Fears about treating men’s health conditions are limiting access to care or are creating potential for harm in the field of pelvic health. Many cisgender women (women whose gender identify matches the sex likely assigned at birth) express concerns about working with cisgender men beyond a lack of knowledge about conditions related to prostate issues, urinary leakage, or genital pain. Are these fears warranted, are they fair? Rather than assert that ciswomen should simply move beyond their concerns, the field of pelvic health and the patients with whom we work may be better served by digging in and talking more openly about such fears. Following are some of the concerns or comments I have heard expressed by cisgender women within the context of treating men’s health matters:

- (Regarding palpation of the penis:) “Is that legal?”
- “I worry about being alone in a room with a man.”
- “What if he gets an erection?”
- “My husband doesn’t want me to work with other men for pelvic health stuff.”
- “I’ve never seen a man’s genitals before and I’m not comfortable with it.”
- “My religion teaches that I should not touch a man other than my husband.”
- “I don’t know what to say when men make suggestive comments.”
- “My supervisor is forcing me to do this work with men when I don’t want to.”
- “I only treat them in side lying because then I don’t have to see their stuff.”
Rather than a reader making a judgement about the above comments, we should ask ourselves as a profession if the above topics have been properly addressed in our training or if we are encouraged to work through this area of professional and personal intersecting concerns. We could view the concerns expressed through the lens of providing equal care, in other words, are we discriminating against someone based on their genitals? Or through a lens of safety- is there an actual (as well as perceived) threat from a cisgender woman who is alone in a treatment room with a cisgender man? If that’s potentially true, how are we mitigating this risk? Where does the anatomical line end between personal beliefs such as “I can touch another man’s shoulder, but not perineal area”? Are we practicing ethically if we are denying access to care or providing less than comprehensive care? Is a therapist truly worried about their primary relationship by doing this work because their partner does not approve? And more importantly, can we provide needed guidance or support to address some of the above obstacles?
I commonly have the opportunity to work with men who have seen other self-identified female therapists first. Here is what I often hear:
- “I could tell that they weren’t comfortable talking to me about this issue.”
- “It didn’t seem like they knew what to do with me.”
- “I got switched over to another therapist after asking some questions about using a penile pump.”
- “I felt really shamed about my condition because they would change the subject.”
- “I called many places and they rejected seeing me because I’m a man.”
- “When I asked if they were going to examine where the pain is [genital area] they said it would be a last resort.”
- “No one ever examined me, just gave me a biofeedback sensor to put in.”
This information is not shared to shame the caring professionals in our field. What needs to happen, however, for elevating the inclusiveness of care, is a continual dialogue and recognition of the support needed to work with sensitive conditions and the vulnerabilities of both patients and providers. It is potentially harmful to reject patients based on gender, or to provide lesser care based on genitals. To further this conversation, the Institute has partnered with author and educator Leticia Nieto, who holds a degree in psychology and who wrote Beyond Inclusion, Beyond Empowerment: A Developmental Strategy to Liberate Everyone. Join Leticia and me (Holly Tanner) for our first 3-hour discussion that emphasizes talking, feeling, and thinking through some of the above concerns and challenges. The class will focus on discussion more than lecture, and will aim to provide a space within which we can speak openly about how to move forward with the goal of improving comfort when working with men’s health issues and improving access to much needed pelvic health care. Note: this class is welcoming to all people with any gender identification, however, the emphasis will be on the topics discussed in this post.
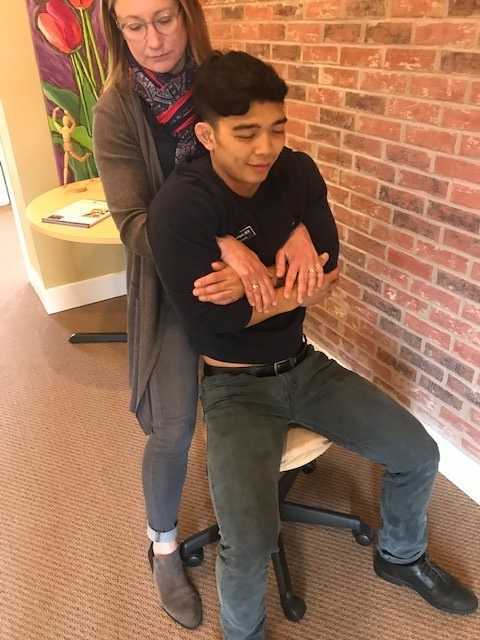
Deb Gulbrandson, PT, DPT is teaming up with Frank J Ciuba DPT, MS to create a new course called Osteoporosis Management: A Comprehensive Approach for Healthcare Professionals! This new course is launching remotely this July 25-26, 2020, and it emphasizes visual imagery cues which leads to enhanced performance for patients. Both course authors are trained by Sara Meeks, and have adapted her method to create this updated, evidence-based course on osteoporosis management.
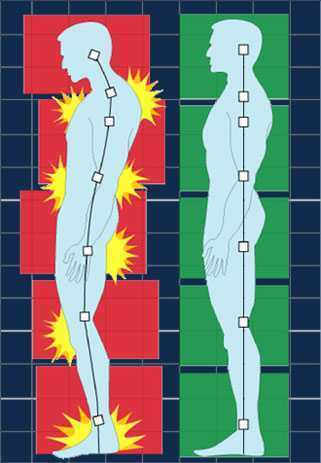
How many times have you told your patients to stand up straight and stop looking down while walking? How’d that work out? Probably not so good. At best you may have noticed a temporary correction only for the patient to return to the formerly mentioned poor posture. We know that balance is affected by alignment of our trunk and spine. 1 Everyone needs to avoid falls but it’s particularly important with osteoporosis patients due to bone fragility.
 We want our patients not only to move, but to move with optimal alignment. According to Fritz, et al 2 in the vhitepaper: “Walking Speed: The Sixth Vital Sign”, walking is a complex functional activity. Our ability to influence motor control, muscle performance, sensory and perceptual function, endurance and habitual activity level can result in a more efficient and safer gait.
We want our patients not only to move, but to move with optimal alignment. According to Fritz, et al 2 in the vhitepaper: “Walking Speed: The Sixth Vital Sign”, walking is a complex functional activity. Our ability to influence motor control, muscle performance, sensory and perceptual function, endurance and habitual activity level can result in a more efficient and safer gait.
Visual imagery cuing had been popular in the sports world for decades. By changing one or two words, physical performance has been shown to improve. 3 In a study involving standing long jump, Wu et al instructed undergraduate students to either “Jump as far as you can and think about extending your legs” (internal focus) or “Jump as far as you can and think about jumping as close to the green target as possible” (external focus). The external focus group jumped 10% farther. Lohse et al 4 and Zachry et al 5 surmised that an external focus reduces the "noise" in the motor system which affects muscular tension and optimal function.
It Starts with Posture
Before you can expect your patients to walk well, they have to stand well- stability before mobility. Assess their posture from all angles and determine where to start. One visual image may change a host of problems. A common postural fault, “slumping” is seen as forward head, increased thoracic kyphosis accompanied with either lumbar hyper or hypo lordosis. Your goal is to get the optimal alignment image that you have in your mind……. into their body.
Most people think in pictures rather than words. 6 Yet the medical industry uses words to communicate. Often we say, “Don’t slouch. Don’t look down.” Telling your patient what not to do is not helpful. Our brain hears the words, “Slouch or look down.” We don’t discern the negative. If I say to you, “Don’t think of a pink elephant,” what does your mind see? How can you not see a pink elephant?
Below are five common visual cues to improve a patient’s posture in standing and walking. These tend to follow the Pareto Principle. 20% of your cues work 80% of the time.
- “In standing, imagine a bungee cord running from the top of your head to the ceiling. Visualize a mother cat lifting her kitten up by the scruff of the neck.”
- “When breathing, imagine an umbrella inside your ribcage, opening up upon inhale, and closing on exhale. Breathe in all directions including into the back of your lungs as if you were filling up the sails of a sailboat.”
- “When walking, widen your collarbones as if they were arrows, shooting off the tips of your shoulders. Imagine your head is a floating balloon, gliding along above your shoulders.”
- “Pretend you are the King (or Queen) of England as you walk among your subjects. “
- “Slide your shoulder blades down toward your opposite hip pockets.”
Choose a cue and instruct your patient. Observe changes in posture, alignment, efficiency of movement, or length of step during gait. Ask your patient for feedback. “What did you notice?” Certain cues resonate more than others. Give them variety and options. The best cues are the ones they create themselves. When a patient says, “You mean like………..?” you know it’s a great cue for them. They have an intuitive understanding and relate to it which translates into their body. A patient’s response to the bungee cord cue was, “You mean like a Christmas ornament hanging from the tree?” My response? Absolutely!
While some visual cues may seem too flowery or not “medical” enough, the research is solid the impact powerful. Plus your patients love it! Visual cues are sticky. They help remind us when we’re out in the real world. Isn’t that the ultimate goal – helping patients become independent in their pursuit of health and safety?
1. Shiro Imagam, et all. Influence of spinal sagittal alignment, body balance, muscle strength, and physical ability on falling of middle-aged and elderly males. Eur Spine J. 2013 Jun;
2. Fritz S. et al White Paper: “Walking Speed: The Sixth Vital Sign” J Geriatr Phys Ther. 2009
3. Wu, et al Effect of Attentional Focus Strategies on Peak Force and Performance in the Standing Long Jump. Joun of Strength and Conditioning Research 2012
4. Lohse and Sherwood Defining the Focus of Attention: Effects of Attention on Perceived Exertion and Fatigue
5. Zachry, T et al. Increased Movement Accuracy and Reduced EMG Activity as a Result of Adopting an External Focus of Attention. Brain Research Bulletin Oct 2005
6. Dynamic Alignment Through Imagery. Franklin, Eric. Second Edition, 2012
Do you work with osteoporosis patients? This may be a trick question because you probably do whether you know it or not- even if you are a pediatric therapist! Osteoporosis is defined by the World Health Organization1 as a systematic skeletal disease characterized by:
- Low bone mass
- Micro-architectural deterioration of bone tissue
- Consequent increase in bone fragility and susceptibility to a fracture
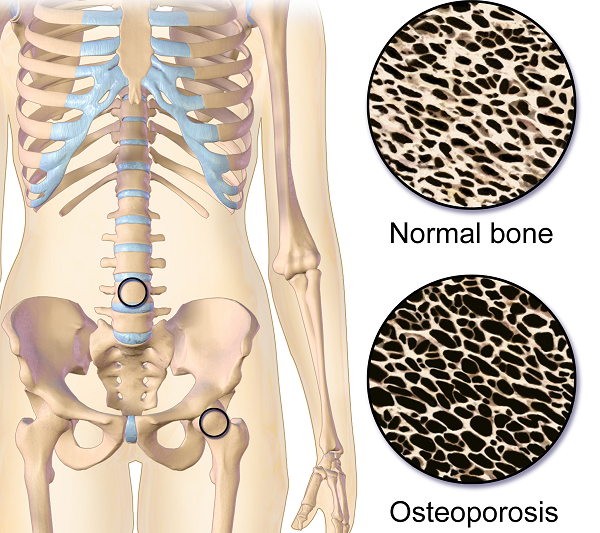 Osteoporosis occurs in men, women and even children. It is sometimes called the “silent disease” because often people don’t know they have it until they break a bone. And even then, compression fractures are painful only 20-30% of the time. Old fractures are often found on x-rays when a person is imaged for illnesses such as pneumonia. According to the National Osteoporosis Foundation2, about one in two women and one in four men over the age of 50 will suffer a fracture due to bone fragility. At this point in time, it is estimated 80% of patients entering Emergency Departments with a fragility fracture (a fall from a standing height) are never followed up for care.
Osteoporosis occurs in men, women and even children. It is sometimes called the “silent disease” because often people don’t know they have it until they break a bone. And even then, compression fractures are painful only 20-30% of the time. Old fractures are often found on x-rays when a person is imaged for illnesses such as pneumonia. According to the National Osteoporosis Foundation2, about one in two women and one in four men over the age of 50 will suffer a fracture due to bone fragility. At this point in time, it is estimated 80% of patients entering Emergency Departments with a fragility fracture (a fall from a standing height) are never followed up for care.
As therapists, we see patients for a variety of diagnoses with co-morbidities but osteoporosis may not be listed. This could be because they have never been identified. We are in a prime position to screen for signs associated with the disorder. Below are the top 3 signs to look for:
- History of fracture from minimal trauma (fall from a standing height, sneeze, lifting groceries, etc.) The typical fracture areas are wrist, hip, and spine although fragility fractures can happen anywhere in the body.
- Hyper-kyphosis. Note, I said hyper-kyphosis, not kyphosis. We are meant to have a thoracic kyphosis but an excessive curve, particularly when it hinges around T8 area may indicate a collapse of the anterior portion of the vertebral bodies. This is the pie shaped wedging seen on x-rays and further increases the stress on the anterior aspect of the spine. Observe your patients’ sagittal posture for proper alignment.
- Loss of height. Ask your patient their tallest height remembered; then measure them. A loss of 4 cm (1.5 inches) or more may indicate fractures in the spine.
Remember pain may or may not accompany a compression fracture. Patients may complain of a “catch” or muscle spasm or nothing at all. These quick and simple screens can alert the healthcare provider and may help prevent further disintegration of the bones. Research is showing that not only weight bearing exercises but a site specific back and hip strengthening program decreases the risk of fracture.3
1. World Health Organization. www.who.int
2. National Osteoporosis Foundation. www.nof.org
3. Current Osteoporosis Reports. Sept, 2010. The Role of Exercise in the Treatment of Osteoporosis. Sinaki M, Pfeifer M, Preisinger E, Itoi E, Rissoli R, Boonen S, Geusens P, Minne HW.
Childbirth fear is associated with lower labor pain tolerance and worse postpartum adjustment.1,2 In addition, psychological distress during pregnancy is associated with adverse consequences in offspring, including detrimental birth outcomes, long-term defects in cognitive development, behavioral problems during childhood and high levels of stress-related hormones.3 These negative consequences of fear and stress during pregnancy have inspired both interest and research into the role of mindfulness training during pregnancy to reduce fear and stress and improve outcomes.
In a randomized controlled trial, first-time mothers in the late 3rd trimester of pregnancy were randomized to attend either a 2.5-day mindfulness-based childbirth preparation course offered as a weekend workshop or a standard childbirth preparation course with no mind-body focus.4 Participants completed self-report assessments pre-intervention, post-intervention, and post-birth, and medical record data were collected. Compared to standard childbirth education, those in the mindfulness-based workshop showed greater childbirth self-efficacy and mindful body awareness, reduced pain catastrophizing and lower post-course depression symptoms that were maintained through postpartum follow-up. Participants in the mindfulness workshop also demonstrated a trend toward a lower rate of opioid analgesia use in labor.
In a qualitative study, researchers conducted in-depth interviews at four to six months postpartum with ten mothers at increased risk of perinatal stress, anxiety and depression and six fathers who had participated in a Mindfulness Based Childbirth and Parenting Program (MBCP).5 The MBCP program integrates mindfulness training into childbirth education. Participants meet for eight 2 hour and 15 minute weekly sessions and a reunion after babies are born. Specific mindfulness practices introduced include body scan, mindful movement, sitting meditation and walking meditation. Also, methods to integrate mindfulness into pain management, parenting and activities of daily living are introduced. Participants are asked to practice at home for 30 min per day in between sessions supported by audio guided instructions and informative texts.
Participants in the MBCP Program described gaining new skills for coping with stress, anxiety and pain, as well as developing insight and self-compassion and improving communication. Participants attributed these improvements to an increased ability to focus and gain a wider perspective as well as adopt attitudes of curiosity, non-judging and acceptance. In addition, they described mindfulness training to be helpful for coping with childbirth and parenting, including breastfeeding troubles, sleep deprivation and stressful moments with the baby.
These findings demonstrate potential therapeutic outcomes of integrating mindfulness training into childbirth preparation. Although this is a young field and more research is warranted, there is substantial research demonstrating mindfulness training improves stress management, pain management and decreases physiological markers of stress in a wide range of patient populations.6, 7 While the interventions in the above two studies introduce mindfulness in a group format, I have also found that patients can greatly benefit from being taught mindful principles and practices in one-on-one treatment sessions.
Carolyn will share her over-30 years of training and experience teaching mindfulness to patients both individually and in group settings in her course, Mindfulness-Based Pain Treatment, coming up on October 26 and 27 in Houston, TX. Participants will return to the clinic with skills to not only help patients, but to also help themselves be less stressed, more mindful providers!
1. Alehagen S, Wijma K, Wijma B. Fear during labor. Acta Obstet Gynecol Scand. 2001;80(4): 315–320.
2. Laursen M, Johansen C, Hedegaard M. Fear of childbirth and risk for birth complications in nulliparous women in the Danish national birth cohort. Br J Obstet Gynaecol. 2009:116(10): 1350–1355.
3. Isgut M, Smith AK, Reimann. The impact of psychological distress during pregnancy on the developing fetus: Biological mechanisms and potential benefits of mindfulness interventions. J Perinat Med. 2017 Dec 20;45(9):999-1011.
4. Duncan LG, Cohn MA, Chao MT. The benefits of preparing for childbirth with mindfulness training: a randomized controlled trial with an active comparison. BMC Pregnancy Childbirth. 2017. May 12;17(1):140.
5. Lonnberg G, Nissen E, Niemi M. What is learned from Mindfulness-Based Childbirth and Parenting Education? – Participants’ experiences. BMC Pregnancy Childbirth. 2018; 18: 466.
6. Hilton L, Hempel S, Ewing BA, et al. Mindfulness meditation for chronic pain: Systematic review and meta-analysis. Ann Behav Med. 2017;51(2):199-213.
7. Pascoe MC, Thompson DR, Jenkins ZM, Ski CF. Mindfulness mediates the physiological markers of stress: Systematic review and meta-analysis. J Psychiatr Res. 2017;95:156-78.
As more and more patients seek care for pelvic floor dysfunction, the need for more qualified practitioners is becoming apparent. Many patients prefer to see a clinician who they identify with, which is why it is important for practitioners of all genders to learn to treat pelvic floor dysfunction. Because much of the public's awareness of pelvic rehab comes out of women's health, the vast majority of pelvic health practitioners are women.
There is currently a shortage of male pelvic health practitioners. To help us understand why it is so important to fix that, we reached out to several male clinicians who have attended the Male Pelvic Floor: Function, Dysfunction, and Treatment course to ask them about the need for more men in the field. Here are some answers to the question:
“Why is it important to have male providers available to treat male patients in the field of pelvic health?”
Grant Headley of Bridgetown Physical Therapy of Portland, Oregon (www.bridgetownpt.com)
While as PT’s we all approach our patients with interest in helping them as individuals, some of our patients feel more comfortable sharing certain details with a provider of the same gender. Many of the hang-ups some men have about receiving care from a female provider are related to an older generation, to certain traditional or religious cultural beliefs, or to certain beliefs about propriety related to receiving care.
As acknowledged in our coursework, generally men have cultural barriers that traditionally do not permit sharing of vulnerability or weakness, especially in the sexual domain. Here are a few unsolicited statements I feel encapsulate what my own male patients have told me: Some heterosexual men feel more comfortable sharing the details of their dysfunction with a man because they find it difficult to admit vulnerability in the presence of a female. Some men prefer not to relay the clinically pertinent details of dysfunctional sexual encounters with a female because they do not wish to make the female practitioner uncomfortable. Many men feel that they can relay more detail about the mechanics of the sexual dysfunction or signs of improvement to a male provider. Some men have told me that they felt their sexual dysfunction was minimized or that they have been treated with patronizing language by a female pelvic PT in the past. Unfortunately, these patients attribute this negative experience to the PT being female, and they are not comfortable having a second opinion with a female.
 Although we strive to present as open-minded and neutral to our patients, they may have an affinity for a male provider. This could foster a more constructive clinical partnership towards working on their goals if they perceive fewer communication barriers. I can offer my own experience as a past patient suffering with pelvic floor dysfunction; I was so desperate for help and I felt so grateful that there was a physical therapist in my city at all that was willing to help me. I did not care that she was female and that I had to receive treatment at a women's health clinic for new mothers in the University Hospital. Many female therapists reading this article have likely transferred lifesaving PT care to scores of men. This organization of H&W that does so much good for a sensitive aspect of men's care is dominated by women- this needs to be acknowledged as a net positive but also appreciated that much of the education and application of care is an adaptation from what has worked for women in the past. Many men will be so grateful to receive care and get better. Some men unfortunately will have barriers to receiving care and for those patients, we can seek out and encourage our male colleagues to get involved in pelvic rehab so we can all provide more access to care.
Although we strive to present as open-minded and neutral to our patients, they may have an affinity for a male provider. This could foster a more constructive clinical partnership towards working on their goals if they perceive fewer communication barriers. I can offer my own experience as a past patient suffering with pelvic floor dysfunction; I was so desperate for help and I felt so grateful that there was a physical therapist in my city at all that was willing to help me. I did not care that she was female and that I had to receive treatment at a women's health clinic for new mothers in the University Hospital. Many female therapists reading this article have likely transferred lifesaving PT care to scores of men. This organization of H&W that does so much good for a sensitive aspect of men's care is dominated by women- this needs to be acknowledged as a net positive but also appreciated that much of the education and application of care is an adaptation from what has worked for women in the past. Many men will be so grateful to receive care and get better. Some men unfortunately will have barriers to receiving care and for those patients, we can seek out and encourage our male colleagues to get involved in pelvic rehab so we can all provide more access to care.
Lance Frank of Flex Physical Therapy in Atlanta (www.flexptatl.com)
Personally, as a male provider in pelvic health, I find that the men I treat are much more comfortable and at ease discussing topics like erections (or lack thereof) and sexual dysfunction, as well as incontinence, or pelvic pain. In a female dominated sub-specialty of physical therapy, sometimes as a male it can be intimidating and even embarrassing for some men to discuss these topics at all, let alone with a female; so having the option to speak and be treated by another male who may better understand the changes, anatomy, and problems they’re experiencing may feel a bit less daunting. Our culture has made male masculinity fragile and I think some populations of men who need pelvic floor rehab may feel embarrassed to be treated by a female clinician if their perception of being seen by a female is emasculating. Ultimately, I think there needs to be more men in this field because there needs to be better visibility of male pelvic health providers in general, as well as better representation of men acknowledging that male pelvic floor disorders exist and are willing and able to treat them.
Eddie Gordon of Flow Rehab in Seattle (www.flowrehab.com)
There are far fewer male physiotherapists treating men with pelvic floor dysfunctions, but I am hopeful this will change for the better. Lack of access to male pelvic physios is a relative barrier to care because some men are more comfortable seeing a male pelvic provider the same way most women would prefer seeing a female pelvic physio. In general, men do not typically seek treatment as frequently or early enough the way most women do. If male pelvic physios are not available, then men may more likely delay treatment, which could potentially worsen their problem. Ironically, when it comes to men with pelvic floor dysfunctions, men are underrepresented, but I am hopeful that more male PT’s will be joining the movement to educate the male population.
Milan Patel of Comprehensive Therapy Services in San Diego (comprehensivetherapy.com)
I believe it's important to have male providers in the pelvic health field for many reasons, one being the opportunity for connection. I think we connect best with reflections of ourselves and for men seeking out a pelvic health provider that can be hard to find. In my experience, pelvic physical therapy works best when your patient can be open and honest, and establishing a strong connection between therapist and patient is the first step. Another reason is that people should have options for the provider they want. In San Diego I am the only male pelvic physical therapy provider which means most men seeking pelvic floor therapy have no choice but to see a female. If you switched the genders in the last sentence you could see how that is problematic. Many women prefer to have their pelvic PT be a female, I just think guys should get the same choice.
Steven Lavender of The Physical Therapy Practice NYC in New York (thephysicaltherapypractice.nyc)
In my experience as a gay male practitioner practicing pelvic floor physio on only men:
Gay male patients usually prefer a gay provider because they feel like they don’t have to explain lifestyle issues and choices, they may be unused to being touched by women, and maybe misogynistic.
Some straight men have told me that they think a male practitioner would know more about their pelvic issues than a woman. Some men don’t think women are strong enough nor have long enough fingers to get to the places they need to be. Some straight men report they might be attracted to a female therapist and get an erection or feel embarrassed about appearing unmanly with their particular pelvic condition.
For some men being touched by a woman is a religious issue so many males of the Jewish and Muslim faiths prefer to see a male practitioner.
Some men could not care less who sees them as long as they get better.
One woman called me for advice or for an appointment from some distance because they "figured a gay man in New York City just might know more about my ass and ass pain than any local jack-assed doctor in my neck of the woods." True story.
If you are interested in learning to treat male patients, the Male Pelvic Floor: Function, Dysfunction, and Treatment course is a great place to start! The course is taking place twice more in 2019, this September 13-15, 2019 in Pasadena, CA, and again in Fort Myers, FL on October 19-21, 2019. We are already booked four times in 2020 as well, so be sure to check out the full course schedule for all available dates.
In the United States, estimated direct medical costs for outpatient visits for chronic pelvic pain (CPP) is more than $2.8 billion per year.1 In a 2017 study in the Clinical Journal of Pain by Sanses et al, a detailed musculoskeletal exam of clients with CPP can assist both physicians as well as physical therapists in differential diagnosis and appropriate referrals for this population.
Evaluating a client with pelvic pain requires a skill set that includes direct pelvic floor as well as musculoskeletal test item clusters. The prioritization of which depends upon many factors including clinician discipline, experience, specialty vs. general setting, as well as client history, presentation and goals. In addition to the direct pelvic floor assessment, there are additional key musculoskeletal screening tests that are an essential part of a pelvic pain assessment. New this year, my course Finding the Driver in Pelvic Pain will incorporate the use of Real Time Ultrasound in neuromuscular assessment and re-education of the pelvic floor and abdominal wall during the Sunday morning lab session.
Peery et al (2012) noted that abdominal pain was one of the most common presenting reasons for an outpatient physician visit in the United States. Abdominal pain is one of the many complaints that our clients may report requiring differential diagnosis including urogynecologic, colorectal, musculoskeletal, visceral or neurogenic causes. Lower abdominal quadrant pain may denote serious emergent pathology. Clinical findings, physical exam and client symptoms in addition to smart differential diagnosis must be used to determine if the abdominal pain is musculoskeletal in nature. Direct access requires physical therapists to perform a skilled initial screening for abdominal pain in order to determine if it is abdominal wall versus a visceral origin. Physicians are fluent in ruling out emergent pathology but may not be familiar with musculoskeletal tests for non-emergent pathology. Assessment of bowel and bladder function and habits are essential to perform. This blog specifically addresses three physical exam tests that can be performed as part of abdominal wall pain screening. According to Cartwright et al, the location of the abdominal pain should drive the evaluation.
Carnett’s test is a simple clinical test that assesses abdominal pain response when a client tenses their abdominal muscles. A positive Carnett’s sign denotes the origin of symptoms within the abdominal wall with a negative tests suggesting intra-abdominal pathology. The test is performed in supine, the clinician gently palpating the area of abdominal pain and has the client lift their head and shoulders off the table. Conditions such as myofascial trigger points, scar and muscular pain would be flared with palpation of the contractile tissue with activation of the abdominal wall muscles. If the pain is due to visceral origin, appendicitis for example, the pain would remain unchanged with palpation with head lift. Although some perform Carnett’s test by lifting both legs off the table, this method may cause unnecessary pain in clients with poor lumbopelvic control. (Figure 1) The head and shoulder lift option is felt to be comparable method of performing Carnett’s test.
Blumberg’s sign is most commonly used to rule in appendicitis, peritonitis or a visceral driver of right lower quadrant pain. The test is performed by the clinician applying deep pressure over McBurney’s point (Figure 2) with an abrupt and rapid release of pressure. Although there are anatomical variations in appendix location, pain reproduction is consistent with a positive test and immediate referral to the ER is indicated.
Thoracic dysfunction, including disc herniation, can result in abdominal pain.2 In thoracic discogenic driven abdominal pain, symptoms would likely be exacerbated by coughing, sneezing, spinal flexion and activities that would increase spinal loading. A simple screening for this is seated thoracic traction. If the client reports reduction or resolution of symptoms with traction, further musculoskeletal tests including regional movement and PIVM testing could be implemented to rule in or rule out need for diagnostic imaging.
In the Herman Wallace course “Finding the Driver in Pelvic Pain” participants learn a comprehensive musculoskeletal screen including abdominal, neural mobility and conductivity, pelvic ring, pelvic floor and biomechanical contributing factors to pelvic pain. Evidence based test item clusters are defined, along with their diagnostic accuracy, for all associated systems in order to outline a comprehensive screen for pelvic pain clients. To learn more about musculoskeletal screening for pelvic pain, check out faculty member Elizabeth Hampton PT, DPT, WCS, PRPC, BCB-PMD’s course Finding the Driver of Pelvic Pain, which is next offered Jun 28, 2019 - Jun 30, 2019 in Columbus, Ohio. We are fortunate to have Dick Poore, President of The Prometheus Group present on Sunday June 30th for technical support for the Real Time Ultrasound portion of the course.
1. Sanses et al. "The Pelvis and Beyond: Musculoskeletal Tender Points in Women with Chronic Pelvic Pain". Clin. J. Pain. 2016 Aug. doi: 10.1097/AJP.0000000000000307
2. Papadakos et al. "Thoracic Disc Prolapse Presenting with Abdominal Pain: Case Report and Review of the Literature". Ann. R. Coll. Surg. Engl. 20019 Jul. doi: 10.1308/147870809X401038
Earlier diagnosis is clearly a huge need for patients with pelvic floor dysfunction. Many patients suffer with their symptoms for years before even hearing the words “pelvic floor,” or realizing that a pelvic floor physical therapist may be able to help. For interstitial cystitis, one large survey article found fewer than 10% of patients with the condition had been correctly diagnosed with IC, even after years of symptoms and visits with multiple doctors.
Even after being diagnosed, patients still don’t learn about how the pelvic floor can be causing or exacerbating their symptoms. In one study of our interstitial cystitis patients, 46% learned about the importance of the pelvic floor on their own and sought out treatment independently, while nearly half felt they were referred by their physician to physical therapy far too late, as a ‘last resort.’ This is despite the fact that many of these patients had seen five or more physicians and physical therapy is considered the most proven treatment for IC by the American Urological Association.
Physicians, orthopedic physical therapists, other practitioners, and patients themselves need a simple, proven way to identify pelvic floor dysfunction to help patients find pelvic floor physical therapy earlier in their medical journey.
In a large survey of our patients with confirmed pelvic floor dysfunction, we examined what symptoms and medical history was most closely correlated with pelvic floor dysfunction. Any screening questionnaire would ideally be able to identify a wide variety of pelvic floor dysfunction, including patients with chronic pelvic pain, pelvic organ prolapse, orthopedic pain with a pelvic floor component (low back, hip, groin), urinary urgency/frequency, and/or bowel dysfunction.
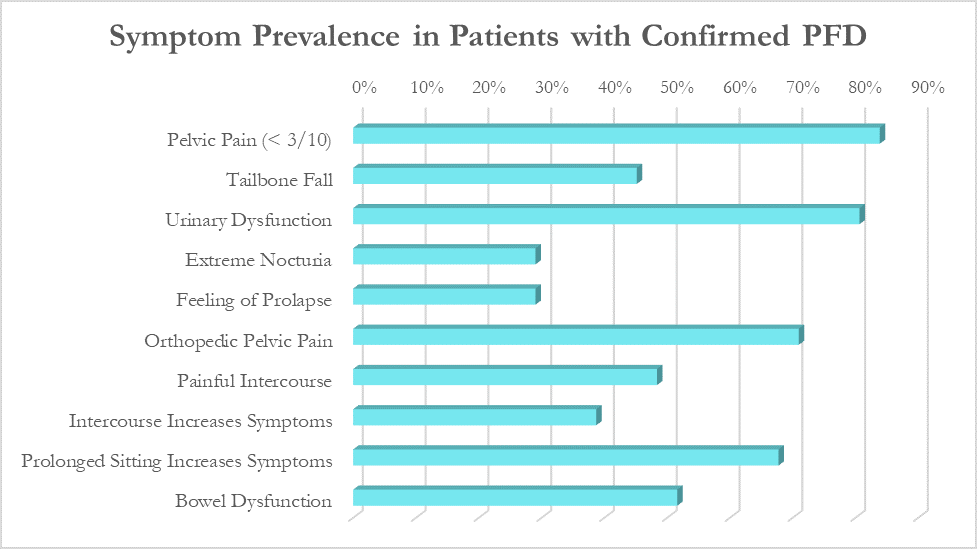
While these patients all had different medical diagnoses, many symptoms were common across the patient population. The most common were pelvic pain (84%), urinary urgency, frequency, or incontinence (81%), orthopedic pelvic pain (71%) and symptoms that worsen with prolonged sitting (68%).
Based on the survey results, we created the Cozean Pelvic Dysfunction Screening Protocol to screen for pelvic floor dysfunction and published the results in the International Pelvic Pain Society (2017). The goal was to correctly identify more than 80% of the patients with pelvic floor dysfunction (sensitivity). For ease of use by both practitioners and patients, the questions were phrased so they could be answered with a simple ‘yes/no’ (as a check box). If patients answers ‘yes’ to 3 or more of the questions, pelvic floor dysfunction is highly likely.
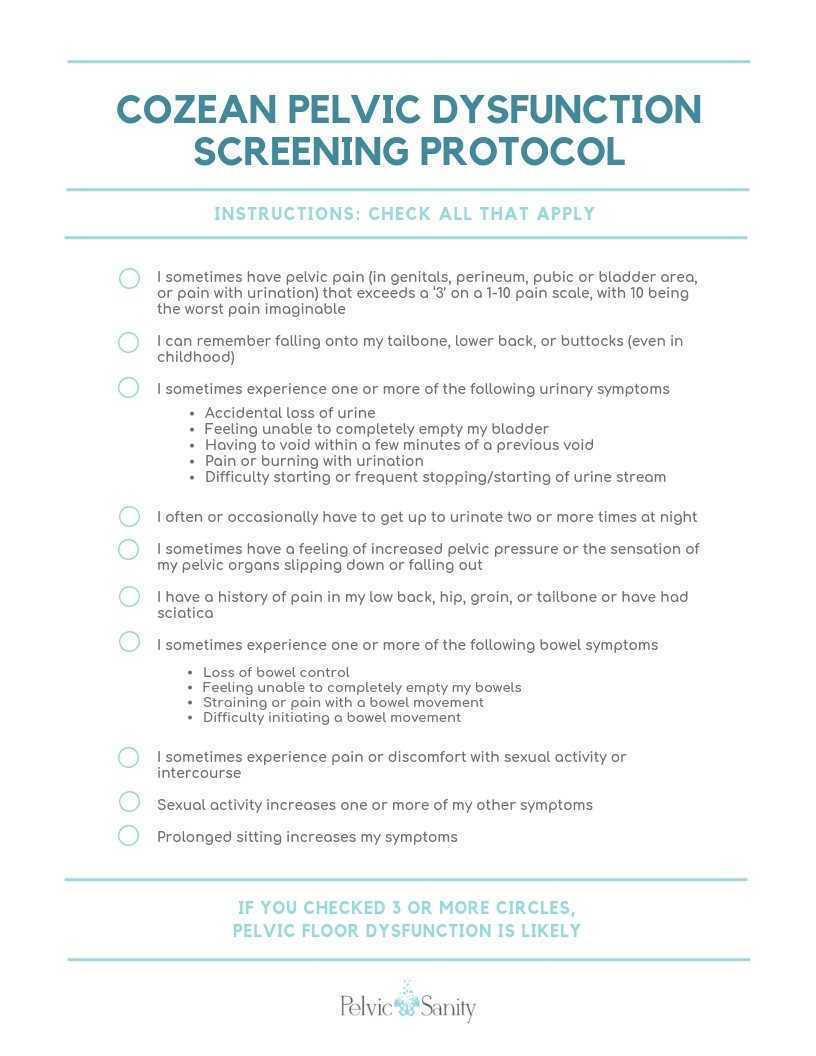 Document available for download at https://docs.wixstatic.com/ugd/d1026c_42a0fda8e5644930950d754619586614.pdf
Document available for download at https://docs.wixstatic.com/ugd/d1026c_42a0fda8e5644930950d754619586614.pdf
Testing the Model
In a model like this, we would expect a normal (bell-shaped) distribution curve of answers from patients with pelvic floor dysfunction. Some patients will score on the high end, others on the low, and the majority would be clustered in the middle. This is what we observe with use of the questionnaire, as seen by the trendline in the blow graph. Most patients with confirmed pelvic floor dysfunction cluster in scores between 3 and 7, with a few scoring at 8 or higher. Less than one out of ten patients with pelvic floor dysfunction score below a 2 on the questionnaire and would not be captured by this measure.
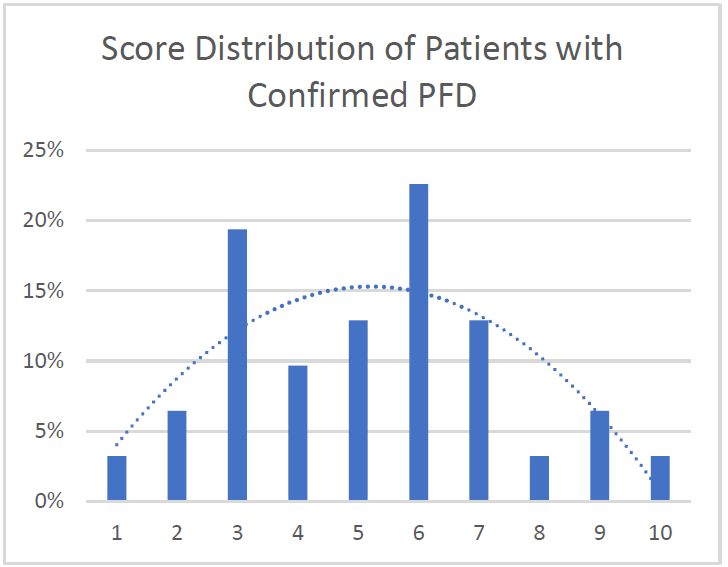
Specificity: 91%. More than 90% of patients with confirmed pelvic floor dysfunction were correctly identified by this screening protocol. Additional testing is required on a general population without PFD to determine the specificity of the questionnaire.
Average: 5.2. Of patients with confirmed PFD, the average score according to this screening protocol was 5.2 with a median score of 5 and a mode of 6. This is in line with what would be expected with a normal distribution curve.
We hope this 10-question survey is able to help patients with pelvic floor dysfunction be diagnosed earlier - whether by their physician, other physical therapists, or themselves – and seek pelvic floor physical therapy earlier in their medical journey. Please feel free to use the printable version of this protocol with your patients or in working with local practitioners.
Nicole Cozean will be teaching the course Interstitial Cystitis: Holistic Evaluation and Treatment in Princeton, NJ from April 6-7, 2019.
 Nicole Cozean is the founder of PelvicSanity physical therapy, in Orange County, California. Nicole was named the 2017 PT of the Year, is the first physical therapist to serve on the ICA Board of Directors, and is the award-winning and best-selling book The Interstitial Cystitis Solution (2016). She is an adjunct professor at her alma mater, Chapman University and teaches continuing education courses through the prestigious Herman & Wallace Institute.
Nicole Cozean is the founder of PelvicSanity physical therapy, in Orange County, California. Nicole was named the 2017 PT of the Year, is the first physical therapist to serve on the ICA Board of Directors, and is the award-winning and best-selling book The Interstitial Cystitis Solution (2016). She is an adjunct professor at her alma mater, Chapman University and teaches continuing education courses through the prestigious Herman & Wallace Institute.
I’m Elizabeth Hampton PT, DPT, WCS, BCB-PMD and I teach “Finding the Driver in Pelvic Pain”, which offers practitioners a systematic screening approach to rule in or rule out contributing factors to pelvic pain. This course helps clinicians to understand and screen for the common co-morbidities associated with pelvic floor dysfunction, like labral tears, discogenic low back pain, nerve entrapments, coccygeal dysfunction, and more. Importantly, it also coaches clinicians to organize information in a way that enables them to prioritize interventions in complex cases. I've noticed that there are some questions that course participants frequently have as they talk through common themes in their care challenges and wrote this blog to share some clinical pearls you may find to be helpful for your own practice or as an explanation to your clients.
Here are some of the most common questions that I get when teaching Finding the Driver in Pelvic Pain:
1) Question: How do I even start to organize information when a client has a complex history and I am feeling overwhelmed?
I write down a road map with key categories: Bowel and bladder; Spine; Sacroiliac Joint/Pubic Symphysis; Hip; Pelvic floor muscles; biomechanics; respiration; neural upregulation; whatever details can be fit into ‘big buckets’ of information. I use it to both organize my thoughts for my notes, as well as educate the client as to what my findings are and the design of their treatment program.
2) Question: How do you get your clients to do a bowel and bladder diary?
I am proud to say that I can talk anyone into a 7 day bowel and bladder diary because I tell them how incredibly helpful it is to understand the way their body responds to what they eat, drink, and daily habits. It’s my secret weapon to snag clients to start connecting with their body and listening to their details, educate about defecation ergonomics and what happens in multiple systems when there is pelvic floor overactivity. It’s a great teaching tool that facilitates self-reflection and how their self-care choices impact their body’s behavior.
3) Question: How do you educate clients about pelvic floor function so they don’t focus so much on Kegels?
Pelvic floor muscles do three things:
-
They contract gently, or powerfully, with no discomfort, and totally normal breathing; PFMs should have the same kind of nuanced control like your voice does: they should be able to do a gentle contraction, like a “whisper” or a powerful contraction, like a “shout”, depending on the task position and intent.
-
They relax fully and completely when the body is resting in support, or they should be able to relax to a supportive level when they are needed posturally. Relaxation should be its own celebrated event!
-
They should be able to relax and gently lengthen.
Faculty member Elizabeth Hampton PT, DPT, WCS, BCB-PMD is the author and instructor of Finding the Driver in Pelvic Pain, a course designed to help practitioners utilize differential diagnosis in evaluating pain. Join Dr. Hampton in Portland, OR on July 27-29, 2018 or November 2-4, 2018 in Phoenix, AZ.
Dr. Nicole Cozean was just awarded the IC/BPS Physical Therapist of the Year by the IC Network, one of the largest patient advocacy groups for interstitial cystitis! Today she shares her treatment approach for this complex dysfunction. Join Dr. Cozean in San Diego on April 28-29, 2018 to learn everything there is to know about interstitial cystitis.
Interstitial cystitis (IC) is a chronic pelvic pain condition characterized by pelvic pain and urinary urgency/frequency. IC is frequently accompanied by other symptoms1, including painful intercourse, low back or hip pain, nocturia, and suprapubic tenderness.
While pelvic floor physical therapy is the most proven treatment for interstitial cystitis, most patients require a multi-disciplinary approach for optimal results. The majority are forced to develop this holistic approach on their own, but one of the most valuable things a physical therapist can provide is assistance in creating their own unique treatment plan. The American Urological Association has released treatment guidelines for interstitial cystitis, and potential treatments fall into several different categories. It is important to note that most treatments aren’t effective for the majority of patients, so a trial-and-error approach is needed to find the right balance for each patient. Tracking symptoms with a weekly symptom log can be a powerful tool to optimize the individual treatment plan.

Summary of the AUA Guidelines for IC – Download Here
Oral Medications
Oral medications are primarily used to reduce pain.Anti-depressants can dampen the nervous system, decreasing the severity of pain reported. Anti-histamines have also been shown to be effective in reducing the pain and symptoms of interstitial cystitis, perhaps because of their ability to reduce inflammation and break the cycle of dysfunction-inflammation-pain (the DIP cycle). Some patients require opioid painkillers for adequate pain control.
Urinary tract analgesics can provide temporary pain relief for some patients, but cannot be taken consistently because they thicken the urine and strain the kidneys. Some patients find success using these medications (Azo, Pyridium, Uribel) during severe pain flares.
The only FDA-approved oral treatment for interstitial cystitis is Pentosan Polysulfate (PPS, Elmiron®). This is commonly prescribed to patients after an IC diagnosis, but has been shown to be effective in only 28-32% of patients. It also requires a long time (often 6-9 months) to build up in the system and take effect, and many patients stop taking the drug before they could see effect because of side effects (including hair loss) or cost. Unfortunately, many patients lose more than a year after their initial diagnosis waiting to see if Elmiron will work for them, when it is unlikely to provide complete relief.
Antibiotics should never be prescribed for IC in the absence of a confirmed infection.
Bladder and Medical Procedures
Bladder instillations deliver numbing medication directly to the bladder through a catheter and can provide temporary pain relief for some patients. If these are effective, they typically are repeated at least weekly as symptoms return. Some patients don’t tolerate the catheterization well, finding the procedure causes more pain than it prevents. Typical bladder instillations consist of Lidocaine, Heparin, or a combination of the two.
Another route of treatment works by artificially stimulating the nerves the innervate the bladder and pelvic floor.Percutaneous tibial nerve stimulation (PTNS) directs electrical impulses from the ankle up through the pelvic floor. This is an outpatient procedure typically performed weekly for a course of 12 weeks. A more permanent option is implanting a device under the skin of the buttock to target the sacral or pudendal nerve root directly.With this procedure, the patient is given a ‘trial run’ with an external device to see how it performs. If significant improvements are noted, the device can be permanently implanted.
Many patients see marked improvement in their symptoms with a home care program. Deep breathing or meditation can calm the nervous system and reduce the amplifying effect of an upregulated nervous system. A stretching regimen targeting the inner thighs, glutes, abdomen, and pelvic floor can relax muscles and reduce nerve irritation in the region. Self-massage can find and eliminate the trigger points that are causing symptoms. Home tools like a foam roller can address external trigger points, while patients can be taught internal self-release with the help of a tool like the PelviWand or another tool.
Elimination Diet
One of the most common misunderstandings about IC centers on the ‘IC Diet.’ In fact, there’s no such thing. While nearly 90% of IC patients report that diet influences their symptoms in some way, the scope and severity of dietary triggers varies greatly between patients. There are a few common culprits - coffee, tea, citrus fruits, artificial sweeteners, tomatoes, cranberry juice - but no guarantee that a patient will be sensitive to all (or any) of these. Many patients read about an ‘IC Diet’ online after receiving their diagnosis, and are convinced that they need to cut out a huge portion of their diet.
Instead, they should be doing an elimination diet focused on identifying their trigger foods.With this approach, they eliminate most of those common culprits and see how it affects their symptoms.If they notice an improvement, they can gradually add foods back into their diet, one at a time, until they see symptoms increase again. This allows patients to identify their specific trigger foods.
Our advice for IC patients is simple - avoid your trigger foods and eat healthy. It doesn’t have to be any more restrictive than that.
There are also several supplements that have shown benefit for patients, either in clinical trials or anecdotally. Prelief (calcium glycerophospate) is an antacid that may reduce the consequences of eating a trigger food. L-Arginine is a semi-essential amino acid that facilitates blood flow and vasodilation; in clinical trials it was shown to be effective for nearly 50% of patients in reducing pain and urinary symptoms. Aloe Vera pills are used by many patients, and thought to help replenish the bladder’s protective layer. Finally, a combination of supplements known as Cystoprotek is also a common supplement taken by IC patients, combining anti-inflammatory flavonoids with molecules that may reinforce the bladder lining.
Complementary and Alternative Medicine
Acupuncture has been shown to provide relief for pelvic pain patients2, with 73% of men with chronic prostatitis (either identical or closely related to IC) reporting improvement. These men received two treatments weekly for six weeks, focusing around the sacral nerve. Women with pelvic pain and painful intercourse have also reported improvements in pain with 10 sessions of acupuncture3.
Cognitive-Behavioral Therapy (CBT) has been shown to help reduce pain in conditions as diverse as cancer, low back pain, and pelvic pain. In pelvic pain, ten one-hour sessions of CBT was shown to provide significant benefit for nearly half of patients4. Supportive psychotherapy was also shown to have benefits for pelvic pain patients.
A multi-disciplinary approach provides the best results for patients. Physical therapists, who see our patients regularly, can be a great resource in suggesting additional treatment options. The American Urological Association IC Guidelines can be an important resource in guiding patients to other options and developing their unique treatment plan.
Information and Resources
For additional patient resources available for download, feel free to visit The IC Solution page.. In our upcoming course for clinicians treating interstitial cystitis (April 28-29, 2018 in San Diego), we’ll focus on the most important physical therapy techniques for IC, home stretching and self-care programs, and information to guide patients in creating a holistic treatment plan.
1. Cozean, N. "Pelvic Floor Physical Therapy in the Treatment of a Patient with Interstitial Cystitis, Dyspareunia, and Low Back Pain: A Case Report". Journal of Women's Health Physical Therapy. 2017
2. Chen R, Nickel JC. "Acupuncture ameliorates symptoms in men with chronic prostatitis/chronic pelvic pain syndrome"Urology. 2003 Jun;61(6):1156-9; discussion 1159.
3. Schlaeger, J, et al. "Acupuncture for the Treatment of Vulvodynia: A Randomized Wait‐List Controlled Pilot Study". Journal of Sexual Medicine. 30 January 2015. https://doi.org/10.1111/jsm.12830
4. Masheb, et al. "A randomized clinical trial for women with vulvodynia: Cognitive-behavioral therapy vs. supportive psychotherapy". PAIN® Volume 141, Issues 1–2, January 2009, Pages 31-40
I work at University of Chicago and we are in the throes of preparing for a (big T) Trauma Center. But I am physical therapist who works with (little t) traumatized patients- as I treat only pelvic or oncology patients (and usually both).
From the online dictionary: Trauma is 1. A deeply distressing or disturbing experience (little t trauma) or 2. Physical injury (injury, damage, wound) yes- big T Trauma. In my experience, the Trauma creates the trauma and the body responds in characteristically uncharacteristic ways (more on this later).
 People in distress/trauma-affected do not respond rationally or characteristically, so I have learned to respond to distress/trauma in a rational, ethical, legal and caring manner. Always. Every time. To the best of my ability, and without shame or blame.
People in distress/trauma-affected do not respond rationally or characteristically, so I have learned to respond to distress/trauma in a rational, ethical, legal and caring manner. Always. Every time. To the best of my ability, and without shame or blame.
Let’s talk briefly about Trauma Informed Approach
This is a (person), program, institution or system that:
- Realizes the widespread impact of trauma and understands potential paths for recovery
- Recognizes the signs and symptoms of trauma in clients, families, staff and others affected
- Responds by fully integrating knowledge about trauma into policies, procedures and practices
- Seeks to actively resist retraumatization
The Tenets of Trauma Informed Approach
- Safety
- Trustworthiness and transparency
- Peer support
- Collaboration and mutuality
- Empowerment, voice and choice
- Cultural, historical and gender issues
Trauma Specific Interventions
- Survivors need to be respected, informed, supported, connected, and hopeful- in their recovery
- Interrelation between trauma and symptoms of trauma such as substance abuse, eating disorders, depression, anxiety, musculoskeletal presentation, and acute crisis- including suicidal/homicidal ideations (coordination with other service providers)
- Work in a collaborative way with survivors, families and friends of survivor, and other service providers in a way that will empower survivors
Types of trauma are varied but I usually treat survivors of emotional, verbal, sexual and medical trauma. I have even treated patients who felt traumatized by other pelvic floor physical therapists (again, no judgement). Since most of my clinical experience include sexual and medical trauma survivorship, I try to reframe these experiences as potential Post Traumatic Growth, especially when working with my oncology patients. For my pelvic patients who divulge sexual trauma, I don’t dictate or name anything. I allow the survivor to make the rules and definitions. Survivors of sexual trauma need extra care when treating pelvic floor dysfunction.
First, when treating survivors of sexual trauma: expect ‘characteristically uncharacteristic’ events to occur. These include the psychological/somatic effects of passing out, flashbacks, seizures, tremors, dissociation and other mechanisms of coping with the trauma. Have a plan ready for these patients.
Triaging the survivor to assess their needs, when trauma has been verbalized/disclosed:
- Are you safe right now?
- Do you need medical treatment right now?
- What do you need to feel in control of (PT session/immediately after disclosure of trauma)?
- You have choices in your treatment and in your response to trauma.
- I believe you.
- Lastly, is this a situation for mandated reporting?
After assisting the survivor in their journey towards healing, it is imperative that you take care of yourself. Making healthy boundaries (with patients and others), taking time to decompress, creating healthy ritualistic behaviors, mindfulness/relaxation and somatic release (like yoga, massage or working out) is crucial to successfully treating patients who have experienced trauma and who have shared that trauma experience with you.
Because I use gentle yoga for both my trauma survivors’ treatment and for my own self-care, my new course implements evidenced based trauma sensitive yoga. Additionally, modifications for manual therapy are explored. The class is designed to be informative and experiential while integrating the Trauma Informed Approaches of Safety, Trustworthiness and transparency, Peer support, Collaboration and mutuality, Empowerment, voice and choice and Cultural, historical and gender issues.
Join me in Trauma Awareness for the Pelvic Therapist, next available this March in Albany, NY.










































