Holly Tanner Short Interview Series - Episode 6 featuring Sandra Gallagher
In today’s interview, Sandra discusses some of the intricacies of working with transitioning patients, her path in working with the LGBTQ+ community, and her new course with H&W. Transgender Patients: Pelvic Health and Orthopedic Considerations is a remote course created by Sandra Gallagher and Caitlin Smigelski. This course provides specific content aimed at teaching pelvic health therapists how to expand their skills for working with people of all gender identities.
Sandra Gallagher has served on varied committees and boards at the state and national level, most recently as the chair of the CAPP-OBC committee for the Academy of Pelvic Health of the APTA. She has presented on the role of PT in gender-affirming vaginoplasty at UCSF Transgender Health Summit, APTA Combined Sections Meeting, and at the 2018 international meeting of the World Professional Association for Transgender Health (WPATH).
In a research study that Sandra facilitated with other colleagues, it was concluded that “Pelvic floor physical therapists identify and help patients resolve pelvic floor-related problems before and after surgery. We find strong support for pelvic floor PT for patients undergoing gender-affirming vaginoplasty.”(1)
Often therapists think of genital surgeries and sexual function when contemplating work with transgender people. However, therapists have far more to offer transgender patients. For providing optimal care, knowledge of the intricacies of gender transition is essential.
Join H&W on October 30th for Transgender Patients: Pelvic Health and Orthopedic Considerations to learn more about gender-affirming genital surgeries and medical interventions that people transitioning might choose.
- David Jiang, Sandra Gallagher, Laura Burchill, Jens Berli, Daniel Dugi 3rd. Implementation of a Pelvic Floor Physical Therapy Program for Transgender Women Undergoing Gender-Affirming Vaginoplasty. Obstet Gynecol. 2019 May;133(5):1003-1011. doi: 10.1097/AOG.0000000000003236.
Holly Tanner Short Interview Series - Episode 5 featuring Sarah Haran
This week The Pelvic Rehab Report sat down with new faculty member Sarah Haran. Sarah instructs the new Weightlifting and Functional Fitness Athletes remote course scheduled for October 16, 2021.
Who are you? Describe your clinical practice.
My name is Sarah Haran and I have been a PT in Seattle, WA since 2007. I graduated from the University of Washington and have been working in outpatient orthopedics ever since. I opened my private, cash practice, Arrow Physical Therapy in 2016 and we specialize in CrossFit athletes, weightlifters, dancers, and patients with hip impingement. I also teach courses on practice development and coach physical therapist entrepreneurs alongside Dr. Kate Blankshain through our business consulting company, Full Draw Consulting.
What made you want to create this course?
My course, Weightlifting and Functional Fitness Athletes, will begin to fill a hole in the training we have as PTs. I was unaware of how to help higher-level athletes until I became a CrossFit athlete myself. In my practice, I have learned that not only are there not enough PTs who understand weightlifting and the "sport of fitness" as CrossFit is called but that there is even some negativity around the sports. The truth is that these activities are not going anywhere and if anything are gaining popularity. We must figure out how to serve these patients and keep them just as healthy as any other patient. I am not a pelvic therapist but I do have a great interest in hip impingement which means that I refer out to pelvic floor PTs quite commonly. It is a privilege to be able to work with these therapists in this course and I look forward to learning from the students too!!
What are some pelvic health concerns with Crossfit, and what is the role of the practitioner?
Pelvic health concerns in Crossfit athletes include urinary function, hip impingement, pelvic pain, prolapse and pressure control aspects, diastasis, and pregnant/postpartum athletes. Urinary function and diastasis are especially not understood by coaches and tend to either be not addressed or referred out. The practitioner's role for these athletes is to be understanding of the language and to be respectful of the athletes. Practitioners can support the athletes by understanding the sport and the movements involved, by helping the athlete modify versus stopping the movements/exercises. This can help the athlete maximize their sports performance while demonstrating that physical therapy is appropriate for their needs.
What does it mean when people say Crossfit is the sport of fitness?
Different types of athletes belong in different categories and it is really hard to compare those categories. With Crossfit, we say we need to include all of these components, and the person that best executes all of these things is the fittest. Crossfit is essentially the sport of fitness. The 10 components of physical exercise that are included in Crossfit are coordination, strength, stamina, flexibility, power, speed, accuracy, agility, balance, and endurance (cardiovascular/respiratory).
Is Crossfit an inclusive sport?
Yes. Crossfit is considered very inclusive. While intensity is the name of the game with Crossfit. Crossfit is also a brand, a workout, and a lifestyle. Nutrition and exercise are prioritized in this community and can be scaled across the lifespan and all ability levels. When looking at Crossfit, fitness is defined as constantly varied functional movements executed at high intensity across broad time and modal domains. In this same vein, health is defined as work capacity across broad time, modal, and age domains. Essentially health is fitness measured across your lifetimE. Crossfit is very inclusive in that it is all ages, all abilities, and is supportive of LGBTQA+ positive. Competitions are inclusive with adaptive categories, And the movement is also involved in Black Lives Matter and with Veterans.
To learn more about working with this population join H&W and Sarah Haran at Weightlifting and Functional Fitness Athletes remote course scheduled for October 16, 2021.
Holly Tanner Short Interview Series - Episode 4 featuring Brianna Durand
Inclusive Care for Gender and Sexual Minorities is a remote course created by faculty member Brianna Durand. This course is for anyone, even if you are unsure about the pronouns or the terminology to use. Brianna created this course to provide the basic foundational knowledge around inclusive and gender-affirming care. The second day of the course provides detailed physiological considerations from the pelvic health and general health standpoint for folx undergoing medical transition.
Brianna became interested in pelvic health research pertaining to the LGBTQ+ community when she was in grad school. She was struck by how the community was not mentioned in most formal education and wanted to meet this knowledge gap.
Gender-affirming care describes ideal medical, surgical, and mental health services sought by transgender, non-binary, and gender non-conforming people. This can range from hormone therapy, to top or bottom surgery, facial hair removal, modification of speech, reduction thyrochondroplasty (tracheal cartilage shave), and voice surgery (1). Also common is the practice of genital tucking or packing, and chest binding. All of which the World Professional Association for Transgender Health lists as medically necessary procedures(2).
Hormone therapy is a common medical intervention and allows for the acquisition of secondary sex characteristics which are more aligned with the individual's gender identity. Research, such as that by Gómez-Gil et al, concludes that there are psychological improvements after gender-affirming treatments such as hormone therapy and surgery (3). Likewise, the denial of access to gender-affirming care is associated with worsened psychological health and high-risk behaviors (4).
Inclusive Care for Gender and Sexual Minorities attendees can expect to be gently guided into the sometimes confusing realm of gender and sexual orientation and identity. This course will provide a safe space to ask all the questions about caring for LGBTQ+ patients and practicing the skills needed to help advance your practice.
Inclusive Care for Gender and Sexual Minorities is scheduled for October 9-10 and covers pelvic floor physical therapy specifically, however it is appropriate and useful for any medical professional as we all have patients in the LGBTQ+ community.
- Madeline B. Deutsch, MD, MPH. Overview of gender-affirming treatments and procedures. UCSF Transgender Care & Treatment Guidelines. June 17, 2016
- WPATH Clarification on Medical Necessity of Treatment, Sex Reassignment, and Insurance Coverage for Transgender and Transsexual People WorldwideWPATH. Transgender Health Information Program. [cited 2014 Jan 21].
- Gómez-Gil E, Zubiaurre-Elorza L, Esteva I, Guillamon A, Godás T, Cruz Almaraz M, et al. Hormone-treated transsexuals report less social distress, anxiety, and depression. Psychoneuroendocrinology. 2012 May;37(5):662-70.
- Sevelius JM. Gender Affirmation: A framework for conceptualizing risk behavior among transgender women of color. Sex Roles. 2013 Jun 1;68(11-12):675-89.
Molly O'Brien-Horn, PT, DPT, CLT is a pelvic health physical therapist in California. She is a teaching assistant with Herman & Wallace and will be acting as a TA in the upcoming remote course, Inclusive Care for Gender and Sexual Minorities. Molly is a Certified Lymphedema Therapist (CLT), an LSVT BIG Parkinson’s Disease certified therapist, a trained childbirth doula, and a trained postpartum doula. She is a member of the American Physical Therapy Association Section of Pelvic Health. She has experience in a variety of physical therapy settings, including pediatric oncology, school-based pediatrics, outpatient orthopedics, and wound care. Her passion, however, is working in the field of pelvic floor physical therapy with children, teens, and adults of all gender identities, all sexualities, and all ability levels. In her spare time, Molly enjoys doing yoga, hiking, and relaxing at the beach.
October is LGBT History Month. This annual occurrence is a month-long observance of lesbian, gay, bisexual, and transgender history, and the history of the gay rights and related civil rights movements. H&W is proud to offer courses for treating the whole patient across the gender and age spectrum. The remote courses featured in this blog are Inclusive Care for Gender and Sexual Minorities with instructor Brianna Durand, and Transgender Patients: Pelvic Health and Orthopedic Considerations with co-instructors Sandra Gallagher and Caitlin Smigelski.

Many LGBTQ+ individuals, drag artists, and cisgender and heterosexual persons engage in binding, tucking, packing, and padding for several reasons. These techniques can be life-changing. Many people use these techniques for gender expression, but they can also be used for gender affirmation.
Gender dysphoria occurs when an individual feels distress due to a mismatch between their assigned gender at birth and their own gender identity. For many folx who are transgender, non-binary, queer, or intersex, these practices help reduce gender dysphoria. Instead, they provide feelings of gender euphoria by creating joy, enhancing mental well-being, and improving quality of life through affirming gender identity. Additionally, these methods can provide safety by helping to protect folx in unsafe and unfamiliar environments. Some of these devices, such as packers, can even be used for sexual function and urination
So how does it all work? Binding is when a person wears a device, called a binder, to flatten or minimize the appearance of their chest. Many folx who identify as transmasculine and non-binary engage in binding. However, not all people who bind identify as transmasculine or non-binary. For example, cis and queer women, and cisgender men with gynecomastia may use binders. Also of note, not all people who bind use the same binding methods. Compression shirts and tops, sports bras, and tape are a few examples of the many different binding methods available.
Conversely, padding can be used to enhance the shape and appearance of one’s body, often at the hips and gluteal regions. Padded bras can also be used to enhance breast size and shape. Many transfeminine, queer, intersex, non-binary, and cisgender women often use some form of padding or shapewear devices to help create a more effeminate silhouette. Drag artists often use some form of padding to modify their appearance for their performances to achieve the optimal look for their drag persona. Transmen and cismen can also use padding. Furthermore, wigs and prosthetics (e.g. silicone breast forms, breastplates, and prosthetic vaginas) can be used by these populations to achieve a desired appearance.
Regarding prosthetics, many transmasculine folx, cisgender men, intersex folx, and queer individuals use prosthetics for packing. When someone packs, they use a phallic-shaped device to enhance the prominence of their genitals, often to create the appearance of a bulge in their pants. Some packers can extend the length of a phallus for sexual play, as well. This can be helpful for transmasculine folx post metoidioplasty, intersex folx who may have anatomical differences in sexual or reproductive anatomy, as well as cisgender men who suffer from erectile dysfunction. Packers are often made of silicone and can also include or not include certain features like pubic hair, moveable foreskin, and testes. However, packers don’t have to be made of silicone and can instead be made from other items, such as a pair of socks. They can have multiple functions and be used for things other than packing, such as standing for urination, sexual pleasure for oneself, and sexual pleasure for partners.
While packing increases the prominence of one’s genitals, tucking, conversely, is used to minimize the prominence of external genitalia by creating a flatter appearance between the legs. This act gets its name from the tucking of one's testicles into the inguinal canals, after which the penis and scrotum are then tucked between the legs back towards the anus. Frequently gaffs, tape, or tucking underwear are used to maintain the genitalia in these positions. Tucking is commonly used by transfeminine, non-binary, and intersex persons. However, tucking is not just limited to these groups, as cismen, drag artists, and other populations can tuck also.
While binding, packing, tucking, and padding have many positives, there can be some inherent drawbacks. For example, tucking can increase the risk of Urinary Tract Infections due to the position of the urethra close to the anus. Binding can alter posture and impact breathing by reducing diaphragmatic and rib mobility. Pads can be uncomfortable and hot, while packing devices, Stand-to-Pee devices, in particular, require regular cleaning to prevent unwanted smells and/or infections. All of these practices carry the risk of skin breakdown or irritation if performed too frequently or with improper technique. However, it is important to remember that even with these and other various drawbacks, these acts can be so lifesaving, gender-affirming, and life-protecting for many folx, that at times, the benefits of performing these practices greatly outweigh the risks.
The ins and outs of binding, packing, tucking, and padding can be quite complex, and there is so much to learn about proper usage and technique.
Want to learn more about these and other things related to LGBTQ+ health? Check out these remote course options:
- Inclusive Care for Gender and Sexual Minorities, Brianna Durand and her TA Molly O'Brien-Horn will dive deeper into these and other topics surrounding LGBTQ+ healthcare to educate pelvic health practitioners on how to provide better, safer, and more skilled care for the LGBTQ+ populations.
- Transgender Patients: Pelvic Health and Orthopedic Considerations, co-instructors Sandra Gallagher and Caitlin Smigelski will expand your skills for working with people of all gender identities. This course includes particular education regarding gender-affirming genital surgeries as well as discussion of other gender-affirming surgeries and medical interventions that people transitioning might choose.
What are you waiting for? Sign up and join us today!
Aparna Rajagopal, co-author of the Breathing and the Diaphragm: Orthopedic Therapists remote course, shares "I have used breathing and evaluation of the diaphragm as a part of pelvic care for several years now...Through my interactions, I have come to realize that although many of the therapists are aware that the diaphragm and breathing are important, they are unsure of how to assess for dysfunctions and address those dysfunctions."
Pelvic floor patients who may benefit from diaphragmatic breathing exercises include those who present with pelvic pain, incontinence, prolapse, and cervical/thoracic/scapular/lumbar pain. The Breathing and the Diaphragm: Orthopedic Therapists remote course will expand the participant's knowledge of the diaphragm and breathing mechanics. This course offers a different perspective on back pain and alignment, along with the ability to assess and connect breathing and the diaphragm to core stability, continence issues, and the autonomic nervous system.
The autonomic nervous system is in charge of those bodily processes that do not require conscious thought. These include digestion, temperature, blood pressure, and breathing. The autonomic nervous system can be hacked or manipulated with deep breathing exercises such as diaphragmatic breathing.
Diaphragmatic breathing involves fully engaging the abdominal muscles and diaphragm when breathing by actively pulling the diaphragm down with each inward breath, allowing the lungs to fill more efficiently. The benefits of diaphragmatic breathing can include lowered heart rate and blood pressure regulation. Patients may also see a decrease in cortisol (a stress hormone), allowing them to relax better (1).
The effects of stress can show as emotional, cognitive, behavioral, or physical symptoms in different people. Pelvic pain can be connected to stress through the pelvic floor stress reflex response. This response is a reaction where the pelvic floor muscles actively contract from a stress trigger, either mental or physical. In such cases, increased muscle contractions can lead to tightness and weakness in the affected muscles. Visualize an agitated, tightened muscle to understand how stress can lead to hypertonic muscles, diarrhea, bladder, and sexual issues
Now let's back up to tie in the stress hormone cortisol. Normal cortisol levels rise and fall in a rhythmic pattern throughout the day, allowing for circadian rhythms. Cortisol also helps immune functions and cell repair. When the body is under stress, cortisol is produced in abnormal levels, leading to compromised immune function, pain, exhaustion, and many other issues. Pelvic conditions connected to abnormal cortisol levels include endometriosis(2), interstitial cystitis (3), vulvovaginal candidiasis, and vulvodynia. If a patient has a high cortisol-related diagnosis, intervention can include diaphragmatic breathing for stress management.
The course Breathing and the Diaphragm: Orthopedic Therapists is curated and taught by Aparna Rajagopal and Leeann Taptich. To learn how to incorporate breathing and the diaphragm into your practice, join the next scheduled remote course on October 23-24, 2021.
- Hopper S, Murray S, Ferrara L, Singleton J. Effectiveness of diaphragmatic breathing for reducing physiological and psychological stress in adults: a quantitative systematic review. JBI Database System Rev Implement Rep. 2019 Sep;17(9):1855-1876. doi:10.11124/JBISRIR-2017-003848.
- Friggi Sebe Petrelluzzi K, Garcia M, Petta C et al. Physical therapy and psychological intervention normalize cortisol levels and improve vitality in women with endometriosis. Journal of Psychosomatic Obstetrics & Gynecology. 2012;33(4):191-198. doi:10.3109/0167482x.2012.729625.
- Schrepf A, O’Donnell M, Luo Y, Bradley C, Kreder K, Lutgendorf S. Inflammation and Symptom Change in Interstitial Cystitis or Bladder Pain Syndrome: A Multidisciplinary Approach to the Study of Chronic Pelvic Pain Research Network Study. Urology. 2016;90:56-61. doi:10.1016/j.urology.2015.12.040.
Holly Tanner Short Interview Series - Episode 3 featuring Lauren Mansell
Lauren Mansell shares, "We're never ready to do this work. We're never ready to be perfect." Her course, Trauma Awareness for the Pelvic Therapist, is for all practitioners, not just physical therapists. Anyone licensed who works with patients can benefit from this topic. However, it can be offputting to put ourselves into a vulnerable position by registering for a course on this topic. Lauren understands this and comes prepared to teach other practitioners about trauma-informed care in the gentlest way possible.
Lauren Mansell, DPT, CLT, PRPC, CYT curated and instructs this course. Lauren worked in counseling and advocacy for sexual assault survivors before becoming a physical therapist. She also brings her experience as a 2017 Fellow of the Chicago Trauma Collective to teach trauma-informed care to medical providers. Trauma-informed care is especially important as the field of pelvic rehabilitation becomes more inclusive.
Pelvic rehabilitation and pelvic therapists really do treat the whole patient. Patients can present with pain, long-term issues, and undisclosed trauma that can be compounded when it includes sex, bladder, or bowel issues. Trauma Awareness for the Pelvic Therapist addresses several topics under this umbrella and spends time on each of the following:
- Explaining and describing compassion fatigue, trauma-informed care as well as anatomy, neurobiology, physiology of trauma, and the polyvagal autonomic nervous system
- Identifying risk factors and Adverse Childhood Experiences (ACEs)
- Formulating techniques for reducing compassion fatigue, secondary trauma, and retraumatization
To learn more about trauma-informed care join H&W this weekend at Trauma Awareness for the Pelvic Therapist this September 25-26, 2021. The course will be offered again in 2022 if you are not available this weekend!
Lubricant use can be a difficult conversation to bring with a patient. There are so many different brands and types of lubricants on the market that it can be overwhelming. Since personal lubricants are available over-the-counter, many users may end up taking home a product that does more harm than good.
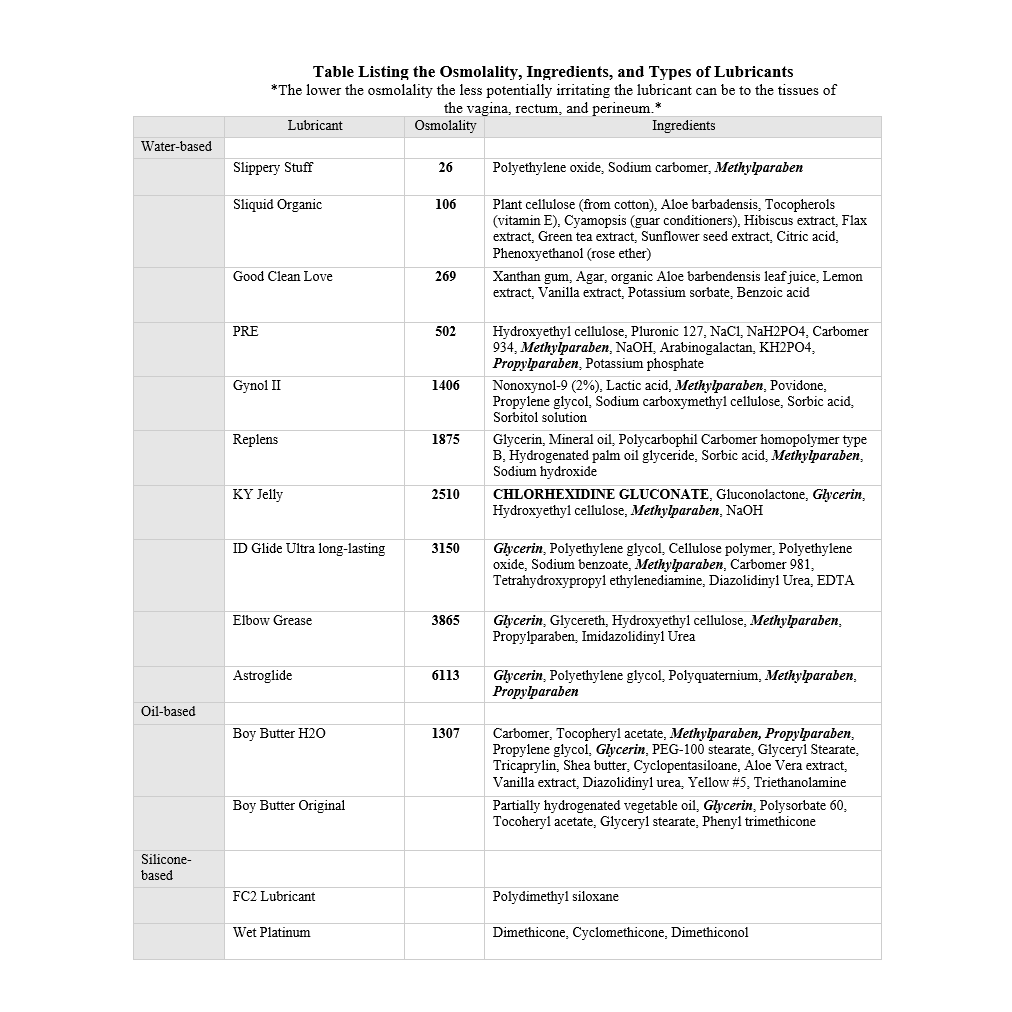
Lubricant varieties include water-based, oil-based, organic or natural, silicone, fertility, and specialty lubricants. Each is made with different ingredients and can be utilized in different situations for personal and medical use. When looking at lubricants, it is important to be mindful of components that can be harmful to pelvic health. These include preservatives, glycerin, petrolatum, warming agents, and osmolality.
Preservatives are commonly added to food and other products to increase shelf life and can affect the microflora of the gastrointestinal, vaginal, and rectal areas (similar to how changes in pH can affect microflora). When this balance becomes disrupted infections can occur.
Bacterial vaginosis, a common type of vaginal infection, is caused when there are less good vaginal bacteria and more bad vaginal bacteria. Some lubricants, KY Jelly specifically, contain Chlorhexidine Gluconate. This ingredient kills Lactobacillus, a good bacterium in the vaginal tract (and GI tract). Another lubricant, Gynol II, had a negative effect on Lactobacillus activity.
Chlorhexidine is another ingredient that can lead to irritation. Lubricants that contain glycerin, petrolatum, or warming additives may contribute to vaginitis. Many physicians recommend that patients who have chronic Candida infections not use lubricants that contain these ingredients.
Osmolality is the concentration of molecules in a product. Hyperosmolar lubricants contain large amounts of glycerin and propylene glycol. This assists in keeping the lubricant wet and does not allow it to evaporate quickly. The more hyperosmolar the lubricant, the more the cells along the vaginal and rectal walls shrivel up and come off, weakening the body’s defenses in that area. Astroglide, Gynol II, and KY Jelly (water-based) are not good at protecting the cells in the vaginal and rectal areas. Good Clean Love (water-based) and PRE (silicone-based) are good at keeping the epithelium intact.
It is important to do your research to select the best lubricant for the individual and intended purpose. Keep in mind that some people may be allergic to certain ingredients (such as parabens) when discussing options. While lubricants that contain artificial flavors, colors, sugars, essential oils, additional additives, or glycerine can generate reactions in different people. H&W does not endorse any lubricant brands over another, although the following brands advertise with us: Good Clean Love and Desert Harvest.
- This is not an exhaustive list of lubricants.
Dezzutti CS, Brown ER, Moncla B, Russo J, Cost M, et al. (2012) Is Wetter Better? An Evaluation of Over-the-Counter Personal Lubricants for Safety and Anti-HIV-1 Activity. 2012; 7(11).
When looking through past blogs from The Pelvic Rehab Report, I ran across this gem submitted by Lauren Mansell explaining Trauma-Informed Approach and her course Trauma Awareness for the Pelvic Therapist. While it is not policy to recycle past articles, this was too good not to share again. Lauren succinctly explains the Trauma-Informed Approach that is instructed in her remote course, Trauma Awareness for the Pelvic Therapist, and it is as pertinent today as it was when first published in 2018.
[as written by Lauren Mansell]…
In my experience, trauma creates the trauma, and the body responds in characteristically uncharacteristic ways.
People in distress/trauma-affected do not respond rationally or characteristically, so I have learned to respond to distress/trauma in a rational, ethical, legal, and caring manner. Always. Every time. To the best of my ability, and without shame or blame.
Let’s talk briefly about Trauma-Informed Approach. This is a (person), program, institution, or system that:
- Realizes the widespread impact of trauma and understands potential paths for recovery
- Recognizes the signs and symptoms of trauma in clients, families, staff, and others affected
- Responds by fully integrating knowledge about trauma into policies, procedures, and practices
- Seeks to actively resist retraumatization
The tenets of Trauma-Informed Approach are:
- Safety
- Trustworthiness and transparency
- Peer support
- Collaboration and mutuality
- Empowerment, voice, and choice
- Cultural, historical, and gender issues
Trauma specific interventions:
- Survivors need to be respected, informed, supported, connected, and hopeful- in their recovery
- Interrelation between trauma and symptoms of trauma such as substance abuse, eating disorders, depression, anxiety, musculoskeletal presentation, and acute crisis- including suicidal/homicidal ideations (coordination with other service providers)
- Work in a collaborative way with survivors, families, and friends of the survivor, and other service providers in a way that will empower survivors.
Types of trauma are varied, but I usually treat survivors of emotional, verbal, sexual, and medical trauma. I have even treated patients who felt traumatized by other pelvic floor physical therapists (again, no judgment). Since most of my clinical experience includes sexual and medical trauma survivorship, I try to reframe these experiences as potential post-traumatic growth, especially when working with my oncology patients. For my pelvic patients who divulge sexual trauma, I don’t dictate or name anything. I allow the survivor to make the rules and definitions. Survivors of sexual trauma need extra care when treating pelvic floor dysfunction.
First, when treating survivors of sexual trauma: expect ‘characteristically uncharacteristic’ events to occur. These include the psychological/somatic effects of passing out, flashbacks, seizures, tremors, dissociation, and other mechanisms of coping with the trauma. Have a plan ready for these patients.
Triaging the survivor to assess their needs, when trauma has been verbalized/disclosed:
- Are you safe right now?
- Do you need medical treatment right now?
- What do you need to feel in control of (PT session/immediately after disclosure of trauma)?
- You have choices in your treatment and in your response to trauma.
- I believe you.
- Lastly, is this a situation for mandated reporting?
After assisting the survivor in their journey towards healing, it is imperative that you take care of yourself. Make healthy boundaries (with patients and others) and take time to decompress, create healthy ritualistic behaviors, mindfulness/relaxation, and somatic release (like yoga, massage, or working out). These are crucial to successfully treating patients who have experienced trauma and who have shared that trauma experience with you.
Because I use gentle yoga for both my trauma survivors’ treatment and for my own self-care, my course implements evidenced-based trauma-sensitive yoga. Additionally, modifications for manual therapy are explored. The class is designed to be informative and experiential while integrating the Trauma-Informed Approaches of Safety, trustworthiness and transparency, peer support, collaboration and mutuality, empowerment, voice and choice and cultural, historical and gender issues.
Join Lauren Mansell and H&W to learn more in the remote course Trauma Awareness for the Pelvic Therapist, scheduled for September 25-26, 2021.
This week The Pelvic Rehab Report sat down with senior teaching assistant and author, Mora A Pluchino, PT, DPT, PRPC, to discuss her new book “The Poop Train”. Mora works at the Bacharach Institute for Rehabilitation and in 2020, she opened her own "after hours" virtual practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. She has been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016, as well as a TA with Herman and Wallace since 2020 with over 150 hours of lab instruction experience!
What or who inspired you to write this book?
My nine-year-old daughter has had issues with constipation since she was two. Our household is no stranger to talking about poop and all things related to poop to manage her tummy issues. I always tried to explain to her the purpose of habits like eating fiber and drinking water, as well as how poop moves through the body. One day my daughter started telling me that her “poop train wasn’t ready to leave the station” and I got the idea for the story!
Can you tell me about your book and the title?
I wanted a title that would be silly but interesting to a child. My goal was to create a book to be easy to read and understand the story about how food enters and leaves our body with resources within and after the book for parents to help manage their child’s bowels. I wanted it to be something that would be fun to read while on the potty, preparing for potty training or if a child is having an issue.
What does your daughter think of “The Poop Train”?
I just asked her and she took my computer over to answer. “I think that you are crazy and you talk about poop way too much! I also think that your book is super cute and even kind of funny. Kids and adults alike are going to love it because it talks about all the parts it needs to but it is not creepy or embarrassing.” - Nina P.
What’s your favorite thing about your book?
I am honestly in love with the illustrations. I had this idea for a few years and couldn’t do anything with it because I’m not good at drawing. I finally connected with the sister of a dear friend who shares my love poop talks and happens to be a talented artist. She brought my idea to life in adorable, inclusive, and simple images!
How do you think writing this book has impacted you as a PT and parent?
Taking Pelvic Floor Level 1 changed my life as a parent. This career path gave me the tools to help my daughter manage her constipation and resultant pelvic floor issues like post-void dribbling and bed-wetting. I wrote this book to help other parents who had similar struggles.
Were there any surprises along this book journey?
Funny story, I proofread my book multiple times along with my husband and a friend. My daughter read the book for the first time and found a TYPO! At that point, it was too late so my book became practically perfect. Hint - the typo is in the resource section!
What advice do you have for other PTs who are interested in writing?
I’d encourage anyone interested in writing something to go for it. Take your idea and nurture it until you can create it! Talk to others if you get stuck. I did this and found the illustrator of my dreams shortly after. And proofread a million times!
Do you think you’ll write another book?
I am finalizing the manuscript for my second pelvic health book. I was so happy with how Elizabeth Wolfe was able to capture the style I wanted that I asked her to work on a second project a few days after we finished our first. “Practically Perfect Pelvic Health 101: A Visual Tour of the Pelvic Floor” will be going to print soon!
How do I get a copy of this book?
“The Poop Train” is available in paperback on Amazon! I am also happy to send copies to fellow pelvic health professionals at a discount. I can be contacted by email at This email address is being protected from spambots. You need JavaScript enabled to view it.!
Mora Pluchino (She/Her)
Holly Tanner Short Interview Series - Episode 2 featuring Deb Gulbrandson
Holly Tanner and Deb Gulbrandson sat down to discuss the Osteoporosis Management Remote Course and why it is important for practitioners to recognize and know how to safely treat and manage osteoporosis patients in their practices.
Deb Gulbrandson shares the goal of the Osteoporosis Management remote course: "This course is based on the Meeks Method created by Sara Meeks, PT, MS, GCS...we have branched out to add information on sleep hygiene, exercise dosing, and basic nutrition for a person with low bone mass. Knowing how to recognize signs, screen for osteoporosis, and design an effective and safe program can be life-changing for these patients."
Join H&W at the Osteoporosis Management remote course, scheduled for September 18-19, 2021, to learn more about treating patients with osteoporosis.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/









































