II. Labor and Delivery
The Baby Always Has a Different Plan
Towards the end of my pregnancy, my doctor ordered an ultrasound to make sure the baby was growing appropriately. This was precautionary as the baby had measured small the last couple appointments. The ultrasound gave us some important information. Baby K was growing appropriately, however, she was breech. At this point, she should have already flipped into the cephalic (head down) position, and it was unlikely that she would turn further along in my pregnancy. I knew what this meant… “C-section” (cesarean). Like so many women before me, this was not what I wanted for my birth plan. Having a planned cesarean had not really crossed my mind. I figured it would only be some kind of emergency that would result in this outcome. Instantly I thought of all the patients I have treated over the years who had cesarean delivery. I thought of abdominal adhesions and scar tissue mobility work that would need to be done postpartum. Naturally, as a physical therapist, I also thought of all the mobility challenges this would bring after baby. Having a cesarean would change my post-partum recovery; I would need more help with lifting, carrying, and we have so many stairs in our house! I know this may sound crazy… but what saddened me the most about cesarean delivery was that I was not going to experience what labor felt like. I felt cheated, in a weird way, I was looking forward to it, almost like a rite of passage. I wanted to analyze labor and delivery from a patient’s standpoint, not just as a therapist. I thought it would help me relate to patients and friends who have experienced labor. All that being said, a scheduled C-section was happening unless that baby miraculously flipped.
 My doctor suggested a version, which is a procedure where your doctor tries to manually turn your baby using an external technique. I had heard it is painful, but I pride myself on being a pretty tough woman who has dealt with some pain, I can do this! Needless to say, the version was painful… Very painful! As a matter of fact, the most painful procedure I have ever encountered. After trying about four times to turn the baby, my doctor asked me if we should try one more time. Although I was miserable, I asked if they thought the baby was close to being in the right position. The looks on my husband’s and doctor’s faces told me that she hadn’t moved at all. We gave it one more try, but that stubborn baby really liked the spot she was in. The plan was to proceed with the scheduled C-section at 39 weeks, unless I went into labor first, then it would be an emergency cesarean delivery.
My doctor suggested a version, which is a procedure where your doctor tries to manually turn your baby using an external technique. I had heard it is painful, but I pride myself on being a pretty tough woman who has dealt with some pain, I can do this! Needless to say, the version was painful… Very painful! As a matter of fact, the most painful procedure I have ever encountered. After trying about four times to turn the baby, my doctor asked me if we should try one more time. Although I was miserable, I asked if they thought the baby was close to being in the right position. The looks on my husband’s and doctor’s faces told me that she hadn’t moved at all. We gave it one more try, but that stubborn baby really liked the spot she was in. The plan was to proceed with the scheduled C-section at 39 weeks, unless I went into labor first, then it would be an emergency cesarean delivery.
At 39 weeks, I woke up the morning of the planned cesarean and thought, “it’s a good day to have a baby”. I was excited to finally meet this little princess, but a little nervous about the cesarean delivery. I was trying not to think about what was going to happen to my abdomen and uterus. I was hoping Baby K would handle all of this safely, and she would be well. My plan for the procedure was distraction, not to think about what was happening, as I knew too much. Sometimes ignorance is bliss. I did not want to think of every unfortunate story I had heard about “spinals”, and “cesareans gone wrong”, so I kept telling myself to trust my doctors and relax. After all, this is what they do every day, and they are good at it. I wasn’t the biggest fan of the numbness and tingling I felt in my legs, as well as the lack of motor control in the lower half of my body once they administered the spinal, but it did the trick.
All I felt during the caesarean was just some tugging on my abdomen as the doctor worked to get baby out and complete the procedure. Luckily, it was all happening behind a partition while my husband held my hand and we told jokes to relieve our nerves. All of a sudden, there was a loud cry, and I felt instant relief. It was my baby, and she had healthy lungs! My doctor popped around the screen and showed me my beautiful brown-haired baby. Next, my husband and the nurses cut the cord and took care of baby. Once she was cleared and safe, they plopped her on my chest. Like a moth to a flame, that baby wriggled herself right onto my breast. It was the purest form of instinct I have ever witnessed. How did that little baby that just entered this world have the innate knowledge to nourish, and the strength to find her food source. It was amazing! Overall, no matter how much you research and plan for labor and delivery, it likely won’t turn out how you plan it. The positive is that our bodies have been delivering babies forever, so trust in your body, and trust in those around you helping with the delivery. The labor and delivery experience is innate.
The following is the first in a three-part blog series which chronicles the peripartum journey of Rachel Kilgore.
I. Pregnancy
 In April, I had my first child, a sweet and healthy baby girl. Reflecting on the last year, what a ride! I have had many of my friends, family members, patients, and acquaintances discuss the journey and challenges of motherhood with me, however, experiencing it first hand was a memorable voyage. I thought I was very prepared and knew what I was getting into, but as usual, nothing compares to first-hand knowledge and experience. From an academic standpoint, I had done my research on everything from conception, what to expect each trimester of pregnancy, and reviewed the many options for labor and delivery. I even was lucky enough to assist in the Herman and Wallace Care for the Post-Partum Patient course with Holly Tanner while I was pregnant! As a practitioner, I love treating pregnant and post-partum patients, it is one of my favorite populations to treat. I love helping these strong, motivated women with pain relief and to teach them management skills to adapt to a new lifestyle and a changed body that has unique musculoskeletal needs.
In April, I had my first child, a sweet and healthy baby girl. Reflecting on the last year, what a ride! I have had many of my friends, family members, patients, and acquaintances discuss the journey and challenges of motherhood with me, however, experiencing it first hand was a memorable voyage. I thought I was very prepared and knew what I was getting into, but as usual, nothing compares to first-hand knowledge and experience. From an academic standpoint, I had done my research on everything from conception, what to expect each trimester of pregnancy, and reviewed the many options for labor and delivery. I even was lucky enough to assist in the Herman and Wallace Care for the Post-Partum Patient course with Holly Tanner while I was pregnant! As a practitioner, I love treating pregnant and post-partum patients, it is one of my favorite populations to treat. I love helping these strong, motivated women with pain relief and to teach them management skills to adapt to a new lifestyle and a changed body that has unique musculoskeletal needs.
First Trimester: Information, Nausea, and Fatigue
I had always had a preconceived notion that I would exercise diligently and eat super healthy through my pregnancy. After all, that was how my lifestyle was before pregnancy, why should it change? That lasted about 6 weeks, until 24-hour episodes of nausea and vomiting overwhelmed me, which continued until the start of the second trimester. I basically just tried to make it through the day without vomiting at work, and would go straight to bed whenever I had the chance. I even had to miss several days of work! I thought it was termed “morning sickness” implying that it went away after morning, but apparently it should be renamed to “forever nausea” as that is what it felt like at the time. Because of the nausea, I wanted nothing to do with food, which in turn lead to constant concern about the baby not getting enough nourishment. Of course, my regular activity levels plummeted. In addition to nausea was constant fear of miscarriage and whether my regular activities were somehow harmful to my baby. Instead of ice cream and pickles, I craved information. What should I be doing, and what should I not be doing?
Second Trimester: Return of Energy, Excitement, Planning and Doing!
When the first day of the second trimester hit, the nausea just went away. I was ecstatic! I got my energy back and was finally enjoying the pregnancy again! I was able to exercise regularly and eat healthy, two of my favorite things. Everything was going well, and it was time to start figuring out this whole baby thing. Luckily, most of my friends are mothers themselves, and they helped guide me. They directed me to great resources to satisfy my quest for knowledge about everything I needed to know for pregnancy, labor delivery, and the baby itself. They helped me decipher what all these baby products were, and what do you actually need. All the fun stuff was happening! We painted the baby’s room, ordered furniture, and planned a baby shower.
Third trimester: Waiting, Exhaustion, Heart Burn, and Reduced Mobility
Everything that happens to my patients happens to me. Third trimester was when I started to really “feel pregnant”. Daily mobility became challenging. I never realized how many times in a workday I show patients correct lifting mechanics or how often I set things on the ground or pick up weights. I started to dread every time I had to pick up something. At work, I would drop my pen on the ground so many times, and why had I never noticed that I did it so often? Luckily, I used my “physical therapy knowledge and skills” and did things I tell my pregnant patients to do; the results were minimal problems with musculoskeletal pain. Techniques such as: Using proper mechanics throughout my day, pulling in my core, and wearing a maternity support if my back was hurting a little. I never really developed severe back pain as is the case for many pregnant women. I completed hip and trunk exercises I usually give my pregnant patients and found they were easy to do and made me feel better... shocking right? Of course I was doing my kegels too! While my musculoskeletal system was doing well, my gastrointestinal system was not. I had never really had heart burn before, but now had it constantly, and found it to be very frustrating and depressing. I love cooking and eating but neither are enjoyable when you have heartburn. The heartburn was so bad it would wake me up every night coughing and chocking on my own acid reflux. Between lack of sleep, heartburn, and reduced mobility, I was getting pretty excited to be done with pregnancy and to finally meet “Baby K” as we had begun calling her. Overall, being pregnant was a very informative experience for me as a person and as a clinician. I often hear my patients tell me of their uncomfortable symptoms during pregnancy involving their musculoskeletal and gastrointestinal systems, however, now I empathize on another level.
Susannah Haarmann, PT, CLT, WCS is the author and instructor of Physical Therapy Treatment for the Breast Oncology Patient. Join her this September 24-25 in Stockton, CA to learn about the various diagnostic tests, medical and surgical interventions to provide appropriate and optimal therapeutic interventions for breast cancer patients.
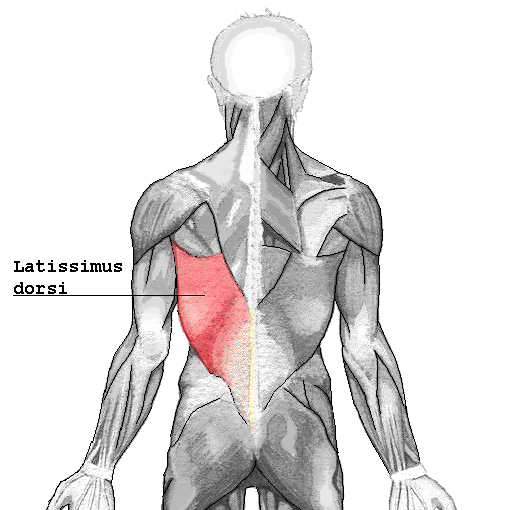 I turned to the literature and found prominent articles discussing breast reconstruction and giving minimal consequence to shoulder function after resection of the latissimus dorsi muscle. As a physical therapist, this left me in a quandary, “Really? Harvesting a portion of the broadest muscle of the back then threading it through the axilla to recreate the breast mound won’t have an impact on shoulder function or back pain? Impressive!” However, this did not correlate with my clinical findings. Often, scapulohumeral rhythm was altered, range of motion restricted and activities limited due to pain and fatigue. Scrutinizing the literature, I found that those articles were mostly unsubstantiated. Here is a quick summary of two systematic reviews published in 2014 addressing what the research really found pertaining to shoulder function after ‘lat flap’ reconstruction:
I turned to the literature and found prominent articles discussing breast reconstruction and giving minimal consequence to shoulder function after resection of the latissimus dorsi muscle. As a physical therapist, this left me in a quandary, “Really? Harvesting a portion of the broadest muscle of the back then threading it through the axilla to recreate the breast mound won’t have an impact on shoulder function or back pain? Impressive!” However, this did not correlate with my clinical findings. Often, scapulohumeral rhythm was altered, range of motion restricted and activities limited due to pain and fatigue. Scrutinizing the literature, I found that those articles were mostly unsubstantiated. Here is a quick summary of two systematic reviews published in 2014 addressing what the research really found pertaining to shoulder function after ‘lat flap’ reconstruction:
Patient impressions:
- Reported incidence of overall functional impairment is 41%. 8
- Overhead activities, lifting and pushing objects and high-level activities such as sport and housework were the most cumbersome. 1,7
- Subjective deficits did not resolve based on length of follow-up. 1
Strength:
- Greatest deficits are noted with reconstruction on the dominant side. 4
- Extension of the shoulder is the most common strength deficit followed by adduction then internal rotation. 8
- Objective strength deficits typically resolved within a year. 8,9
- Rehab should be ordered pro-actively. 4
Range of Motion:
- Active flexion is the most common restriction followed by abduction. 8
- Rarely were these restrictions severe. 5,6
- Restrictions were greatest post-operatively likely due to alterations in shoulder biomechanics, scar formation and post-operative pain.
- Discrepancies were found regarding resolution of range of motion without rehab. 5,8
- No clinically significant functional morbidity was found when therapy was provided from post-op day one. 2,3
Other reported complications that may impact function:
- Taratino, Banic and Fischer noted that capsular contracture was the most significant and recurrent complication in their study.10
- 50% reported post-operative numbness and tightness.1
- Scar tissue adhesions were associated with functional limitations.2,3
In conclusion, is it feasible to say that the latissimus dorsi muscle bears little consequence to function after reconstruction? I’m going to trust what the researchers performing the systematic reviews say:
- Physicians and researchers Lee and Mun state the following; “over 20 percent of the patients undergoing latissimus dorsi muscle transfer suffered from considerable disability…7% of patients changed their job postoperatively. These results suggest that considerable discomfort, even to the extent of limitation on daily activity, can be developed after latissimus dorsi muscle harvest, as opposed to the previous assumption that latissimus dorsi muscle harvest may not lead to serious disability” .8
- Smith does give merit to the fact that most strength deficits resolve within 6 to 12 months due to other muscles compensating for function, however, she states “standardization of physical therapy protocols is imperative as it appears to have a measurable positive impact.” Immediately after this statement she remarks that physical therapy is rarely included in the physician’s plan of care.9
I guess it is time we start talking to our surgical oncologists and plastic surgeons.
1. Adams, Jr., W., Lipschitz, A., Ansari, M., Kenkel, J., & Rohrich, R. J. (2004). Functional donor site morbidity following LD muscle flap transfer. Annals of Plastic Surgery, 53(1), 6–11.
2. de Oliveira, R., Nascimento, S., Derchain, S. & Sarian, L. (2013). Immediate breast reconstruction with a latissimus dorsi flap has no detrimental effects on shoulder motion or postsurgical complications up to 1 year after surgery. Plas¬tic and Reconstructive Surgery, 131(5), 673e–680e.
3. de Oliveira, R. R., Pinto e Silva, M. P., Costa Gurgel, M. S., Pas¬tori-Filho, L., & Sarian, L. O. (2010). Immediate breast re¬construction with transverse latissimus dorsi flap does not affect the short-term recovery of shoulder range of motion after mastectomy. Annals of Plastic Surgery, 64(4), 402– 408.
4. Forthomme, B., Heymans, O., Jacquemin, D., Klinkenberg, S., Hoff¬mann, S., Grandjean, F. X.,...Croisier, J. L. (2010). Shoulder function after latissimus dorsi transfer in breast reconstruc-tion. Clinical Physiology and Functional Imaging, 30, 406– 412.
5. Giordano, S., Kääriäinen, M., Alavaikko, J., Kaistila, T. & Kuok¬kanen, H. (2011). Latissimus dorsi free flap harvesting may affect the shoulder joint in long run. Scandinavian Journal of Surgery, 100, 202–207.
6. Hamdi, M., Decorte, T., Demuynck, M., Defrene, B., Fredricks, A., VanMaele, G.,...Monstrey, S. (2008). Shoulder func¬tion after harvesting a thoracodorsal artery perforator flap. Plastic and Reconstructive Surgery, 122(4), 1111–1117.
7. Koh, C. E., & Morrison, W. A. (2009). Functional impairment af¬ter latissimus dorsi flap. Australian Journal of Surgery, 79, 42–47. http://dx.doi.org/10.1111/j.1445-2197.2008.04797.x
8. Lee, K.T., Mun, G.H., (2014).A systematic review of functional donor-site morbidity after latissimus dorsi muscle transfer, Plast. Reconstr. Surg. 134: 303.
9. Smith, S., (2014). Functional morbidity following latissimus dorsi flap breast reconstruction. J Adv Pract Oncol, 5, 181–187.
10. Tarantino, I., Banic, A., & Fischer, T. (2006). Evaluation of late results in breast reconstruction by latissimus dorsi flap and prosthesis implantation. Plastic and Reconstructive Surgery, 117(5), 1387–1394.
Nancy Cullinane PT, MHS, WCS is today's guest blogger. Nancy has been practicing pelvic rehabilitation since 1994 and she is eager to share her knowledge with the medical community at large. Thank you, Nancy, for contributing this excellent article!
Clinically valid research on the efficacy and safety of therapeutic exercise and activities for individuals with osteoporosis or vertebral fractures is scarce, posing barriers for health care providers and patients seeking to utilize exercise as a means to improve function or reduce fracture risk1,2. However, what evidence does exist strongly supports the use of exercise for the treatment of low Bone Mineral Density (BMD), thoracic kyphosis, and fall risk reduction, three themes that connect repeatedly in the body of literature addressing osteoporosis intervention.
 Sinaki et al3 reported that osteoporotic women who participated in a prone back extensor strength exercise routine for 2 years experienced vertebral compression fracture at a 1% rate, while a control group experienced fracture rates of 4%. Back strength was significantly higher in the exercise group and at 10 years, the exercise group had lost 16% of their baseline strength, while the control group had lost 27%. In another study, Hongo correlated decreased back muscle strength with an increased thoracic kyphosis, which is associated with more fractures and less quality of life. Greater spine strength correlated to greater BMD4. Likewise, Mika reported that kyphosis deformity was more related to muscle weakness than to reduced BMD5. While strength is clearly a priority in choosing therapeutic exercise for this population, fall and fracture prevention is a critical component of treatment for them as well. Liu-Ambrose identified quadricep muscle weakness and balance deficit statistically more likely in an osteoporotic group versus non osteoporotics6. In a different study, Liu-Ambrose demonstrated exercise-induced reductions in fall risk that were maintained in older women following three different types of exercise over a six month timeframe. Fall risk was 43% lower in a resistance-exercise training group; 40% lower in a balance training exercise group, and 37% less in a general stretching exercise group7.
Sinaki et al3 reported that osteoporotic women who participated in a prone back extensor strength exercise routine for 2 years experienced vertebral compression fracture at a 1% rate, while a control group experienced fracture rates of 4%. Back strength was significantly higher in the exercise group and at 10 years, the exercise group had lost 16% of their baseline strength, while the control group had lost 27%. In another study, Hongo correlated decreased back muscle strength with an increased thoracic kyphosis, which is associated with more fractures and less quality of life. Greater spine strength correlated to greater BMD4. Likewise, Mika reported that kyphosis deformity was more related to muscle weakness than to reduced BMD5. While strength is clearly a priority in choosing therapeutic exercise for this population, fall and fracture prevention is a critical component of treatment for them as well. Liu-Ambrose identified quadricep muscle weakness and balance deficit statistically more likely in an osteoporotic group versus non osteoporotics6. In a different study, Liu-Ambrose demonstrated exercise-induced reductions in fall risk that were maintained in older women following three different types of exercise over a six month timeframe. Fall risk was 43% lower in a resistance-exercise training group; 40% lower in a balance training exercise group, and 37% less in a general stretching exercise group7.
These studies allow us to unequivocally conclude that spinal extensor strengthening and therapeutic activities aimed at improving balance and decreasing fall risk are tantamount as therapeutic interventions for osteoporosis. But postural education/modification and weight bearing activities aimed at stimulating osteoblast production intended to improve BMD are a reasonable component of an osteoporosis treatment plan, despite the lack of concrete evidence for them. Nutrition and mineral supplementation with calcium and vitamin D have been shown to reduce morbidities, and hence we should incorporate this education into our treatment plans as well8, 9. Studies on the efficacy of vibration platforms hold promise, but thus far, have not been substantiated as an evidence-based intervention to improve BMD.
Too Fit To Fracture: outcomes of a Delphi consensus process on physical activity and exercise recommendations for adults with osteoporosis with or without vertebral fractures1,2 is a multiple-part publication in the journal Osteoporosis International, based upon an international consensus process by expert researchers and clinicians in the osteoporosis field. These publications include exercise and physical activity recommendations for individuals with osteoporosis based upon a separation of patients into to three groups: osteoporosis based on BMD without fracture; osteoporosis with one vertebral fracture; and osteoporosis with multiple spine fractures, hyperkyphosis and pain. This group of experts emphasize the importance of teaching safe performance of ADLs with respect to bodymechanics as a priority to accompany strength, balance, fall & fracture prevention, nutrition and pharmacotherapy management. They promote establishment of an individualized program for each patient with adaptable variations of these concepts, with the most accommodation allotted for individuals with multiple vertebral compression fractures. An example of such an adaptation is altering prone back extensions such as those documented in the studies by Sinaki and Hongo, into supine shoulder presses, thus strengthening the back extensors in a less gravitationally demanding posture. Osteoporosis Canada has adapted the main concepts from these publications into a patient-friendly, instructional website with reproducible handouts at http://www.osteoporosis.ca/osteoporosis-and-you/too-fit-to-fracture/
A firm conclusion from the Too Fit to Fracture project is that higher quality outcomes studies are desperately needed to assist all healthcare providers in managing osteoporosis more effectively and comprehensively, and to do so prior to the onset of debilitating fractures that tend to produce serious comorbidities.
1. Giangregorio et al. Too Fit to Fracture: exercise recommendations for individuals with osteoporosis or osteoporotic vertebral fracture. Osteoporosis International. 2014; 25(3): 821-835
2. Giangregorio et al. Too Fit to Fracture: outcomes of a Delphi consensus process on physical activity and exercise recommendations for adults with osteoporosis with or without vertebral fracture. Osteoporosis International. 2015; 26(3):891-910
3. Sinaki et al. Stronger back muscles reduce the incidence of vertebral fractures: a prospective 10 year follow-up of postmenopausal women. Bone. 2002; 30: 836-841 4. Hongo et al. Effect of low-intensity back exercise on quality of life and back extensor strength in patients with osteoporosis; a randomized controlled trial.Osteoporosis International. 2007; 10: 1389-1395
5. Mika et al. Differences in thoracic kyphosis and in back muscle strength in women with bone loss due to osteoporosis. Spine. 2005; 30(2): 241-246
6. Liu-Ambrose et al. Older women with osteoporosis have increased postural sway and weaker quadriceps strength than counterparts with normal bone mass: overlooked determinants of fracture risk? J Gerontology, Series A Biolog Sci Med Sci. 2003; 58(9): M862-866
7. Liu-Ambrose et al. The beneficial effects of group-based exercise on fall risk profile and physical activity persist 1 year post intervention in older women with low bone mass: follow-up after withdrawal of exercise. J Am Geriat Soc. 2005; 53 (10): 1767-1773
8. Ensrud et al. Weight change and fractures in older women: study of osteoporotic fractures research group. Archives Int Med. 1997; 157 (8): 857-863
9. Kemmler et al. Exercise effects on fitness and bone mineral density in early postmenopausal women: 1-year EFOPS results. Med and Sci in Sports Ex. 2002; 34 (12): 2115-2123
In manual therapy training, we do not learn just one position to mobilize a joint, so why should pelvic floor muscle training be limited by the standard training methods? There is almost always at least one patient in the clinic that fails to respond to the “normal” treatment and requires a twist on conventional therapy to get over a dysfunction. Thankfully, classes like “Integrative Techniques for Pelvic Floor and Core Function” provide clinicians with the extra tools that might help even just one patient with lingering symptoms.
 In 2014, Tenfelde and Janusek considered yoga as a treatment for urge urinary incontinence in women, referring to it as a “biobehavioral approach.” The article reviews the benefits of yoga as it relates to improving the quality of life of women with urge urinary incontinence. Yoga may improve sympatho-vagal balance, which would lower inflammation and possibly psychological stress; therefore, the authors suggested yoga can reduce the severity and distress of urge UI symptoms and their effect on daily living. Since patho-physiologic inflammation within the bladder is commonly found, being able to minimize that inflammation through yoga techniques that activate the efferent vagus nerve (which releases acetylcholine) could help decrease urge UI symptoms. The breathing aspect of yoga can reduce UI symptoms as it modulates neuro-endocrine stress response symptoms, thus reducing activation of psychological and physiologic stress and inflammation associated with stress. The authors concluded the mind-body approach of yoga still requires systematic evaluation regarding its effect on pelvic floor dysfunction but offers a promising method for affecting inflammatory pathways.
In 2014, Tenfelde and Janusek considered yoga as a treatment for urge urinary incontinence in women, referring to it as a “biobehavioral approach.” The article reviews the benefits of yoga as it relates to improving the quality of life of women with urge urinary incontinence. Yoga may improve sympatho-vagal balance, which would lower inflammation and possibly psychological stress; therefore, the authors suggested yoga can reduce the severity and distress of urge UI symptoms and their effect on daily living. Since patho-physiologic inflammation within the bladder is commonly found, being able to minimize that inflammation through yoga techniques that activate the efferent vagus nerve (which releases acetylcholine) could help decrease urge UI symptoms. The breathing aspect of yoga can reduce UI symptoms as it modulates neuro-endocrine stress response symptoms, thus reducing activation of psychological and physiologic stress and inflammation associated with stress. The authors concluded the mind-body approach of yoga still requires systematic evaluation regarding its effect on pelvic floor dysfunction but offers a promising method for affecting inflammatory pathways.
Pang and Ali (2015) focused on complementary and alternative medicine (CAM) treatments for interstitial cystitis (IC) and bladder pain syndrome (BPS). Since conventional therapy has not been definitely determined for the IC/BPS population, CAM has been increasingly used as an optional treatment. Two of the treatments under the CAM umbrella include yoga (mind-body therapy) and Qigong (an energy therapy). Yoga can contribute to IC/BPS symptom relief via mechanisms that relax the pelvic floor muscle. Actual yoga poses of benefit include frog pose, fish pose, half-shoulder stand and alternate nostril breathing. According to a systematic review, Qigong and Tai Chi can improve function, immunity, stress, and quality of life. Qigong has been effective in managing chronic pain, although not specifically evidenced with IC/BPS groups. Qigong has also been shown to reduce stress and anxiety and activate the brain region that suppresses pain. The CAM gives a multimodal approach for treating IC/BPS, and this has been recommended by the International Consultation on Incontinence Research Society.
Evidence is emerging in every area of treatment these days, so it is only a matter of time before randomized controlled trials regarding alternative treatment methods for the pelvic floor begin to fill pages of our professional journals. Yoga, Qigong, Tai Chi, biologically based therapies, manipulative and body-based approaches, and whole medical systems all offer safe, effective treatment options for the IC/BPS and urinary incontinence patient populations. The more we use these extra treatment tools and document the results, the more likely we will see clinical trials proving their efficacy.
Tenfelde, S and Janusek, L. (2014). Yoga: A Biobehavioral Approach to Reduce Symptom Distress in Women with Urge Urinary Incontinence. THE JOURNAL OF ALTERNATIVE AND COMPLEMENTARY MEDICINE. 20 (10), 737–742. http://doi.org/10.1089/acm.2013.0308
Pang, R., & Ali, A. (2015). The Chinese approach to complementary and alternative medicine treatment for interstitial cystitis/bladder pain syndrome.Translational Andrology and Urology, 4(6), 653–661. http://doi.org/10.3978/j.issn.2223-4683.2015.08.10
Dr. Dischiavi is a Herman & Wallace faculty member who authored and teaches Biomechanical Assessment of the Hip & Pelvis: Manual Movement Therapy and the Myofascial Sling System, available this August in Boston, MA.
STEM is an acronym for science, technology, engineering, and math. These fields are deeply intertwined and taking this approach could potentially be a way to facilitate the physical therapist’s appreciation of human movement.
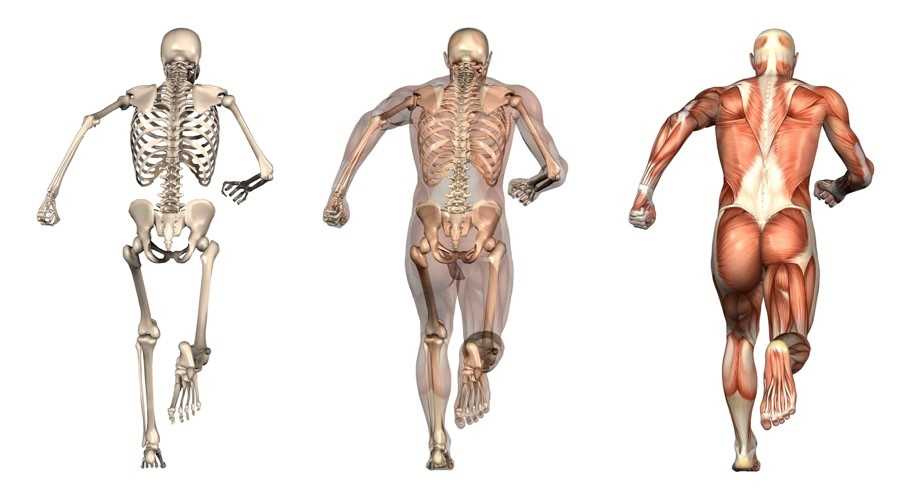
 Science: I would bet most physical therapists would agree that science is the cornerstone of our profession. It is time to look across all the landscapes of science to better understand the physical principles that govern movement. Biotensegrity is a great example of how science from a field such as cellular biology can help possibly explain how we maintain an erect posture when the rigid bony structure of our skeleton is only connected from bone to bone by soft tissues [1]. The brain and central nervous system regulates muscle tone, and it is resting muscle tone that give our bodies the ability to be upright. Without resting muscle tone, we would crumple to the ground as a heap of bones within a bag of skin. Since the CNS can either up or down regulate muscle tone, this allows us to create the rigidity we need to accomplish higher level movements such as sport, and then return to a resting state after the movements are performed (see running skeleton picture below). This theory of organismic support was bred within the scientific field of cellular biology, and can potentially be applied effectively to the human organism. As physical therapists, I agree we need to be skeptical of new ideas, but we also need to embrace the idea that the physical sciences have applied to nature for centuries, and it is possible these various scientific fields can help us unlock new ideas and allow us to look at things through a different lens.
Science: I would bet most physical therapists would agree that science is the cornerstone of our profession. It is time to look across all the landscapes of science to better understand the physical principles that govern movement. Biotensegrity is a great example of how science from a field such as cellular biology can help possibly explain how we maintain an erect posture when the rigid bony structure of our skeleton is only connected from bone to bone by soft tissues [1]. The brain and central nervous system regulates muscle tone, and it is resting muscle tone that give our bodies the ability to be upright. Without resting muscle tone, we would crumple to the ground as a heap of bones within a bag of skin. Since the CNS can either up or down regulate muscle tone, this allows us to create the rigidity we need to accomplish higher level movements such as sport, and then return to a resting state after the movements are performed (see running skeleton picture below). This theory of organismic support was bred within the scientific field of cellular biology, and can potentially be applied effectively to the human organism. As physical therapists, I agree we need to be skeptical of new ideas, but we also need to embrace the idea that the physical sciences have applied to nature for centuries, and it is possible these various scientific fields can help us unlock new ideas and allow us to look at things through a different lens.
 Technology: As not only a practicing physical therapist, but as a newly appointed assistant professor within a budding physical therapy program it is my duty to embrace evidence based practice. I believe without question, when evidence that is sound exists it should help direct patient care. It is also clear that our tests and measures that are currently being utilized to help develop new evidence are lacking, specifically with regard to human movement and sport performance.
Technology: As not only a practicing physical therapist, but as a newly appointed assistant professor within a budding physical therapy program it is my duty to embrace evidence based practice. I believe without question, when evidence that is sound exists it should help direct patient care. It is also clear that our tests and measures that are currently being utilized to help develop new evidence are lacking, specifically with regard to human movement and sport performance.
Sports performance is such a complex system (more on this later) we can’t expect to study things such as injury prevention at slow speeds utilizing maneuvers that aren’t even seen in the sport itself. Recently, Bahr [2] suggested that screening for sports injuries is pretty much a futile effort as he titled his article “Why screening tests to predict injury do not work - and probably never will…: a critical review.” Eventually technology will need to be developed that can measure high speed movement across multiple planes and ranges of motion, and essentially capture the complex spiraling that occurs with human movement and the bodies effort to attenuate ground reaction forces. This concept can be illustrated in the current work of Tak and Langhout [3] who have developed a novel approach to measure hip ROM in soccer players. They have essentially performed a thorough needs analysis of the kicking motion and determined that the classical method of measuring hip ROM doesn’t take into account the body’s need to spiral itself to gain the energy in the system needed to kick a ball [Fig 1]. This global understanding of the dynamic integration of the kinetic chain (which is covered in my hip course!) is what has led them to design this new method to measure hip ROM. Now, we will need technological advancements to capture, record, and measure these types of positions across three planes and at high speeds to establish the data that will eventually lead to evidence that will translate into sport. This is a great example of how clinical innovation sometimes precedes actual evidence to support its use. As William Blake was quoted as saying “what is now proven was once only imagined.”
 Engineering: Structural engineering should be included in every physical therapy education program. There are many basic structural engineering principles that directly apply to a physical therapists practice. For example, the principal of elastics is frequently discussed within structural engineering. Elastics describes to what extent deformation is proportional to the forces applied to a particular material. In physical therapy muscles are that particular material, muscles must have elasticity and extensibility, not flexibility! In elastics, a rubber band is often used as a simple example to explain this engineering concept.
Engineering: Structural engineering should be included in every physical therapy education program. There are many basic structural engineering principles that directly apply to a physical therapists practice. For example, the principal of elastics is frequently discussed within structural engineering. Elastics describes to what extent deformation is proportional to the forces applied to a particular material. In physical therapy muscles are that particular material, muscles must have elasticity and extensibility, not flexibility! In elastics, a rubber band is often used as a simple example to explain this engineering concept.
A rubber band will elongate and develop potential energy until release and then unleash kinetic energy. Our human movement system relies heavily on the principle of elastics. The rectus femoris is a two-joint muscle across the hip. During gait and running the rectus femoris is elongated as the hip moves into extension, this elongation builds its potential energy until the foot comes off the ground to initiate the swing phase, and the kinetic energy released in the system allows momentum to carry the lower extremity forward.
 I would add that possibly the twisting created by the contralateral counter trunk rotation and reciprocating arm and leg swing that accompanies the hip extension is what creates tension throughout the entire anterior chain, similar to why Tak and Langhout feel its important to take up all soft tissue slack three dimensionally to effectively measure hip ROM needed for a soccer kick. It is considering that the elasticity in the entire system (organism) is needed to create an efficient human movement, which is kicking a ball in this example. When the body utilizes passive lengthening of muscle chains, as in elastics, it allows the body to move more efficiently. This is described by Chu [4] who reports that in the pitching motion maximizing force development in the large muscles of the core and legs produces more than 51%- 55% of the kinetic energy that is transferred to the hand [Fig 2]. The thoracolumbar fascia is involved in the kinetic chain during throwing activities and connects the lower limbs through the gluteus maximus muscle to the upper limbs through the latissimus dorsi. This idea of a dynamic integration of the kinetic chain is the main concept of the exercise portion of my hip course!
I would add that possibly the twisting created by the contralateral counter trunk rotation and reciprocating arm and leg swing that accompanies the hip extension is what creates tension throughout the entire anterior chain, similar to why Tak and Langhout feel its important to take up all soft tissue slack three dimensionally to effectively measure hip ROM needed for a soccer kick. It is considering that the elasticity in the entire system (organism) is needed to create an efficient human movement, which is kicking a ball in this example. When the body utilizes passive lengthening of muscle chains, as in elastics, it allows the body to move more efficiently. This is described by Chu [4] who reports that in the pitching motion maximizing force development in the large muscles of the core and legs produces more than 51%- 55% of the kinetic energy that is transferred to the hand [Fig 2]. The thoracolumbar fascia is involved in the kinetic chain during throwing activities and connects the lower limbs through the gluteus maximus muscle to the upper limbs through the latissimus dorsi. This idea of a dynamic integration of the kinetic chain is the main concept of the exercise portion of my hip course!
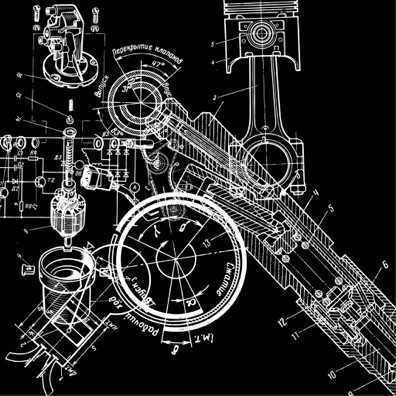
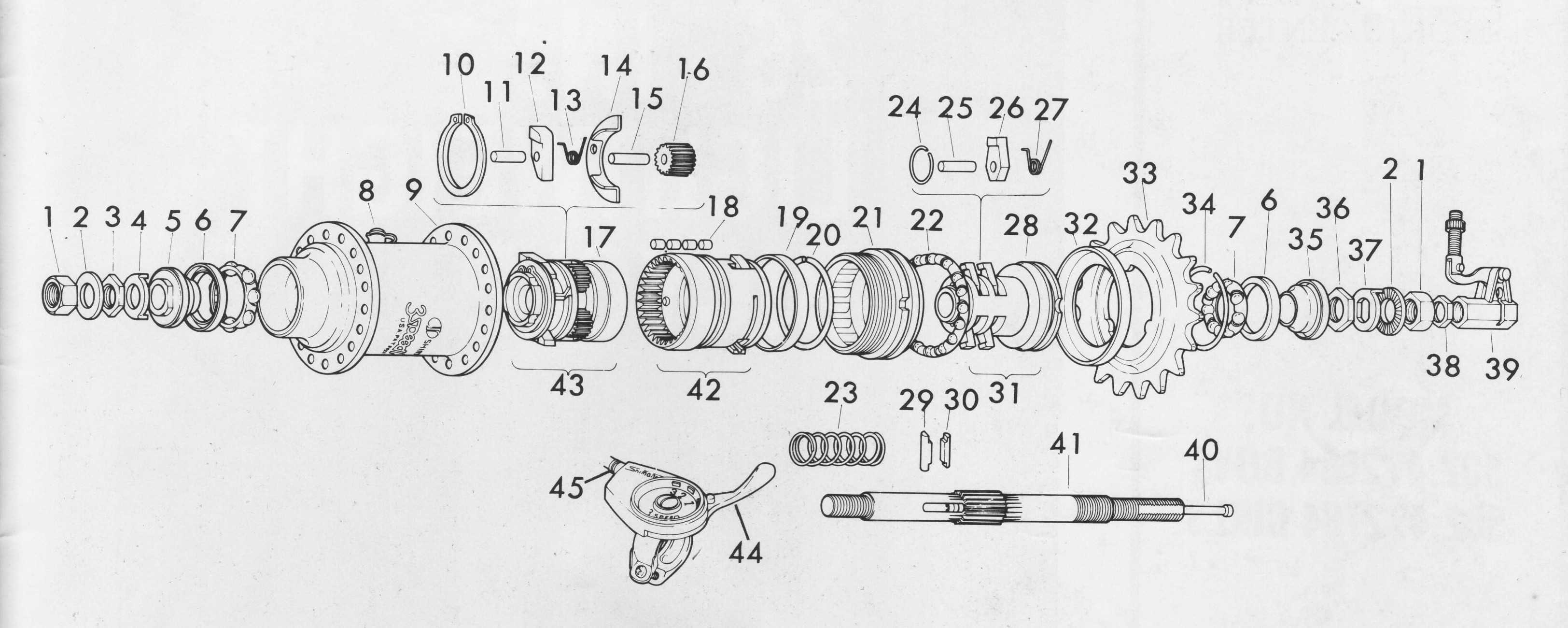
 Math: The dynamic systems theory is an area of mathematics that most physical therapists probably don’t consider during everyday treatment. Little do they know, every treatment decision we as therapists make for our patient/clients has some root found in the dynamic systems theory. In fact, it is a fitting description when this theory is applied to human movement. Human movement is an incredibly complex system comprised of many different systems all working at the same time. Paul Glazier recently offered a Grand Unified Theory (GUT) for sports performance [5] and he discusses in detail the various systems and dynamic elements involved in sports performance from musculoskeletal, to neural, to cognitive, environmental, hormonal, and emotional just to name a few. The systems at work during sport when combined are exponential and most likely infinite. This is why it is so difficult to try and capture all these dynamic systems in a laboratory setting with the current technology available. In my hip course offered through Herman & Wallace I offer a novel paradigm to help clinicians construct therapeutic exercise programs using the hip as a cornerstone to human movement. I try to compact these various systems into 8 overlapping elements related to sport performance. When each of these 8 components are “exploded” as you might see in an engineering schematic where an engine is exploded to see all the parts that make the engine or more simply explained using a cheeseburger as the example [Fig 3]. Sure its easy to spot the cheeseburger when its whole just like when you see an athlete on the field running it seems obvious. Once the cheeseburger is “exploded” you can now isolate each sub-element included in your cheeseburger. This cheeseburger example is an obvious over-simplification, but if we exploded the bun to see the underlying grain and the seeds and so on…you now start to get an idea of how deep and intertwined all these subsystems are. Interestingly, the engine and the cheeseburger have finite parts and fit together, the human system has different parts in different systems depending on the sport and who might be playing it, under ever-changing scenery, and so on. So you can now see how the 8 components I outline in my course can house many different aspects of these dynamic systems. Although, I think this is progress with regard to the current state of the evidence, specifically with regard to utilizing the hip during movement, there are other systems at work that clinicians simply cannot control, such as gender, hormonal, environmental, etc…The idea is to try to identify and then manipulate modifiable factors whenever possible. These concepts are more clearly described and implemented in my hip course! Please come and check it out, and let me know what you think!
Math: The dynamic systems theory is an area of mathematics that most physical therapists probably don’t consider during everyday treatment. Little do they know, every treatment decision we as therapists make for our patient/clients has some root found in the dynamic systems theory. In fact, it is a fitting description when this theory is applied to human movement. Human movement is an incredibly complex system comprised of many different systems all working at the same time. Paul Glazier recently offered a Grand Unified Theory (GUT) for sports performance [5] and he discusses in detail the various systems and dynamic elements involved in sports performance from musculoskeletal, to neural, to cognitive, environmental, hormonal, and emotional just to name a few. The systems at work during sport when combined are exponential and most likely infinite. This is why it is so difficult to try and capture all these dynamic systems in a laboratory setting with the current technology available. In my hip course offered through Herman & Wallace I offer a novel paradigm to help clinicians construct therapeutic exercise programs using the hip as a cornerstone to human movement. I try to compact these various systems into 8 overlapping elements related to sport performance. When each of these 8 components are “exploded” as you might see in an engineering schematic where an engine is exploded to see all the parts that make the engine or more simply explained using a cheeseburger as the example [Fig 3]. Sure its easy to spot the cheeseburger when its whole just like when you see an athlete on the field running it seems obvious. Once the cheeseburger is “exploded” you can now isolate each sub-element included in your cheeseburger. This cheeseburger example is an obvious over-simplification, but if we exploded the bun to see the underlying grain and the seeds and so on…you now start to get an idea of how deep and intertwined all these subsystems are. Interestingly, the engine and the cheeseburger have finite parts and fit together, the human system has different parts in different systems depending on the sport and who might be playing it, under ever-changing scenery, and so on. So you can now see how the 8 components I outline in my course can house many different aspects of these dynamic systems. Although, I think this is progress with regard to the current state of the evidence, specifically with regard to utilizing the hip during movement, there are other systems at work that clinicians simply cannot control, such as gender, hormonal, environmental, etc…The idea is to try to identify and then manipulate modifiable factors whenever possible. These concepts are more clearly described and implemented in my hip course! Please come and check it out, and let me know what you think!
I’m hoping the STEM approach can possibly make it into physical therapy curriculums to illustrate to future physical therapists that there are many different disciplines at work with regard to physical therapy, and taking a global view of these elements can certainly be worthwhile.
1. Ingber, D.E., N. Wang, and D. Stamenovic, Tensegrity, cellular biophysics, and the mechanics of living systems. Rep Prog Phys, 2014. 77(4): p. 046603.
2. Bahr, R., Why screening tests to predict injury do not work-and probably never will...: a critical review. Br J Sports Med, 2016.
3. Tak, I., et al., Hip Range of Motion Is Lower in Professional Soccer Players With Hip and Groin Symptoms or Previous Injuries, Independent of Cam Deformities. Am J Sports Med, 2016. 44(3): p. 682-8.
4. Chu, S.K., et al., The Kinetic Chain Revisited: New Concepts on Throwing Mechanics and Injury. PM R, 2016. 8(3 Suppl): p. S69-77.
5. Glazier, P.S., Towards a Grand Unified Theory of sports performance. Hum Mov Sci, 2015.
Figure 1


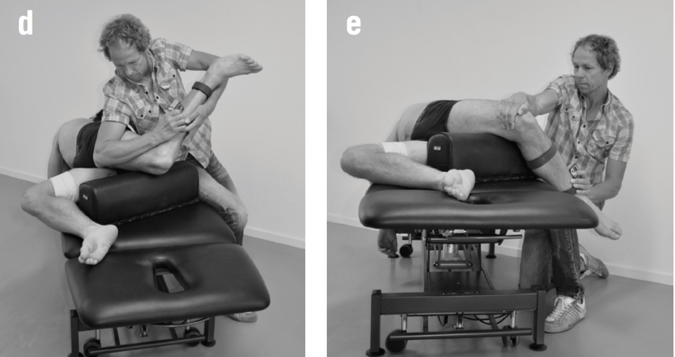
Figure 2
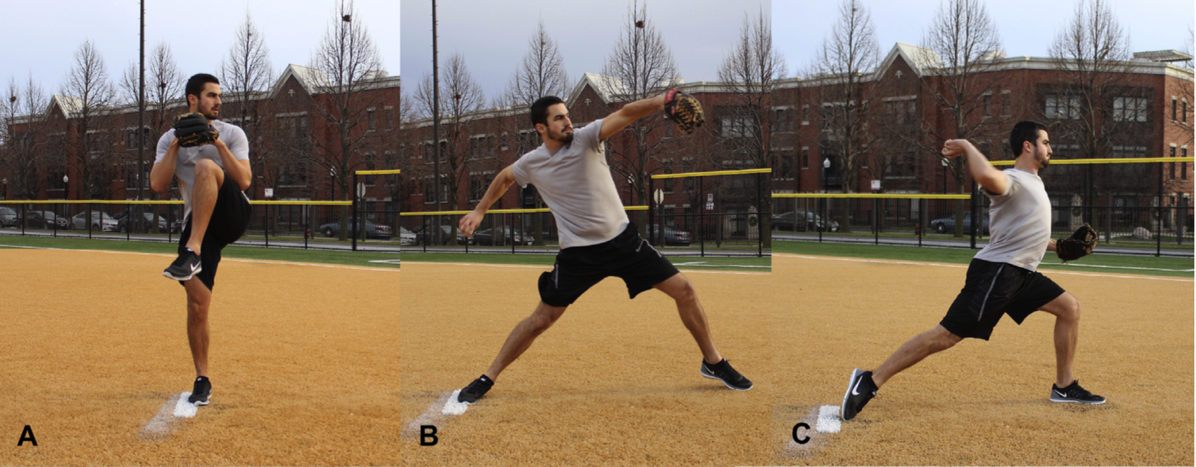
Figure 3
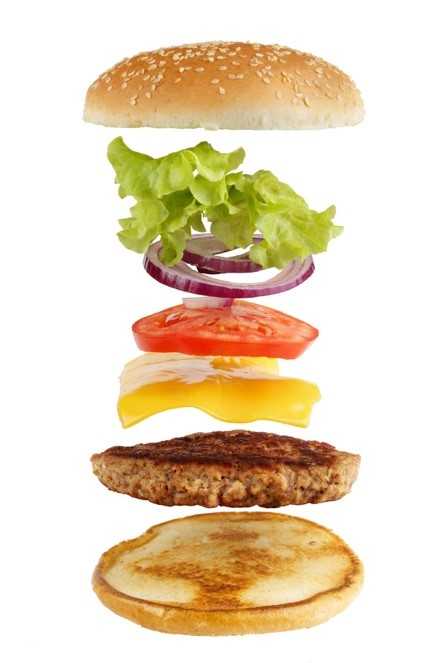
Figure 4
Today's blog is a contribution from Kristen Digwood, DPT, CLT, of the Elite Pelvic Rehab clinic in Wilkes-Barre, PA.
Urgency urinary incontinence (UUI), which is the involuntary loss of urine associated with urgency, is a common health problem in the female population. The effects of UUI result in limitations to daily activity and quality of life.
Current guidelines recommend conservative management as a first-line therapy in urinary incontinence, defined as "interventions that do not involve treatment with drugs or surgery targeted to the type of incontinence".
 Electrical stimulation is commonly used as part of a treatment program for women with UUI. There are several methods and parameters that can be used to improve urge incontinence, however the magnitude of the alleged benefits and best parameters is not completely established. Studies have suggested that the use of electrical stimulation to inhibit an overactive bladder functions to modulate unwanted detrusor contractions by way of sensory afferent stimulation of S2 and S3. This causes parasympathetic inhibition. In addition to this effect, contraction of the pelvic floor muscles results in inhibition and relaxation of the detrusor muscle which reduces urinary urgency.
Electrical stimulation is commonly used as part of a treatment program for women with UUI. There are several methods and parameters that can be used to improve urge incontinence, however the magnitude of the alleged benefits and best parameters is not completely established. Studies have suggested that the use of electrical stimulation to inhibit an overactive bladder functions to modulate unwanted detrusor contractions by way of sensory afferent stimulation of S2 and S3. This causes parasympathetic inhibition. In addition to this effect, contraction of the pelvic floor muscles results in inhibition and relaxation of the detrusor muscle which reduces urinary urgency.
Common methods of electrical stimulation include suprapubical, transvaginal, sacral and tibial nerves stimulation.
As with any medical treatment, practitioners seek the most effective methods and parameters to achieve the patient’s goals. A recent systematic review of electrical stimulation in the treatment of UUI included nine trials to treat UUI were included with total of 534 female patients. Most patients in the trials were close to 55 years of age. Five articles (total of nine) described a frequency of twice-weekly therapy and sessions of 20 minutes. Twelve weeks was the most common duration of therapy. All the studies applied an intensity of stimulation below 100 mA, with four of them (4/9) using 10 hz as the frequency. Intervaginal electrical stimulation showed the greatest subjective improvement and was the most effective.
The most frequent outcome measure was bladder diary, used in all papers; subjective satisfaction was used in 8; and quality-of-life questionnaires in 6, from a total of 9 papers.
The study noted that reports about electrical stimulation generally lack information on its cost-effectiveness. This is an important point, especially because in therapies with similar benefits cost may be one of the factors to indicate the most appropriate treatment. If we consider the relatively few adverse effects, low cost, and similar effectiveness when compared to medication, intravaginal electrical stimulation, according to available data, appears to be a good alternative treatment for UUI.
1. Thüroff JW, Abrams P, Andersson KE, Artibani W, Chapple CR, Drake MJ, et al.: EAU guidelines on urinary incontinence. Eur Urol. 2011; 59: 387-400.
2. Kralj B. The treatment of female urinary incontinence by functional electrical stimulation. In:Ostergard DR, Dent AD (eds). Urogenecology and Urodynamics. 3rd ed. Baltimore, MD: Williams and Wilkins; 1991.
3. Eriksen, BC. Electrical Stimulation. In: Benson JT editor. Female pelvic floor disorders: investigation and management. New York:Norton, 1992; 219-231.
4. Lucas Schreiner , Thais Guimarães dos Santos , Alessandra Borba Anton de Souza, et al. Int. braz j urol. vol.39 no.4 Rio de Janeiro July/Aug. 2013.
Vaginal wall thinning associated with menopausal changes can cause vaginal burning and pain, limitations in sexual function, and vaginal redness or even changes in discharge. Because these symptoms can mimic many other conditions such as pelvic floor muscle dysfunction or an infection, it is necessary for the pelvic rehabilitation therapist to be alert to identifying vaginal atrophy as an issue to rule out so that patients can access appropriate medical care when needed.
 Atrophic vaginitis (AV) is a condition of the vaginal walls associated with tissue thinning, discomfort, and inflammation. The tissue changes often extend into the vulvar area as well. Atrophic vaginitis may also be called vaginal atrophy, vulvovaginal atrophy, urogenital atrophy, or genitourinary syndrome of menopause. Although we tend to associate menopause with women who are in their 40’s or 50’s, any woman who has stopped having her menstrual cycles or who has had a significant reduction in her cycles may be at risk for vaginal atrophy. Any woman who has had a hysterectomy may also be at risk of this thinning of the vaginal walls. Common symptoms of vaginal wall thinning include vaginal dryness, tissue irritation, redness, itching, and a “burning” pain. Interruption in sleep, limitations in activities of daily living, and changes in mood and temperament have also been reported.
Atrophic vaginitis (AV) is a condition of the vaginal walls associated with tissue thinning, discomfort, and inflammation. The tissue changes often extend into the vulvar area as well. Atrophic vaginitis may also be called vaginal atrophy, vulvovaginal atrophy, urogenital atrophy, or genitourinary syndrome of menopause. Although we tend to associate menopause with women who are in their 40’s or 50’s, any woman who has stopped having her menstrual cycles or who has had a significant reduction in her cycles may be at risk for vaginal atrophy. Any woman who has had a hysterectomy may also be at risk of this thinning of the vaginal walls. Common symptoms of vaginal wall thinning include vaginal dryness, tissue irritation, redness, itching, and a “burning” pain. Interruption in sleep, limitations in activities of daily living, and changes in mood and temperament have also been reported.
One common pharmacological intervention for vaginal and vulvar atrophy is the topical application of hormone creams such as estrogen. A recent study examined the effects of low dose estrogen therapy on bacteria that populates the vaginal walls.Shen et al., 2016 This bacteria may be causal or correlated to vaginal health, and also appears related to estrogen levels. Sixty women diagnosed with atrophic vaginitis were treated with low dose estrogen therapy and followed for four weeks to assess the vaginal microbiotia via mid-vaginal swabs. Following are highlights from the linked study’s findings,
- Prior to treatment, in symptomatic postmenopausal women the Lactobacilli species were less abundant and made up 11.2% of the community, while in asymptomatic women, the communities were more than 50% lactobacilli
- Gardnerella was more abundant than Lactobacillus in women with atrophic vaginitis
- Overall diversity of bacterial communities between healthy women and those with atrophic vaginitis was not significantly different
- In response to treatment with estrogen, women with AV reported improved symptoms and decreased vaginal pH
- Serum estradiol improved on average from approximately 42 pmol/L to 168 pmol/L by week 2, with little change from week 2 to week 4
- Lactobacillus count was negatively correlated with symptoms (i.e., more Lactobacillis = less symptoms) and Gardnerella and Atopobium counts were positively correlated with symptoms
- There were variations noted in how each woman’s vaginal bacterial communities responded to the estrogen therapy in that some women had a dominance of other bacteria after 4 weeks even though their symptoms decreased
In conclusion, the authors stated that “…a Lactobacillus-dominated vaginal community may be considered as one of the signs of AV treatment success…” along with reduced symptoms and increased serum estradiol levels. Prior studies have recognized barriers to treatment that include lack of patient knowledge of vulvar and vaginal atrophy, failure to discuss associated symptoms with physicians, concerns about safety of treatments or poor symptom relief with prescribed interventions.Kingsburg et al., 2013 This leaves the pelvic rehabilitation provider in a excellent role of educating women in the signs and symptoms of atrophic vaginitis, observing the tissues for changes, and communicating with referring providers and prescribers if a concern is noted. Furthermore, failure to recognize the potential for vaginal atrophy and treating these tissues with manual therapy or exercise may injure or exacerbate the problem.
Interested in learning more? Keep an eye out for a Menopause Rehabilitation and Symptom Management course with Michelle Lyons!
Changes in the Vagina and Vulva. Retrieved June 27, 2016 from http://www.menopause.org/for-women/sexual-health-menopause-online/changes-at-midlife/changes-in-the-vagina-and-vulva
Kingsberg, S. A., Wysocki, S., Magnus, L., & Krychman, M. L. (2013). Vulvar and vaginal atrophy in postmenopausal women: findings from the REVIVE (REal Women's VIews of Treatment Options for Menopausal Vaginal ChangEs) survey. The journal of sexual medicine, 10(7), 1790-1799.
Shen, J., Song, N., Williams, C. J., Brown, C. J., Yan, Z., Xu, C., & Forney, L. J. (2016). Effects of low dose estrogen therapy on the vaginal microbiomes of women with atrophic vaginitis. Scientific reports, 6.
Vaginal Atrophy. Retrieved June 27, 2016 from http://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/home/ovc-20200167
Spending the past 5 years watching a lot of Disney Junior and reading Dr. Seuss, professional journal reading is generally reserved for the sanctuary of the bathroom. When patients ask if I’ve heard of certain new procedures or therapies, I try to sound intelligent and make a mental note to run a PubMed search on the topic when I get home. Making the effort to stay on top of research, however, makes you a more confident and competent clinician for the information-hungry patient and encourages physicians to respect you when it comes to discussing their patients.
A 2016 article in Translational Andrology and Urology, Lin et al., explored rehabilitation of men post radical prostatectomy on a deeper level, trying to prove that brain-derived neurotrophic factor (BDNF) promotes nerve regeneration. In many radical prostatectomies, even when the nerve-sparing approach is used, there is injury to the cavernous nerves, which course along the posterolateral portion of the prostate. Cavernous nerve injury can cause erectile dysfunction in 60.8-93% of males postoperatively. The authors discussed Schwann cells as being vital for maintaining integrity and function of peripheral nerves like the cavernous nerve. They hypothesized that BDNF, a member of the neurotrophin family that supports neuron survival and prevents neuronal death, activates the JAK/STAT (Janus kinase /signal transducer and activator of transcription) pathway in Schwann cells, thus facilitating axonal regeneration via secretion of cytokines (IL-6 and OSM-M). Through scientific experiment on a cellular level (please refer to the article for the specific details), the authors were able to confirm their hypothesis. Schwann cells do, in fact, produce cytokines that contribute to the regeneration of cavernous nerves.
From a different cellular perspective, Haahr et al., (2016) performed an open-label clinical trial involving intracavernous injection of “autologous adipose-derived regenerative cells” (ADRCs) in males experiencing erectile dysfunction (ED) after radical prostatectomy. Current treatments with PDE-5 inhibitors do not give satisfactory results, so the authors performed a human phase 1, single-arm trial to further the research behind the use of adipose-derived stem cells for ED. Some limitations included the study was un-blinded and had no control group. Seventeen males who had ED after radical prostatectomy 5-18 months prior to the study were followed for 6 months post intracavernosal transplantation. The primary outcome was safety/tolerance of stem cell treatment, and the secondary was improvement of ED. The single intracavernosal injection of freshly isolated autologous adipose-derived cells resulted in 8 of 17 men regaining erectile function for intercourse; however, the men who were not continent did not regain erectile function. The end results showed the procedure was safe and well-tolerated. There was a significant improvement in scores for the International Index of Erectile Function-5 (IIEF-5), suggesting this therapy may be a promising one for ED after radical prostatectomy.
In the clinic, we need to treat our patients to the best of our ability. Taking the Post-Prostatectomy Patient Rehabilitation course is vital if even just one patient enters your office seeking treatment. Keeping up on research (even that which seems too full of forgotten science) and learning new manual techniques and exercises can help us rise as clinicians prepared to optimize patients’ function.
Lin, G., Zhang, H., Sun, F., Lu, Z., Reed-Maldonado, A., Lee, Y.-C., … Lue, T. F. (2016). Brain-derived neurotrophic factor promotes nerve regeneration by activating the JAK/STAT pathway in Schwann cells. Translational Andrology and Urology, 5(2), 167–175. http://doi.org/10.21037/tau.2016.02.03
Haahr, M. K., Jensen, C. H., Toyserkani, N. M., Andersen, D. C., Damkier, P., Sørensen, J. A., … Sheikh, S. P. (2016). Safety and Potential Effect of a Single Intracavernous Injection of Autologous Adipose-Derived Regenerative Cells in Patients with Erectile Dysfunction Following Radical Prostatectomy: An Open-Label Phase I Clinical Trial. EBioMedicine, 5, 204–210. http://doi.org/10.1016/j.ebiom.2016.01.024
Yoga offers a compelling mind-body approach to maternal care that is forward thinking and aligns with the World Health Organization and Institute of Medicine’s recommendations for patient-centered care. But let’s take a look at WHY postpartum care MUST change in order to establish need for the entry of yoga into postpartum care.
Maternal Health Track Record
The United States and similarly developed countries have a very poor track record for postpartum care. The record is so poor that the problem in the US has been labeled a “human rights failure.”1
 On its own, the US has the worst track record for not only postpartum care, but for maternal and infant mortality and first-day infant death rate in the developed world (Save the Children 2013). Between 1999-2008, global mortality rates decreased by 34% while the US’s rates doubled for mothers.1
On its own, the US has the worst track record for not only postpartum care, but for maternal and infant mortality and first-day infant death rate in the developed world (Save the Children 2013). Between 1999-2008, global mortality rates decreased by 34% while the US’s rates doubled for mothers.1
Patient satisfaction also suffers under the current model of care, with many more mothers experiencing postpartum depression, a significant risk factor for both mother and baby during and after pregnancy.
The increase in mortality and poor outcomes can, in part, be attributed not to underuse, but overuse of medical intervention during pregnancy and birth. 2,3,4 Countries that have “access to woman-centered care have fewer deaths and lower health care costs”; and, hospital system reviews in the US show that reducing medical interventions are both reducing cost and improving outcomes.1,4,5
The notorious lack of accountability (reporting system) in maternal health care also plagues the US and suggests that maternal deaths are even higher than currently reported, leading to Coeytaux’s conclusion that the “United States is backsliding.”1
Improving Postpartum Outcomes with Integrated Physical Therapy Care
In After the Baby’s Birth, maternal health advocate Robin Lim writes,
"All too often, the only postpartum care an American woman can count on is one fifteen minute appointment with her doctor, six weeks after she has given birth. This six-week marker ends an arbitrary period within which she is supposed to have worked out most postpartum questions for herself. This neglect of postpartum women is not just poor healthcare, it is abusive, particularly to women suffering from painful physical and/or psychological disorders following childbirth."
Physical therapists can be instrumental change agents in improving current postpartum care, especially through the integration of contemplative sciences like yoga. Yoga can be the cornerstone of holistically-driven, person-centered care, especially in comorbid conditions such as pelvic pain and depression, where pharmacological side effects, stigma, can severely diminish adherence to biomedical interventions.6 Coeytaux, as well as other authors, clearly correlate the reduction of maternal mortality with improved postpartum care. The World Health Organization recommends that postpartum checkups should include screening for:
- Back pain
- Incontinence (stress)
- Hemorrhoids
- Constipation
- Fatigue
- Breast pain
- Perineal pain
- Depression
- Painful or difficult intercourse
- Headaches
- Bowel problems
- Dizziness or fainting
 A physical therapist is a vital team member in not only screening for many of the
A physical therapist is a vital team member in not only screening for many of the
listed problems above, but in managing them. It is important to note that other countries, like France, deliver high quality postpartum rehab care plus in-home visits, all while spending far less than the US on maternal care.
The World Health Organization, however, clarifies the vital importance of postpartum care delivery by making a significant recommendation for a paradigm shift in biomedical care.7
Yoga as a “Best Care Practice” for Postpartum Care
The WHO recommends the use of a biopsychosocial model of care, which yoga is ideally suited to provide via its ancient, multi-faceted person-centered philosophy. Medical Therapeutic Yoga is a unique method of combining evidence-based rehabilitation with yoga to emerge with a new paradigm of practice. MTY:
- Addresses the mother as a person, not as a condition or diagnosis.
- Empowers mothers with self-care strategies for systems-based, not just musculoskeletal or neuromuscular, change.
- Addresses all domains of biopsychosocial impairment.
- Teaches interdisciplinary partnership-based theory, which is integral to creative collaborative discourse and innovation in postpartum care.
- Equips clinicians with business service, website development, practice paradigm, and social media campaign tools to fully develop the new clinical niche of Professional Yoga Therapy practice.
- Promotes patient advocacy, health promotion, and public health education via mainstreaming yoga into rehabilitative and medical services.
- Provides the gender context for prescription that traditional yoga is lacking.
- Evolves yoga for use in prenatal and postpartum care.
Physical therapy screening and intervention in the postpartum is vital, but the addition of yoga can optimize postpartum care and has enormous potential to be a “Best Care Practice” for postpartum care in rehabilitation.
As a mind-body intervention, yoga during pregnancy can increase birth weight, shorten labor, decrease pre-term birth, decrease instrument-assisted birth, reduce perceived pain, stress, anxiety sleep disturbances, and general pregnancy-related discomfort and quality of life physical domains.8-9
In addition to the typical physical therapy intervention for postpartum physical therapy, the MTY paradigm provides:
- self-care strategies for psychoemotional health and social engagement, increasing self-efficacy, confidence, and self-worth,
- a concise container for clinical-decision through its algorithmic programming,
- psychoemotional and neuroendocrine intervention,
- nutritional counseling and resource utilization,
- energetic adjunct therapies steeped in Ayurvedic science,
- executive functioning and cognitive support,
- epigenetic effect, and
- inter- and intrarelational development.
Postpartum integrated physical therapy care can provide more comprehensive care than rehab alone because of its multi-faceted biopsychosocial structure and systems-based model of care. Ginger’s course, Yoga as Medicine for Labor, Delivery, and Postpartum provides evidence-based methodology for prenatal and postpartum practice that streamlines clinical decision-making and intervention through introduction of a yogic model of assessment.
To learn more about Ginger’s course, visit Yoga as Medicine for Labor, Delivery, and Postpartum
Coeytauz et al., Maternal Mortality in the US: A Human Rights Failure. Contraception Editorial, March 2011. http://www.arhp.org/publications-and-resources/contraception-journal/march-2011
Kuklina E, Meikle S, Jamieson D, et al. Severe obstetric morbidity in the US, 1998–2005. Obstet Gynecol. 2009;113:293–299.
Tita ATN, Landon MB, Spong CY, et al. Timing of elective cesarean delivery at term and neonatal outcomes. NEJM. 2009;360:111–120.
Clark SL, Belfort MA, Byrum SL, Meyers JA, Perlin JB. Improved outcomes, fewer cesarean deliveries, and reduced litigation: results of a new paradigm in patient safety. Am J Obstet Gynecol. 2008;199:e1–105.e7.Abstract | Full Text | Full-Text PDF (100 KB)
Oshiro BT. Decreasing elective deliveries before 39 weeks of gestation in an integrated health care system. Obstet Gynecol. 2009;113:804–811.
Buttner, M. M., Brock, R. L., O'Hara, M. W., & Stuart, S. (2015). Efficacy of yoga for depressed postpartum women: A randomized controlled trial. Complementary Therapies in Clinical Practice, 21(2), 94-100. doi:10.1016/j.ctcp.2015.03.003 [doi]
WORLD HEALTH ORGANIZATION., 2002. Towards a common language for functioning, disability and health : ICF. Geneva: World Health Organisation.
Curtis, K., Weinrib, A., & Katz, J. (2012). Systematic review of yoga for pregnant women: Current status and future directions. Evidence-Based Complementary and Alternative Medicine : ECAM, 2012, 715942. doi:10.1155/2012/715942 [doi]
Sharma, M., & Branscum, P. (2015). Yoga interventions in pregnancy: A qualitative review. Journal of Alternative and Complementary Medicine (New York, N.Y.), 21(4), 208-216. doi:10.1089/acm.2014.0033 [doi]