Congratulations to Jane Blair Johe, PT, PRPC on becoming one of the newest Certified Pelvic Rehabilitation Practitioners! Read our interview with Blair below.
 Tell us about your clinical practice
Tell us about your clinical practice
I work in a free standing outpatient PT center of a large 4 hospital affiliation. 70% lymphedema 30% pelvic floor rehab.
How did you get involved in the pelvic rehabilitation field?
I was already the lymphedema PT (LANA cert.) when I moved to WV. The women's health PT was moving to another state and asked me to please pick up her bladder incontinence patients.
What patient population do you find most rewarding in treating and why?
I do like pelvic pain clients as I can work with other PT’s on staff to problem solve . Both patients and their doctors are so grateful.
If you could get a message out to physical therapists about pelvic rehabilitation what would it be?
That you cannot ignore a very important group of muscles (PF) whether you are treating backs, hips etc. or pain and weakness or balance issues…. it plays such a vital role in wellbeing. Any of these clients should be questioned about bowel and bladder issues.
What has been your favorite Herman & Wallace Course and why?
I took my first course from them in September and was so impressed (compared to other courses)
What lesson have you learned from a Herman & Wallace instructor that has stayed with you?
the PT pelvic floor assessment. Correct postures , breathing and “safe” effort of bowel movements.
What do you find is the most useful resource for your practice?
MedBridge Courses
What motivated you to earn PRPC?
If I only had one pelvic floor referral, I would like to give the best service possible to that client. My referring MD’s are very happy too.
What makes you the most proud to have earned PRPC?
I thought it was a many faceted subject and combined many aspects of my 45 years of physical therapy practice. It made me feel that I do know my profession that I love.
What advice would you give to physical therapists interested in earning PRPC?
Have a broad back ground in multiple areas of PT then I highly recommend Herman and Wallace courses as the best path.
What is in store for you in the future?
A urologist in town contacted me today to set up referring for pre surgery PT (prostate surgery).
 The following guest post comes to us from Angie Johnson, a physical therapist with Kaiser Permanente in Portland, OR.
The following guest post comes to us from Angie Johnson, a physical therapist with Kaiser Permanente in Portland, OR.
Did you know that the pelvic floor muscles are actually quite thin? “Pelvic floor muscles are able to produce enough force to overcome changes in intra-abdominal pressure during less rigorous activities of daily living,“ but in activities such as coughing and jumping, “intra-abdominal pressure clearly exceeds the maximum force generated by pelvic floor muscles alone.”1 But we know that people are continent of urine during these activities, so it begs to question what structures help support the pelvic floor during high force events?
In our journey of pelvic rehabilitation and evidence-based medicine, researchers have determined that contributors to pelvic floor function include trunk stabilization2 and co-contraction of the abdominal wall (especially transverse abdominus)3,4. But this is only the beginning of the story. To add to this picture, new research, recently published in the Journal of Women’s Health Physical Therapy (January/April 2016) validates what we as practitioners already know; hip muscles play a crucial role in optimal pelvic floor functioning.
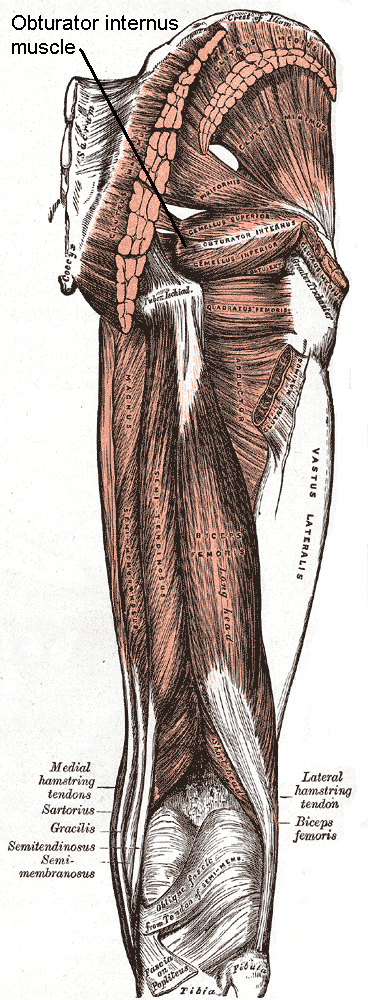
Knowledge of the anatomy of the pelvic floor and hip musculature helps to give us more understanding of the continence mechanism during high force activity. Obturator internus, which can be easily palpated through the vaginal wall “acts to externally rotate the hip. Interesting, this muscle actually shares a fascial attachment with the pelvic floor muscles.”
Researchers from a team at San Diego State University asked the very pertinent question: If you strengthen obturator internus do you strengthen the pelvic floor muscles too? To answer this question, they conducted a randomized control trial of 40 nulliparous women, aged 18-35, who were assigned to a hip exercise or control group. Both hip external rotator strength and pelvic floor muscle strength (via the Peritron™ perineometer) were measured in all of the women. The exercise group was then asked to perform clamshell exercises, isometric wall external rotation and “monster walks” as their specific hip exercises. The prescription of the exercises were 3 sets of 10 repetitions 3 days per week for 12 weeks. One session each week was supervised in the laboratory to ensure proper execution.
After the 12 weeks, the exercise group had an increase in hip external rotation strength, but also in pelvic floor muscle peak pressure. That was without any specific pelvic floor strengthening exercises at all. Strengthen the hips by doing these three exercises, and pelvic floor strength increases!! This is exciting and fantastic news for us as pelvic floor therapists and a good message to convey to our patients.
The results of this study are preliminary, but if you are treating pelvic floor weakness, hip external rotation strengthening exercises in addition to the traditional kegel strengthening exercises are a must. Go ahead – let’s all get hippie!
Tuttle LJ, DeLozier ER, Harter KA et al. The Role of the Obturator Internus Muscle in Pelvic Floor Function. Journal of Women’s Health Physical Therapy. 2016; 40, 1 pg 15-19
Sapsford R. Rehabilitation of pelvic floor muscles utilizing trunk stabilization. Man Ther 2004;9(1):31-42
Sapsford RR, Hodges PW, Ricahrdson CA, Cooper DH, Markwell SJ, Jull GA. Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neruourol Urodyn 2001;20(1):3-12
Sapsord RR, Hodges PW. Contraction of the pelvic floor muscles during abdominal maneuvers. Arch Phys Med REhabil. 2001;82(8):1081-1088
“…visceral manual therapy can produce immediate hypoalgesia in somatic structures segmentally related to the organ being mobilized…”
This statement is taken from an article written by MCSweeney and colleagues published in the Journal of Bodywork and Movement Therapies in 2012. The authors, who state that there is a lack of research that explains underlying mechanisms for visceral mobilization, aimed to determine if visceral mobilization could produce local and/or systemic effects towards hypoalgesia. The measurement of hypoalgesia, defined by the IASP as “diminished pain in response to a normally painful stimulus,” was assessed by use of a hand-held manual digital pressure algometer for pressure pain threshold (PPT). Sixteen asymptomatic subjects were recruited from an osteopathic school and were treated on separate occasions with a visceral mobilization of the sigmoid colon, a sham intervention of manual contact on the abdomen, and a control of no intervention. Six females (mean age 23.7) and ten males (mean age 27.7) completed the single-blinded, randomized study.

The clinical practice relevance was difficult to determine, however, this study used new techniques to determine that there is an immediate and measurable effect on the body. While therapists who treat with visceral mobilization and other soft tissue techniques know that the interventions have helped their patients, having further experimental and clinical validation of the value of these techniques is critical. If you are interested in learning more about fascial approaches to easing pain and improving function in your patients, check out the courses offered by faculty member Ramona Horton.
Ramona will be teaching her Mobilization of the Myofascial Layer: Pelvis and Lower Extremities course three times this year, with the next event in Nashua, NH June 3-5. Her Mobilization of Visceral Fascia: The Urinary System course is available three times as well, next in Kirkland, WA on June 24-26. If you're ready for the advanced course, and some wine tasting(!), check out Mobilization of Visceral Fascia: The Reproductive System of Men and Women on October 14-16 in Medford, OR.
McSweeney, T. P., Thomson, O. P., & Johnston, R. (2012). The immediate effects of sigmoid colon manipulation on pressure pain thresholds in the lumbar spine. Journal of bodywork and movement therapies, 16(4), 416-423.
In Megan Pribyl’s course on Nutrition Perspectives for the Pelvic Rehab Therapist, she discusses a wide variety of useful topics specific to nutrition and pelvic health. In her lecture on “Nutritional Homeostasis”, Megan counsels against missing an underlying eating disorder when working with a patient who has bowel issues. Work by Abraham and Kellow (2013) is cited, and in their article published in BMC Gastroenterology, the authors concur that many patients who have functional gastrointestinal complaints may also have disordered eating. How then, can we tell these patients apart, and get patients the most appropriate care? First let’s look at their research.
 Patients who were admitted to a specialty unit for those with eating disorders in Australia were studied and were found to have conditions such as anorexia nervosa, bulimia nervosa, polycystic ovarian syndrome, treated celiac disease, and treated bipolar depression. All of the 185 patients completed the Rome II Modular Questionnaire to identify symptoms consistent with functional gastrointestinal (GI) dysfunction. They also completed the Eating and Exercise Examination which collected data about behaviors including objective binge eating, self-induced vomiting, laxative use and excessive exercise.
Patients who were admitted to a specialty unit for those with eating disorders in Australia were studied and were found to have conditions such as anorexia nervosa, bulimia nervosa, polycystic ovarian syndrome, treated celiac disease, and treated bipolar depression. All of the 185 patients completed the Rome II Modular Questionnaire to identify symptoms consistent with functional gastrointestinal (GI) dysfunction. They also completed the Eating and Exercise Examination which collected data about behaviors including objective binge eating, self-induced vomiting, laxative use and excessive exercise.
Esophageal discomfort (heartburn and chest pain of non cardiac origin) was associated with excess exercise (more than 5 days/week). Self-induced vomiting was identified primarily in the patients diagnosed with bulimia. One interesting finding the researchers noted is that for patients who have disorder eating, pelvic floor symptoms that are not associated with functional constipation are a prominent feature. This data begs the question, how can we best screen for disordered eating in patients who present with bowel dysfunction that otherwise may fit with the symptoms and presentation of patients who do not have disordered eating?
Our first step may be to include important conditions and symptoms on our written or computer-based intake forms. Is “disordered eating” or bulimia, anorexia-nervosa included on your intake forms for patients? What about symptoms like heartburn, laxative use, or vomiting? (As an important aside, I always remember being surprised by a patient who had urinary incontinence when she told me that she leaked with vomiting. She had gone through a gastric bypass surgery and would vomit several times per week as a reaction to difficulty digesting food. There may be a few good reason therefore to include vomiting on a checklist.) As pelvic rehab providers, we can understand how frequent vomiting may lead to dehydration, intrabdominal and intrapelvic pressure, potential pelvic floor dysfunction, or how disordered eating may lead to other bowel dysfunctions such as constipation and/or fecal incontinence. If we also hold space for eating issues to be a concern, we may find that asking some valuable questions provides more information.
If you would like to learn more about nutrition and the pelvic health connections, you still have time to sign up for Megan Pribyl’s nutrition course which takes place in Lodi, California this June!.
Abraham, S., & Kellow, J. E. (2013) "Do the digestive tract symptoms in eating disorder patients represent functional gastrointestinal disorders?" BMC gastroenterology, 13(1), 1.
If an infomercial played in pre-op waiting rooms explaining all the possible side effects or problems a patient may encounter after surgery, I wonder how many people would abort their scheduled mission. As if having an abdominal or pelvic surgery were not enough for a patient to handle, some unfortunate folks wind up with small bowel obstruction as a consequence of scar tissue forming after the procedure. Instead of having yet another surgery to get rid of the obstruction, which, in turn, could cause more scar tissue issues, studies are showing manual therapy, including visceral manipulation, to be effective in treating adhesion-induced small bowel obstruction.
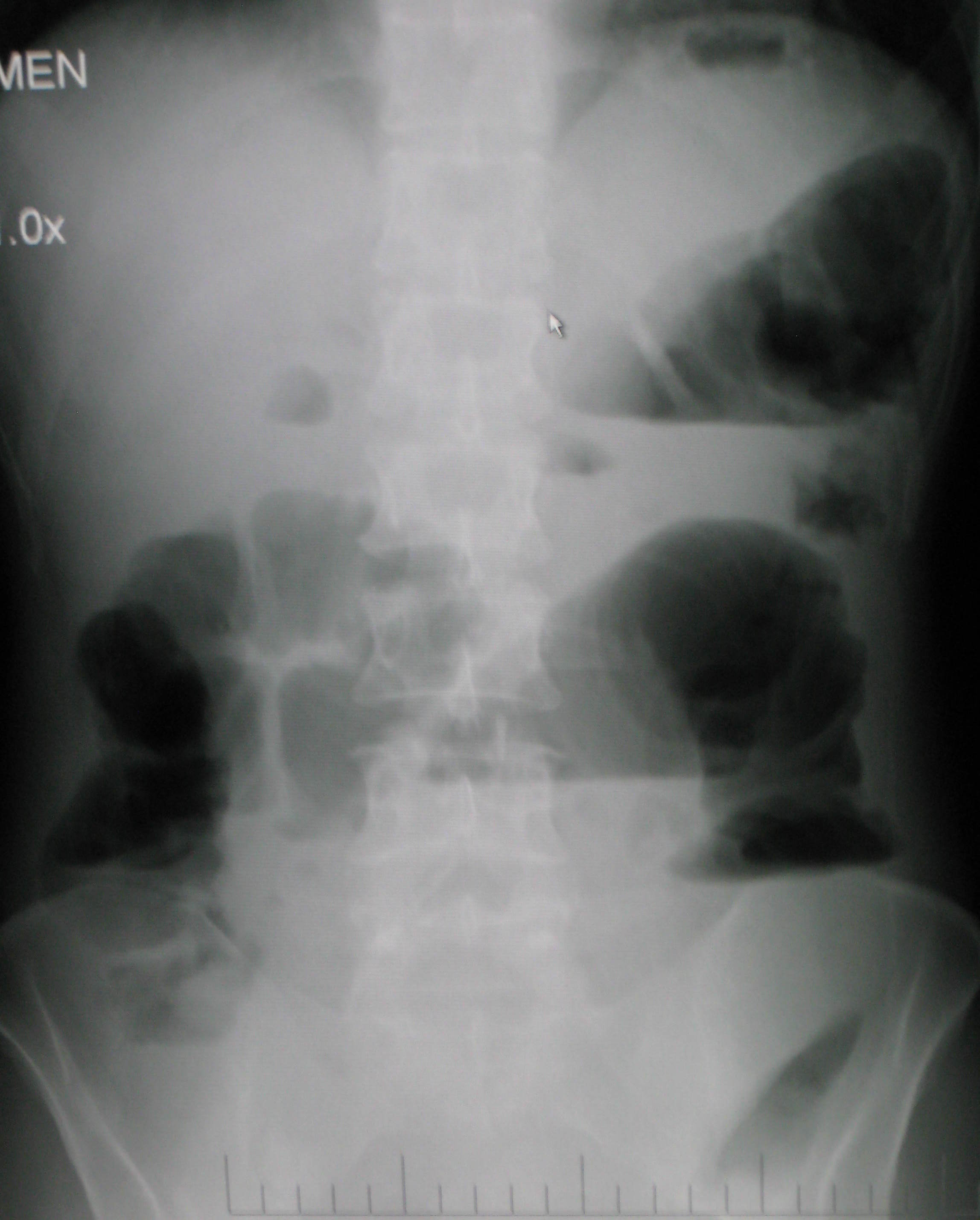 Amanda Rice and colleagues published a paper in 2013 on the non-surgical, manual therapy approach to resolve small bowel obstruction (SBO) caused by adhesions as evidenced in two case reports. One patient was a 69 year old male who had 3 hernia repairs and a laparotomy for SBO with resultant abdominal scarring and 10/10 pain on the visual analog scale. The other patient was a 49 year old female who endured 7 abdominopelvic surgeries for various issues over the course of 30 months and presented with 7/10 pain and did not want more surgical intervention for SBO. Both patients received 20 hours of intensive manual physical therapy over a period of 5 days. The primary focus was to reduce adhesions in the bowel and abdominal wall for improved visceral mobility, but treatment also addressed range of motion, flexibility, and postural strength. The female patient reported 90% improvement in symptoms, with significant decreases in pain during bowel movements or sexual intercourse, and the therapist noted increased visceral and myofascial mobility. Both patients were able to avoid further abdominopelvic surgery for SBO, and both patients were still doing well at a one year follow up.
Amanda Rice and colleagues published a paper in 2013 on the non-surgical, manual therapy approach to resolve small bowel obstruction (SBO) caused by adhesions as evidenced in two case reports. One patient was a 69 year old male who had 3 hernia repairs and a laparotomy for SBO with resultant abdominal scarring and 10/10 pain on the visual analog scale. The other patient was a 49 year old female who endured 7 abdominopelvic surgeries for various issues over the course of 30 months and presented with 7/10 pain and did not want more surgical intervention for SBO. Both patients received 20 hours of intensive manual physical therapy over a period of 5 days. The primary focus was to reduce adhesions in the bowel and abdominal wall for improved visceral mobility, but treatment also addressed range of motion, flexibility, and postural strength. The female patient reported 90% improvement in symptoms, with significant decreases in pain during bowel movements or sexual intercourse, and the therapist noted increased visceral and myofascial mobility. Both patients were able to avoid further abdominopelvic surgery for SBO, and both patients were still doing well at a one year follow up.
In 2016, a prospective, controlled survey based study by Rice et al., determined the efficacy of treating SBO with a manual therapy approach referred to as Clear Passage Approach (CPA). The 27 subjects enrolled in the study received this manual therapy treatment for 4 hours, 5 days per week. The CPA includes techniques to increase tissue and organ mobility and release adhesions. The therapist applied varying degrees of pressure across adhered bands of tissue, including myofascial release, the Wurn Technique for interstitial spaces, and visceral manipulation. The force used and the time spent on each area were based on patient tolerance. The SBO Questionnaire considered 6 domains (diet, pain, gastrointestinal symptoms, medication, quality of life, and pain severity) and was completed by 26 of the subjects pre-treatment and 90 days after treatment. The results revealed significant improvements in pain severity, overall pain, and quality of life. Suggestive improvements were noted in gastrointestinal symptoms as well as tissue and organ mobility via improvement in trunk extension, rotation, and side bending after treatment. Overall, the authors conclude the manual therapy treatment of SBO is a safe and effective non-invasive approach to use, even for the pediatric population with SBO.
Myofascial release and visceral manipulation can disrupt the vicious cycle of adhesions causing small bowel obstruction after abdominopelvic surgical “invasion.” Learning specific techniques we may never have thought of can make a huge impact on certain patient populations. Quality of life for our patients often depends on how willing we are to increase our own knowledge and skill base.
Rice, A. D., King, R., Reed, E. D., Patterson, K., Wurn, B. F., & Wurn, L. J. (2013). Manual Physical Therapy for Non-Surgical Treatment of Adhesion-Related Small Bowel Obstructions: Two Case Reports . Journal of Clinical Medicine, 2(1), 1–12. PubMed Link
Rice, A. D., Patterson, K., Reed, E. D., Wurn, B. F., Klingenberg, B., King, C. R., & Wurn, L. J. (2016). Treating Small Bowel Obstruction with a Manual Physical Therapy: A Prospective Efficacy Study. BioMed Research International, 2016, 7610387. http://doi.org/10.1155/2016/7610387
 Dr. Peter Philip, a faculty member with the Herman & Wallace Institute, has published a new book! "Pelvic Pain and Dysfunction: A Differential Diagnosis Manual" is available now through Thieme Medical Publishers. We caught up with Dr. Philip to learn a bit more about his project.
Dr. Peter Philip, a faculty member with the Herman & Wallace Institute, has published a new book! "Pelvic Pain and Dysfunction: A Differential Diagnosis Manual" is available now through Thieme Medical Publishers. We caught up with Dr. Philip to learn a bit more about his project.
Peter is also the author and instructor of two courses offered through Herman & Wallace. Sacroiliac Joint Evaluation and Treatment is an opportunity to learn an exercise and stabilization approach to pelvic girdle, sacroiliac joint, and pelvic ring dysfunction. This course is available twice in 2016; May 21-22 in Austin, TX and later on November 6-7 in Bayshore, NY. Peter's other course, Differential Diagnostics of Chronic Pelvic Pain: Interconnections of the Spine, Neurology and the Hips, expands the practitioner's diagnostic toolkit for complicated chronic pelvic pain patients. This course is available on August 19-21 in Nashville, TN. Don't miss out!
H&W: Thanks for doing this interview, Peter! What's new?
Dr. Philip: After years of research, and writing, my textbook has been published and is ready for the public.
H&W: That's great! What can you tell us about the book?
Dr. Philip: It's called Pelvic Pain and Dysfunction; a Differential Diagnosis Manual, and it has been published by Thieme. Thieme is based out of Stuttgart Germany and is the world’s largest distributor of medical textbooks and journals! The purpose of the book is to answer the questions that so many clinicians have as it relates to their patient’s pain, such as:
- Why are there muscle spasms?
- How can the pain seemingly spread from one organ to the next? Or even from one system to another?
- How can I effectively and efficiently evaluate my patients who suffer with pelvic, bladder, bowel, or visceral pain and dysfunction?
- And so much more
The textbook also outlines a revolutionary strategy that immediately provides the patient with a reduction in their pain, and often immediate resolution of tight “spasms” or “trigger points”. The mysteries of how and why our patients' pain changes and progresses are outlined in a clear, linear fashion that integrates into a practitioner's current practice. The purpose of the textbook is to provide a means of understanding where pain originates and how to isolate it to a specific region. Once isolated, the book instructs how to treat that region effectively.
H&W: you mean to tell me that you’ve created a method which allows a suffering patient to experience “immediate relief”?
Dr. Philip: Yes! And it's actually quite simple once you understand the anatomy, and the integration of the central nervous system, the peripheral nervous system, psychology, viscera, muscles, tendons, ligaments, and nerves.
H&W: Who is this textbook written for?
Dr. Philip: the textbook is written for all my colleagues who treat patients with pelvic pain. Medical Doctors and Doctors of Science in both the United States and Germany have reviewed the material and found the information, concepts and strategies to be useful.
H&W: how did you put this all together?
Dr. Philip: I realized years ago that the field of pelvic health did not take into consideration the multiple facets that may be involved in a patient’s pain. Many strategies employed simply address restrictions in tissue mobility by “stretching” or “massaging” without taking into consideration the reason these structures are limited in mobility, or have spasms. Knowing why a structure is limited in its mobility or is spastic will allow the clinician to immediately address the suffering patient's needs and promote healing, even if the patient has been suffering for decades.
H&W: but how did you come up with this process?
Dr. Philip: my background is in non-surgical orthopedic medicine. Having three degrees in orthopedic physical therapy, and a certification by the International Academy of Orthopedic Medicine, I applied the differential diagnostic concepts of orthopedic medicine to the pelvic pain population with great success! Using the principles found within this textbook the clinician will have the opportunity to address the exact tissue at fault, provide a near immediate resolution of their pain, and provide a means for the patient to completely regain their wellness and move forward in their life.
H&W: I can see why you are so excited. Is this textbook available yet?
Dr. Philip: yes it is. It can be found at http://www.thieme.com/books-main/obstetrics-and-gynecology/product/3517-pelvic-pain-and-dysfunction. I put in a lot of effort to keep the book comfortably priced at $99.00! I know how tight cash can be for students and the working professional, so keeping it affordable was paramount to me.
H&W: What a fantastic project. Thank you so very much for taking the time to share it with us!
Dr. Philip: It's been a pleasure. Thank you to the Herman and Wallace Institute for allowing me to introduce my textbook and to teach these concepts and strategies.
I lived in Seattle during my pregnancies, where practicing yoga is almost as common as drinking coffee. I never accepted my friends’ invitations to partake in a perinatal yoga classes, mostly because I do not know how to do it, and I simply ran instead. My friends reaped the benefits of the meditation and strengthening involved when it came to delivering their babies. Researchers have been trying to measure the physical benefits from performing yoga during pregnancy, both for the mother and the fetus, and scientifically support the efficacy of participating in peripartum yoga.
 In a systematic review of studies regarding yoga for pregnant women, Curtis, Weinrib, and Katz (2012) explored the literature on yoga for pregnancy. Six studies were included in the review, only 3 of which were randomized controlled trials. The aspects of yoga included in the trials were postures, breathing practices, meditation, deep relaxation, counseling on lifestyle change, and chanting and anatomy information. The programs in the trials began either between 18-20 weeks gestation or between 26-28 weeks. The yoga was practiced either 3 times per week for 30-60 minutes or 60 minutes daily. Control groups included walking, standard prenatal exercise, or general nursing care. The literature review suggested improvements were noted regarding quality of life and self-efficacy, discomfort and pain during labor, and birth weight and preterm births. Due to the limited number of trials, only a general positive commendation of yoga during pregnancy could be made from this research.
In a systematic review of studies regarding yoga for pregnant women, Curtis, Weinrib, and Katz (2012) explored the literature on yoga for pregnancy. Six studies were included in the review, only 3 of which were randomized controlled trials. The aspects of yoga included in the trials were postures, breathing practices, meditation, deep relaxation, counseling on lifestyle change, and chanting and anatomy information. The programs in the trials began either between 18-20 weeks gestation or between 26-28 weeks. The yoga was practiced either 3 times per week for 30-60 minutes or 60 minutes daily. Control groups included walking, standard prenatal exercise, or general nursing care. The literature review suggested improvements were noted regarding quality of life and self-efficacy, discomfort and pain during labor, and birth weight and preterm births. Due to the limited number of trials, only a general positive commendation of yoga during pregnancy could be made from this research.
In 2015, Jiang et al. looked at 10 randomized controlled trials from 2004 to 2014 regarding yoga and pregnancy. The authors found consistent evidence showing a positive correlation between yoga intervention and lower incidence of prenatal disorders and small gestational age. Lower levels of stress and pain as well as higher relationship scores were noted with yoga. The studies showed yoga to be a safe and effective means of exercise during pregnancy, but the authors agreed further randomized controlled studies still need to be performed.
A 2015 randomized control trial by Rakhshani et al. examined the effect of yoga on utero-fetal-placental circulation during pregnancy considered high-risk. The yoga group consisted of 27 women who received standard care plus 60 minute yoga sessions 3 times per week and practice at home. The control group included 32 women who received standard care and walked 30 minutes in the morning and evening. The intervention began at the 13th week of gestation and concluded at the end of the 28th week. Yoga intervention involved yoga postures, relaxation and breathing exercises, and visualization with guided imagery. The authors conceded larger studies need to be performed to confirm the results of their randomized controlled trial; however, they concluded yoga visualization and guided imagery can significantly improve uteroplacental and fetoplacental circulation.
Although further studies are needed to make evidence-based claims regarding yoga during pregnancy, the general consensus deems yoga appropriate and safe. As with any exercise program, a tailored approach for each individual is prudent. Yoga includes many components, and current trials consistently indicate the visualization/imagery aspect is safe and beneficial during pregnancy, even when high risk. In retrospect, when I had placenta previa, perhaps I should’ve traded my running shorts for yoga pants!
Curtis, K., Weinrib, A., & Katz, J. (2012). Systematic Review of Yoga for Pregnant Women: Current Status and Future Directions. Evidence-Based Complementary and Alternative Medicine : eCAM, 2012, 715942.
Jiang Q, Wu Z, Zhou L, Dunlop J, Chen P. (2015). Effects of yoga intervention during pregnancy: a review for current status. American Journal of Perinatology. 32(6):503-14..
Rakhshani, A., Nagarathna, R., Mhaskar, R., Mhaskar, A., Thomas, A., & Gunasheela, S. (2015). Effects of Yoga on Utero-Fetal-Placental Circulation in High-Risk Pregnancy: A Randomized Controlled Trial. Advances in Preventive Medicine, 2015, 373041.
Pain with sitting is a common complaint that patients may present to the clinic with. While excess sitting has been shown to be detrimental to the human body, sitting is part of our everyday culture ranging from sitting at a meal, traveling in the car, or doing work at a desk. Often, physical therapists disregard the coccyx or tailbone as the possible pain generator, simply because they are fearful of assessing it, have no idea where it is, or have never learned about it being a pain generator in their education.
Coccydynia is the general term for “pain over the coccyx.” Patients with coccydynia will complain of pain with sitting or transitioning from sit to stand. Despite the coccyx being such a small bone at the end of the spine, it serves as a large attachment site for many important structures of interest that are important in pelvic floor support and continence: ¹
- Anterior: Levator ani muscles, Sacrococcygeal ligament
- Lateral: Coccygeal muscles, Sacrospinous ligament, Sacrotuberous ligament, Glute maximus muscle fibers
- Inferiorly: Iliococcygeus
 Along with serving as a major attachment site for the above structures it provides a support for weightbaring in the seated position and provides structural support for the anus. Women are five times more likely to develop coccydynia than men, with the most common cause being an external trauma like a fall, or an internal trauma like a difficult childbirth. 1,2 In a study of 57 women suffering from postpartum coccydynia, most deliveries that resulting in coccyx pain were from use of instruments such as a forceps delivery or vacuum assisted delivery. A BMI over 27 and having greater than or equal to 2 vaginal deliveries resulted in a higher rate of coccyx luxation during birth. ³ Other causes of coccyx pain can be non traumatic such as rapid weight loss leading to loss of cushioning in sitting, hypermobility or hypomobility of the sacrococcygeal joint, infections like a pilonidal cyst, or pelvic floor muscle dysfunction. ¹ When assessing a patient with coccyx pain, it is also of the upmost importance to rule out red flags, as there are multiple cases cited in the literature of tumors such as retrorectal tumors or cysts being the cause of coccyx pain. These masses must be examined by a doctor to determine if they are malignant or benign, and if excision is necessary. Sometimes these masses can be felt as a bulge on rectal examination. 4,5
Along with serving as a major attachment site for the above structures it provides a support for weightbaring in the seated position and provides structural support for the anus. Women are five times more likely to develop coccydynia than men, with the most common cause being an external trauma like a fall, or an internal trauma like a difficult childbirth. 1,2 In a study of 57 women suffering from postpartum coccydynia, most deliveries that resulting in coccyx pain were from use of instruments such as a forceps delivery or vacuum assisted delivery. A BMI over 27 and having greater than or equal to 2 vaginal deliveries resulted in a higher rate of coccyx luxation during birth. ³ Other causes of coccyx pain can be non traumatic such as rapid weight loss leading to loss of cushioning in sitting, hypermobility or hypomobility of the sacrococcygeal joint, infections like a pilonidal cyst, or pelvic floor muscle dysfunction. ¹ When assessing a patient with coccyx pain, it is also of the upmost importance to rule out red flags, as there are multiple cases cited in the literature of tumors such as retrorectal tumors or cysts being the cause of coccyx pain. These masses must be examined by a doctor to determine if they are malignant or benign, and if excision is necessary. Sometimes these masses can be felt as a bulge on rectal examination. 4,5
A multidisciplinary approach including physical therapy, ergonomic adaptations, medications, injections, and, possibly, psychotherapy leads to the greatest chance of success in patients with prolonged coccyx pain. 1 Special wedge shaped sitting cushions can provide relief for patients in sitting and help return them to their social activities during treatment. Physical therapy includes manual manipulation and internal work to the pelvic floor muscles to alleviate internal spasms and ligament pain. Intrarectal coccyx manipulation can potentially realign a dislocated sacrococcygeal joint or coccyx. 1 Taping methods can be used as a follow up to coccyx manipulation to help hold the coccyx in the new position and allow for optimal healing. Often coccyx pain patients have concomitant pathologies such as pelvic floor muscle dysfunction, sacroilliac or lumbar spine pain, and various other orthopedic findings that are beneficial to address. When conservative treatments fail, injections or a possible coccygectomy may be considered.
Luckily conservative treatment is successful in about 90% of cases. ¹ All of the above conservative tools will be taught in the upcoming Coccyx Pain Evaluation and Treatment course on April 23-24th, 2016 in Columbia, MO taught by Lila Abbate PT, DPT, OCS, WCS, PRPC. By learning how to treat coccyx pain appropriately, you will be a key provider in solving many unresolved sitting pain cases that are not resolved with traditional orthopedic physical therapy.
1. Lirette L, Chaiban G, Tolba R, et al. Coccydynia: An overview of the anatomy, etiology, and treatment of coccyx pain. The Ochsner Journal. 2014; 14:84-87.
2. Marinko L, Pecci M. Clinical Decision Making for the Evaluation and Management of Coccydynia: 2 Case Reports. JOSPT. 2014; 44(8): 615
3. Maigne JY, Rusakiewicz F, Diouf M. Postpartum coccydynia: a case series study of 57 women. Eur J Phys Rehabil Med. 2012; 48 (3): 387-392.
4. Levine R, Qu Z, Wasvary H. Retrorectal Teratoma. A rare cause of pain in the tailbone. Indian J Surg. 2013; 75(2): 147-148.
5. Suhani K, Ali S, Aggarwal L, et al. Retrorectal cystic hamartoma: A problematic tail. J Surg Tech Case Rep. 2104; 6(2): 56-60.
Faculty member Carolyn McManus, PT, MS, MA is the instructor of Mindfulness Based Pain Treatment, a course which enables practitioners to learn about the impacts of cognitive and emotional state on pain. Herman & Wallace was very lucky to have her join the faculty in 2014, and she has written in to share more about her reasons for doing so. Join her in the Bay Area this May 14-15!
I am inspired to teach for Herman and Wallace because I need more colleagues to help meet the continual demand for my skills and treatment approach. I teach patients mindfulness, body awareness and strategies to self-regulate the nervous system. Patients need to learn how to pay attention to the body in a therapeutic manner, release muscle tension, reduce the stress reaction and adopt an attitude that promotes healing and well-being. With the ability to rest the mind in the present moment, listen to the body with mindful awareness and take control of reactions to stress and pain, patients can reduce pain, make greater progress with exercise programs and improve activity levels. There is a huge demand for this treatment approach. I always have a full schedule and an insanely long wait list. More therapists who can offer mindfulness-based pain treatment are needed.
I also want to get the word out that there is a lot we can do to prevent chronic pain. Research suggests that a reduction in pain inhibitory mechanisms contribute to persistent pain. These mechanisms can be influenced by stress and cognitive and emotional modulation. Working with patients in pain for over 30 years, I have developed a clear and simple way to explain the role of cognitive and emotional factors in pain perception. I find that once patients truly understand how their reactions can amplify or inhibit nociceptive pathways, they are empowered to take an active role in a holistic treatment approach. We can improve the chances of recovery for patients at risk of chronic pain by identifying them early early on and providing them with education and mindfulness-based strategies to self-regulate the nervous system. Patients can be offered specific skills to reduce the stress reaction, fear, catastrophic thinking and the negative attitudes that amplify and prolong pain.
I want to teach other therapists to successfully help patients in pain in the way I have for many years. One recent course participant made my day when she said to me, “I now have so much more to offer my patients.”
If you are interested in offering a new course with Herman & Wallace, don't hesitate to reach out! Fill out the form at https://www.hermanwallace.com/teach-with-us and let us know about your course idea and why you would be a good fit for the team.
The following is a guest post from Isa Herrera, MSPT, CSCS owner of Renew Physical Therapy in New York, NY. Isa recently launched her new online course "Low Level Laser Therapy For Female Pelvic Pain Conditions" found at www.PelvicPainRelief/laser.
 Physical therapists deal with chronic pain that can be problematic to treat and manage on a daily basis. There is an arsenal of tools, exercises and techniques at their disposal, but many times using a modality can help accelerate the pain-relieving process for their patients. Pelvic floor physical therapists in particular treat an extremely difficult type of chronic pain loosely classified under the umbrella term "pelvic pain." Pelvic pain can express itself as vulvodynia, clitorodynia, provoked vestibulodynia, pudendal nerve neuralgia, vaginismus and/or dyspareunia. These conditions are common, with 1 in 3 women suffering from pelvic and/or sexual pain in the United States. It is estimated that approximately 30 million suffer from this silent epidemic. As physical therapists we are on the first line of defense and we must be prepared to provide the pain relief that these women so desperately seek.
Physical therapists deal with chronic pain that can be problematic to treat and manage on a daily basis. There is an arsenal of tools, exercises and techniques at their disposal, but many times using a modality can help accelerate the pain-relieving process for their patients. Pelvic floor physical therapists in particular treat an extremely difficult type of chronic pain loosely classified under the umbrella term "pelvic pain." Pelvic pain can express itself as vulvodynia, clitorodynia, provoked vestibulodynia, pudendal nerve neuralgia, vaginismus and/or dyspareunia. These conditions are common, with 1 in 3 women suffering from pelvic and/or sexual pain in the United States. It is estimated that approximately 30 million suffer from this silent epidemic. As physical therapists we are on the first line of defense and we must be prepared to provide the pain relief that these women so desperately seek.
Secret Weapon for Pelvic Pain Is Finally Here
Chronic pelvic pain is very different from other types of pain because it's intimately connected to our emotional, spiritual and psychological states, and can involve the nervous, endocrine, visceral, gynecological, urological and muscular systems. It can be very difficult to treat, and can require anywhere from six months to one year of physical therapy, depending on patient presentation and history.
This lengthy course of treatment requires a fresh approach to therapy and modalities. When I started treating this population I had many difficulties controlling their pain and I had to think differently. Electrical stimulation and ultrasound were not working as well as I'd hoped, providing insufficient pain relief to these patients. I needed a modality that, when incorporated with my pelvic pain treatment, could help produce immediate and long-lasting pain-relieving effects. I needed a modality that could significantly decrease pain within one session, and that my patients could believe in because of the results.
Low-level laser therapy (LLLT) proved to be my secret weapon when treating women with chronic pelvic pain. (I frequently call it "light therapy," because many patients don't like the term "laser.") I have been successfully using light therapy for nearly ten years. It helped my patients keep their pain at bay, and many request that I use it as part of their therapy. I have had incredible patient outcomes when I use LLLT. Of course, for light therapy to work with this difficult population a foundational knowledge and established protocols are required.
LLLT was approved by the FDA in 2002. At that time, the modality was hailed by the New England Patriots and the U.S. Olympic Committee, among others, for its ability to help top athletes quickly return from injury. Endorsements from these organizations piqued my interest and I decided to research its principles. I now know firsthand about the miraculous effects of LLLT. From my own personal experience and from treating thousands of patients I realized that LLLT could be used on many levels.
LLLT is unique: it is a cellular bio-stimulator and is used to increase vitality of cells as well as processes that occur within the cell. The goal with LLLT is to stimulate health and vitality within the cell to produce pain relief, collagen synthesis, anti-inflammatory effects, and endorphin production. Pain- relieving results can be felt in the first visit.
New Look at Low-Level Laser Therapy
My ten years of experience using LLLT have led me to develop low-level laser protocols for female pelvic floor conditions. These protocols are extremely useful for any practitioners wanting to purchase a laser as a new pain-relieving modality for their clinic.
LLLT has changed the way I treat all pain syndromes. It's had such a positive impact that I've created laser protocols for vulvodynia, scar and bladder pain. I also created a special class for the Herman and Wallace Institute program for physical therapists who treat chronic pelvic pain. I encourage any colleagues specializing in this population to investigate this remarkable modality and to attend the online class. If you are looking for something different and a modality that will change the way you treat, come and learn how to use if effectively. My Low-Level Laser Therapy for Female Pelvic Floor Conditions online course incorporates evidence-based science into the low-level laser protocols that you can bring into your practice immediately. This online continuing educational course is designed to provide a thorough introduction to LLLT and its application to female pelvic pain conditions. It is approved for 13 CEU’s and contains ten modules. All ten modules provide step-by-step treatment protocols, videos and PowerPoints. This online class includes protocols for bladder pain, scar pain, coccyx pain, vulvodynia, clitorodynia, provoked vestibulodynia, pudendal nerve neuralgia, vaginismus and dyspareunia.
This new and exciting online class will put you and your practice on the forefront finally providing pain relief for your patients that lasts and improves your outcome measures.
For more info on the low-level laser online training class for female pelvic floor conditions go to www.PelvicPainRelief/laser.
Basford et al. Laser therapy: a randomized, controlled trial of the effects of low-intensity Nd:YAG laser irradiation on musculoskeletal back pain. Arch Phys Med Rehabil (1999) vol. 80 (6) pp. 647-52.
Bjordal et al. A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust J Physiother (2003) vol. 49 (2) pp. 107-16.
Chow et al. The effect of 300 mW, 830 nm laser on chronic neck pain: a double-blind, randomized, placebo-controlled study. Pain (2006) vol. 124 (1-2) pp. 201-10.
Harlow BL, Kunitz CG, Nguyen RHN, et al. Prevalence of symptoms consistent with a diagnosis of vulvodynia: population-based estimates from 2 geographic regions. Am J Obstet Gynecol. 2014; 210:40.
Kostantinovic et al. Low level laser therapy for acute neck pain with radiculopathy: a double-blind placebo-controlled randomized study. Pain Medicine (2010) vol. 11 pp. 1169-1178.
Mathias SD1, Kuppermann M, Liberman RF, et al. Chronic pelvic pain: prevalence, health-related quality of life, and economic correlates. Obstet Gynecol. 1996;87(3):321–327.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/







































