Constipation, which includes rectal evacuation disorders, slow transit constipation, and IBS to name a few is one of the most common gastrointestinal disorders worldwide (1,2). The complexity of constipation and its impact on a person’s health and quality of life is often misunderstood and common treatment strategies such as diet, exercise, hydration, and stress management can be an oversimplification of what is necessary to effectively manage the disorder (1). From a rehabilitation lens, it is pivotal to prioritize the function of the nervous system when developing a treatment strategy for constipation, considering the nervous system is the central control mechanism of all functions and processes in the human body.
Dry needling, specifically, dry needling with electrical stimulation, is one of the most impactful tools we have in rehabilitation to improve the health and function of the nervous system. Dry needling has evolved from a procedure that utilizes a monofilament needle to deliver mechanical input into “trigger points” in muscle tissue to include the use of a monofilament needle for the delivery of electrical stimulation, which is often described as percutaneous electrical stimulation or neuromodulation. The use of electrical stimulation with dry needling can have a profound effect on improving the healing capacity of tissues and the overall functional recovery of the human body primarily due to the impact it has on the nervous system. Therefore, we must have a sound understanding of the neuroanatomy and physiology of any region of the body and the associated dysfunction to effectively develop and implement a treatment plan.
The gastrointestinal system is considered the most complicated system in our body in terms of the number of structures involved in function and regulation and the enormity of neurons that innervate the gastrointestinal tract, and it is yet to be fully understood (3). The enteric nervous system, which is commonly considered the third branch of the autonomic nervous system, is at the center of regulatory control of the gastrointestinal (GI) tract and precisely coordinates the function of GI neurons, glial cells, macrophages, interstitial cells, and enteroendocrine cells which drives gut motility and secretions (3). It is interesting to note that the sophistication of the enteric nervous system allows the GI tract to be able to function independently of any neural inputs from the central nervous system (3,4). However, normal physiologic functioning of the GI tract is influenced by bidirectional neuronal connections between the enteric and central nervous systems which is known as the “brain-gut-axis” (3).
Embedded in the walls of the GI tract are the myenteric and submucosal plexuses of the enteric nervous system, which innervate the GI tract and uniquely provide both excitatory and inhibitory motor neurons (4). The myenteric plexus lies between the longitudinal and circular muscle layers of the GI tract and coordinates smooth muscle movements or gut propulsions (“motility”) while the submucosal plexus is found within the connective tissues of the submucosa and regulates secretion, absorption, and blood flow in the GI tract (3,4).
The sympathetic and parasympathetic nervous systems influence the function of the GI tract primarily through integrated neuronal activity with the enteric nervous system versus direct innervation to the wall of the gut, with the exception of blood vessels and sphincters which receive direct sympathetic innervation (3).
Sympathetic inputs to the GI tract regulate secretion and motility and parasympathetic inputs to the distal colon are important for colonic motility and defecation (3).
The function of the somatic nervous system innervating key structures involved with defecation should be equally prioritized to comprehensively evaluate factors contributing to constipation. This may include spinal nerves from the thoracolumbar and sacral vertebral segments, the iliohypogastric and ilioinguinal nerves, the pudendal nerve, the levator ani nerve, and even the phrenic nerve if we are considering the innervation and function of the diaphragm and the importance of breathing mechanics and control of intraabdominal pressure during voiding.
From a treatment perspective, the most impactful window of access to modulate activity in the gastrointestinal tract using dry needling with electrical stimulation is targeting spinal nerves and associated peripheral nerves and their target organs (primarily muscle tissue) that converge with our autonomic nervous system innervating the gut (5). Additionally, electrical stimulation applied directly over the involved target tissue in the GI tract can help facilitate changes in GI function because the enteric nervous system is embedded in the wall of the GI lumen. The rationale for the use of neuromodulation to impact the function of the gastrointestinal tract is that our system is a bioelectric system, therefore, the application of electrical stimulation can have a profound impact on neuromuscular function which is interrelated with neurovascular, neuroimmune function, neuroinflammatory function, neuroendocrine function and so on (5, 6, 7). There is even evidence that electrical stimulation can impact the concentration of bacterial populations in the GI tract which can influence the overall function of the gut. Lastly, ongoing dysfunction in gastrointestinal tissue or any visceral tissue can create neuromotor dysfunction in associated somatic tissues that may include pain, tissue sensitization, abnormal muscle tone, and abnormal motor control strategies which can be effectively and efficiently treated with dry needling and electrical stimulation.
In conclusion, dry needling with electrical stimulation is one the best tools used in conjunction with traditional rehabilitation strategies to create meaningful, sustainable improvements in the function of the human body. If you want to learn more about the implementation of dry needling into your practice as it relates to constipation or gastrointestinal disorders, join us on an upcoming course!
Dry Needling and Pelvic Health: Foundational Concepts and Techniques
Dry Needling and Pelvic Health 2: Advanced Concepts and Neuromodulation
Dry Needling and Pelvic Health: Pregnancy and Postpartum Considerations
References
- Forootan M, Bagheri N, Darvishi M. Chronic constipation: A review of literature. Medicine (Baltimore). 2018;97(20):e10631. doi:10.1097/MD.0000000000010631
- Black CJ, Ford AC. Chronic idiopathic constipation in adults: epidemiology, pathophysiology, diagnosis and clinical management. Med J Aust. 2018;209(2):86-91. doi:10.5694/mja18.00241
- Sharkey KA, Mawe GM. The enteric nervous system. Physiol Rev. 2023;103(2):1487-1564. doi:10.1152/physrev.00018.2022
- Spencer NJ, Hu H. Enteric nervous system: sensory transduction, neural circuits and gastrointestinal motility. Nat Rev Gastroenterol Hepatol. 2020;17(6):338-351. doi:10.1038/s41575-020-0271-2
- Larauche M, Wang Y, Wang PM, et al. The effect of colonic tissue electrical stimulation and celiac branch of the abdominal vagus nerve neuromodulation on colonic motility in anesthetized pigs. Neurogastroenterol Motil. 2020;32(11):e13925. doi:10.1111/nmo.13925
- Zhang C, Chen T, Fan M, et al. Electroacupuncture improves gastrointestinal motility through a central-cholinergic pathway-mediated GDNF releasing from intestinal glial cells to protect intestinal neurons in Parkinson's disease rats. Neurotherapeutics. 2024;21(4):e00369.
- Jacobson A, Yang D, Vella M, Chiu IM. The intestinal neuro-immune axis: crosstalk between neurons, immune cells, and microbes. Mucosal Immunol. 2021;14(3):555-565. doi:10.1038/s41385-020-00368-1
AUTHOR BIO:
Tina Anderson, MS PT
 Tina Anderson (she/her) received her Master of Science in Physical Therapy in 2001 from Grand Valley State University located in Grand Rapids, Michigan. She graduated from Michigan State University in 1996 with a Bachelor of Science in Kinesiology. Tina specializes in treating patients with complex neuromusculoskeletal dysfunction including dysfunctions of the pelvic floor. Tina earned her dry-needling certification in 2006 and has been teaching dry-needling nationwide since 2008. Tina was integral in pioneering dry-needling techniques for the pelvic floor and surrounding neuroanatomical structures. She currently owns and operates a private physical therapy practice in Aspen, Colorado. Tina and her family, including their new “fur” child Beatrice, love living and playing in the Rocky Mountains!
Tina Anderson (she/her) received her Master of Science in Physical Therapy in 2001 from Grand Valley State University located in Grand Rapids, Michigan. She graduated from Michigan State University in 1996 with a Bachelor of Science in Kinesiology. Tina specializes in treating patients with complex neuromusculoskeletal dysfunction including dysfunctions of the pelvic floor. Tina earned her dry-needling certification in 2006 and has been teaching dry-needling nationwide since 2008. Tina was integral in pioneering dry-needling techniques for the pelvic floor and surrounding neuroanatomical structures. She currently owns and operates a private physical therapy practice in Aspen, Colorado. Tina and her family, including their new “fur” child Beatrice, love living and playing in the Rocky Mountains!
At Herman & Wallace, we’re committed to providing practitioners with the knowledge and skills they need to offer the best care possible. We’ve heard your feedback regarding the lack of familiarity with rectal balloon catheters, and we’re excited to announce a new remote course: Anorectal Balloon Catheters: Introduction and Practical Application.
Course Overview
This short but comprehensive course offers 5.5 contact hours dedicated to the essential aspects of using rectal balloon catheters in treating patients experiencing defecatory dysfunction. It is designed for those who have completed Pelvic Function Level 1.
While this course will be conducted remotely, participants are required to register with another clinician to facilitate hands-on lab practice.
Learning Objectives
Participants will explore a range of topics, including:
- Understanding Anatomy and Physiology: Gain insights into the relevant anatomy and pathophysiology associated with defecatory conditions.
- Assessment Techniques: Learn how to assess sensation in the anal canal related to defecation using balloon catheters.
- Treatment Planning: Develop appropriate treatment plans for patients with hypersensitivity and hyposensitivity affecting defecation.
- Indications and Contraindications: Understand when balloon training is appropriate and explore in-depth treatment guidelines.
- Data Interpretation: Learn how to interpret assessment data gathered during balloon catheter evaluations and formulate effective treatment strategies.
Join Us
Anorectal Balloon Catheters: Introduction and Practical Application is perfect for practitioners eager to enhance their skill set in managing defecatory dysfunction through advanced techniques. We invite you to join senior faculty Allison Arial on December 14th for this enriching educational opportunity.
Don’t miss the chance to expand your expertise and improve your clinical practice. Register now and be part of a course designed to elevate the standard of care for your patients!
An Ancient Science with a Modern Evidence-Based Approach
A 15-year-old patient walked into the clinic with her mom presenting with symptoms of constipation, lower abdominal spasms, and pain with bowel movements. Over the course of the visit, I learned that she was on medication for depression and was also suffering from chronic anxiety. Anxiety pervaded every aspect of her life, from things happening during the day to her near and far future. Her symptoms were worse when her anxiety was high and she struggled to relax her body and mind.
So, in addition to teaching her a program with breathing exercises, self-abdominal massage, pelvic girdle stretching, and the use of a squatty potty, I also taught her perineal self-acupressure at the acupoint Central Vessel 1 (CV 1) for constipation and two self-regulation points Central Vessel 17 (CV 17) and Yintang (EX-HN 3) for alleviating her anxiety.
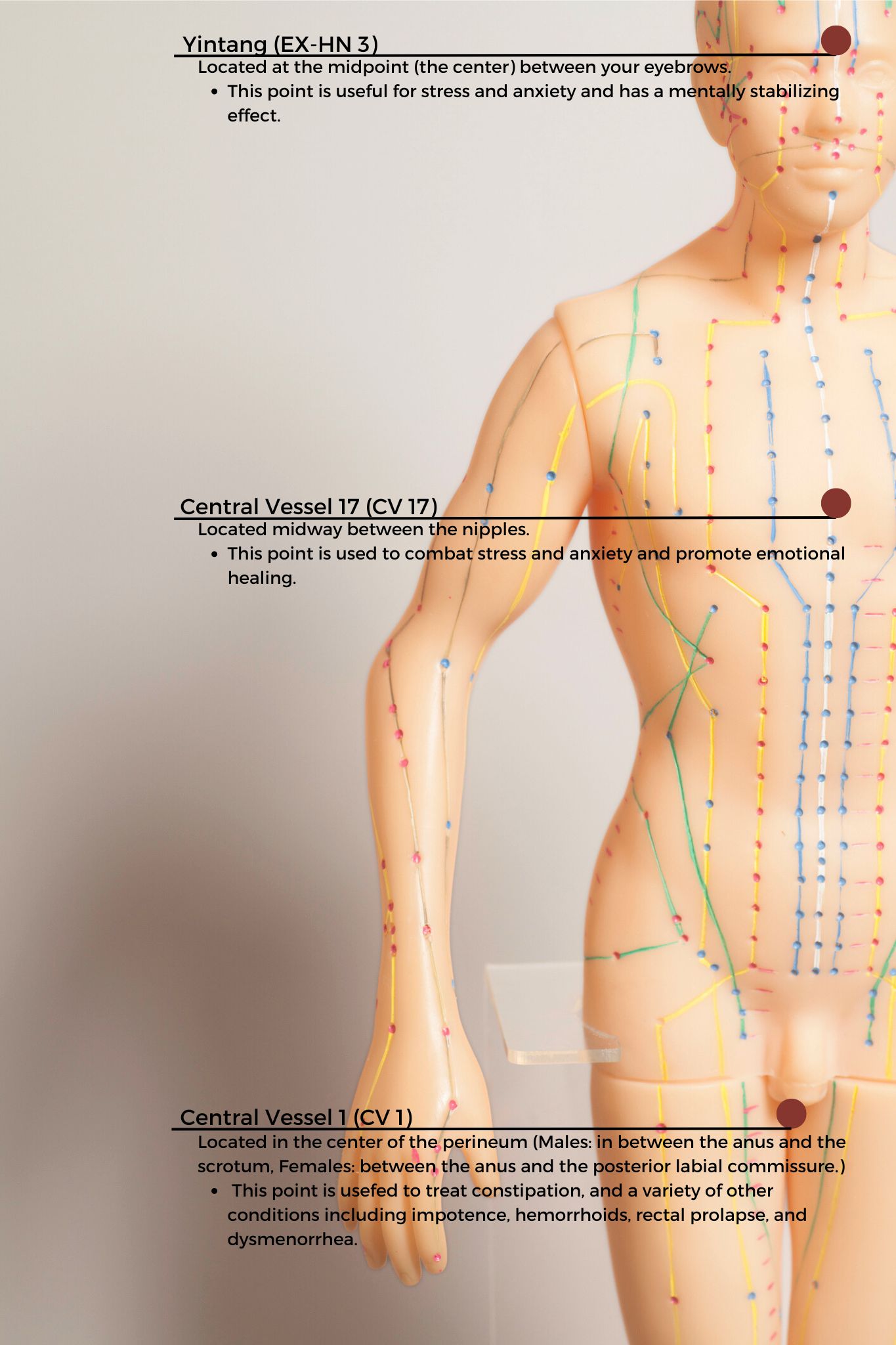 CV1 also known as Huiyin is located at the perineum. A study by Abbott et al. reported that the perineal self-acupressure technique was found to be remarkably effective with statistically significant and clinically meaningful improvements in Patient Assessments of Constipation Quality of Life (PAC-QOL All), modified Bowel Function Index (BFI), and the Short-Form Health Survey (SF-12v2). Huiyin is used in Traditional Chinese Medicine (TCM) not only to treat constipation, but also a variety of conditions including impotence, hemorrhoids, rectal prolapse, and dysmenorrhea. CV17 is located at the center of the chest and is known to be a point for emotional healing while Yintang (EX-HN 3) is located between the eyebrows and is known to have a mentally stabilizing effect in Traditional Chinese Medicine (TCM).
CV1 also known as Huiyin is located at the perineum. A study by Abbott et al. reported that the perineal self-acupressure technique was found to be remarkably effective with statistically significant and clinically meaningful improvements in Patient Assessments of Constipation Quality of Life (PAC-QOL All), modified Bowel Function Index (BFI), and the Short-Form Health Survey (SF-12v2). Huiyin is used in Traditional Chinese Medicine (TCM) not only to treat constipation, but also a variety of conditions including impotence, hemorrhoids, rectal prolapse, and dysmenorrhea. CV17 is located at the center of the chest and is known to be a point for emotional healing while Yintang (EX-HN 3) is located between the eyebrows and is known to have a mentally stabilizing effect in Traditional Chinese Medicine (TCM).
The patient returned the next visit and reported that her abdominal spasms were 50% better and she no longer had pain with bowel movements. She also reported that she felt calmer and was able to use the perineal self-acupressure technique to evacuate very quickly. Over the past several years, I have found that adding Acupressure to my clinical practice has added so much value as an Integrative holistic tool to complement traditional care.
Evidence-based Integrative health and medicine practices blend traditional physical therapy methods with holistic practices that address the whole person-physically, mentally, emotionally, and spiritually (Justice et al). Acupressure is considered an Integrative medicine practice and is based on traditional Chinese meridian theory in which acupuncture points are pressed to stimulate the flow of energy or Qi. Acupuncture meridians are believed to form a network throughout the body, connecting peripheral tissues to each other and to the central viscera. This tissue network is also continuous with more specialized connective tissues such as periosteum, perimysium, perineurium, pleura, peritoneum, and meninges (Kaptchuk).
There is robust scientific evidence supporting acupressure as an effective non-pharmacological therapy for the management of a host of conditions such as anxiety, insomnia, chronic pelvic pain, dysmenorrhea, infertility, constipation, digestive disturbances, and urinary dysfunctions to name a few.
Acupressure has demonstrated the ability to improve heart rate variability, and thus decrease sympathetic nervous system activity. By decreasing sympathetic nervous system stimulation, the release of stress hormones such as epinephrine and cortisol is decreased, and the relaxation response can be augmented, which may correlate with decreasing levels of pain, stress, and anxiety (Monson et al).
To learn more about Acupressure, join the upcoming remote course Acupressure for Optimal Pelvic Health scheduled for October 12th-13th. This course introduces practitioners to the basics of traditional Chinese medicine (TCM), acupuncture & acupressure, and provides an introduction to Yin yoga. Of the 12 major Meridians or energy channels, the focus is on the majority of acupoints in the Bladder, Kidney, Stomach, and Spleen meridians. In addition, there are other important meridian points that stimulate the nervous system and can be used for self-regulation, improving the flow of Qi the life force energy to improve the physiological functioning of the organs. The course also explores Yin poses within each meridian to channelize energy through neurodynamic pathways with powerful integrative applications across multiple systems. If you are not able to attend the October course date, then check out the website for the options scheduled for 2025.
References
- Chen SR, Hou WH, Lai JN, Kwong JSW, Lin PC. Effects of Acupressure on Anxiety: A Systematic Review and Meta-Analysis. J Integr Complement Med. 2022;28(1):25-35. doi:10.1089/jicm.2020.0256
- Abbott R, Ayres I, Hui E, Hui KK. Effect of perineal self-acupressure on constipation: a randomized controlled trial. J Gen Intern Med. 2015;30(4):434-439.
- Kaptchuk TJ. 2000. The web that has no weaver. Understanding Chinese medicine. Chicago: Contemporary Publishing Group, Inc.
- Justice C, Sullivan MB, Van Demark CB, Davis CM, Erb M. Guiding Principles for the Practice of Integrative Physical Therapy. Phys Ther. 2023;103(12):pzad138. doi:10.1093/ptj/pzad138
- Monson E, Arney D, Benham B, et al. Beyond Pills: Acupressure Impact on Self-Rated Pain and Anxiety Scores. J Altern Complement Med. 2019;25(5):517-521.
- Abaraogu UO, Igwe SE, Tabansi-Ochiogu CS. Effectiveness of SP6 (Sanyinjiao) acupressure for relief of primary dysmenorrhea symptoms: A systematic review with meta- and sensitivity analyses. Complement Ther Clin Pract. 2016;25:92-105
- He Y, Guo X, May BH, et al. Clinical Evidence for Association of Acupuncture and Acupressure With Improved Cancer Pain: A Systematic Review and Meta-Analysis. JAMA Oncol. 2020;6(2):271-278. doi:10.1001/jamaoncol.2019.5233
AUTHOR BIO
Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200
 Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 (she/her) graduated from Columbia University, New York with a Doctor of Physical Therapy degree. Rachna has been working in outpatient hospital and private practice settings for over 15 years with a dual focus on Orthopedics and Pelvic Health. She was instrumental in starting one of the first Women’s Health Programs in an outpatient orthopedic clinic setting in Mercer County, New Jersey in 2009. She has authored articles on pelvic health for many publications. She is a Certified Integrated Manual Therapist through Great Lakes Seminars, is Board-certified in Orthopedics, is a certified Pelvic Rehab Practitioner, and is also a registered yoga teacher through Yoga Alliance. Rachna has trained in both Hatha Yoga and Yin Yoga traditions and brings the essence of Yoga to her clinical practice.
Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 (she/her) graduated from Columbia University, New York with a Doctor of Physical Therapy degree. Rachna has been working in outpatient hospital and private practice settings for over 15 years with a dual focus on Orthopedics and Pelvic Health. She was instrumental in starting one of the first Women’s Health Programs in an outpatient orthopedic clinic setting in Mercer County, New Jersey in 2009. She has authored articles on pelvic health for many publications. She is a Certified Integrated Manual Therapist through Great Lakes Seminars, is Board-certified in Orthopedics, is a certified Pelvic Rehab Practitioner, and is also a registered yoga teacher through Yoga Alliance. Rachna has trained in both Hatha Yoga and Yin Yoga traditions and brings the essence of Yoga to her clinical practice.
Rachna currently practices in an outpatient setting. The majority of her clinical orthopedic practice has focused on treating musculoskeletal, neurological, pre- and post-operative surgical conditions to name a few. She specializes in working with pelvic health patients who have bowel & bladder issues with high pelvic pain which sparked her interest in Eastern holistic healing traditions and complementary medicine. She has spent many hours training in holistic healing workshops with teachers based worldwide. She is a member of the American Physical Therapy Association and a member of APTA’s Academy of Orthopaedic Physical Therapy and Academy of Pelvic Health Physical Therapy.
Rachna also owns TeachPhysio, a PT education and management consulting company. Her course Acupressure for Optimal Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional, and energy body.
The diagnosis of chronic constipation may seem like a simple concept; however, bowel patients can be a challenging group within our pelvic health population. The interesting part about treating these patients is that constipation can result in a variety of complaints. Diaz et al confirmed this in their 2023 research. Their article shared that “Constipation encompasses several subtypes, each with its unique characteristics and underlying factors.”(1) Common complaints can include frequency, size, length, and consistency which can become overwhelming for the practitioner to decide which clinical complaints seem the most important to focus on.
Knowing how to effectively treat these patients and ask the right questions is valuable in the scheme of pelvic floor rehab, secondary to overlapping symptoms and etiology of chronic constipation. Consideration needs to be taken into account for any outside factors that can also contribute to patient complaints. For example, taking different prescription medications, supplements, and eating different foods can all influence the patient's stool frequency and formation (2). Realizing where this issue stems from is the deep-dive question to get a handle on their complaints.
Bowel frequency can be one of the biggest clinical challenges for clinicians to educate patients to master – consistency is key! Understanding what their normal frequency should be, or what it should be now, is part of the clinical judgment skill when setting goals. If your patient is only getting a natural bowel movement urge every 10 days, their goal of daily BMs, at first, should be emotionally readjusted so that they don’t feel like they have failed their rehabilitation goals.
Learning colon physiology helps to understand normal vs abnormal motility and can be helpful in treating your patient’s constipation. In my course, Bowel Pathology and Physiology we discuss the physiological reflex that controls the lower motility of the GI tract following a meal (3). When patients present with chronic constipation, they may be experiencing a profound loss of the gastrocolic reflex. The course is filled with clinical pearls and research tidbits that help to improve or slow down colonic motility. Join me in the next course offering on September 14-15, 2024 to learn more.
Resources:
- Diaz S, Bittar K, Hashmi MF, et al. [Updated 2023 Nov 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513291/
- Araújo MM, Botelho PB. Probiotics, prebiotics, and synbiotics in chronic constipation: Outstanding aspects to be considered for the current evidence. Front Nutr. 2022 Dec 8;9:935830. doi: 10.3389/fnut.2022.935830. PMID: 36570175; PMCID: PMC9773270.
- Mawer S, Alhawaj AF. Physiology, Defecation. 2023 Nov 13. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 30969554.
AUTHOR BIO
Lila Abbate, PT, DPT, MS, OCS, WCS, PRPC
 Lila Abbate is the Director/Owner of New Dimensions Physical Therapy. She graduated from Touro College in Dix Hills, NY with a Bachelor of Science (BS) in Health Sciences and a Master of Arts (MA) in Physical Therapy in 1997. She completed her Advanced Masters in Manual Orthopedic Physical Therapy (MS) at Touro College, Bayshore, NY in 2003 and continued to pursue her Doctor of Physical Therapy (DPT) at Touro in 2005. Dr. Abbate is a Board-Certified Specialist by the American Physical Therapy Association in Orthopedics (OCS) 2004 and Women’s Health (WCS) 2011. She obtained the Certified Pelvic Rehabilitation Practitioner (PRPC) from the Herman & Wallace Institute in 2014. She is a Diane Lee/LJ Lee, Integrated Systems Model (ISM) graduate and completed the New York series in 2012.
Lila Abbate is the Director/Owner of New Dimensions Physical Therapy. She graduated from Touro College in Dix Hills, NY with a Bachelor of Science (BS) in Health Sciences and a Master of Arts (MA) in Physical Therapy in 1997. She completed her Advanced Masters in Manual Orthopedic Physical Therapy (MS) at Touro College, Bayshore, NY in 2003 and continued to pursue her Doctor of Physical Therapy (DPT) at Touro in 2005. Dr. Abbate is a Board-Certified Specialist by the American Physical Therapy Association in Orthopedics (OCS) 2004 and Women’s Health (WCS) 2011. She obtained the Certified Pelvic Rehabilitation Practitioner (PRPC) from the Herman & Wallace Institute in 2014. She is a Diane Lee/LJ Lee, Integrated Systems Model (ISM) graduate and completed the New York series in 2012.
Dr. Abbate has been an educator for most of her physical therapy career. She has experience as a full-time faculty at Touro College, Manhattan Campus from 2002 to 2006 teaching the biomechanical approach to orthopedic dysfunction and therapeutic exercise as well as massage/soft tissue work that highlighted trigger point work, scar management, and myofascial release. She is currently on faculty as a Lecturer at Columbia University teaching the private practice section Business & Management course (since 2016) along with the Pelvic Health elective (since 2012). She teaches nationally and internationally with the Herman & Wallace Pelvic Rehabilitation Institute teaching advanced courses of her own intellectual property: Orthopedic Assessment for the Pelvic Health Therapist, Bowel Pathology Function, Dysfunction and the Pelvic Floor, Coccydynia & Painful Sitting: Orthopedic Implications. She was a co-writer for the Pudendal Neuralgia course and teaches the Pelvic Function Series, and Pregnancy/Postpartum Series. She has written two book chapters in 2016: Pelvic Pain Management by Valvoska and Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies by Chughtai.
Lila is a member of the American Physical Therapy Association, the National Vulvodynia Association, the American Urogynecology Association, the International Pelvic Pain Society, and is also a Senior Physical Therapy consultant for SI Bone, a sacroiliac joint instrumentation company.
Lila Abbate PT, DPT, OCS, WCS, PRPC is the creator and instructor of Bowel Pathology, Function, & Dysfunction and Coccydynia and Painful Sitting. She also co-wrote the course Pudendal Neuralgia and Nerve Entrapment with fellow H&W faculty member Pamela Downey.
Often pelvic health physical therapists are nervous about treating patients with bowel dysfunction and constipation. Lila Abbate's mentor, Elise Stettner, is proud to be a PT who treats bowel conditions. “Any PT can treat urinary symptoms. The patients who are really suffering are those with bowel dysfunctions.” She passed this passion on to Lila, who is the creator and instructor of the Bowel Pathology, Function, & Dysfunction scheduled next on November 13-14, 2021.
Bowel dysfunctions and constipation are often embarrassing for those who suffer from them and thus are often under-reported, which may lead to statistical underrepresentation. The statistics that we do have show that the average prevalence of constipation worldwide in adults is 16%, and for adults over the age of 60 is over 33.5%. (1) Everyone has a different normal for bowel habits which makes it hard to define a normal frequency. Constipation can generally be defined as less than three bowel movements per week and can present as infrequent bowel movements or difficult passage of stools that lasts for several weeks.
There are many potential facets to pelvic floor muscle problems concerning constipation. Lila shares that she recommends that therapists provide a muscle activity assessment in a sitting position, and can even utilize computerized-biofeedback, with the patient's hip and knees at different heights can help determine the best position for muscle relaxation during defecation. At times, it can also be useful to incorporate abdominal massage in resolving a patient's constipation. Abdominal massage for bowel function is useful in motivating peristalsis in the gut, plus there are no known side effects. This is a safe and non-invasive way to manage constipation and can be taught to the patient for them to perform on their own as needed.
In the Bowel Pathology, Function, & Dysfunction Remote Course Lila focuses on teaching registrants about the details of normal gut motility, bowel function, medical tests, and medications relating to diagnosing and treating the medical side of bowel dysfunction. Some of the highlighted lectures are about fecal incontinence, chronic constipation, and abdominal pain and how they relate to pelvic floor muscle dysfunction and physical therapy interventions.
Also commonly encountered in pelvic rehabilitation practices are patients with coccyx pain. You may not think of constipation when treating coccydynia. However, defecation is one of the functional complaints that can be present. The coccyx can interfere with defecation as documented in a case study by Salar et al. They reported that the patient presented with an anteverted coccyx, and complained of "worsening rectal pain developing an hour before defecation and lasting for several hours afterward.” (2)
Lila Abbate also instructs the Coccydynia and Painful Sitting Remote Course. This course is a 1-day deep dive into treating patients who complain of coccyx pain with sitting and defecation. Lila shares that "The coccyx course is orthopedically-based and. I take my love of manual, osteopathic treatment, and combine it with the women’s health internal treatment aspects so that we can move more quickly to get patients back on the path to improved function and recovery."
When asked about the approach she took in creating the course, Lila explains, "this course looks at patients from a holistic approach from the top of their heads down to their feet. In taking on the topic of coccydynia, I focused on honing basic observation skills and using some of my favorite tools in my toolbox. These include the Hesch Method, integrated systems model, traditional osteopathic, and mobilization approaches mixed with internal vaginal and rectal muscle treatment skill sets."
Join faculty member Lila Abbate this November at her upcoming course Bowel Pathology, Function, & Dysfunction scheduled for November 13-14, 2021, or plan ahead and register for the Coccydynia and Painful Sitting Remote Course scheduled for February 4, 2022.
- Forootan, M; Bagheri, N; Darvishi, M. Chronic Constipation: A review of the literature. Medicine (Baltimore) 2018: May. PMID: 29768326 PMCID: PMC5976340 doi:10.1097/MD.0000000000010631
- Salar et al.: Defecation pain and coccydynia due to an anteverted coccyx: a case report. Journal of Medical Case Reports 2012 6:175. doi:10.1186/1752-1947-6-175

Rachna Mehta, PT, DPT, CIMT, OCS, PRPC is the author and instructor of the new Acupressure for Pelvic Health course. Rachna brings a wealth of experience to her physical therapy practice and has a personal interest in various eastern holistic healing traditions. Her course Acupressure for Optimal Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional, and energy body.
Constipation is a common functional gastrointestinal disorder, with prevalence in the general population of approximately 20%. In the elderly population, the incidence of constipation is higher compared to the younger population, with elderly females suffering more often from severe constipation (1).
Is there a magic button in the perineum that makes it easier to defecate? In case you have wondered, the answer is YES!!!
A study done recently by Dr. Ryan Abbott and colleagues at UCLA’s Department of Medicine found just that. A randomized control trial was conducted with 100 subjects who had functional constipation, half randomized to treatment and half to the control group. The treatment group received training in self perineal acupressure along with standard treatment options. The control group only received information about standard constipation treatment options.
Perineal self-acupressure technique was found to be remarkably effective with statistically significant and clinically meaningful improvements in Patient Assessments of Constipation Quality of Life (PAC-QOL All), modified Bowel Function Index (BFI), and the Short-Form Health Survey (SF-12v2). Patients in the treatment group also reported substantial satisfaction with perineal self-acupressure technique:
- 72% of the treatment group reported that the perineal pressure technique helped them to “break up, soften, or pass stools."
- 54% reported that the technique helped them to “avoid having hemorrhoid or lessened the impact of existing hemorrhoid."
- 72% reported that the technique helped them to “avoid or better manage the effects of constipation."
- 82% of the treatment group patients indicated that they would continue to use the technique, and 72% indicated that they would recommend the technique to family and friends (2).
In this study, perineal acupressure was applied at the Acupressure point Huiyin or CV 1 located at the perineum. Huiyin is used in Traditional Chinese Medicine (TCM) not only to treat constipation, but also a variety of conditions including impotence, hemorrhoids, rectal prolapse, and dysmenorrhea. In addition, there are several key Acu-points like St 36 on the Stomach meridian and CV 6 which can help with constipation and digestive disorders.
Acupressure is based on Traditional Chinese meridian theory in which acupuncture points are pressed to stimulate the flow of energy or Qi and these points reflect disorders of visceral conditions and organs.
Acupuncture meridians are believed to form a network throughout the body, connecting peripheral tissues to each other and to the central viscera. This tissue network is also continuous with more specialized connective tissues such as periosteum, perimysium, perineurium, pleura, peritoneum, and meninges (3).
Dr. Abbott’s study suggests that clinicians should consider incorporating perineal self-acupressure technique as a first-line treatment for constipation, along with conventional interventions such as increased exercise and dietary fiber intake. Benefits include being non-invasive and non-pharmacological treatment intervention for constipation with likely a lower risk for side effects and complications than commonly used medications such as stool softeners, fiber supplements, stimulants, laxatives, and lubricants (2).
As medical providers, we are uniquely trained to combine our orthopedic skills with mindfulness-based holistic interventions to empower our patients by giving them the tools and self-care regimens to live healthier pain-free lives.
The upcoming remote course Acupressure for Optimal Pelvic Health, scheduled for July 24-25, 2021, brings a unique evidence-based approach on the use of potent Acupressure points for treating a wide variety of pelvic health conditions including chronic pelvic pain, dysmenorrhea, constipation, digestive disturbances and urinary dysfunctions to name a few.
The course also offers an introduction to Yin yoga and explores Yin poses within each meridian to channelize energy through neurodynamic pathways with powerful integrative applications across multiple systems.
References
- Vazquez Roque M, Bouras EP. Epidemiology and management of chronic constipation in elderly patients. Clin Interv Aging. 2015;10:919-930.
- Abbott R, Ayres I, Hui E, Hui KK. Effect of perineal self-acupressure on constipation: a randomized controlled trial. J Gen Intern Med. 2015;30(4):434-439.
- Kaptchuk TJ. 2000. The web that has no weaver. Understanding Chinese medicine. Chicago: Contemporary Publishing Group, Inc.
5. Lee EJ, Frazier SK. The efficacy of acupressure for symptom management: a systematic review. J Pain Symptom Manage. 2011;42(4):589-603.

Erica Vitek, MOT, OTR, BCB-PMD, PRPC has attended extensive post-graduate rehabilitation education in the area of Parkinson disease and exercise. She is certified in LSVT (Lee Silverman Voice Treatment) BIG and is a trained PWR! (Parkinson Wellness Recovery) provider, both focusing on intensive, amplitude, and neuroplasticity-based exercise programs for people with Parkinson disease. Erica has taken a special interest in the unique pelvic floor, bladder, bowel, and sexual health issues experienced by individuals diagnosed with Parkinson disease. You can learn more about this topic in Erica's course, Parkinson Disease and Pelvic Rehabilitation, scheduled for July 23-24, 2021.
Parkinson disease (PD) non-motor symptoms can be even more impactful on quality of life than the cardinal motor symptoms most are familiar with, bradykinesia, rigidity, tremor, and postural instability. The list of non-motor symptoms is extensive affecting many body systems including cognitive, sensory, and autonomic.
Constipation is one of the most common autonomic non-motor symptoms experienced by people with Parkinson disease with studies showing 20-89% prevalence (1). As the disease progresses, individuals are more likely to experience symptoms that suggest a strong relationship between neurodegeneration and bowel dysfunction, such as, decreased frequency of bowel movements, difficulty expelling stool, and diarrhea (2). Constipation has also been hypothesized to be an early indicator for the development of Parkinson disease, and there is ongoing research in this area. It has yet to be shown that constipation is specific enough to predict the development of PD.
Developing an understanding of Parkinson disease constipation and how it differs from other individuals with constipation can have a strong impact on our recommended pelvic rehabilitation plans of care. In a study published by Zhang, M. et al., 2021, they looked at the characteristics of Parkinson disease with constipation (PDC) compared to functional constipation (FC). Functional constipation is generally defined as difficult, infrequent, or incomplete defecations (3). One of the main findings in this study was a significant difference between the groups when looking at resting rectal and anal canal pressures. In the PDC group, resting rectal and anal pressures were significantly lower. These resting pressures are mainly controlled by the internal anal sphincter resting tension which is supported by the autonomic nervous system. This leads the researchers to speculate there may be autonomic nervous system neuropathy in people with PD
They then looked at simulated defecation, which also showed that the PDC group had significantly lower rectal defecation pressure and a lower anal relaxation rate. Since rectal pressures during defecation assist in effective anal relaxation, the researchers state, “a coordinated movement disorder results” and that people with PD may have “pelvic floor cooperative motion disorder” (1). Additionally, the researchers noted that abnormal abdominal pressure is another main contributing factor to the low rectal defecatory pressure in PDC. Abdominal pressure is a key factor in driving complete and efficient rectal defecation. This is also a finding in numerous other studies in the literature unique in PDC.
The results of Zhang, M. et al., 2021 reveal the need for pelvic health practitioners to help train coordinated defecation efforts in people with Parkinson disease. In my course, Parkinson disease and Pelvic Rehab, we will have an in-depth discussion about how training defecatory dynamics is different in people with PD. Muscle training principles in this population are very unique. Understanding the underlying causal factors of dysfunction will have a significant impact when helping patients with Parkinson disease manage constipation.
- Zhang, M., Yang, S., Li, X. C., Zhu, H. M., Peng, D., Li, B. Y., ... & Tian, C. (2021). Study on the characteristics of intestinal motility of constipation in patients with Parkinson's disease. World Journal of Gastroenterology, 27(11), 1055.
- Sakakibara, R. (2021). Gastrointestinal dysfunction in movement disorders. Neurological Sciences, 1-11.
- Lacy, B. E., Mearin, F., Chang, L., Chey, W. D., Lembo, A. J., Simren, M., & Spiller, R. (2016). Bowel disorders.Gastroenterology 150 (6), 1393-1407.
For over 25 years my practice has had a focus on children suffering from bloating, gas, abdominal pain, fecal incontinence and constipation. Functional Gastrointestinal Disorders (FGID) are disorders of the brain -gut interaction causing motility disturbance, visceral hypersensitivity, altered immune function, gut microbiota and CNS processing. (Hyams et al 2016). Did you know that children who experience chronic constipation that do not get treated have a 50% chance of having issues for life?
 The entire GI system is as amazing as it is and complicated. Its connection to the nervous system is fascinating, making it a very sensitive system. In her book GUT, Giulia Enders talks about Ninety percent of the serotonin we need comes from our gut! The psychological ramifications of ignoring the problem are too great (Chase et el 2018). Last year an 18-year-old patient of mine had to decline a scholarship to an Ivy League University because she needed to live at home due to her bowel management problem.
The entire GI system is as amazing as it is and complicated. Its connection to the nervous system is fascinating, making it a very sensitive system. In her book GUT, Giulia Enders talks about Ninety percent of the serotonin we need comes from our gut! The psychological ramifications of ignoring the problem are too great (Chase et el 2018). Last year an 18-year-old patient of mine had to decline a scholarship to an Ivy League University because she needed to live at home due to her bowel management problem.
Unfortunately, FGID conditions can lead to suicide and death. Over 15 years ago my children’s pediatrician told me about an 11-year-old boy who hung himself because he had encopresis. In 2016 a 16-year-old girl suffered a cardiac arrest and died because of constipation.
The problems with children are different than for adults and need to be addressed with a unique approach.
How do physical therapists treat pediatric FGID?
- Have a solid foundation in the gastrointestinal system
- Coordinate muscle functions from top to bottom!
- Identify common childhood patterns
- Learn treatment techniques and strategies to address the issues specifically
Study and understand gastrointestinal anatomy, physiology, function and examination techniques. The entire GI system is as amazing as it is complicated. Its connection to the nervous system is fascinating, making it a very sensitive system. Ninety percent of the serotonin we need comes from our gut! The psychological ramifications of ignoring the problem are too great.
What do the Pelvic Floor Muscles (PFM) have to do with it?
Encopresis leads to a weak internal/external anal sphincter and pelvic floor muscles and constipation leads to pelvic floor muscles that can’t relax. Confused? When the Rectal Anal Inhibitory Reflex or RAIR fails from bypass diarrhea the sphincter muscles relax, and feces leaks out. This constant leakage leads to weak sphincter and pelvic floor muscles. When it happens on a regular basis most children don’t feel it, however their peers smell it and life changes.
My course, Pediatric Functional Gastrointestinal Disorders, teaches how to coordinate the muscle function based on the tasks required.
How did this start?
One painful bowel movement can lead to withholding for the next due to fear of the pain happening again. The muscles of the pelvic floor then tighten to hold the poop in. This actually does not make the muscle strong but instead makes it confused. The muscle then is controlled by the consistency of poop being too hard and painful to let out or too loose and not able to hold in.
Managing functional GI disorders is a process. It takes the bowel a long time to re-train and it requires patience and skill to know how to do it. Many therapists and patients themselves get frustrated and compliance fails. This is mostly due to lack of knowing how to titrate medications and give the bowel what it needs (other than proper nutrition that is!) It's like retraining a person to walk after a stroke, the brain needs to relearn normal bowel sensations.
Most families don’t realize how severe constipation can be. It is an insidious problem that gets ignored until it is too late.
Typically, what I hear from parents is their child was diagnosed with constipation and was advised to take a daily laxative. So, which one is the best one? How do they all work? Once leakage occurs again the laxative is discontinued as we think the bowel must be empty and this medication is causing the leaks which is counterproductive. Now the frustrating cycle of backing up or being constipated begins again. The constipation returns, the laxative is restarted, the loose stool leaks out and the laxative is stopped and that is the REVOLVING DOOR or what I refer to as children riding the “Constipation Carousel”. The bowel is an amazingly beautiful, smart but also sensitive organ that does not like this back and forth and therefore will not learn how to be normal. In the meantime, they experience distended abdomens and dysmorphia ending up in eating disorder clinics. I had an 11-year-old girl taking Amitriptyline for abdominal pain all because of a pressure problem in the gut not knowing how to work the pelvic floor with the diaphragm and her core.
No two children are the same and no two colons are the same. Laxatives need to be titrated to the specific needs of your child’s colon and motility of their colon not their age or body weight.
The success in getting children to have regular bowel movements of normal consistency without any fecal leaks is based not only teaching how to titrate laxatives but also how to sense urge, become aware of the pelvic floor muscles and learn how NOT to strain to defecate, retrain the core and diaphragm with the ribcage and integrate developmental strategies for function. Teaching Interoception- what my body feels like when I have an urge- is an important part of this course. This is especially important for those children born with anorectal malformations or congenital problems such as imperforate anus or Hirschsprung’s Disease.
In this class we use visceral techniques, manual therapy techniques, sensory techniques and neuromuscular reeducation and coordination to retrain the entire system.
Come and explore the amazing gut with me and learn how to improve the health and well-being of your patients, in Pediatric Functional Gastrointestinal Disorders!
1. Hyams, JS, et al. Childhood Functional Gastrointestinal Disorders: Child/Adolescent. Gastroenterology volume 150, 2016;1456-1468.
2. Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features and rome IV. Gastroenterology 2016;150:1262-1279
3. Robin SG, Keller C, Zwiener R, et al. Prevalence of Pediatric Functional Gastrointestinal Disorders Utilizing the Rome IV Criteria. J Pediatr 2018; 195:134.
4. Koppen IJN, Vriesman MH, Saps M, Rajindrajith S, Shi X, van Etten-Jamaludin FS, Di Lorenzo C, Benninga MA, Tabbers MM. Prevalence of Functional Defecation Disorders in Children: A Systematic Review and Meta-Analysis. J Pediatr. 2018 Jul;198:121-130.e6. doi: 10.1016/j.jpeds.2018.02.029. Epub 2018 Apr 12.
5. Zar-Kessler C, Kuo B, Cole E, Benedix A, Belkind-Gerson, J. Benefit of pelvic floor physical therapy in pediatric patients with dyssynergic defecation constipation. 2019 Dig Dis https://doi.org/10.1159/000500121/
6. Chase J, Bower W, Susan Gibb S. et al. Diagnostic scores, questionnaires, quality of life, and outcome measures in pediatric continence: A review of available tools from the International Children’s Continence Society. J Ped Urol (2018) 14, 98e107
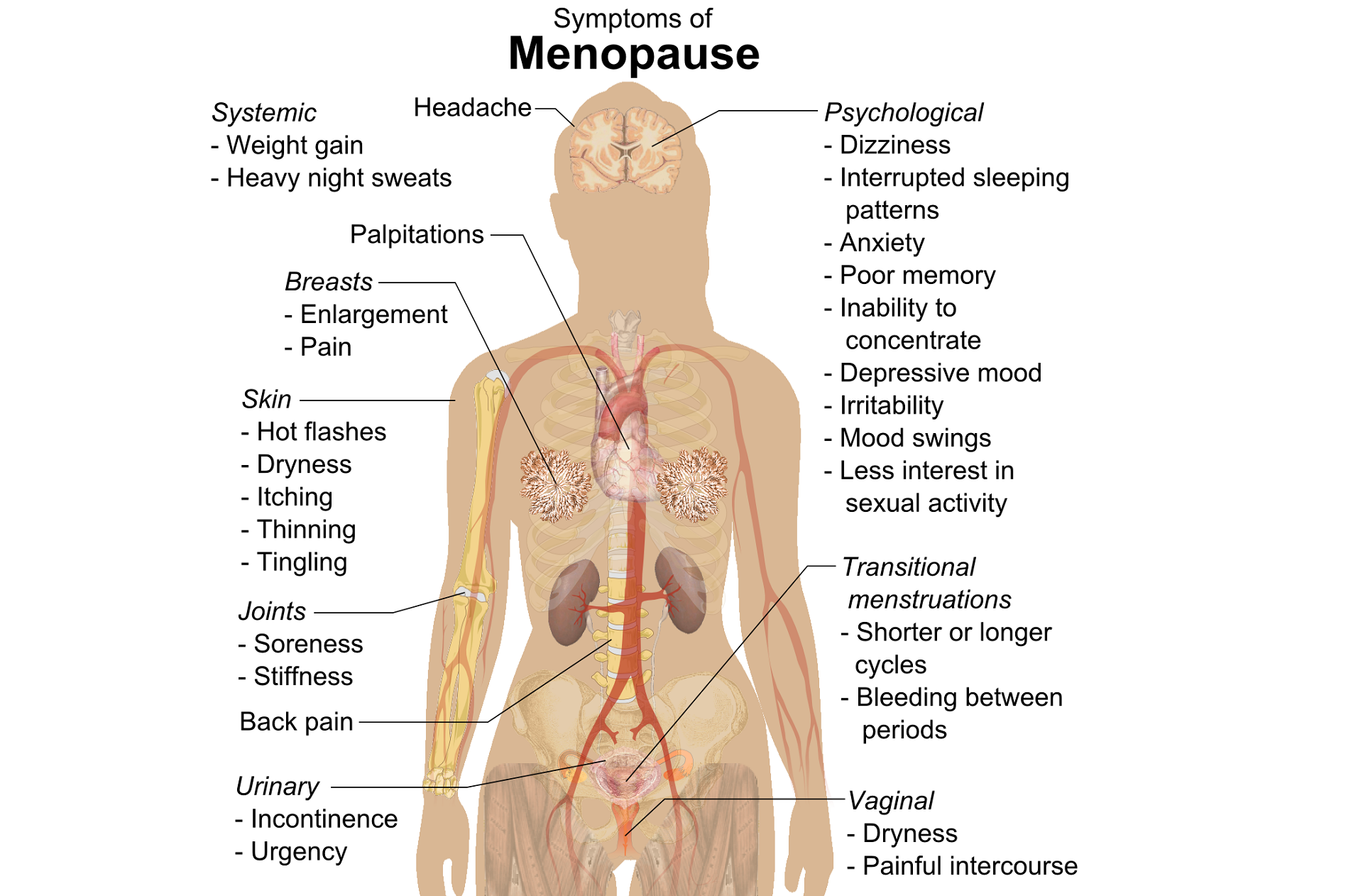
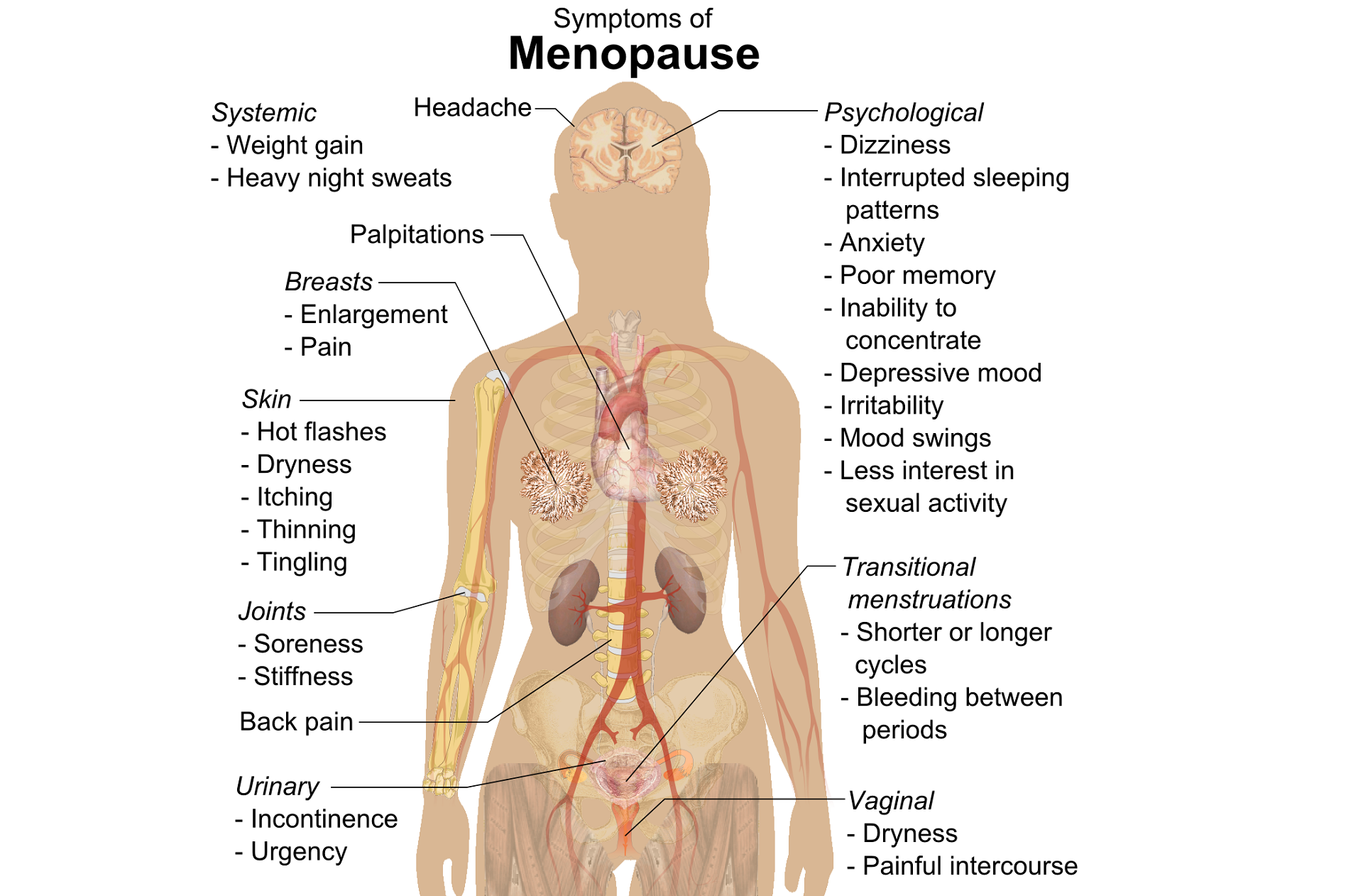
Perimenopausal pelvic health issues are, for many of us, some of the most common issues that we see in the women that we work with. Urinary incontinence is one of the most important issues for peri- and postmenopausal women. In Melville’s study1 of U.S. women, half of the participants between the ages of 50 and 90 experienced urine leakage every month. Zhu’s 2008 study2 looked at the risk factors for SUI - Multiple vaginal deliveries, Age/postmenopausal status, Chronic pelvic pain, Obesity, lack of exercise, constipation, and hypertension. But what is not often (enough) looked at in the research, is the link between urinary dysfunction and sexual dysfunction – usually because questions aren’t asked or assumptions are made. In Mestre et al’s 2015 paper3, they write ‘…Integrating sexual health in clinical practice is important. In women with pelvic floor disorders, the evaluation of the anatomical defects, lower urinary tract function and the anorectal function often receives more attention than sexual function.’
 But are they linked?
But are they linked?
In Moller’s exploration of this topic, they report that lower urinary tract symptoms (LUTS) have a profound impact on women’s physical, social, and sexual wellbeing. Unsurprisingly (to pelvic rehab specialists at least!), they found that the LUTS are likely to affect sexual activity. Conversely, sexual activity may affect the occurrence of LUTS. The aims of the Moller study were to elucidate to which extent LUTS affect sexual function and to which extent sexual function affect LUTS in an unselected population of middle-aged women in 1 year. A questionnaire was sent to 4,000 unselected women aged 40–60 years. Compared to women having sexual relationship, a statistically significant 3 to 6 fold higher prevalence of LUTS was observed in women with no sexual relationship. In women who ceased sexual relationship an increase in the de novo occurrence of most LUTS was observed. In women who resumed sexual relationship a decrease in LUTS was observed. In women whose sexual activity was unchanged no change in the occurrence of LUTS. So they rightfully concluded ‘…sexual inactivity may lead to LUTS and vice versa.’
In my Menopause course, we will explore the range of perimenopausal pelvic health issues that many women face and their inter-related nature – not just with each other but also how orthopaedic, endocrine and gastro-intestinal health issues influence pelvic health and wellness. Interested in learning more? Come and join the conversation in California in February 2018!
1. Melville JL, et al. Urinary incontinence in US women: a population-based study. Arch Intern Med 2005;165(5):537-42 - See more at: http://www.nursingcenter.com/lnc/JournalArticle?Article_ID=698029#sthash.cm8A90tS.dpuf
2. Zhu L1, Lang J, Wang H, Han S, Huang J. Menopause. 2008 May-Jun;15(3):566-9. The prevalence of and potential risk factors for female urinary incontinence in Beijing, China
3. Mestre M, Lleberia J, Pubill J, Espuña-Pons M Actas Urol Esp. 2015 Apr;39(3):175-82. Epub 2014 Aug 28. Questionnaires in the assessment of sexual function in women with urinary incontinence and pelvic organ prolapse.
One of my dear patients was recently diagnosed with Ehlers-Danlos sydrome (EDS). The diagnosis brought a sense of relief for sweet Katie who for years struggled with numerous health problems and was often misunderstood and under cared for by the medical community. Katie was referred to me 2 years ago at 28 for pelvic pain, endometriosis and IC. Upon exam we also discovered a significant elimination disorder and paradoxical elimination. Katie regularly timed her elimination and was spending at times up to 2 hours trying to empty her bowels. As we worked together we uncovered bilateral hip dysplasia, left hip labral tear, ilioinguinal and pudendal neruralgia and POTS (Postural Orthostatic Hypotension Syndrome). Katie already had a history of anxiety and depression but managed well with good family and friend support. When the diagnosis of EDS came, she finally felt like she had an explanation for why her body is like it is. This brought great relief as well as the knowledge that her condition was genetic and her conditions needed to be managed as best as possible to give her the most function, but would likely never be fully resolved.
 In her book "A Guide to Living with Ehler's Danlos Syndrome" Isobel Knight does a beautiful job outlining the various genetic subtypes of Ehlers Danlos but also highlighting the fact that EDS hypermobility type (Type III) does not just affect the connective tissue in the musculoskeletal sytem leading to joint instability and hypermoblity, muscle tears, dislocations, subluxations, hip dysplasia and flat feet. EDS can also affect the body's systemic collagen leading to increased risk for endometriosis, POTS, Renauds, bladder problems, fibromyalgia, headaches, restless legs, ashtma, consitpation, bloatedness, prolapse, IBS symptoms, anxiety, depression and learning difficulties. She notes that some people have only a few of these systemic symptoms while others may be more affected. Per Isobel: "it is important that all symptoms are treated seriously and not ridiculed and that the appropriate medical support is given to them when necessary."
In her book "A Guide to Living with Ehler's Danlos Syndrome" Isobel Knight does a beautiful job outlining the various genetic subtypes of Ehlers Danlos but also highlighting the fact that EDS hypermobility type (Type III) does not just affect the connective tissue in the musculoskeletal sytem leading to joint instability and hypermoblity, muscle tears, dislocations, subluxations, hip dysplasia and flat feet. EDS can also affect the body's systemic collagen leading to increased risk for endometriosis, POTS, Renauds, bladder problems, fibromyalgia, headaches, restless legs, ashtma, consitpation, bloatedness, prolapse, IBS symptoms, anxiety, depression and learning difficulties. She notes that some people have only a few of these systemic symptoms while others may be more affected. Per Isobel: "it is important that all symptoms are treated seriously and not ridiculed and that the appropriate medical support is given to them when necessary."
It seems that EDS is becoming more widely recognized. As rehabilitation specialists we should be alert to problems stemming from joint hypermobility when we notice how our patients position themselves. Often legs are curled up or double crossed. Upon questioning we might find that the patient has a history of being "double jointed" or was able to do "party tricks" with their bodies. The Bighton scale is a test of joint hypermobility which we should all be familiar with. It is also important to note that a patient may have hypermobility without having EDS, and that EDS is usually associated with pain. A rheumatologist, or in Katie's case a geneticist, can help confirm a suspected EDS diagnosis.
If you have a patient with hypermobliiy or with EDS, know that their ability to know where their body is in space is limited as their joints have much more range of motion than normal. The proprioceptors do not fire well at mid range and the patient will have to be trained to become accustomed to neutral joint positions. This was really painful for Katie and it took a huge mental and physical effort. She is getting stronger now and it is becoming easier to achieve. Stretching and soft tissue massage can feel really good when your muscles have to work so hard to maintain your joints in healthy positions. Patients should be instructed to not stretch into end range and also not "hang out" on their ligaments. Some patients may have to begin just with isometrics. I used Sara Meeks' program for safe and effective floor exercise with Katie. The floor gave her support while she strengthened her core muscles. Then she was able to progress to seated and seated on a ball as well as standing exercises. She loves the body blade! Yoga, Pilates, exercise in water can be effective for strength, propriception and movement reeducation. Mirrors are helpful for increasing position sense.
It is also helpful to note that even patients with EDS may be hypermobile in some joints and hypomobile in others. Isobel reports that her SI joints were extremely unstable while her thoracic spine was very rigid to the point that her lung capacity was affected. Having her therapist work on the hypomobility and doing breath work was life changing.
As pelvic health therapists and rehabilitation providers we may be the first professional to suspect EDS in a patient. There is a great deal that we and the greater medical and holistic community can do to help patients with EDS lead lives with less pain and dysfunction.