The following is a guest post from Isa Herrera, MSPT, CSCS owner of Renew Physical Therapy in New York, NY. Isa recently launched her new online course "Low Level Laser Therapy For Female Pelvic Pain Conditions" found at www.PelvicPainRelief/laser.
 Physical therapists deal with chronic pain that can be problematic to treat and manage on a daily basis. There is an arsenal of tools, exercises and techniques at their disposal, but many times using a modality can help accelerate the pain-relieving process for their patients. Pelvic floor physical therapists in particular treat an extremely difficult type of chronic pain loosely classified under the umbrella term "pelvic pain." Pelvic pain can express itself as vulvodynia, clitorodynia, provoked vestibulodynia, pudendal nerve neuralgia, vaginismus and/or dyspareunia. These conditions are common, with 1 in 3 women suffering from pelvic and/or sexual pain in the United States. It is estimated that approximately 30 million suffer from this silent epidemic. As physical therapists we are on the first line of defense and we must be prepared to provide the pain relief that these women so desperately seek.
Physical therapists deal with chronic pain that can be problematic to treat and manage on a daily basis. There is an arsenal of tools, exercises and techniques at their disposal, but many times using a modality can help accelerate the pain-relieving process for their patients. Pelvic floor physical therapists in particular treat an extremely difficult type of chronic pain loosely classified under the umbrella term "pelvic pain." Pelvic pain can express itself as vulvodynia, clitorodynia, provoked vestibulodynia, pudendal nerve neuralgia, vaginismus and/or dyspareunia. These conditions are common, with 1 in 3 women suffering from pelvic and/or sexual pain in the United States. It is estimated that approximately 30 million suffer from this silent epidemic. As physical therapists we are on the first line of defense and we must be prepared to provide the pain relief that these women so desperately seek.
Secret Weapon for Pelvic Pain Is Finally Here
Chronic pelvic pain is very different from other types of pain because it's intimately connected to our emotional, spiritual and psychological states, and can involve the nervous, endocrine, visceral, gynecological, urological and muscular systems. It can be very difficult to treat, and can require anywhere from six months to one year of physical therapy, depending on patient presentation and history.
This lengthy course of treatment requires a fresh approach to therapy and modalities. When I started treating this population I had many difficulties controlling their pain and I had to think differently. Electrical stimulation and ultrasound were not working as well as I'd hoped, providing insufficient pain relief to these patients. I needed a modality that, when incorporated with my pelvic pain treatment, could help produce immediate and long-lasting pain-relieving effects. I needed a modality that could significantly decrease pain within one session, and that my patients could believe in because of the results.
Low-level laser therapy (LLLT) proved to be my secret weapon when treating women with chronic pelvic pain. (I frequently call it "light therapy," because many patients don't like the term "laser.") I have been successfully using light therapy for nearly ten years. It helped my patients keep their pain at bay, and many request that I use it as part of their therapy. I have had incredible patient outcomes when I use LLLT. Of course, for light therapy to work with this difficult population a foundational knowledge and established protocols are required.
LLLT was approved by the FDA in 2002. At that time, the modality was hailed by the New England Patriots and the U.S. Olympic Committee, among others, for its ability to help top athletes quickly return from injury. Endorsements from these organizations piqued my interest and I decided to research its principles. I now know firsthand about the miraculous effects of LLLT. From my own personal experience and from treating thousands of patients I realized that LLLT could be used on many levels.
LLLT is unique: it is a cellular bio-stimulator and is used to increase vitality of cells as well as processes that occur within the cell. The goal with LLLT is to stimulate health and vitality within the cell to produce pain relief, collagen synthesis, anti-inflammatory effects, and endorphin production. Pain- relieving results can be felt in the first visit.
New Look at Low-Level Laser Therapy
My ten years of experience using LLLT have led me to develop low-level laser protocols for female pelvic floor conditions. These protocols are extremely useful for any practitioners wanting to purchase a laser as a new pain-relieving modality for their clinic.
LLLT has changed the way I treat all pain syndromes. It's had such a positive impact that I've created laser protocols for vulvodynia, scar and bladder pain. I also created a special class for the Herman and Wallace Institute program for physical therapists who treat chronic pelvic pain. I encourage any colleagues specializing in this population to investigate this remarkable modality and to attend the online class. If you are looking for something different and a modality that will change the way you treat, come and learn how to use if effectively. My Low-Level Laser Therapy for Female Pelvic Floor Conditions online course incorporates evidence-based science into the low-level laser protocols that you can bring into your practice immediately. This online continuing educational course is designed to provide a thorough introduction to LLLT and its application to female pelvic pain conditions. It is approved for 13 CEU’s and contains ten modules. All ten modules provide step-by-step treatment protocols, videos and PowerPoints. This online class includes protocols for bladder pain, scar pain, coccyx pain, vulvodynia, clitorodynia, provoked vestibulodynia, pudendal nerve neuralgia, vaginismus and dyspareunia.
This new and exciting online class will put you and your practice on the forefront finally providing pain relief for your patients that lasts and improves your outcome measures.
For more info on the low-level laser online training class for female pelvic floor conditions go to www.PelvicPainRelief/laser.
Basford et al. Laser therapy: a randomized, controlled trial of the effects of low-intensity Nd:YAG laser irradiation on musculoskeletal back pain. Arch Phys Med Rehabil (1999) vol. 80 (6) pp. 647-52.
Bjordal et al. A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust J Physiother (2003) vol. 49 (2) pp. 107-16.
Chow et al. The effect of 300 mW, 830 nm laser on chronic neck pain: a double-blind, randomized, placebo-controlled study. Pain (2006) vol. 124 (1-2) pp. 201-10.
Harlow BL, Kunitz CG, Nguyen RHN, et al. Prevalence of symptoms consistent with a diagnosis of vulvodynia: population-based estimates from 2 geographic regions. Am J Obstet Gynecol. 2014; 210:40.
Kostantinovic et al. Low level laser therapy for acute neck pain with radiculopathy: a double-blind placebo-controlled randomized study. Pain Medicine (2010) vol. 11 pp. 1169-1178.
Mathias SD1, Kuppermann M, Liberman RF, et al. Chronic pelvic pain: prevalence, health-related quality of life, and economic correlates. Obstet Gynecol. 1996;87(3):321–327.
Today we are honored to present our featured Certified Pelvic Rehabilitation Practitioner Jessica Dorrington, PT, MPT, OCS, PRPC, CMPT, CSCS! Jessica was kind enough to answer a few questions about her role in pelvic rehab.
Describe your clinical practice:
Our clinic practice is an outpatient orthopedic private practice. We are committed to making individual results accessible through compassionate therapeutic care. Our practice spans treating men, women and children through a realm of urologic, gynecologic, obstetric, and colorectal conditions- as well as orthopedic conditions.
 How did you get involved in the pelvic rehabilitation field?
How did you get involved in the pelvic rehabilitation field?
Initially, I was an outpatient orthopedic physical therapist. Within the first few months of my career, the clinic I was working at needed someone to just “teach Kegel exercises”. When I realized the impact that you could have on someone’s life, I was immediately drawn to the pelvic rehabilitation field. I saw getting someone even 75 percent improvement was a whole different success than getting a shoulder patient 75 percent better that could now throw their ball to their dog. It was restoring relationships, saving marriages, and giving women the freedom to go do things they could not do before.
What/who inspired you to become involved in pelvic rehabilitation?
My patients inspire me every day. I initially started treating incontinence patients and then gradually added chronic pain patients to my case load. Each patient that achieved such success with pelvic rehabilitation inspired me to wanting to learn more and reach out to more patient’s in need of physical therapy. This led me into treating men and children with pelvic rehabilitation issues. My favorite story that initially started me on my career path was a 95 year old women who came to me for low back pain. I asked her if she had any incontinence. After 4 visits, she removed a pessary (that she had for the past 55 years-since the birth of her last child) and was painfree and fully continent!
What patient population do you find most rewarding in treating and why?
My favorite patients are those that have seen every specialist and have complex histories. Being able to really listen to their story and give them answers in a health care setting that has not found a solution to their condition is such a wonderful experience. Our professional affords us such a great opportunity to really get to know these patients, dive deep into their history and put the puzzle pieces together for them in a way most professions do not have time for in our current medical model.
If you could get a message out to physical therapists about pelvic rehabilitation what would it be?
As I have grown as a practitioner over the years, the biggest message I have is to really listen to each story. Even a simple SI joint dysfunction patient or a seemingly straight forward stress incontinence patient can have subjective and objective information that really points to the root of the issue. We can really serve these patients the best and premier care if we are up to date on our dermatologic, hormonal influences, musculoskeletal system, and are strong orthopedic clinicians.
What has been your favorite Herman & Wallace Course and why?
Michelle Lyons Athlete and the Pelvic Floor course was wonderful. Michelle is a gifted facilitator of education, has so many pearls of valuable resources and tidbits. She also does a wonderful job combining the orthopedic and pelvic floor world together.
What lesson have you learned from a Herman & Wallace instructor that has stayed with you?
Holly has been truly inspirational to me as she is so passionate about her career and passionate about our profession. Her education on hormones really helps me to sort out for patients when I feel there is a hormonal influence.
What do you find is the most useful resource for your practice?
A pelvic model and Adrian Louw’s Explanation of Pain/Neuroscience education has been such a great resource. For most pelvic pain patient’s there is some sort of sensitive nervous system overlie and the way he educates patients has been lifechanging. The other strong resource has been motivational interviewing education. This allows to really guide these patients in a way that assesses their readiness and motivation for change. The other resource is using the rehabilitative ultrasound imaging. Jackie Whittaker has been such a wonderful mentor to me and this resource has revolutionized the way that I treat diastasis patients, local stabilization, and men and pediatric populations.
What motivated you to earn PRPC?
I am doing more speaking engagements to other medical providers and am doing a lot of mentorship. Being in these roles, I feel having credentials to back the clinical experience is really valuable.
What makes you the most proud to have earned PRPC?
I took the exam without studying, largely because I wanted to see if my skills and knowledge was antiquated (being I have been doing pelvic floor therapy x 14 years). I found the test to be really fun and challenging in an exciting way. The case studies were true examples of the complex patients we treat and so I enjoyed the process.
What advice would you give to physical therapists interested in earning PRPC?
My advice would be to really do some great critical reasoning around your current patients. We learn best by our patients and doing a practice of critically thinking and differential diagnosis around your current patients will give a platform for this. I recalled treating several patients during the examination and could picture very similar patient presentations. The other piece I would recommend is reviewing your anatomy and pharmacology.
What is in store for you in the future?
I am continually blessed to be able to lead a wonderful team of therapists at our outpatient private practice. We are launching a labor and delivery program and post-partum evaluations. Educating the medical community at large has been a focus of mine and I would like to continue to do so to get the word out about pelvic floor PT. I have been asked to speak at the United Nations next Spring and will be presenting about Pelvic Floor in relation to Motherhood Maternity. Mentorship to pelvic floor therapists and students also continues to be a focus.
What role do you see pelvic health playing in general well-being?
I strongly feel pelvic health therapists could play a role in every orthopedic patient’s care. We have so many tools to really evaluate patients from a full body spectrum and have the ability to address any lumbopelvic condition with true depth. Having this vital information about their bodies can really empower all individuals to return to what they love to do in an active healthy lifestyle!
Dr. Steve Dischiavi, MPT, DPT, SCS, ATC, COMT, a Herman & Wallace faculty member, recently co-authored a peer reviewed manuscript which reviewed hip focused exercise programs. Dr. Dischiavi currently teaches a hip related course in the Herman & Wallace curriculum titled “Biomechanical Assessment of the Hip & Pelvis: Dynamic Integration of the Myofascial Sling Systems.”
 "An evidence based review of hip focused neuromuscular exercise interventions to address dynamic lower extremity valgus", published in the Journal of Sports Medicine, presents evidence related to current hip focused interventions within the physical therapy profession. We know that there has been an enormous increase in the amount of hip related diagnoses and surgeries, and this calls for better knowledge from the clinicians on how to manage these particular hip related pathologies. The review finds that insufficient research has been done "to identify and understand the mechanistic relationship between optimized biomechanics during sports and hip-focused neuromuscular exercise interventions... improved strength does not always result in changes to important biomechanical variables, and improved biomechanics in sports-related tasks does not necessarily equal improved biomechanical variables in performance of the sport itself".
"An evidence based review of hip focused neuromuscular exercise interventions to address dynamic lower extremity valgus", published in the Journal of Sports Medicine, presents evidence related to current hip focused interventions within the physical therapy profession. We know that there has been an enormous increase in the amount of hip related diagnoses and surgeries, and this calls for better knowledge from the clinicians on how to manage these particular hip related pathologies. The review finds that insufficient research has been done "to identify and understand the mechanistic relationship between optimized biomechanics during sports and hip-focused neuromuscular exercise interventions... improved strength does not always result in changes to important biomechanical variables, and improved biomechanics in sports-related tasks does not necessarily equal improved biomechanical variables in performance of the sport itself".
Biomechanical Assessment of the Hip & Pelvis is an opportunity to explore manual movement therapy with a skilled researcher and practitioner. Dr. Dischiavi has woven a very creative and innovative philosophy to help clinicians design more comprehensive hip focused therapeutic interventions. His in-depth knowledge of the evidence has allowed him to create a program that will challenge clinicians in new ways to look at the hip, pelvis, and lower extremity and how the kinetic chain can be influenced by approaching it using a new lens.
Participants of his course will learn new ways to activate and strengthen groups of pelvic muscles that will benefit all patients from pelvic health clients, to professional athletes, to your elderly population. “All patients have the same bones, muscles, and gravitational pulls acting on them, its how they use these systems that varies significantly. A philosophical science can be generated, but the art is in implementing that science.”
Participants in the Biomechanical Assessment of the Hip & Pelvis course have enjoyed being challenged to look at the hip and pelvis in a different way. Practitioners will leave the course having learned a whole new way to develop and implement therapeutic exercises which are a different approach from the single plane non-weight bearing exercises that are traditionally prescribed to patients.
There are many courses and philosophies on how to screen for lower extremity injuries and how to evaluate movement dysfunction. What is really lacking for clinicians are options for therapeutic exercises which target the hip and pelvis in a relevant and functional manner. Most hip focused programs currently emphasize single plane movements and are dominated with concentric focused exercise. Dr. Dischiavi’s focus is targeted directly at human movement emphasizing tri-planar movements that are primarily eccentric in nature, recognizing that this is how the human body functions.
Come to the Biomechanical Assessment of the Hip & Pelvis: Manual Movement Therapy and the Myofascial Sling System in Seattle this June, or in Boston this August!
Congratulations to Dr. Sarah Capodagli, DPT, our featured practitioner of the week! Dr. Capodagli owns and operates CorrEra Physical Therapy, and she is in the process of expanding her practice in Buffalo, NY. We were curious to hear more from her about running a practice in Buffalo, and Sarah was kind enough to write in. Thanks, Sarah!
 Although Buffalo is considered the second largest city in the state of New York, we often operate like a small town. We value community and for just about any business, the best marketing tool is word of mouth. If you need a new roof, new car, or a good doctor, well, ask around and I guarantee that you will find someone who “knows a guy,” to help or advise. I cannot speak for every city, though when I think of Buffalo, NY, I think of family. When you see your family in need, you help.
Although Buffalo is considered the second largest city in the state of New York, we often operate like a small town. We value community and for just about any business, the best marketing tool is word of mouth. If you need a new roof, new car, or a good doctor, well, ask around and I guarantee that you will find someone who “knows a guy,” to help or advise. I cannot speak for every city, though when I think of Buffalo, NY, I think of family. When you see your family in need, you help.
A few years ago I was working in a large oncology hospital and one of my primary roles was running the pelvic floor rehabilitation program for men living with or being treated for prostate cancer. I loved this work; however, I saw greater need in our community for not only the proper conservative care and treatment, but also for the information about pelvic health to be shared more publicly with men and women. Although opening my own clinic in a suburb of this “City of Good Neighbors” was not always the plan, when given the opportunity to grow into my own practice by a chiropractor friend, I jumped at the chance and have never looked back. It was a big jump, but for me, the fear of regret in never trying was so much worse than the fear of failure.
The greatest challenge was in actually starting my practice and beginning to educate the community and physicians. In a larger metropolis there is more awareness of this specialty and referrals come more naturally when conservative options are made known to patients. In the beginning I reached out to a mentor, utilized many tools available on the Herman & Wallace website, held free community events, and spent my first few months focused on networking. Once introduced to some fabulously conservative docs, birthing professionals, and physical therapists who were aware of the benefits of pelvic floor rehab, I really started to see the growth. I became an advocate for patients – a navigator in this sometimes confusing and frustrating system. People want conservative options and when happy patients return to their physicians with improved symptoms and quality of life, well, now your reputation establishes you as one of the “go-to” practitioners in the community.
Though patience and persistence are crucial in this process of growth, I’m also a firm believer that, as Dr. Francis Peabody stated, “the secret of the care of the patient is in caring for the patient.” This belief is what sets me apart, and in a small community this is what really matters. One of my favorite books is The Go-Giver by Bob Burg and John D. Mann. I always want my practice and the growth of my business to reflect the strategies of value, service, influence, and authenticity emphasized in this story. In a community where community is valued, I truly believe that if you stay teachable and positive, the care you put into your practice will always pay off.
Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC is a published researcher and practitioner who has worked in the realms of brain injury, lymphedema, and oncology. Now she's leading the charge to encourage rehabilitation practitioners to utilize ultrasound diagnostic imaging with their patients, and you can learn these techniques in her Rehabilitative Ultrasound Imaging - Women's Health and Orthopedic Topics course taking place May 1 - 3 in Dayton, OH. We've partnered with SonoSite to make the best ultrasound equipment available for participants in this course.
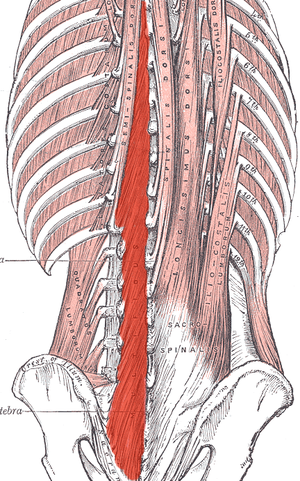 Most of us are treating patients who have back pain of some nature, and we know the importance of the local stabilizing muscles including the transverse abdominis, the lumbar multifidus, and the pelvic floor muscles. These muscles work together to provide tension and create a corset of stability throughout the trunk. A common goal is to rehabilitate these muscles in order to restore motor control and strength, but the muscle depth can make them difficult to assess and palpate.
Most of us are treating patients who have back pain of some nature, and we know the importance of the local stabilizing muscles including the transverse abdominis, the lumbar multifidus, and the pelvic floor muscles. These muscles work together to provide tension and create a corset of stability throughout the trunk. A common goal is to rehabilitate these muscles in order to restore motor control and strength, but the muscle depth can make them difficult to assess and palpate.
I recently read a study that is looking at the development of a test to identify lumbar multifidus function. Herbert et al. found promising results when looking at this “multifidus lift test” for inter-rater reliability and concurrent validity to identify dysfunction in the multifidus. They compared the results of this test with real-time ultrasound imaging of the lumbar multifidus. Inter-rater reliability was excellent and free from errors of bias and prevalence. Concurrent validity was demonstrated through its relationship with the reference standard results at L4-L5, but not so much for L5-S1. This preliminary research supports the reliability and validity of the multifidus lift test to assess lumbar multifidus function at some spinal levels. If this test could be further validated for other spinal levels it would be very beneficial for therapists who are using a specific stabilization program to treat patients.
Until this test is further developed and validated how can therapists know for sure that their patient is truly activating their multifidus? Ultrasound imaging is the answer! Ultrasound imaging gives therapists real-time feedback for whether a patient is able to correctly activate a muscle or not. It is also a wonderful biofeedback tool for patients who are trying to rehabilitate these muscles. Getting your hands on an ultrasound machine can be tough, but therapists who work in a hospital system may have an easier time than you'd think. I have worked with many therapists to help them get access to ultrasound units through “hand me down” units from imaging or labor and delivery departments. I also have helped private practice therapists set up a working relationship with a physician who has an ultrasound in their office. Thinking outside of the box can allow clinicians to gain access to ultrasound units without having to spend a lot of money. Join me in Dayton Ohio this May to hear more about how ultrasound imaging can improve your practice and allow you to incorporate a specific stabilization program into your toolbox.
Herbert JJ, Koppenhaver SL, Teyhen DS, Walker BF, Fritz JM. The evaluation of lumbar multifidus muscle function via palpation: reliability and validity of a new clinical test. Spine J. 2015; 15(6): 1196-202.
The following comes to us from Carolyn McManus, PT, MS, MA, our resident expert in the power of mindfulness and it's applications to rehabilitation. Carolyn was recently featured in a video from the Journal of the American Medical Association for her contributions to a newly published research article. Join Carolyn at her course, Mindfulness Based Pain Treatment: A Biopsychosocial Approach to the Treatment of Chronic Pain on May 14th and 15th in California's Bay Area!
 Neuroimaging studies show that cortical and sub-cortical brain regions associated with cognitive and emotional processing connect directly with descending pain modulating circuits arising in the brainstem. As diminished nociceptive inhibition by descending pain modulation is a likely contributing factor to the persistence of pain, these cortical and sub-cortical connections to relevant brainstem regions provide a means by which maladaptive cognitive and emotional processing can contribute to the persistence of pain1. It is possible that strategies to help patients self-regulate cognitions and emotions could promote pain reduction through restoring the balance between excitatory and inhibitory mechanisms of the descending pain modulatory system.
Neuroimaging studies show that cortical and sub-cortical brain regions associated with cognitive and emotional processing connect directly with descending pain modulating circuits arising in the brainstem. As diminished nociceptive inhibition by descending pain modulation is a likely contributing factor to the persistence of pain, these cortical and sub-cortical connections to relevant brainstem regions provide a means by which maladaptive cognitive and emotional processing can contribute to the persistence of pain1. It is possible that strategies to help patients self-regulate cognitions and emotions could promote pain reduction through restoring the balance between excitatory and inhibitory mechanisms of the descending pain modulatory system.
To be mindful is to rest the mind in the present moment with stability and acceptance and without additional cognitive or emotional elaboration. Mindful body awareness is a central component. Training in mindful awareness has been shown to improve attention regulation, emotional processing and body awareness and contribute to reduced pain intensity, catastrophizing, depression and anxiety2,3,4,5. Training in mindfulness has also been shown to modulate brain activity in areas associated with body awareness and pain processing6,7. It is possible that the adaptive modulation of cortical and sub-cortical areas engaged with mindful cognitive, emotional and physical self-regulation could contribute to reducing pain through improving the balance between excitatory and inhibitory mechanisms of the descending pain modulatory system.
One of my patients reflected the clinical benefits of mindfulness training when he said, “I needed to learn how to not freak out when my exercises or daily activities increased my pain. Focusing my mind on the present moment was enormously helpful. I would tell myself, “Breathe. Just be here. Calm down.” By breathing and relaxing I could take control of how I was reacting and I immediately saw a difference. My pain did not increase out of control.”
I am thrilled to be sharing my 30+ year experience in mindfulness and patient care in my upcoming course through Herman and Wallace.
1. Ossipov M, Morimura K, Porreca F. Descending pain modulation and chronification of pain. Curr Opin Support Palliat Care 2014;8(2):143-151.
2. Holzel BK, Lazar SW, Guard T, et al. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect Psychol Science. 2011;6: 537–559.
3. Reiner K, Tibi L, Lipsitz JD. Do mindfulness-based interventions reduce pain intensity? A critical review of the literature. Pain Med. 2013 Feb;14(2):230-42.
4. Lakhan SE, Schofield KL. Mindfulness-based therapies in the treatment of somatization disorders: a systematic review and meta-analysis. PLoS One. 2013 Aug 26;8(8):e71834.
5. Schutze , Slater H, O’Sullivan P, et al. Mindfulness-based functional therapy: A preliminary open trial of an integrated model of care for people with persistent low back pain. Front Psychol. 2014 Aug 4;5:839.
6. Zeidan F, Martucci KT, Kraft RA, et al. Brain mechanisms supporting modulation of pain by mindfulness meditation. J Neurosci. 2011 Apr 6;31(14):5540-8.
7. Nakata H, Sakamoto K, Kakigi R. Meditation reduces pain-related activity in the anterior cingulated cortex, insula, secondary somatosensory cortex and thalamus. Front psychol. 2014;5:1489.
“Please stress the need to examine men…For some reason, most female PT`s shy away from a male’s private parts totally. It would be great if females were taught that it's important to go there…And treat us as equals in this arena.”
 This is an excerpt from a recent email we received at Herman & Wallace headquarters, and it highlights a common theme, that of patient access to care. While there are many factors driving patient access to pelvic health, availability of therapists trained in various conditions is certainly one major issue. By the time any patient is referred to pelvic rehabilitation, they have already overcome the challenge of many providers not being aware that there is help for pelvic health issues, and insurance or payment hurdles that can also cause a patient to delay or avoid recommended treatment. Many physical therapy programs have done an outstanding job in developing and marketing women’s health programs, with men’s health programs addressing post-prostatectomy care or male pelvic pain coming along almost as an afterthought.
This is an excerpt from a recent email we received at Herman & Wallace headquarters, and it highlights a common theme, that of patient access to care. While there are many factors driving patient access to pelvic health, availability of therapists trained in various conditions is certainly one major issue. By the time any patient is referred to pelvic rehabilitation, they have already overcome the challenge of many providers not being aware that there is help for pelvic health issues, and insurance or payment hurdles that can also cause a patient to delay or avoid recommended treatment. Many physical therapy programs have done an outstanding job in developing and marketing women’s health programs, with men’s health programs addressing post-prostatectomy care or male pelvic pain coming along almost as an afterthought.
So what is really limiting the care of men who wish to overcome urinary, pain, or sexual dysfunction? For many locations around the country, there simply is not enough awareness of the scope of pelvic rehab, the nearest pelvic rehab provider may be far away geographically (or have a months-long waiting list), or the clinic may limit pelvic healthcare to women. If the clinic chooses to only provide care to women, what are we being discriminating about? The word “discriminate” has at least two rather distinct definitions, one that is more negative, and meaning that we are acting in an unjust or prejudicial manner, and another that simply means we are recognizing a difference between patient groups. If we choose to discriminate against treating men in a pelvic health setting, it’s easy to understand that if a therapist has never been instructed in how to examine a male patient, it may be prudent to avoid such evaluation until training is completed. We can find examples of this situation in other aspects of clinical care: if I have never taken proper training in evaluation of the vestibular system, for example (a condition that historically has not always been comprehensively instructed in school), then it’s in my best interest (and that of the patient) to only provide such care once I have taken appropriate training.
If our care of male pelvic health conditions is due to lack of specific training, what is our professional responsibility for acquiring training in conditions such as post-prostatectomy urinary incontinence, male genital pain, or erectile dysfunction? If we are to serve the pelvic health populations well, our training should progress to include lifespan issues for all ages and all genders. If we actively choose to avoid treating a population or condition, is that fair to the community seeking care? The ethics of choosing not to treat patients of a particular gender or condition are interesting to consider, but are not the scope of this post. On the other hand, the business side of being able to market to and welcome male patients in our clinics is very positive, and of course, all of our patients tend to be grateful for what we offer.
If you are interested in learning more about male pelvic healthcare, the Institute has several courses that can help you do so. These courses include an introduction to men at the Pelvic Floor Level 2A course, the Male Pelvic Floor: Function, Dysfunction and Treatment course (3 days dedicated to evaluation and treatment of urinary, sexual, and pain dysfunction), the Post-Prostatectomy course, as well as several manual therapy courses such as our myofascial courses. It is understandable that pelvic health for men may be less familiar territory for many of us based on our graduate training and experiences. If fear or discomfort is holding us back, at least attending a training course can help provide strategies and tools for gaining more comfort in treating men. We are at an exciting time in the pelvic health field when treating men is gaining more ground. If you are not already, join this exciting movement by signing up for one of the many classes available to you!
Faculty member Lila Bartkowski- Abbate PT, DPT, MS, OCS, WCS, PRPC teaches the Bowel Pathology, Function, Dysfunction and the Pelvic Floor course for Herman & Wallace. Join her in Tampa on April 2-3, or one of the other two events currently open for registration.
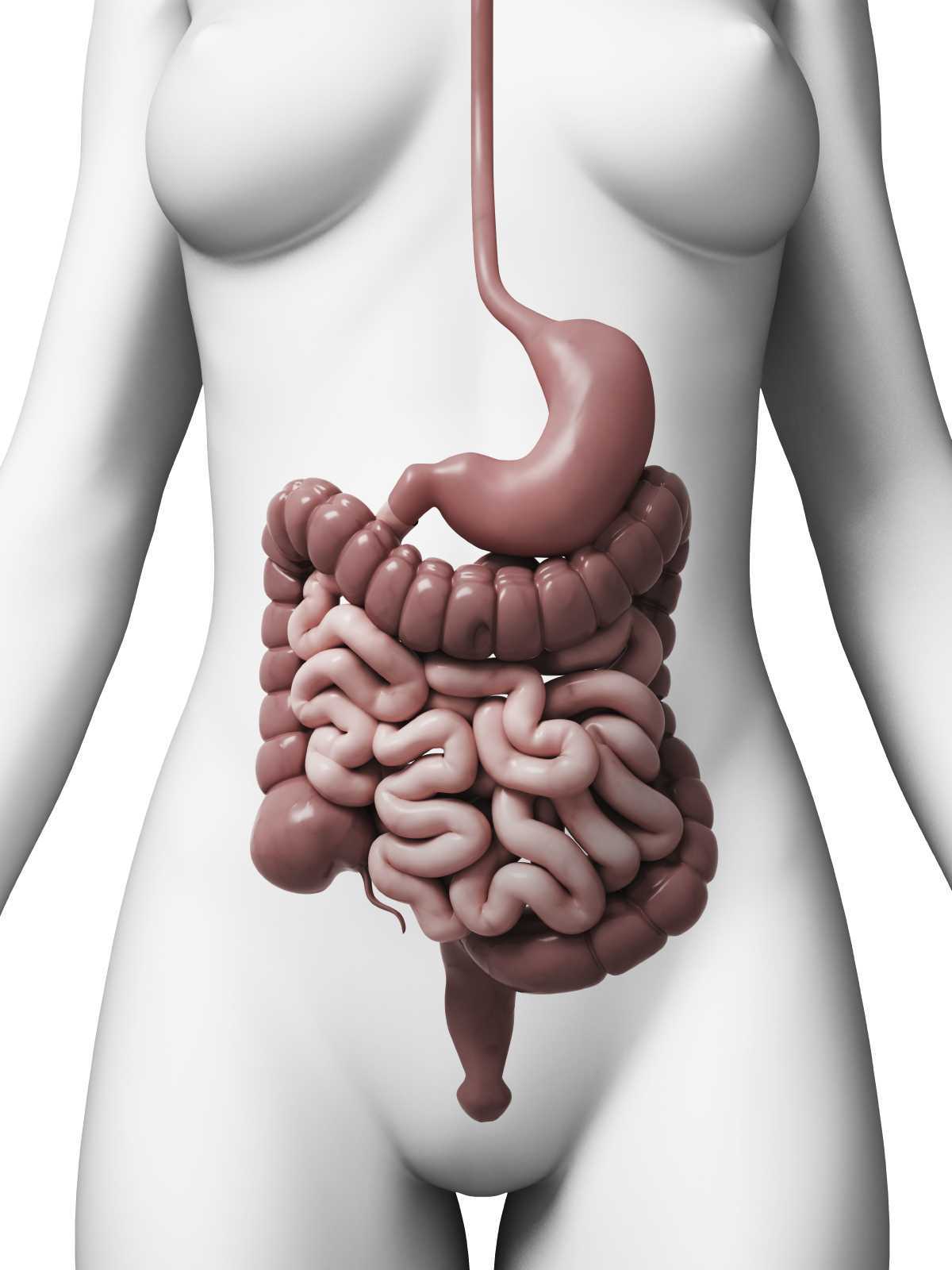 Constipation, an often under reported health issue, afflicts about 30% of Americans. ¹ The diagnosis of chronic constipation may seem like a simple concept, however the etiology of chronic constipation presents itself in many different forms. Dyssynergic defecation is one of many factors that can lead to a presentation of chronic constipation in a patient. Dyssynergic defecation or “paradoxical contraction” occurs when the muscles of the abdominals, puborectalis sling, and external anal sphincter function inappropriately while attempting a bowel movement. ² The lack of coordination of these muscles results in a contraction versus a lengthening of the pelvic floor muscles with baring down. Dyssynergic defecation is different than a structural issue such as a rectocele or hemorrhoids causing the inability to pass stool effectively or constipation due to slow colon transit time or pathological disease. Making the diagnosis of dyssynergic defecation by symptoms alone is often not reliable secondary to overlap of similar symptoms with chronic constipation due to factors such as a structural issue, irritable bowel syndrome (IBS), or irritable bowel disease (IBD). The diagnosis of dyssynergic defecation can be difficult and is often made through physiologic testing such as balloon expulsion testing or MRI with defecography. ² However, physical therapists can often manually feel that a paradoxical contraction is happening when asking a patient to bare down on evaluation.
Constipation, an often under reported health issue, afflicts about 30% of Americans. ¹ The diagnosis of chronic constipation may seem like a simple concept, however the etiology of chronic constipation presents itself in many different forms. Dyssynergic defecation is one of many factors that can lead to a presentation of chronic constipation in a patient. Dyssynergic defecation or “paradoxical contraction” occurs when the muscles of the abdominals, puborectalis sling, and external anal sphincter function inappropriately while attempting a bowel movement. ² The lack of coordination of these muscles results in a contraction versus a lengthening of the pelvic floor muscles with baring down. Dyssynergic defecation is different than a structural issue such as a rectocele or hemorrhoids causing the inability to pass stool effectively or constipation due to slow colon transit time or pathological disease. Making the diagnosis of dyssynergic defecation by symptoms alone is often not reliable secondary to overlap of similar symptoms with chronic constipation due to factors such as a structural issue, irritable bowel syndrome (IBS), or irritable bowel disease (IBD). The diagnosis of dyssynergic defecation can be difficult and is often made through physiologic testing such as balloon expulsion testing or MRI with defecography. ² However, physical therapists can often manually feel that a paradoxical contraction is happening when asking a patient to bare down on evaluation.
Patients with dyssynergic defecation may present to pelvic floor physical therapy with complaints of: ¹ ²
- Abdominal symptoms such as bloating, pain, and cramping
- Poor response to laxatives and fiber supplementation that does not fully resolve their issue
- Have had testing for anatomical or neurological abnormalities with no significant findings
- Complaints of concomitant pelvic pain due to over activity of the pelvic floor muscles
Physical Therapists specializing in pelvic floor rehab can be a valuable part of the medical team with treating these patients. Biofeedback training by physical therapists has been shown to decrease anorectal related constipation symptoms and abdominal symptoms in patients with dyssynergic defecation. In a sample of 77 patients with dyssynergic defecation, physical therapists provided biofeedback training for 6-8 weeks that included manual and verbal feedback, surface EMG, exercises using a rectal catheter, rectal ballooning to improve rectal sensory abnormalities, ultrasound, pelvic floor and abdominal massage, electrical stimulation if needed, and core strengthening and stretching to improve the patients’ maladaptive habits while attempting to pass a bowel movement. Significant decreases were seen on all three domains (abdominal, rectal, and stool) on the PAC-SYM (Patient Assessment of Constipation) questionnaire post biofeedback training. ² It is noteworthy that 74% of these patients presented to the clinic with complaints of abdominal symptoms such as bloating, pain, discomfort, and cramping.
Knowing how to effectively treat these patients and ask the right questions is valuable in the scheme of pelvic floor rehab secondary to overlapping symptoms of different causes of chronic constipation. Physical therapists are able to provide these patients with conservative treatment that can effectively improve or eliminate their problem, recognize dyssynergic defecation as a possible differential diagnosis, and refer to the appropriate medical professional for further testing. Recognizing and treating dyssynergic defecation is something physical therapists will learn how to become effective at in the upcoming Herman and Wallace Course: Bowel Pathology, Function, Dysfunction & the Pelvic Floor April 2-3 in Tampa, FL and October 8-9 in Fairfield, CA.
1. Sahin M, Dogan I, Cengiz M et al. (2015). The impact of anorectal biofeedback therapy on quality of life of patients with dyssynergic defecation. Turk J Gastroenterol. 26(2):140-144
2. Baker J, Eswaran S, Saad R, et al. (2015). Abdominal symptoms are common and benefit from biofeedback therapy in patients with dyssynergic defecation. Clin Transl Gastroenterol. 30(6)e105. doi: 10.1038/ctg.2015.3
Many therapists start their career feeling a bit intimidated to work with women who are pregnant. A common and understandable concern is that something the therapist will do during examination or treatment may harm the patient. While there are certainly things to avoid when working with a patient who is pregnant there are also many therapeutic strategies that can help a woman thrive during her pregnancy and beyond. When women have pre-existing issues such as a disease or physical challenge, or when she develops an illness during pregnancy, the therapist needs to rely upon more knowledge- this knowledge is something she rarely learns in school, but more likely in continuing education environments. A recent article asked the question “are women getting sicker, and are there more high-risk pregnancies now than ever before?”
 Researchers studied trends in maternal morbidity and mortality in the United States in order to answer this question, and the answer is a definitive “yes”. Several studies describe increases in the rates of maternal morbidity, with issues such as cardiac and pulmonary complications, and the severe blood pressure fluctuations associated with eclampsia. Gestational diabetes, and postpartum rates for hemorrhage, perineal lacerations, and maternal infections have also risen. Part of the reason for more women carrying pregnancies more successfully or longer when they are ill may be contributed to newer treatments for conditions such as diabetes, yet this does not explain entirely the increase in maternal morbidity. Increased cesarean births, longer labors with epidural anesthesia, pre-pregnancy obesity, rates of multifetal pregnancies, and the rising age of mothers are other factors to be considered.
Researchers studied trends in maternal morbidity and mortality in the United States in order to answer this question, and the answer is a definitive “yes”. Several studies describe increases in the rates of maternal morbidity, with issues such as cardiac and pulmonary complications, and the severe blood pressure fluctuations associated with eclampsia. Gestational diabetes, and postpartum rates for hemorrhage, perineal lacerations, and maternal infections have also risen. Part of the reason for more women carrying pregnancies more successfully or longer when they are ill may be contributed to newer treatments for conditions such as diabetes, yet this does not explain entirely the increase in maternal morbidity. Increased cesarean births, longer labors with epidural anesthesia, pre-pregnancy obesity, rates of multifetal pregnancies, and the rising age of mothers are other factors to be considered.
The more we know as health care providers about how maternal morbidity affects our rehabilitation efforts, the more we can contribute to a woman’s pregnancy and postpartum health. If you would like to learn more about caring for women during pregnancy and during the postpartum period, Herman & Wallace offers the Pregnancy and Postpartum Series. The following courses are available this year:
Care of the Pregnant Patient - Somerset, NJ
Apr 30, 2016 - May 1, 2016
Care of the Pregnant Patient - Akron, OH
Sep 10, 2016 - Sep 11, 2016
Peripartum Special Topics - Seattle, WA
Nov 12, 2016 - Nov 13, 2016
Tillett, J. (2015). Increasing Morbidity in the Pregnant Population in the United States. The Journal of perinatal & neonatal nursing, 29(3), 191-193.
Faculty member, Ginger Garner PT, L/ATC, PYT will be giving 2 lectures at this year’s annual Montreal International Symposium for Therapeutic Yoga, or MISTY for short, in Montreal, Quebec. The first is a 2-hour lecture titled, Vocal Liberation, and the second is a 4-hour lecture titled, Hip Preservation: Yoga Reconsidered, Visit http://www.homyogaevents.com to learn more.
 Yoga is, unarguably, a popular contemplative science, enjoying 36.7 million practitioners in the US alone, up from 20.4 million in 2012.1 A 16 billion dollar industry, yoga is one of the most widely utilized methods of complementary and integrative medicine in America today. In 2008, the editor of Yoga Journal declared “yoga as medicine” as the next great wave. That was right in the middle of the Great Recession, when the last thing on the collective healthcare industry’s mind was yoga.
Yoga is, unarguably, a popular contemplative science, enjoying 36.7 million practitioners in the US alone, up from 20.4 million in 2012.1 A 16 billion dollar industry, yoga is one of the most widely utilized methods of complementary and integrative medicine in America today. In 2008, the editor of Yoga Journal declared “yoga as medicine” as the next great wave. That was right in the middle of the Great Recession, when the last thing on the collective healthcare industry’s mind was yoga.
What happened during the same time frame as the interest in yoga surged?
Our expanded knowledge of hip anatomy, physiology, and pathophysiology exploded onto the medical scene, providing more information than ever about how to address, preserve, and otherwise attend to the hip joint. Prior to this new age of research, the hip was relegated to a joint worthy of no more than a tendonitis, bursitis, or osteoarthritis diagnosis. A person was simply a hip replacement candidate or not. There was no other option once a hip joint had prematurely degenerated. Now, that has all changed, thanks to technological advances in diagnostic testing and investigation.
Yet, the worlds of hip preservation and rehabilitation and yoga have yet to join hands. Many of my patients and colleagues have suffered from unnecessary hip injuries, from labral tears, all types of impingement, and compounding secondary diagnoses such as torn hamstrings, sports hernias, gluteal tendinopathy, to pelvic pain, all due to yoga practice. Some suffered injuries in yoga class during a single traumatic injury, and some injuries were drawn out over years of accumulated microinjury to capsuloligamentous, bony, or cartilaginous structures.
Hip labral injuries (HLI) have vastly increased over the last 10 years, perhaps making HLI the newest orthopaedic diagnosis of the 21st century. This discovery also makes surgical and conservative management of HLI uncharted territory. Conservative therapy includes nonsurgical and post-surgical rehabilitation, and since the average time from injury to diagnosis is 2.5 years, there are many people with hip, pelvic, back, or sacroiliac joint pain that have undiagnosed hip labral tears.
I should make myself quite clear, however. I am not out to demonize yoga or fear-monger the practice of yoga or how it may wreck a person’s body (to use recently controversial language).
My purpose is two-fold: To clarify 1) “what” and “how” yoga can be a safe, effective form or physical therapy and rehabilitation for the hip and pelvis, as well as to 2) underscore the areas where yoga posture practice should be evolved to prevent injury.
To that end, I have written and will be presenting a new 4-hour workshop entitled, Hip Preservation: Yoga Reconsidered, at the Montreal International Symposium on Therapeutic Yoga (MISTY) this weekend in Canada. The lecture is relevant for yoga teachers, yoga enthusiasts, yoga therapists, and health care professionals who are interested in learning how to prevent hip injury in yoga practice.
The workshop will introduce identification of imbalances that could contribute to HLI, as well as understand the common mistakes made in yoga practice that could increase HLI or hip impingement. Understanding the pain patterns that surround HLI are also critical to safe and therapeutic yoga practice and will be discussed. Discussion of structure, function, ability and “dis”ability of the hip, including their major substrates, will help identify the “red flags” in yoga practice, identifying high risk populations and those who need postural modification(s) and/or outside referral to physical therapy.
I am looking forward to instructing a high energy, action-packed hands-on learning session at MISTY on March 19-20, along with my presenting a 2-hour lecture on maximizing public speaking impact through Vocal Liberation: The Voice as Therapy.
- The Voice as a Linking Science for Clinical and Business Efficacy
- Hip Preservation: Yoga Reconsidered
- Ginger’s lecture overview - Montreal International Symposium for Therapeutic Yoga
Want to learn more?
Bring Ginger’s 16 hour continuing education course, Differential Diagnosis for Hip Labral Injuries to your facility in 2017 through Herman & Wallace Pelvic Rehabilitation Institute.
Yoga in America 2016 Survey. Yoga Alliance and Yoga Journal. January 2016.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/






































