As musculoskeletal specialists, we are adept at identifying postural dysfunction. I often explain to patients how their ribcage might shift posteriorly relative to the plumb line and how gravity can amplify forces on specific structures. To help patients understand the difference between their habitual non-optimal posture and a more optimally aligned posture, many occupational and physical therapists use the IPA’s Vertical Compression Test (VCT). This test effectively demonstrates how improved alignment facilitates better weight transfer through the base of support. Sometimes this test reproduces back or pelvic pain which allows the patient to understand how their posture might be a contributing factor to them not feeling their best. In addition to the VCT, I incorporate Mountain Pose as an additional kinesthetic tool for postural retraining.
 Many moons ago, I was working with a lovely client on embodied postural awareness using Mountain Pose. I suggested she could close her eyes if she felt comfortable (some people will feel safer lowering their gaze instead of closing their eyes). Working from the ground up, she realized her weight was predominantly in her heels. When I guided her to shift her weight forward by hinging from the talocrural joint, she experienced an “aha moment,” saying, “It feels like my pelvic floor just sighed.” She hadn’t been aware that her habitual posture involved standing with her weight behind the plumb line, which contributed to overactivity of the posterior pelvic floor. Once she adjusted her base of support from the ground up, she felt a significant release in her habitual tension.
Many moons ago, I was working with a lovely client on embodied postural awareness using Mountain Pose. I suggested she could close her eyes if she felt comfortable (some people will feel safer lowering their gaze instead of closing their eyes). Working from the ground up, she realized her weight was predominantly in her heels. When I guided her to shift her weight forward by hinging from the talocrural joint, she experienced an “aha moment,” saying, “It feels like my pelvic floor just sighed.” She hadn’t been aware that her habitual posture involved standing with her weight behind the plumb line, which contributed to overactivity of the posterior pelvic floor. Once she adjusted her base of support from the ground up, she felt a significant release in her habitual tension.
At our follow-up visit, the client noted an increase in her postural awareness. She was surprised by how frequently she noticed her pelvic floor gripping in a state of overactivity. She also reported enhanced awareness during her standing yoga postures in class. Grounding down through the feet, cued as imagining the soles of the feet getting magnetically drawn into the floor, can be a useful verbal cue to assist with letting go of unnecessary gripping. The experience of achieving embodied optimal alignment has given her greater self-efficacy, and she’s successfully translated this improved postural awareness into her daily life. Self-awareness and empowerment are central goals in my physical therapy practice, and integrating yoga into this process makes my clinical work even more fulfilling.
To learn more, join Dustienne in her remote course Yoga for Pelvic Pain this September 14-15! This course discusses a variety of pelvic conditions including interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia. Dustienne also describes the role of yoga within the medical model, contraindicated postures, and how to incorporate yoga home programs as therapeutic exercise and neuromuscular re-education both between visits and after discharge in this course.
Author Bio:
Dustienne Miller PT, MS, WCS, CYT

Dustienne Miller is the creator of the two-day course Yoga for Pelvic Pain and an instructor for Pelvic Function Level 1. Born out of an interest in creating yoga home programs for her patients, she developed a pelvic health yoga video series called Your Pace Yoga in 2012. She is a contributing author in two books about the integration of pelvic health and yoga, Yoga Mama: The Practitioner’s Guide to Prenatal Yoga (Shambhala Publications, 2016) and Healing in Urology (World Scientific). Prior conference and workshop engagements include APTA's CSM, International Pelvic Pain Society, Woman on Fire, Wound Ostomy and Continence Society, and the American Academy of Physical Medicine and Rehabilitation Annual Assembly.
Her clinical practice, Flourish Physical Therapy, is located in Boston's Back Bay. She is a board-certified women's health clinical specialist recognized by the American Board of Physical Therapy Specialties. Dustienne weaves yoga, mindfulness, and breathwork into her clinical practice, having received her yoga teacher certification through the Kripalu Center for Yoga and Health in 2005.
Dustienne's love of movement carried over into her physical therapy and yoga practice, stemming from her previous career as a professional dancer. She danced professionally in New York City for several years, most notably with the national tour of Fosse. She bridged her dance and physical therapy backgrounds working for Physioarts, who contracted her to work backstage at various Broadway shows and for Radio City Christmas Spectacular. She is an assistant professor of musical theater and jazz dance at the Boston Conservatory at Berklee.
Dustienne passionately believes in the integration of physical therapy and yoga within a holistic model of care. Her course aims to provide therapists and patients with an additional resource centered on supporting the nervous system and enhancing patient self-efficacy.
Trauma. The word holds so many meanings. Say the word and depending on your perspective - it could mean Trauma (like trauma center which is physical injury focused) or trauma (like unwanted experience causing adverse socioemotional consequences). In medical environments, the former would be qualified as ‘Big T’ Trauma, and the latter would be ‘little t’ trauma. Once you are immersed in the ‘little t’ trauma field, the Big and little traumas change meanings. The Big T Trauma would describe a significant event, whereas the little t trauma would include multiple, smaller microaggressions accumulating into adverse effects.
I have worked in trauma since 1996. And the changes have been vast. Thankfully, long gone are the days that I am educating physicians in the ER on how to complete a rape kit and how to perform care that is patient-focused and empowering. I would like to think that advocates are no longer having to explain to medical providers that RU22 is not an ‘abortion pill’ but a medicine that is required to be offered BY LAW in Illinois (SASETA) to reduce the risk of implantation after a rape. I started working in ERs advocating for the medical and legal rights of sexual assault survivors BEFORE Law-and-Order SVU brought these patients into mainstream culture in 1999. Thank you, Olivia and Elliot for bringing this awareness into our living rooms.
When I was a mental health counselor in the 90s and 2000s, it was quite remarkable that trauma was not included in mental health services. PTSD definitions were changing frequently within the DSM (Diagnostic Statistical Manual) during this time. Definitions and inclusion of trauma within mental health continue to change frequently to this day. In the 90s, I was working with youth in lower socioeconomic populations and their trauma was both palpable and unseen. Also, during this time, education and awareness of developmentally appropriate sexual health were not a thing! I remember my supervisor calling me and asking me what to do with a teenage female who was masturbating with a brush. And I was like OK - which side of the brush… is she masturbating for pleasure which is normal/appropriate or is she hurting herself and we need to screen her for sexual abuse? I screened her for abuse (my supervisor was not comfortable- she ended up disclosing her own abuse) and the teenager did not disclose abuse or self-harming behaviors, so it was normal sexual behavior. I could go on about cultural and gender taboos, but that is literally power for the course.
When I made the change from mental health to physical therapy in the mid-late 2000s it soon became apparent that trauma was not considered within rehabilitation. In 2011, I created the first in-service on trauma - focusing on education, awareness, and teaching Polyvagal theory. Stephen Porges introduced Polyvagal much earlier in 1994 and I am looking forward to the day he receives the Nobel Prize for his work, as he should. I am ecstatic that Polyvagal is no longer an obscure construct. I see many friends and fellow clinicians normalizing the terms neuroception and interoception, and I am elated. This is quite different from when ten ten-plus years ago, the response to my course was a not-so-friendly ‘Stay in your lane, PT’ (and this is not addressing the fact that our fellow OT and SLP comrades are doing this challenging work). I am so glad that is not the case anymore. Trauma-informed care (TIC) is becoming the norm, not the exception. And I am so happy to see what other rehabilitation specialists are doing within the field! There is so much space for us all.
Here is an outline of what we expand upon within the course Trauma Awareness for the Pelvic Therapist:
Trauma-informed care (TIC) is a universal approach within healthcare that recognizes and responds to the impact of traumatic experiences on individuals. It aims to create a supportive environment that promotes healing and recovery while minimizing the risk of re-traumatization. The core principles of trauma-informed care include understanding the prevalence and effects of trauma, recognizing the signs and symptoms of trauma in patients and staff, and integrating knowledge about trauma into practices, policies, and procedures. In order to understand the effects of trauma, an understanding of neurobiology of the brain and function of the autonomic nervous system are foundational.
Key Principles of Trauma-Informed Care:
Safety:
Ensuring physical and emotional safety for the CLINICIAN, clients, and staff. This involves creating an environment where individuals feel secure and respected.
Trustworthiness and Transparency:
Building trust through clear, consistent, and transparent practices. Ensuring that decision-making processes are transparent, and that information is shared openly.
Peer Support:
Encouraging and incorporating peer support and mutual self-help as essential components of trauma-informed care. Peer support helps to build trust, enhance collaboration, and promote recovery.
Collaboration and Mutuality:
Emphasizing partnership and the leveling of power differences between staff and clients. Everyone involved in the care process collaborates and shares in the decision-making.
Empowerment, Voice, and Choice:
Prioritizing the empowerment of individuals and recognizing their strengths. Offering choices and supporting individuals in their decisions helps to foster autonomy and resilience.
Cultural, Historical, and Gender Issues:
Being responsive to cultural, historical, and gender contexts. This involves recognizing and addressing the impact of systemic oppression and discrimination and promoting cultural competence among staff.
Implementation Strategies
Training and Education:
Providing ongoing training for EVERYONE on the principles of trauma-informed care and the impact of trauma. This includes recognizing trauma responses and learning how to create a supportive environment.
Policy and Procedure Review:
Introducing TIC and revising organizational policies and procedures to ensure they reflect trauma-informed principles. This includes practices related to intake, assessment, treatment planning, and discharge.
Environment Modification:
Creating physical spaces that promote a sense of safety and calm. This can involve changes to the layout, lighting, noise levels, and decor.
Client/Patient Involvement:
Involving clients in the planning and evaluation of services to ensure their perspectives and needs are considered.
Support Systems:
Providing support for EVERYONE to prevent burnout and secondary traumatic stress. This can include supervision, debriefing sessions, and access to mental health resources.
Trauma is personal and individualized. There is no one size fits all or one technique can be used for all.
Benefits of Trauma-Informed Care:
Improved Outcomes:
Trauma-informed care can lead to better engagement, adherence to treatment, and overall outcomes for clients/patients.
Reduced Re-traumatization:
By creating a supportive and understanding environment, the risk of re-traumatizing individuals (read: ALL of us) is minimized.
Enhanced Trust:
Building trust between clients/patients and providers fosters better communication and a stronger therapeutic relationship.
Empowerment and Recovery:
Empowering individuals to take an active role in their care promotes recovery and resilience.
Remember, trauma-informed care is a comprehensive approach that involves understanding, recognizing, and responding to the effects of trauma. By integrating trauma-informed principles into practice as UNIVERSAL PRECAUTIONS, we can create safer, more supportive environments that promote healing and recovery for ourselves and all individuals.
It has been an honor to bring this course, Trauma Awareness for the Pelvic Therapist, into the rehabilitation space. In the last 10 years, and especially since COVID-19, it is beautiful to see how TIC has become mainstream. One word of caution: We need to watch out for end-of-spectrum gas lighting. We all have seen patients whose symptoms and experiences have been minimized when their trauma has not been taken into consideration. This can also happen at the other end of the spectrum. I had a patient who sought out gynecological treatment from a ‘trauma-focused gynecologist.’ This patient we all know - chronic pelvic pain with a history of endo, PCOS, IBS-M, and IC. When she went to this clinician, she was told that her pain was caused by trauma, whether she remembered the trauma or not. The patient is a counselor and has been doing much work with her mental health team. She was open to ‘unknown trauma’ but we both thought she should seek another provider. Two weeks later, she had surgery for appendicitis.
TIC allows us to refocus on our work within rehabilitation and is open and supportive towards all people. This work is AMAZING. This work is HARD. This work is quite frankly one of the reasons we were placed on this earth. To be present for another person’s pain, whatever type of pain that is - is one of the most special care one can give to another.
Please be so proud of all the work you have done. Know that you are enough. And that you can be present for others. I hope you find even more support and knowledge with any trauma course that you choose to take, I just hope to meet you in mine on September 21-22!
AUTHOR BIO:
Lauren Mansell DPT, CLT, PRPC
 Lauren received her Doctor of Physical Therapy degree from Governors State University and a Bachelor's Degree in Psychology and Sociology from Northwestern University. Before becoming a physical therapist, Lauren counseled suicidal and homicidal SES at-risk youth who had survived sexual violence. Lauren was certified as a medical and legal advocate for sexual assault survivors in 1999 and has advocated for over 130 sexual assault survivors of all ages in the ED. Lauren's physical therapy specialty certifications include Certified Lymphedema Therapist (CLT), Pelvic Rehabilitation Professional Certificate (PRPC), and Certified Yoga Therapist (CYT). She is a board member of the Chicagoland Pelvic Floor Research Consortium, American Physical Therapy Association Section of Women's Health and Section of Oncology.
Lauren received her Doctor of Physical Therapy degree from Governors State University and a Bachelor's Degree in Psychology and Sociology from Northwestern University. Before becoming a physical therapist, Lauren counseled suicidal and homicidal SES at-risk youth who had survived sexual violence. Lauren was certified as a medical and legal advocate for sexual assault survivors in 1999 and has advocated for over 130 sexual assault survivors of all ages in the ED. Lauren's physical therapy specialty certifications include Certified Lymphedema Therapist (CLT), Pelvic Rehabilitation Professional Certificate (PRPC), and Certified Yoga Therapist (CYT). She is a board member of the Chicagoland Pelvic Floor Research Consortium, American Physical Therapy Association Section of Women's Health and Section of Oncology.
As adjunct faculty, Lauren teaches Special Topics: Pelvic Rehabilitation Physical Therapy at Governors State University. Lauren works at the University of Chicago providing pelvic rehabilitation, lymphedema, and oncological physical therapy within Therapy Services and the Center of Supportive Oncology. She treats pelvic pain, urinary incontinence, bowel dysfunction, sexual dysfunction, lymphedema, lymph node transfer/bypass, stem cell transplant, and bowel/bladder/sexual/functional concerns of patients undergoing HIPEC (hyperthermal intraperitoneal chemotherapy). Lauren is a 2017 Fellow of the Chicago Trauma Collective. As a trauma-sensitive practitioner, her goal is to empower patients to create meaningful, healthful lifestyle changes to improve their physiology and wellness
More than Just Sticking It In! Getting Past Plateaus with Vaginal Trainers (Dilators) for Vaginismus

Lifelong vaginismus is a condition where a person experiences pain or difficulty with vaginal insertion from the first attempt. This could include the insertion of a tampon, gynecologic speculum, finger, penis, or sex toy. Many patients report, "I always had trouble with tampons" and may avoid using them altogether. They might also avoid pelvic exams and face significant challenges with receptive sexual activity.
Pelvic trainers, also known as dilators, vaginal trainers, or accommodators, can be effective tools for addressing lifelong vaginismus. However, as a pelvic health clinician, you may have noticed that some patients reach a plateau, getting "stuck" at a certain size trainer. Lifelong vaginismus is believed to be due to uncontrolled spasms of the pelvic floor muscles surrounding the vaginal opening. These spasms can hinder the insertion of progressively larger trainers and are not easily managed through passive stretching alone.
Instead, combining passive stretching with techniques like breathing and contract-relax exercises can be beneficial. Using muscle contractions may seem counterintuitive, but they can effectively promote muscle relaxation and control. Let's explore four scientific perspectives on how this works.
- Physiology of Skeletal Muscle
Skeletal muscle, which includes the pelvic floor muscles, responds to isometric contractions by activating Golgi Tendon Organs (GTOs) embedded in the muscle fibers. When GTOs are activated, they send signals to the spinal cord, triggering a reflex that inhibits the same muscle. Essentially, an isometric contraction causes the muscle to inhibit itself. This technique, known as "hold-relax" in Proprioceptive Neuromuscular Facilitation (PNF) stretching, may increase flexibility in the pelvic floor muscles when performed around the trainers.
- Neurological Effects
Repeated, sub-maximal contractions followed by gentle stretching and intentional relaxation can increase corticospinal excitability, promoting motor learning and performance (Christiansen et al., 2018). Over time, practicing voluntary contraction and relaxation, along with breathing exercises, helps patients gain more control over the muscles surrounding the vagina.
- Pain Science Perspective
Voluntary contractions activate the motor cortex in the brain, which has two effects on inhibiting pain (Lopes et al., 2019):
- Inhibition of the thalamic nuclei (lateral spinothalamic tract), limiting nociceptive messages.
- Activation of the periaqueductal gray, which contains enkephalin-producing cells that release endogenous opioids to suppress pain.
These effects reduce pain and facilitate the progressive insertion of vaginal trainers.
- Graded Exposure
Graded exposure involves gradually increasing exposure to an activity that causes fear or anxiety. Starting with the smallest size, trainers are inserted to the "just the start of discomfort" point (not to pain). This is followed by breathing exercises and gentle voluntary contractions and relaxations ("hold-relax" technique) along with passive stretching. As discomfort lessens, the trainer can be inserted further, repeating the steps. This process, over several sessions, allows progression to larger trainer sizes, reducing fear and anxiety while increasing functional insertion and decreasing pain.
Practical Application
During a session, a patient may insert a trainer just to the point of discomfort. The clinician can then guide them through the hold-relax routine:
- Take a breath in.
- Exhale and gently squeeze the pelvic floor muscles around the trainer – hold, hold, hold (through the full exhale).
- Release the muscles while inhaling again.
Repeat for 3-5 repetitions. After the last hold-relax, keep the muscles relaxed while gently pressing the trainer to stretch along the vaginal wall for 30-60 seconds, maintaining the same insertion depth. Repeat these steps for the posterior, left, and right vaginal walls (avoiding the anterior wall to prevent irritation of the urethra). These instructions can be adapted based on the individual patient.
In the Vaginismus and Vulvovaginal Dyspareunia course, participants learn and practice these steps, along with other techniques for addressing painful vaginal intercourse. The course covers selecting trainers, using lubricants, sexual positions, props and aids, perineal scar massage, and specific manual therapy treatments. It also provides guidance on discussing sexual activity with patients, including when to pause or continue, and how to involve partners. A rehabilitative treatment decision-making algorithm based on examination findings helps clinicians determine the most effective treatment combinations for each patient. Join us in the next Vaginismus and Vulvovaginal Dyspareunia course, scheduled for September 14, 2024.
For patients struggling with vaginal trainer progression, try these breathing, hold-relax, and gentle stretching techniques in your clinic this week. It may transform trainers from a frustrating obstacle into a useful and functional tool.
References:
Christiansen, L., Madsen, M. J., Bojsen-Møller, E., Thomas, R., Nielsen, J. B., & Lundbye-Jensen, J. (2018). Progressive practice promotes motor learning and repeated transient increases in corticospinal excitability across multiple days. Brain stimulation, 11(2), 346-357.
Lopes, P. S. S., Campos, A. C. P., Fonoff, E. T., Britto, L. R. G., & Pagano, R. L. (2019). Motor cortex and pain control: exploring the descending relay analgesic pathways and spinal nociceptive neurons in healthy conscious rats. Behavioral and Brain Functions, 15(1), 1-13.
AUTHOR BIO
Darla Cathcart, PT, DPT, PhD, WCS, CLT

Darla graduated from Louisiana State University (Shreveport, LA) with her physical therapy degree, performed residency training in Women’s Health PT at Duke University, and completed a Ph.D. at the University of Arkansas Medical Sciences. Her dissertation research focused on using non-invasive brain stimulation to augment behavioral interventions for women with lifelong vaginismus, and her ongoing line of research focuses on painful intercourse and post-Cesarean rehabilitation.
Darla’s certifications and training include Women’s Health Certified Specialist (WCS, board certification through the American Board of Physical Therapy Specialties). Certificate of Achievement in Pelvic Physical Therapy (CAPP-Pelvic). Certificate of Achievement in Pregnancy & Postpartum Physical Therapy (CAPP-OB). Certified Lymphedema Therapist (CLT).
Darla began her women’s health physical therapy career in her first job while working with pregnant women with musculoskeletal problems in a private outpatient therapy clinic in Shreveport, LA (with a focus on spine rehab). While there, she developed and hosted an exercise class for pregnant women. She would go on to develop a mom-and-baby postpartum exercise class while in her Duke residency in Durham, NC. She went on to develop the pelvic, pregnancy, and post-breast cancer/lymphedema PT program at Christus-Schumpert Health System in Shreveport, LA. During this time, she participated in educating women in the labor and birth preparatory classes hosted by the hospital; she also taught the women’s health course for physical therapy students at LSU-Shreveport. Darla went on to serve as a full-time faculty member in the physical therapy program at the University of Central Arkansas in Conway, AR, where she taught women’s health topics, documentation, therapeutic exercise, professional development, and human physiology. She recently owned a private PT practice that is dedicated to pelvic (bowel, bladder, and pelvic pain) and pregnancy/postpartum conditions in Conway, AR. Darla now is a full-time faculty member in the entry-level Physical Therapy program at Graceland University.
Darla currently serves as the President of the Academy of Pelvic Health of the American Physical Therapy Association. She has several peer-reviewed and non-peer-reviewed scientific publications. Amongst some of these, she co-authored “Clinical Summary: Urinary Incontinence” for PTNow.org in April 2015. She authored the chapter titled “The Female Hip and Pelvis” in Orthopedic Management of the Hip and Pelvis (S Cheatham, M Kolber, Elsevier, 2015). She chaired the committee for and participated heavily in the development of the Certificate of Achievement in Pregnancy/Postpartum (CAPP-OB) course series for the Section on Women’s Health of the American Physical Therapy Association. Darla has spoken and instructed many courses in local, national, and international settings on a variety of pelvic, pregnancy/postpartum, and other women’s health physical therapy topics. Darla has served as the Director of Education (2011-2014) and as Vice President (2015-2016) for the Section on Women’s Health, American Physical Therapy Association. She also served as a technical expert panel member on Treatments for Fecal Incontinence, Agency for Healthcare Research and Quality in 2014-2015. She also volunteered as a Women’s Health Certified Specialist Exam Standardization Task Force member in May 2013. Darla received several awards from the Section on Women’s Health: CAPP-OB Instructor of the Year (2017); Course Site Hostess of the Year (2018); and Volunteer of the Year (2015). She also received Clinical Instructor of the Year while serving as a clinical instructor a pelvic health physical therapy student from Elon University in 2011.

Do you feel you lack a firm understanding of how to comprehensively treat pregnant and postpartum athletes? Maybe you don’t feel confident in knowing how to modify activity for this population, or you feel that most high-intensity activity should be ceased during pregnancy and early postpartum.
If this is you, might I encourage you to take our upcoming course on special considerations for Pregnant and Postpartum High-Intensity Athletes?
While this patient population is like the general population in many ways, there is a certain nuance in evaluating pregnant and postpartum athletes. This is especially true for elite or high-intensity athletes. Considering the demands of many of these high-intensity sports (running, powerlifting, CrossFit, Orange Theory) it is imperative that pelvic therapists also understand orthopedics, and vice versa. In bridging this gap between specialties, we have the opportunity to optimize performance, while ensuring our patients also remain healthy.
Keeping this in mind, our evaluation will look a bit different than traditional pelvic and orthopedic evaluations. Specifically, each respective specialty should be screening the other. If you are a pelvic therapist, you should also be screening the lumbar spine, SI joint, Hip joint, and mid-thoracic spine. You should also be performing a functional movement analysis that is specific to their desired sport. If you are an orthopedic therapist, you should also be screening for diastasis recti, pressure management capability, and pelvic floor tension and/or weakness. While orthopedic therapists will not be performing an internal exam like their pelvic therapist counterparts, there are still several screening methods that can be used to determine if a patient requires referral to a pelvic PT. And that is exactly what this course aims to do.
Pregnancy and Postpartum Considerations for High-Intensity Athletics aims to bridge the gap between pelvic and orthopedic therapists and to help educate providers on how to evaluate this patient population with confidence. We will cover special medical considerations for this patient population, ways in which to modify activity for this population, and how to keep them doing what they love safely throughout pregnancy and postpartum. So, if you would like to learn more about working with pregnant and postpartum athletes, go ahead and sign up for our September 15th course offering. We’d love to have you!
AUTHOR BIO
Emily McElrath PT, DPT, MTC, CIDN
 Emily McElrath is a native of New Orleans and received her undergraduate degree in Athletic Training at the University of Southern Mississippi and went on to receive her Doctorate of Physical Therapy from the University of St. Augustine for Health Sciences. She is highly trained in Sports and Orthopedics and has a passion for helping women achieve optimal sports performance. Emily is certified in manual therapy and dry needling, which allows her to provide a wide range of treatment skills including joint and soft tissue mobilization. She is an avid runner and Cross-fitter and has personal experience modifying these activities during pregnancy and postpartum. While not working, Emily enjoys time with her husband and two kids.
Emily McElrath is a native of New Orleans and received her undergraduate degree in Athletic Training at the University of Southern Mississippi and went on to receive her Doctorate of Physical Therapy from the University of St. Augustine for Health Sciences. She is highly trained in Sports and Orthopedics and has a passion for helping women achieve optimal sports performance. Emily is certified in manual therapy and dry needling, which allows her to provide a wide range of treatment skills including joint and soft tissue mobilization. She is an avid runner and Cross-fitter and has personal experience modifying these activities during pregnancy and postpartum. While not working, Emily enjoys time with her husband and two kids.

Caring for patients who have experienced trauma requires a skillset beyond basic knowledge of pelvic health assessment and intervention. With one-third of women experiencing intimate partner violence, and estimates of rape reports to formal agencies (e.g., police, medical professionals) ranging from only 5–33% (Fisher, Cullen, & Turner, 2000; Kilpatrick et al., 2007; Krebs et al., 2007; Rennison, 2002), we can safely say that the gender-based violence women uniquely experience is likely grossly under-reported.
Additionally, the World Health Organization reports that violence and sexual violence against women is a major global public health problem. Estimates published by WHO indicate that globally about 1 in 3 (30%) of women ages 15-49 worldwide have been subjected to either physical and/or sexual intimate partner violence or non-partner sexual violence in their lifetime.
In terms of violence, the vast majority is, sadly, intimate partner violence; that is, violence committed by your own partner. Further, the overall risk of any gender reporting intimate partner violence is 1 in 7 for people who identify as men, and 1 in 5 for people who identify as female, according to the last reported statistics from the CDC.
For trauma risk in general, the chance of any gender experiencing trauma, including ACEs, or Adverse Childhood Experiences, is as high as over 70%. The first comprehensive study on PTSD (post-traumatic stress disorder) and trauma in the US was not conducted until 1990, which reported that 60.7% of men and 51.2% of women reported at least one exposure to trauma. From there, the estimated population lifetime prevalence of 5.7% for men and 12.8% for women (Kilpatric et al 2013).
The statistics on violence against the LGBTQIA community are even more alarming. A survey found that transgender people (16+) are victimized over four times more often than cisgender people and that transgender women and men had higher rates of violent victimization than cisgender women and men. Overall, about 50% of the violent victimizations were not reported to police. A separate 2022 survey showed that LGBT people experienced 6.6 violent hate crime victimizations per 1,000 persons compared with non-LGBT people's 0.6 per 1,000 persons (odds ratio = 8.30, 95% confidence interval = 1.94, 14.65).
 If you are working with this population, there is a long list of adverse impacts known to affect all genders who have experienced trauma, especially if they go on to develop PTSD or complex PTSD (cPTSD), and even more so if the person experienced an ACE. A traumatic event is defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM5) as a direct or indirect witness (indirect means learning about the trauma of a loved one) to actual or threatened death, serious injury, or sexual violence, either of which can induce PTSD. Four symptom clusters define PTSD in the DSM5:
If you are working with this population, there is a long list of adverse impacts known to affect all genders who have experienced trauma, especially if they go on to develop PTSD or complex PTSD (cPTSD), and even more so if the person experienced an ACE. A traumatic event is defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM5) as a direct or indirect witness (indirect means learning about the trauma of a loved one) to actual or threatened death, serious injury, or sexual violence, either of which can induce PTSD. Four symptom clusters define PTSD in the DSM5:
- Intrusive symptoms - recurrent and unwanted memories, nightmares, flashbacks, and intense distress or physiological reactivity after exposure to traumatic reminders.
- Avoidance symptoms - avoidance of trauma-related thoughts, feelings, or reminders.
- Persistent negative beliefs - negative emotions related to the trauma (such as guilt, shame, anger, horror), loss of interest in significant activities, feelings of alienation from others, and an inability to experience positive or loving emotions.
- Alterations in arousal and reactivity - irritability or aggression, self-destructive or reckless behavior, hypervigilance, exaggerated startle response, and problems with concentration and sleep.
Some of the signs of cPTSD can include:
- Behavioral difficulties (e.g. impulsivity, aggressiveness, sexual acting out, alcohol/drug misuse, and self-destructive behavior)
- Emotional difficulties (e.g. affect lability, rage, depression, and panic)
- Cognitive difficulties (e.g. dissociation and pathological changes in personal identity)
- interpersonal difficulties (e.g. chaotic personal relationships)
- Somatization (resulting in many visits to medical practitioners)
Some of the musculoskeletal and lifestyle manifestations of experiencing trauma and even just stress include:
- Musculoskeletal tension or “trauma posturing” (aka constant guarding)
- Upregulated sympathetic nervous system response (aka fight or flight)
- Increased stress hormones - adrenaline, noradrenaline, cortisol
- Low back pain
- Headaches
- Sleep disturbances due to clenching, grinding, or nightmares
- Indigestion, ulcers, IBS, bloating, impaired or slowed gastrointestinal motility
- Poor circulation due to poor breathing patterns
- Increased heart rate, blood pressure
- Decreased fertility in women and men
- Worsening or influence on PMS and perimenopause/menopause
- Sexual dysfunction including decreased sexual desire, and/or erectile dysfunction)
- Increased risk of hypertension and heart attack
- Chronic activation of the HPA Axis
- Upregulated glucocorticoids, resulting in decreased immune function and increased systemic inflammation
- Increased risk for chronic fatigue syndrome, metabolic disorders including diabetes and obesity, and depression
- Increased risk for reflux and increased swallowing issues due to laryngeal tension
- Muscle tension dysphonia
- Chronic hoarseness, laryngitis, or psychogenic dysphonia
- Poor cognitive function and executive functioning
With regard to pelvic health, Yehuda et al posit that “because some symptoms of PTSD, such as nightmares, intrusive memories, and insomnia, are so distressing and result in such great restrictions in overall quality of life, sexual dysfunction is often not presented as a top priority by treatment-seeking patients.” The researchers also cite multiple studies which no longer support that sexual dysfunction only arises from sexual trauma. They write, “studies of nonsexual trauma including combat, accidents, and criminal victimization have now also established an association with sexual dysfunction in men and women including sexual desire, arousal, orgasm, activity, and satisfaction.” For example, Cosgrove et al found that male combat-exposed veterans (n = 90) rates of erectile dysfunction were 85% in veterans with PTSD compared with 22% in veterans without PTSD.
Trauma Can Literally Steal Your Voice
 Further, trauma, no matter what type, intimately impacts the voice. The condition of losing your voice after trauma is known as psychogenic dysphonia or aphonia. It is characterized by the loss of volitional control over phonation after psychological events such as anxiety, depression, conversion reaction, or personality disorders, cites Baker (2003). It can also develop after viruses, with COVID-19 bringing not just respiratory consequences but a unique multi-system impact with negative consequences for the pelvic floor, such as occurs after prolonged coughing, hospitalization, and/or intubation.
Further, trauma, no matter what type, intimately impacts the voice. The condition of losing your voice after trauma is known as psychogenic dysphonia or aphonia. It is characterized by the loss of volitional control over phonation after psychological events such as anxiety, depression, conversion reaction, or personality disorders, cites Baker (2003). It can also develop after viruses, with COVID-19 bringing not just respiratory consequences but a unique multi-system impact with negative consequences for the pelvic floor, such as occurs after prolonged coughing, hospitalization, and/or intubation.
Any emotionally or psychologically taxing event that occurs in proximity to loss of vocal control must be investigated, in order to understand the qualitative variables that may be present in the voice dysfunction. It doesn’t even take trauma to steal your voice, since stress is cited as a top driver for muscle tension dysphonia.
For example, I have had multiple clinical cases where women struggle with their voice decades after experiencing sexual assault in college or in an intimate relationship, but chose to “keep it a secret” and not report it. I’ve also seen patients with post-COVID or long COVID who report severe struggles with return to exercise or full activities of daily living due to concomitant respiratory and pelvic floor difficulties. Further, I have treated patients who presented after accidental damage to the recurrent laryngeal nerve during surgery and are struggling to recover both their voice and pelvic floor function. Finally, I have countless patients who have been medically gaslit and told their voice and pelvic floor pain are unrelated.
Regardless of the reason, we have an obligation as pelvic health clinicians to provide the best evidence-informed care possible. The Voice to Pelvic Floor (V2PF) method is one such way to provide trauma-informed and psych-informed pelvic healthcare. The V2PF approach is a systems-based way to evaluate the patient looking at the connection between three diaphragms:
- The orofacial/cervico-laryngeal diaphragm
- The respiratory diaphragm
- The pelvic diaphragm
The purpose of a V2PF approach is to provide a deeper understanding of polyvagal theory, anatomy and physiology, neuropsychology, trauma-informed principles, as well as sociocultural issues that impact our world, in order to allow us to function as primary care providers in pelvic health across the lifespan.
Want more information? Learn how to assess and plan interventions using a voice-to-pelvic floor trauma-informed approach at Dr. Garner’s course – The Voice and the Pelvic Floor scheduled on September 7th, 2024.
Sources
- Kilpatrick D.G., Resnick H.S., Milanak M.E., Miller M.W., Keyes K.M., Friedman M.J.National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress2013;26: 537- 547.
- Sexual Victimization of College Women | Office of Justice Programs [WWW Document], n.d. URL https://www.ojp.gov/ncjrs/virtual-library/abstracts/sexual-victimization-college-women (accessed 8.6.24).
- CDC, 2024. About Intimate Partner Violence [WWW Document]. Intimate Partner Violence Prevention. URL https://www.cdc.gov/intimate-partner-violence/about/index.html (accessed 8.6.24).
- Campus Sexual Assault (CSA) Study | Office of Justice Programs [WWW Document], n.d. URL https://www.ojp.gov/ncjrs/virtual-library/abstracts/campus-sexual-assault-csa-study (accessed 8.6.24).
- Rennison, C.M., 2002. Rape and Sexual Assault: Reporting to Police and Medical Attention, 1992-2000: (387542004-001). https://doi.org/10.1037/e387542004-001
- Kilpatrick, D.G., Ruggiero, K.J., Acierno, R., Saunders, B.E., Resnick, H.S., Best, C.L., 2003. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the National Survey of Adolescents. Journal of Consulting and Clinical Psychology 71, 692–700. https://doi.org/10.1037/0022-006X.71.4.692
- Flores, A.R., Meyer, I.H., Langton, L., Herman, J.L., 2021. Gender Identity Disparities in Criminal Victimization: National Crime Victimization Survey, 2017–2018. Am J Public Health 111, 726–729. https://doi.org/10.2105/AJPH.2020.306099
- First, M.B. (Ed.), 2022. Diagnostic and statistical manual of mental disorders: DSM-5-TR, Fifth edition, text revision. ed. American Psychiatric Association Publishing, Washington, DC.
- Flores, A.R., Stotzer, R.L., Meyer, I.H., Langton, L.L., 2022. Hate crimes against LGBT people: National Crime Victimization Survey, 2017-2019. PLoS One 17, e0279363. https://doi.org/10.1371/journal.pone.0279363
- Yehuda, R., Lehrner, A., Rosenbaum, T.Y., 2015. PTSD and Sexual Dysfunction in Men and Women. J Sex Med 12, 1107–1119. https://doi.org/10.1111/jsm.12856
- Cosgrove, D.J., Gordon, Z., Bernie, J.E., Hami, S., Montoya, D., Stein, M.B., Monga, M., 2002. Sexual dysfunction in combat veterans with post-traumatic stress disorder. Urology 60, 881–884. https://doi.org/10.1016/S0090-4295(02)01899-X
- Baker, J., 2003. Psychogenic voice disorders and traumatic stress experience: a discussion paper with two case reports. J Voice 17, 308–318. https://doi.org/10.1067/s0892-1997(03)00015-8
- VA.gov | Veterans Affairs [WWW Document], n.d. URL https://www.ptsd.va.gov/professional/treat/essentials/complex_ptsd.asp (accessed 8.6.24).
- Siracusa, C., Gray, A., 2020. Pelvic Floor Considerations in COVID-19. Journal of Women’s Health Physical Therapy 44, 144–151. https://doi.org/10.1097/JWH.0000000000000180
AUTHOR BIO:
Dr. Ginger Garner PT, DPT, ATC-Ret

Dr. Ginger Garner PT, DPT, ATC-Ret is a clinician, author, educator, and longtime advocate for improving access to physical therapy services, especially pelvic health. She is the founder and CEO of Living Well Institute, where she has been certifying therapists and doctors in Medical Therapeutic Yoga & Integrative Lifestyle Medicine since 2000. She also owns and practices at Garner Pelvic Health, in Greensboro NC, where she offers telehealth and in-person wellness and therapy services. Ginger is the author of multiple textbooks and book chapters, published in multiple languages. She has also presented at over 20 conferences worldwide across 6 continents across a range of topics impacting the pelvic girdle, health promotion, and integrative practices.
Ginger is an active member of APTA, serving as the Legislative Chair for APTA North Carolina, as a Congressional Key Contact for APTA Private Practice, and in the Academy of Pelvic Health. Ginger lives in Greensboro, NC with her partner, 3 sons, and their rescue pup, Scout Finch. Visit Ginger at the websites above and on Instagram and YouTube.

When I was diagnosed with Thyroid Cancer, I’ll be honest, one of my first thoughts was “Thank goodness this won’t directly affect my pelvic floor.” I think as someone who has experienced pelvic floor problems in the past and worked in the pelvic health field for many years, this is probably a somewhat normal reaction, but it wasn’t the standard from my parents and other loved ones. They wanted answers and information and because Thyroid cancer didn’t fall into my niche knowledge of pelvic health, I had to do some research.
Let’s start by saying that thyroid Cancer is the most pervasive endocrine cancer in the world (Bray, 2018). It is the sixth most common cancer in females in the United States (Siegel, 2019). Thyroid cancer incidence and outcomes depend on where the patient lives with Ethiopia and the Philippines having the highest death rates (Deng, 2020). There has been a rise in the diagnosis of thyroid cancer which studies attribute to access to health care, ultrasound, training of those doing the ultrasound, use of fine needle aspiration biopsy, and changes in monitoring and management guidelines (Megwalu & Moon, 2022). The five-year survival rate for people diagnosed with Thyroid Cancer is around 98.5% (Boucai et al. 2024). There are a few types of Thyroid Cancer and Papillary Thyroid Cancer accounts for 84% of all cases (Boucai et al. 2024). There are also follicular, medullary, and anaplastic forms making up the remaining cases (Boucai et al. 2024).
When I tell people I have Thyroid Cancer one of their first questions is “What were your symptoms, how did you know?!” The short answer is, I didn’t know. My cancer journey started when I found out I had a 3 cm nodule that had grown a “significant” amount since my last ultrasound. My endocrinologist said the growth was enough to warrant a fine needle aspiration biopsy. In reading about this diagnosis, it seems many cases of Thyroid Cancers are asymptomatic and detected during a routine physical examination or found incidentally with diagnostic imaging (Boucai et al. 2024).
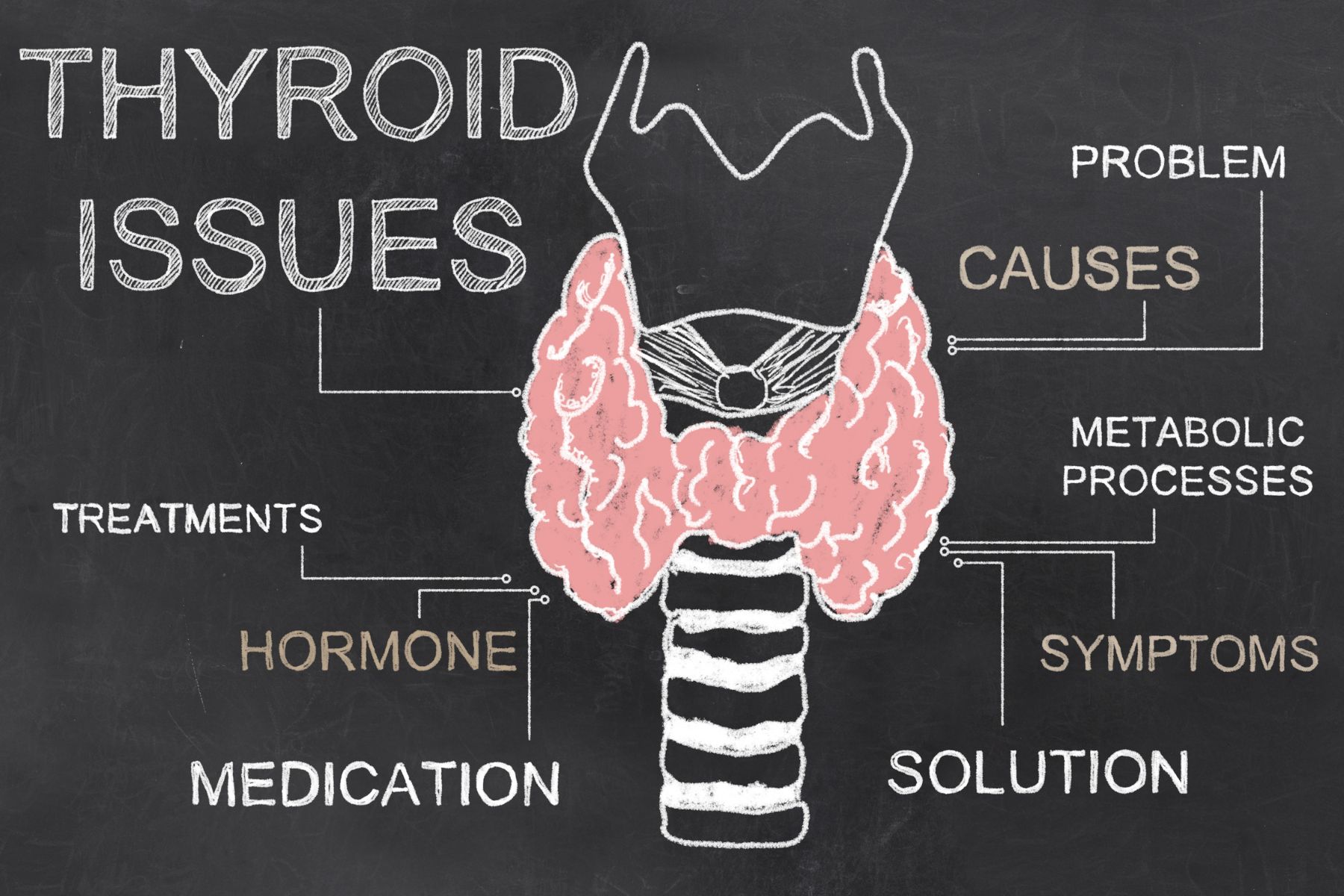 Some other symptoms, mostly related to a growing tumor could include lumps in the throat, a hoarse voice lasting three or more weeks, trouble swallowing or breathing, neck pain/pressure, and swollen cervical lymph nodes. If we had a patient with such complaints, referring them to their primary provider for further diagnostics would be very appropriate. Medullary thyroid cancer does have the ability to increase bowel movements and cause diarrhea and therefore should be on a pelvic health provider’s radar for differential diagnosis. The good news is that the solution to most cases of Thyroid Cancer is surgical removal of the thyroid with the option to perform radioactive iodine ablation treatment. There are other targeted therapies available if the cancer does not respond to radioactive iodine including antiangiogenic multikinase inhibitors and medications for specific genetic mutations (Boucai et al. 2024).
Some other symptoms, mostly related to a growing tumor could include lumps in the throat, a hoarse voice lasting three or more weeks, trouble swallowing or breathing, neck pain/pressure, and swollen cervical lymph nodes. If we had a patient with such complaints, referring them to their primary provider for further diagnostics would be very appropriate. Medullary thyroid cancer does have the ability to increase bowel movements and cause diarrhea and therefore should be on a pelvic health provider’s radar for differential diagnosis. The good news is that the solution to most cases of Thyroid Cancer is surgical removal of the thyroid with the option to perform radioactive iodine ablation treatment. There are other targeted therapies available if the cancer does not respond to radioactive iodine including antiangiogenic multikinase inhibitors and medications for specific genetic mutations (Boucai et al. 2024).
Let’s get to the good part, the therapeutic indications! How can we best support our patients going through Thyroid Cancer or after they have completed treatment?
There are a few things to consider and based on the setting you work on, you may or may not be the one to provide these services.
First, if the patient has a partial or total thyroidectomy, they will have a surgical incision which means a scar to work on and connective tissue restriction. We can help them to mobilize and soften this scar to maintain their cervical range of motion and help the scar to heal better, be less painful, and be more visually appealing. If the therapist has the training, education, and/or application of lymphatic drainage is also very valuable in this healing time.
The patient will have activity restrictions for 1 - 4 weeks depending on the severity of the procedure, including needing rest, eating soft foods, avoiding extremes of ROM of the neck and upper extremities, and regaining vocal control. Working with a patient prior to surgery to review ways to conserve energy and prepare themselves and their home for surgery can be invaluable, especially if the patient doesn’t have a huge support system available post-operatively. Food shopping, meal prepping, and convenience stations set up in the home can make post-operative recovery much smoother.
From personal experience, the throat irritation from the intubation was the most annoying and longest-lasting symptom. My surgeon used electrical stimulation with my intubation to my vocal cords to avoid damage to them. The mucous and hoarseness this created lasted a full 7 days. I still had voice limitations for about a month after and had to work to regain my full voice. Everyone handles pain differently though, and others may feel more pain. My provider, a very seasoned ENT, said they typically found post-thyroid patients had less discomfort than their patients with tonsillectomy or adenoid removal. This can give your patient a benchmark of what to expect if they’ve had one of those surgeries. We can give recommendations to our clients to help with pain management such as using rest, ice, gentle movement, breathing exercises, and meditation to help manage the discomfort, while also taking their pain medication regularly.
As a pelvic floor therapist, as soon as I hear pain medication is involved, I want to make sure that we are keeping the bowels happy. If we have a patient expecting this type of surgery and treatment, we can help guide them to fiber-filled foods and fluid intake to avoid constipation (as long as they don’t have restrictions). If constipation is not something they typically experience, this may be their first introduction to things like osmotic laxatives and a squatty potty and we can be the person who presents them with this education if they need it.
There will be a few things going on hormonally after the surgery. Because the thyroid has been removed, the patient will be hypothyroid unless they take synthetic thyroid hormone or have a partial thyroidectomy where the remaining half has continued to function and adjust. Hypothyroidism can cause many symptoms, but related to our patients in pelvic health, we might see constipation, fatigue, skin changes, menstrual cycle changes, musculoskeletal complaints, and intolerance to temperature changes. If we see our patient experiencing any of these, we can refer them back to their provider to have their levels checked. We can also tailor our plan of care to adjust for some of these things.
 Another more life-threatening complication that can happen is disruption of the parathyroid glands. These produce the calcium needed to regulate muscles and nerves. With calcium levels too low, a person can experience some uncomfortable and possibly dangerous symptoms such as feeling foggy and confused, muscle tremors, heart arrhythmias, and even seizures if the levels get too low. These little guys sit right under the thyroid and can be traumatized or accidentally removed with the thyroid. After surgery, patients will likely be taking a calcium supplement and have instructions to take it if they feel this way, but they may need a reminder from their very caring and observant therapist.
Another more life-threatening complication that can happen is disruption of the parathyroid glands. These produce the calcium needed to regulate muscles and nerves. With calcium levels too low, a person can experience some uncomfortable and possibly dangerous symptoms such as feeling foggy and confused, muscle tremors, heart arrhythmias, and even seizures if the levels get too low. These little guys sit right under the thyroid and can be traumatized or accidentally removed with the thyroid. After surgery, patients will likely be taking a calcium supplement and have instructions to take it if they feel this way, but they may need a reminder from their very caring and observant therapist.
When we think about how else Thyroid Cancer could affect our patients, I think it is important to consider the emotional aspect. Even though it’s a very common, easy-to-treat cancer with a high “cure rate,” it is still cancer. From personal experience, providers are so used to treating more sick people, that they have an almost blase attitude towards the treatment. I’ve spoken to others with endocrine cancer and heard similar stories. We have the “friendly” cancer, why stress or make haste about anything? There is a lack of haste or urgency, which can feel disconcerting when you just want to be cancer-free ASAP.
The incision, if surgery is needed, is directly to the anterior aspect of the neck. It's hard to hide the scar unless you wear a turtleneck. Most surgeons try to make the incision in a fold of the neck, but this may not be possible if lymph nodes also need to be dissected. Scars also take about a year to remodel and “silver.” We can further help our patients feel more confident with their scars by reminding them to avoid sunlight and utilize silicone patches to soften and protect the area to allow the scar to mature into a minimally noticeable line. There is still a reminder every time the patient looks in the mirror and this may affect all aspects of their life including their confidence in areas like sexual intimacy.
The last area to consider would be if a person needs the radioactive iodine treatment. Although this treatment is not “aggressive” like chemo or traditional targeted radiation, it can be a stressor to a patient. Radioactive iodine ablation has an extensive prep, multi-procedure application, and post-treatment quarantine phase that can be very disruptive to a person’s life. Pelvic health providers won’t be actively managing this phase, but being a friendly ear to bounce iodine-free recipe ideas off of and commiserate with the inability to ingest dairy for 3+ weeks can help make your patient feel supported and heard.
I have been fortunate enough to take Herman & Wallace’s Oncology series and so I felt prepared to treat and manage patients with these types of cancer. It was my own Thyroid Cancer journey that gave me hands-on experience with what it is like to be a cancer patient. It's been interesting to have to advocate in a medical system that doesn’t always listen to patients. I’ve also had to re-find who I am after having a pretty significant medical episode. These experiences always help give me perspective to be a better provider to my patients and bring more personalized care to them. I encourage you to take these classes, as cancer really affects so many lives. My most comforting providers during this time have been those who have taken the time to answer my questions, hold space for my worries, and have humor with me during this bizarre time.
The HW Oncology Series includes:
- Oncology of the Pelvic Floor Level 1 - Introduction (*Certified Lymphatic Therapists may skip this course)
- The next scheduled course is on November 2-3
- Oncology of the Pelvic Floor Level 2A - Male Pelvic and Colorectal Cancers
- The next scheduled course is on September 7-8
- Oncology of the Pelvic Floor Level 2B - Urogynecological Cancers
- The next scheduled course is on December 7-8
References:
- Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., & Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians, 68(6), 394-424.
- Boucai, L., Zafereo, M., & Cabanillas, M. E. (2024). Thyroid cancer: a review. Jama, 331(5), 425-435.
- Deng, Y., Li, H., Wang, M., Li, N., Tian, T., Wu, Y., ... & Dai, Z. (2020). Global burden of thyroid cancer from 1990 to 2017. JAMA network Open, 3(6), e208759-e208759.
- Megwalu, U. C., & Moon, P. K. (2022). Thyroid cancer incidence and mortality trends in the United States: 2000–2018. Thyroid, 32(5), 560-570.
- Siegel RL, Miller KD, Jemal A 2019 Cancer statistics, 2019. CA Cancer J Clin 66:7–30.
AUTHOR BIO:
Mora Pluchino, PT, DPT, PRPC

I am a graduate of Stockton University with my BS in Biology (2007) and Doctorate of Physical Therapy (2009). I have experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. I began treating Pelvic Health patients in 2016 and now have experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much I have not treated since beginning this journey and I am always happy to further my education to better help my patients meet their goals.
I strive to help all of my patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at the present time. In 2020, I opened my own practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. I have been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. I have also been a TA with Herman & Wallace since 2020 and have over 150 hours of lab instruction experience.
The diagnosis of chronic constipation may seem like a simple concept; however, bowel patients can be a challenging group within our pelvic health population. The interesting part about treating these patients is that constipation can result in a variety of complaints. Diaz et al confirmed this in their 2023 research. Their article shared that “Constipation encompasses several subtypes, each with its unique characteristics and underlying factors.”(1) Common complaints can include frequency, size, length, and consistency which can become overwhelming for the practitioner to decide which clinical complaints seem the most important to focus on.
Knowing how to effectively treat these patients and ask the right questions is valuable in the scheme of pelvic floor rehab, secondary to overlapping symptoms and etiology of chronic constipation. Consideration needs to be taken into account for any outside factors that can also contribute to patient complaints. For example, taking different prescription medications, supplements, and eating different foods can all influence the patient's stool frequency and formation (2). Realizing where this issue stems from is the deep-dive question to get a handle on their complaints.
Bowel frequency can be one of the biggest clinical challenges for clinicians to educate patients to master – consistency is key! Understanding what their normal frequency should be, or what it should be now, is part of the clinical judgment skill when setting goals. If your patient is only getting a natural bowel movement urge every 10 days, their goal of daily BMs, at first, should be emotionally readjusted so that they don’t feel like they have failed their rehabilitation goals.
Learning colon physiology helps to understand normal vs abnormal motility and can be helpful in treating your patient’s constipation. In my course, Bowel Pathology and Physiology we discuss the physiological reflex that controls the lower motility of the GI tract following a meal (3). When patients present with chronic constipation, they may be experiencing a profound loss of the gastrocolic reflex. The course is filled with clinical pearls and research tidbits that help to improve or slow down colonic motility. Join me in the next course offering on September 14-15, 2024 to learn more.
Resources:
- Diaz S, Bittar K, Hashmi MF, et al. [Updated 2023 Nov 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513291/
- Araújo MM, Botelho PB. Probiotics, prebiotics, and synbiotics in chronic constipation: Outstanding aspects to be considered for the current evidence. Front Nutr. 2022 Dec 8;9:935830. doi: 10.3389/fnut.2022.935830. PMID: 36570175; PMCID: PMC9773270.
- Mawer S, Alhawaj AF. Physiology, Defecation. 2023 Nov 13. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 30969554.
AUTHOR BIO
Lila Abbate, PT, DPT, MS, OCS, WCS, PRPC
 Lila Abbate is the Director/Owner of New Dimensions Physical Therapy. She graduated from Touro College in Dix Hills, NY with a Bachelor of Science (BS) in Health Sciences and a Master of Arts (MA) in Physical Therapy in 1997. She completed her Advanced Masters in Manual Orthopedic Physical Therapy (MS) at Touro College, Bayshore, NY in 2003 and continued to pursue her Doctor of Physical Therapy (DPT) at Touro in 2005. Dr. Abbate is a Board-Certified Specialist by the American Physical Therapy Association in Orthopedics (OCS) 2004 and Women’s Health (WCS) 2011. She obtained the Certified Pelvic Rehabilitation Practitioner (PRPC) from the Herman & Wallace Institute in 2014. She is a Diane Lee/LJ Lee, Integrated Systems Model (ISM) graduate and completed the New York series in 2012.
Lila Abbate is the Director/Owner of New Dimensions Physical Therapy. She graduated from Touro College in Dix Hills, NY with a Bachelor of Science (BS) in Health Sciences and a Master of Arts (MA) in Physical Therapy in 1997. She completed her Advanced Masters in Manual Orthopedic Physical Therapy (MS) at Touro College, Bayshore, NY in 2003 and continued to pursue her Doctor of Physical Therapy (DPT) at Touro in 2005. Dr. Abbate is a Board-Certified Specialist by the American Physical Therapy Association in Orthopedics (OCS) 2004 and Women’s Health (WCS) 2011. She obtained the Certified Pelvic Rehabilitation Practitioner (PRPC) from the Herman & Wallace Institute in 2014. She is a Diane Lee/LJ Lee, Integrated Systems Model (ISM) graduate and completed the New York series in 2012.
Dr. Abbate has been an educator for most of her physical therapy career. She has experience as a full-time faculty at Touro College, Manhattan Campus from 2002 to 2006 teaching the biomechanical approach to orthopedic dysfunction and therapeutic exercise as well as massage/soft tissue work that highlighted trigger point work, scar management, and myofascial release. She is currently on faculty as a Lecturer at Columbia University teaching the private practice section Business & Management course (since 2016) along with the Pelvic Health elective (since 2012). She teaches nationally and internationally with the Herman & Wallace Pelvic Rehabilitation Institute teaching advanced courses of her own intellectual property: Orthopedic Assessment for the Pelvic Health Therapist, Bowel Pathology Function, Dysfunction and the Pelvic Floor, Coccydynia & Painful Sitting: Orthopedic Implications. She was a co-writer for the Pudendal Neuralgia course and teaches the Pelvic Function Series, and Pregnancy/Postpartum Series. She has written two book chapters in 2016: Pelvic Pain Management by Valvoska and Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies by Chughtai.
Lila is a member of the American Physical Therapy Association, the National Vulvodynia Association, the American Urogynecology Association, the International Pelvic Pain Society, and is also a Senior Physical Therapy consultant for SI Bone, a sacroiliac joint instrumentation company.

The HW admin team has been hard at work filling speaker spots, building breakout sessions, and creating fun new experience ideas for the upcoming 2025 conference.
If you're into pelvic health then this is the conference for you. HWConnect was created to provide a top-tier networking event for pelvic rehabilitation practitioners that focuses on providing a safe environment for professional development, exposure to new products, and sharing inspiration for all things pelvic health.
HWConnect features keynote speakers, breakouts, labs, and educational sessions. Topics range from pediatrics with Dawn Sandalcidi to gender-affirming care with Ken McGee. HWConnect is all about connection - the name says it all. Network. Learn. Grow. Repeat. 
Registering is as easy as 1, 2, 3!
- Complete online registration.
- Book travel and lodging. HWConnect will be held at the Hilton Seattle Airport & Conference Center and HW has special pricing set up for attendees.
- Show up, and don't forget to stop by and say hello to all of your favorite HW team members!
Need More Information?
- Keynote Speakers are the indomitable Dawn Sandalcidi, PT, RCMT, BCB-PMD (she/her), Nancy Norton, RN (she/her), and Leticia Nieto, PsyD, LMFT, TEP (she/her).
- Speakers include Ken McGee, PT, DPT (they/he), Dr. Cindy Mosbrucker (she/her), Meryl Alappattu, PT, PhD (she/her), and Carole High Gross, PT, DPT, PRPC (she/her).
- Breakout sessions, workshops, and labs include yoga, meditation, rehabilitative ultrasound imaging, squat analysis, and MORE - all led by your favorite HW faculty including Dustienne Miller, Nari Clemons, and Allison Ariail.
- HW proudly welcomes second-time conference sponsor CMT.
- Vendor Hall featuring exhibitors including Intimate Rose, Slippery Stuff, and Raise the Pelvic Floor.
- Non-profit booths feature the Kenya Scholarship Foundation and Open Arms Perinatal Services. Read this past blog to learn more about the Kenya Scholarship Foundation.
- Special Podcast Guests feature Callie and Rachel from Pelvic Service Announcement (PSA) and Courtney from Raise the Pelvic Floor.
For more information and a full lineup check out the HWConnect 2025 page!
Already Coming to HWConnect?
That's amazing!
Herman & Wallace would love your help spreading the word about HWConnect 2025 and the chance to connect with the amazing people in our community. Check out this page where you can review and share all the programming we’ve booked thus far. https://hermanwallace.com/connect-2025
We look forward to seeing you at HWConnect 2025!
Dawn is debuting a new course, Pediatric Postural Development, with Herman & Wallace on September 29, 2024.
Most physical and occupational therapists learn about one diaphragm in school: the respiratory diaphragm. But did you know that Osteopathic Manipulative Medicine recognizes 5 different diaphragms within the body? They include tentorium cerebelli, tongue, thoracic outlet, respiratory diaphragm, and pelvic floor. (1)
The intricate myofascial connections between all these diaphragms are fascinating! But as a pediatric pelvic floor therapist, what’s the significance of these connections when you look at kids’ functional mobility and strength?
The pelvic floor and respiratory diaphragm are the two main structures that we’ll be discussing today. You’ll learn how they develop during infancy and childhood and how their functional relationship affects your assessment and treatment for kids with bowel and bladder dysfunction.
Development Of The Pelvis, Spine, And Diaphragm During Infancy
Pelvic Structure At Birth
 Pelvic structure and spinal curvatures develop based on the activities of infants and young children. The educational role that you have as a pediatric therapist is significant during a child’s first years of life, especially for children with congenital or developmental delays. Doing your best to help them achieve these developmental goals will greatly affect their life in later years.
Pelvic structure and spinal curvatures develop based on the activities of infants and young children. The educational role that you have as a pediatric therapist is significant during a child’s first years of life, especially for children with congenital or developmental delays. Doing your best to help them achieve these developmental goals will greatly affect their life in later years.
At birth, the pelvis of the baby is funnel shaped and the respiratory diaphragm is oblique. You can observe a neonate with a wide rib cage, which only allows for a short descent of the ribs. You can hear evidence of this as a newborn’s cry is very short. At this time, their pelvic floor has no posture.
Cervical Lordosis
The first curve to develop in an infant is cervical lordosis. Neck control improves as the head is challenged against gravity. In an upright position, the neck is challenged to maintain a neutral position. In prone, the neck is challenged to extend and re-enforces a lordotic curve.
Tummy time is important to begin at a young age. Not only do kids develop neck and core strength, but extending the neck in a prone establishes proper cervical lordosis for later in life.
Thoracic Kyphosis And Ribcage
Thoracic kyphosis develops when a child begins sitting. Again, thinking about sitting from a trunk control perspective is important, but establishing proper kyphotic alignment should not be overlooked. A mild degree of kyphosis is normal, but congenital deformities can exaggerate children’s kyphosis and increase the difficulty of achieving good sitting posture.
Independent sitting is an important milestone itself and further affects: (2)
- object perception
- language development
- spatial memory
- visual processing
- overall cognition
When treating infants, let’s remember to teach how important the skill of independent sitting is. We will discuss this further in the last section and how it relates to pelvic floor function.
As an infant increases their activity in the quadruped position, the diaphragm angle gets steeper inside the ribcage. This angle also increases through weight-bearing positions and with the development of the scapular stabilizers around the ribcage.
Lumbar Lordosis And Sacrum
Standing influences lumbar lordosis. Once again, standing challenges core stability and develops strength. But also recognize how standing helps the child establish proper lordotic lumbar posture.
Furthermore, in standing, the diaphragm orientation changes. The diaphragm becomes more parallel to the pelvic floor. As the diaphragm establishes a more horizontal orientation with standing and walking, the muscular tone increases as it responds to the vertical pressure and pull of the viscera.
This upright position also develops the pelvic floor to counteract the pressure of the viscera being pulled down by gravity. Counternutation of the sacrum protects the pelvic floor from full visceral pressures.
Let’s take a look at the functional relationship as the diaphragm and pelvic floor develop.
Functional Relationship Of Diaphragm And Pelvic Floor During Childhood
 When the diaphragm and pelvic floor are developed in their horizontal orientations, they begin moving together during breathing. When inhaling, the diaphragm and pelvic floor descend as the ribcage and abdominal cavity expand. When exhaling, the diaphragm and pelvic floor ascend. The continued alternating movement mobilizes the viscera and creates a lymphatic pump.
When the diaphragm and pelvic floor are developed in their horizontal orientations, they begin moving together during breathing. When inhaling, the diaphragm and pelvic floor descend as the ribcage and abdominal cavity expand. When exhaling, the diaphragm and pelvic floor ascend. The continued alternating movement mobilizes the viscera and creates a lymphatic pump.
This relationship between the diaphragm and pelvic floor is why it’s so important to look at breathing mechanics in kids. Ribcage mechanics and good diaphragm strength and tone affect the mobilization of the viscera, including the stomach and intestines. This is especially relevant when treating kids with constipation.
If you watch constipated children breathe, you will notice that they often breathe more anteriorly through their bellies instead of up and down. You will also notice minimal or no expansion of the ribcages.
Additionally, when the viscera descend, this cues the pelvic floor to activate and continue developing. Around ages 2-3, the pelvic floor develops enough stretch to react to bowel and bladder function. This is the age when children typically develop urinary continence.
Although therapists usually use the term pelvic “floor”, it’s important for you to consider this as a “diaphragm”. The pelvic “diaphragm” is a dynamic partition that serves to adjust pressures and pump fluids within the body.
Lymphatics throughout the trunk, head, and limbs are all regulated by the pumping of the body’s five diaphragms. The diaphragms work together to regulate pressures, pulling fluids and toxins into the lymph system to detoxify the body. The colon has a great lymphatic network, so this is especially important in kids with bowel issues.
Now you understand how the respiratory diaphragm and pelvic floor influence function in typically developing children. What about kids with impaired functional mobility or impaired gross motor delays? Let’s dive into these considerations.
Pediatric Postural Impairments And Gross Motor Developmental Delays
 Children with physical developmental delays will have delayed pelvic floor control as well. As you learned earlier in this blog, establishing control in positions including prone, sitting, quadruped, and standing, develops a baby’s spinal curvatures.
Children with physical developmental delays will have delayed pelvic floor control as well. As you learned earlier in this blog, establishing control in positions including prone, sitting, quadruped, and standing, develops a baby’s spinal curvatures.
If children have conditions such as spina bifida or cerebral palsy, those developmental positions may be delayed or sometimes never reached.
Improper spinal curvature early in life will affect a child’s ability to attain or maintain postural positions required for voiding and defecation. This will also delay the development of the relationship between the diaphragm and pelvic floor control.
Start looking at these milestones not only from your perspective of postural control and gross motor function but also to help improve their bowel and bladder function:
- holding head up in prone
- sitting independently
- quadruped reaching and crawling
- standing independently
- walking
If a child never stands or walks, they will struggle to develop diaphragm and pelvic floor control because gravity will not challenge this system. Spending time in upright positions by using assistive devices such as standers or walkers will help develop respiratory capacity and pelvic floor control.
When you have this treatment outlook, you can help parents shift their perspectives too. Parents of children with disabilities are often overwhelmed and tired. Help them to understand the benefits of continued work in practicing and attaining developmental postural and motor skills.
 The new course, Pediatric Postural Development debuts on September 29, 2024 and focuses on the role of the pelvic floor, diaphragm, and core. This one-day course is designed to help therapists understand the development of the diaphragm and pelvic floor muscles (PFM) as they relate to core function and continence in children. Learn how to connect the ribcage, the diaphragm, and the pelvic floor for proper core activation, as well as receive instruction in anatomy and development of the diaphragm and its relationship to the pelvic floor/core. The information presented in the course applies to children who have been diagnosed with Cerebral Palsy, Down syndrome, ASD, Hypotonia, and more.
The new course, Pediatric Postural Development debuts on September 29, 2024 and focuses on the role of the pelvic floor, diaphragm, and core. This one-day course is designed to help therapists understand the development of the diaphragm and pelvic floor muscles (PFM) as they relate to core function and continence in children. Learn how to connect the ribcage, the diaphragm, and the pelvic floor for proper core activation, as well as receive instruction in anatomy and development of the diaphragm and its relationship to the pelvic floor/core. The information presented in the course applies to children who have been diagnosed with Cerebral Palsy, Down syndrome, ASD, Hypotonia, and more.
References:
- Bordoni B. The Five Diaphragms in Osteopathic Manipulative Medicine: Myofascial Relationships, Part 1. Cureus. 2020 Apr 23;12(4):e7794. doi: 10.7759/cureus.7794. PMID: 32461863; PMCID: PMC7243635.
- Kretch, K. S., Marcinowski, E. C., Hsu, Y., Koziol, N. A., Harbourne, R. T., Lobo, M. A., & Dusing, S. C. (2023). Opportunities for learning and social interaction in infant sitting: Effects of sitting support, sitting skill, and gross motor delay. Developmental Science, 26(3), e13318. https://doi.org/10.1111/desc.13318
Special thanks to Dawn for allowing The Pelvic Rehab Report to reprint her article, originally published on her website at kidsbowelbladder.com.
AUTHOR BIO:
Dawn Sandalcidi PT, RCMT, BCB-PMD
 Dawn Sandalcidi is a trailblazer and leading expert in the field of pediatric pelvic floor disorders. She graduated from SUNY Upstate Medical Center in 1982 and is actively seeing patients in her clinic Physical Therapy Specialists, Centennial CO.
Dawn Sandalcidi is a trailblazer and leading expert in the field of pediatric pelvic floor disorders. She graduated from SUNY Upstate Medical Center in 1982 and is actively seeing patients in her clinic Physical Therapy Specialists, Centennial CO.
Dawn is a national and international speaker in the field, and she has gained so much from sharing experiences with her colleagues around the globe. In addition to lecturing internationally on pediatric bowel and bladder disorders, Dawn is also a faculty instructor at the Herman & Wallace Pelvic Rehab Institute. Additionally, she runs an online teaching and mentoring platform for parents and professionals.
In 2017, Dawn was invited to speak at the World Physical Therapy Conference in South Africa about pediatric pelvic floor dysfunction and incontinence. Dawn is also Board-Certified Biofeedback in Pelvic Muscle Dysfunction (BCB-PMD). She has also been published in the Journals of Urologic Nursing and Section of Women’s Health.
In 2018, Dawn was awarded the Elizabeth Noble Award by the American Physical Therapy Association Section on Women's Health for providing Extraordinary and Exemplary Service to the Field of Physical Therapy for Children.

Ask yourself these 5 questions:
- Do you understand the importance of conducting medication reviews with all your patients?
- Can you confidently discuss the medications used in the treatment of pelvic floor, gastrointestinal (GI), and genitourinary conditions?
- Are you able to describe the common side effects of medications routinely used in pelvic health?
- Can you analyze the impact medications may have on a patient’s complaints and their treatment plan and outcomes?
- Are you able to effectively communicate with patients and other healthcare providers about medications?
If you answered "no" to any of these questions or are preparing for an upcoming PRPC or WCS exam, the Pharmacologic Considerations for the Pelvic Health Provider course is designed for you!
The Role of Medication Review in Rehabilitation Therapy
While managing medications is not within the scope of practice for rehabilitation therapists, it is crucial to review patient medications during the initial evaluation and on an ongoing basis. Therapists must assess the impact of medications on treatment and patient outcomes to ensure patient safety.
Why Pharmacology Knowledge Matters!
Aging Population: With an aging population, many patients over the age of 65 are on more than five medications, increasing the risk of side effects, adverse drug reactions, and drug interactions.
Informed Discussions: A solid grasp of pharmacology allows therapists to engage in informed discussions with patients and collaborate effectively with other healthcare providers.
Alternative Approaches: Understanding pharmacology enables therapists to explore recent medications, supplements, or alternative approaches that may minimize side effects, mitigate impacts on quality of life, and enhance function.
Evidence-Based Practices: Keeping current on advancements in pharmacology is essential for delivering effective, evidence-based physical therapy interventions.
Benefits of Pharmacology Understanding in Rehabilitation
Safe and Effective Treatment: A thorough understanding of pharmacology helps provide safe and effective treatment.
Optimized Rehab Strategies: Knowledge of pharmacology allows therapists to optimize rehabilitation strategies.
Patient Empowerment: Educating patients about their medications empowers them to make informed decisions.
Recognizing Red Flags: Identifying potential red flags related to medication use.
Improved Collaboration: Pharmacology knowledge improves collaboration with other healthcare providers.
Course Offering
Join Kristina Koch for the virtual course Pharmacologic Considerations for the Pelvic Health Provider on August 17th to deepen your understanding and stay up-to-date on the medications used in treating pelvic floor and women's and men's health dysfunctions. This course will provide you with the essential knowledge to confidently manage medication-related aspects of patient care, ensuring better outcomes and enhanced patient safety.
AUTHOR BIO
Kristina Koch, PT, DPT, MS, Board Certified Specialist in Women's Health PT (2013-2023), CLT

Kristina received her Master of Science in Physical Therapy in 1996 from Springfield College in Massachusetts. In 2001, while living in the Los Angeles area, Kristina started specializing in the treatment of pelvic floor dysfunction including bowel/bladder issues and pelvic pain, and in 2021, she went on to earn her doctorate of physical therapy from The College of St. Scholastica. During her time in Los Angeles, she was fortunate to work with and, be mentored by fellow Herman and Wallace faculty member, Jenni Gabelsburg, DPT, WCS, MSc, MTC. Kristina is a Board Certified Specialist in Women's Health Physical Therapist (2013-2023) by the American Board of Physical Therapy Specialties. She then received her lymphatic therapist certification (CLT) in 2015.
Kristina has successfully helped establish women’s health and pelvic floor physical therapy programs in San Diego, California, and Colorado Springs, CO where she currently works in private practice. Kristina treats men, women, children, trans and gender non-binary individuals in her practice. In addition, Kristina serves as a guest lecturer for graduate physical therapy students at Regis University in Denver, CO, and provides educational lectures to medical providers and local community groups. Outside of work, Kristina enjoys spending time with her husband and two children, skiing, running, and hiking.