Today's guest post comes to us from Kelly Feddema, PT, PRPC. Kelly practices pelvic floor physical therapy in the Mayo Clinic Health System in Mankato, MN, and she became a Certified Pelvic Rehabilitation Practitioner in February of 2014. To learn more about diastasis recti abdominis, consider attending Care of the Postpartum Patient!
It can be a struggle to treat patients with diastasis recti if they don't seek treatment early after giving birth. Many therapists may often find themselves thinking “if I only could have started them sooner.” Why does this condition often get missed at postpartum examinations? I personally deal with symptoms from an undiagnosed diastasis, and I'm a therapist! I didn’t really pay attention to it until I started down the road of becoming a pelvic floor therapist.
 Diastasis recti can be a difficult diagnosis to treat, as the patient may come to us when they are already one year postpartum, and not everyone agrees on the what are the best treatments. To crunch or not crunch? To use a brace or not to brace? It would be great if we had a similar healthcare system to France, where the norm is to have 10-20 postpartum rehabilitation visits with women after child birth. While therapy is available in the United States, women must ask for it.
Diastasis recti can be a difficult diagnosis to treat, as the patient may come to us when they are already one year postpartum, and not everyone agrees on the what are the best treatments. To crunch or not crunch? To use a brace or not to brace? It would be great if we had a similar healthcare system to France, where the norm is to have 10-20 postpartum rehabilitation visits with women after child birth. While therapy is available in the United States, women must ask for it.
There are many programs out there from the more well-known Tupler Technique and Mutu programs to others that come up when searching for exercise ideas. The American Physical Therapy Association (APTA) has a basic program to work on isolating the transverse abdominis (TrA) muscle and then progressing movements in the legs while keeping the TrA activated.
Some research by Paul Hodges and Diane Lee from 2016 in the Journal of Orthopedic Sports Physical Therapy indicates that narrowing the inter-rectus distance with a TrA contraction might improve force transfer between the sides of the abdominals and in turn, improve abdominal mechanics.
Another study in Physiotherapy from December of 2014 by AG Pascoal, et.al. utilized ultrasound to determine the effect of isometric contraction of the abdominal muscles on inter-rectus distance in postpartum women. They found that the while the inter-rectus distance in postpartum women was understandably higher than controls, it significantly lowered during an isometric contraction of the abdominal muscles.
One year later, a study in the same journal by MF Sancho, et.al. had similar findings when studying women who had a vaginal delivery and women who had Cesarean deliveries. They found that abdominal crunch exercises were successful in reducing inter-rectus distance, but drawing-in exercises were not.
As with a lot of research, the findings lead to more questions and ideas to explore. I think it is safe to say that starting safe re-education of the muscles as early as possible is going to provide women the most benefit in reducing diastasis recti, and that will help to prevent further issues in the abdominal and pelvic region.
As practitioners, we understand the value of a yoga practice for multiple systems. Yoga improves cardiovascular function, pulmonary function, improves flexibility, builds strength, improves balance, and cultivates resiliency. Prenatal yoga is deemed safe and widely practiced. Beyond not laying prone after the first trimester, what are modifications for practicing yoga while pregnant? Is there any evidence to demonstrate if specific yoga postures are safe from both the maternal and fetal perspective?
 Polis et al set out to determine the safety of specific yoga postures using vital signs, pulse oximetry, tacometry, and fetal heart rate monitoring. The patients were diverse in age, race, BMI, gestational age, parity, and yoga experience. Exclusionary criteria included preeclampsia, placenta previa, bleeding in the 2nd or 3rd trimester, gestational diabetes, BMI greater than 35 and other medical conditions that presented contraindications.
Polis et al set out to determine the safety of specific yoga postures using vital signs, pulse oximetry, tacometry, and fetal heart rate monitoring. The patients were diverse in age, race, BMI, gestational age, parity, and yoga experience. Exclusionary criteria included preeclampsia, placenta previa, bleeding in the 2nd or 3rd trimester, gestational diabetes, BMI greater than 35 and other medical conditions that presented contraindications.
The maternal and fetal responses were tested in 26 yoga postures. The selected postures, much like most yoga classes, offered a variety of physical positions. The standing, seated, twists and balancing postures chosen were: Easy Pose, Seated Forward Bend, Cat Pose, Cow Pose, Mountain Pose, Warrior 1, Standing Forward Bend, Warrior 2, Chair Pose, Extended Side Angle Pose, Extended Triangle Pose, Warrior 3, Upward Salute, Tree Pose, Garland Pose, Eagle Pose, Downward Facing Dog, Child’s Pose, Half Moon Pose, Bound Angle Pose, Hero Pose, Camel Pose, Legs up the Wall Pose, Happy Baby Pose, Lord of the Fishes Pose and Corpse Pose.
Balancing postures were modified to decrease fall risk. Warrior 3, Tree Pose, Eagle Pose, and Half Moon Pose were performed at the wall or using a chair for support. The addition of a yoga block to bring the floor closer to the practitioner was used for Extended Side Angle Pose, Extended Triangle Pose, and Garland Pose.
Four poses that have previously been theorized to be contraindicated were studied in this group. These postures are Child’s Pose, Corpse Pose, Downward Facing Dog, and Happy Baby. No adverse reactions were discovered for this specific population during the intervention or in the 24 hour follow-up as reported by email.
Now that we have this data, what do we do with it?
We have the opportunity to educate our non-high-risk patients that the previously theorized contraindicated postures listed above were safe for the self-selected group in this study. Those who are in high-risk categories should understand that even though yoga is not a high impact activity, there should be clearance from the OB team to ensure expectant mothers are moving as safely as possible. With proper guidance, yoga is a safe form of exercise and stress reduction which can optimize physical and mental health during the prenatal period and prepare for birth.
Dustienne Miller is the author and instructor of Yoga for Pelvic Pain. Join her in Kansas City, MO on April 7, 2018 - April 8, 2018 to learn about treating interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia with a yoga approach.
Polis RL, Gussman D, Kuo YH. Yoga in Pregnancy. Obstet Gynecol 2015;126:1237–41
A 2016 study by Kaori et al examined the effect of self administered perineal stimulation for nocturia in elderly women. A prior study using rodents found a soft roller used decreased overactive bladder syndrome (OAB), but a hard roller did not produce the same results. Kaori et al performed a similar study for elderly women in a randomized, placebo controlled, double blind crossover. Participants were 79-89 years old women who applied simulation to perineal skin for 1 minute at bedtime, using either active (soft, sticky elastomer) roller or a placebo (hard polylestrene roller). Participants did a 3-day baseline, followed by 3-day stimulation, then 4 days rest, then other stimuli for 3 days. There were 24 participants, 22 completed the study: 9 with OAB, 13 without OAB. The placement of the roller was not on the skin of the perineal body, but rather on the general peri-anal area with the diagram from the study showing an area just medial to the gluteal crease—where one would find the ischial tuberosity-- and anterior and lateral to the anal sphincter.
 Across the subjects with OAB, change with the elastomer roller (soft and sticky feel) was more statistically significant than with the hard roller. Baseline micturition for the participants was 3.2+/- 1.2 times per night, measured as the number of urination between going to bed and arising. The group as a whole did not have a statistically significant difference, measured by at least one less time arising per night. However, in the OAB group, the difference was significant. The researchers theorized that the soft and sticky texture may induce more firing of somatic afferents nerve fibers.
Across the subjects with OAB, change with the elastomer roller (soft and sticky feel) was more statistically significant than with the hard roller. Baseline micturition for the participants was 3.2+/- 1.2 times per night, measured as the number of urination between going to bed and arising. The group as a whole did not have a statistically significant difference, measured by at least one less time arising per night. However, in the OAB group, the difference was significant. The researchers theorized that the soft and sticky texture may induce more firing of somatic afferents nerve fibers.
The most commonly prescribed treatment for overactive bladder is anticholinergic therapy, but the side effects, including cognitive changes and lack of significant difference from controls, as well as the drying effect of these drugs in a post-menopausal-low-estrogen-pelvis, bring up questions of whether this is the best option in the elderly.(6)
In anesthetized animals, electrical stimulation and noxious stimuli decrease frequency of bladder contractions when applied to the perineal area (3-5). Somatic, afferent nerve stimuli (those theorized to be active with the soft roller) are used to treat OAB by modalities such as acupuncture and transcutaneous electrical stimulation to the perineum (2). So, stimulation of somatic visceral afferent nerves in the perineal region seems to have an effect on the bladder. However, with manual therapies, it seems we can also affect the somatic or visceral afferents. Essentially, visceral afferents convey information to the central nervous system about local changes in chemical and mechanical environments of a number of organ systems(7). Doing manual therapy between the urethral and bladder fascia would also theoretically cause stimulation of the visceral afferents to the central nervous system about that organ (bladder).
In our pelvic floor intro class (Pelvic Floor Level 1) at Herman Wallace, we discuss the role of Bradley’s neurology loop 3 and the inverse relationship between pelvic floor contraction (lifting the perineal area) and the bladder. One suppression technique we discuss is the contraction of the pelvic floor to quiet or inhibit bladder activity in the bladder retraining program. Bladder retraining has evidence level A (strong) for improving urgency and frequency with overactive bladder.
Clinicians who are ready to raise their manual game may try using the skills of prior series courses and adding the sophistication of manual techniques in the abdomen and pelvis to increase afferent firing in patients with OAB, as well as freeing up any fascial restrictions that may be interfering with full bladder excursion.
In the newly written Capstone course, we combine the prior level of education from the pelvic series (bladder strategies) with manual techniques to address the endopelvic fascia at the bladder base, in the fascial articulations along the perineum, and along its attachments to the coccyx, as well as combining internal work with sacral techniques to facilitate S234 afferents for bladder control. We discuss studies, such as this one, to explore advanced concepts of bladder and urethral fascial mechanics and neural entrapment affecting the bladder. We move out of the pelvic muscle and into the fascial contents of the abdominopelvic region, to allow such firing of the somatic afferents. And the perineal stimulation? We have an entire lab for perineal tissue and its effect on pelvic function. Physical therapists can manually address the perineum, urethral and bladder fascia with Capstone techniques. With such intervention, we get more CNS communication.
So, what about the roller? Well, the soft roller created change in rodents in a couple of studies. (Sato 2010). In this human study, it helped with OAB. Certainly, manual therapies in the region of the endopelvic fascia and suprapubic region may be of help for also stimulating the visceral afferents. Also, it could be worth it to have a high fall risk elderly patient with OAB type nocturia follow up your treatments with one minute of soft washcloth stroking in the area of the perineum for one minute at bedtime to see if it helps decrease the number of voids on a night time bladder diary.
Nari Clemons, PT, PRPC is a Herman & Wallace faculty member who helped author the Pelvic Floor Series Capstone: Advanced Topics in Pelvic Rehab course. She is also the creator and instructor of Pelvic Nerve Manual Assessment and Treatment.
Main study: PLoS One. 2016 Mar 22;11(3):e0151726. doi: 10.1371/journal.pone.0151726. eCollection 2016.Effects of a Gentle, Self-Administered Stimulation of Perineal Skin for Nocturia in Elderly Women: A Randomized, Placebo-Controlled, Double-Blind Crossover Trial.Iimura K1,2, Watanabe N2, Masunaga K3, Miyazaki S1,2,4, Hotta H2, Kim H5, Hisajima T1,4, Takahashi H1,4, Kasuya Y3.
2. Exp Ther Med. 2013 Sep;6(3):773-780. Epub 2013 Jul 9., Acupuncture for the treatment of urinary incontinence: A review of randomized controlled trials.Paik SH1, Han SR, Kwon OJ, Ahn YM, Lee BC, Ahn SY.
3. Guo ZF. Transcutaneious electrical nerve stimulation in the treatment of patients with poststroke urinary incontinence. Clin Interv Aging. 2014; 851-6.
4. Sato A, The impact of somatosensory input on autonomic functions. Reve Physiol Biochem Pharmacol. 1997;130;1-328
5. Sato A. Mechanism of the reflex inhibition of micturition conractions of the urinary bladder elicited by acupuncture-like stimulation in anesthetized rats. Neurosci res. 1992 15:189-98
6). Effects of a Gentle, Self-Administered Stimulation of Perineal Skin for Nocturia in Elderly Women: A Randomized, Placebo-Controlled, Double-Blind Crossover Trial. Iimura K, Watanabe N, Masunaga K, Miyazaki S, Hotta H, Kim H, Hisajima T, Takahashi H, Kasuya Y. PLoS One. 2016 Mar 22;11(3):e0151726. doi: 10.1371/journal.pone.0151726. eCollection 2016.
7) John C. Longhurst, Liang-Wu Fu, in Primer on the Autonomic Nervous System (Third Edition), 2012
I love adding flax seed to my recipes when I bake. I even hide it in yogurt with crushed graham crackers for my kids. It is a powerful nutrient that can be consumed without knowing it! Although the specific mechanism for its efficacy on prostate health continues to be researched, studies over the last several years applaud flax seed for its benefits and encourage me to keep sneaking it in my family’s diet.
 In 2008, Denmark-Wahnefried et al. performed a study to see if flax seed supplementation alone (rather than in combination with restricting dietary fat) could decrease the proliferation rate of prostate cancer prior to surgery. Basically, flax seed is a potent source of lignan, which is a phytoestrogen that acts like an antioxidant and can reduce testosterone and its conversion to dihydrotestosterone. It is also rich in plant-based omega-3 fatty acids. In this study, 161 prostate cancer patients, at least 3 weeks prior to prostatectomy, were divided into 4 groups: 1) normal diet (control); 2) 30g/day of flax seed supplementation; 3) low-fat diet; and 4) flax seed supplementation combined with low-fat diet. Results showed the rate of tumor proliferation was significantly lower in the flax seed supplemented group. The low-fat diet was proven to reduce serum lipids, consistent with previous research for cardiovascular health. The authors concluded, considering limitations in their study, flax seed is at least safe and cost-effective and warrants further research on its protective role in prostate cancer.
In 2008, Denmark-Wahnefried et al. performed a study to see if flax seed supplementation alone (rather than in combination with restricting dietary fat) could decrease the proliferation rate of prostate cancer prior to surgery. Basically, flax seed is a potent source of lignan, which is a phytoestrogen that acts like an antioxidant and can reduce testosterone and its conversion to dihydrotestosterone. It is also rich in plant-based omega-3 fatty acids. In this study, 161 prostate cancer patients, at least 3 weeks prior to prostatectomy, were divided into 4 groups: 1) normal diet (control); 2) 30g/day of flax seed supplementation; 3) low-fat diet; and 4) flax seed supplementation combined with low-fat diet. Results showed the rate of tumor proliferation was significantly lower in the flax seed supplemented group. The low-fat diet was proven to reduce serum lipids, consistent with previous research for cardiovascular health. The authors concluded, considering limitations in their study, flax seed is at least safe and cost-effective and warrants further research on its protective role in prostate cancer.
In 2017, de Amorim et al. investigated the effect of flax seed on epithelial proliferation in rats with induced benign prostatic hyperplasia (BPH). The 4 experimental groups consisting of 10 Wistar (outbred albino rats) rats each were as follows: 1) control group of healthy rats fed a casein-based diet (protein in milk); 2) healthy rats fed a flax seed-based diet; 3) hyperplasia-induced rats fed a casein diet; and 4) hyperplasia-induced rats fed a flax seed diet. Silicone pellets full of testosterone propionate were implanted subcutaneously in the rats to induce hyperplasia. Once euthanized at 20 weeks, the prostate tissue was examined for thickness and area of epithelium, individual luminal area, and total prostatic alveoli area. Results showed the hyperplasia induced rats fed a flax seed-based diet had smaller epithelial thickness as well as a reduced proportion of papillary projections found in the prostatic alveoli. These authors determined flax seed exhibits a protective role for the epithelium of the prostate in animals induced with BPH.
Bisson, Hidalgo, Simons, and Verbruggen2014 hypothesized a lignan-fortified diet could decrease the risk of BPH. The authors used an extract rich in lignan obtained from flax seed hulls. Four groups of 12 Wistar rats were used, with 1 negative control group and 3 groups with testosterone propionate (TP)-induced BPH (1 positive control, and 2 with diets containing 0.5% or 1.0% of the extract). Over a 5 week period, the 2 BPH-induced groups consuming the lignan extract starting 2 weeks prior to the BPH induction demonstrated a significant inhibition of prostate growth from the TP compared to the positive control group. These authors concluded the lignan-rich flax seed hull extract prevented BPH induction.
From BPH to prostate cancer, flax seed has proven a noteworthy supplement for preventative health. A tablespoon of flax seed in a muffin recipe is likely not a life-changing dose, but it’s a start. Nutrition Perspectives for the Pelvic Rehab Therapist enlightens practitioners with even more healthy choices, and Post-Prostatectomy Patient Rehabilitation gives you the necessary tools to help patients recover from prostate cancer.
Demark-Wahnefried, W., Polascik, T. J., George, S. L., Switzer, B. R., Madden, J. F., Ruffin, M. T., … Vollmer, R. T. (2008). Flax seed Supplementation (not Dietary Fat Restriction) Reduces Prostate Cancer Proliferation Rates in Men Presurgery. Cancer Epidemiology, Biomarkers & Prevention : A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology, 17(12), 3577–3587. http://doi.org/10.1158/1055-9965.EPI-08-0008
de Amorim Ribeiro, I.C., da Costa, C.A.S., da Silva, V.A.P. et al. (2017). Flax seed reduces epithelial proliferation but does not affect basal cells in induced benign prostatic hyperplasia in rats. European Journal of Nutrition. 56: 1201. https://doi.org/10.1007/s00394-016-1169-1
Bisson JF, Hidalgo S, Simons R, Verbruggen M. 2014. Preventive effects of lignan extract from flax hulls on experimentally induced benign prostate hyperplasia. Journal of Medicinal Food. 17(6): 650-656. http://doi.org/10.1089/jmf.2013.0046
You have been treating a highly motivated 24-year-old woman with a diagnosis of Interstitial Cystitis/Painful Bladder Syndrome (IC/BPS). The plan of care includes all styles of manual therapy, including joint mobilization, soft tissue mobilization, visceral mobilization, and strain counterstrain. You utilize neuromuscular reeducation techniques like postural training, breath work, PNF patterns, and body mechanics. Your therapeutic exercise prescription includes mobilizing what needs to move and strengthening what needs to stabilize. Your patient is feeling somewhat better, but you know she has the ability to feel even more at ease in their day to day. Is there anything else left in the rehab tool box to use?
 Kanter et al. set out to discover if mindfulness-based stress reduction (MBSR) was a helpful treatment modality for (IC/BPS). The authors were interested in both the efficacy of a treatment centered on stress reduction and the feasibility of women adopting this holistic option.
Kanter et al. set out to discover if mindfulness-based stress reduction (MBSR) was a helpful treatment modality for (IC/BPS). The authors were interested in both the efficacy of a treatment centered on stress reduction and the feasibility of women adopting this holistic option.
The American Urological Association defined first-line treatments for IC/PBS to include relaxation/stress management, pain management and self-care/behavioral modification. Second-line treatment is pelvic health rehab and medications. The recruited patients had to be concurrently receiving first- and second-line treatments, and not further down the treatment cascade like cystoscopies and Botox.
The control group (N=11) received the usual care (as described above in first- and second-line treatments). The intervention group (N=9) received the usual care plus enrollment in an 8-week MBSR course based on the work of Jon Kabat- Zinn. The weekly course was two hours in the classroom supplemented with a 4-CD guide and book for home meditation practice carryover. The course content included meditation, yoga postures, and additional relaxation techniques.
The patients who participated in the MBSR program reported improved symptoms post-treatment, and perhaps more notably, their pain self-efficacy score (PSEQ) significantly improved. All but one of the participants reported feeling “more empowered” to control their bladder symptoms.
As clinicians working so intimately with our patients, we are often given the privilege of bearing witness to the emotional pain of healing chronic, persistent pelvic pain. We understand how terribly frightening it is for our patients to feel like they will never get better and we see this come out sometimes as fear-avoidance, which has the potential to cascade further into other areas of the social sphere.
If we are able to encourage holistic methods of building strategies to handle the challenges of IC/BPS, our patients will be set up for success in ways beyond the treatment room. While we hope for immediate results in the form of pain relief (which five patients in the study did), we also can appreciate the strategy building for resiliency in the face of persistent pain. As a very strong woman said, “hope serves us best when we do not attach specific outcomes to it”.
Dustienne Miller is the author and instructor of Yoga for Pelvic Pain. Join her in Manchester, NH on September 7-8, 2019 or in Buffalo, NY on October 5-6, 2019 to learn about treating interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia with a yoga approach.
Kanter G, Kommest YM, Qaeda F, Jeppson PC, Dunivan GC, Cichowski, SB, and Rogers RG. Mindfulness-Based Stress Reduction as a Novel Treatment for Interstitial Cystitis/Bladder Pain Syndrome: A Randomized Controlled Trial. Int Urogynecol J. 2016 Nov; 27(11): 1705–1711.
The expression, “the canary in the coal mine” comes from a long ago practice of coalminers bringing canaries with them into the coalmines. These birds were more sensitive than humans to toxic gasses and so, if they became ill or died, the coalminers knew they had to get out quickly. The canaries were a kind of early warning signal before it was too late. Even though the practice has been discontinued, the metaphor lives on as a warning of serious danger to come.
Osteoporosis, which means porous bones, has been called a silent disease because often an individual doesn’t know he or she has it until they break a bone. The three common areas of fracture are the wrist, the hip, or the spine. Osteoporosis fractures are called fragility fractures, meaning they happen from a fall of standing height or less. We should not break a bone just by a fall unless there is an underlying cause which makes our bones fragile.
 Wrist fractures typically happen when a person starts to fall and puts his or her arms out to catch themselves. They often are seen in the Emergency Department but seldom followed up with an Osteoporosis workup. According to the International Osteoporosis Foundation’s Capture the Fracture program, 80% of fracture patients are never offered screening and / or treatment for osteoporosis. As professionals working with patients who often have co-morbidities, we can be the ones to screen for osteoporosis and balance problems, particularly if our patients have a history of fractures. These screens include the following:
Wrist fractures typically happen when a person starts to fall and puts his or her arms out to catch themselves. They often are seen in the Emergency Department but seldom followed up with an Osteoporosis workup. According to the International Osteoporosis Foundation’s Capture the Fracture program, 80% of fracture patients are never offered screening and / or treatment for osteoporosis. As professionals working with patients who often have co-morbidities, we can be the ones to screen for osteoporosis and balance problems, particularly if our patients have a history of fractures. These screens include the following:
1. Check for the three most common signs of osteoporosis:
a. History of fractures
b. Hyper-kyphosis of the thoracic spine
c. Loss of height equal or greater than 4 cm.
2. Grip Strength
Low grip strength in women is associated with low bone density1
3. Rib-pelvic distance- less than two fingerbreadths.
With the patient standing with their back to you, arms raised to 90 degrees, check the distance from the lowest rib to the iliac crest. Two fingerbreadths or less may be indicative of a vertebral fracture.
A prior fracture is associated with an 86% increased risk of any fracture based on a 2004 meta-analysis by Kanis, Johnell, and De Laet in Bone 2. Fracture predicts fracture. It is our duty as professionals and as human beings to intervene by screening and referring out even if this is not the primary reason we are treating this patient. Fractures from osteoporosis can be devastating, resulting in increased risk of mortality at worst and a diminished quality of life at best. Look for the canaries in the coal mine. Our patients deserve to live the quality of life they envision.
Deb Gulbrandson, PT, DPT, CEEAA teaches the Meeks Method for Osteoporosis Management seminars for Herman and Wallace around the country.
1. Dixon WG et al. Low grip strength is associated with bone mineral density and vertebral fracture in women. Rheumatology 2005;44:642-646
2. Kanis JA, Johnell O, De Laet C, et al. (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35:375
When I work prn in inpatient rehabilitation, I have access to each patient’s chart and can really focus on the systems review and past medical history, which often gives me ample reasons to ask about pelvic floor dysfunction. So, of course, I do. I have yet to find a gynecological cancer survivor who does not report an ongoing struggle with urinary incontinence. And sadly, they all report that they just deal with it.
 Bretschneider et al.2016 researched the presence of pelvic floor disorders in females with presumed gynecological malignancy prior to surgical intervention. Baseline assessments were completed by 152 of the 186 women scheduled for surgery. The rate of urinary incontinence (UI) at baseline was 40.9% for the subjects, all of whom had uterine, ovarian, or cervical cancer. Stress urinary incontinence (SUI) was reported by 33.3% of the women, urge incontinence (UI) by 25%, fecal incontinence (FI) by 3.9%, abdominal pain by 47.4%, constipation by 37.7%, and diarrhea by 20.1%. The authors concluded pelvic floor disorders are prevalent among women with suspected gynecologic cancer and should be noted prior to surgery in order to provide more thorough rehabilitation for these women post-operatively.
Bretschneider et al.2016 researched the presence of pelvic floor disorders in females with presumed gynecological malignancy prior to surgical intervention. Baseline assessments were completed by 152 of the 186 women scheduled for surgery. The rate of urinary incontinence (UI) at baseline was 40.9% for the subjects, all of whom had uterine, ovarian, or cervical cancer. Stress urinary incontinence (SUI) was reported by 33.3% of the women, urge incontinence (UI) by 25%, fecal incontinence (FI) by 3.9%, abdominal pain by 47.4%, constipation by 37.7%, and diarrhea by 20.1%. The authors concluded pelvic floor disorders are prevalent among women with suspected gynecologic cancer and should be noted prior to surgery in order to provide more thorough rehabilitation for these women post-operatively.
Ramaseshan et al.2017 performed a systematic review of 31 articles to study pelvic floor disorder prevalence among women with gynecologic malignant cancers. Before treatment of cervical cancer, the prevalence of SUI was 24-29% (4-76% post-treatment), UI was 8-18% (4-59% post-treatment), and FI was 6% (2-34% post- treatment). Cervical cancer treatment also caused urinary retention (0.4-39%), fecal urge (3-49%), dyspareunia (12-58%), and vaginal dryness (15-47%). Uterine cancer showed a pre-treatment prevalence of SUI (29-36%), UUI (15-25%), and FI (3%) and post-treatment prevalence of UI (2-44%) and dyspareunia (7-39%). Vulvar cancer survivors had post-treatment prevalence of UI (4-32%), SUI (6-20%), and FI (1-20%). Ovarian cancer survivors had prevalence of SUI (32-42%), UUI (15-39%), prolapse (17%) and sexual dysfunction (62-75%). The authors concluded pelvic floor dysfunction is prevalent among gynecologic cancer survivors and needs to be addressed.
Lindgren, Dunberger, & Enblom2017 explored how gynecological cancer survivors (GCS) relate their incontinence to quality of life, view their physical activity/exercise ability, and perceive pelvic floor muscle training. The authors used a qualitative interview content analysis study with 13 women, age 48–82. Ten women had UI and 3 had FI after treatment (2 had radiation therapy, 5 had surgery, and 6 had surgery as well as radiation therapy). The results showed a reduction in physical and psychological quality of life and sexual activity because of incontinence. Having minimal to no experience or even awareness of pelvic floor training, 9 out of the 10 women were willing to spend 7 hours a week to improve their incontinence. Practical and emotional coping strategies also helped these women, and they all declared they had the cancer treatments without being informed of the risk of incontinence, which impacted their attitude and means of handling the situation.
Research shows incontinence is a common occurrence after gynecological cancer treatment. It impacts quality of life after surviving a serious illness, and many women do not know pelvic floor therapy can improve their situation. Oncology and the Female Pelvic Floor is an ideal course for practitioners to take to help increase their knowledge on how to educate and treat this population.
Bretschneider, C. E., Doll, K. M., Bensen, J. T., Gehrig, P. A., Wu, J. M., & Geller, E. J. (2016). Prevalence of pelvic floor disorders in women with suspected gynecological malignancy: a survey-based study. International Urogynecology Journal, 27(9), 1409–1414. http://doi.org/10.1007/s00192-016-2962-3
Ramaseshan, A.S., Felton, J., Roque, D., Rao, G., Shipper, A.G., Sanses, T.V.D. (2017). Pelvic floor disorders in women with gynecologic malignancies: a systematic review. International Urogynecology Journal. http://doi.org/10.1007/s00192-017-3467-4
Lindgren, A., Dunberger, G., & Enblom, A. (2017). Experiences of incontinence and pelvic floor muscle training after gynaecologic cancer treatment. Supportive Care in Cancer, 25(1), 157–166. http://doi.org/10.1007/s00520-016-3394-9
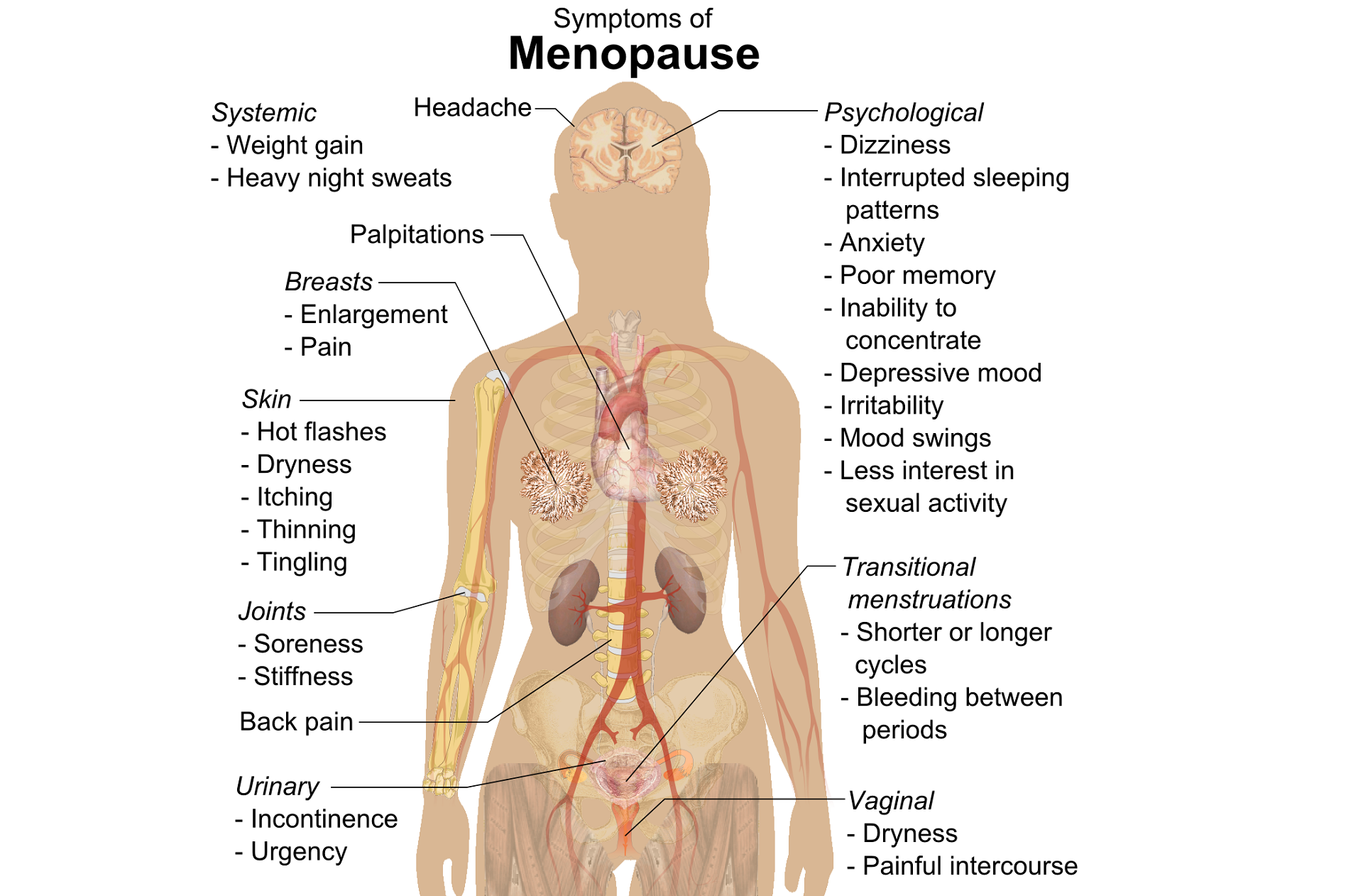
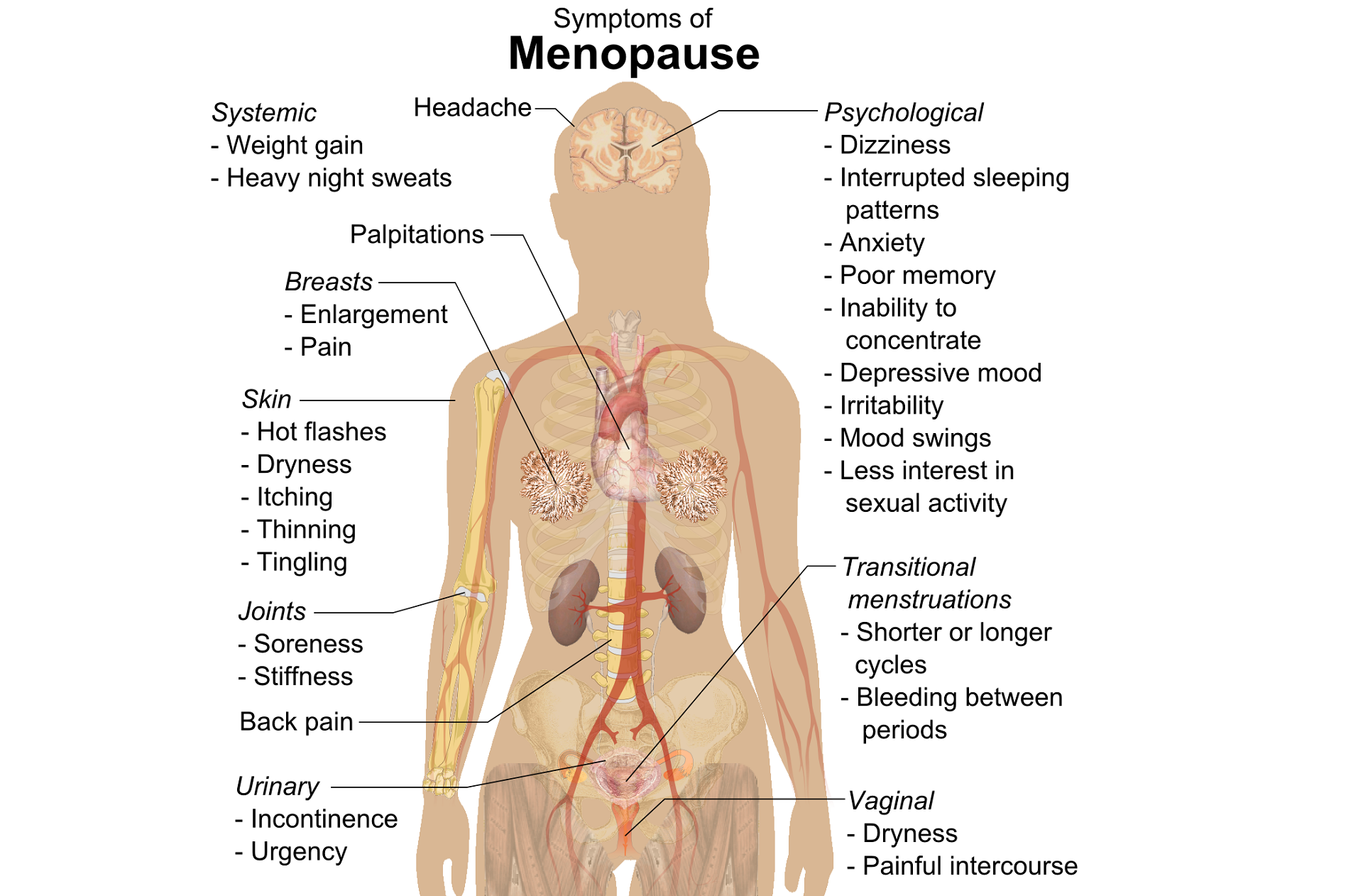
Perimenopausal pelvic health issues are, for many of us, some of the most common issues that we see in the women that we work with. Urinary incontinence is one of the most important issues for peri- and postmenopausal women. In Melville’s study1 of U.S. women, half of the participants between the ages of 50 and 90 experienced urine leakage every month. Zhu’s 2008 study2 looked at the risk factors for SUI - Multiple vaginal deliveries, Age/postmenopausal status, Chronic pelvic pain, Obesity, lack of exercise, constipation, and hypertension. But what is not often (enough) looked at in the research, is the link between urinary dysfunction and sexual dysfunction – usually because questions aren’t asked or assumptions are made. In Mestre et al’s 2015 paper3, they write ‘…Integrating sexual health in clinical practice is important. In women with pelvic floor disorders, the evaluation of the anatomical defects, lower urinary tract function and the anorectal function often receives more attention than sexual function.’
 But are they linked?
But are they linked?
In Moller’s exploration of this topic, they report that lower urinary tract symptoms (LUTS) have a profound impact on women’s physical, social, and sexual wellbeing. Unsurprisingly (to pelvic rehab specialists at least!), they found that the LUTS are likely to affect sexual activity. Conversely, sexual activity may affect the occurrence of LUTS. The aims of the Moller study were to elucidate to which extent LUTS affect sexual function and to which extent sexual function affect LUTS in an unselected population of middle-aged women in 1 year. A questionnaire was sent to 4,000 unselected women aged 40–60 years. Compared to women having sexual relationship, a statistically significant 3 to 6 fold higher prevalence of LUTS was observed in women with no sexual relationship. In women who ceased sexual relationship an increase in the de novo occurrence of most LUTS was observed. In women who resumed sexual relationship a decrease in LUTS was observed. In women whose sexual activity was unchanged no change in the occurrence of LUTS. So they rightfully concluded ‘…sexual inactivity may lead to LUTS and vice versa.’
In my Menopause course, we will explore the range of perimenopausal pelvic health issues that many women face and their inter-related nature – not just with each other but also how orthopaedic, endocrine and gastro-intestinal health issues influence pelvic health and wellness. Interested in learning more? Come and join the conversation in California in February 2018!
1. Melville JL, et al. Urinary incontinence in US women: a population-based study. Arch Intern Med 2005;165(5):537-42 - See more at: http://www.nursingcenter.com/lnc/JournalArticle?Article_ID=698029#sthash.cm8A90tS.dpuf
2. Zhu L1, Lang J, Wang H, Han S, Huang J. Menopause. 2008 May-Jun;15(3):566-9. The prevalence of and potential risk factors for female urinary incontinence in Beijing, China
3. Mestre M, Lleberia J, Pubill J, Espuña-Pons M Actas Urol Esp. 2015 Apr;39(3):175-82. Epub 2014 Aug 28. Questionnaires in the assessment of sexual function in women with urinary incontinence and pelvic organ prolapse.
When reading published research on a subject matter directly relating to what we do in our career, we may need to remember the expression, “Don’t throw the baby out with the bathwater.” Sometimes the test results for a promising hypothesis are not statistically significant, and we can close our minds to the concept entirely. If we skim the abstract and hone in on the “results” or “conclusion” rather than reading the whole article, particularly a study’s limitations, we may drop a sound clinical pearl down the drain.
A research article published in May 2017 by Amorim et al., looked at the force generation and maintenance of the pelvic floor muscles when combined with hip adduction or abduction contractions. They hypothesized that pelvic floor muscle (PFM) contraction combined with hip abduction contraction (rather than adduction) should produce a greater PFM contraction because of the myofascial connection of the obturator internus to the levator ani muscle. The study included 20 nulliparous women without pelvic floor dysfunction. The pelvic floor muscle contraction was measured in isolation, with 30% and 50% maximum hip adduction contraction, and with 30% and 50% maximum hip abduction contraction. The forces were measured with a cylindrical, intravaginal strain-gauge for PFM and another strain-gauge around the hips for adduction/abduction force generation. The women were given visual feedback to help them obtain the required hip contraction force. An average of 3 contractions (10 seconds each with a 1 minute rest) was used for each condition. This was all performed again 4 weeks later.
 The results of this study by Amorim et al.2017 did not support the hypothesis. No statistically significant difference was found among any of the conditions measured. The intravaginal PFM force generation was not different when combined with hip abduction versus hip adduction contraction. Neither hip adduction nor abduction made a significant change in force of the PFM contraction compared to isolated PFM contraction. The authors had to conclude there is no evidence to support the efficacy of combining PFM training with contraction of the hip abductors or adductors.
The results of this study by Amorim et al.2017 did not support the hypothesis. No statistically significant difference was found among any of the conditions measured. The intravaginal PFM force generation was not different when combined with hip abduction versus hip adduction contraction. Neither hip adduction nor abduction made a significant change in force of the PFM contraction compared to isolated PFM contraction. The authors had to conclude there is no evidence to support the efficacy of combining PFM training with contraction of the hip abductors or adductors.
Even Amorim et al., admitted the study had limitations, and the benefit of PFM training combined with the hip contractions could exist under more “chronic” conditions rather than the brief testing period used in the research. They also used healthy women who had no children, which could make for a different outcome than if they used women with pelvic dysfunction. The specificity of the strain-gauges and the feedback given was not flawless. The authors encouraged further study on the subject. Perhaps there could be an important correlation between PFM and hip abduction contraction not yet found.
Reading research is an integral part of being a responsible healthcare professional, but without solid discernment, we could be entranced or blinded by bubbles as the “baby” escapes us. Taking a course (online or in person) that enhances overall understanding of a subject matter such as the correlation between the lumbopelvic region and the hip can equip the practitioner with a broader foundation upon which clinical decisions can be made. Recognize what concepts to keep and which to wash away, and realize one patient may benefit from what a randomized controlled trial could not cleanly prove to work.
Amorim, A. C., Cacciari, L. P., Passaro, A. C., Silveira, S. R. B., Amorim, C. F., Loss, J. F., & Sacco, I. C. N. (2017). Effect of combined actions of hip adduction/abduction on the force generation and maintenance of pelvic floor muscles in healthy women. PLoS ONE, 12(5), e0177575. http://doi.org/10.1371/journal.pone.0177575
One of my greatest nemeses when I was racing at 30 years of age was a woman in her 50’s. Although I hated losing to her, I was always inspired by her speed at her age. She motivated me to continue training hard, realizing my fastest days could be yet to come. As I now race in the “master’s” category in my 40’s, I still find myself crossing the line behind an older competitor occasionally. Research shows I should take heart and keep in step with females who continue to move their bodies beyond menopause.
 Mazurek et al., (2017) studied how organized physical activity among post-menopausal women could reduce cardiovascular risk. The study included 35 sedentary women aged 64.7 ± 7.7 years who had no serious health issues. They all participated in the Active Leisure Time Programme (ALTP) 3 times per day for 40–75 minute sessions for 2 weeks, including 39 physical activities. Exercise intensity stayed within 40–60% of maximal HR, and ratings of perceived exertion (RPE) on the Borg scale stayed between 8 and 15 points. This exercise training was followed by 3 months of the Prevent Falls in the Elderly Programme (PFEP), which is a general fitness exercise program to prevent falls in the elderly. Health status was measured at baseline, 2 weeks into the program, and after 3 months. The results showed significant reductions in central obesity, which increased the exercise and aerobic capacity of the subjects and improved lipid profiles. A significant reduction also occurred in the absolute 10-year risk of death from cardiac complications. The authors concluded these exercise programs could be effective in preventing primary and secondary cardiovascular disease in the >55 years old female population.
Mazurek et al., (2017) studied how organized physical activity among post-menopausal women could reduce cardiovascular risk. The study included 35 sedentary women aged 64.7 ± 7.7 years who had no serious health issues. They all participated in the Active Leisure Time Programme (ALTP) 3 times per day for 40–75 minute sessions for 2 weeks, including 39 physical activities. Exercise intensity stayed within 40–60% of maximal HR, and ratings of perceived exertion (RPE) on the Borg scale stayed between 8 and 15 points. This exercise training was followed by 3 months of the Prevent Falls in the Elderly Programme (PFEP), which is a general fitness exercise program to prevent falls in the elderly. Health status was measured at baseline, 2 weeks into the program, and after 3 months. The results showed significant reductions in central obesity, which increased the exercise and aerobic capacity of the subjects and improved lipid profiles. A significant reduction also occurred in the absolute 10-year risk of death from cardiac complications. The authors concluded these exercise programs could be effective in preventing primary and secondary cardiovascular disease in the >55 years old female population.
Nyberg et al., (2016) took a physiological look at exercise training on the vascular function of pre- and postmenopausal women, studying the prostanoid system. Prostanoids are vasoconstrictors, and prostacyclins are vasodilators. The loss of estrogen in menopause affects the ability of the vasodilators to function properly or even be produced, thus contributing to vascular decline. The authors checked the vasodilator response to an intra-arterial fusion of a prostacyclin analog epoprostenol as well as acetylocholine in 20 premenopausal and 16 early postmenopausal women before and after a 12-week exercise program. Pre-exercise, the postmenopausal women had a reduced vasodilator response. The women also received infusion of ketorolac (an inhibitor of cyclooxygenase) along with acetylcholine, creating a vasoconstriction effect, and the vascular response was reduced in both groups. The infusions and analyses were performed again after 12 weeks of exercise training, and the exercise training increased the vasodilator response to epoprostenol and acetylcholine in the postmenopausal group. The reduced vasodilator response to epoprostenol prior to exercise in early postmenopausal women suggests hormonal changes affect the capacity of prostacyclin signaling; however, the prostanoid balance for pre and postmenopausal women was unchanged. Ultimately, the study showed exercise training can still have a positive effect on the vascularity of newly postmenopausal women.
There are randomized controlled clinical trials and scientific evidence supporting the importance to keep moving as women (and men) age. Menopause should not be a self-proclaimed pause from activity in life. Not everyone has to become a competitive athlete to preserve cardiac and vascular integrity as we age, but we need to engage in some physical activity to keep our systems running for years to come.
Those interested in learning more about menopause rehabilitation considerations should consider attending Menopause Rehabilitation and Symptom Management.
Mazurek, K., Żmijewski, P., Kozdroń, E., Fojt, A., Czajkowska, A., Szczypiorski, P., Tomasz Mazurek, T. (2017). Cardiovascular Risk Reduction in Sedentary Postmenopausal Women During Organised Physical Activity. Kardiologia Polska. 75, 5: 476–485. http://doi:10.5603/KP.a2017.0035
Nyberg, M., Egelund, J., Mandrup, C., Nielsen, M., Mogensen, A., Stallknecht, B., Bangsbo, J., Hellsten, Y. (2016). Early Postmenopausal Phase Is Associated With Reduced Prostacyclin-Induced Vasodilation That Is Reversed by Exercise Training: The Copenhagen Women Study. Hypertension. 68:1011-1020. https://doi.org/10.1161/HYPERTENSIONAHA.116.07866