with it, and I am so grateful I did.
My astute Pelvic Health Mentors (Alissa Meredith, PT, MPT and Destiny Bochinski, PT, DPT, PRPC) highly encouraged me to take the foundational Pelvic Floor Series (which has been updated to the Pelvic Function Series this year) through Herman & Wallace. I was already familiar with Herman & Wallace through my exposure at Washington University in St. Louis, where they host various Herman & Wallace courses. I am so glad I chose to follow my Pelvic Health educational path with Herman & Wallace Rehabilitation Institute. I was lucky enough to be taught Pelvic Floor Level 1 (now called Pelvic Function Level 1) by the venerable and entertaining Holly Herman & Kathe Wallace. Fast forward 10 years and I have taken the full Pelvic Floor Series, Ramona Horton’s Visceral Fascia Mobilization Series, Male Pelvic Health, Nutritional Perspectives, Pregnancy Course, IC, Rehabilitative Ultrasound, and a myriad of other Herman & Wallace continuing education courses. I have a wide arsenal of didactic information, manual skills, proficiency in biofeedback modalities use, and clinical experiences to treat the gamut of simple to complex pelvic and orthopedic patients. Citing the incredible Ramona Horton, MPT, DPT, I completely agree that Pelvic Health is applying Orthopedics within the pelvic cavity. I am grateful to have a practice that is largely Pelvic Health-based with a smattering of Orthopedics. In reality, I practice ~65-70% Pelvic Health and 30-35% Orthopedics.
Across my professional journey, I started as the third Pelvic Health PT at the clinic where I work, to now being one of eight Pelvic Health PT providers at that same comprehensive outpatient rehab center, Scripps Rehabilitation Services in Encinitas. I am lucky to be part of a burgeoning Pelvic Health Team at our clinic site as well as across the larger health system. I was lucky to be mentored by two amazing colleagues, including now a Herman & Wallace Instructor, Destiny Bochinski, who I continue to work with and collaborate well with. I am appreciative of the opportunity to continue to grow professionally by serving as a Pelvic Health mentor at my clinic and TA for Herman & Wallace, which I’ve been doing since 2020.
Thank you for letting me share my story, which is one of seizing a ripe opportunity and allowing my career path to evolve with an initial spark that I didn’t early on envision would be my path, but I love where I’ve been and my trajectory forward.
AUTHOR BIO
Jackie Castillo, PT, DPT, MSC
 Jackie Castillo, PT, DPT, MSCI is a Board-Certified Orthopedic Clinical Specialist based out of San Diego, CA who practices Pelvic Health and Orthopedic Physical Therapy at Scripps Rehabilitation Services in Encinitas. She received her DPT and MSCI (Master of Science in Clinical Investigation) Degrees from Washington University in St. Louis in 2013. She received her BS in Animal Physiology & Neuroscience from the University of California, San Diego in 2005. She has served as a Teaching Assistant for Herman & Wallace since 2020. She intends to sit for the Herman & Wallace PRPC Exam this year. She enjoys running, yoga, walking her puppy, hiking, biking, and exploring good food and drink with her soon-to-be husband, family, and close friends.
Jackie Castillo, PT, DPT, MSCI is a Board-Certified Orthopedic Clinical Specialist based out of San Diego, CA who practices Pelvic Health and Orthopedic Physical Therapy at Scripps Rehabilitation Services in Encinitas. She received her DPT and MSCI (Master of Science in Clinical Investigation) Degrees from Washington University in St. Louis in 2013. She received her BS in Animal Physiology & Neuroscience from the University of California, San Diego in 2005. She has served as a Teaching Assistant for Herman & Wallace since 2020. She intends to sit for the Herman & Wallace PRPC Exam this year. She enjoys running, yoga, walking her puppy, hiking, biking, and exploring good food and drink with her soon-to-be husband, family, and close friends.

Imagine you’re a provider who has foundational information about the pelvic floor. Maybe you’ve just started taking coursework for adults, you may have taken a pediatric pelvic health class or maybe you’ve been treating adults for years. You know the anatomy, the physiology, and the general treatment practice guidelines.
- Your clinic gets a call about a baby with colic and your supervisor asks you if you could treat it. Do you accept the evaluation?
- You see a post on a “mommy Facebook group” asking for potty training tips for a child who is withholding stool during potty training. Do you tag your business/practice as a resource that can help?
- You have a family friend with a child struggling with voiding during the school day and they ask you for advice as a pelvic health provider. Do you have ideas on how to guide them?
- A patient you are seeing for pelvic floor issues asks you to start treating their teenager because they have “the same issues.” Does this seem scary to you?
Pediatric Pelvic Floor Play Skills is a class written to be a supplement to other pelvic health education classes a pelvic floor therapist has likely taken. This class helps providers take the pelvic health knowledge they have, and learn activities they can perform with different ages of children to help work on their pelvic floor function. The class shows videos of actual treatment sessions of different children in different age groups showing how to integrate stretching, strengthening, coordination, and other fun activities into a therapy visit.
One of the tricky parts of working with children is including the child in their plan of care and coordinating with caregivers. Pediatric Pelvic Floor Play Skills talks about specific concerns and considerations by age, as well as strategies to bring to a provider's practice. This class is for the provider who does not have a lot of experience treating pediatric patients and wants to learn how to make sessions enjoyable and effective.
This class includes sample home programs, equipment purchase lists (with a budget in mind), tips for helping get families on board with the implementation of care, and resources such as outcomes measures, developmental milestone checklists, and recommendations things parents ask for like how to talk about periods and sex.
The next Pediatric Pelvic Floor Play Skills remote course is scheduled for June 29th, come spend a day learning how to integrate what you already know into a playful session for your tiniest of clients to your angstiest teenager.
AUTHOR BIO
Mora Pluchino, PT, DPT, PRPC
 I am a graduate of Stockton University with my BS in Biology (2007) and Doctorate of Physical Therapy (2009). I have experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. I began treating Pelvic Health patients in 2016 and now have experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much I have not treated since beginning this journey and I am always happy to further my education to better help my patients meet their goals.
I am a graduate of Stockton University with my BS in Biology (2007) and Doctorate of Physical Therapy (2009). I have experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. I began treating Pelvic Health patients in 2016 and now have experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much I have not treated since beginning this journey and I am always happy to further my education to better help my patients meet their goals.
I strive to help all of my patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at the present time. In 2020, I opened my own practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. I have been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. I have also been a TA with Herman and Wallace since 2020 and have over 150 hours of lab instruction experience.

Congratulations on completing Pelvic Function Level 1 (PF1) and entering the world of pelvic rehabilitation. Are you ready for your next course but not quite sure which one to take? Well, you’re not alone. Everyone’s pelvic health educational journey is different based on their interests and patient demographics and there are a lot of course options available.
I’m going to zero in on the intermediate-level courses in the Pelvic Function Series for you as HW does recommend that practitioners take at least one or two of these. If you’ve looked at the course page you’ve noticed that there are three courses with a Level 2 designation – as well as a lab course. What does this mean? These courses are designed to be a progression of knowledge and skills learned in the foundational course Pelvic Function Level 1.
Here are the intermediate courses:
- Pelvic Function Level 2A (PF2A) - Colorectal Pelvic Health, Pudendal Neuralgia, and Coccyx Pain
- Labs provide an introduction to internal anorectal examination for all genders.
- Pelvic Function Level 2B (PF2B) Urogynecologic Examination and Treatment Interventions
- Labs provide external abdominal and pelvic and internal vaginal approaches.
- Pelvic Function Level 2C (PF2C) Men’s Pelvic Health and Rehabilitation
- Labs provide external abdominal, gluteal, perineal, and internal anorectal approaches.
- Modalities and Pelvic Function (PFMOD) The Pelvic Health Toolkit
- Labs provide supervised instruction to practice modalities.
Ready for a more in-depth look at the courses? Here is a more detailed breakdown:
Pelvic Function Level 2A (PF2A) Colorectal Pelvic Health, Pudendal Neuralgia, and Coccyx Pain
This course is intended for the pelvic health clinician who treats patients with common functional gastrointestinal (GI) dysfunctions and is interested in learning internal anorectal examination and the use of balloon re-training.
In this course, you will learn about common functional gastrointestinal (GI) dysfunctions including irritable bowel syndrome, fecal incontinence, and constipation. Course topics provide an introduction to nutrition for bowel health, colorectal conditions, and oncology. Participants will be educated on how diagnoses such as hemorrhoids, fistulas, fissures, and anorectal pain including pudendal neuralgia and coccygodynia may be improved with pelvic rehabilitation.
Practical, trauma-aware, hands-on labs provide supervised instruction of pelvic function evaluation with external observation, palpation, and internal anorectal examination of pelvic skeletal and soft tissues. These labs include an external perineal and internal anorectal approach as well as education in the use of balloon re-training.
Pelvic Function Level 2B (PF2B) Urogynecologic Examination and Treatment Interventions
This course is intended for the pelvic health clinician who treats patients with conditions including urinary incontinence, chronic pelvic pain (CPP), and pelvic organ prolapse.
In this course, you will learn, with increased specificity, evaluation for urogynecologic conditions as well as an overview of medical management, and multi-disciplinary pelvic healthcare. Course topics provide a more in-depth understanding of urinary incontinence, chronic pelvic pain (CPP), and pelvic organ prolapse. Participants will be educated on how diagnoses such as interstitial cystitis/painful bladder syndrome (IC/PBS), urinary tract infections, vaginismus, vulvar pain, dyspareunia, polycystic ovarian syndrome (PCOS), and endometriosis may be improved with pelvic rehabilitation.
Practical, trauma-aware, hands-on labs provide supervised instruction of pelvic structures in relationship to the vaginal canal and surrounding structures such as the lumbopelvic nerves, the uterus, urethra, bladder, and rectum. Interventions instructed will include patient management of trunk and pelvic pressure, relaxation training, breathing, and manual therapies for a variety of pelvic dysfunctions. These labs include an external abdominal and pelvic and internal vaginal approach.
Pelvic Function Level 2C (PF2C) Men’s Pelvic Health and Rehabilitation
This course is intended for pelvic health clinicians who are interested in treating male pelvic health conditions.
In this course, you will learn critical detailed information about men’s pelvic health conditions including post-prostatectomy urinary incontinence, erectile dysfunction, and chronic pelvic pain (CPP). Participants will be educated on how diagnoses such as hard/flaccid, urgency/frequency, scrotal, testicular, and penile pain may be improved with pelvic rehabilitation.
Practical, trauma-aware, hands-on labs provide supervised instruction of pelvic health evaluation with external observation, palpation, and internal anorectal examination of pelvic structures and soft tissues. These labs include an external abdominal, gluteal, perineal, and internal anorectal approach.
Modalities and Pelvic Function (PFMOD) The Pelvic Health Toolkit
This course is for the pelvic health clinician who has the opportunity to use modalities as an adjunct to their patient's care and goes beyond the "Big 3" (E-Stim, Biofeedback, and Ultrasound).
In this course, you will learn about and practice a variety of modalities. Modalities in PFMOD include biofeedback, cold laser/light therapy, electrotherapy, real-time ultrasound imaging, belts, braces, supports, lubricants, myofascial tools/techniques, and “special topics” that can be used to assist in relaxation, bowel and bladder health, and sexual function. Specialized knowledge from experts in different subjects will be shared throughout the course.
Certain modalities that are impractical to practice live will be shared and demonstrated via video. These Interventions include shockwave, rehabilitative ultrasound imaging, dry needling, and light therapy.
Practical, trauma-aware, hands-on labs provide supervised instruction to practice utilizing biofeedback and other modalities to allow kinesthetic learning before prescribing and recommending them to patients.
Previous course sponsors who have provided samples and products have included:
- Nix
- Flyte
- OhNut
- Replens
- RockTape
- Bellies Inc.
- Ice Soothers
- BabyBellyBand
- Intimate Rose
- The Pro Group
- Good Clean Love
- Cushion Your Assets
If you are interested in taking an intermediate-level Pelvic Function Course but still have questions, then please contact us.
The journey to and through motherhood is, no doubt, filled with an array of emotional, mental, and physical changes. It can and should be, one of the most empowering times in a person’s life, but it can start to feel overwhelming when there is any degree of uncertainty or when there are obstacles that present themselves throughout the journey. The body is expected to change and grow in ways that are both magical and daunting for the birthing person and the clinicians in the pelvic health arena should be providing the education to help the pendulum swing towards the magic. Unfortunately, access to this education is sparse, recommendations can be conflicting (pending who you're talking to), and an understanding of the services that we can, and should be, providing in the perinatal period are not well defined nor understood by the majority of the healthcare continuum of providers.
During pregnancy, the body transforms with such beautiful intent. The overarching intention is to support adaptation to nurture and accommodate the developing fetus. During this transformation, the body will inevitably undergo physiologic changes in every system of the body, including the neuromusculoskeletal system. These changes in the neuromusculoskeletal system can contribute to the common ailments and complaints of our clients who are pregnant. Pregnancy-related low back pain, pelvic girdle pain, pubic symphysis dysfunction, and neuropathy are amongst some of those ailments whose symptom drivers are the nerves and muscles. As pelvic health clinicians, what is our best effort to treat these tissues during the gestational period?
How does dry needling fit in during pregnancy?
The way we approach tissue dysfunction during the gestational period is no different than at other times in a person’s life. We do, however, have to consider things like the stage of gestation, appropriate zones of treatment, dosage, and patient positioning for certain interventions, one of those being dry needling. In regards to dry needling intervention, we avoid implementing this in the first trimester secondary to the higher risk of spontaneous miscarriage.
There is no evidence to suggest that dry needling intervention would contribute to spontaneous miscarriage. However, as a clinician, we want to protect ourselves so as not to be associated with this unfortunate adverse event. We also withhold implementing dry needling in the zones of the thoracolumbar junction, the pelvic floor musculature, and the anterior abdominal musculature throughout the entire gestational period; this is due to avoiding the region of innervation to the uterus to mitigate association with a possible spontaneous pre-term labor and to abstain placing a needle within geographic proximity to the developing fetus. Otherwise, dry needling is an appropriate intervention for the management of neuromusculoskeletal conditions in this patient population, especially when other clinical approaches for pain mitigation (i.e.: pharmaceutical use) are contraindicated or simply not offered by other healthcare providers. A properly trained clinician can safely implement dry needling as a powerful intervention for pain relief and neuromuscular reset to allow for better activity and load tolerance during the gestational period. Improving activity and load tolerance for the expecting mother has a multitude of benefits for both physical and mental wellness.
Amazing!! What about in the postpartum period?
In the postpartum period, the body will inevitably go through a massive shift in the overall performance of the neuromuscular system. Birth-related neuromuscular dysfunction is common following both vaginal and cesarian delivery due to the mechanical and biochemical stressors placed on the involved tissues, a concept that shouldn’t be surprising for the rehabilitative clinician. Consider your postoperative patient following a total knee replacement; there is a certain degree of expectation surrounding neuromuscular shutdown following the procedure secondary to the inflammatory cascade that follows. Performance for daily activities such as ambulation, transitional movements, and ability to participate in recreational tasks is limited during the acute and subacute recovery period. It takes time to regain mobility of the involved joints and the neuromuscular coordination and strength of the impacted tissues. We progress the patient through our plan of care to reset the dysfunctional tissues, reinforce good movement strategies, and reload the tissues back to function. The neuromuscular performance following a vaginal or cesarean delivery is no different. The muscle groups impacted following birth are typically those of the core canister including the diaphragm, abdominal wall, pelvic floor, and lumbopelvic posterior stabilizers.
One of the best reset tools we have as rehabilitative clinicians is dry needling. We are able to specify treatment to the tissue targets that are unique to each client’s symptom presentation while utilizing electrical stimulation to influence the nervous system for both tissue recovery and performance. Being a bioelectric system, our bodies respond beautifully to this type of input, especially when followed with appropriate interventions to reinforce neuromotor coordination and functional loading. This sequence of interventions optimizes the overall function of the nervous system which ultimately dictates the behavior and performance of the rest of the body. As it relates to our postpartum clientele this should be something we are considering in the immediate postpartum period to optimize birth recovery, especially for the heavily impacted tissues like the abdominal wall, lumbopelvic stabilizers and pelvic floor.
We have a continuously developing body of evidence that supports the utilization of dry needling for tissue health and performance. The mechanisms behind this are biomechanical, biochemical, vascular, and neural in nature. There is also emerging evidence that is exploring the utilization of dry needling with electrical stimulation (aka neuromodulation) for wound healing. The possible impact that we can have on the healing of episiotomy incisions, cesarean incisions, or perineal tears in the acute and subacute postpartum stage is encouraging given the evidence, and has also been seen to be very powerful anecdotally.
If you want to learn more about the implementation of dry needling into your practice as it relates to the perinatal period, join us on an upcoming Dry Needling and Pelvic Health: Pregnancy and Postpartum Considerations! There are two more courses scheduled this year. One this summer in Arlington VA on June 22-23, and the other this fall in Seattle WA on October 18-20.
AUTHOR BIO
Kelly Sammis, PT, DPT, OCS, PCES, AFDN-S, CLT
 Kelly Sammis is a physical therapist, educator of dry needling and all things pelvic, Pilates instructor, wife, and mama living and working in Parker, Colorado. Her passion for treatment in physical therapy is in sports performance, pelvic health, and overall wellness. She specializes in the treatment of male and female pelvic floor dysfunction, athletic injury/return to sport, sports performance, and persistent pain. Her formal education took place at Ohio University (2007) and The University of St Augustine for Health Sciences (2010).
Kelly Sammis is a physical therapist, educator of dry needling and all things pelvic, Pilates instructor, wife, and mama living and working in Parker, Colorado. Her passion for treatment in physical therapy is in sports performance, pelvic health, and overall wellness. She specializes in the treatment of male and female pelvic floor dysfunction, athletic injury/return to sport, sports performance, and persistent pain. Her formal education took place at Ohio University (2007) and The University of St Augustine for Health Sciences (2010).
She is a Midwest native with a strong history of treating persistent pain, pelvic floor, and return to sport dysfunctions. Kelly serves as lead faculty developing and teaching dry needling and pelvic health courses nationwide. When she is not treating clients or teaching you can find her spending time with her husband, two children, and labradoodle, Dexter, exploring our landscapes and the beautiful mountains of Colorado!
Herman & Wallace offers a number of downloadable products on our website for your clinical practice, and we want to put you in charge of deciding which new products we create and offer!
What is a Prefund?
The HW philosophy is that we should only be making products that are useful to our practitioners. In our efforts to create the most valuable products and keep the price as low as possible, we have launched a new Prefund product development program.
Need more information? Check out the Prefund FAQs.
Here is how it works:
- Herman & Wallace creates a product concept, a description of the product and its contents, without fully creating the product.
- The product concept can be found on the HW Product Page as a “Prefund” product for a limited period of 7 days. In this case, the products will be available from May 22, 2024 until midnight on May 28, 2024.
- All product concepts include:
- A description of the product
- Product content list: patient forms, PowerPoint files, handouts, mapping tools, etc
- Standard retail price of the product once it is launched
- Prefund retail price of the product - which is 40% lower than the retail price
- All product concepts include:
- Practitioners who would like to buy the product can prefund the product concept at a 40% discount on the standard retail price in exchange for receiving the product upon Herman & Wallace completing its development.
- If you see a product you'd like to purchase, then prefund it! If the product gets enough pre-funders, then HW will develop the product.
- Once the product is developed, we'll email your product to you.
There is NO RISK!
Prefunding a product carries NO RISK. If the product does not receive enough prefunding by the end of the trial period, Herman & Wallace will refund 100% of the amount contributed by each prefunder.
Product concepts to choose from:
Prefund and Downloadable Products are available on the HW Product Page.
- Inclusivity for Beginners
- Pricing: Prefund $45, Standard $75
- This product includes tips and pearls of wisdom to enhance your understanding of diversity, equality, and inclusivity as well as tools like up-to-date terminology and definitions to help practitioners create a safe and welcoming environment for clients.
- Birth Prep for Pelvic Health Clients
- Pricing: Prefund $90, Standard $150
- This product will make it incredibly easy for you to host a Birth Prep class for any audience.
- Trauma Informed Care Checklist
- Pricing: Prefund $45, Standard $75
- This product will help you review the concepts of trauma-informed care and check in with yourself and the practices of your workplace. It will then provide guidelines and tips to provide the best possible trauma-informed care to your clients.
- Hosting a Pelvic Floor Student
- Pricing: Prefund $60, Standard $100
- This is the perfect document to help prepare any clinician for a pelvic health student.
- Quick Reference Treatment Checklists
- Pricing: Prefund $45, Standard $75
- These quick informative checklists include topics like constipation, stress incontinence, urge incontinence, pelvic organ prolapse, hemorrhoid management, and painful insertion.
Carpe Diem
By prefunding a product, you are helping guide what resources HW creates. This keeps prices lower on all products by assuring we don’t spend resources creating products that our audience does not value. If a prefund concept does not get funded, you get a 100% refund. If it does meet the minimum, you will receive the product concept you prefunded at a significant discount!
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/










































