Trauma. The word holds so many meanings. Say the word and depending on your perspective - it could mean Trauma (like trauma center which is physical injury focused) or trauma (like unwanted experience causing adverse socioemotional consequences). In medical environments, the former would be qualified as ‘Big T’ Trauma, and the latter would be ‘little t’ trauma. Once you are immersed in the ‘little t’ trauma field, the Big and little traumas change meanings. The Big T Trauma would describe a significant event, whereas the little t trauma would include multiple, smaller microaggressions accumulating into adverse effects.
I have worked in trauma since 1996. And the changes have been vast. Thankfully, long gone are the days that I am educating physicians in the ER on how to complete a rape kit and how to perform care that is patient-focused and empowering. I would like to think that advocates are no longer having to explain to medical providers that RU22 is not an ‘abortion pill’ but a medicine that is required to be offered BY LAW in Illinois (SASETA) to reduce the risk of implantation after a rape. I started working in ERs advocating for the medical and legal rights of sexual assault survivors BEFORE Law-and-Order SVU brought these patients into mainstream culture in 1999. Thank you, Olivia and Elliot for bringing this awareness into our living rooms.
When I was a mental health counselor in the 90s and 2000s, it was quite remarkable that trauma was not included in mental health services. PTSD definitions were changing frequently within the DSM (Diagnostic Statistical Manual) during this time. Definitions and inclusion of trauma within mental health continue to change frequently to this day. In the 90s, I was working with youth in lower socioeconomic populations and their trauma was both palpable and unseen. Also, during this time, education and awareness of developmentally appropriate sexual health were not a thing! I remember my supervisor calling me and asking me what to do with a teenage female who was masturbating with a brush. And I was like OK - which side of the brush… is she masturbating for pleasure which is normal/appropriate or is she hurting herself and we need to screen her for sexual abuse? I screened her for abuse (my supervisor was not comfortable- she ended up disclosing her own abuse) and the teenager did not disclose abuse or self-harming behaviors, so it was normal sexual behavior. I could go on about cultural and gender taboos, but that is literally power for the course.
When I made the change from mental health to physical therapy in the mid-late 2000s it soon became apparent that trauma was not considered within rehabilitation. In 2011, I created the first in-service on trauma - focusing on education, awareness, and teaching Polyvagal theory. Stephen Porges introduced Polyvagal much earlier in 1994 and I am looking forward to the day he receives the Nobel Prize for his work, as he should. I am ecstatic that Polyvagal is no longer an obscure construct. I see many friends and fellow clinicians normalizing the terms neuroception and interoception, and I am elated. This is quite different from when ten ten-plus years ago, the response to my course was a not-so-friendly ‘Stay in your lane, PT’ (and this is not addressing the fact that our fellow OT and SLP comrades are doing this challenging work). I am so glad that is not the case anymore. Trauma-informed care (TIC) is becoming the norm, not the exception. And I am so happy to see what other rehabilitation specialists are doing within the field! There is so much space for us all.
Here is an outline of what we expand upon within the course Trauma Awareness for the Pelvic Therapist:
Trauma-informed care (TIC) is a universal approach within healthcare that recognizes and responds to the impact of traumatic experiences on individuals. It aims to create a supportive environment that promotes healing and recovery while minimizing the risk of re-traumatization. The core principles of trauma-informed care include understanding the prevalence and effects of trauma, recognizing the signs and symptoms of trauma in patients and staff, and integrating knowledge about trauma into practices, policies, and procedures. In order to understand the effects of trauma, an understanding of neurobiology of the brain and function of the autonomic nervous system are foundational.
Key Principles of Trauma-Informed Care:
Safety:
Ensuring physical and emotional safety for the CLINICIAN, clients, and staff. This involves creating an environment where individuals feel secure and respected.
Trustworthiness and Transparency:
Building trust through clear, consistent, and transparent practices. Ensuring that decision-making processes are transparent, and that information is shared openly.
Peer Support:
Encouraging and incorporating peer support and mutual self-help as essential components of trauma-informed care. Peer support helps to build trust, enhance collaboration, and promote recovery.
Collaboration and Mutuality:
Emphasizing partnership and the leveling of power differences between staff and clients. Everyone involved in the care process collaborates and shares in the decision-making.
Empowerment, Voice, and Choice:
Prioritizing the empowerment of individuals and recognizing their strengths. Offering choices and supporting individuals in their decisions helps to foster autonomy and resilience.
Cultural, Historical, and Gender Issues:
Being responsive to cultural, historical, and gender contexts. This involves recognizing and addressing the impact of systemic oppression and discrimination and promoting cultural competence among staff.
Implementation Strategies
Training and Education:
Providing ongoing training for EVERYONE on the principles of trauma-informed care and the impact of trauma. This includes recognizing trauma responses and learning how to create a supportive environment.
Policy and Procedure Review:
Introducing TIC and revising organizational policies and procedures to ensure they reflect trauma-informed principles. This includes practices related to intake, assessment, treatment planning, and discharge.
Environment Modification:
Creating physical spaces that promote a sense of safety and calm. This can involve changes to the layout, lighting, noise levels, and decor.
Client/Patient Involvement:
Involving clients in the planning and evaluation of services to ensure their perspectives and needs are considered.
Support Systems:
Providing support for EVERYONE to prevent burnout and secondary traumatic stress. This can include supervision, debriefing sessions, and access to mental health resources.
Trauma is personal and individualized. There is no one size fits all or one technique can be used for all.
Benefits of Trauma-Informed Care:
Improved Outcomes:
Trauma-informed care can lead to better engagement, adherence to treatment, and overall outcomes for clients/patients.
Reduced Re-traumatization:
By creating a supportive and understanding environment, the risk of re-traumatizing individuals (read: ALL of us) is minimized.
Enhanced Trust:
Building trust between clients/patients and providers fosters better communication and a stronger therapeutic relationship.
Empowerment and Recovery:
Empowering individuals to take an active role in their care promotes recovery and resilience.
Remember, trauma-informed care is a comprehensive approach that involves understanding, recognizing, and responding to the effects of trauma. By integrating trauma-informed principles into practice as UNIVERSAL PRECAUTIONS, we can create safer, more supportive environments that promote healing and recovery for ourselves and all individuals.
It has been an honor to bring this course, Trauma Awareness for the Pelvic Therapist, into the rehabilitation space. In the last 10 years, and especially since COVID-19, it is beautiful to see how TIC has become mainstream. One word of caution: We need to watch out for end-of-spectrum gas lighting. We all have seen patients whose symptoms and experiences have been minimized when their trauma has not been taken into consideration. This can also happen at the other end of the spectrum. I had a patient who sought out gynecological treatment from a ‘trauma-focused gynecologist.’ This patient we all know - chronic pelvic pain with a history of endo, PCOS, IBS-M, and IC. When she went to this clinician, she was told that her pain was caused by trauma, whether she remembered the trauma or not. The patient is a counselor and has been doing much work with her mental health team. She was open to ‘unknown trauma’ but we both thought she should seek another provider. Two weeks later, she had surgery for appendicitis.
TIC allows us to refocus on our work within rehabilitation and is open and supportive towards all people. This work is AMAZING. This work is HARD. This work is quite frankly one of the reasons we were placed on this earth. To be present for another person’s pain, whatever type of pain that is - is one of the most special care one can give to another.
Please be so proud of all the work you have done. Know that you are enough. And that you can be present for others. I hope you find even more support and knowledge with any trauma course that you choose to take, I just hope to meet you in mine on September 21-22!
AUTHOR BIO:
Lauren Mansell DPT, CLT, PRPC
 Lauren received her Doctor of Physical Therapy degree from Governors State University and a Bachelor's Degree in Psychology and Sociology from Northwestern University. Before becoming a physical therapist, Lauren counseled suicidal and homicidal SES at-risk youth who had survived sexual violence. Lauren was certified as a medical and legal advocate for sexual assault survivors in 1999 and has advocated for over 130 sexual assault survivors of all ages in the ED. Lauren's physical therapy specialty certifications include Certified Lymphedema Therapist (CLT), Pelvic Rehabilitation Professional Certificate (PRPC), and Certified Yoga Therapist (CYT). She is a board member of the Chicagoland Pelvic Floor Research Consortium, American Physical Therapy Association Section of Women's Health and Section of Oncology.
Lauren received her Doctor of Physical Therapy degree from Governors State University and a Bachelor's Degree in Psychology and Sociology from Northwestern University. Before becoming a physical therapist, Lauren counseled suicidal and homicidal SES at-risk youth who had survived sexual violence. Lauren was certified as a medical and legal advocate for sexual assault survivors in 1999 and has advocated for over 130 sexual assault survivors of all ages in the ED. Lauren's physical therapy specialty certifications include Certified Lymphedema Therapist (CLT), Pelvic Rehabilitation Professional Certificate (PRPC), and Certified Yoga Therapist (CYT). She is a board member of the Chicagoland Pelvic Floor Research Consortium, American Physical Therapy Association Section of Women's Health and Section of Oncology.
As adjunct faculty, Lauren teaches Special Topics: Pelvic Rehabilitation Physical Therapy at Governors State University. Lauren works at the University of Chicago providing pelvic rehabilitation, lymphedema, and oncological physical therapy within Therapy Services and the Center of Supportive Oncology. She treats pelvic pain, urinary incontinence, bowel dysfunction, sexual dysfunction, lymphedema, lymph node transfer/bypass, stem cell transplant, and bowel/bladder/sexual/functional concerns of patients undergoing HIPEC (hyperthermal intraperitoneal chemotherapy). Lauren is a 2017 Fellow of the Chicago Trauma Collective. As a trauma-sensitive practitioner, her goal is to empower patients to create meaningful, healthful lifestyle changes to improve their physiology and wellness

Caring for patients who have experienced trauma requires a skillset beyond basic knowledge of pelvic health assessment and intervention. With one-third of women experiencing intimate partner violence, and estimates of rape reports to formal agencies (e.g., police, medical professionals) ranging from only 5–33% (Fisher, Cullen, & Turner, 2000; Kilpatrick et al., 2007; Krebs et al., 2007; Rennison, 2002), we can safely say that the gender-based violence women uniquely experience is likely grossly under-reported.
Additionally, the World Health Organization reports that violence and sexual violence against women is a major global public health problem. Estimates published by WHO indicate that globally about 1 in 3 (30%) of women ages 15-49 worldwide have been subjected to either physical and/or sexual intimate partner violence or non-partner sexual violence in their lifetime.
In terms of violence, the vast majority is, sadly, intimate partner violence; that is, violence committed by your own partner. Further, the overall risk of any gender reporting intimate partner violence is 1 in 7 for people who identify as men, and 1 in 5 for people who identify as female, according to the last reported statistics from the CDC.
For trauma risk in general, the chance of any gender experiencing trauma, including ACEs, or Adverse Childhood Experiences, is as high as over 70%. The first comprehensive study on PTSD (post-traumatic stress disorder) and trauma in the US was not conducted until 1990, which reported that 60.7% of men and 51.2% of women reported at least one exposure to trauma. From there, the estimated population lifetime prevalence of 5.7% for men and 12.8% for women (Kilpatric et al 2013).
The statistics on violence against the LGBTQIA community are even more alarming. A survey found that transgender people (16+) are victimized over four times more often than cisgender people and that transgender women and men had higher rates of violent victimization than cisgender women and men. Overall, about 50% of the violent victimizations were not reported to police. A separate 2022 survey showed that LGBT people experienced 6.6 violent hate crime victimizations per 1,000 persons compared with non-LGBT people's 0.6 per 1,000 persons (odds ratio = 8.30, 95% confidence interval = 1.94, 14.65).
 If you are working with this population, there is a long list of adverse impacts known to affect all genders who have experienced trauma, especially if they go on to develop PTSD or complex PTSD (cPTSD), and even more so if the person experienced an ACE. A traumatic event is defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM5) as a direct or indirect witness (indirect means learning about the trauma of a loved one) to actual or threatened death, serious injury, or sexual violence, either of which can induce PTSD. Four symptom clusters define PTSD in the DSM5:
If you are working with this population, there is a long list of adverse impacts known to affect all genders who have experienced trauma, especially if they go on to develop PTSD or complex PTSD (cPTSD), and even more so if the person experienced an ACE. A traumatic event is defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM5) as a direct or indirect witness (indirect means learning about the trauma of a loved one) to actual or threatened death, serious injury, or sexual violence, either of which can induce PTSD. Four symptom clusters define PTSD in the DSM5:
- Intrusive symptoms - recurrent and unwanted memories, nightmares, flashbacks, and intense distress or physiological reactivity after exposure to traumatic reminders.
- Avoidance symptoms - avoidance of trauma-related thoughts, feelings, or reminders.
- Persistent negative beliefs - negative emotions related to the trauma (such as guilt, shame, anger, horror), loss of interest in significant activities, feelings of alienation from others, and an inability to experience positive or loving emotions.
- Alterations in arousal and reactivity - irritability or aggression, self-destructive or reckless behavior, hypervigilance, exaggerated startle response, and problems with concentration and sleep.
Some of the signs of cPTSD can include:
- Behavioral difficulties (e.g. impulsivity, aggressiveness, sexual acting out, alcohol/drug misuse, and self-destructive behavior)
- Emotional difficulties (e.g. affect lability, rage, depression, and panic)
- Cognitive difficulties (e.g. dissociation and pathological changes in personal identity)
- interpersonal difficulties (e.g. chaotic personal relationships)
- Somatization (resulting in many visits to medical practitioners)
Some of the musculoskeletal and lifestyle manifestations of experiencing trauma and even just stress include:
- Musculoskeletal tension or “trauma posturing” (aka constant guarding)
- Upregulated sympathetic nervous system response (aka fight or flight)
- Increased stress hormones - adrenaline, noradrenaline, cortisol
- Low back pain
- Headaches
- Sleep disturbances due to clenching, grinding, or nightmares
- Indigestion, ulcers, IBS, bloating, impaired or slowed gastrointestinal motility
- Poor circulation due to poor breathing patterns
- Increased heart rate, blood pressure
- Decreased fertility in women and men
- Worsening or influence on PMS and perimenopause/menopause
- Sexual dysfunction including decreased sexual desire, and/or erectile dysfunction)
- Increased risk of hypertension and heart attack
- Chronic activation of the HPA Axis
- Upregulated glucocorticoids, resulting in decreased immune function and increased systemic inflammation
- Increased risk for chronic fatigue syndrome, metabolic disorders including diabetes and obesity, and depression
- Increased risk for reflux and increased swallowing issues due to laryngeal tension
- Muscle tension dysphonia
- Chronic hoarseness, laryngitis, or psychogenic dysphonia
- Poor cognitive function and executive functioning
With regard to pelvic health, Yehuda et al posit that “because some symptoms of PTSD, such as nightmares, intrusive memories, and insomnia, are so distressing and result in such great restrictions in overall quality of life, sexual dysfunction is often not presented as a top priority by treatment-seeking patients.” The researchers also cite multiple studies which no longer support that sexual dysfunction only arises from sexual trauma. They write, “studies of nonsexual trauma including combat, accidents, and criminal victimization have now also established an association with sexual dysfunction in men and women including sexual desire, arousal, orgasm, activity, and satisfaction.” For example, Cosgrove et al found that male combat-exposed veterans (n = 90) rates of erectile dysfunction were 85% in veterans with PTSD compared with 22% in veterans without PTSD.
Trauma Can Literally Steal Your Voice
 Further, trauma, no matter what type, intimately impacts the voice. The condition of losing your voice after trauma is known as psychogenic dysphonia or aphonia. It is characterized by the loss of volitional control over phonation after psychological events such as anxiety, depression, conversion reaction, or personality disorders, cites Baker (2003). It can also develop after viruses, with COVID-19 bringing not just respiratory consequences but a unique multi-system impact with negative consequences for the pelvic floor, such as occurs after prolonged coughing, hospitalization, and/or intubation.
Further, trauma, no matter what type, intimately impacts the voice. The condition of losing your voice after trauma is known as psychogenic dysphonia or aphonia. It is characterized by the loss of volitional control over phonation after psychological events such as anxiety, depression, conversion reaction, or personality disorders, cites Baker (2003). It can also develop after viruses, with COVID-19 bringing not just respiratory consequences but a unique multi-system impact with negative consequences for the pelvic floor, such as occurs after prolonged coughing, hospitalization, and/or intubation.
Any emotionally or psychologically taxing event that occurs in proximity to loss of vocal control must be investigated, in order to understand the qualitative variables that may be present in the voice dysfunction. It doesn’t even take trauma to steal your voice, since stress is cited as a top driver for muscle tension dysphonia.
For example, I have had multiple clinical cases where women struggle with their voice decades after experiencing sexual assault in college or in an intimate relationship, but chose to “keep it a secret” and not report it. I’ve also seen patients with post-COVID or long COVID who report severe struggles with return to exercise or full activities of daily living due to concomitant respiratory and pelvic floor difficulties. Further, I have treated patients who presented after accidental damage to the recurrent laryngeal nerve during surgery and are struggling to recover both their voice and pelvic floor function. Finally, I have countless patients who have been medically gaslit and told their voice and pelvic floor pain are unrelated.
Regardless of the reason, we have an obligation as pelvic health clinicians to provide the best evidence-informed care possible. The Voice to Pelvic Floor (V2PF) method is one such way to provide trauma-informed and psych-informed pelvic healthcare. The V2PF approach is a systems-based way to evaluate the patient looking at the connection between three diaphragms:
- The orofacial/cervico-laryngeal diaphragm
- The respiratory diaphragm
- The pelvic diaphragm
The purpose of a V2PF approach is to provide a deeper understanding of polyvagal theory, anatomy and physiology, neuropsychology, trauma-informed principles, as well as sociocultural issues that impact our world, in order to allow us to function as primary care providers in pelvic health across the lifespan.
Want more information? Learn how to assess and plan interventions using a voice-to-pelvic floor trauma-informed approach at Dr. Garner’s course – The Voice and the Pelvic Floor scheduled on September 7th, 2024.
Sources
- Kilpatrick D.G., Resnick H.S., Milanak M.E., Miller M.W., Keyes K.M., Friedman M.J.National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress2013;26: 537- 547.
- Sexual Victimization of College Women | Office of Justice Programs [WWW Document], n.d. URL https://www.ojp.gov/ncjrs/virtual-library/abstracts/sexual-victimization-college-women (accessed 8.6.24).
- CDC, 2024. About Intimate Partner Violence [WWW Document]. Intimate Partner Violence Prevention. URL https://www.cdc.gov/intimate-partner-violence/about/index.html (accessed 8.6.24).
- Campus Sexual Assault (CSA) Study | Office of Justice Programs [WWW Document], n.d. URL https://www.ojp.gov/ncjrs/virtual-library/abstracts/campus-sexual-assault-csa-study (accessed 8.6.24).
- Rennison, C.M., 2002. Rape and Sexual Assault: Reporting to Police and Medical Attention, 1992-2000: (387542004-001). https://doi.org/10.1037/e387542004-001
- Kilpatrick, D.G., Ruggiero, K.J., Acierno, R., Saunders, B.E., Resnick, H.S., Best, C.L., 2003. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the National Survey of Adolescents. Journal of Consulting and Clinical Psychology 71, 692–700. https://doi.org/10.1037/0022-006X.71.4.692
- Flores, A.R., Meyer, I.H., Langton, L., Herman, J.L., 2021. Gender Identity Disparities in Criminal Victimization: National Crime Victimization Survey, 2017–2018. Am J Public Health 111, 726–729. https://doi.org/10.2105/AJPH.2020.306099
- First, M.B. (Ed.), 2022. Diagnostic and statistical manual of mental disorders: DSM-5-TR, Fifth edition, text revision. ed. American Psychiatric Association Publishing, Washington, DC.
- Flores, A.R., Stotzer, R.L., Meyer, I.H., Langton, L.L., 2022. Hate crimes against LGBT people: National Crime Victimization Survey, 2017-2019. PLoS One 17, e0279363. https://doi.org/10.1371/journal.pone.0279363
- Yehuda, R., Lehrner, A., Rosenbaum, T.Y., 2015. PTSD and Sexual Dysfunction in Men and Women. J Sex Med 12, 1107–1119. https://doi.org/10.1111/jsm.12856
- Cosgrove, D.J., Gordon, Z., Bernie, J.E., Hami, S., Montoya, D., Stein, M.B., Monga, M., 2002. Sexual dysfunction in combat veterans with post-traumatic stress disorder. Urology 60, 881–884. https://doi.org/10.1016/S0090-4295(02)01899-X
- Baker, J., 2003. Psychogenic voice disorders and traumatic stress experience: a discussion paper with two case reports. J Voice 17, 308–318. https://doi.org/10.1067/s0892-1997(03)00015-8
- VA.gov | Veterans Affairs [WWW Document], n.d. URL https://www.ptsd.va.gov/professional/treat/essentials/complex_ptsd.asp (accessed 8.6.24).
- Siracusa, C., Gray, A., 2020. Pelvic Floor Considerations in COVID-19. Journal of Women’s Health Physical Therapy 44, 144–151. https://doi.org/10.1097/JWH.0000000000000180
AUTHOR BIO:
Dr. Ginger Garner PT, DPT, ATC-Ret

Dr. Ginger Garner PT, DPT, ATC-Ret is a clinician, author, educator, and longtime advocate for improving access to physical therapy services, especially pelvic health. She is the founder and CEO of Living Well Institute, where she has been certifying therapists and doctors in Medical Therapeutic Yoga & Integrative Lifestyle Medicine since 2000. She also owns and practices at Garner Pelvic Health, in Greensboro NC, where she offers telehealth and in-person wellness and therapy services. Ginger is the author of multiple textbooks and book chapters, published in multiple languages. She has also presented at over 20 conferences worldwide across 6 continents across a range of topics impacting the pelvic girdle, health promotion, and integrative practices.
Ginger is an active member of APTA, serving as the Legislative Chair for APTA North Carolina, as a Congressional Key Contact for APTA Private Practice, and in the Academy of Pelvic Health. Ginger lives in Greensboro, NC with her partner, 3 sons, and their rescue pup, Scout Finch. Visit Ginger at the websites above and on Instagram and YouTube.

I will never forget when my sister, my bestie, told me she wanted to end her life. We were on the phone late one night, tears flowing. Depression was always a companion, but I had never heard her in such a state of despair. We made a plan that she would call the suicide hotline, then call her therapist and her doctor in the morning for urgent care. She made it through the night. Later, I went to her therapist with her so I could better understand and support my sister. She did her due diligence, adjusting medication and staying open and honest in therapy. Suicidal ideations would sometimes flare when there were triggers, but she was able to work through them, and now they are in the past.
Contrast that story with another. Ryan was a sweet woman who developed pudendal neuralgia after a routine hysterectomy. Right away, she told me she had a counselor who she loved who helped her navigate life with DID (Dissociative Identity Disorder) and that I’d probably be interacting with various personalities during our sessions. She helped me understand how to best support her during her care. We worked well together, and although she struggled with both the pain and the unfairness of what happened to her, she was well supported. Then her sweet dog passed away. It was so hard for her. She kept going through pain and heartache and found another pooch to adopt. And then the next visit, she didn’t show. And the next, and the next. And then I found out she was gone. Suicide. This hit me hard. Were there signs that I missed? Was there anything I could have done?
As pelvic rehab providers, we sometimes see people who have intense physical pain often combined with significant emotional wounds. In a study of 713 women seeking support for pelvic pain, 46.8 reported having sexual or physical abuse history, and 31.3 were positive for PTSD (1).
Chronic pelvic pain impacts all aspects of people’s lives: physical, financial, relational, emotional, and mental. People can also become dependent on narcotics or recreational drugs which may lead to intentional or accidental overdose, per Philip Hall, a gynecologist in Australia (2).
In a study of 13,500 women with endometriosis, half reported experiencing suicidal thoughts (3).
So what’s our role as health care providers?
It’s important to note that not everyone who is considering suicide will admit it, and not everyone who thinks about suicide will follow through with it. However, all threats of suicide should be taken seriously. Let people know you care, they are not alone, and help is available.
Ask questions: It may feel scary, but it won’t push someone into harmful action. The Columbus Protocol, listed below, uses three questions to identify suicide risk. If someone answers yes to any question, they have a significantly higher risk of suicide and need support(4).
- Have you wished you were dead or wished you could go to sleep and not wake up?
- Have you had any thoughts about killing yourself?
- Have you thought about how you might do this?
Be observant of warning signs:
- people may talk about taking their own life, wishing they could end things, wishing they were never born
- you may observe extreme mood swings
- the person may start putting their affairs in order
- there may have been a recent trauma or crisis
- you may notice withdrawal or sudden calmness
- the person may participate in risky or reckless behavior
If someone admits to planning for suicide, as health care providers, we MUST take supportive action. If your facility does not have a protocol, consider these steps:
- Call 911 and perhaps a friend or family member to meet the person at the hospital
- Stay with the person until help arrives
- Remove any objects that may be used for harm
- Listen with kindness and understanding
- Stay Connected: studies show that follow up after an event decreases the risk of suicide death(5)
It’s helpful also to note the following protective behaviors, as reported by psychiatry.org(6):
- Connection with health care providers
- Strong connections between family, friends, community
- Skillfulness around problem-solving and conflict resolution

Knowing what to look for, what questions to ask, and how to get someone the help they need empowers health care providers to provide the best support for patients struggling with suicidal ideation and contemplation.
There are local and national resources for us as well.
The National Suicide Prevention Lifeline: 1-800-273-(TALK) (1-800-273-8255). The Lifeline provides 24/7, free and confidential support for people in distress, prevention and crisis resources for you or your loved ones, and best practices for professionals in the United States(7).
References:
- Meltzer-Brody, S., Leserman, J., Zolnoun, D., Steege, J., Green, E., & Teich, A. (2007). Trauma and posttraumatic stress disorder in women with chronic pelvic pain. Obstetrics & Gynecology, 109 (4), 902-908.
- https://standrewshospital.com.au/about-us/news/news-listing/2016/09/05/chronic-pelvic-pain-linked-to-suicides-in-young-women
- https://www.bbc.com/news/health-49897873
- https://cssrs.columbia.edu/the-columbia-scale-c-ssrs/about-the-scale/
- Motto, J. A., & Bostrom, A. G. (2001). A randomized controlled trial of postcrisis suicide prevention. Psychiatric Services52(6), 828-833.
- https://www.psychiatry.org/patients-families/suicide-prevention
- https://suicidepreventionlifeline.org/
Holly Tanner Short Interview Series - Episode 3 featuring Lauren Mansell
Lauren Mansell shares, "We're never ready to do this work. We're never ready to be perfect." Her course, Trauma Awareness for the Pelvic Therapist, is for all practitioners, not just physical therapists. Anyone licensed who works with patients can benefit from this topic. However, it can be offputting to put ourselves into a vulnerable position by registering for a course on this topic. Lauren understands this and comes prepared to teach other practitioners about trauma-informed care in the gentlest way possible.
Lauren Mansell, DPT, CLT, PRPC, CYT curated and instructs this course. Lauren worked in counseling and advocacy for sexual assault survivors before becoming a physical therapist. She also brings her experience as a 2017 Fellow of the Chicago Trauma Collective to teach trauma-informed care to medical providers. Trauma-informed care is especially important as the field of pelvic rehabilitation becomes more inclusive.
Pelvic rehabilitation and pelvic therapists really do treat the whole patient. Patients can present with pain, long-term issues, and undisclosed trauma that can be compounded when it includes sex, bladder, or bowel issues. Trauma Awareness for the Pelvic Therapist addresses several topics under this umbrella and spends time on each of the following:
- Explaining and describing compassion fatigue, trauma-informed care as well as anatomy, neurobiology, physiology of trauma, and the polyvagal autonomic nervous system
- Identifying risk factors and Adverse Childhood Experiences (ACEs)
- Formulating techniques for reducing compassion fatigue, secondary trauma, and retraumatization
To learn more about trauma-informed care join H&W this weekend at Trauma Awareness for the Pelvic Therapist this September 25-26, 2021. The course will be offered again in 2022 if you are not available this weekend!
 Last week- on May 6 amid a pandemic- the Department of Education released changes to Title IX. Title IX is a 1972 Civil Rights Act that bans sexual discrimination within the educational system. Sadly, the new provisions within the 2,033 page document include the following changes:
Last week- on May 6 amid a pandemic- the Department of Education released changes to Title IX. Title IX is a 1972 Civil Rights Act that bans sexual discrimination within the educational system. Sadly, the new provisions within the 2,033 page document include the following changes:
- Narrows the definition of sexual harassment
- Reduces options to survivors of sexual assault, dating violence and stalking
- Reduces liability of colleges and universities
- Reduces mandated reporting of sexual violence
- Deregulates federal guidelines to protect sexual violence survivors
- Changes the ‘standard of proof’ from ‘preponderance’ to ‘clear and convincing’
- Bolsters protections for perpetrators
- Allows for live hearings and cross examinations of the assault survivor
- Only investigates if assault reported to ‘certain people’
23% of undergraduates and 11% of graduate students report having experienced sexual violence, AND we know survivors under-report assaults. We talk extensively about medical and legal considerations for sexual violence survivors in my "Empowering the Sexual Assault Survivor" course. Participants who took my course will need to know those protections we discussed just a few days ago are slated to be rolled back. Today, in my remote course "Trauma Informed Care", we lay the physiological and neurobiological framework for empowering the sexual assault survivor. Following that, in addition to how to continue empowering for survivors, we elaborated on the legal changes listed above.
Outrageously, these Title IX deregulating provisions are to go into effect August 14, 2020 while schools are struggling to keep students safe amid coronavirus pandemic. Again, let us look at these percentages (23% of undergraduates, and 11% of graduate students) and think about who needs safety and protection.
Schools do have choice in whether they roll back their protections to survivors of sexual violence. If you're looking for ways to help, you may want to reach out to your alma mater and ask what changes they are planning to make in the context of this new deregulation and disempowerment of Title IX protections. Maybe contact your local sexual assault coalition and see how you can become involved. You could also contact your legislature and/or leave comment on www.regulations.gov (search title IX and education).Empower yourself so that you can empower others! As a physical therapist specialized in pelvic rehabilitation, empowering survivors of sexual violence happens every day in my practice. I hope you feel empowered, supported and successful in doing this challenging work too!
It’s OK to be feeling (insert feeling) right now. (maybe: sad, fearful, angry, denial, numb, anxious, avoidant, bored?)
 It’s OK to acknowledge those feelings.
It’s OK to acknowledge those feelings.
It’s also OK to create a plan and direction about what we may do about our feelings, thoughts, and actions.
We can change how we think, what we do and ultimately how we feel.
Breathe. Place a hand on your chest and a hand on your abdomen. Practice inhaling long and deep as if you were pouring the air into your body- first filling the lower hand and then filling the top hand. Pause for a moment when you feel your canister is full and then exhale slowly (top to bottom or bottom to top- either works fine). I prefer breathing through my nose for inhale and exhale but know if you are congested, mouth breathing is fine or you can inhale through the nose and exhale through the mouth- find what works for you. Work on increasing the number counted (silently in your mind) while you inhale, pause briefly and then exhale- making that number count on exhale the same or even longer. Make it a game to see how long and deep your breath can become. Reduce intensity if feeling lightheaded.
Focus on your breath and feel calmness. Return to this breathing whenever you can.
Body Scan/Progressive Relaxation. Take a moment and scan your body for pain or tension. You can start at the top of your body or where your feet are grounded to floor. Notice your body and allow it to be, without judgement. Then starting from the top of your body or the bottom, contract your muscles systematically and then relax. Or focus on the muscle group and allow the muscles to relax and slacken. Maybe send your long, deep breath to each area? Maybe think of color washing each area? Make your scan personal and positive for you. Check-in to your body without judgement and send gratefulness for the work your amazing body does.
Stand Big. Find a wall and place your backside onto it. Pretend there is a string at the crown of your head and imagine your head being pulled up towards the ceiling. Lift your chest as you are standing tall and use your slow, steady, deep breathing to create bigness and calmness. Relax your shoulders. Maybe place the back of your hands onto wall and feel the opening of your chest. Once you have practiced this posture, you can refer to this posture during your day. Stand big, breathe big, be big.
Intentionally SCHEDULE into your life what you love. Schedule time listening to your favorite music. Maybe take up playing an instrument? Practice singing in the shower or car. Set a timer and dance fervently. Create time to draw or paint or write. Make a recipe. Get frozen berries and make smoothies. Maybe add frozen spinach to your smoothie?
Pick up a book. Play a game, cards or even solitaire. Practice Sudoku. Take a bath or shower. Go for a long walk while keeping your distance from others. Find a workout you can do at home that makes you feel powerful. Whatever you love, turn it into a scheduled ritual. Make one small goal and work towards it. Focus on what we can do instead of what we cannot. Find some activity and fulfill a passion just for you. Make sleep a priority and know if you have a bad night, that the next night you will likely sleep better. Perhaps create a sleeping ritual? Call others and ask what they are doing for themselves? Remember to forgive yourself and to feel or express the feelings that are within you. We are all going through this together. Make you a priority and schedule yourself some HAPPY.
Lastly- try to limit the news, your phone and the frig. All of these can create negative feelings that do not fulfill us.
Breathe. Find love in positive activities. Be brave. Be grateful. Forgive.
We are all in this together.
Lauren Mansell DPT, CLT, PRPC is the author and instructor of the Trauma Awareness for the Pelvic Therapist course. She is also offering several courses via Zoom video conference during the Covid-19 pandemic, which can be found on our Remote Learning Opportunities page. Prior to becoming a physical therapist, Lauren counseled suicidal and homicidal SES at-risk youth who had survived sexual violence. Lauren was certified as a medical and legal advocate for sexual assault survivors in 1999 and has advocated for over 130 sexual assault survivors of all ages in the ED. Lauren's physical therapy specialty certifications include Certified Lymphedema Therapist (CLT), Pelvic Rehabilitation Professional Certificate (PRPC) and Certified Yoga Therapist (CYT). She is a board member of Chicagoland Pelvic Floor Research Consortium, American Physical Therapy Association Section of Women's Health and Section of Oncology.
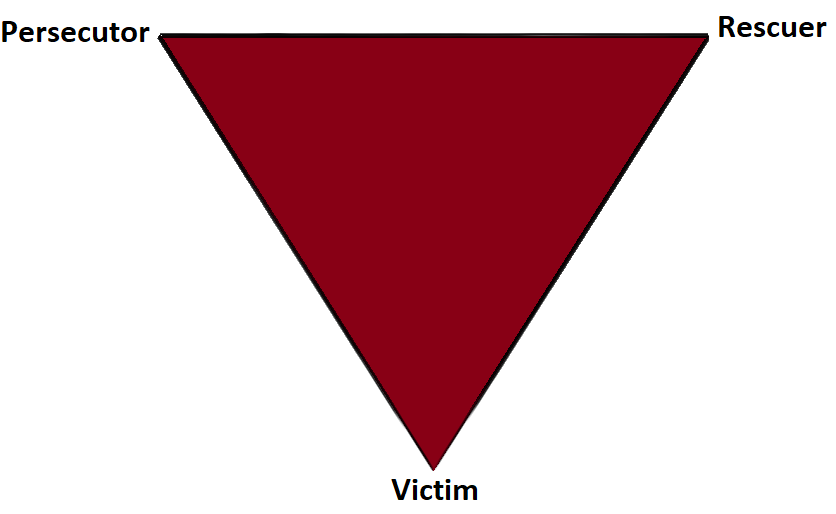
Part 2: The Drama Triangle
This is part two of a three-part series on self-care and preventing practitioner burnout from faculty member Jennafer Vande Vegte, MSPT, BCB-PMD, PRPC. Part One is available here. Jennafer is the co-author and co-instructor of the along with Nari Clemons, PT, PRPC.
Augh, I was so frustrated with myself. I fell for it again. Here’s the scenario: a patient came in suffering excruciating pain. She had been to see a pelvic health professional as well as various medical professionals and was unable to get relief and answers for her rectal pain. She was desperate and called me “her last hope.” Phrases used included, “I need you! Fix me! I hear you are a miracle worker! If you can’t help me no one can!” And just like that I took on the role of Rescuer.
In 1968 a psychiatrist named Stephen Karpman developed a model of personal interaction that he called the Conflict Triangle. It has also become known as the Karpman Triangle, The Drama triangle or the Victim triangle. Per Wikipedia:
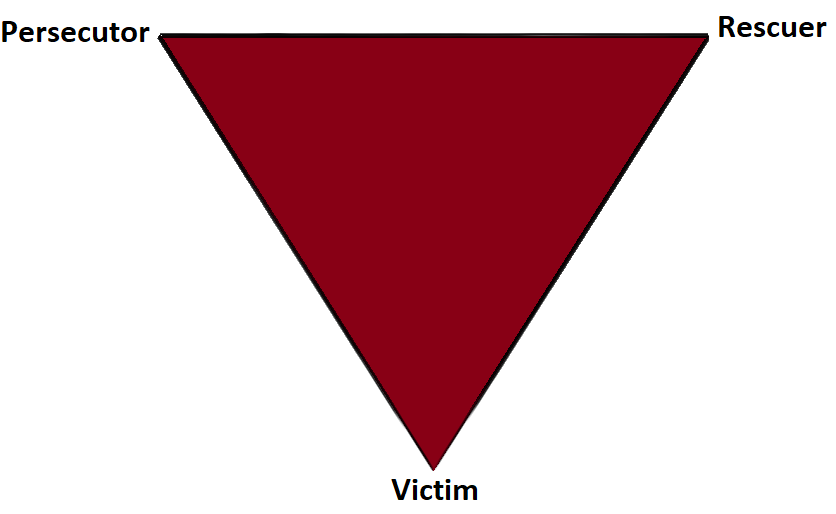
The Victim: The Victim's stance is "Poor me!" The Victim feels oppressed, helpless, hopeless, powerless and ashamed. They seem unable to make decisions, solve problems, take pleasure in life or achieve insight. The Victim, if not being persecuted, will seek out a Persecutor and also a Rescuer who may save the day, but may also perpetuate the Victim's negative feelings.
The Rescuer: The Rescuer's line is "Let me help you." A classic enabler, the Rescuer feels guilty if they don't rush to the rescue. Yet their rescuing has negative effects: It keeps the Victim dependent and gives the Victim permission to fail. The rewards derived from this rescue role are that the focus is taken off of the Rescuer. When they focus their energy on someone else, it enables them to ignore their own anxiety and issues. This rescue role is also pivotal because their actual primary interest is really an avoidance of their own problems disguised as concern for the victim’s needs.
The Persecutor: (a.k.a. Villain) The Persecutor insists, "It's your fault." The Persecutor is controlling, blaming, critical, oppressive, angry, authoritative, rigid, and superior.
 What is interesting about this triangle is that the roles are constantly shifting. In full rescuer mode, I gladly took on this patient, intent on solving her problems. Over time, I saw that my consistent coaching for lifestyle change and self-care was falling on deaf ears. My patient was not following through with anything I asked of her; therefore my treatment plan was not working. The patient began to get frustrated with me. I then cast myself as the victim. She became my persecutor! While perhaps in her mind, I had failed as the rescuer, she was still the victim and I had become her persecutor. At the time, I did not have the skills to know how to navigate this situation in a positive or helpful way. Finally I sought the advice of my supervisor and my therapist to draw up a contract with this patient. The contract outlined each of our responsibilities. If either of us didn’t fulfill our responsibilities, the consequence would be ending our professional relationship. When she persisted, unwilling to do her part, I discharged her per our agreement.
What is interesting about this triangle is that the roles are constantly shifting. In full rescuer mode, I gladly took on this patient, intent on solving her problems. Over time, I saw that my consistent coaching for lifestyle change and self-care was falling on deaf ears. My patient was not following through with anything I asked of her; therefore my treatment plan was not working. The patient began to get frustrated with me. I then cast myself as the victim. She became my persecutor! While perhaps in her mind, I had failed as the rescuer, she was still the victim and I had become her persecutor. At the time, I did not have the skills to know how to navigate this situation in a positive or helpful way. Finally I sought the advice of my supervisor and my therapist to draw up a contract with this patient. The contract outlined each of our responsibilities. If either of us didn’t fulfill our responsibilities, the consequence would be ending our professional relationship. When she persisted, unwilling to do her part, I discharged her per our agreement.
I learned so much from this experience. Here are some things that I have implemented and may be helpful in your practice if you have similar challenges.
- In an initial visit with a new patient I explain that the patient and I make a team and we each have a role to play in reaching the patient’s goals.
- If someone says, “Fix me!” I say, “Think of me as your coach, I can show you how to help your body heal, but it’s your job to do the work.”
- When I hear, “Everyone says you are a miracle worker.” I say, “That is so kind, but it doesn’t work that way. Healing is complicated and everyone has their own journey.”
- In this way, with baby steps, we can get OUT of the drama triangle and into healthy relationships with our patients and the people in our lives.
- Consider the Winner's Triangle published by Acey Choy in 1990.
In her blog NextMeCoaching, Jessica Vader coaches on turning Drama and Control into a Winning situation.
The three roles in the Winner’s Triangle.
Vulnerable – a victim should be encouraged to accept their vulnerability, problem solve, and be more self-aware.
Assertive – a persecutor should be encouraged to ask for what they want, be assertive, but not punishing.
Caring – a rescuer should be encouraged to show concern and be caring, but not over reach and problem solve for others.
If you struggle with professional and personal boundaries, you are not alone, and you can get support. Consider talking with your supervisor, a counselor, reading a good book on the subject, and or taking Boundaries, Mediation and Self Care, a course offering through Herman and Wallace that was designed to help pelvic health professionals stay healthy and inspired while equipping therapists with new tools to share with their patients.
We hope you will join us for Boundaries, Mediation and Self Care this November 9-11, 2019 in San Diego, CA.
Look forward to my next blog where saying no takes an unexpected turn.
The number of individuals who identify as transgender is growing each year. The Williams Institute estimated in 2016 that 0.6% of the U.S. population or roughly 1.4 million people identified as transgender (Flores, 2016). This was a 50% increase from a 2011 survey which estimated only 0.3% or 700,000 people identified as transgender (Gates, 2011). Though these numbers are growing each year, due to increased visibility and social acceptance, it is presumed that these numbers are underreported due to inadequate survey methods, stigma/fear associated with “coming out” and deficient definitions of the multitude of options for gender identity (Flores, 2016).

Though organizations such as WPATH have attempted to standardized care, the patient experience and reception of quality care are significantly lacking. In 2015 the National Center for Transgender Equality performed a groundbreaking survey of 27,215 respondents with the aim to “understand the lives and experiences of transgender people in the United States and the disparities that many transgender people face” (“About,”n.d., para. 1). This survey revealed that 33% of individuals who saw a health care provider had at least one negative experience related to being transgender (National Center for Transgender Equality, 2015). Negative experiences included; being refused treatment, verbal harassment, physically or sexually assault, and teaching the provider about transgender people in order to get appropriate care (National Center for Transgender Equality, 2015). Alternatively, 23% of respondents did not see a doctor when they needed to because of fear of being mistreated as a transgender person (National Center for Transgender Equality, 2015). Though these statistics are staggering and affronting there is hope for a better future.
Research for the care of these patients, specifically related to pelvic floor physical therapy, is on the rise. In the Annals of Plastic Surgery, an article was published with the purpose to capture incidence and severity of pelvic floor dysfunction pre-surgery, monitor any progression of symptoms with standardized outcome measures and highlight the role of physical therapy in the treatment of patients undergoing vaginoplasty (Manrique, et al., 2019). While in the Journal of Obstetrics & Gynecology a retrospective case series similarly focused on physical therapy pre and post-operatively highlighting dilator selection and success, pelvic floor dysfunction including bowel and bladder as well as reported abuse history (Jiang, Gallagher, Burchill, Berli, & Dugi, 2019). Through articles such as these clinicians can expect an uptick in calls questioning if they treat these patients. This begs the question of, "How can you best prepare?"
The answer is simple, attend continuing education. It is where you can not only learn evidence-based evaluation and treatment but also connect with other providers and mentors that care for these patients. In 2020 Herman & Wallace will be offering a continuing education course that serves this exact purpose. Keep your eyes on next years offerings, as spaces will surely fill quickly.
About. (n.d.). Retrieved May 15, 2019, from http://www.ustranssurvey.org/about
Dora Richter. (2019, May 09). Retrieved May 15, 2019, from https://en.wikipedia.org/wiki/Dora_Richter
Jiang, D. D., Gallagher, S., Burchill, L., Berli, J., & Dugi, D. (2019). Implementation of a Pelvic Floor Physical Therapy Program for Transgender Women Undergoing Gender-Affirming Vaginoplasty. Obstetrics & Gynecology,133(5), 1003-1011. doi:10.1097/aog.0000000000003236
Manrique, O. J., Adabi, K., Huang, T. C., Jorge-Martinez, J., Meihofer, L. E., Brassard, P., & Galan, R. (2019). Assessment of Pelvic Floor Anatomy for Male-to-Female Vaginoplasty and the Role of Physical Therapy on Functional and Patient-Reported Outcomes. Annals of Plastic Surgery,82(6), 661-666. doi:10.1097/sap.0000000000001680
National Center for Transgender Equality. (2015). Annual report of the U.S. Transgender Survey. Retrieved May 15, 2019, from https://transequality.org/sites/default/files/docs/usts/USTS-Executive-Summary-Dec17.pdf
Wpath. (n.d.). Standards of Care version 7. Retrieved May 15, 2019, from https://www.wpath.org/publications/soc
 In July of this year, I was invited to present in Christchurch, New Zealand as part of a teaching tour that took in Singapore, Australia and Tasmania. The topic of my class was female pelvic pain, so we discussed Endometriosis, Vulvodynia, Sexual Health and many other sub-topics but we had several discussions about the effects of trauma on pelvic pain. For those who have visited Christchurch, it is a beautiful city but it is still reeling from a series of massive earthquakes, that started in September 2010. The most devastating was in February 2011, when 185 people were killed and 6600 people were injured. Everywhere you go in Christchurch, there are reminders – from the constant buzz of ongoing construction, to structures that are waiting demolition, like the beautiful old cathedral that was beside our hotel. Usually, when I teach, we do some ‘housekeeping’ announcements about fire drills and exits; in Christchurch it was ‘In the event of an earthquake…’. I wondered how the near constant reminders were affecting the inhabitants, so I read of how ‘…people called living with continual shaking, damaged infrastructure, insurance battles and unrelenting psychological stress ‘the new normal’. There are several ongoing research studies, looking at the effects of this trauma and how it is still having an effect on the people of Christchurch.
In July of this year, I was invited to present in Christchurch, New Zealand as part of a teaching tour that took in Singapore, Australia and Tasmania. The topic of my class was female pelvic pain, so we discussed Endometriosis, Vulvodynia, Sexual Health and many other sub-topics but we had several discussions about the effects of trauma on pelvic pain. For those who have visited Christchurch, it is a beautiful city but it is still reeling from a series of massive earthquakes, that started in September 2010. The most devastating was in February 2011, when 185 people were killed and 6600 people were injured. Everywhere you go in Christchurch, there are reminders – from the constant buzz of ongoing construction, to structures that are waiting demolition, like the beautiful old cathedral that was beside our hotel. Usually, when I teach, we do some ‘housekeeping’ announcements about fire drills and exits; in Christchurch it was ‘In the event of an earthquake…’. I wondered how the near constant reminders were affecting the inhabitants, so I read of how ‘…people called living with continual shaking, damaged infrastructure, insurance battles and unrelenting psychological stress ‘the new normal’. There are several ongoing research studies, looking at the effects of this trauma and how it is still having an effect on the people of Christchurch.
If you’ve attended Pelvic Floor Level 1 with Herman & Wallace, you’ll remember we quote a study from Van der Welde about the effects of perceived danger on muscle activity in the upper trapezius and pelvic floor muscles. We also discuss the work of Levine, of ‘Waking the Tiger’ fame, who explores the somatic effects of trauma in our bodies – and how trauma, much like pain, is whatever we say it is.
I became intrigued with the topic, so I was delighted to hear that Lauren Mansell has created a course to deal exactly with this topic. I was even more delighted when she sat down for a chat with me to explore the nuances of trauma awareness, boundary setting and self-care for therapists, especially pelvic therapists, who work with those who have experienced trauma of any kind.
I hope you find this conversation as interesting as I did! Here is our conversation:
1. ‘Vaginismus, a Component of a General Defensive Reaction. An Investigation of Pelvic Floor Muscle Activity during Exposure to Emotion-Inducing Film Excerpts in Women with and without Vaginismus’ van der Velde, J & Laan, Ellen & Everaerd, W. (2001)
2. ‘Waking The Tiger’ by Peter A. Levine (1997)
In a previous post on The Pelvic Rehab Report Sagira Vora, PT, MPT, WCS, PRPC told us how "women with sexually adverse experiences tend to have impaired genital response when in consensual sexual situations, however, women who do not have sexual abuse histories and but have sexual pain tend to have appropriate genital response." Today Sagira helps us understand how the pelvic floor responds to consensual sexual activity in women with a history of sexual trauma.
Today we try to look for answers for questions that came up during the last blogs.
 How does the cohort that has had adverse sexual experiences present? How do women with history of sexual trauma process sexual experiences? How does the pelvic floor present or respond to consensual sexual situations when a woman has been abused in the past?
How does the cohort that has had adverse sexual experiences present? How do women with history of sexual trauma process sexual experiences? How does the pelvic floor present or respond to consensual sexual situations when a woman has been abused in the past?
To answer these questions, it’s important to understand two facts about the pelvic floor. 1) the pelvic floor plays a role in emotional processing1, and 2) muscle activity in all muscles, including the pelvic floor, increases with exposure to stress and during anxiety evoking experiences2.
We explored in the last blog that women with sexual abuse histories responded with increased pelvic floor overactivity when watching movie clips with sexually threatening and consensual sexual content. Apparently, for women with sexual abuse history even consensual sexual situations can be experienced as threatening1.
Lehrer et. al. found overactivity in the neuronal and hormonal circuits that increase sexual arousal and activity. These circuits are already overactive in individuals who have Post Traumatic Stress Disorder (PTSD), and increased activity can increase anxiety, fear and other symptoms of PTSD instead of normal sexual arousal and excitement during a sexual experience2. For the woman with PTSD this means that sexual arousal signals impending threat rather than pleasure1. And as we already learned in previous blogs and above that when humans feel threatened they respond by tightening muscles and most notably the pelvic floor muscle.
Significant co-relation is found between sexual abuse, subsequent PTSD and chronic pelvic pain3. Hooker et. al, found irritable bowel syndrome, pelvic pain, and physical and sexual abuse to be the most commonly diagnosed together4. More importantly, when patients were successfully treated for PTSD they continued to be 2.7 times more likely to have pelvic floor dysfunction and 2.4 times more likely to have sexual dysfunction. This builds the case for interventions that are multidisciplinary to help patients of abuse and sexual assault, with the pelvic floor therapist playing a significant role.
In the next blog, lets explore how the pelvic floor therapist can work with a counselor and a sex therapist to help the woman with sexual pain dysfunction.
Anna Padoa and Talli Rosenbaum. The overactive pelvic floor. Springer. 1st ed. 2016
Yehuda R, Lehrner A, Rosenbaum TY. PTSD and sexual dysfunction in men and women. J Sex Med. 2015:12(5):1107-19
Blok BF. Holstege G. The neuronal control of micturition and its relation to the emotional motor system. Prog Brain Res. 1996; 107:113-26
Para ML, Chen LP, Goranson EN, Sattler AL, Colbenson KM, Seime RJ, Et. al. Sexual abuse and lifetime diagnoses of somatic disorders. JAMA. 2013; 302:550-61
Hooker AB, van Moorst BR, van Haarst EP, Van Ootegehem NAM, van Dijken DKE, Heres MHB, Chronic pelvic pain: evaluation of the epidemiology, baseline characteristics, and clinical variables via a prospective and multidisciplinary approach. Clin Exp Obstet Gynecol. 2013; 40:492-8