![By Mikael Häggström (Own work) [CC0], via Wikimedia Commons](https://upload.wikimedia.org/wikipedia/commons/thumb/d/d9/Symptoms_of_menopause_%28raster%29.png/512px-Symptoms_of_menopause_%28raster%29.png) Sleep difficulties are a common problem among women in the menopausal period, with hot flashes and night sweats commonly interfering with a restful night’s sleep. According to Baker and colleaguesBaker, 2015 , disturbed sleep is present in 40-60% of women in the menopausal transition. The authors also point out that insomnia is not well characterized, with poor identification of a physiologic basis for the sleep disturbances. In the research linked above, perimenopausal women diagnosed with clinical insomnia (n=38) were compared to women who did not have insomnia (n=34). Outcome measures included the Beck Depression Inventory, the Greene Climacteric Scale, sleep diaries, sleep studies, and nocturnal hot flashes via dermal conductance meters.
Sleep difficulties are a common problem among women in the menopausal period, with hot flashes and night sweats commonly interfering with a restful night’s sleep. According to Baker and colleaguesBaker, 2015 , disturbed sleep is present in 40-60% of women in the menopausal transition. The authors also point out that insomnia is not well characterized, with poor identification of a physiologic basis for the sleep disturbances. In the research linked above, perimenopausal women diagnosed with clinical insomnia (n=38) were compared to women who did not have insomnia (n=34). Outcome measures included the Beck Depression Inventory, the Greene Climacteric Scale, sleep diaries, sleep studies, and nocturnal hot flashes via dermal conductance meters.
Results of the study concluded that women with insomnia, compared with controls, had higher levels of psychologic, somatic, vasomotor symptoms, and had higher scores on the depression inventory, shorter sleep duration, and lower sleep efficiency. Women with insomnia were also more likely to have hot flashes, with number of hot flashes predicting awakenings during the sleep study. Episodes of wakefulness after sleep onset, and decreased time of sleep were noted in the women who were diagnosed with new-onset insomnia.
Because untreated insomnia is associated with negative consequences including hypertension, stroke, diabetes, and depression, the authors suggest that women who are diagnosed with insomnia should be treated for their insomnia. If you are interested in learning about natural methods to manage and reduce hot flashes, among many other interesting topics, you will likely enjoy Herman & Wallace faculty Michelle Lyons and her newer course: Special Topics in Women’s Health. The next chance to hear Michelle discuss these topics is in Denver in January. Bring your skis!
Baker, Fiona C. et al. "Insomnia in women approaching menopause: Beyond perception" Psychoneuroendocrinology, Volume 60, 96-104 October 2015
How many of us have heard a subjective report from a patient that clearly implicates the coccyx as the problem but quickly think, “I’m sure as heck not going there!”? We cross our fingers, hoping the patient will get better anyway by treating around the issue. That is like trying to get a splinter out of a finger by massaging the hand. As nice as the treatment may feel, the tip of the finger still has a sharp, throbbing pain at the end of the day, because the splinter, the source of the pain, has not been touched directly. For most therapists, the coccyx is an overlooked (and even ignored) splinter in the buttocks.
![By Sanba38 (Own work) [GFDL (http://www.gnu.org/copyleft/fdl.html), CC-BY-SA-3.0 (http://creativecommons.org/licenses/by-sa/3.0/) or FAL], via Wikimedia Commons](https://upload.wikimedia.org/wikipedia/commons/thumb/f/f6/Splinter.jpg/256px-Splinter.jpg) A colleague of mine had a patient with relentless coccyx pain for 7 years and was about to lose a relationship, as well as his mind, if someone did not help him. He had therapy for his lumbar spine with “core stabilization,” and he had pain medicine, anti-inflammatory drugs, and inflatable donuts to sit upon to relieve pressure, but his underlying pain remained unchanged. Luckily for this man, his “last resort” was trained in manual therapy and assessed the need for internal coccyx mobilization to resolve his symptoms. The patient’s desperation for relief overrode any embarrassment or hesitation to receive the treatment. After a few treatments, the man’s life was changed because someone literally dug into the source of pain and skillfully remedied the dysfunction.
A colleague of mine had a patient with relentless coccyx pain for 7 years and was about to lose a relationship, as well as his mind, if someone did not help him. He had therapy for his lumbar spine with “core stabilization,” and he had pain medicine, anti-inflammatory drugs, and inflatable donuts to sit upon to relieve pressure, but his underlying pain remained unchanged. Luckily for this man, his “last resort” was trained in manual therapy and assessed the need for internal coccyx mobilization to resolve his symptoms. The patient’s desperation for relief overrode any embarrassment or hesitation to receive the treatment. After a few treatments, the man’s life was changed because someone literally dug into the source of pain and skillfully remedied the dysfunction.
Marinko and Pecci (2014) presented 2 case reports of patients with coccydynia and discussed clinical decision making for the evaluation and management of the patients. The patient with a traumatic onset of pain had almost complete relief of pain and symptoms after 3 treatment sessions of manual therapy to the sacrococcygeal joint. The patient who experienced pain from too much sitting did not respond with any long term relief from the manual therapy and had to undergo surgical excision. The first patient was treated in the acute stage of injury, but the second patient had a cortisone injection initially and then the manual treatment in this study 1 year after onset of pain. Both patients experienced positive outcomes in the end, but at least 1 patient was spared the removal of her coccyx secondary to manual work performed in what some therapists consider “uncharted territory.”
A systematic literature review was published in 2013 by Howard et al. on the efficacy of conservative treatment on coccydinia. The search spanned 10 years and produced 7 articles, which clearly makes this a not-so-popular area of research. No conclusions could be made on how effective the various treatments of manual therapy, injections, or radiofrequency interventions were because of the insufficient amount of research performed on the topic.
In an evidence-based era for physical therapy intervention, sometimes we limit ourselves in our treatment approaches. What if the best interventions just have yet to be oozing with clinical trials and published outcomes? The first person to pull a splinter out of a finger did not have a peer-reviewed guide instructing one to use 2 fingers to wrap around the splinter and pull it out of the skin. Coccyx mobilization internally and externally is a legitimate treatment without a lot of notoriety. The Coccyx Pain, Evaluation, and Treatment course uses the most current evidence to expand your knowledge of anatomy and pathology and hone your palpation skills to evaluate and treat an area where you never thought you’d go.
References: Howard, P. D., Dolan, A. N., Falco, A. N., Holland, B. M., Wilkinson, C. F., & Zink, A. M. (2013). A comparison of conservative interventions and their effectiveness for coccydynia: a systematic review. The Journal of Manual & Manipulative Therapy, 21(4), 213–219. http://doi.org/10.1179/2042618613Y.0000000040
Marinko LN, Pecci M. (2014). Clinical decision making for the evaluation and management of coccydynia: 2 case reports. J Orthop Sports Phys Ther, 44(8):615-21. doi: 10.2519/jospt.2014.4850
Research published in a Nursing journal highlights the need for pelvic rehab providers to assess for sexual dysfunction in women before, during, and after pregnancy. 200 women were interviewed about their return to sexual activity after pregnancy and childbirth, and the results demonstrate that women can (and do) have limitations in their sexual function around the entire peripartum period.
![By Nina Matthews (Flickr: head to head) [CC BY 2.0 (http://creativecommons.org/licenses/by/2.0)], via Wikimedia Commons](https://upload.wikimedia.org/wikipedia/commons/thumb/8/86/Silhouette_or_a_pregnant_woman_and_her_partner-14Aug2011.jpg/492px-Silhouette_or_a_pregnant_woman_and_her_partner-14Aug2011.jpg) The results of the survey concluded that before pregnancy 33.5% of the women reported sexual dysfunction, and this number increased to 76% during pregnancy, and to 43.5% following delivery. The types of sexual dysfunction included dyspareunia, vaginismus, and decreased desire and orgasm. The authors of the study correlated dysfunctions with Catholic religion, vaginal delivery without suture, dyspareunia during pregnancy, vaginismus before pregnancy, and with working more than 8 hours per day.
The results of the survey concluded that before pregnancy 33.5% of the women reported sexual dysfunction, and this number increased to 76% during pregnancy, and to 43.5% following delivery. The types of sexual dysfunction included dyspareunia, vaginismus, and decreased desire and orgasm. The authors of the study correlated dysfunctions with Catholic religion, vaginal delivery without suture, dyspareunia during pregnancy, vaginismus before pregnancy, and with working more than 8 hours per day.
The information collected in this study raise important points with a variety of topics related to sexual function. How we as providers aim to address these topics with women can have a critical impact on the health of a woman and her family. Let’s look at some action items this research can lead us to:
- Include methods of asking about sexual health in your written and verbal evaluations
- Educate colleagues about bringing up sexual health with women throughout the lifespan
- Avoid assuming that a woman would not want to be sexually active during pregnancy
- Recognize that personal beliefs (including religion) play a role in sexual health, and that a patient can be encouraged to talk to her spiritual advisor or a trusted professional if concerns arise
- Talk about healthy workloads, options for modifications at work, and strategize with patients about rest breaks or decreasing work hours if financially able
This type of research can lead to many more questions, such as how religious beliefs impact sexual function during pregnancy, what the effect of physiologic changes versus fatigue can have on libido, or if women who have intervention for dyspareunia prior to pregnancy have decreased sexual dysfunction after pregnancy. Most of us were not instructed in how to dialog about these types of questions, and of course some topics, like religion, are potentially very sensitive to bring up with our patients.
If you would like more practical advice about the clinical implications for sexual medicine across the lifespan and among all genders, consider a trip to San Diego this November to learn from Herman & Wallace co-founder Holly Herman at Sexual Medicine for Men and Women: A Rehabilitation Perspective!
Holanda, J. B. D. L., Abuchaim, E. D. S. V., Coca, K. P., & Abrão, A. C. F. D. V. (2014). Sexual dysfunction and associated factors reported in the postpartum period. Acta Paulista de Enfermagem, 27(6), 573-578.
How often do we hear of patients trying to explain their sexual pain to a partner, only to be doubted, not believed, or guilt tripped into having sex because of the lack of understanding of the condition? I’d say about as often as we hear of the other unfortunate misunderstandings about the nature of painful sexual function, such as people not wanting to be in a relationship for fear of sexual dysfunction limiting their participation, or believing that healthy sex is gone for good. Most of us are familiar with the phrase, “not tonight- I’ve got a headache” yet how often is the truth really that a person has a “pelvic ache?” And do headaches and pelvic pain go together? That is the question posed in research published in the journal Headache.
 For 72 women who were being treated for chronic headache, a survey was administered to assess for associations between sexual pain and libido, a history of abuse, and to determine the number of women being treated for sexual pain. Nearly 71% of the women were diagnosed on the International Classification of Headache Disorders (ICHD)-III criteria with chronic migraines, nearly 17% with medication overuse headache, 10% with both chronic overuse headache and migraine. Below are some of the statistics from the survey.
For 72 women who were being treated for chronic headache, a survey was administered to assess for associations between sexual pain and libido, a history of abuse, and to determine the number of women being treated for sexual pain. Nearly 71% of the women were diagnosed on the International Classification of Headache Disorders (ICHD)-III criteria with chronic migraines, nearly 17% with medication overuse headache, 10% with both chronic overuse headache and migraine. Below are some of the statistics from the survey.
| Symptom | % Respondents who Experienced Symptom |
| Pelvic region pain brought on by sexual activity | 44% |
| Pelvic region pain preventing from engaging in sexual activity | 18% |
| Among women who had pain: | |
| Reported pain for < 1 year | 3% |
| Reported pain for 1-5 years | 35% |
| Reported pain for 6-10 years | 29% |
| Reported pain for > 10 years | 32% |
Although the next statistics should not be so surprising based on prior literature and on our work in the clinics, 50% of the women had not discussed their pelvic pain with a provider. Of the women who had discussed their pelvic pain with a provider, 37.5% were currently receiving treatment, 31% had not received any treatment, 31% had received care in the past, and 1% did not provide an answer. Reasons for not receiving treatment included that no treatment was offered, pain was not severe enough to warrant care, or fear of pursuing treatment due to embarrassment. Unfortunately, rehabilitation was not a significant part of the treatment plan, even though all but one of the women said they would want to pursue care if available.
Other interesting associations were made in the article, which is available as full text in the link above, including rates of sexual abuse, and associations between types of headaches and pelvic pain. The bottom line is that headaches and pelvic pain can occur together, and that based on this research, many women are still suffering for long periods of time without accessing care for pelvic pain. When it comes to headaches, there are many types of headaches, and many other conditions that occur and can cause pain in the head, face, and neck. If you would like to sharpen your clinical tools related to headaches, as well as dizziness and vertigo, you still have time to sign up for the Institute’s new continuing education course on Neck Pain, Headaches, Dizziness, and Vertigo that takes place in Rockville in November.
Peyronie’s disease is a condition in which there are fibrotic plaques (sometimes calcified) that can cause a curvature in the penis, most notable during erection. Pain as well as urinary and sexual dysfunction may occur with Peyronie's disease. Increased attention has been given in recent years to the relationship between male hormones, erectile dysfunction, and Peyronie's disease. According to the Mayo Clinic, testosterone, the predominant hormone affecting male physical characteristics, peaks during adolescence and early adulthood. Testosterone gradually decreases about 1% per year once a man reaches age 30-40. Some men experience symptoms from the decline in testosterone and these symptoms can include decreased sexual function, sleep disturbances changes in bone density and muscle bulk, as well as changes in cognition and depression. Because other factors and conditions can cause similar symptoms, patients with any of these changes should talk to their medical provider to rule out diabetes, thyroid dysfunction, depression, sleep apnea, and medication side effects, according to Mayo.
 In an article published in 2012, Iacono and colleagues studied the correlation between age, low testosterone, fibrosis of the cavernosal tissues, and erectile dysfunction. 47 patients diagnosed with erectile dysfunction (ED) were included, with 55% of the 47 men being older than age 65. Having increased fibrosis corresponded to having a positive Rigiscan test- meaning that a nocturnal test of penile rigidity demonstrated abnormal nighttime erections. Low levels of testosterone also corresponded to erectile dysfunction. (This is an open access article with full text available) Another published article agreed with the above in that low testosterone is associated with Peyronie’s disease and/or erectile dysfunction. The authors are cautious, however, in describing the association between the variables, as causation towards plaque formation characteristic of Peyronie’s is not known.
In an article published in 2012, Iacono and colleagues studied the correlation between age, low testosterone, fibrosis of the cavernosal tissues, and erectile dysfunction. 47 patients diagnosed with erectile dysfunction (ED) were included, with 55% of the 47 men being older than age 65. Having increased fibrosis corresponded to having a positive Rigiscan test- meaning that a nocturnal test of penile rigidity demonstrated abnormal nighttime erections. Low levels of testosterone also corresponded to erectile dysfunction. (This is an open access article with full text available) Another published article agreed with the above in that low testosterone is associated with Peyronie’s disease and/or erectile dysfunction. The authors are cautious, however, in describing the association between the variables, as causation towards plaque formation characteristic of Peyronie’s is not known.
The larger question about Peyronie’s disease is what a patient can do to improve the symptoms of the condition. Therapists who treat male patients are increasingly interested in this question, and many are working with their patients to address the known soft tissue dysfunction. Interventions may include teaching patients to perform soft tissue mobilizations and stretches to the restricted tissue, and educating the patient in what the available literature tells us about rehabilitation of this condition. Hopefully, as male pelvic rehabilitation continues to grow in popularity, more therapists will contribute case studies and participate in higher levels of research so that more men can add conservative care of Peyronie’s to their list of treatment options.
To learn more about what the literature tells us about Peyronie’s and other male pelvic rehabilitation conditions, the Male Pelvic Floor continuing education course is taking place in Seattle in November, and you won't want to miss it!
Have you ever tried to make a fitted sheet reach all corners of a mattress when there is a small, defective seam stitched into the middle of the fabric? No matter how much you pull or tug, the sheet won’t hug the last corner just right. If you get it to stay, the opposite corner flips off from the extra tension. Unless you release the snag the stitching created, you won’t ever get the sheet to fit smoothly. This is like the myofascial system in the body, where a snag in one area can affect another proximally or distally when normal movement tries to occur.
 Even the pelvic floor can get myofascial restrictions and trigger points; however, this area is often ignored and seemingly insignificant when not fully understood. Pelvic floor fascial restrictions and trigger points can have paramount implications for the pelvic, abdominal, hip, and lumbar regions. This why pelvic rehabilitation practitioners should be equipped to evaluate and treat myofascial snags.
Even the pelvic floor can get myofascial restrictions and trigger points; however, this area is often ignored and seemingly insignificant when not fully understood. Pelvic floor fascial restrictions and trigger points can have paramount implications for the pelvic, abdominal, hip, and lumbar regions. This why pelvic rehabilitation practitioners should be equipped to evaluate and treat myofascial snags.
Pastore and Katzman (2012) published an article stating that 14%-23% of women with chronic pelvic pain have myofascial pelvic pain, and up to 78% of women with interstitial cystitis have myofascial trigger points. Once a trigger point in pelvic floor musculature is identified through palpation, it can refer pain to the perineum, vagina, urethra, and rectum, which seems obvious; however, pain may also refer to the abdomen, back, trunk, hip, buttocks, and lower leg. If palpation can provoke a referral pattern of pain, stretching and/or contraction of the musculature with that myofascial restriction will surely provoke a cascade of symptoms. How can we as clinicians just let statistics like this slide and figure “someone else should do that examination and fix it?” To demonstrate the efficacy in treating myofascial trigger points in pelvic musculature, consider the following study. Anderson et al (2015) had 374 patients follow a protocol of pelvic floor myofascial release of trigger points with an internal trigger point wand along with paradoxical relaxation therapy for 6 months. The goal was to see if patients with chronic pelvic pain syndrome could reduce their medication after following the protocol. At 6 months, a 36.9% reduction in medication use was noted in a complete case analysis, and a 22.7% reduction was revealed in the modified intention to treat (mITT) analysis. Patients no longer needing to take medication significantly correlated with the reduction of overall symptoms from following the protocol.
Knowing how to find and treat pelvic floor myofascial trigger points can lead to reduction of pain in women (and men) and even help reduce the need for medication for their chronic pelvic pain symptoms. Stop trying to make a bed without discerning if the base layer is free of snags. Learning how to go deeper to feel what’s under the covers can help unveil a source of potentially chronic, disabling pain. You can learn how to skillfully treat the “hidden” dysfunction by attending a Myofascial Release for Pelvic Dysfunction course with Ramona Horton.
References:
Pastore, E. A., & Katzman, W. B. (2012). Recognizing Myofascial Pelvic Pain in the Female Patient with Chronic Pelvic Pain. Journal of Obstetric, Gynecologic, and Neonatal Nursing : JOGNN / NAACOG, 41(5), 680–691. http://doi.org/10.1111/j.1552-6909.2012.01404.x
Anderson , R., Harvey, R., Wise, D., Smith, J., Nathanson, B., Sawyer, T. (2015 March). Chronic Pelvic Pain Syndrome: Reduction of Medication Use After Pelvic Floor Physical Therapy with an Internal Myofascial Trigger Point Wand. Applied Psychophysiology and Biofeedback. Volume 40, Issue 1, pp 45-52
The concept of patient compliance, or adherence (a more preferred term), has been the subject of many medical studies, and adherence in pelvic rehabilitation is an aspect of rehab of critical interest. Recently published results of a survey questioning providers and the public about adherence in pelvic floor muscle training offers an insightful perspective. Researchers Frawley, Dumoulin, and McClurg conducted a web-based survey which was published in published in Neurourology and Urodynamics. The survey was completed by 515 health professionals and by 51 individuals from the public. Interestingly, but perhaps not surprisingly, health professionals and public respondents placed different value on which factors related to rehabilitation contributed the most to adherence.
 Data collected in the study included topics such as barriers to adherence in pelvic floor muscle training (PFMT), perception of potential benefit of PFMT, therapy-related factors including therapeutic relationship, socioeconomic factors, and issues surrounding short-term versus long-term adherence, for example. For the providers, poor motivation was rated high as a barrier to short-term adherence, whereas the patients rated perception of minimal benefit from PFMT as the most important barrier. Facilitators of pelvic muscle training included aspects of access such as having appointments outside of the typical workday, or having childcare available, transportation, and not being bored by the exercise program or feeling that the therapist has adequate training and skills.
Data collected in the study included topics such as barriers to adherence in pelvic floor muscle training (PFMT), perception of potential benefit of PFMT, therapy-related factors including therapeutic relationship, socioeconomic factors, and issues surrounding short-term versus long-term adherence, for example. For the providers, poor motivation was rated high as a barrier to short-term adherence, whereas the patients rated perception of minimal benefit from PFMT as the most important barrier. Facilitators of pelvic muscle training included aspects of access such as having appointments outside of the typical workday, or having childcare available, transportation, and not being bored by the exercise program or feeling that the therapist has adequate training and skills.
As suggested by the authors, perhaps that most important variable agreed upon by both providers and public is that of perceived benefit. In other words, patients need to believe that the exercise program can alleviate symptoms and that what they are doing in their particular program is going to achieve positive results rather than wasting time on a home program that will not be effective. This issue is one that can be easily remedied through appropriate patient education, communication with the patient about whether or not they understand the potential value and expected recovery through program participation, and adequate training of the therapist that allows for proper diagnosis and treatment planning. The study concludes by emphasizing that health providers “need to be aware of the importance of long-term patient perception of PFMT…”
If you are interested in advancing your diagnostic or treatment planning skills, check out the pelvic floor series of continuing education courses and the many specialty courses that the Institute offers.
Coccyx pain is a frequently encountered condition in pelvic rehabilitation practices. Although sitting is one of the primary limitations for patients who present with coccyx pain, or coccygodynia, defecation can be included in the list of functional complaints. This brings to mind the question: what does the coccyx do during defecation?
Coccygeal mobility was examined using MRI in this study by Grassi and colleagues. The authors included 112 subjects for the dynamic MRI research in positions of maximal contraction as well as straining for evacuation. Included in the study were subjects who complained of constipation, sense of incomplete evacuation of bowels, pain (not coccyx pain), organ prolapse, and minor trauma. Although the MRI was completed with the patient in supine (a non-functional defecation position), the authors reported that during a straining maneuver, the coccyx moves into extension, or backwards.
What if the coccyx does not move into extension during a straining maneuver? Is it possible for the coccyx to interfere with defecation? This appears to be true for a patient who appeared as the subject in the Journal of Medical Case Reports. The patient presented with an anteverted coccyx, and complained of “…worsening rectal pain developing an hour before defecation and lasting for several hours afterwards.” Pain was also reported during sitting on a hard surface. (See the linked article for an interesting image of the coccyx position and what is described as “rectal impingement.”) The patient was treated with coccygectomy which appeared to significantly reduce the symptoms (there are no outcomes tools reported in the case study, so progress reported is vague.) Although removal of the coccyx was the treatment in this particular case, the authors state that first-line treatment for coccyx pain includes conservative measures such as seat cushioning, coccygeal massage, stretching and manipulation, and injections, and that the majority of patients will respond favorably to these interventions.
There is more to learn about the coccyx and its role in defecation, sitting, and other daily functions. Faculty member Lila Abbate teaches a great course called Coccyx Pain, Evaluation & Treatment and it is a great opportunity to learn some new evaluation and treatment techniques. Join her this October 25-26 in Bay Shore, NY.
Cognition in later years may be affected by premature menopause, according to an article published online in the British Journal of Obstetrics and Gynaecology. In the study 4,868 women at least 65 years old were assessed on a cognitive test battery and were evaluated for clinical dementia. Associations between the subject’s age at menopause, surgical versus natural menopause, use of menopausal hormone therapy, and cognitive function later in life were studied. According to introductory concepts described in the article, estrogen level changes postmenopause are associated with brain atrophy and memory complaints.
Tests were administered at baseline, and again at 2, 4 and 7 years from baseline. Tools included the Mini-Mental State Examination (MMSE) for global cognitive function, Benton’s Visual Retention Test (BVRT) for visual memory assessment, Isaacs Set Test for verbal fluency or semantic access, and the Trail Making Tests A and B for timed visual motor tasks of psychomotor speed and attention and executive function. Unrelated to cognitive function, The Rosow and Breslau mobility and Instrumental Activities of Daily Living scales, the Centre for Epidemiology Studies Depression Scale (CES-D), and other instruments were used to assess socioeconomic, demographic, lifestyle and health information. Dementia was also evaluated by a trained psychologist (or neurologist if subject was suspected to have dementia) and cases were assessed by a panel of dementia experts as a third step in the process.
Natural menopause was noted in 79% of the subjects, surgical menopause in 10%, and 11% due to other causes including radiation, chemotherapy, or unknown. Less than 1 in 7 women was currently using hormone therapy, and over 1/5 used hormone therapy at menopause (most commonly reported treatment was transdermal estradiol- median time of use was 10 years).
The authors concluded that variables such as verbal fluency, visual memory, psychomotor speed and global cognitive function can be negatively impacted by premature menopause. Specifically, premature menopause including premature ovarian failure or surgical menopause at 40 years of age or less was independently associated with increased risk of poor verbal fluency and visual memory later in life. Premature menopause was also associated with increased risk of psychomotor speed and global cognitive decline. The primary conclusion of the article is that when an ovariectomy is being considering in younger women, the potential negative impact on cognitive function should make up part of the risk/benefit discussion. Hormonal influence during various stages of a woman’s life can have a dramatic impact on many variables impacting quality of life and rehabilitation efforts. To learn more about menopause, the Institute offers several courses that contain information about rehabilitation for women throughout the lifespan.
Herman & Wallace offers an excellent course called "Menopause Rehabilitation and Symptom Management ", where you can learn about evaluating and treating menopause patients. Forward thinking therapists can provide an integrative, safe and effective/evidence based approach, such as menopausal weight loss, cardiovascular health promotion and mind body awareness, and Menopause: A Rehabilitation Approach - Atlanta, GA on March 19-20, 2016 is a great opportunity to learn such skills.
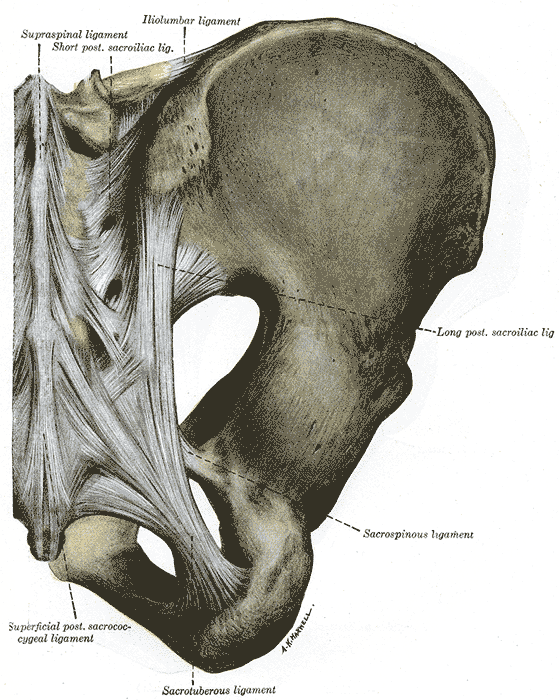
You’ve done a thorough evaluation of the lumbar spine. You’ve done all the special tests for hip pathology, but something is missing. Of course it could be a pelvic floor issue, but what else? Think about the middle child who gets ignored even if making a commotion or goes unnoticed unless being tripped over when standing still. Perhaps the missing link to your patient’s dysfunction is the sacroiliac joint, that “in between” area. If you are unsure how to assess and deal with the “middle child,” learning more about Sacroiliac Joint and Evaluation is something to add to your professional bucket list.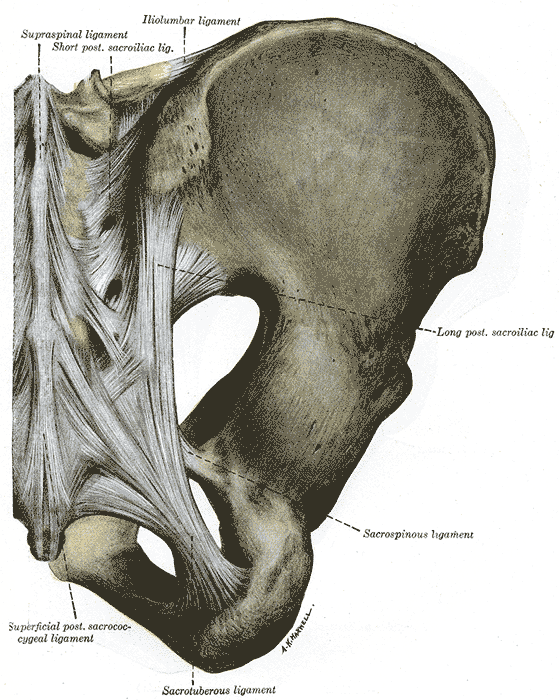
According to the special tests book by Chad Cook, a pain mapping test suggests a referral pattern of SI dysfunction as pain in the buttock unilaterally, below the level of L5, without symptoms in the midline. Often we are on a mission to make the lumbar spine the source of symptoms, but this provides some guideline as to where the pain would be located if the SI joint were the guilty party. If pain is found above L5, the SI joint is likely not the primary tissue in lesion. If the pain is bilateral, the issue is more than just SI joint.(Cook, 2013)
The special tests to diagnose SI joint dysfunction have been considered in a cluster. According to Laslett, distraction, compression, thigh thrust, Gaenslens, and Patricks are the primary tests used to assess SI dysfunction. Three or more of these tests being positive can help a clinician rule in SI joint as a diagnosis, with SI joint blocks being just as predictive. When pain cannot be centralized, and three of the tests are positive, there is a 77% probability the SI joint is the source of pain; and, in the pregnant population, there is an 89% chance the SI joint is the culprit of pain.(Laslett, 2008)
While parents keep up with the oldest and youngest, the middle child can be hard at work causing dysfunction that disrupts the whole family. Likewise, the sacroiliac joint can be hypermobile, hypomobile or have ligamentous strain, yet we therapists may ignore any signs until the lumbar spine or hip or pelvic floor are suddenly provocative. The longer an SI joint dysfunction goes undiagnosed and untreated, the greater the likelihood of pelvic floor dysfunction, secondary to its intimate relationship to the area. A catawampus ilium position on the sacrum can cause hip pain, and the ilium’s relationship to the sacrum can aggravate the lumbar spine. We just need to use all our diagnostic tools to discern what is making our patients symptomatic and then prioritize the treatment.
Taking the upcoming sacroiliac course through Herman Wallace (Sep. 12-13 in New Orleans) will make the “middle child” become respected, understood, and never left wanting again. Review the anatomy, explore and proficiently perform the special tests, and effectively implement treatment and stabilization of the SI joint during this course. You owe your patients the ability to understand the lumbar region and pelvic ring in their entirety and leave no source of pain a mystery.
References:
Cook, C., & Hegedus, E. (2013). Orthopedic physical examination tests: An evidence-based approach. Upper Saddle River, N.J.: PearsonPrentice Hall.
Laslett, M. (2008). Evidence-Based Diagnosis and Treatment of the Painful Sacroiliac Joint. The Journal of Manual & Manipulative Therapy, 16(3), 142–152.