Since the passing of Title IX in 1972, which protects people from sex discrimination in education or activity programs receiving federal funding, the number of females participating in sports has greatly increased. The National Federation of State High School Associations states that in 2011 nearly 3.2 million girls are participating in high school sports.
Unfortunately, a consequence of this increased participation in sports is a higher prevalence in urinary incontinence (UI) and stress urinary incontinence (SUI) in female athletes. Borin et al looked at the ability of nulliparous female athletes to generate intracavity perineal pressure in comparison to nonathletic women. The study demonstrated that higher mean pressures were generated by nonathletic women in comparison to the athletic women group and that lower perineal pressures in the athletic women were also related to number of games per year and time spent on sport specific workouts and strength training workouts.
UI and SUI are underreported in the general population and also in the athletic population. As health care professionals it is important to screen for UI and SUI in our clients. Physical therapy interventions using pelvic floor muscle rehabilitation have shown to decrease the severity of UI and SUI (Rivalta et al, Hulme). Rivalta used internal methods to improve the function of the pelvic floor muscle. Hulme’s success was achieved through activation of the pelvic floor muscles’ extrinsic synergists.
 |
 |
Pilates is often used in physical therapy as a therapeutic tool to improve lumbar stability with studies showing increases in abdominal strength (Sekendiz), trunk extensor endurance (Sekendiz) and to improve posture (Kloubec). Pilates is often also used in pelvic floor muscle rehabilitation and can easily be modified for low level clients. For example the use of resistance can assist supporting the weight of the leg. Practical proof, while lying supine in neutral lumbar spine position, stretch an arm and a leg away from center, notice the difficulty to maintain neutral spine. Now hold a resistance strap, which is also attached to the foot, and notice how maintaining neutral lumbar spine is easier to maintain (pictured above).
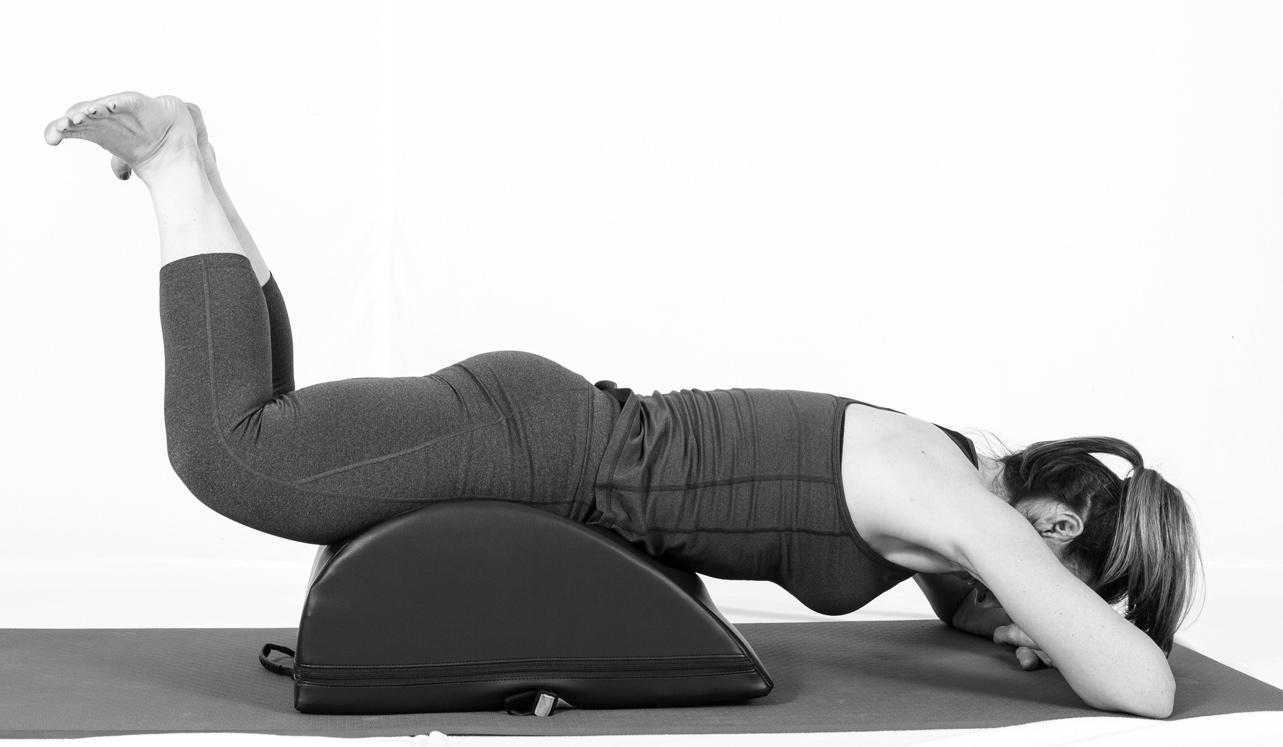
Pilates can also be modified for the higher level client or more athletic client. The use of arc barrels, BOSUs or the Hooked on Pilates MINIMAX (pictured belowy) allow the athletic client to achieve an inverted position, unloading the pelvic floor muscles. In the inverted position, pelvic floor muscles may be activated as intrinsic and/or extrinsic synergists of the pelvic floor muscles are also activated. These types of exercises may be more appealing to the athletic client ensuring continuation of the exercise post discharge from physical therapy.
 |
 |
Borin LC, Nunes FR, Guirro EC. Assessment of pelvic floor muscle pressure in female athletes. PMR. 2013; 5(3):189-193.
Hulme, Janet. Beyond Kegels 3rd edition, 2012 Phoenix Publishing Co. Missoula, Montana
Kloubec JA. Pilates for improvement of muscle endurance, flexibility, balance and posture. J Strength Cond Res. 2010;24:661-667.
Rivalta M, Sughunolfi MC, Micali S, De Stafani S, Torcasio F, Bianchi G, Urinary incontinence and sport. First and preliminary experience with a combined pelvic floor rehabilitation program in three female athletes. Health Care Women Int. 2010;31(5);330-334.
Sekendiz B, Altun O, Korkusuv F, Akin S, Effects of pilates exercise on trunk strength, endurance and flexibility in sedentary adult females. J Bodyw Mov Ther. 2005;9:52-57.
One of the dilemmas for many clinicians new to pelvic rehab is trying to figure out which equipment to purchase, and how to convince their employer (or themselves) to purchase the equipment. A common question in relation to equipment for pelvic rehabilitation is “what do I really need?” In a perfect world, and based on both existing and emerging research as well as clinical practice recommendations, we would all have access to pressure biofeedback and real-time ultrasound to help us document and train our patients in best strategies. The truth, however, lies in the fact that when those devices are not available, clinical practice can gain meaningful information from our best tools: our eyes and our hands. Certainly when completing research about pelvic floor generated pressures we might choose pressure biofeedback, and when looking for muscle activation patterns, needle EMG is the right choice, but no one should deny patients the opportunity to learn how to increase or decrease muscle activity, focus on movement retraining, and learn strategies to decrease improve quality of life and function because the latest technology is unavailable.
 Recent research published in the Brazilian Journal of Physical Therapy helps affirm the value of vaginal palpation in an article that assessed the relationship between vaginal palpation, vaginal squeeze pressure, electromyography and ultrasound. Eighty women between the ages of 18 and 35 years old, who had never given birth, and who had no known pelvic floor dysfunction were given a thorough evaluation using a multitude of evaluative methods. These methods included vaginal digital palpation (using Modified Oxford scale), vaginal squeeze pressure, electromyographic activity, diameter of the bulbocavernosus muscles as well as bladder neck movement using transperineal ultrasound. The muscles were assessed in a supine, hooklying position. A strong and positive correlation was found between pelvic floor muscle function and pelvic floor muscle contraction pressure. A less strong correlation was found between pelvic muscle function and pressure and electromyography and ultrasound.
Recent research published in the Brazilian Journal of Physical Therapy helps affirm the value of vaginal palpation in an article that assessed the relationship between vaginal palpation, vaginal squeeze pressure, electromyography and ultrasound. Eighty women between the ages of 18 and 35 years old, who had never given birth, and who had no known pelvic floor dysfunction were given a thorough evaluation using a multitude of evaluative methods. These methods included vaginal digital palpation (using Modified Oxford scale), vaginal squeeze pressure, electromyographic activity, diameter of the bulbocavernosus muscles as well as bladder neck movement using transperineal ultrasound. The muscles were assessed in a supine, hooklying position. A strong and positive correlation was found between pelvic floor muscle function and pelvic floor muscle contraction pressure. A less strong correlation was found between pelvic muscle function and pressure and electromyography and ultrasound.
Vaginal pelvic muscle assessment via palpation has been shown to be more accurate when assessed by more experienced therapists, and use of multiple methods may be most valuable in gaining the most accurate data. In addition to validating the usefulness of pelvic muscle palpation as an evaluative tool, the authors point out that transperineal ultrasound may also be the most appropriate tool for pediatric patients or patients who are otherwise not appropriate for internal pelvic muscle assessment.
Pereira, V. S., Hirakawa, H. S., Oliveira, A. B., & Driusso, P. (2014). Relationship among vaginal palpation, vaginal squeeze pressure, electromyographic and ultrasonographic variables of female pelvic floor muscles. Brazilian journal of physical therapy, 18(5), 428-434.
Rarely does a patient with sacroiliac joint dysfunction come to see us with a goal of having surgery. Sometimes surgery winds up being the last resort for relief if our efforts and the patient’s commitment to physical therapy and prescribed exercises fail. Some of the most recent research shows positive results from minimally invasive surgery; however, the bottom line is to make sure the most educated, clinically accurate diagnosis has been made in implicating the SI joint as the source of pain.
Capobianco et al (2015) performed a prospective multi-center trial regarding SI joint fusion using a minimally invasive technique in women with post-partum pain in the pelvic girdle. Eligibility for the study required subjects to have 3 out of 5 positive SI joint stress tests and at least 50% relief with image-guided intra-articular SI joint block with a local anesthetic. Of the 172 subjects in the study, 20 of the 100 females had post-partum pelvic girdle pain, and 52 subjects were male. Significant improvements in pain, quality of life, and function were found for not only the post-partum group but all groups 12 months after surgery. Worth noting is one to three weeks after surgery, the subjects engaged in physical therapy, two times per week for six weeks.
Whang et al (2015) assessed the 6-month outcomes of SI joint fusion using triangular titanium implants versus non-surgical management in a prospective randomized controlled trial. Of the 148 subjects chosen based on similar diagnostic criteria as the study mentioned above, 102 underwent surgery, and 46 had non-surgical management. Non-surgical management involved appropriate pain medication administration, physical therapy, intra-articular SI joint steroid injections, and radiofrequency ablation of sacral nerve roots, all based on individual needs. The surgical group subjects in this study were also asked to have physical therapy two times per week for six weeks anywhere from one to three weeks post-op. The results in a six month follow up showed “clinical success” of >80% in the surgical group and <25% in the non-surgical management group.
The Journal of Neurosurgery: Spine presented an article in July 2015 by Zaidi et al with results of a systematic review of literature regarding the surgical and clinical effectiveness of SI joint fusion. The studies included open as well as minimally invasive surgery, and the causes of surgery included SI joint degeneration and arthritis, SIJ dysfunction, postpartum instability, posttraumatic, idiopathic, pathological fractures, and HLA-B27+/rheumatoid arthritis. A mean rate of satisfaction with open surgery was 54%; whereas, the mean was 84% with minimally invasive surgery. Ultimately, the authors concluded, “serious consideration of the cause of pain” is necessary before embarking on SI joint fusion as the evidence for the surgery’s efficacy is lacking.
So, who is responsible for making the definite diagnosis for SI joint dysfunction? As many patients get minimal time in doctor offices, we have a professional responsibility to competently perform a thorough evaluation for our patients. When the diagnosis is “SI joint dysfunction,” rule out the lumbar spine and hip; and, of course, when “low back pain” or “hip pain” fills the diagnosis line, rule out/in the SI joint. If you are confused about how, it is time to consider taking the Sacroiliac Joint Evaluation and Treatment course!
References:
Capobianco, R., Cher, D., & for the SIFI Study Group. (2015). Safety and effectiveness of minimally invasive sacroiliac joint fusion in women with persistent post-partum posterior pelvic girdle pain: 12-month outcomes from a prospective, multi-center trial. SpringerPlus, 4, 570. http://doi.org/10.1186/s40064-015-1359-y
Zaidi, Hasan A., Montoure, Andrew J., and Dickman, Curits A. (2015). Surgical and clinical efficacy of sacroiliac joint fusion: a systematic review of the literature. Journal of Neurosurgery: Spine. (23)1:59-66. DOI: 10.3171/2014.10.SPINE14516
Whang, P., Cher, D., Polly, D., Frank, C., Lockstadt, H., Glaser, J., … Sembrano, J. (2015). Sacroiliac Joint Fusion Using Triangular Titanium Implants vs. Non-Surgical Management: Six-Month Outcomes from a Prospective Randomized Controlled Trial. International Journal of Spine Surgery, 9, 6. http://doi.org/10.14444/2006
The following post comes to us in part from Ginger Garner, PT, ATC, PYT, who teaches three yoga courses for Herman & Wallace; Yoga for Pelvic Pain, Yoga as Medicine for Pregnancy, and Yoga as Medicine for Labor and Postpartum. Check out her poster at the Combined Sections Meeting this weekend in Anaheim!

Maternal health care in the United States is abysmal. Especially wretched is care and support of women post-partum. Our insurance system is partially to blame by dictating that women receive only one visit with the provider who participated in the delivery of their baby 6 weeks after the baby is born, no matter the method of delivery. This is often after most of the scary, unexpected side effects of delivery, like heavy bleeding, nipple pain, urinary incontinence, difficulty with bowel movements, scar pain and tremendous mood swings have begun to ease. Only the women who are the most persistent, or those who have chosen unique care models (like out of hospital births with midwives), seem to get real support post-partum, leaving marginalized and less self-driven women to fend for themselves.
What if research could show that immediately treating some of the side effects of birth, like diastasis recti abdominus, which occurs in 50-60% of post-partum women, could result in improved outcomes in the long run? What if someone could prove that retraining and strengthening the abdominal wall as part of a biopsychosocial model empowering women could change the costly effects of prolapse and urinary incontinence treatment later on in life? What if that research aimed to show that treating women in partnership will all care providers was the most effective? These are big questions, but through research beginning with Diastasis Recti Abdominis (DRA), some Women’s Health Physical Therapists trained in Medical Therapeutic Yoga are hoping to highlight some answers.
At CSM in San Diego next month, these researchers (listed below) are presenting a poster via the Section on Women’s Health showcasing their paper, Diastasis Recti Abdominis: A Narrative Review. They found that good, solid research focusing on the co-morbidities and treatment of DRA is really lacking. Most well-done studies focus on the reliability and validity of measurement techniques, showing that calipers and ultrasound are the most valid and reliable ways to measure the gap. There is not even agreement on what precise measurement technically constitutes a DRA, though most agree that normal inter-recti distance is 15-25mm supraumbilically among parous females with digital calipers. (Chiarello 2013).
Besides the obvious cosmetic and general strengthening concerns, why do we care about physical therapy care for a post-partum DRA? Spitznagle’s retrospective chart review of women presenting for gynecological care with a mean age of 52 found that 52% had DRA and 66% of them had a least one support-related pelvic floor muscle dysfunction. Those with DRA were more likely to have pelvic organ prolapse, urinary incontinence and fecal incontinence. Another study by Parker found a DRA prevalence of 74.4% among women with back or pelvic area pain who had delivered at least one child and sought PT. They found a significant difference in VAS pain levels in those with DRA and abdominal or pelvic pain compared to those without DRA. More well-done, prospective studies are really needed to correlate these sequalea in later life to DRA post-partum.
The topic of how to retrain the abdominal wall to restore optimal function and cosmetic appearance is hot in the blogosphere right now. Does it matter if the width of the diastasis recti is reduced? Or is it a matter of having tension in the linea alba as the clinician sinks his/her fingers toward the spine? Biomechanically we know that in order to improve stiffness in the trunk, we need synergistic and symmetrical firing of the diaphragm, transversus abdominis, multifidus and the pelvic floor with proper timing and contraction of the hip and external abdominal muscles. Benjamin completed a review of the research on the effects of exercise in the antenatal and postnatal periods and concluded that antenatal exercise may be protective against the formation of a DRA, but that the available studies are of such poor quality and varied in the way that abdominal/core strengthening was applied in the post-partum population, that it is impossible to tell how or why exercise may or may not help with DRA!
There is clearly a huge hole in the literature and as usual, new mothers are suffering. Women are spending money on programs they find on the internet that are not backed by solid research, because there is not any! Regarding DRA, post-partum women in our country desperately need well-done, high quality studies promoting a specific and well-described exercise for healing. In addition, in our patriarchal health care model, we need to show without a shadow of a doubt that treating post-partum muscle weakness, body mechanics issues and DRA is essential for saving money in the long run on prolapse and urinary incontinence surgery, as well as decreasing expenditure on back pain treatments.
If our discipline could provide this research, ALL women could have access to personal, post-partum recovery. As an established part of the health care system and with longer treatment times and the chance to get to know our patients better, physical therapists are the IDEAL healthcare practitioners to ensure that post-partum women are getting adequate physical retraining, but also psycho-social support that is so lacking in the United States.
The Women’s Health Poster Presentations at CSM in Anaheim will be on Saturday, Feb 20 from 1-3PM. I look forward to meeting with some of you and visiting about what you are working on to further the cause of improving maternal health care and DRA treatment.
Ginger Garner PT, ATC, PYT, Professional Yoga Therapy Institute, Emerald Isle, NC
Elizabeth Trausch, DPT, PYT Des Moines University, Des Moines IA
Stefanie Foster, PT, PYT Asana with Intelligence, Houston, TX
Paige Raffo, PT, PYT, CPI, Balance+Flow Physio, Bellevue, WA
Janet Drake, PT, LCCE, FACCE, PYT, Central Bucks Physical Therapy, Doylestown, PA
Stacie Razzino, PT, PYT, Free Motion Physical Therapy, Melbourne, FL
Blog post by Libby Trausch, DPT
Spitznagle T, Leong F, Van Dillen L, Prevalence of diastasis recti abdominis in a urogynecological patient population, International Urogynecology Journal. 2007; 18: 321-328.
Chiarello CM, Mcauley JA. Concurrent validity of calipers and ultrasound imaging to measure interrecti distance. Orthop Sports Phys Ther. 2013; 43(7): 495-503
Benjamin DR, et al., Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy. 2014 Mar;100(1):1-8.
The following is a guest post from Nancy Fish, LCSW, MPH who will be presenting at the Alliance for Pelvic Pain Retreat on May 20-22 in Ellenville, NY. Check out this flier to learn more about the retreat.
Gaining a Sense of Hope and Empowerment
Nancy Fish, LCSW, MPH (co-author, with Deborah Coady,M.D. of Healing Painful Sex)
About the Alliance For Pelvic Pain Retreat, May 20-22, 2016, Ellenville, NY
When thinking about registering for the Alliance for Pelvic Pain Patient Retreat, I imagine you are asking yourself “Why would a person suffering from pelvic pain, with more medical appointments than is humanly possible to handle, add another item on an already overwhelming “to do” list?” It would be completely understandable if that is your initial reaction. So why is this retreat a must in your path to physical and emotional healing? There are so many reasons why this retreat can be a life-altering event but I’ll just name a few compelling ones. As a psychotherapist who specializes in pelvic pain (I am also a pelvic pain patient) the primary challenges I hear from most of my clients are:
- “I feel so alone.”
- “This is too embarrassing to talk about with ANYONE.”
- ”I feel so hopeless and that there is nothing that can help me.”
- “I feel like I will never have sex again.”
- “Who will want me?”
- “No doctor understands this and no doctor can help me.”
If you are reading this blog, I’m sure you can identify with a few if not all of these statements. If only ONE of these statements is something you relate to, then the AFPP retreat is an event you cannot afford to miss. It will provide you with invaluable tools to address all of your concerns. You will have access to some of the world’s most renowned medical, physical therapy, and mental health professionals specializing in the integrative treatment of pelvic pain who will be able to answer any of your questions or concerns. There will be opportunities to register for significantly discounted one on one sessions with expert physical therapists, an Acupuncturist, a yoga instructor, and services from the EarthMind Wellness Center at Honors Haven. You will also be with other individuals who share the same concerns and challenges and you will not have to explain issues like “why you can’t sit” or “why this pain makes you feel you are going crazy.” For the first time in a long time you will not have to justify behaviors or decisions that you are confronted with on a daily basis – you can just be you.
One of the greatest tools you will gain from this retreat is empowerment. Pelvic pain can be so disempowering and our goal is give you the ability to empower yourself so you begin or continue on the path of self-healing through a combination of medical and integrative health techniques. I never ask any of my clients to use a technique that I don’t use myself. And I have found that medical interventions are often essential but not enough. Overcoming pelvic pain takes an “East meets the West” approach using a daily practice of mindfulness, meditation, and other integrative techniques. Participants leave the retreat with a new support system, a sense of self-empowerment, and a host of self-healing practices (such as a physical therapy home program) that will be invaluable on your journey to recovery – and most important, A RENEWED SENSE OF HOPE.
(Spaces are limited so please book your reservation as soon as possible. Also, for funding opportunities, all participants should go to Gofundme.com.)
The following post comes to us from Herman & Wallace faculty member Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC. Allison authored "Use of transabdominal ultrasound imaging in retraining the pelvic-floor muscles of a woman postpartum" and is a leading expert in the use of ultrasound imaging for pelvic rehab. She is the author and instructor of the Rehabilitative Ultrasound Imaging: Women’s Health and Orthopedic Topics offered with Herman & Wallace.
In the pelvic floor series we learn how to perform examinations for cystoceles and rectoceles. It can be more difficult for therapists to examine and quantify the degree of uterine descent. In the last few years translabial ultrasound imaging has also been used to identify what is happening in the anterior compartment upon Valsalva and pelvic floor contraction, including the uterus. This is helpful when trying to determine the degree of uterine prolapse. Degree of pelvic organ descent visible on by ultrasound has been shown to have a near-linear relationship with measures on the POPQ.
 Clinically we see that some patients with severe prolapses have few symptoms, while other patients with smaller prolapses will have more severe complaints of symptoms. This can be puzzling to the clinician who is trying to treat prolapse patients. Shek and Dietz performed a study to set cutoff measures of uterine descent that will predict symptoms of prolapse. Translabial ultrasound imaging was performed on 538 women with 263 women reporting prolapse symptoms. Seventy-five percent of the women presented with grade two or greater prolapse on the POPQ, with most of being cystoceles or rectoceles. The women with more complaints of symptoms of prolapse were more likely to have uterine prolapse. There was a strong association between degree of uterine descent and symptoms of prolapse. They determined that an optimal cutoff to predict symptoms of prolapse due to uterine descent is a cervix descending to 15 mm above the pubic symphysis.
Clinically we see that some patients with severe prolapses have few symptoms, while other patients with smaller prolapses will have more severe complaints of symptoms. This can be puzzling to the clinician who is trying to treat prolapse patients. Shek and Dietz performed a study to set cutoff measures of uterine descent that will predict symptoms of prolapse. Translabial ultrasound imaging was performed on 538 women with 263 women reporting prolapse symptoms. Seventy-five percent of the women presented with grade two or greater prolapse on the POPQ, with most of being cystoceles or rectoceles. The women with more complaints of symptoms of prolapse were more likely to have uterine prolapse. There was a strong association between degree of uterine descent and symptoms of prolapse. They determined that an optimal cutoff to predict symptoms of prolapse due to uterine descent is a cervix descending to 15 mm above the pubic symphysis.
This study intrigues me and makes me wonder how much we are focusing on cystoceles and rectoceles and not looking at uterine prolapses. Using translabial ultrasound imaging is a nice tool to allow the clinician to see what is going on with all of the pelvic organs. With one Valsalva maneuver you are able to assess a lot of information including support of the pelvic organs. It also gives the clinician another way to quantify the degree of prolapse. Ultrasound imaging is a wonderful tool that clinicians can use for assessment as well as a biofeedback tool. If you are interested in learning how to perform this type of assessment, I will be teaching Rehabilitative Ultrasound Imaging: Women’s Health and Orthopedic Topics May 1-3 in Dayton, OH.
Shek KL, Dietz HP. What is abnormal uterine descent on translabial ultrasound? Int. Urogynecol J. 2015; 26(12)1783-7.
Exercise in pregnancy is a loaded topic. We commonly see images of women doing vigorous exercise in late pregnancy accompanied by judgmental statements about the safety of such activity not only for the woman, but also for the baby. Many myths persist about exercise in pregnancy, and it’s our role as health care specialists to educate women about what is known about exercising. Holly Herman, co-founder of the Herman & Wallace Pelvic Rehabilitation Institute, has been educating providers about this topic for most of her career. Anyone lucky enough to take a course on pregnancy and postpartum issues from Holly Herman knows that her style of teaching is effective and her passion is contagious. From Holly’s use of patient stories to wonderful humor, you can really “get it” when it comes to clinical concepts and strategies. One of Holly’s clinical pearls that really stuck with me after learning about exercise and pregnancy is the research completed by James Clapp in his book “Exercise in Pregnancy”. In short, the book dispels the myth that women shouldn’t exercise in pregnancy and in fact reports on the benefits of exercise to both Mom and baby for labor, delivery, and beyond. In signature style, Holly held this book up in front of the class and to great laughter said, “And this is the book you should buy for your mother-in-law.”
 Another myth that has been perpetuated in relation to pregnancy, labor and delivery is the notion that exercising can make the pelvic floor muscles short, tight, and more narrow, making delivery more difficult. In an article we reported on previously about women being “too tight to give birth” the authors concluded that strong pelvic floor muscles do not lead to challenges with birthing. (Bo et al., 2013) In a more recent article that addressed this issue, Kari Bo and colleagues studied 274 women for levator hiatus (LH) width to see if exercising in late pregnancy did in fact narrow this space. At week 37 of gestation, the exercisers were measured to have a significantly larger LH than the non-exercisers. (Exercisers were defined as women who exercised 30 minutes or more 3 times per week versus the non-exercisers.) The authors conclude that there were not any significant differences in labor outcomes or in delivery outcomes between the groups. (Bo et al., 2015)
Another myth that has been perpetuated in relation to pregnancy, labor and delivery is the notion that exercising can make the pelvic floor muscles short, tight, and more narrow, making delivery more difficult. In an article we reported on previously about women being “too tight to give birth” the authors concluded that strong pelvic floor muscles do not lead to challenges with birthing. (Bo et al., 2013) In a more recent article that addressed this issue, Kari Bo and colleagues studied 274 women for levator hiatus (LH) width to see if exercising in late pregnancy did in fact narrow this space. At week 37 of gestation, the exercisers were measured to have a significantly larger LH than the non-exercisers. (Exercisers were defined as women who exercised 30 minutes or more 3 times per week versus the non-exercisers.) The authors conclude that there were not any significant differences in labor outcomes or in delivery outcomes between the groups. (Bo et al., 2015)
Without a doubt, the patient’s obstetrician gives primary direction to the patient when any high-risk issues are present. Most women however, are basing their exercise choices on experience, on misinformation, myths, or popular opinion. It is our responsibility to engage women in conversations about her health, wellness, and fitness, and to appropriately counsel on exercise during pregnancy and the postpartum period. Most of us lacked proper education about this important population in our primary graduate training, and therefore must seek out information to fill in the gaps. If you are interested in filling in any gaps, join us at one of our peripartum courses around the country. Your next opportunities to take these courses are:
Care of the Postpartum Patient - Seattle, WA
Mar 12, 2016 - Mar 13, 2016
Care of the Pregnant Patient - Somerset, NJ
Apr 30, 2016 - May 1, 2016
Care of the Pregnant Patient - Akron, OH
Sep 10, 2016 - Sep 11, 2016
Bø, K., Hilde, G., Jensen, J. S., Siafarikas, F., & Engh, M. E. (2013). Too tight to give birth? Assessment of pelvic floor muscle function in 277 nulliparous pregnant women. International urogynecology journal, 24(12), 2065-2070.
Bø, K., Hilde, G., Stær-Jensen, J., Siafarikas, F., Tennfjord, M. K., & Engh, M. E. (2015). Does general exercise training before and during pregnancy influence the pelvic floor “opening” and delivery outcome? A 3D/4D ultrasound study following nulliparous pregnant women from mid-pregnancy to childbirth. British journal of sports medicine, 49(3), 196-199.
Clapp, J. F., Cram, C. (2012) Exercising Through Your Pregnancy. Addicts Books
A few years ago, I was convinced my left hip pain was due to osteoarthritis. When my hip locked up after a 14 mile run, my manual therapist husband differentially diagnosed the pain as discogenic. Partly in denial and partly wanting to know the extent of the “damage,” I got an x-ray of my left hip, which was completely normal, and a lumbar MRI, which wasn't pretty. The source of my hip pain was a disc bulge at L3-4 and L4-5 with a Schmorl's node at L5-S1 to boot. Instead of riding the train of thought that we treat what hurts, therapists need to disembark and look further for the source, as suggested in the course, “Finding the Driver in Pelvic Pain.”
 A case report published in the International Journal of Sports Physical Therapy by Livingston, Deprey, and Hensley (2015) documents the discovery of a deeper problem than the referring diagnosis of greater trochanteric pain syndrome. A 29 year old female had to stop running because of lateral hip pain that began 3 months after increasing the intensity and frequency of her running and low impact plyometrics. She had pain in sitting and while running. During the evaluation, she demonstrated a positive Trendelenburg, weak and painless hip abductors, and a positive single leg hop test on concrete. When the pain was not elicited with single leg hop on a foam surface, the patient was referred back to the physician for magnetic resonance imaging. The patient was later diagnosed with an acetabular stress fracture. The therapist’s thorough examination helped prevent possible avascular necrosis or a more traumatic fracture of the pelvis.
A case report published in the International Journal of Sports Physical Therapy by Livingston, Deprey, and Hensley (2015) documents the discovery of a deeper problem than the referring diagnosis of greater trochanteric pain syndrome. A 29 year old female had to stop running because of lateral hip pain that began 3 months after increasing the intensity and frequency of her running and low impact plyometrics. She had pain in sitting and while running. During the evaluation, she demonstrated a positive Trendelenburg, weak and painless hip abductors, and a positive single leg hop test on concrete. When the pain was not elicited with single leg hop on a foam surface, the patient was referred back to the physician for magnetic resonance imaging. The patient was later diagnosed with an acetabular stress fracture. The therapist’s thorough examination helped prevent possible avascular necrosis or a more traumatic fracture of the pelvis.
In a 2013 issue of the same journal, Podschum et al. presents a case report on deciphering the diagnosis in a female runner with deep gluteal pain with pelvic involvement. A 45 year old female marathon runner reported pulling her hamstring and complained of left ischial tuberosity pain with aching into the gluteal and pubic ramus regions that eventually forced her to stop running. She had pain in sitting and could not tolerate speed work. She had a history of low back and pelvic floor pain, with an MRI showing osteitis pubis, a lateral L3-4 bulge, and facet hypertrophy at L4-5. The physical therapist ruled out lumbar disc lesion, radiculopathy, sacroiliac joint dysfunction, and hip labral tear with special tests. Initial treatment focused on the differential diagnoses of hamstring syndrome and ischiogluteal bursitis based on subjective complaints and objective findings. After 4 visits, her deep ache shifted to the inferior pubic ramus in sitting as the ischial tuberosity pain diminished. A trained therapist then conducted a thorough pelvic floor exam. Pelvic floor hypertonic dysfunction was diagnosed and took over the “driver’s seat” as the focus for the rest of the treatment of this patient. Symptoms resolved and the patient returned to running marathons without any of her initial presenting symptoms.
If we let specific pain complaints guide our treatment, we will run out of steam with the lack of progress. Finding the true source of symptoms is critical in physical therapy. Sometimes so much is going on with our patients we have to sort through the weeds before we can access the actual road to recovery. The lumbar spine, hips, and pelvic floor create an intricate map of U-turns and two-way streets, so we need to deepen our understanding of how to navigate the regions. Only then will be able to confidently diagnose the “driver” and let the other areas call “shotgun.”
References:
Livingston, J. I., Deprey, S. M., & Hensley, C. P. (2015). DIFFERENTIAL DIAGNOSTIC PROCESS AND CLINICAL DECISION MAKING IN A YOUNG ADULT FEMALE WITH LATERAL HIP PAIN: A CASE REPORT. International Journal of Sports Physical Therapy, 10(5), 712–722.
Podschun, L., Hanney, W. J., Kolber, M. J., Garcia, A., & Rothschild, C. E. (2013). DIFFERENTIAL DIAGNOSIS OF DEEP GLUTEAL PAIN IN A FEMALE RUNNER WITH PELVIC INVOLVEMENT: A CASE REPORT. International Journal of Sports Physical Therapy, 8(4), 462–471.
There's a lot going on in the world of pelvic rehab, and continuing education is no exception! This March, Herman & Wallace is hosting NINE courses around the country. It's a lot to keep up with, so we thought you might appreciate a brief overview of what's coming up next!
Where's this pain coming from?
Pelvic pain can have many sources, and Elizabeth Hampton wants to help you quickly get to the source. Finding the Driver in Pelvic Pain empowers you to play detective in order to help even the most complex patients. Don't miss out on Finding the Driver in Pelvic Pain in San Diego, CA on March 4-6, 2016
What goes in eventually comes out
How important is a good diet? For most of us eating healthy is important, and for many pelvic rehab patients it is a necessity. That's why Megan Pribyl wrote her "Nutrition Perspectives for the Pelvic Rehab Therapist" course. This beginner level course is intended to expand the your knowledge of the metabolic underpinnings for local to systemically complex disorders. Don't miss out on Nutrition Perspectives for the Pelvic Rehab Therapist - Kansas City, MO - March 5-6, 2016!
There's fascia everywhere!
Fascial mobilization is a rising star in pelvic rehab treatment techniques, and Ramona Horton is excited to share it with you! "Mobilization of the Myofascial Layer: Pelvis and Lower Extremity" is the best opportunity you'll get to learn about the evaluation and treatment of myofascia for pelvic dysfunction. Check it out on our continuing education course page. Ramona will be teaching these techniques in Santa Barbara, CA on March 11-13.
Giving birth hurts
Sometimes the newborn is the one to get all the attention, but what about the new mother? Be sure that you can help postpartum women with symptoms like postural dysfunction, pelvic girdle dysfunction, diastasis recti abdominis and more by attending Care of the Postpartum Patient in Seattle, WA this March 12-13, taught by the wonderful Holly Tanner!
Vulvar pain is easy to have and hard to lose
12% of women in the US have vulvar pain for 3 or more months at some stage in their life. It takes a multidisciplinary approach to address all the causes and co-morbidities, and that is exactly what you'll get at Dee Hartmann's Vulvodynia: Assessment and Treatment in Houston, TX on March 12-13, 2016. Dee aims to address the vicious cycle of pain, visceral and sexual dysfunction, and the general hit to quality of life that patients with vulvodynia suffer from.
The challenge of SI joint pain
The sacroiliac joint, pelvic girdle, and pelvic ring sure can take a beating, and Peter Philip knows how to keep you moving. Through exercise and stabilization, the pelvic rehab practitioner can quickly treat pain in the lumbopelvic-hip complex. Learn all about the direct and indirect anatomy that influences the sacroiliac joint, and then get ready to find and treat the source of pain and dysfunction in Sacroiliac Joint Treatment in Minneapolis, MN on March 19-20, 2016.
Taxes and Menopause
The menopause transition is not something many people look forward to. For some women it goes more smoothly than others, and it's the less fortunate ones who need access to a well-trained pelvic care professional. Michelle Lyons is flying in from Ireland to help you to become that pro! Be it vaginal atrophy, sexual health dysfunction, pelvic organ prolapse, or any other of the myriad possible symptoms of menopause, you'll be equipped to handle them all after attending Menopause: A Rehabilitation Approach in Atlanta, GA on March 19-20, 2016.
The following post comes to us from Dee Hartmann, PT, DPT who is the author and instructor of Vulvodynia: Assessment and Treatment. To learn evaluation and treatment techniques for vulvar pain, join Dee in in Houston, TX this March 12-13. Early registration pricing expires soon!
 I recently heard a young, vivacious urologist present treatment options for overactive bladder to a group of nursing professionals (SUNA). To my delight as the only PT in the audience, I was pleased that physical therapy was her first line of treatment for this difficult population of chronic pelvic pain patients. As a women’s health PT, we know that chronic vulvar pain suffers experience many of the same dysfunctions, including pelvic floor muscle over-activity.
I recently heard a young, vivacious urologist present treatment options for overactive bladder to a group of nursing professionals (SUNA). To my delight as the only PT in the audience, I was pleased that physical therapy was her first line of treatment for this difficult population of chronic pelvic pain patients. As a women’s health PT, we know that chronic vulvar pain suffers experience many of the same dysfunctions, including pelvic floor muscle over-activity.
The physician’s presentation included two very emphatic statements—“physical therapy always hurts” and “no one in this group of patients should ever do Kegel exercises”. She went on to explain that anyone with pelvic floor muscle over activity should only be taught to relax; that “if they were seeing a practitioner who was telling them to do Kegels, they needed to find another PT”. As she’s not a PT, I challenged her on her second comment. I was too annoyed to address the first.
I appreciate that, as a urologist, she may not know that we learned some time ago that rest for chronic muscle tension, like chronic low back, has been proven ineffective[1]. Rather, research suggests that increased mobility and strengthening prove more effective in the long term to decrease pain by restoring normal muscle function. As pelvic floor muscles are voluntary, striated muscles, it only makes sense that the same findings apply. Those who oppose active pelvic floor muscle active exercise suggest that the over-active state of the pelvic floor muscles causes vulvar pain. I agree. However, simply relaxing dysfunctional pelvic floor muscles and expecting them to work effectively seems a bit short-sighted. Normal pelvic floor muscle function is integral to efficient core stability as well as sphincteric control, pelvic visceral support, and sexual function. Why not begin rehab for these ladies with an active exercise program, directed at renewing pelvic floor muscle motor control, with resulting decreased introital pain, improved function (sphincteric , supportive, and sexual), and improved core support?
As for the urologist’s first statement, mark me down as totally opposed. My professional experience suggests the need to replicate familiar vulvar pain and then find abnormal physical findings in the trunk, hips, viscera, and pelvis that are contributory. Rather than utilizing any treatment that causes additional pain, addressing associated abnormal findings that immediately decrease pelvic floor muscle resting tone and palpated vulvar pain, seems much more productive.
[1] Waddell G. "Simple low back pain: rest or active exercise?" Ann Rheum Dis 1993;52:317.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/







































