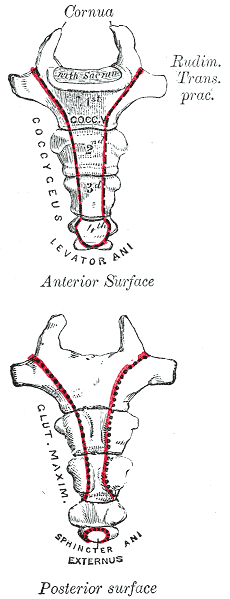
In my mid 20’s I had a sudden onset of severe, persistent pain at the bottom of my spine. I had fallen while running on trails and thought maybe I had fractured my coccyx. It hurt terribly to sit, especially on hard surfaces. When I finally succumbed to seeing a doctor, he diagnosed me with a pilonidal cyst and performed a simple excision of the infection right there in the office. I recall passing out on the table and waking up with an open wound stuffed with gauze. What I thought was “just” coccydynia turned out to be something completely different, requiring a specific and immediately effective treatment.
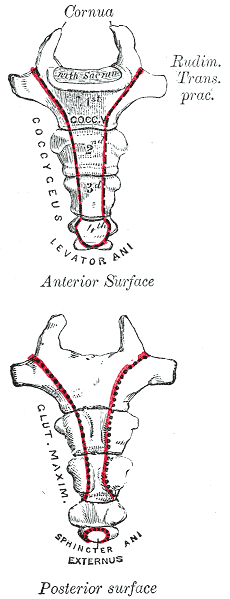 Differential diagnosis is essential in all medical professions. Blocker, Hill, and Woodacre2011 presented a case report on persistent coccydynia and the necessity of differential diagnosis. A 59-year old female reported constant coccyx pain after falling at a wedding. Her initial x-rays were normal, as was an MRI a year later, despite continued pain. Neither an ultrasound nor abdominal CT scan was performed until 16 months after the onset of pain, which was 2 months after she started having bladder symptoms. A CT scan then showed a tumor stemming from her sacrum and coccyx, and an MRI confirmed the sacrum as the tumor location. Chordomas are primary bone tumors generally found at the sacrum and coccyx or the base of the skull. They are relatively rare; however, they do exist in males and females and can present as low back pain, a soft tissue mass, or bladder/bowel obstruction. Clinicians need to listen for red flags of night pain and severe, unrelenting pain and ensure proper examination is performed for accurate diagnosis and expedient treatment.
Differential diagnosis is essential in all medical professions. Blocker, Hill, and Woodacre2011 presented a case report on persistent coccydynia and the necessity of differential diagnosis. A 59-year old female reported constant coccyx pain after falling at a wedding. Her initial x-rays were normal, as was an MRI a year later, despite continued pain. Neither an ultrasound nor abdominal CT scan was performed until 16 months after the onset of pain, which was 2 months after she started having bladder symptoms. A CT scan then showed a tumor stemming from her sacrum and coccyx, and an MRI confirmed the sacrum as the tumor location. Chordomas are primary bone tumors generally found at the sacrum and coccyx or the base of the skull. They are relatively rare; however, they do exist in males and females and can present as low back pain, a soft tissue mass, or bladder/bowel obstruction. Clinicians need to listen for red flags of night pain and severe, unrelenting pain and ensure proper examination is performed for accurate diagnosis and expedient treatment.
In a more recent case study by Gavriilidid & Kyriakou 2013, a 73 year old male presented with 6 months of tailbone pain, worse with sitting and rising from sitting. The physician initially referred him to a surgeon for a pilonidal cyst he diagnosed upon palpation. The surgeon found an unusual mass and performed a biopsy, which turned out to be a sacrococcygeal chordoma. The tumor was excised surgically along with the gluteal musculature, coccyx, and the fifth sacral vertebra, as well as a 2cm border of healthy tissue to minimize risk of recurrence of the chordoma. These authors reported coccygodynia is most often caused by pilonidal disease, clinically confirmed by abscess/sinus, fluid drainage, and midline skin pits. They concluded from this case study if one or more of those characteristic findings are absent, differential diagnoses of chordoma, perineural cyst, giant cell tumour, intra-osseous lipoma, or intradural Schwannoma should be investigated.
Honestly, if I were not a physical therapy tech when my coccyx started killing me 20 years ago, I am not sure I would have gone to the doctor right away. My boss called me out when I winced every time I sat down, and he sent me off to get an exam. The majority of patients are not blurting out specific details about buttock pain when they come for evaluation. Modesty prevails but does not always benefit a patient with persistent coccydynia. Thankfully I did not have a chordoma, but the pain was intense enough to bring me to tears, and it could have required surgery if I had not been diagnosed early enough. Providing a comfortable environment for our patients during their initial encounter can help them feel less vulnerable and discuss the root of their pain. If we can decipher between chordoma and other causes of coccydynia, we may strike a chord that saves a patient from a poor outcome.
The Herman & Wallace course "Coccyx Pain Evaluation & Treatment" is an excellent opportunity to learn new differential diagnosis techniques for coccyx pain patients. The next opportunity to attend this course is March 25-26 in Tampa, Florida.
Blocker, O., Hill, S., & Woodacre, T. (2011). Persistent coccydynia – the importance of a differential diagnosis. BMJ Case Reports, 2011, bcr0620114408. http://doi.org/10.1136/bcr.06.2011.4408
Gavriilidis, P., & Kyriakou, D. (2013). Sacrococcygeal chordoma, a rare cause of coccygodynia. The American Journal of Case Reports, 14, 548–550. http://doi.org/10.12659/AJCR.889688
My job as a pelvic floor therapist is rewarding and challenging in so many ways. I have to say that one of my favorite "job duties" is differential diagnosis. Some days I feel like a detective, hunting down and piecing together important clues that join like the pieces of a puzzle and reveal the mystery of the root of a particular patient's problem. When I can accurately pinpoint the cause of someone's pain, then I can both offer hope and plan a road to healing.
 Recently a lovely young woman came into my office with the diagnosis of dyspareunia. As you may know dyspareunia means painful penetration and is somewhat akin to getting a script that says "lower back pain." As a therapist you still have to use your skills to determine the cause of the pain and develop an appropriate treatment plan.
Recently a lovely young woman came into my office with the diagnosis of dyspareunia. As you may know dyspareunia means painful penetration and is somewhat akin to getting a script that says "lower back pain." As a therapist you still have to use your skills to determine the cause of the pain and develop an appropriate treatment plan.
My patient relayed that she was 6 months post partum with her first child. She was nursing. Her labor and delivery were unremarkable but she tore a bit during the delivery. She had tried to have intercourse with her husband a few times. It was painful and she thought she needed more time to heal but the pain was not changing. She was a 0 on the Marinoff scare. She was convinced that her scar was restricted. "Oh Goodie," I thought. "I love working with scars!" But I said to her, "Well, we will certainly check your scar mobility but we will also look at the nerves and muscles and skin in that area and test each as a potential pain source, while also completing a musculoskeletal assessment of the rest of you."
Her "external" exam was unremarkable except for adductor and abdominal muscle overactivity. Her internal exam actually revealed excellent scar healing and mobility. There was significant erythemia around the vestibule and a cotton swab test was positive for pain in several areas. There was also significant muscle overactivity in the bulbospongiosis, urethrovaginal sphincter and pubococcygeus muscles. Also her vaginal pH was a 7 (it should normally be a 4, this could indicate low vaginal estrogen). I gave her the diagnosis of provoked vestibulodynia with vaginismus. Her scar was not the problem after all.
Initially for homework she removed all vulvar irritants, talked to her doctor about trying a small amount of vaginal estrogen cream, and worked on awareness of her tendency to clench her abdominal, adductor, and pelvic floor muscles followed by focused relaxation and deep breathing. In the clinic I performed biofeedback for down training, manual therapy to the involved muscles, and instructed her in a dilator program for home. This particular patient did beautifully and her symptoms resolved quite quickly. She sent me a very satisfied email from a weekend holiday with her husband and daughter.
Although this case was fairly straightforward, it is a great example of how differential diagnosis is imperative to deciding and implementing an effective treatment plan for our patients. In Herman & Wallace courses you will gain confidence in your evaluation skills and learn evidence based treatment processes that will enable you to be more confident in your care of both straightforward and complex pelvic pain cases. Hope to see you in class!
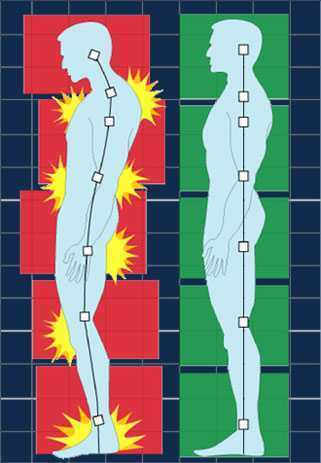
Posture is a concept that rehab clinicians have long hung our hats on, and yet updated models of evaluation and care take into account the truth that there are plenty of humans functioning in poor postures who do not complain of musculoskeletal pain or other dysfunctions. Is postural dysfunction always, or never, causative? As with many things in life, the answer is likely somewhere in between. If our patient arrives at the clinic with a dysfunctional posture and improving their alignment eases discomfort and improves function, we have provided help with addressing posture. It is also likely that we have spent a bit too much time lecturing on the elusive “ideal” posture, when in fact dynamic and adaptive postures are more often occurring throughout a person’s day. Certainly computer postures add to a patient’s movement challenge, and we continue to learn more about the best ways for patients to manage the otherwise potentially static and unhealthy positions that add to many of our patients’ issues.
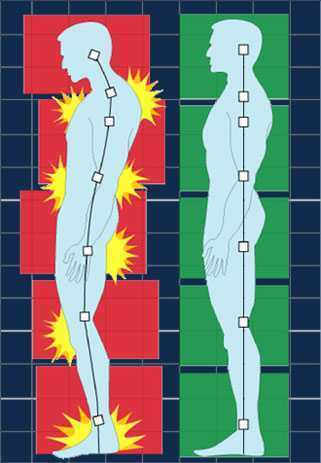 In regards to the pelvic floor, does changing standing lumbopelvic posture affect pelvic floor muscle (PFM) activation? This is the question asked by researchers from Queen’s University in Canada. (Capson et al., 2011) Sixteen women ages 22-41 who had never given birth and who were continent participated in the study. They were assessed completing five tasks in three different postures: normal lumbopelvic posture, hyperlordosis, and hypolordosis. The tasks included quiet standing, maximal effort cough, Valsalva maneuver, pelvic floor maximal voluntary contraction, and a load-catching activity. A vaginal sensor was to use to collect electromyographic activity of the pelvic floor, and sensors were placed on trunk muscles including the rectus abdominus, external and internal obliques, and erector spinae. A perineometer was utilized separately to record manometry measures, and 3D motion analysis was used to position women in the appropriate lumbopelvic angles. Key results of the investigation are summarized below:
In regards to the pelvic floor, does changing standing lumbopelvic posture affect pelvic floor muscle (PFM) activation? This is the question asked by researchers from Queen’s University in Canada. (Capson et al., 2011) Sixteen women ages 22-41 who had never given birth and who were continent participated in the study. They were assessed completing five tasks in three different postures: normal lumbopelvic posture, hyperlordosis, and hypolordosis. The tasks included quiet standing, maximal effort cough, Valsalva maneuver, pelvic floor maximal voluntary contraction, and a load-catching activity. A vaginal sensor was to use to collect electromyographic activity of the pelvic floor, and sensors were placed on trunk muscles including the rectus abdominus, external and internal obliques, and erector spinae. A perineometer was utilized separately to record manometry measures, and 3D motion analysis was used to position women in the appropriate lumbopelvic angles. Key results of the investigation are summarized below:
- Baseline EMG activity of the PFMs and the trunk muscles was significantly lower in supine versus standing
- PFM EMG activity in standing hypolordotic was higher than normal or typical posture
- Trunk muscle EMG activity did not significantly change during the 3 quiet standing postures
- For maximal PFM contraction and for cough, Valsalva, and load-catching, lower EMG activity was measured in standing in hyperlordotic or hypolordotic postures compared to “normal” or habitual posture
- With cough, all muscles except the erector muscles demonstrated increased activity
- In general, EMG activity was increased in trunk muscles when the subjects were in their habitual posture
- Related to timing of the rectus abdominus (RA) muscles, the RA were activated 106 ms before the PFM
- In standing, the intravaginal pressure was significantly higher in the hypolordotic posture compared to hyperlordotic posture
How can we put this valuable research to work in the clinic? This study validates a typical EMG activity finding of increased activity during standing versus lying, which makes sense given the pelvic tasks of working against gravity. In addition, it may be the case that our patients can generate an optimal amount of pelvic muscle contraction (when strengthening) in a more neutral posture. It may also be worth considering that for our patients who are chronically holding, perhaps a tendency for them to be in a hypolordotic posture is perpetuating their dysfunction. The data on timing of trunk and pelvic floor muscles was less consistent, although not less interesting. This research can also be implemented as an evaluation and intervention in the clinic- let’s be sure that we are using methods of feedback such as EMG, real-time ultrasound, or pressure biofeedback in various and functional positions. Then we can find out what seems to work best for our patient, whether the goal is to increase or decrease muscle activity and function.
Capson, A. C., Nashed, J., & Mclean, L. (2011). The role of lumbopelvic posture in pelvic floor muscle activation in continent women. Journal of Electromyography and Kinesiology21(1), 166-177.
Assuring patients with chronic pain they are not crazy by explaining the neurophysiology behind what is happening in their brain and body can be life changing. Increasing our patients’ knowledge about physical conditions can reduce anxiety and provide hope. As a healthcare provider, being confident in your differential diagnosis skills can help narrow down the physical source of pain, weed out the psychological components, and connect the dots to the neurological influence on the patient’s persistent symptoms.
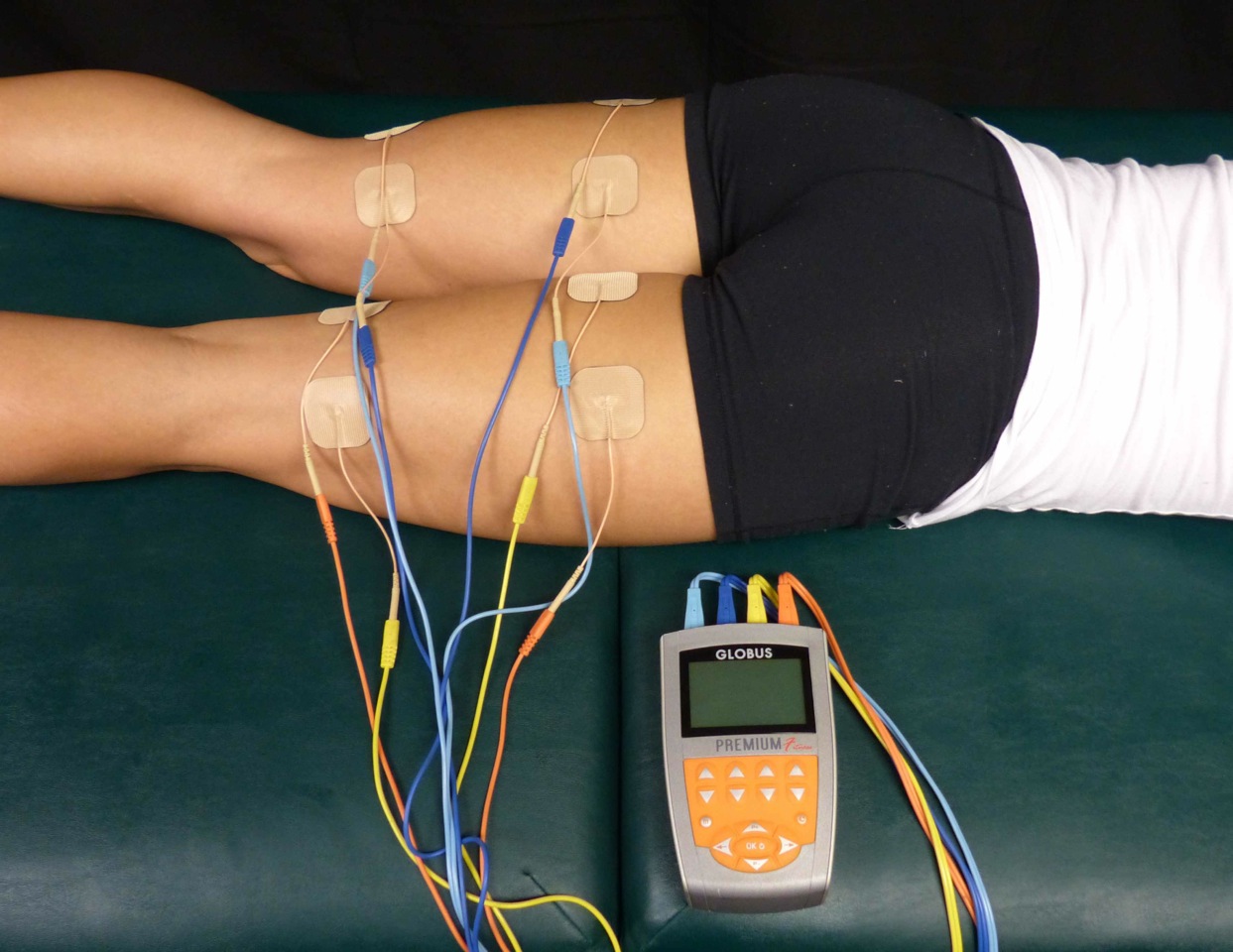 A 2015 article in Pain Medicine (Gurian et al) found a direct association between pain sensitivity and treatment of chronic pelvic pain. The study involved 58 women with at least 6 months of pelvic pain, and they were evaluated on pain threshold using transcutaneous electrical nerve stimulation before treatment and 6 months after a multidisciplinary approach to treatment of the pelvic pain. Pain intensity was also evaluated using the visual analog scale and the McGill questionnaire. Depending on the specific condition, treatment included manual therapy, physical therapy, pain medications, laparoscopy, oral contraceptives, nutrition intervention, or psychological support. After receiving treatment for 6 months, the pain threshold mean improved from 14.2 to 17.4. The effect sizes of 0.86 in the group with pain reduction and 0.53 in the group not achieving pain reduction were both within the 95% confidence interval. The authors concluded in this study that central sensitization does occur in patients with chronic pelvic pain, and treatment can reduce the general pain sensitivity of the patient.
A 2015 article in Pain Medicine (Gurian et al) found a direct association between pain sensitivity and treatment of chronic pelvic pain. The study involved 58 women with at least 6 months of pelvic pain, and they were evaluated on pain threshold using transcutaneous electrical nerve stimulation before treatment and 6 months after a multidisciplinary approach to treatment of the pelvic pain. Pain intensity was also evaluated using the visual analog scale and the McGill questionnaire. Depending on the specific condition, treatment included manual therapy, physical therapy, pain medications, laparoscopy, oral contraceptives, nutrition intervention, or psychological support. After receiving treatment for 6 months, the pain threshold mean improved from 14.2 to 17.4. The effect sizes of 0.86 in the group with pain reduction and 0.53 in the group not achieving pain reduction were both within the 95% confidence interval. The authors concluded in this study that central sensitization does occur in patients with chronic pelvic pain, and treatment can reduce the general pain sensitivity of the patient.
Kutch et al., (2015) performed a study regarding the change in men’s resting state of neuromotor connectivity as affected by chronic prostatitis or chronic pelvic pain syndrome (CP/CPPS), showing men are also subject to central sensitization. Fifty-five men (28 males with pelvic pain for at least 3 months and 27 healthy males) completed the study, with resting state functional magnetic resonance imaging detecting the functional connectivity of the pelvis with the motor cortex (pelvic-motor). The right posterior insula and pelvic-motor functional connectivity was found to be significantly different in men with chronic pelvic pain and prostatitis versus the healthy control group. Contraction of the pelvic floor corresponded with activation of the medial aspect of the motor cortex, while the left motor cortex was more associated with contraction of the right hand. The authors concluded this relationship may explain the viscerosensory and motor processing changes that occur in men with CP/CPPS and could be the most important marker of brain function alteration in this group of patients.
As more research is being done on the neurophysiological level of pain, more truth can support the “it’s all in your head” accusation. However, it is a positive light to shed for a patient. The brain is powerful and controls how pain is perceived globally. Proper treatment of a chronic pelvic floor condition, for women and men, can help reduce stress on the brain and lessen pain sensitivity and perception in our patients. Never let a patient pursue the self-perception that they are crazy. Explain central sensitization and how sometimes the brain wins in the war of “mind over matter”; however, give them hope, explaining how the proper treatment can lessen the intensity of the battle wounds.
Maria Beatriz Ferreira Gurian, Omero Benedicto Poli Neto, Julio Cesar Rosa e Silva, Antonio Alberto Nogueira, Francisco Jose Candido dos Reis. (2015). Reduction of Pain Sensitivity is Associated with the Response to Treatment in Women with Chronic Pelvic Pain. Pain Medicine. 16 (5) 849-854; DOI: 10.1111/pme.12625
Kutch, J. J., Yani, M. S., Asavasopon, S., Kirages, D. J., Rana, M., Cosand, L., … Mayer, E. A. (2015). Altered resting state neuromotor connectivity in men with chronic prostatitis/chronic pelvic pain syndrome: A MAPP: Research Network Neuroimaging Study. NeuroImage : Clinical, 8, 493–502. http://doi.org/10.1016/j.nicl.2015.05.013
Faculty member Lila Bartkowski- Abbate PT, DPT, MS, OCS, WCS, PRPC teaches the Bowel Pathology, Function, Dysfunction and the Pelvic Floor course for Herman & Wallace. Join her in Tampa on April 2-3, or one of the other two events currently open for registration.
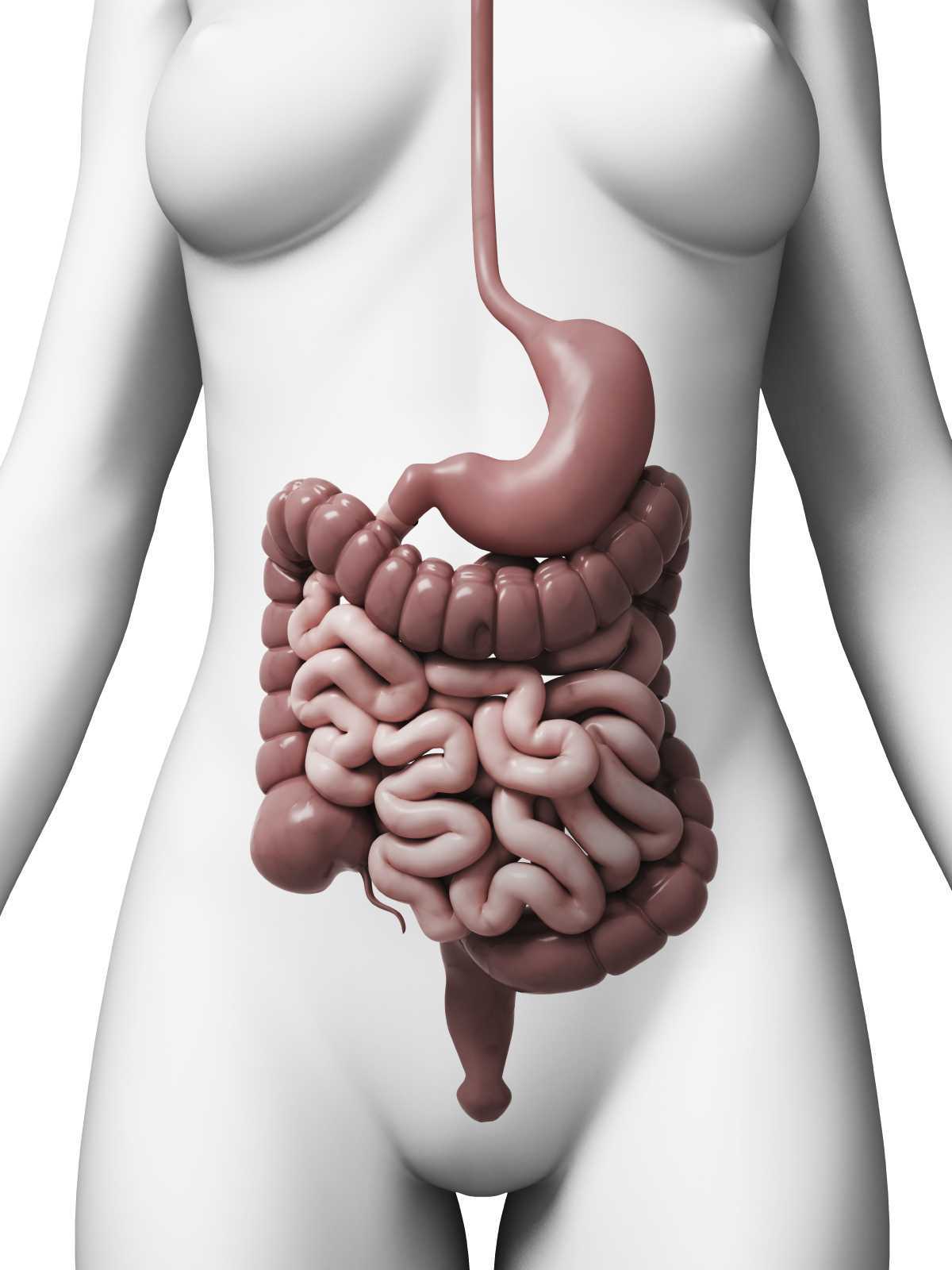
 Constipation, an often under reported health issue, afflicts about 30% of Americans. ¹ The diagnosis of chronic constipation may seem like a simple concept, however the etiology of chronic constipation presents itself in many different forms. Dyssynergic defecation is one of many factors that can lead to a presentation of chronic constipation in a patient. Dyssynergic defecation or “paradoxical contraction” occurs when the muscles of the abdominals, puborectalis sling, and external anal sphincter function inappropriately while attempting a bowel movement. ² The lack of coordination of these muscles results in a contraction versus a lengthening of the pelvic floor muscles with baring down. Dyssynergic defecation is different than a structural issue such as a rectocele or hemorrhoids causing the inability to pass stool effectively or constipation due to slow colon transit time or pathological disease. Making the diagnosis of dyssynergic defecation by symptoms alone is often not reliable secondary to overlap of similar symptoms with chronic constipation due to factors such as a structural issue, irritable bowel syndrome (IBS), or irritable bowel disease (IBD). The diagnosis of dyssynergic defecation can be difficult and is often made through physiologic testing such as balloon expulsion testing or MRI with defecography. ² However, physical therapists can often manually feel that a paradoxical contraction is happening when asking a patient to bare down on evaluation.
Constipation, an often under reported health issue, afflicts about 30% of Americans. ¹ The diagnosis of chronic constipation may seem like a simple concept, however the etiology of chronic constipation presents itself in many different forms. Dyssynergic defecation is one of many factors that can lead to a presentation of chronic constipation in a patient. Dyssynergic defecation or “paradoxical contraction” occurs when the muscles of the abdominals, puborectalis sling, and external anal sphincter function inappropriately while attempting a bowel movement. ² The lack of coordination of these muscles results in a contraction versus a lengthening of the pelvic floor muscles with baring down. Dyssynergic defecation is different than a structural issue such as a rectocele or hemorrhoids causing the inability to pass stool effectively or constipation due to slow colon transit time or pathological disease. Making the diagnosis of dyssynergic defecation by symptoms alone is often not reliable secondary to overlap of similar symptoms with chronic constipation due to factors such as a structural issue, irritable bowel syndrome (IBS), or irritable bowel disease (IBD). The diagnosis of dyssynergic defecation can be difficult and is often made through physiologic testing such as balloon expulsion testing or MRI with defecography. ² However, physical therapists can often manually feel that a paradoxical contraction is happening when asking a patient to bare down on evaluation.
Patients with dyssynergic defecation may present to pelvic floor physical therapy with complaints of: ¹ ²
- Abdominal symptoms such as bloating, pain, and cramping
- Poor response to laxatives and fiber supplementation that does not fully resolve their issue
- Have had testing for anatomical or neurological abnormalities with no significant findings
- Complaints of concomitant pelvic pain due to over activity of the pelvic floor muscles
Physical Therapists specializing in pelvic floor rehab can be a valuable part of the medical team with treating these patients. Biofeedback training by physical therapists has been shown to decrease anorectal related constipation symptoms and abdominal symptoms in patients with dyssynergic defecation. In a sample of 77 patients with dyssynergic defecation, physical therapists provided biofeedback training for 6-8 weeks that included manual and verbal feedback, surface EMG, exercises using a rectal catheter, rectal ballooning to improve rectal sensory abnormalities, ultrasound, pelvic floor and abdominal massage, electrical stimulation if needed, and core strengthening and stretching to improve the patients’ maladaptive habits while attempting to pass a bowel movement. Significant decreases were seen on all three domains (abdominal, rectal, and stool) on the PAC-SYM (Patient Assessment of Constipation) questionnaire post biofeedback training. ² It is noteworthy that 74% of these patients presented to the clinic with complaints of abdominal symptoms such as bloating, pain, discomfort, and cramping.
Knowing how to effectively treat these patients and ask the right questions is valuable in the scheme of pelvic floor rehab secondary to overlapping symptoms of different causes of chronic constipation. Physical therapists are able to provide these patients with conservative treatment that can effectively improve or eliminate their problem, recognize dyssynergic defecation as a possible differential diagnosis, and refer to the appropriate medical professional for further testing. Recognizing and treating dyssynergic defecation is something physical therapists will learn how to become effective at in the upcoming Herman and Wallace Course: Bowel Pathology, Function, Dysfunction & the Pelvic Floor April 2-3 in Tampa, FL and October 8-9 in Fairfield, CA.
1. Sahin M, Dogan I, Cengiz M et al. (2015). The impact of anorectal biofeedback therapy on quality of life of patients with dyssynergic defecation. Turk J Gastroenterol. 26(2):140-144
2. Baker J, Eswaran S, Saad R, et al. (2015). Abdominal symptoms are common and benefit from biofeedback therapy in patients with dyssynergic defecation. Clin Transl Gastroenterol. 30(6)e105. doi: 10.1038/ctg.2015.3
Faculty member, Ginger Garner PT, L/ATC, PYT will be giving 2 lectures at this year’s annual Montreal International Symposium for Therapeutic Yoga, or MISTY for short, in Montreal, Quebec. The first is a 2-hour lecture titled, Vocal Liberation, and the second is a 4-hour lecture titled, Hip Preservation: Yoga Reconsidered, Visit http://www.homyogaevents.com to learn more.
 Yoga is, unarguably, a popular contemplative science, enjoying 36.7 million practitioners in the US alone, up from 20.4 million in 2012.1 A 16 billion dollar industry, yoga is one of the most widely utilized methods of complementary and integrative medicine in America today. In 2008, the editor of Yoga Journal declared “yoga as medicine” as the next great wave. That was right in the middle of the Great Recession, when the last thing on the collective healthcare industry’s mind was yoga.
Yoga is, unarguably, a popular contemplative science, enjoying 36.7 million practitioners in the US alone, up from 20.4 million in 2012.1 A 16 billion dollar industry, yoga is one of the most widely utilized methods of complementary and integrative medicine in America today. In 2008, the editor of Yoga Journal declared “yoga as medicine” as the next great wave. That was right in the middle of the Great Recession, when the last thing on the collective healthcare industry’s mind was yoga.
What happened during the same time frame as the interest in yoga surged?
Our expanded knowledge of hip anatomy, physiology, and pathophysiology exploded onto the medical scene, providing more information than ever about how to address, preserve, and otherwise attend to the hip joint. Prior to this new age of research, the hip was relegated to a joint worthy of no more than a tendonitis, bursitis, or osteoarthritis diagnosis. A person was simply a hip replacement candidate or not. There was no other option once a hip joint had prematurely degenerated. Now, that has all changed, thanks to technological advances in diagnostic testing and investigation.
Yet, the worlds of hip preservation and rehabilitation and yoga have yet to join hands. Many of my patients and colleagues have suffered from unnecessary hip injuries, from labral tears, all types of impingement, and compounding secondary diagnoses such as torn hamstrings, sports hernias, gluteal tendinopathy, to pelvic pain, all due to yoga practice. Some suffered injuries in yoga class during a single traumatic injury, and some injuries were drawn out over years of accumulated microinjury to capsuloligamentous, bony, or cartilaginous structures.
Hip labral injuries (HLI) have vastly increased over the last 10 years, perhaps making HLI the newest orthopaedic diagnosis of the 21st century. This discovery also makes surgical and conservative management of HLI uncharted territory. Conservative therapy includes nonsurgical and post-surgical rehabilitation, and since the average time from injury to diagnosis is 2.5 years, there are many people with hip, pelvic, back, or sacroiliac joint pain that have undiagnosed hip labral tears.
I should make myself quite clear, however. I am not out to demonize yoga or fear-monger the practice of yoga or how it may wreck a person’s body (to use recently controversial language).
My purpose is two-fold: To clarify 1) “what” and “how” yoga can be a safe, effective form or physical therapy and rehabilitation for the hip and pelvis, as well as to 2) underscore the areas where yoga posture practice should be evolved to prevent injury.
To that end, I have written and will be presenting a new 4-hour workshop entitled, Hip Preservation: Yoga Reconsidered, at the Montreal International Symposium on Therapeutic Yoga (MISTY) this weekend in Canada. The lecture is relevant for yoga teachers, yoga enthusiasts, yoga therapists, and health care professionals who are interested in learning how to prevent hip injury in yoga practice.
The workshop will introduce identification of imbalances that could contribute to HLI, as well as understand the common mistakes made in yoga practice that could increase HLI or hip impingement. Understanding the pain patterns that surround HLI are also critical to safe and therapeutic yoga practice and will be discussed. Discussion of structure, function, ability and “dis”ability of the hip, including their major substrates, will help identify the “red flags” in yoga practice, identifying high risk populations and those who need postural modification(s) and/or outside referral to physical therapy.
I am looking forward to instructing a high energy, action-packed hands-on learning session at MISTY on March 19-20, along with my presenting a 2-hour lecture on maximizing public speaking impact through Vocal Liberation: The Voice as Therapy.
- The Voice as a Linking Science for Clinical and Business Efficacy
- Hip Preservation: Yoga Reconsidered
- Ginger’s lecture overview - Montreal International Symposium for Therapeutic Yoga
Want to learn more?
Bring Ginger’s 16 hour continuing education course, Differential Diagnosis for Hip Labral Injuries to your facility in 2017 through Herman & Wallace Pelvic Rehabilitation Institute.
Yoga in America 2016 Survey. Yoga Alliance and Yoga Journal. January 2016.
Rarely does a patient with sacroiliac joint dysfunction come to see us with a goal of having surgery. Sometimes surgery winds up being the last resort for relief if our efforts and the patient’s commitment to physical therapy and prescribed exercises fail. Some of the most recent research shows positive results from minimally invasive surgery; however, the bottom line is to make sure the most educated, clinically accurate diagnosis has been made in implicating the SI joint as the source of pain.
Capobianco et al (2015) performed a prospective multi-center trial regarding SI joint fusion using a minimally invasive technique in women with post-partum pain in the pelvic girdle. Eligibility for the study required subjects to have 3 out of 5 positive SI joint stress tests and at least 50% relief with image-guided intra-articular SI joint block with a local anesthetic. Of the 172 subjects in the study, 20 of the 100 females had post-partum pelvic girdle pain, and 52 subjects were male. Significant improvements in pain, quality of life, and function were found for not only the post-partum group but all groups 12 months after surgery. Worth noting is one to three weeks after surgery, the subjects engaged in physical therapy, two times per week for six weeks.
Whang et al (2015) assessed the 6-month outcomes of SI joint fusion using triangular titanium implants versus non-surgical management in a prospective randomized controlled trial. Of the 148 subjects chosen based on similar diagnostic criteria as the study mentioned above, 102 underwent surgery, and 46 had non-surgical management. Non-surgical management involved appropriate pain medication administration, physical therapy, intra-articular SI joint steroid injections, and radiofrequency ablation of sacral nerve roots, all based on individual needs. The surgical group subjects in this study were also asked to have physical therapy two times per week for six weeks anywhere from one to three weeks post-op. The results in a six month follow up showed “clinical success” of >80% in the surgical group and <25% in the non-surgical management group.
The Journal of Neurosurgery: Spine presented an article in July 2015 by Zaidi et al with results of a systematic review of literature regarding the surgical and clinical effectiveness of SI joint fusion. The studies included open as well as minimally invasive surgery, and the causes of surgery included SI joint degeneration and arthritis, SIJ dysfunction, postpartum instability, posttraumatic, idiopathic, pathological fractures, and HLA-B27+/rheumatoid arthritis. A mean rate of satisfaction with open surgery was 54%; whereas, the mean was 84% with minimally invasive surgery. Ultimately, the authors concluded, “serious consideration of the cause of pain” is necessary before embarking on SI joint fusion as the evidence for the surgery’s efficacy is lacking.
So, who is responsible for making the definite diagnosis for SI joint dysfunction? As many patients get minimal time in doctor offices, we have a professional responsibility to competently perform a thorough evaluation for our patients. When the diagnosis is “SI joint dysfunction,” rule out the lumbar spine and hip; and, of course, when “low back pain” or “hip pain” fills the diagnosis line, rule out/in the SI joint. If you are confused about how, it is time to consider taking the Sacroiliac Joint Evaluation and Treatment course!
References:
Capobianco, R., Cher, D., & for the SIFI Study Group. (2015). Safety and effectiveness of minimally invasive sacroiliac joint fusion in women with persistent post-partum posterior pelvic girdle pain: 12-month outcomes from a prospective, multi-center trial. SpringerPlus, 4, 570. http://doi.org/10.1186/s40064-015-1359-y
Zaidi, Hasan A., Montoure, Andrew J., and Dickman, Curits A. (2015). Surgical and clinical efficacy of sacroiliac joint fusion: a systematic review of the literature. Journal of Neurosurgery: Spine. (23)1:59-66. DOI: 10.3171/2014.10.SPINE14516
Whang, P., Cher, D., Polly, D., Frank, C., Lockstadt, H., Glaser, J., … Sembrano, J. (2015). Sacroiliac Joint Fusion Using Triangular Titanium Implants vs. Non-Surgical Management: Six-Month Outcomes from a Prospective Randomized Controlled Trial. International Journal of Spine Surgery, 9, 6. http://doi.org/10.14444/2006
A few years ago, I was convinced my left hip pain was due to osteoarthritis. When my hip locked up after a 14 mile run, my manual therapist husband differentially diagnosed the pain as discogenic. Partly in denial and partly wanting to know the extent of the “damage,” I got an x-ray of my left hip, which was completely normal, and a lumbar MRI, which wasn't pretty. The source of my hip pain was a disc bulge at L3-4 and L4-5 with a Schmorl's node at L5-S1 to boot. Instead of riding the train of thought that we treat what hurts, therapists need to disembark and look further for the source, as suggested in the course, “Finding the Driver in Pelvic Pain.”
 A case report published in the International Journal of Sports Physical Therapy by Livingston, Deprey, and Hensley (2015) documents the discovery of a deeper problem than the referring diagnosis of greater trochanteric pain syndrome. A 29 year old female had to stop running because of lateral hip pain that began 3 months after increasing the intensity and frequency of her running and low impact plyometrics. She had pain in sitting and while running. During the evaluation, she demonstrated a positive Trendelenburg, weak and painless hip abductors, and a positive single leg hop test on concrete. When the pain was not elicited with single leg hop on a foam surface, the patient was referred back to the physician for magnetic resonance imaging. The patient was later diagnosed with an acetabular stress fracture. The therapist’s thorough examination helped prevent possible avascular necrosis or a more traumatic fracture of the pelvis.
A case report published in the International Journal of Sports Physical Therapy by Livingston, Deprey, and Hensley (2015) documents the discovery of a deeper problem than the referring diagnosis of greater trochanteric pain syndrome. A 29 year old female had to stop running because of lateral hip pain that began 3 months after increasing the intensity and frequency of her running and low impact plyometrics. She had pain in sitting and while running. During the evaluation, she demonstrated a positive Trendelenburg, weak and painless hip abductors, and a positive single leg hop test on concrete. When the pain was not elicited with single leg hop on a foam surface, the patient was referred back to the physician for magnetic resonance imaging. The patient was later diagnosed with an acetabular stress fracture. The therapist’s thorough examination helped prevent possible avascular necrosis or a more traumatic fracture of the pelvis.
In a 2013 issue of the same journal, Podschum et al. presents a case report on deciphering the diagnosis in a female runner with deep gluteal pain with pelvic involvement. A 45 year old female marathon runner reported pulling her hamstring and complained of left ischial tuberosity pain with aching into the gluteal and pubic ramus regions that eventually forced her to stop running. She had pain in sitting and could not tolerate speed work. She had a history of low back and pelvic floor pain, with an MRI showing osteitis pubis, a lateral L3-4 bulge, and facet hypertrophy at L4-5. The physical therapist ruled out lumbar disc lesion, radiculopathy, sacroiliac joint dysfunction, and hip labral tear with special tests. Initial treatment focused on the differential diagnoses of hamstring syndrome and ischiogluteal bursitis based on subjective complaints and objective findings. After 4 visits, her deep ache shifted to the inferior pubic ramus in sitting as the ischial tuberosity pain diminished. A trained therapist then conducted a thorough pelvic floor exam. Pelvic floor hypertonic dysfunction was diagnosed and took over the “driver’s seat” as the focus for the rest of the treatment of this patient. Symptoms resolved and the patient returned to running marathons without any of her initial presenting symptoms.
If we let specific pain complaints guide our treatment, we will run out of steam with the lack of progress. Finding the true source of symptoms is critical in physical therapy. Sometimes so much is going on with our patients we have to sort through the weeds before we can access the actual road to recovery. The lumbar spine, hips, and pelvic floor create an intricate map of U-turns and two-way streets, so we need to deepen our understanding of how to navigate the regions. Only then will be able to confidently diagnose the “driver” and let the other areas call “shotgun.”
References:
Livingston, J. I., Deprey, S. M., & Hensley, C. P. (2015). DIFFERENTIAL DIAGNOSTIC PROCESS AND CLINICAL DECISION MAKING IN A YOUNG ADULT FEMALE WITH LATERAL HIP PAIN: A CASE REPORT. International Journal of Sports Physical Therapy, 10(5), 712–722.
Podschun, L., Hanney, W. J., Kolber, M. J., Garcia, A., & Rothschild, C. E. (2013). DIFFERENTIAL DIAGNOSIS OF DEEP GLUTEAL PAIN IN A FEMALE RUNNER WITH PELVIC INVOLVEMENT: A CASE REPORT. International Journal of Sports Physical Therapy, 8(4), 462–471.
There's a lot going on in the world of pelvic rehab, and continuing education is no exception! This March, Herman & Wallace is hosting NINE courses around the country. It's a lot to keep up with, so we thought you might appreciate a brief overview of what's coming up next!
Where's this pain coming from?
Pelvic pain can have many sources, and Elizabeth Hampton wants to help you quickly get to the source. Finding the Driver in Pelvic Pain empowers you to play detective in order to help even the most complex patients. Don't miss out on Finding the Driver in Pelvic Pain in San Diego, CA on March 4-6, 2016
What goes in eventually comes out
How important is a good diet? For most of us eating healthy is important, and for many pelvic rehab patients it is a necessity. That's why Megan Pribyl wrote her "Nutrition Perspectives for the Pelvic Rehab Therapist" course. This beginner level course is intended to expand the your knowledge of the metabolic underpinnings for local to systemically complex disorders. Don't miss out on Nutrition Perspectives for the Pelvic Rehab Therapist - Kansas City, MO - March 5-6, 2016!
There's fascia everywhere!
Fascial mobilization is a rising star in pelvic rehab treatment techniques, and Ramona Horton is excited to share it with you! "Mobilization of the Myofascial Layer: Pelvis and Lower Extremity" is the best opportunity you'll get to learn about the evaluation and treatment of myofascia for pelvic dysfunction. Check it out on our continuing education course page. Ramona will be teaching these techniques in Santa Barbara, CA on March 11-13.
Giving birth hurts
Sometimes the newborn is the one to get all the attention, but what about the new mother? Be sure that you can help postpartum women with symptoms like postural dysfunction, pelvic girdle dysfunction, diastasis recti abdominis and more by attending Care of the Postpartum Patient in Seattle, WA this March 12-13, taught by the wonderful Holly Tanner!
Vulvar pain is easy to have and hard to lose
12% of women in the US have vulvar pain for 3 or more months at some stage in their life. It takes a multidisciplinary approach to address all the causes and co-morbidities, and that is exactly what you'll get at Dee Hartmann's Vulvodynia: Assessment and Treatment in Houston, TX on March 12-13, 2016. Dee aims to address the vicious cycle of pain, visceral and sexual dysfunction, and the general hit to quality of life that patients with vulvodynia suffer from.
The challenge of SI joint pain
The sacroiliac joint, pelvic girdle, and pelvic ring sure can take a beating, and Peter Philip knows how to keep you moving. Through exercise and stabilization, the pelvic rehab practitioner can quickly treat pain in the lumbopelvic-hip complex. Learn all about the direct and indirect anatomy that influences the sacroiliac joint, and then get ready to find and treat the source of pain and dysfunction in Sacroiliac Joint Treatment in Minneapolis, MN on March 19-20, 2016.
Taxes and Menopause
The menopause transition is not something many people look forward to. For some women it goes more smoothly than others, and it's the less fortunate ones who need access to a well-trained pelvic care professional. Michelle Lyons is flying in from Ireland to help you to become that pro! Be it vaginal atrophy, sexual health dysfunction, pelvic organ prolapse, or any other of the myriad possible symptoms of menopause, you'll be equipped to handle them all after attending Menopause: A Rehabilitation Approach in Atlanta, GA on March 19-20, 2016.
You went through Herman and Wallace’s Pelvic Floor 1 course and were ready to treat your clients with incontinence and prolapse……….then you started getting referrals for clients with pelvic pain.
You have 45-60 minutes (or longer if you are lucky) to create a safe and comfortable environment, skillfully establish trust and rapport and gather objective and subjective data to get to the bottom of their pain. You want to give them the summary of your findings, their rehab road map and something to work on at home. By the end of the visit, you need to have completed their problem list and plan of care. Where do you start?
 No pressure, right?
No pressure, right?
Clinicians are under a huge amount of pressure to get clients better and faster, which can result in rushing treatment before differential diagnosis is complete. A thorough approach enables us to say, with confidence, what the drivers of their condition are or at the very least what they are not. It is safe to say that no one single issue drives pelvic pain: it is a condition that is unique to each individual and requires a right AND left brain toolbox to unravel the ball of yarn that is pelvic pain.
A client with severe groin and labial pain was referred to my office for a second PT course of care. Her previous course of PT (by an outstanding clinician) focused on intrapelvic visceral work and postural corrections. The client’s pain had remained unchanged. Her visceral mobility, posture, joint biomechanics, neural upregulation, core muscle inhibition, myofascial trigger points, dysfunctional voiding and deconditioning were most definitely significant factors. The initial evaluation aligned with severe OA with a labral tear being the primary driver of her pain. I am no guru: it was with evidence-based sensitive and specific testing I was confident that this woman needed a new hip and that no amount of physical therapy could improve her pain as quickly or efficiently as a hip replacement. She DID need a customized PT pre-op course of care to prepare her for a great outcome. When she got a new hip, we incorporated all key factors into her post op rehab and she is back to her goals of hiking and having sex with her husband. (But not at the same time, as far as I know.)
Before you jump to conclusions, I am not a surgery happy PT. I work with orthopedic surgeons and interventional pain docs as frequently as I work with Reiki healers, craniosacral therapists and acupuncturists. I want to fill my toolbox with right as well as left brained tools, from the most subtle of manual interventions and precise movement re-education to dynamic mobilization and strengthening interventions. As a profession we are called to utilize evidence-based treatment as well as innovative interventions that may be researched one day. Every evidence-based practice was once an unresearched clinical intervention based on clinical reasoning and perhaps gut instinct.
As pelvic health therapists, our work requires high EQ as well as IQ to earn client trust as well as differential diagnosis abilities to design their plan of care. Before we can ask for more visits, we need to justify the reasons behind the request based on solid clinical reasoning including objective data. Certainly in 45 minutes it can be difficult if not impossible to perform a comprehensive pelvic health and musculoskeletal evaluation. That being said, we need to address main categories of foundational evaluation testing to capture their data in a thorough manner.
“Finding the Driver in Pelvic Pain” is a course that enables the clinician to perform a foundational comprehensive musculoskeletal and pelvic health exam to find the evidence based factors in the client’s pain. We are called to deliver care that integrates both the art and science of physical therapy and healing. If we just use the ‘art’, or only the ‘science’, we miss key elements in our differential diagnosis which could delay the client getting better.