This post was written by H&W instructor Michelle Lyons, PT, MISCP, who authored and instructs the course, Special Topics in Women’s Health: Endometriosis, Infertility & Hysterectomy. She will be presenting this course this February!

Endometriosis is a common gynaecological disorder, affecting up to 15% of women of reproductive age. Because endometriosis can only be diagnosed surgically, and also because some women with the disease experience relatively minor discomfort or symptoms, there is some controversy regarding the estimates of prevalence, with some authorities stating that as many as one and three women may have endometriosis (Eskenazi & Warner 1997)
There is a wide spectrum of symptoms of endometriosis, with little or no correlation between the acuteness of the disease and the severity of the symptoms (Oliver & Overton 2014). The most commonly reported symptoms are severe dysmenorrhoea and pelvic pain between periods. Dyspareunia, dyschezia and dysuria are also commonly seen. These pain symptoms can be severe and have been reported to lead to work absences by 82% of women, with an estimated cost in Europe of €30 billion per year (EST 2005). Secondary musculoskeletal impairments caused by may include: lumbar, sacroiliac, abdominal and pelvic floor pain, muscle spasms/ myofascial trigger points, connective tissue dysfunction, urinary urgency, scar tissue adhesion and sexual dysfunction (Troyer 2007) – all of which may be responsive to skilled pelvic rehab intervention.
Endometriosis can lead to inflammation, scar tissue and adhesion formation and myofascial dysfunction throughout the abdominal and pelvic regions. This can set up a painful cycle in the pelvic floor muscles secondary to the decrease in pelvic and abdominal organ/muscle/fascia mobility which can subsequently lead to decreased circulation, tight muscles, myofascial trigger points, connective tissue dysfunction and pain and possible neural irritation.
Abdominal trigger points and pain can be commonly seen after laparascopic surgery for diagnosis or treatment. We know that fascially, the abdominal muscles are closely connected with the pelvic floor muscles and dysfunction in one group may trigger dysfunction in the other, as well as causing associated stability, postural and dynamic stability issues.
The pain created by muscle tension and dysfunction, may lead to further pain and increasing central sensitisation and further disability. Unfortunately for the endometriosis patient, as well as dealing with the problems already associated with endometriosis, she may also develop a spectrum of secondary musculo-skeletal problems, including pelvic floor dysfunction – and for some patients this may actually be responsible for the majority of their pain (Troyer 2007).
The skilled pelvic rehab therapist has much to offer this under-served patient population in terms of reducing pain and dysfunction, educating regarding self-care and exercise and helping to restore quality of life. Interested in learning more? Join me for my new course: ‘Special Topics in Women’s Health: Endometriosis, Infertility & Hysterectomy’ in San Diego this February or Chicago in June.
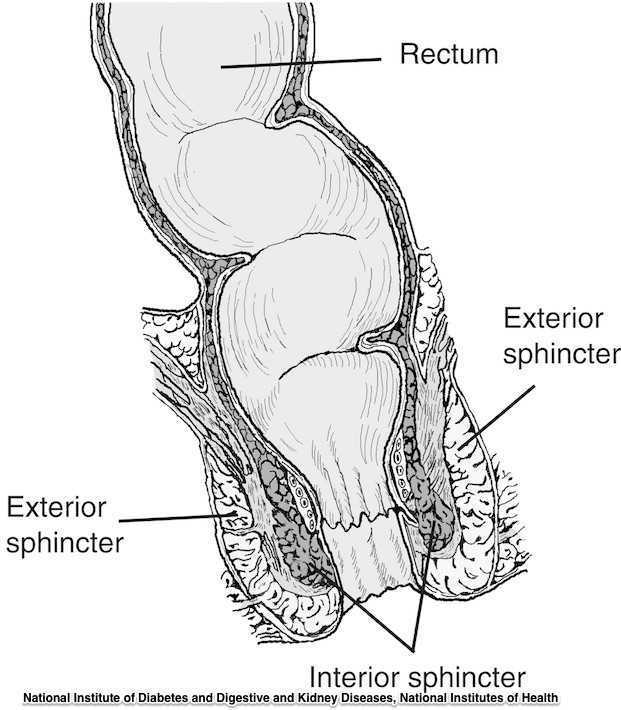
Guidelines for the management of 3rd and 4th degree tears were updated and published last month by The Royal College of Obstetricians & Gynaecologists. The purpose of the guidelines are to provide evidence-based guidelines on diagnosis, management and treatment of 3rd and 4th degree perineal tears. These types of tears are also referred to as obstetric anal sphincter injuries, or OASIS. The authors acknowledge an increased rate of reported anal sphincter injuries in England that may in part be due to increased awareness and detection of the issue. In terms of classification of anal sphincter injuries, the following is recommended (note the different levels at grade 3:
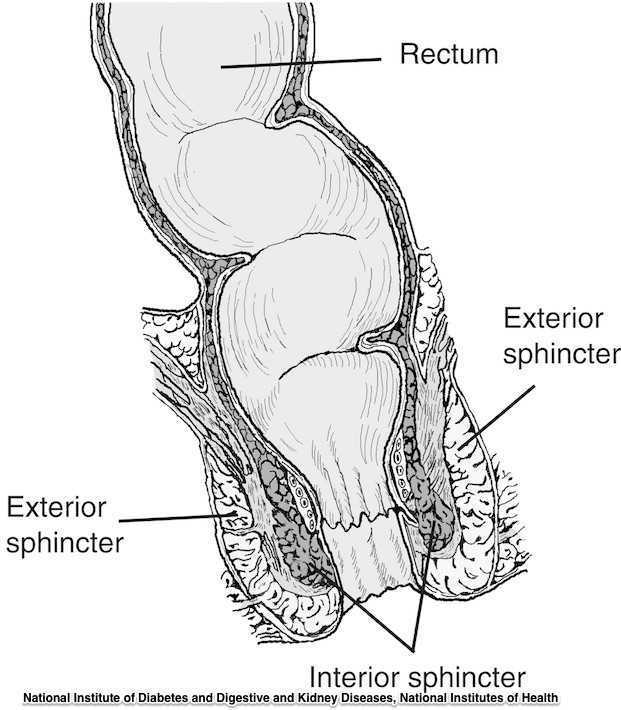
- 1st degree tear: injury to the perineal skin and/or the vaginal mucosa
- 2nd degree tear: injury to the perineum involving the perineal muscles but not involving the anal sphincter.
- 3rd degree tear: injury to the perineum involving the the anal sphincter complex
- Grade 3a tear: Less than 50% of the external anal sphincter (EAS) thickness is torn.
- Grade 3b tear: More than 50% of the EAS thickness is torn.
- Grade 3c tear: Both the EAS and the internal anal sphincter (OAS) are torn.
- 4th degree tear: Injury to the perineum involving the anal sphincter complex (EAS and IAS) and the anorectal mucosa.
Risk factors for anal injury are also outlined in the guidelines, although the authors point out that accurate prediction based on the risk factors is not reliable. The noted risk factors are as below:
- Asian ethnicity
- Nulliparity
- Birthweight greater than 4 kg (8.8 lb)
- Shoulder distocia
- Occipito-posterior position
- Prolonged 2nd stage labor
- Instrumented delivery
Recommendations worth noting include Level A evidence that warm compression during the 2nd stage of labor reduces the risk of OASIS. A noted best practice recommendation is that “Women should be advised that physiotherapy following repair of OASIS could be beneficial.” Guidelines such as these from The Royal College of Obstetricians & Gynaecologists can help in creating common language and in making recommendations that improve communication and expectations between patients and providers.
If you are interested in learning more about anal tears, Herman & Wallace offers several courses which cover the topic. For postpartum care specifically, check out Care of the Postpartum Patient.
As pelvic rehab providers, we may find it easy to talk to our patients about sexual function when it is a patient who comes to us with a sexually relevant problem or directly related diagnosis, such as dyspareunia or limited intercourse participation due to prolapse symptoms. However, are we talking to our other patients about sexual function? Are they talking to us about it? What about our orthopedic patients - are we routinely asking them about how their problem can affect their sexual function? Some recent studies found that 32% of patients planning to undergo a Total Hip Replacement (THR) had reported concerns about difficulties with sexual activityBaldursson, Wright. Was the fact that they could not participate in sexual activity due to the hip pain a driving factor when considering the hip replacement, maybe? Just because a patient doesn’t ask, does not mean that they don’t want to know how their orthopedic injury affects sexual function. Resuming sexual function is an important quality of life goal that is included on few outcome assessment forms, however, there are some that address this subject such as the Oswestry Disability Index for Low Back Pain. Discussion of this topic should be addressed more routinely than it is.
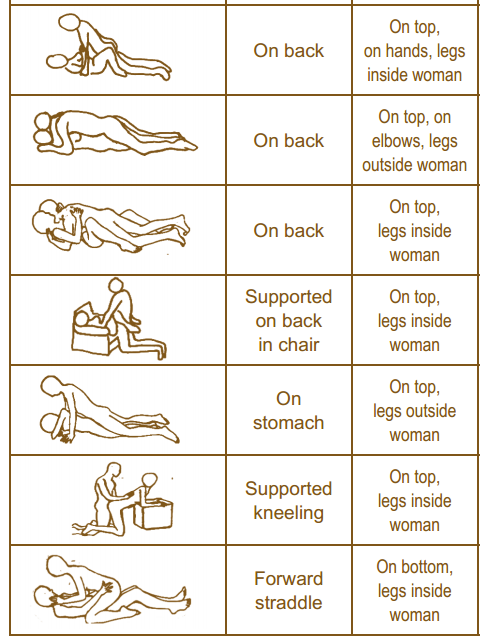
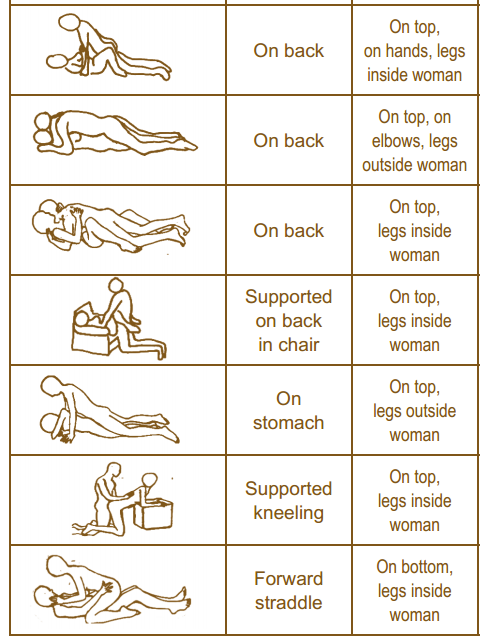
It is important to remember that just because a patient is not in our office for a directly related sexual problem, it is still important to at least open up the dialogue about sexual health. One study in 2013 had patients complete a questionnaire on their sexual function after undergoing a total hip or total knee replacement and 90% reported improved overall sexual functionRathod, et al.. We should try to make the conversation part of our routinely delivered information for a total joint replacement, for example when telling our THR patient, you can resume driving at 3-6 weeks (or when cleared by surgeon), you have Range of Motion precautions of avoiding internal rotation, hip flexion past 90 degrees, and hip adduction (crossing the legs) for the length specified by your surgeon (if it was a posterior approach THR), and you can resume sexual function at 3-6 weeks (or when cleared by the surgeon), or when you feel ready after that. It is important to give the patient some kind of guideline about when they can expect to resume sexual activity, however, always emphasize that it should be resumed when the patient is ready so they don’t feel pressured before they are ready. Also as pelvic rehab practitioners we can offer them guidance about what positions may be best for them when returning to sexual activity to put less strain on the prosthesis and hip as well as help them be comfortable. To continue with our example for THR (posterior approach) their precautions are likely to restrict hip flexion past 90 degrees, hip internal rotation, and adduction, so for a man or woman following THR lying on their back would be a safe position.
As physical therapists it is our job to provide guidance. Instead of telling people what not to do, helping them find a safe way to do things they want to do to maintain function should always be our goal. Sexual activity participation is definitely an important function for quality of life that is often overlooked and not discussed, so talk to your patient about it, they will likely appreciate it.
One useful tool to learn more about positioning for sexual activity is the Herman & Wallace product “Orthopedic Considerations for Sexual Activity.” It provides a great list of positions with pros and cons of each position, and is a helpful visual aid for your patients to help them return to sexual function safely with consideration of their respective injuries.
Baldursson, H., & Brattström, H. (1979). Sexual difficulties and total hip replacement in rheumatoid arthritis. Scandinavian journal of rheumatology, 8(4), 214-216.
Wright, J. G., Rudicel, S. A. L. L. Y., & Feinstein, A. R. (1994). Ask patients what they want. Evaluation of individual complaints before total hip replacement. Journal of Bone & Joint Surgery, British Volume, 76(2), 229-234.
Rathod PA, Deshmuka AJ, Ranawat AS, Rodriguez JA. Sexual function improves significantly following total hip and knee arthroplasty: a prospective study. Program and abstracts of the 2013 meeting of the American Academy of Orthopedic Surgeons; March 19-23, 2013; Chicago, Illinois. Poster P023.
Happy Tuesday! Today we are fortunate enough to hear from Stefanie Foster, who just earned her designation as a Certified Pelvic Rehabilitation Practitioner! Thank you for your time, Stefanie, and congratulations!
Describe your clinical practice:
I have a private practice specializing in pelvic health and related orthopedic conditions. My clinical practice is infused with my training in yoga, pelvic rehab, women’s functional nutrition, orthopedic manual physical therapy, and movement system impairment syndromes.
 How did you get involved in the pelvic rehabilitation field?
How did you get involved in the pelvic rehabilitation field?
I first became curious about the pelvic floor muscles as a consequence of treating orthopedic conditions. No matter what you’re working with in that setting– back pain, hip pain, even shoulder or foot, central stability or the core is of utmost importance. I started to wonder what was going on with the respiratory diaphragm and pelvic floor when we were doing all this abdominal bracing that was (and still is in some circles) all the rage. I arranged a clinical in-service with Susan Steffes to come give us a little overview and talk about how to screen for when someone needed to see a pelvic PT. After that little hour, my interest was piqued and I knew I had to learn more…hence my first H&W class.
What/who inspired you to become involved in pelvic rehabilitation?
It was a gradual inspiration, beginning with Susan. Then, I would have to say Holly and Kathe; my experience in Level 1 forever changed my professional trajectory. As far as the “what”, clinically I am always very attracted to the zebras, the complex conditions, the things that are slipping through the cracks in the medical system, the underserved…and everything about pelvic rehabilitation is that. It’s also a big public health...uh I’ll say opportunity rather than crisis. As a profession, we are doing better, but we still have a long way to go before everyone knows what we can do. Imagine how many people we could help if EVERYONE knew?! It’s really exciting!!
What patient population do you find most rewarding in treating and why?
I love working with patients who come in with a student’s mind. The ones who are curious, ask questions, take notes, and consistently do their homework typically develop a great working relationship with me and have excellent outcomes.
If you could get a message out to physical therapists about pelvic rehabilitation what would it be?
To my former orthopedic-focus-only self and anyone in the same boat, it would be to stop pretending the pelvic floor doesn’t matter in your practice. At the very least, when you’re doing your red flag screen and ask if the patient has had any changes in bowel or bladder, stop downplaying it when the patient mentions they have had some minor leaks or constipation. Refer them to a pelvic rehab specialist! Don’t scare them, just tell them it’s common and there’s pharma-free help out there!
What has been your favorite Herman & Wallace Course and why?
Holly and Kathe taught my Level 1 and it was one of THE BEST courses I’ve ever taken (I’m not just saying that because it’s for their site!). They somehow managed to simultaneously have us rolling on the floor laughing, feeling incredibly supported and comfortable, and leave us ready to walk out the door and treat patients Monday morning. Incredible.
What is in store for you in the future?
More teaching and research. I am passionately curious about several unanswered questions and could keep myself busy the rest of my life investigating and sharing my findings. Right now, the relationship of orthopedic conditions and movement impairments of the hip with pelvic floor-related complaints has mesmerized me!
What role do you see pelvic health playing in general well-being?
If you look at the yoga tradition, the pelvic floor is our base, our ground, our safety, our manifestation into the world… Everything we work with - bladder, bowel, sexual function, birth – is so basic to life on earth! Treatment of these conditions is truly life enhancing! Without the pelvic floor and related structures functioning optimally, it’s challenging to get the rest of the system to function optimally.
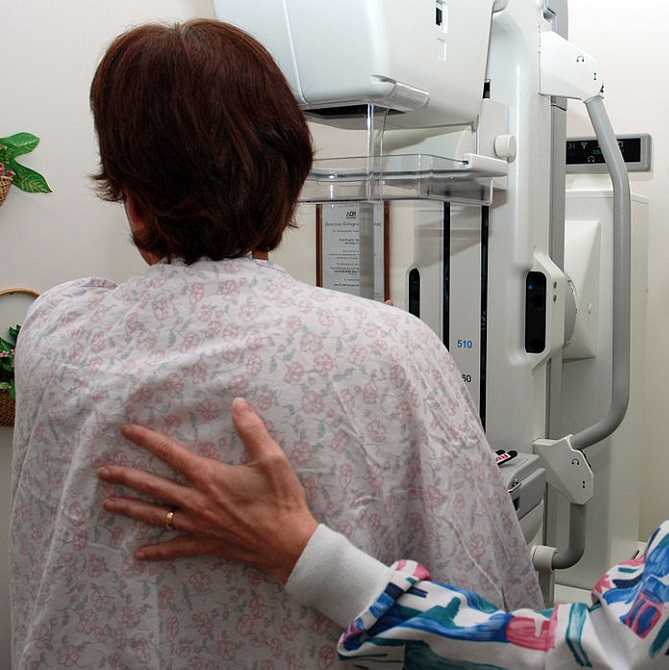
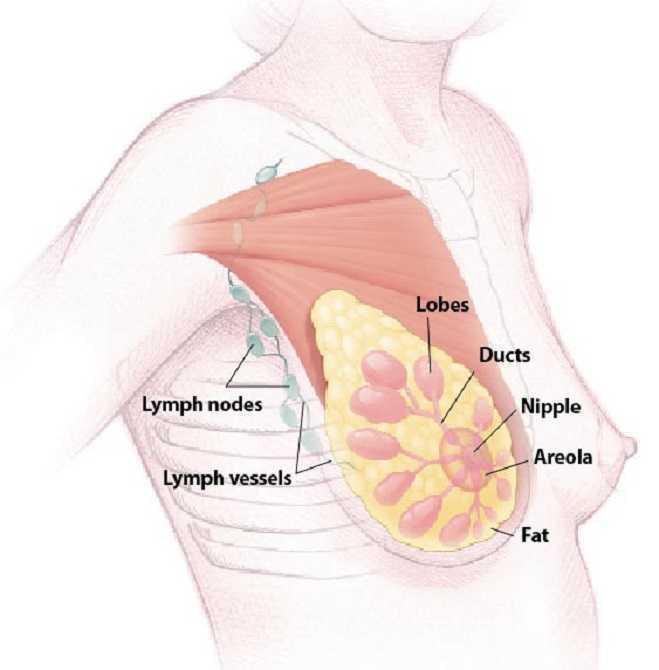
My first experience treating a patient with shoulder pain and limitations post-mastectomy just happened to be a local doctor’s sister. Luckily, I did not know this until a few sessions into her therapy. Ultimately, even more than normal, this patient’s outcome was a make or break situation for a future referral source. Her incredible spirit and optimism made the prognosis an inevitably positive one. Whether or not I had manual therapy training was a moot point, according to current research; however, from my perspective, I would not have been as competent in treating her without it.
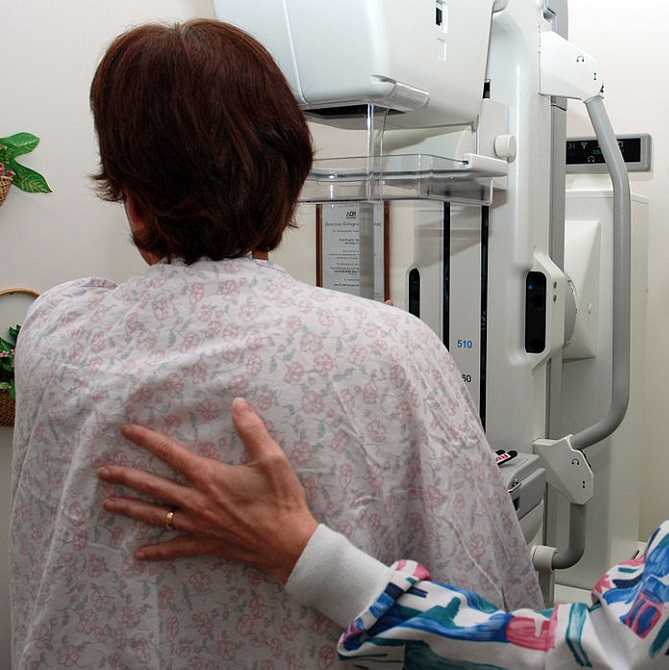 In June 2015, De Groef et al. performed a review of literature to investigate the efficacy of physical therapy for upper extremity impairments after surgical intervention for breast cancer. Eighteen randomized controlled studies were chosen for review regarding the efficacy of passive mobilization, myofascial therapy, manual stretching, and/or exercise therapy after breast cancer treatment. In the studies reviewed, physical therapy began at least 6 weeks post-surgical intervention. Combining general exercise with stretching was confirmed effective on range of motion (ROM) by 2 studies. One study showed the effect of passive mobilization with massage was null for pain or impaired ROM. No study showed any effect of myofascial therapy, one poor quality study supported the use of passive mobilization alone, and one study showed no effect of stretching alone. Active exercises were found more effective than no therapy or simply education in five studies. Early intervention was found to be beneficial for shoulder ROM in 3 studies, but 4 other studies supported delayed exercise to promote wound healing longer. Ultimately, pain and impaired shoulder ROM after operative treatment for breast cancer have been treated effectively by a multifactorial approach of stretching and active exercise. The efficacy of passive mobilization, stretching, and myofascial therapy needs to be investigated with higher quality research in the future.
In June 2015, De Groef et al. performed a review of literature to investigate the efficacy of physical therapy for upper extremity impairments after surgical intervention for breast cancer. Eighteen randomized controlled studies were chosen for review regarding the efficacy of passive mobilization, myofascial therapy, manual stretching, and/or exercise therapy after breast cancer treatment. In the studies reviewed, physical therapy began at least 6 weeks post-surgical intervention. Combining general exercise with stretching was confirmed effective on range of motion (ROM) by 2 studies. One study showed the effect of passive mobilization with massage was null for pain or impaired ROM. No study showed any effect of myofascial therapy, one poor quality study supported the use of passive mobilization alone, and one study showed no effect of stretching alone. Active exercises were found more effective than no therapy or simply education in five studies. Early intervention was found to be beneficial for shoulder ROM in 3 studies, but 4 other studies supported delayed exercise to promote wound healing longer. Ultimately, pain and impaired shoulder ROM after operative treatment for breast cancer have been treated effectively by a multifactorial approach of stretching and active exercise. The efficacy of passive mobilization, stretching, and myofascial therapy needs to be investigated with higher quality research in the future.
Another review of literature in 2010 by McNeely et al. used 24 studies to analyze the effectiveness of exercise intervention for upper extremity impairments after breast cancer surgical intervention. Ten of the studies focused on early versus late intervention, and all supported the earlier implementation of post-surgical exercises for ROM; however, wound drain volume and duration were increased in the subjects engaged in earlier exercises. Fourteen studies showed structured exercise intervention improved shoulder ROM significantly in the post-op period, and a 6-month follow up continued to show improved upper extremity function. No lymphedema risk was noted in any of the studies.
As with many areas of physical therapy, better research is needed to support what we do. We often treat with success in the clinic despite lack of strength in the evidence-based realm. After implementing glenohumeral and scapulothoracic mobilizations, soft tissue work in the posterior cervical and scapular muscles (avoiding lymph nodes), stretching, progressive resisted strengthening, and a home program, my patient regained full range of motion and function of the affected shoulder after her mastectomy. In retrospect, I should have written up a case study on this patient to contribute to our profession. At least after my patient was discharged, the clinic where I worked received a healthy supply of future referrals from her sister because of the positive results achieved with therapy.
If you are interested in learning evaluation and treatment techniques which can benefit breast oncology patients, consider a Herman & Wallace Physical Therapy Treatment for the Breast Oncology Patient course in 2016.
De Groef A, Van Kampen M, Dieltjens E, Christiaens MR, Neven P, Geraerts I, Devoogdt N. (2015). Effectiveness of postoperative physical therapy for upper-limb impairments after breast cancer treatment: a systematic review. Archives of Physical Medicine and Rehabilitation. 96(6):1140-53. doi: 10.1016/j.apmr.2015.01.006. Epub 2015 Jan 13.
McNeely ML, Campbell K, Ospina M, Rowe BH, Dabbs K, Klassen TP, Mackey J, Courneya K. (2010). Exercise interventions for upper-limb dysfunction due to breast cancer treatment. The Cochrane Database System of Reviews. (6):CD005211. doi: 10.1002/14651858.CD005211.pub2.
 This week we are proud to feature Christy Ciesla, PT, DPT, PRPC! She just earned her Pelvic Rehabilitation Practitioner Certification, and was kind enough to share some of her thoughts with the Pelvic Rehab Report. You can read the interview below. Congratulations to Christy and all the other PRPC practitioners!
This week we are proud to feature Christy Ciesla, PT, DPT, PRPC! She just earned her Pelvic Rehabilitation Practitioner Certification, and was kind enough to share some of her thoughts with the Pelvic Rehab Report. You can read the interview below. Congratulations to Christy and all the other PRPC practitioners!
Tell us about your clinical practice:
I am currently coordinating a Women and Men’s Health program at the Miriam Hospital (The Men’s Health Center and The Women’s Medicine Collaborative) in Rhode Island. We are fortunate to be a team of 5 skilled pelvic therapists and to work with the some of the best physicians and surgeons in New England. We work with so many different patients. I am currently most excited about our involvement in a tremendous Cancer Survivorship Program offered here at the Women’s Medicine Collaborative.
How did you get involved in Pelvic Rehab?
I have always been actively involved in women’s issues, even as a college student, helping with programming for the Women’s Resource Center on campus. After I had my first son in 2003, I became very interested in working with pregnant and postpartum women, and the pelvic rehab involvement took off from there. I was sent my first male patient in 2008, and found that I enjoyed working with men just as much as working with women in this area.
What/who inspired you to become involved in pelvic rehabilitation?
I went to Elizabeth Noble’s OB/Gyn and Prenatal Exercise Courses in 2004. During the course, we talked quite a bit about birth and the pelvic floor. I left there fascinated with the field, and took my first pelvic floor course a couple of years later.
What patient population do you find most rewarding in treating and why?
I love treating all of my patients, but perhaps the most rewarding feeling is when I can help a cancer survivor SURVIVE their cancer. All too often, when the treatment ends, the patient is left to feel alone with all of the effects of chemo, radiation and surgical trauma. They have incontinence, pelvic pain, and sexual dysfunction, and feel lost. Being able to offer a light in the darkness to these people is the greatest gift that pelvic rehabilitation has given me.
If you could get a message out to physical therapists about pelvic rehabilitation what would it be?
You will never have more of a rewarding experience than you will when you help your patients pee, poop and have sex without dysfunction. I mean, really….what else is there to life?!
What has been your favorite Herman & Wallace Course and why?
PF 1 has still got to be my favorite. It was the most packed with great info, Holly was my instructor, and I was first introduced to the magical world of pelvic rehabilitation. I will never forget that experience.
What lesson have you learned from a Herman & Wallace instructor that has stayed with you?
One of the things that has been consistently conveyed in all of my courses with H&W is the importance of caring for, respecting, and honoring our patients for having the bravery to address these sensitive issues, and to share them with us. The coursework prepared me with the knowledge I needed to help my patients, but the amazing instructors also helped me be a better provider in other ways.
What motivated you to earn PRPC?
So far, I have taken 7 Herman and Wallace courses (8 including the PF 1 course that Holly did privately for my facility and I was able to assist with). It just seemed right to be certified through this wonderful institute. It is what I do every day, all day, and I felt that I needed these credentials to go further with my career in this field.
How does pelvic floor muscle function differ in women with symptoms of overactive bladder compared to symptomatic women? A study completed by Knight and colleagues included determining if pelvic floor muscle surface electromyography (EMG) and pelvic floor muscle (PFM) performance were different among these groups. Scores regarding anxiety, life stress, and quality of life were assessed. Symptoms of overactive bladder can include urinary urgency, frequency, nocturia, and leakage of urine. Subjects in this study had "dry" overactive bladder, meaning that the patients did not experience leakage associated with the urgency.
28 women with urinary urges and frequency were age-matched to 28 asymptomatic controls. Participants completed the Beck Anxiety Inventory, Pelvic Floor Distress Inventory, Pelvic Floor Impact Questionnaire, and the Recent Life Changes Questionnaire. Surface EMG was utilized to assess pelvic floor muscle function. Results of the study included that women with urinary urgency and frequency had significantly more anxiety than women in the control group. Surface EMG measures (pathway vaginal sensor was used with self-placement) were not significantly different for ability to contract or relax the PFM. Scores on the PFIQ and the RLCQ were significantly higher for women with overactive bladder. The authors conclude that, although a causative relationship could not be made between overactive bladder and anxiety, there exists a relationship between the two conditions.
Another interesting study which compared interventions of yoga versus mindfulness for women who have symptoms of urinary urge incontinence found that mindfulness-based stress reduction was effective for reducing urinary incontinence episodes whereas yoga was not. This study followed a pilot directed by the same primary investigator which showed similar positives results of mindfulness training on urinary urge incontinence.
What are the clinical questions we may draw from these research reports? Does anxiety cause urinary urgency and frequency, or does urinary urgency and frequency cause anxiety? We all have felt the intense stress of having to empty our bladders and not knowing where the nearest restroom (or freeway exit) is. We also know how the bladder and bowels are affected by stress- how many times did you visit the port-a-potty before that last 5K run? As is the case with many conditions with which our patients present, we may not know if one started the other, and most likely, the combination of issues resulted in dysfunction. Regardless, in our pelvic rehabilitation practices we have the tools to help patients learn about their anatomy, physiology, power in healing, and skills to affect urinary urgency and frequency.
The day my son was born, my daughter had not defecated for 5 days, and her pain was getting pretty intense. My husband and his mom took her to Seattle Children’s Hospital for help, and they suggested using Miralax and sent them away. When they got back to my hospital room, my daughter was straining so hard it looked like she was about to give birth! Being physical therapists, my husband and I massaged her little muscles and told her to take deep breaths, and eventually she did the deed, yet not without a heart-breaking struggle. Little did I know then there is actually research to back up our emergency, instinctual technique.
 Zivkovic et al (2012) performed a study regarding the use of diaphragmatic breathing exercises and retraining of the pelvic floor in children with dysfunctional voiding. They defined dysfunctional voiding as urinary incontinence, straining, weakened stream, feeling the bladder has not emptied, and increased EMG activity during the discharge of urine. Although this study focuses primarily on urinary issues, it also includes constipation in the treatment and outcomes. Forty-three patients between the ages of 5 and 13 with no neurological disorders were included in the study. The subjects underwent standard urotherapy (education on normal voiding habits, appropriate fluid intake, keeping a voiding chart, and posture while voiding) in addition to pelvic floor muscle retraining and diaphragmatic breathing exercises. The results showed 100% of patients were cured of their constipation, 83% were cured of urinary incontinence, and 66% were cured of nocturnal enuresis.
Zivkovic et al (2012) performed a study regarding the use of diaphragmatic breathing exercises and retraining of the pelvic floor in children with dysfunctional voiding. They defined dysfunctional voiding as urinary incontinence, straining, weakened stream, feeling the bladder has not emptied, and increased EMG activity during the discharge of urine. Although this study focuses primarily on urinary issues, it also includes constipation in the treatment and outcomes. Forty-three patients between the ages of 5 and 13 with no neurological disorders were included in the study. The subjects underwent standard urotherapy (education on normal voiding habits, appropriate fluid intake, keeping a voiding chart, and posture while voiding) in addition to pelvic floor muscle retraining and diaphragmatic breathing exercises. The results showed 100% of patients were cured of their constipation, 83% were cured of urinary incontinence, and 66% were cured of nocturnal enuresis.
More recently, Farahmand et al (2015) researched the effect of pelvic floor muscle exercise for functional constipation in the pediatric population. Stool withholding and delayed colonic transit are most often the causes for children having difficulty with bowel movements. Behavioral modifications combined with laxatives still left 30% of children symptomatic. Forty children between the ages of 4 and 18 performed pelvic floor muscle exercise sessions at home, two times per day for 8 weeks. The children walked for 5 minutes in a semi-sitting (squatting) position while being supervised by parents. The patients increased the exercise duration 5 minutes per week for the first two weeks and stayed the same over the next six weeks. The results showed 90% of patients reported overall improvement of symptoms. Defecation frequency, fecal consistency and decrease in fecal diameter were all found to be significantly improved. Although not statistically significant, the number of patients with stool withholding, fecal impaction, fecal incontinence, and painful defecation decreased as well.
Parents may not be as aware of their children’s voiding habits once they are cleared from diaper duty after successful potty training occurs. To help prevent issues, keep the basics covered, such as making sure children are exercising regularly or being active, drinking plenty of fluids, and eating a diet that includes plenty of fiber. My daughter was only 26 months old when her constipation became a problem, so the stool softener was ultimately the way to go at that time, and everything worked out naturally over the next year. If she were still experiencing functional constipation, I would be delighted to know teaching her pelvic floor exercises (relaxation being the key aspect) and diaphragmatic breathing could be effective for keeping my crazy little girl regular in at least that area of her life!
Zivkovic V, Lazovic M, Vlajkovic M, Slavkovic A, Dimitrijevic L, Stankovic I, Vacic N. (2012). Diaphragmatic breathing exercises and pelvic floor retraining in children with dysfunctional voiding. European J ournal of Physical Rehabilitation Medicine. 48(3):413-21. Epub 2012 Jun 5.
Farahmand, F., Abedi, A., Esmaeili-dooki, M. R., Jalilian, R., & Tabari, S. M. (2015). Pelvic Floor Muscle Exercise for Paediatric Functional Constipation.Journal of Clinical and Diagnostic Research : JCDR, 9(6), SC16–SC17. http://doi.org/10.7860/JCDR/2015/12726.6036
Milk duct blockage is a common condition in breast feeding mother’s that can cause a multitude of problems including painful breasts, mastitis, breast abscess, decreased milk supply, breast feeding cessation, and poor confidence with decreased quality of life. A recent study in 2015 in The Journal of Women’s Health Physical Therapy1, showed that physical therapy (PT) maybe a helpful treatment for the lactating mother experiencing milk duct blockage when conservative measures have failed. Common conservative measures typically recommended are self-massage, heat, and regular feedings. The World Health Association, the American Academy of Pediatrics, and Academy of Breast Feeding Medicine, all recommend breast feeding as the primary source for nutrition for infants. There are many benefits to both the mother, and the infant, when breast feeding is used as the primary source for nutrition in infants. Having blocked milk ducts make it difficult and painful to breast feed and can lead to poor confidence for the mother and a frustrated baby as the milk supply could be reduced or inadequate. The primary health concern for blocked milk ducts is mastitis. Mastitis is defined as an infection of breast tissue leading to pain, redness, swelling, and warmth, possibly fever and chills and can lead to early cessation of breast feeding.
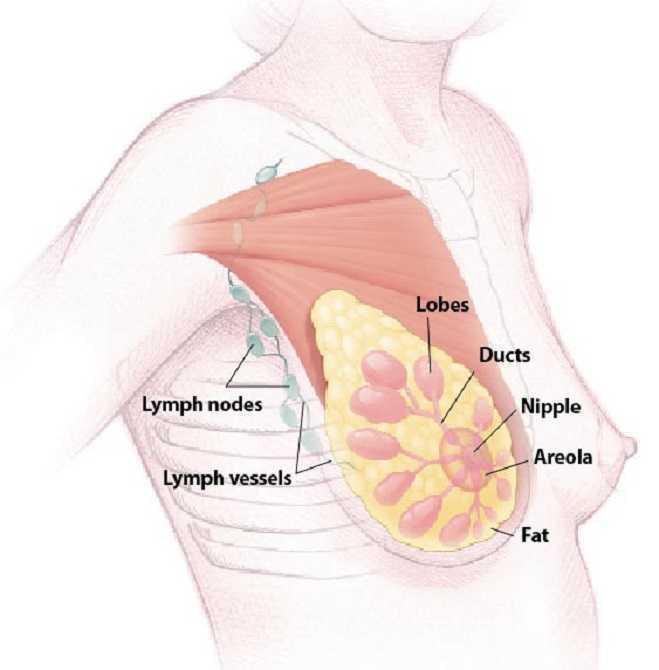 A blocked milk duct is not a typical referral to PT, however, this study outlined a protocol used for 30 patients with one or more blocked milk ducts that were referred to PT by a qualified lactation consultant. This study was a prospective pre/posttest cohort study. As an outcome measure, this study utilized a Visual Analog Scale (VAS) for 3 descriptive areas: pain, difficulty breast feeding, and confidence in independently nursing before and after treatment. The treatment protocol included moist heat, thermal ultrasound, specific manual therapy techniques, and patient education for treatment and prevention of the blockage(s). The thermal ultrasound and moist heating provided the recommend amount of heat to relax tissue around the blockage. Ultrasound also provided a mechanical effect that assists in the breaking up of the clog and increased pain threshold for the patient to improve tolerance to the manual clearing techniques. Next, the specific manual therapy was provided to directly unclog the blockage(s), and lastly the education provided was to help the patient identify and clear future blockages to prevent recurrence. 22 of the 30 patients were seen for 1-2 visits, 6 were seen for 3-4 visits, and none of the mother’s condition progressed to infective mastitis or developed breast abscess’s.
A blocked milk duct is not a typical referral to PT, however, this study outlined a protocol used for 30 patients with one or more blocked milk ducts that were referred to PT by a qualified lactation consultant. This study was a prospective pre/posttest cohort study. As an outcome measure, this study utilized a Visual Analog Scale (VAS) for 3 descriptive areas: pain, difficulty breast feeding, and confidence in independently nursing before and after treatment. The treatment protocol included moist heat, thermal ultrasound, specific manual therapy techniques, and patient education for treatment and prevention of the blockage(s). The thermal ultrasound and moist heating provided the recommend amount of heat to relax tissue around the blockage. Ultrasound also provided a mechanical effect that assists in the breaking up of the clog and increased pain threshold for the patient to improve tolerance to the manual clearing techniques. Next, the specific manual therapy was provided to directly unclog the blockage(s), and lastly the education provided was to help the patient identify and clear future blockages to prevent recurrence. 22 of the 30 patients were seen for 1-2 visits, 6 were seen for 3-4 visits, and none of the mother’s condition progressed to infective mastitis or developed breast abscess’s.
The results of the study showed the protocol used was helpful to ease pain, reduce difficulty with breast feeding, and improve confidence with independent breast feeding for lactating women that participated in the study. Although treatment of blocked milk ducts in lactating mothers is not a common PT referral, this study shows that PT may be one more helpful treatment for a patient experiencing this problem that is not responding to traditional conservative treatment. Since breast feeding is important to both mother and infant and is the primary recommended source for infant nutrition, it is important that a lactating mother receives quick, effective treatment for blocked milk ducts to prevent onset of mastitis and breast abscess that lead to early cessation of breast feeding. The cited study recommends that women who suspect a blocked milk duct or are having problems with breast feeding always seek care from a certified lactation consultant first, and that PT may be a referral that is made.
Cooper, B. B., & Kowalsky, D. S. (2015). Physical Therapy Intervention for Treatment of Blocked Milk Ducts in Lactating Women. Journal of Women’s Health Physical Therapy, 39(3), 115-126.
Postpartum lower extremity nerve injuries is an important topic that we have previously discussed on the blog. A review article(O'Neal 2015) published in the International Anesthesia Research Society journal discusses maternal neurological complications following childbirth. This article, designed to help anesthesiologists identify the symptoms of a neuropathy, discusses diagnosis, management, and treatment. With the incidence of obstetric neuropathy in the postpartum period estimated at 1%, most of the nerve dysfunction is related to compression injuries. Symptoms may include, but are not limited to, lower extremity pain, weakness, numbness, or bowel and bladder dysfunction. Neuraxial anesthesia can also occur, with issues such as epidural hematoma or an epidural abscess. Risk factors are described in the article as having a prolonged second stage of labor, instrumented delivery, being of short stature and nulliparity (delivering for the first time.)
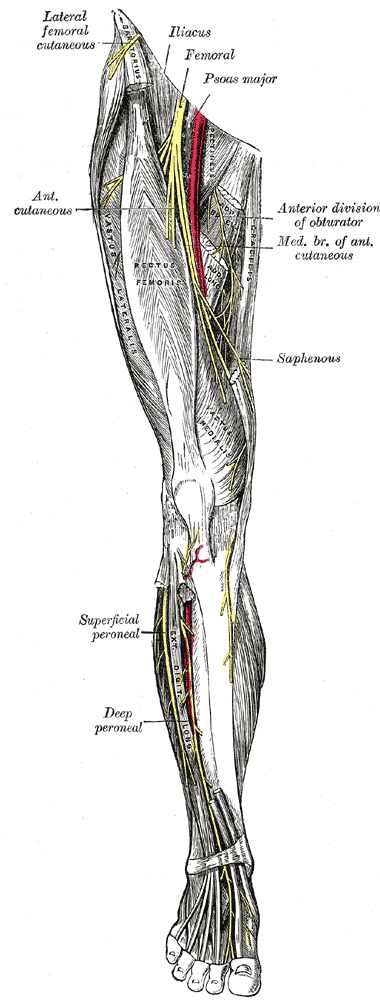 Clinical pearls listed in the article include the following information that may be helpful in understanding a patient’s condition:
Clinical pearls listed in the article include the following information that may be helpful in understanding a patient’s condition:
- intramedullary spinal cord syndromes (inside the spinal cord) are usually painless, whereas the peripheral nerve syndromes (involving the spinal nerve roots, plexus, and single nerves) usually cause pain
- bowel and bladder dysfunction often occurs early in the case of conus medullaris and late in the event of cauda equina syndrome
- cauda equina syndrome often causes polyradicular pain, leg weakness, numbness, and deep tendon reflex changes and involves multiple roots
- conus medullaris syndrome is not painful and causes saddle anesthesia and lack of significant sensory and motor symptoms in the lower extremities
In relation to prevention of neuropathies, the authors suggest that women who have diabetes or who have a preexisting neuropathy should be given extra attention. This may include protective padding during labor and delivery as well as frequent repositioning. Pelvic rehabilitation providers are a key player in the arena of birthing. Caring for women and educating them about peripartum issues is critical to helping women both prevent and heal from challenges encountered in relation to pregnancy and childbirth. If you would like to learn more about the topic of peripartum nerve dysfunctions, as well as many other special topics, please join us for the continuing education course Care of the Postpartum Patient. Your next opportunity to take this course will be in Seattle next March!
O’Neal, M. A., Chang, L. Y., & Salajegheh, M. K. (2015). Postpartum Spinal Cord, Root, Plexus and Peripheral Nerve Injuries Involving the Lower Extremities: A Practical Approach. Anesthesia & Analgesia, 120(1), 141-148.