Faculty member Lila Bartkowski- Abbate PT, DPT, MS, OCS, WCS, PRPC teaches the Bowel Pathology, Function, Dysfunction and the Pelvic Floor course for Herman & Wallace. Join her in Tampa on April 2-3, or one of the other two events currently open for registration.
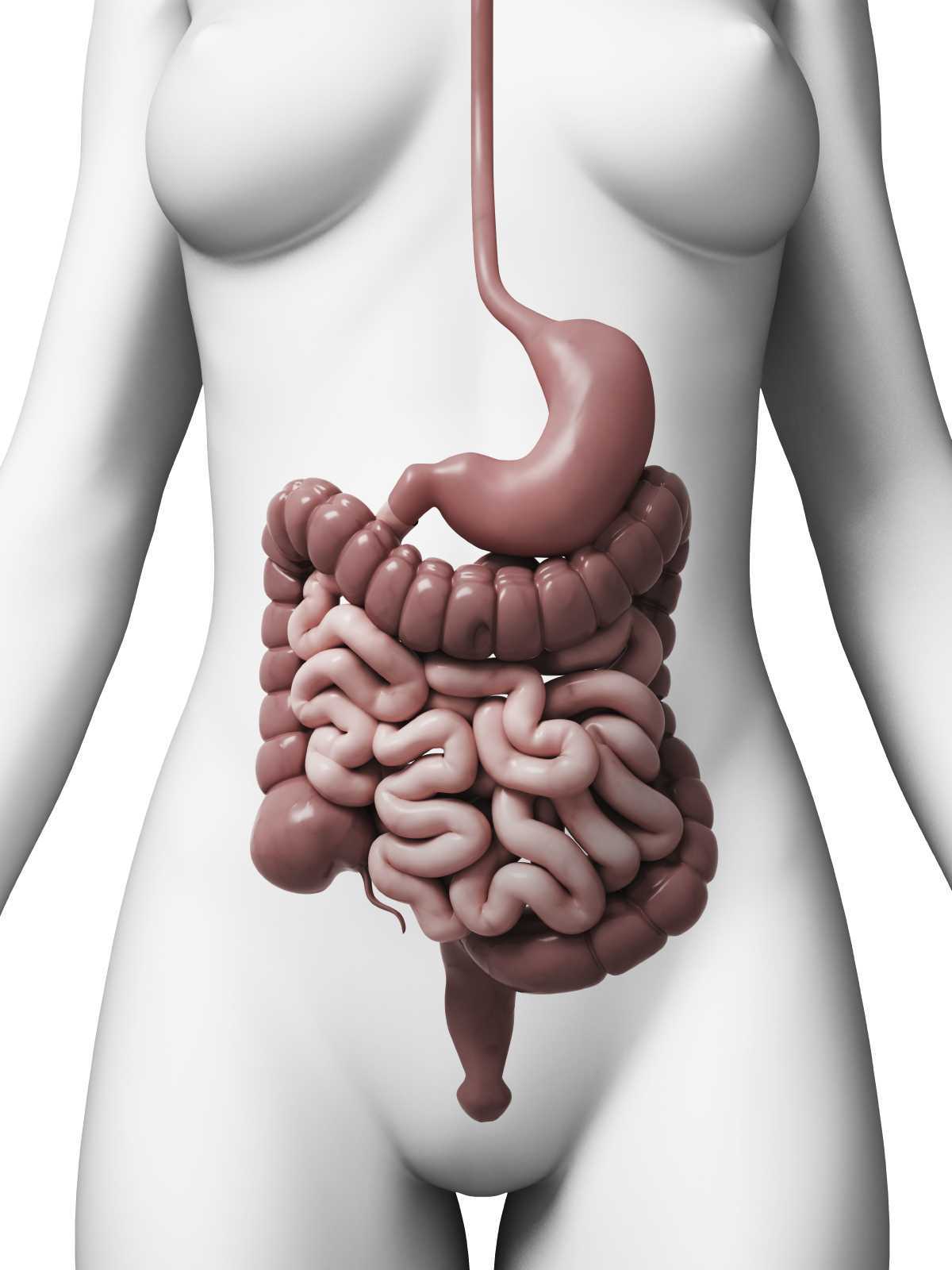
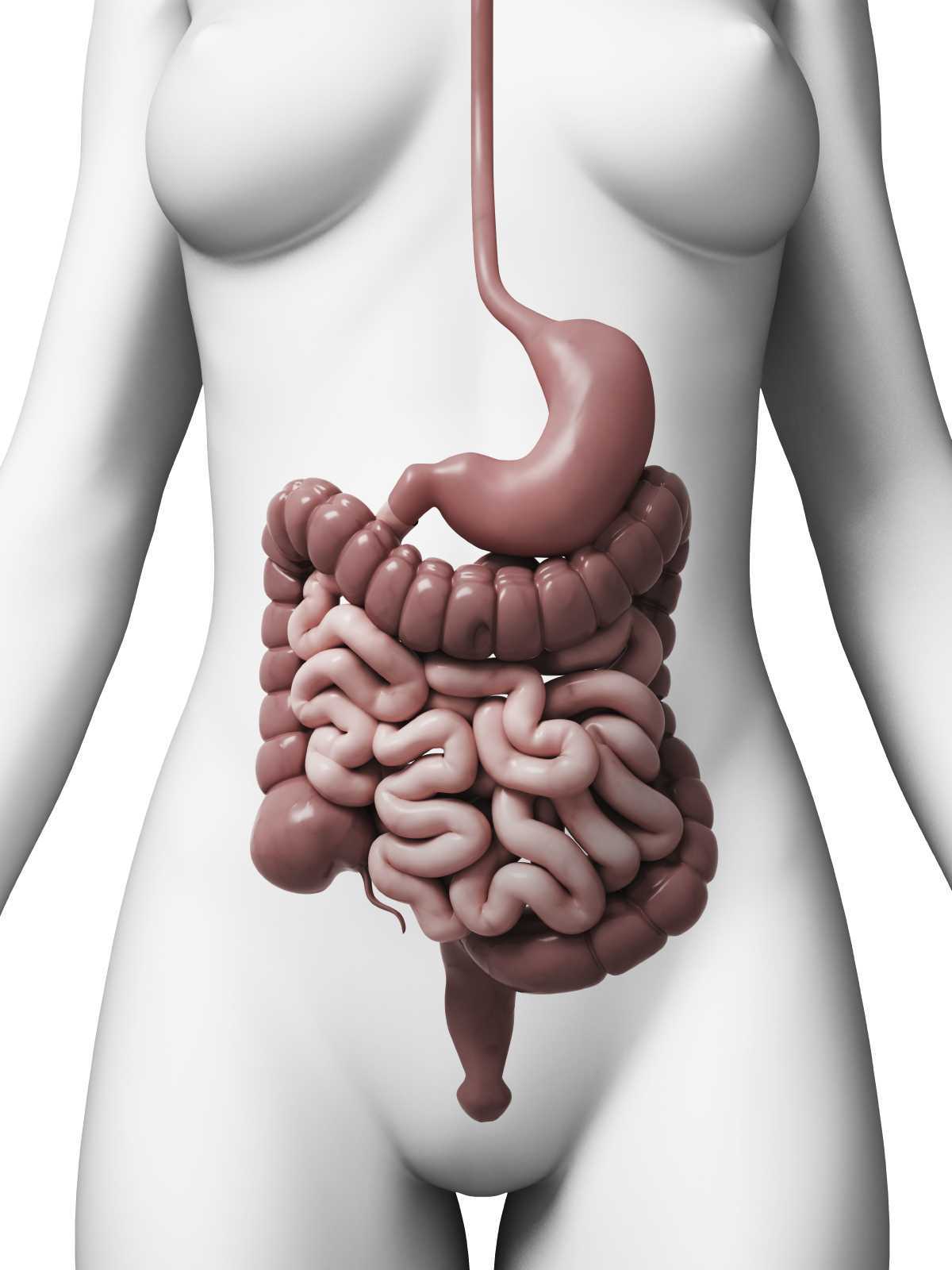 Constipation, an often under reported health issue, afflicts about 30% of Americans. ¹ The diagnosis of chronic constipation may seem like a simple concept, however the etiology of chronic constipation presents itself in many different forms. Dyssynergic defecation is one of many factors that can lead to a presentation of chronic constipation in a patient. Dyssynergic defecation or “paradoxical contraction” occurs when the muscles of the abdominals, puborectalis sling, and external anal sphincter function inappropriately while attempting a bowel movement. ² The lack of coordination of these muscles results in a contraction versus a lengthening of the pelvic floor muscles with baring down. Dyssynergic defecation is different than a structural issue such as a rectocele or hemorrhoids causing the inability to pass stool effectively or constipation due to slow colon transit time or pathological disease. Making the diagnosis of dyssynergic defecation by symptoms alone is often not reliable secondary to overlap of similar symptoms with chronic constipation due to factors such as a structural issue, irritable bowel syndrome (IBS), or irritable bowel disease (IBD). The diagnosis of dyssynergic defecation can be difficult and is often made through physiologic testing such as balloon expulsion testing or MRI with defecography. ² However, physical therapists can often manually feel that a paradoxical contraction is happening when asking a patient to bare down on evaluation.
Constipation, an often under reported health issue, afflicts about 30% of Americans. ¹ The diagnosis of chronic constipation may seem like a simple concept, however the etiology of chronic constipation presents itself in many different forms. Dyssynergic defecation is one of many factors that can lead to a presentation of chronic constipation in a patient. Dyssynergic defecation or “paradoxical contraction” occurs when the muscles of the abdominals, puborectalis sling, and external anal sphincter function inappropriately while attempting a bowel movement. ² The lack of coordination of these muscles results in a contraction versus a lengthening of the pelvic floor muscles with baring down. Dyssynergic defecation is different than a structural issue such as a rectocele or hemorrhoids causing the inability to pass stool effectively or constipation due to slow colon transit time or pathological disease. Making the diagnosis of dyssynergic defecation by symptoms alone is often not reliable secondary to overlap of similar symptoms with chronic constipation due to factors such as a structural issue, irritable bowel syndrome (IBS), or irritable bowel disease (IBD). The diagnosis of dyssynergic defecation can be difficult and is often made through physiologic testing such as balloon expulsion testing or MRI with defecography. ² However, physical therapists can often manually feel that a paradoxical contraction is happening when asking a patient to bare down on evaluation.
Patients with dyssynergic defecation may present to pelvic floor physical therapy with complaints of: ¹ ²
- Abdominal symptoms such as bloating, pain, and cramping
- Poor response to laxatives and fiber supplementation that does not fully resolve their issue
- Have had testing for anatomical or neurological abnormalities with no significant findings
- Complaints of concomitant pelvic pain due to over activity of the pelvic floor muscles
Physical Therapists specializing in pelvic floor rehab can be a valuable part of the medical team with treating these patients. Biofeedback training by physical therapists has been shown to decrease anorectal related constipation symptoms and abdominal symptoms in patients with dyssynergic defecation. In a sample of 77 patients with dyssynergic defecation, physical therapists provided biofeedback training for 6-8 weeks that included manual and verbal feedback, surface EMG, exercises using a rectal catheter, rectal ballooning to improve rectal sensory abnormalities, ultrasound, pelvic floor and abdominal massage, electrical stimulation if needed, and core strengthening and stretching to improve the patients’ maladaptive habits while attempting to pass a bowel movement. Significant decreases were seen on all three domains (abdominal, rectal, and stool) on the PAC-SYM (Patient Assessment of Constipation) questionnaire post biofeedback training. ² It is noteworthy that 74% of these patients presented to the clinic with complaints of abdominal symptoms such as bloating, pain, discomfort, and cramping.
Knowing how to effectively treat these patients and ask the right questions is valuable in the scheme of pelvic floor rehab secondary to overlapping symptoms of different causes of chronic constipation. Physical therapists are able to provide these patients with conservative treatment that can effectively improve or eliminate their problem, recognize dyssynergic defecation as a possible differential diagnosis, and refer to the appropriate medical professional for further testing. Recognizing and treating dyssynergic defecation is something physical therapists will learn how to become effective at in the upcoming Herman and Wallace Course: Bowel Pathology, Function, Dysfunction & the Pelvic Floor April 2-3 in Tampa, FL and October 8-9 in Fairfield, CA.
1. Sahin M, Dogan I, Cengiz M et al. (2015). The impact of anorectal biofeedback therapy on quality of life of patients with dyssynergic defecation. Turk J Gastroenterol. 26(2):140-144
2. Baker J, Eswaran S, Saad R, et al. (2015). Abdominal symptoms are common and benefit from biofeedback therapy in patients with dyssynergic defecation. Clin Transl Gastroenterol. 30(6)e105. doi: 10.1038/ctg.2015.3
Many therapists start their career feeling a bit intimidated to work with women who are pregnant. A common and understandable concern is that something the therapist will do during examination or treatment may harm the patient. While there are certainly things to avoid when working with a patient who is pregnant there are also many therapeutic strategies that can help a woman thrive during her pregnancy and beyond. When women have pre-existing issues such as a disease or physical challenge, or when she develops an illness during pregnancy, the therapist needs to rely upon more knowledge- this knowledge is something she rarely learns in school, but more likely in continuing education environments. A recent article asked the question “are women getting sicker, and are there more high-risk pregnancies now than ever before?”
 Researchers studied trends in maternal morbidity and mortality in the United States in order to answer this question, and the answer is a definitive “yes”. Several studies describe increases in the rates of maternal morbidity, with issues such as cardiac and pulmonary complications, and the severe blood pressure fluctuations associated with eclampsia. Gestational diabetes, and postpartum rates for hemorrhage, perineal lacerations, and maternal infections have also risen. Part of the reason for more women carrying pregnancies more successfully or longer when they are ill may be contributed to newer treatments for conditions such as diabetes, yet this does not explain entirely the increase in maternal morbidity. Increased cesarean births, longer labors with epidural anesthesia, pre-pregnancy obesity, rates of multifetal pregnancies, and the rising age of mothers are other factors to be considered.
Researchers studied trends in maternal morbidity and mortality in the United States in order to answer this question, and the answer is a definitive “yes”. Several studies describe increases in the rates of maternal morbidity, with issues such as cardiac and pulmonary complications, and the severe blood pressure fluctuations associated with eclampsia. Gestational diabetes, and postpartum rates for hemorrhage, perineal lacerations, and maternal infections have also risen. Part of the reason for more women carrying pregnancies more successfully or longer when they are ill may be contributed to newer treatments for conditions such as diabetes, yet this does not explain entirely the increase in maternal morbidity. Increased cesarean births, longer labors with epidural anesthesia, pre-pregnancy obesity, rates of multifetal pregnancies, and the rising age of mothers are other factors to be considered.
The more we know as health care providers about how maternal morbidity affects our rehabilitation efforts, the more we can contribute to a woman’s pregnancy and postpartum health. If you would like to learn more about caring for women during pregnancy and during the postpartum period, Herman & Wallace offers the Pregnancy and Postpartum Series. The following courses are available this year:
Care of the Pregnant Patient - Somerset, NJ
Apr 30, 2016 - May 1, 2016
Care of the Pregnant Patient - Akron, OH
Sep 10, 2016 - Sep 11, 2016
Peripartum Special Topics - Seattle, WA
Nov 12, 2016 - Nov 13, 2016
Tillett, J. (2015). Increasing Morbidity in the Pregnant Population in the United States. The Journal of perinatal & neonatal nursing, 29(3), 191-193.
As pelvic rehabilitation providers, it may be safe to assume a lot of us are treating adults with bladder and bowel dysfunction. Often we get questions from these patients about treatment for children with voiding dysfunction. How comfortable are we treating children for these problems and what would we do? Pediatric voiding dysfunction and bowel problems are common and can have significant consequences to quality of life for the child and the family, as well as negative health consequences to the lower urinary tract if left untreated. No clear gold standard of treatment for pediatric voiding dysfunction has been established and treatments range from behavioral therapy to medication and surgery.
 A randomized controlled trial in 2013 that was published in European Journal of Pediatrics, explores treatment options for pediatric voiding dysfunction. Pediatric voiding dysfunction is defined as involuntary and intermittent contraction or failure to relax the urethral striated sphincter during voluntary voiding. The dysfunctional voiding can present with variable symptoms including urinary urgency, urinary frequency, incontinence, urinary tract infections, and abnormal flow of urine from bladder back up the ureters (vesicoureteral reflux).
A randomized controlled trial in 2013 that was published in European Journal of Pediatrics, explores treatment options for pediatric voiding dysfunction. Pediatric voiding dysfunction is defined as involuntary and intermittent contraction or failure to relax the urethral striated sphincter during voluntary voiding. The dysfunctional voiding can present with variable symptoms including urinary urgency, urinary frequency, incontinence, urinary tract infections, and abnormal flow of urine from bladder back up the ureters (vesicoureteral reflux).
The 2013 study compared 60 children over one year who were diagnosed with dysfunctional voiding into two treatment groups. One group received behavioral urotherapy combined with PFM (pelvic floor muscle) exercises while the other group received just behavioral urotherapy. The behavioral urotherapy consisted of hydration, scheduled voiding, toilet training, and high fiber diet. Voiding pattern, EMG (electromyography) activity during voids, urinary urgency, daytime wetting, and PVR (post-void residue) were assessed at the beginning and end of the one year study with parents completing a voiding and bowel habit chart as well as uroflowmetry with pelvic floor muscle sEMG (surface electromyography) was administered to the child for voiding metrics.
All parents and children in both groups received education about urinary and gastrointestinal tract function as well as healthy bladder habits, effects of high fiber diet, scheduled voiding, and normal mechanics of toilet training. For the group that completed PFM exercises and education, they participated in 12 sessions (2x/week for 30 minutes) to learn the PFM exercises under the guidance of a single physical therapist. There was bimonthly follow up for both groups throughout the 12 months to ensure retention and application of the behavioral urotherapy.
The goal of the PFM exercises for the children was too restore the normal function of the PFM’s and their coordination with abdominal muscles. The exercises that the children completed, included exercises with and without a swiss ball. The exercises without a swiss ball included breathing with the diaphragm, Transversus Abdominus muscle isolation, hip adductor squeeze (isolation), bridging with PFM relaxation, and cat/camel to improve lumbopelvic coordination. Swiss ball exercises included seated PFM contraction and relaxation exercise with a seated lift and relax, supine bridge with roll out on the ball with PFM contraction, and supine swiss ball lift with the legs and pelvic contraction. (Pictures and more details about how the exercises were carried out in the article itself.)
The conclusion of the study was that the functional PFM exercises with swiss ball combined with behavioral urotherapy reduced the frequency of urinary incontinence, PVR (post void residue), and the severity of constipation in children with voiding dysfunction. The children in the combined group showed improvements with voiding pattern, reduced EMG activity during voids, reduced urgency, reduced daytime wetting, and improvements with more complete emptying with voids (reduced PVR).
The Functional PFM exercises are easy to teach and easy for children to complete. They are a safe, inexpensive, and effective treatment option for children with dysfunctional voiding. PFM exercises combined with behavioral urotherapy seems to be a logical treatment option for treating pediatric voiding dysfunction.
To learn more about pediatric bowel and bladder dysfunction and treatment for it consider attending Dawn Sandalcidi's Pediatric and Pelvic Floor Dysfunction course. The three opportunities in 2016 are Pediatric Incontinence - Augusta, GA April 16-18, Pediatric Incontinence - Torrance, CA June 11-12, and Pediatric Incontinence - Waterford, CT on September 17-18.
Seyedian, S. S. L., Sharifi-Rad, L., Ebadi, M., & Kajbafzadeh, A. M. (2014). Combined functional pelvic floor muscle exercises with Swiss ball and urotherapy for management of dysfunctional voiding in children: a randomized clinical trial. European Journal of Pediatrics, 173(10), 1347-1353.
Rarely does a patient with sacroiliac joint dysfunction come to see us with a goal of having surgery. Sometimes surgery winds up being the last resort for relief if our efforts and the patient’s commitment to physical therapy and prescribed exercises fail. Some of the most recent research shows positive results from minimally invasive surgery; however, the bottom line is to make sure the most educated, clinically accurate diagnosis has been made in implicating the SI joint as the source of pain.
Capobianco et al (2015) performed a prospective multi-center trial regarding SI joint fusion using a minimally invasive technique in women with post-partum pain in the pelvic girdle. Eligibility for the study required subjects to have 3 out of 5 positive SI joint stress tests and at least 50% relief with image-guided intra-articular SI joint block with a local anesthetic. Of the 172 subjects in the study, 20 of the 100 females had post-partum pelvic girdle pain, and 52 subjects were male. Significant improvements in pain, quality of life, and function were found for not only the post-partum group but all groups 12 months after surgery. Worth noting is one to three weeks after surgery, the subjects engaged in physical therapy, two times per week for six weeks.
Whang et al (2015) assessed the 6-month outcomes of SI joint fusion using triangular titanium implants versus non-surgical management in a prospective randomized controlled trial. Of the 148 subjects chosen based on similar diagnostic criteria as the study mentioned above, 102 underwent surgery, and 46 had non-surgical management. Non-surgical management involved appropriate pain medication administration, physical therapy, intra-articular SI joint steroid injections, and radiofrequency ablation of sacral nerve roots, all based on individual needs. The surgical group subjects in this study were also asked to have physical therapy two times per week for six weeks anywhere from one to three weeks post-op. The results in a six month follow up showed “clinical success” of >80% in the surgical group and <25% in the non-surgical management group.
The Journal of Neurosurgery: Spine presented an article in July 2015 by Zaidi et al with results of a systematic review of literature regarding the surgical and clinical effectiveness of SI joint fusion. The studies included open as well as minimally invasive surgery, and the causes of surgery included SI joint degeneration and arthritis, SIJ dysfunction, postpartum instability, posttraumatic, idiopathic, pathological fractures, and HLA-B27+/rheumatoid arthritis. A mean rate of satisfaction with open surgery was 54%; whereas, the mean was 84% with minimally invasive surgery. Ultimately, the authors concluded, “serious consideration of the cause of pain” is necessary before embarking on SI joint fusion as the evidence for the surgery’s efficacy is lacking.
So, who is responsible for making the definite diagnosis for SI joint dysfunction? As many patients get minimal time in doctor offices, we have a professional responsibility to competently perform a thorough evaluation for our patients. When the diagnosis is “SI joint dysfunction,” rule out the lumbar spine and hip; and, of course, when “low back pain” or “hip pain” fills the diagnosis line, rule out/in the SI joint. If you are confused about how, it is time to consider taking the Sacroiliac Joint Evaluation and Treatment course!
References:
Capobianco, R., Cher, D., & for the SIFI Study Group. (2015). Safety and effectiveness of minimally invasive sacroiliac joint fusion in women with persistent post-partum posterior pelvic girdle pain: 12-month outcomes from a prospective, multi-center trial. SpringerPlus, 4, 570. http://doi.org/10.1186/s40064-015-1359-y
Zaidi, Hasan A., Montoure, Andrew J., and Dickman, Curits A. (2015). Surgical and clinical efficacy of sacroiliac joint fusion: a systematic review of the literature. Journal of Neurosurgery: Spine. (23)1:59-66. DOI: 10.3171/2014.10.SPINE14516
Whang, P., Cher, D., Polly, D., Frank, C., Lockstadt, H., Glaser, J., … Sembrano, J. (2015). Sacroiliac Joint Fusion Using Triangular Titanium Implants vs. Non-Surgical Management: Six-Month Outcomes from a Prospective Randomized Controlled Trial. International Journal of Spine Surgery, 9, 6. http://doi.org/10.14444/2006
The following post comes to us from Herman & Wallace faculty member Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC. Allison authored "Use of transabdominal ultrasound imaging in retraining the pelvic-floor muscles of a woman postpartum" and is a leading expert in the use of ultrasound imaging for pelvic rehab. She is the author and instructor of the Rehabilitative Ultrasound Imaging: Women’s Health and Orthopedic Topics offered with Herman & Wallace.
In the pelvic floor series we learn how to perform examinations for cystoceles and rectoceles. It can be more difficult for therapists to examine and quantify the degree of uterine descent. In the last few years translabial ultrasound imaging has also been used to identify what is happening in the anterior compartment upon Valsalva and pelvic floor contraction, including the uterus. This is helpful when trying to determine the degree of uterine prolapse. Degree of pelvic organ descent visible on by ultrasound has been shown to have a near-linear relationship with measures on the POPQ.
 Clinically we see that some patients with severe prolapses have few symptoms, while other patients with smaller prolapses will have more severe complaints of symptoms. This can be puzzling to the clinician who is trying to treat prolapse patients. Shek and Dietz performed a study to set cutoff measures of uterine descent that will predict symptoms of prolapse. Translabial ultrasound imaging was performed on 538 women with 263 women reporting prolapse symptoms. Seventy-five percent of the women presented with grade two or greater prolapse on the POPQ, with most of being cystoceles or rectoceles. The women with more complaints of symptoms of prolapse were more likely to have uterine prolapse. There was a strong association between degree of uterine descent and symptoms of prolapse. They determined that an optimal cutoff to predict symptoms of prolapse due to uterine descent is a cervix descending to 15 mm above the pubic symphysis.
Clinically we see that some patients with severe prolapses have few symptoms, while other patients with smaller prolapses will have more severe complaints of symptoms. This can be puzzling to the clinician who is trying to treat prolapse patients. Shek and Dietz performed a study to set cutoff measures of uterine descent that will predict symptoms of prolapse. Translabial ultrasound imaging was performed on 538 women with 263 women reporting prolapse symptoms. Seventy-five percent of the women presented with grade two or greater prolapse on the POPQ, with most of being cystoceles or rectoceles. The women with more complaints of symptoms of prolapse were more likely to have uterine prolapse. There was a strong association between degree of uterine descent and symptoms of prolapse. They determined that an optimal cutoff to predict symptoms of prolapse due to uterine descent is a cervix descending to 15 mm above the pubic symphysis.
This study intrigues me and makes me wonder how much we are focusing on cystoceles and rectoceles and not looking at uterine prolapses. Using translabial ultrasound imaging is a nice tool to allow the clinician to see what is going on with all of the pelvic organs. With one Valsalva maneuver you are able to assess a lot of information including support of the pelvic organs. It also gives the clinician another way to quantify the degree of prolapse. Ultrasound imaging is a wonderful tool that clinicians can use for assessment as well as a biofeedback tool. If you are interested in learning how to perform this type of assessment, I will be teaching Rehabilitative Ultrasound Imaging: Women’s Health and Orthopedic Topics May 1-3 in Dayton, OH.
Shek KL, Dietz HP. What is abnormal uterine descent on translabial ultrasound? Int. Urogynecol J. 2015; 26(12)1783-7.
Food, at its basic level, provides us with nutrition and sustenance to perform our daily activities. Populations in tune with nature’s cycles of food tend to eat what is available locally based on climate and growth seasons. When societies move beyond simply eating food for energy, but also for flavor, pleasure, and even status, the face of nutrition changes. Whereas some diseases come from a lack of nutrition, many diseases we are faced with in the United States also come from an overabundance of food, with too many calories or too much sugar making up common causes of lack of health. The knowledge within the field of disordered eating is vast, and patients struggling with disordered eating may be fortunate enough to work with a specialist to help recover healthier habits. Even without a diagnosis of disordered eating, many us can identify with unhealthy eating habits, often guided by stress, fatigue, or emotions.
 Prior research has studied how we access willpower under different conditions of cognitive stress. In part of this research, participants were given a number to recall (either 2 digits or 7 digits) and then while walking to another location were offered a snack of either fruit salad or chocolate cake. The authors found that the participants who had to recall a 7 digit number more often chose the chocolate cake, leading the researchers to theorize about the role of higher-level processing and making choices. (Shiv et al., 1999) While we may be aware of a tendency to overeat (or make poorer food choices) during times of stress, fatigue, or emotional distress, changing the habits can be very challenging.
Prior research has studied how we access willpower under different conditions of cognitive stress. In part of this research, participants were given a number to recall (either 2 digits or 7 digits) and then while walking to another location were offered a snack of either fruit salad or chocolate cake. The authors found that the participants who had to recall a 7 digit number more often chose the chocolate cake, leading the researchers to theorize about the role of higher-level processing and making choices. (Shiv et al., 1999) While we may be aware of a tendency to overeat (or make poorer food choices) during times of stress, fatigue, or emotional distress, changing the habits can be very challenging.
Resources that discuss improving our eating choices in the face of “emotional eating” offers many alternatives, or ways to soothe ourselves without eating. In her books about this topic, clinical psychologist Susan Albers offers advice that may be helpful for our own habit building and for offering basic advice for our patients who struggle with the issue. (While offering advice to patients about healthy eating and habits is within our scope of practice, if a patient has need for a referral to a counselor, psychologist, or nutritionist, we can coordinate such a referral with the patient’s primary care provider.) In her book titled “50 More Ways to Soothe Yourself Without Food: Mindfulness Strategies to Cope with Stress and End Emotional Eating”, Dr. Albers offers many strategies for altering our habits. Some of these ideas include using acupressure points, breathing, rituals, self-massage, yoga, writing, dancing, art, tea, or sex to defer ourselves from poor eating habits. While eating can be enjoyable and pleasurable, when our patients are struggling with over-eating or eating foods that don’t support nutritional or healing goals, having a discussion about these issues may be useful.
If you are interested in learning more about nutrition, consider joining your pelvic rehab colleagues at one of the two Nutrition Perspectives for the Pelvic Rehab Therapist courses this year! Your first chance to attend will be in Kansas City on March 5-6, and later on in Lodi, CA June 25-26.
Albers, S. (2015). 50 More Ways to Soothe Yourself Without Food: Mindfulness Strategies to Cope with Stress and End Emotional Eating. New Harbinger Publications.
Shiv, B., & Fedorikhin, A. (1999). Heart and mind in conflict: The interplay of affect and cognition in consumer decision making. Journal of consumer Research, 26(3), 278-292.
Occasionally, as pelvic rehab providers, we will encounter the question from our patients, “Do vaginal weights help with urinary incontinence and pelvic floor performance?” The premise behind the use of vaginal cones or balls is that holding them actively in your vagina with your pelvic floor muscles helps to increase the performance (strength and endurance) of the pelvic floor muscles, assisting in reduction of urinary incontinence.

Of the searched studies, all were randomized or quasi-randomized controlled trials. The primary outcomes of the searched studies were pelvic floor muscle performance (strength or endurance) and/or urinary incontinence, both assessed with a valid or reliable method. 37 potentially useful articles were reviewed out of 1324 based on the search criteria, but only one article met all of the inclusion criteria and was included in this review with 192 relevant participants (Wilson and Herbison).
In the included study, the group that used vaginal cones (compared to control group) showed a statistically significant lower rate of urinary incontinence. However, when compared to the pelvic exercises group, the continence rates were similar at 12 months post-partum between the cone group and the exercising group. At 24-44 months post-partum, continence rates amongst all groups were similar, but follow-up rates were very low.
As pelvic rehabilitation providers, it is our job to promote pelvic health and assist our post-partum patients with their pelvic impairments, providing them with options to meet their goals. This review does not make a scientific statement of a preferred mode of pelvic exercise, however, it gives us one more option to consider when teaching patients about how to improve pelvic muscle performance to increase urinary continence following child birth. Pelvic exercise enhances pelvic performance, so if your patient would prefer to use vaginal cones or balls to do their pelvic exercise versus completing pelvic exercises without them, do what works best for the patient. One can argue that any pelvic exercise is better than none in improving performance. The use of vaginal cones or balls may be helpful for urinary continence in post-partum women, and provides us with one tool more when promoting pelvic health in our patients.
Oblasser, C., Christie, J., & McCourt, C. (2015). Vaginal cones or balls to improve pelvic floor muscle performance and urinary continence in women post-partum: A quantitative systematic review. Midwifery, 31(11), 1017-1025.
Wilson, P. D., & Herbison, G. P. (1998). A randomized controlled trial of pelvic floor muscle exercises to treat postnatal urinary incontinence. International Urogynecology Journal, 9(5), 257-264.
While working with a 71 year old lady one day, I asked her about her sleep habits, thinking she would describe her neck position, since that it was I was treating. She quickly commented she gets up one to two times every night to use the bathroom. Without any hesitation, she then declared her sister and her friends all do the same thing. No one she knows who is close to her age can sleep through the night without having to pee. Realizing this was more of an issue for my patient than her neck at night, I proceeded to look into the research behind these nighttime escapades of the elderly.
In the Journal of Clinical Sleep Medicine in 2013, Zeitzer et al. performed research regarding insomnia and nocturia in older adults. The introduction explains how 40-70% of older adults experience insomnia, and the greatest cause for sleep disturbance is the need to urinate in the middle of the night (nocturia). In epidemiological studies, between two-thirds and three-quarters older adults report disrupted sleep due to nocturia. The study performed by these authors involved men (average age of 64.3) and women (average age of 62.5) recording their sleep and toileting habits over the course of 2 weeks. The results showed over half the reported awakenings at night were secondary to nocturia. They had worse restfulness and efficiency of sleep associated with the log-reported need to get up to use the bathroom.
 In a 2014 study by Tyagi, et al., the effect of nocturia on the behavioral treatment for insomnia in older adults was explored. The authors noted how nocturia being the primary reason for waking up at night increased proportionately with age with results ranging from 39.9% in people 18-44 years of age to 77.1% in the 65 years old or above population. The 79 participants in this study underwent brief behavioral treatment for their chronic insomnia or only received information. People with and without nocturia both demonstrated significant improvements in quality of sleep after receiving brief behavioral treatment versus the control group; however, the effect size was larger in the participants without nocturia. The authors concluded nocturia needs to be addressed first in order to experience the full benefit of behavior treatment for insomnia.
In a 2014 study by Tyagi, et al., the effect of nocturia on the behavioral treatment for insomnia in older adults was explored. The authors noted how nocturia being the primary reason for waking up at night increased proportionately with age with results ranging from 39.9% in people 18-44 years of age to 77.1% in the 65 years old or above population. The 79 participants in this study underwent brief behavioral treatment for their chronic insomnia or only received information. People with and without nocturia both demonstrated significant improvements in quality of sleep after receiving brief behavioral treatment versus the control group; however, the effect size was larger in the participants without nocturia. The authors concluded nocturia needs to be addressed first in order to experience the full benefit of behavior treatment for insomnia.
On a neurological level, a study from November 2015 by Smith, Kuchel, and Griffiths reported there could be a neural basis for voiding dysfunction in older adults. They found 3 separate neural circuits control voiding, and damage to the pathways feeding these circuits increases with age and can increase urge incontinence. Older adults experiencing neurological deficits may have difficulty discerning what to do when there is urgency and are susceptible to becoming incontinent. The authors recommend treatment of not just the bladder in older people but also therapies to address the structural and functional abnormalities of the neural circuits to provide the greatest results.
So, the next time I saw my patient, I explained to her she is definitely not alone in her nightly rendezvous to the bathroom when it comes to her age group. She has accepted this as “just how things are.” I would like to think there is something more we can do for the elderly population to keep them out of the nocturia “night club.” Taking the Geriatric Pelvic Floor Rehabilitation course by Heather S. Rader, PT, DPT, BCB-PMD, seems like an essential step in the right direction.
Tyagi, S., Resnick, N. M., Perera, S., Monk, T. H., Hall, M. H., & Buysse, D. J. (2014). Behavioral Treatment of Chronic Insomnia in Older Adults: Does Nocturia Matter? Sleep, 37(4), 681–687.
Zeitzer, J. M., Bliwise, D. L., Hernandez, B., Friedman, L., & Yesavage, J. A. (2013). Nocturia Compounds Nocturnal Wakefulness in Older Individuals with Insomnia. Journal of Clinical Sleep Medicine : JCSM : Official Publication of the American Academy of Sleep Medicine, 9(3), 259–262.
Smith, Phillip P., Kuchel, George A., Griffiths, Derek. (2015). Functional Brain Imaging and the Neural Basis for Voiding Dysfunction in Older Adults. Clinics in Geriatric Medicine. 31(4), 549–565.
Postpartum lower extremity nerve injuries is an important topic that we have previously discussed on the blog. A review article(O'Neal 2015) published in the International Anesthesia Research Society journal discusses maternal neurological complications following childbirth. This article, designed to help anesthesiologists identify the symptoms of a neuropathy, discusses diagnosis, management, and treatment. With the incidence of obstetric neuropathy in the postpartum period estimated at 1%, most of the nerve dysfunction is related to compression injuries. Symptoms may include, but are not limited to, lower extremity pain, weakness, numbness, or bowel and bladder dysfunction. Neuraxial anesthesia can also occur, with issues such as epidural hematoma or an epidural abscess. Risk factors are described in the article as having a prolonged second stage of labor, instrumented delivery, being of short stature and nulliparity (delivering for the first time.)
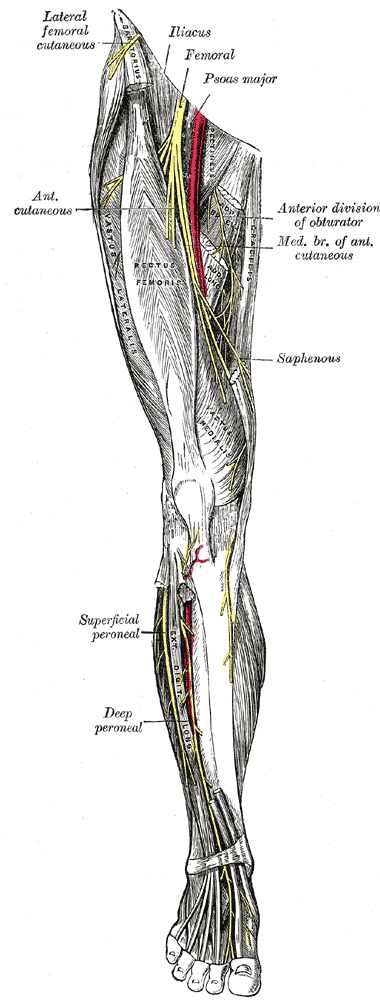 Clinical pearls listed in the article include the following information that may be helpful in understanding a patient’s condition:
Clinical pearls listed in the article include the following information that may be helpful in understanding a patient’s condition:
- intramedullary spinal cord syndromes (inside the spinal cord) are usually painless, whereas the peripheral nerve syndromes (involving the spinal nerve roots, plexus, and single nerves) usually cause pain
- bowel and bladder dysfunction often occurs early in the case of conus medullaris and late in the event of cauda equina syndrome
- cauda equina syndrome often causes polyradicular pain, leg weakness, numbness, and deep tendon reflex changes and involves multiple roots
- conus medullaris syndrome is not painful and causes saddle anesthesia and lack of significant sensory and motor symptoms in the lower extremities
In relation to prevention of neuropathies, the authors suggest that women who have diabetes or who have a preexisting neuropathy should be given extra attention. This may include protective padding during labor and delivery as well as frequent repositioning. Pelvic rehabilitation providers are a key player in the arena of birthing. Caring for women and educating them about peripartum issues is critical to helping women both prevent and heal from challenges encountered in relation to pregnancy and childbirth. If you would like to learn more about the topic of peripartum nerve dysfunctions, as well as many other special topics, please join us for the continuing education course Care of the Postpartum Patient. Your next opportunity to take this course will be in Seattle next March!
O’Neal, M. A., Chang, L. Y., & Salajegheh, M. K. (2015). Postpartum Spinal Cord, Root, Plexus and Peripheral Nerve Injuries Involving the Lower Extremities: A Practical Approach. Anesthesia & Analgesia, 120(1), 141-148.
The day my son was born, my daughter had not defecated for 5 days, and her pain was getting pretty intense. My husband and his mom took her to Seattle Children’s Hospital for help, and they suggested using Miralax and sent them away. When they got back to my hospital room, my daughter was straining so hard it looked like she was about to give birth! Being physical therapists, my husband and I massaged her little muscles and told her to take deep breaths, and eventually she did the deed, yet not without a heart-breaking struggle. Little did I know then there is actually research to back up our emergency, instinctual technique.
 Zivkovic et al (2012) performed a study regarding the use of diaphragmatic breathing exercises and retraining of the pelvic floor in children with dysfunctional voiding. They defined dysfunctional voiding as urinary incontinence, straining, weakened stream, feeling the bladder has not emptied, and increased EMG activity during the discharge of urine. Although this study focuses primarily on urinary issues, it also includes constipation in the treatment and outcomes. Forty-three patients between the ages of 5 and 13 with no neurological disorders were included in the study. The subjects underwent standard urotherapy (education on normal voiding habits, appropriate fluid intake, keeping a voiding chart, and posture while voiding) in addition to pelvic floor muscle retraining and diaphragmatic breathing exercises. The results showed 100% of patients were cured of their constipation, 83% were cured of urinary incontinence, and 66% were cured of nocturnal enuresis.
Zivkovic et al (2012) performed a study regarding the use of diaphragmatic breathing exercises and retraining of the pelvic floor in children with dysfunctional voiding. They defined dysfunctional voiding as urinary incontinence, straining, weakened stream, feeling the bladder has not emptied, and increased EMG activity during the discharge of urine. Although this study focuses primarily on urinary issues, it also includes constipation in the treatment and outcomes. Forty-three patients between the ages of 5 and 13 with no neurological disorders were included in the study. The subjects underwent standard urotherapy (education on normal voiding habits, appropriate fluid intake, keeping a voiding chart, and posture while voiding) in addition to pelvic floor muscle retraining and diaphragmatic breathing exercises. The results showed 100% of patients were cured of their constipation, 83% were cured of urinary incontinence, and 66% were cured of nocturnal enuresis.
More recently, Farahmand et al (2015) researched the effect of pelvic floor muscle exercise for functional constipation in the pediatric population. Stool withholding and delayed colonic transit are most often the causes for children having difficulty with bowel movements. Behavioral modifications combined with laxatives still left 30% of children symptomatic. Forty children between the ages of 4 and 18 performed pelvic floor muscle exercise sessions at home, two times per day for 8 weeks. The children walked for 5 minutes in a semi-sitting (squatting) position while being supervised by parents. The patients increased the exercise duration 5 minutes per week for the first two weeks and stayed the same over the next six weeks. The results showed 90% of patients reported overall improvement of symptoms. Defecation frequency, fecal consistency and decrease in fecal diameter were all found to be significantly improved. Although not statistically significant, the number of patients with stool withholding, fecal impaction, fecal incontinence, and painful defecation decreased as well.
Parents may not be as aware of their children’s voiding habits once they are cleared from diaper duty after successful potty training occurs. To help prevent issues, keep the basics covered, such as making sure children are exercising regularly or being active, drinking plenty of fluids, and eating a diet that includes plenty of fiber. My daughter was only 26 months old when her constipation became a problem, so the stool softener was ultimately the way to go at that time, and everything worked out naturally over the next year. If she were still experiencing functional constipation, I would be delighted to know teaching her pelvic floor exercises (relaxation being the key aspect) and diaphragmatic breathing could be effective for keeping my crazy little girl regular in at least that area of her life!
Zivkovic V, Lazovic M, Vlajkovic M, Slavkovic A, Dimitrijevic L, Stankovic I, Vacic N. (2012). Diaphragmatic breathing exercises and pelvic floor retraining in children with dysfunctional voiding. European J ournal of Physical Rehabilitation Medicine. 48(3):413-21. Epub 2012 Jun 5.
Farahmand, F., Abedi, A., Esmaeili-dooki, M. R., Jalilian, R., & Tabari, S. M. (2015). Pelvic Floor Muscle Exercise for Paediatric Functional Constipation.Journal of Clinical and Diagnostic Research : JCDR, 9(6), SC16–SC17. http://doi.org/10.7860/JCDR/2015/12726.6036