How does a male sports and orthopedic physical therapist come to teach about pelvic health and wellness? I was fortunate enough to spend ten years in the NHL as the physical therapist and athletic trainer for the Florida Panthers. Ice hockey is one of the sports that has the highest incidence of groin strains among other pelvic related pathologies.1 As a clinician that was responsible for taking care of the world’s best hockey players, I was challenged to understand the interconnected relationships between the lumbopelvic-hip complex very quickly.
 In the early years of my career development and the treatment of mostly males with pelvic pathologies, I leaned heavily on pelvic health professionals to help me understand an area of the body I received little training on in school and even less in my clinical care as a sports and orthopedic manual physical therapist. After years of treating hip and pelvic pathologies on my players I became more comfortable in this enigmatic area of the body. A good friend of mine was on faculty with Herman & Wallace and we frequently would communicate and compare notes. She was treating an increasing number of “sports hernias” (now termed athletic pubalgia or core muscle injury) and was relying on me to help her understand this injury and how to treat it. In turn, she helped me understand what went on in the pelvic health profession and what those therapists were trained to treat and how they went about it.
In the early years of my career development and the treatment of mostly males with pelvic pathologies, I leaned heavily on pelvic health professionals to help me understand an area of the body I received little training on in school and even less in my clinical care as a sports and orthopedic manual physical therapist. After years of treating hip and pelvic pathologies on my players I became more comfortable in this enigmatic area of the body. A good friend of mine was on faculty with Herman & Wallace and we frequently would communicate and compare notes. She was treating an increasing number of “sports hernias” (now termed athletic pubalgia or core muscle injury) and was relying on me to help her understand this injury and how to treat it. In turn, she helped me understand what went on in the pelvic health profession and what those therapists were trained to treat and how they went about it.
This collaboration eventually led to me joining Herman & Wallace and offering a sports and orthopedic perspective to pelvic floor consideration. I have attended Herman & Wallace’s Pelvic Floor courses to fully understand the training that a pelvic health therapist undergoes. Admittedly, I do not perform internal work because I have found a niche helping clinicians such as myself who understand that the pelvic floor is a key variable in human movement and we need to understand it at a much higher level than what we are exposed to in school, but don’t have the career trajectory of becoming an internal practitioner of the pelvic floor.
I have designed the Athletes and Pelvic Rehabilitation course to reach both the sports and orthopedic clinician as well as the pelvic health practitioner who might be a veteran of pelvic floor education and treatment. Both groups will leave this course with additional tools for their clinical tool box in the realms of manual therapy and exercise.2 Here are some of the objectives for the course:
- Provide clinicians that do not perform internal work a better and more complete understanding of how the pelvic floor integrates into human movement, particularly higher-level activities such as running, lifting and all types of sporting movements.
- Provide both the experienced and pelvic floor early learner with a comprehensive paradigm of exercise theory, development and progressions as well as how to provide non-internal manual therapy to influence the performance of the pelvic floor.
- Provide strategies for clinicians to determine when your patient would be better served with a referral to a pelvic health practitioner and what the current evidence is to support your decision.
- Create innovative and engaging therapeutic exercise programs (home exercise programs too!) for your patients directed at the pelvis with specific attention to upright and functional positioning.
What do people who have attended courses with Dr. Dischiavi have to say? Janna wrote the following email to Herman & Wallace about Steve's Course:
"Good morning. I wanted to make sure that you knew what a fantastic clinician you have to join your team in Steve Dischiavi. I am a practicing OB and orthopedic therapist and felt this course was fantastic! Usually the main goal is to come away with a couple of clinical "pearls." I felt as though I came away with a full days worth of "pearls." I really liked that the course was not totally pelvic floor based, however was totally relevant to the women's health population, but it will also apply to the majority of my current patient population as well. Thank you for the opportunity to learn from Steve!"
1. Orchard JW. Men at higher risk of groin injuries in elite team sports: a systematic review. Br J Sports Med. 2015;49(12):798-802.
2. Tuttle L. The Role of the Obturator Internus Muscle in Pelvic Floor Function. Journal of Women’s Health Physical Therapy. 2016;40(1):15-19.
In the spring of 2019, myself and two lab assistants will have the privilege of teaching PF1 to Kenyan physical therapists through the Kenya Medical Training College (KMTC) in Nairobi, Kenya. The program at KMTC started six years ago by Washington DC-based physical therapist Richard Jackson, and The Jackson Clinics Foundation (Teachandtreat.org), with a focus on orthopedic manual therapy. A neuro rehab program ensued two years later, and the aim for this women’s health program is to build a three level course series similar to the way it is taught in the United States. The goal of all of these programs is to transition them to Kenyan faculty within six years, which has recently occurred in the orthopedic component. Herman & Wallace Pelvic Rehab Institute has graciously agreed to donate curriculum content to the women’s health course component.
 Teaching assistant Terri Lannigan, PT, DPT, OCS, who has taught the lumbopelvic girdle course in the orthopedic program, and also practices women’s health physical therapy in the US, began laying the groundwork for this program with her students and in the Nairobi community last December. “Not only is there a tremendous need, but there is a lot of excitement from a group of students currently taking courses in the program, that women’s health education is coming to KMTC!”
Teaching assistant Terri Lannigan, PT, DPT, OCS, who has taught the lumbopelvic girdle course in the orthopedic program, and also practices women’s health physical therapy in the US, began laying the groundwork for this program with her students and in the Nairobi community last December. “Not only is there a tremendous need, but there is a lot of excitement from a group of students currently taking courses in the program, that women’s health education is coming to KMTC!”
Over the past month, I have been editing the Pelvic Floor 1 course to tailor it to our Kenyan physical therapist audience. The overwhelming majority of Kenyan PT’s do not have access to biofeedback or electric stim, so those sections will be omitted. As there are no documentation or coding requirements in the Kenyan health system, those sections of curriculum will also be edited out. Many of Terri’s PT students complained of significant underemployment, so we will keep the marketing component in our lectures, in hopes to promote expansion of women’s health PT to a larger segment of the Kenyan population.
Meanwhile, teaching assistant Kathy Golic, PT of Overlake Hospital Medical Center’s Pelvic Health Program in Bellevue, WA has headed up the data collection for a lecture on managing fistula and obstetric trauma. Kathy has accumulated data from many sources and conferred with several PTs currently involved in both clinical education as well as direct patient care in multiple African nations, to help us to create relevant, meaningful and culturally appropriate curriculum for this section of the PF1 course.
Pelvic Floor Level 1 will be offered between March 25 – April 6, 2019 at Kenya Medical Training College. We will post photos and additional information of our class and our experiences. We are grateful to Herman and Wallace and The Jackson Clinics Foundation for allowing us to be involved in this exciting endeavor.
Faculty member Nari Clemons, PT, PRPC recently created a two-course series on the manual assessment and treatment of nerves. The two courses, Lumbar Nerve Manual Assessment and Treatment and Sacral Nerve Manual Assessment and Treatment, are a comprehensive look at the nervous system and the various nerve dysfunctions that can impact pelvic health. The Pelvic Rehab Report caught up with Nari to discuss these new courses and how they will benefit pelvic rehab practitioners.

What is "new" in our understanding of nerves? Are there any recent exciting studies that will be incorporated into this course?
The course is loaded with a potpourri of research regarding nerves and histological and morphological studies. There are some fascinating correlations we see with nerve restrictions, wherever they are in the body. Frequently the nerves are compressed in fascial tunnels or areas of muscular overlap, then the nerve, wherever the location, frequently has local vascular axonal change, which increases the diameter of the nerve and prohibits gliding without pain. This causes local guarding and protective mechanisms. Changing pressure on the nerve can change that axonal swelling and allow gliding without pain.
New pain theory also supports that much of pain perception is the body perceiving danger or injury to a nerve. By clearing up the path of the nerve and mobilizing it, we can decrease the body's perception of nerve entrapment and thus create change in pain levels.
What do you hope practitioners will get out of this series that they can't find anywhere else?
I hope they will leave the course able to treat the nerves of the region, which is essentially the transmission pathway for most pelvic pain. I don't know of other courses that have this emphasis.
You've recently split your nerve course in two. Why the split?
I didn't want this class to be a bunch of nerve theory without the manual intervention to make change. After running the labs in local study groups, we found it took more time for people's hands to learn the language, art, and techniques of nerve work. To truly do the work justice and for participants to have a firm grasp of the manual techniques without being rushed, we found it takes time, and I wanted to honor that, as well as treating enough of the related factors and anatomy to make real and lasting change for patients.
How did you decide to divide up content?
Basically, we divided them up by anatomical origin:
The lumbar course covers the nerves of the lumbar plexus, the abdominal wall when treating diastasis, and treatment of the inguinal canal (obturator nerve, femoral nerve, iliohypogastric, ilioinguinal, genitofemoral nerves). Also, the lumbar nerves have more effect in the anterior hip, anterior pelvis, and abdominal wall.
The sacral nerve course covers all the nerves of the sacral plexus (pudendal, sciatic, gluteal/cluneal, posterior femoral cutaneous, sciatic, and coccygeal nerves), as well as subtle issues in the sacral base and subtle coccyx derangement work as well as the relationship with the uterus and sacrum, to take pressure off the sacral plexus. The sacral nerves have more effect in the posterior and inferior pelvis and into the posterior leg and gluteals.
What are the main stories that either course tells?
Both courses tell the story of getting closer to the root of the pain to make more change in less time. Muscles generally just respond to the message the nerve is sending. Yet, by treating the nerve compression directly, we are getting much closer to the root of the issue and have more lasting results by changing the source of abnormal muscle tone. Rather than an intellectual exercise of discourse on nerves, we devote ourselves to the art of manual therapy to change the restrictions on the pathway of the nerve and in the nerve itself.
If someone went to the old nerve course, what's the next best step for them?
The first course was initially all the lumbar nerves with a dip into the pudendal nerve. They would want to take the sacral nerve course, as those nerves were not covered in the first round.
Anything else you would like to share about these courses?
Sure. Essentially, we will take each nerve and do the following:
- Thoroughly learn the path of the nerve
- Fascially clear the path of the nerve
- Manually lengthen supportive structures and tunnels that surround the nerve.
- Directly mobilize the nerve
- Glide the nerve
- Learn manual local regional integration techniques for the nerve after treatment
- Receive handouts for and practice home program for strengthening and increasing mobility in the path of the nerve
Join Nari at one of the following events to learn valuable evaluation and treatment techniques for sacral and lumbar nerves
Upcoming sacral nerve courses:
Sacral Nerve Manual Assessment and Treatment - Winfield, IL
Oct 11, 2019 - Oct 13, 2019
Sacral Nerve Manual Assessment and Treatment - Tampa, FL
Dec 6, 2019 - Dec 8, 2019
Upcoming lumbar nerve courses:
Lumbar Nerve Manual Assessment and Treatment - Phoenix, AZ
Jan 11, 2019 - Jan 13, 2019
Lumbar Nerve Manual Assessment and Treatment - San Diego, CA
May 3, 2019 - May 5, 2019
My name is Tina Allen. I teach a course called Manual Therapy Techniques for the Pelvic Rehab Therapist. I developed this course in 2016 out of desire to help clinicians feel comfortable in their palpation and hands on skills.
 My journey as a pelvic rehab therapist started with a patient whispering to me in the middle of a busy sports/ortho clinic gym; “is it normal to leak when you laugh”. I was treating her after her total hip replacement and my first question was “where are you leaking”? I was concerned that her incision was leaking, that she had an infection and it was beyond me to understand why it would happen when she laughed! I was 24 years old and 2 years out of PT school. Little did I know, that one whispered question would lead me to where I am today. I am in my 25th year as a PT and 20th year specializing in pelvic rehabilitation.
My journey as a pelvic rehab therapist started with a patient whispering to me in the middle of a busy sports/ortho clinic gym; “is it normal to leak when you laugh”. I was treating her after her total hip replacement and my first question was “where are you leaking”? I was concerned that her incision was leaking, that she had an infection and it was beyond me to understand why it would happen when she laughed! I was 24 years old and 2 years out of PT school. Little did I know, that one whispered question would lead me to where I am today. I am in my 25th year as a PT and 20th year specializing in pelvic rehabilitation.
When I started out there just were not many classes. I spent time learning from physicians, reading anything I could find and applying ‘general ‘orthopedic principles to the pelvis. I traveled to clinics and learned from other clinicians. I soaked up anything I could and brought it back to my clinical practice. When Holly Herman and Kathe Wallace asked me to teach with them I was humbled, honored and terribly nervous. Holly and Kathe where two of my greatest resources and to be able to teach along side them to help others along was humbling. As I prepared to teach I realized the breadth of what we do as pelvic rehab clinicians has grown exponentially since I started out.
Over the past 10 years of teaching the pelvic series with H&W; I noticed that for some of the participants there was a gap in confidence in palpation skills and in treatment techniques applied to the pelvic floor region. For most, it’s confidence in what they are feeling and where they are. This course came out of wanting to fill that gap. I wanted to allow a space that clinicians could come and spend two days learning, affirming and building confidence in their hands. They could then take those skills and confidence back to their clinics and help more patients.
The thought of writing this course was daunting. First off, written words are not my thing. Don’t get me wrong I love to read but me coming up with what to put on paper, much less a power point slide, frightened me. With much encouragement and support from colleagues and H&W, I got to work. The first thing was to think about what techniques to include. At some point after 20 years in the field, your hands just do the work and you don’t think about how you do something. My colleague and dear friend Katy Rice allowed me to sit down with her, practice a technique and then write down each specific step to do the skill. She would read them over and then attempt to do the technique by following only the written instructions. I also had patients who were instrumental in helping me choose what techniques to include. They would say to me “that is what made all the difference for me; it has to be included in what you teach others. “
I would think about who taught me each technique, whether it was a course, another clinician or a patient. I know that I did not make any of these up myself; while I may have modified a technique to work with my hands I did not originate them. Holly Tanner was so kind to brain storm with me and lead me to references for some of the techniques that we as clinicians use every day and that I was planning to include.
What happened next was months of me sitting at the kitchen table combing through books, articles, course manuals and online videos looking for origins of the techniques I use every day in my clinical practice. I wanted to be sure to give credit to sources. It was tedious but also inspiring to realize that some of these techniques have been around and documented since 1956 (Dicke, E., & Bischof-Seeberger, I.) and also that the same techniques are sited by multiple different sources. After about 6 months of our kitchen table not being suitable for dinner it was time to see what I had gathered and how it would all fit together. The result was this 2 day course: Manual Therapy Techniques for the Pelvic Rehab Therapist which has seven labs including internal, external and combination techniques, home program/self care ideas and time for brainstorming treatment progressions. Join me in Philadelphia, PA this October 20 - 21 to learn these essential skills.
Nutrition Perspectives for the Pelvic Rehab Therapist
There are moments when I pause and realize how far we’ve come in a short period of time, and then others when I’m acutely reminded how far we have yet to go. Our destination is an integrative health care system which addresses nourishment first and early versus last, not at all, or only when all else fails. My mission is to support the concept of nourishment first and early though sharing of “Nutrition Perspectives for the Pelvic Rehab Therapist” through the Herman & Wallace Pelvic Rehab Institute.
 After each weekend I teach Nutrition Perspectives for the Pelvic Rehab Therapist, I feel affirmed that this class, this information is vital and at times life-changing for practicing clinicians. And every time I teach, participants share that they take away much more than they expected. It’s a course that makes accessible complex concepts to entry level participants while offering timely and cutting edge integrative instruction to the advanced clinician eager to incorporate this knowledge into their practice. Supportive literature is woven throughout the tapestry of the course.
After each weekend I teach Nutrition Perspectives for the Pelvic Rehab Therapist, I feel affirmed that this class, this information is vital and at times life-changing for practicing clinicians. And every time I teach, participants share that they take away much more than they expected. It’s a course that makes accessible complex concepts to entry level participants while offering timely and cutting edge integrative instruction to the advanced clinician eager to incorporate this knowledge into their practice. Supportive literature is woven throughout the tapestry of the course.
After the most recent live course event, a participant shared with me a letter she received from a patient in 2016 who mentions the lack of nutritional attention during her cancer treatment. I want to share with you the essence of this letter:
“In October 2015, I was diagnosed with cancer. The following December I started treatments of radiation and chemotherapy. I really appreciate all the fine employees who helped me through care and treatments. Every clinician I came across, whether a doctor, nurse, phlebotomist, radiation and chemo teams, and my PT, were all exceptional in showing care, concern and knowledge.
However, one area I felt was lacking in was nutrition. I was frequently offered a standard hospital-issue protein drink. When offered, I explained that I would not take it due to it containing high fructose corn syrup (HFCS). I asked if they knew that HFCS was like putting and accelerant on a fire? I received a smile and a nod of head as to say they understood.
I was also offered soda pop to wash down bad tasting medicines/ liquids I was to take. I opted to just down the medication without chasing it as I didn’t want to exacerbate my condition. While taking chemotherapy, I was offered snacks containing HFCS and other non-nutritive so-called foods.
I was also offered limited entree choices, but there were plenty of pies, cakes, jellies, and other non-nutritive foods to choose from. All Items I would not consider for a cancer diet or even a healthy diet. I finally took a picture of the menu selection sheet as I thought no one would believe such a thing could happen.
I received excellent care throughout your system with the exception of nutrition . I would ask that you take a look at making menus with truly healthy options as well as giving patients options that do not contain ingredients that feed the cancer.”
While this letter addresses an inpatient issue at one regional health system, it correspondingly brings into focus the irony present in the vast majority of health care settings across the nation from inpatient to outpatient settings: there is a profound lack of clarity about what it means to be nourished, especially when we are at our most vulnerable.
I cannot claim “Nutrition Perspectives” will solve our nation-wide problem, however, I am certainly encouraging a movement towards a collective understanding of the imperative fact that food is medicine - powerful medicine - and we must as front-line practitioners harness what this understanding can offer. Pelvic rehab practitioners are uniquely positioned to process this information and begin immediately sharing it in clinical practice.
Like many providers, this same participant shared with me that upon receipt of this letter two years ago, she struggled to make progress with what and how to offer nutritional information - mainly because of the overwhelming nature of the subject, and also because of the conflicting and oftentimes confusing information traditionally shared with the public. After attending Nutrition Perspectives, she said “I cannot even begin to describe how much your course has met ALL my hopes for helping clients!….I had struggled to put something together and here it all is - so unbelievably grateful.”
And that’s what this course is all about - empowering you as you broaden your scope of knowledge in a way that teaches you not facts, but deep understanding. Once that foundational understanding is laid, this grass-roots effort will progress like putting an accelerant on the integrative movement. Soon we’ll see the inclusion of nourishment information as first-line practice, and the lives impacted in a positive way will continue to grow.
Please join me at the next opportunity to share in this live experience with other like-minded clinicians. Nutrition Perspectives for the Pelvic Rehab Therapist will be coming to Denver, CO September 15 & 16, 2018!
I’m Elizabeth Hampton PT, DPT, WCS, BCB-PMD and I teach “Finding the Driver in Pelvic Pain”, which offers practitioners a systematic screening approach to rule in or rule out contributing factors to pelvic pain. This course helps clinicians to understand and screen for the common co-morbidities associated with pelvic floor dysfunction, like labral tears, discogenic low back pain, nerve entrapments, coccygeal dysfunction, and more. Importantly, it also coaches clinicians to organize information in a way that enables them to prioritize interventions in complex cases. I've noticed that there are some questions that course participants frequently have as they talk through common themes in their care challenges and wrote this blog to share some clinical pearls you may find to be helpful for your own practice or as an explanation to your clients.
Here are some of the most common questions that I get when teaching Finding the Driver in Pelvic Pain:
1) Question: How do I even start to organize information when a client has a complex history and I am feeling overwhelmed?
I write down a road map with key categories: Bowel and bladder; Spine; Sacroiliac Joint/Pubic Symphysis; Hip; Pelvic floor muscles; biomechanics; respiration; neural upregulation; whatever details can be fit into ‘big buckets’ of information. I use it to both organize my thoughts for my notes, as well as educate the client as to what my findings are and the design of their treatment program.
2) Question: How do you get your clients to do a bowel and bladder diary?
I am proud to say that I can talk anyone into a 7 day bowel and bladder diary because I tell them how incredibly helpful it is to understand the way their body responds to what they eat, drink, and daily habits. It’s my secret weapon to snag clients to start connecting with their body and listening to their details, educate about defecation ergonomics and what happens in multiple systems when there is pelvic floor overactivity. It’s a great teaching tool that facilitates self-reflection and how their self-care choices impact their body’s behavior.
3) Question: How do you educate clients about pelvic floor function so they don’t focus so much on Kegels?
Pelvic floor muscles do three things:
-
They contract gently, or powerfully, with no discomfort, and totally normal breathing; PFMs should have the same kind of nuanced control like your voice does: they should be able to do a gentle contraction, like a “whisper” or a powerful contraction, like a “shout”, depending on the task position and intent.
-
They relax fully and completely when the body is resting in support, or they should be able to relax to a supportive level when they are needed posturally. Relaxation should be its own celebrated event!
-
They should be able to relax and gently lengthen.
Faculty member Elizabeth Hampton PT, DPT, WCS, BCB-PMD is the author and instructor of Finding the Driver in Pelvic Pain, a course designed to help practitioners utilize differential diagnosis in evaluating pain. Join Dr. Hampton in Portland, OR on July 27-29, 2018 or November 2-4, 2018 in Phoenix, AZ.
Erica Vitek, MOT, OTR, BCB-PMD, PRPC is the author and instructor of Neurologic Conditions and Pelvic Floor Rehab, a new course coming to Grand Rapids, MI and Philadelphia, PA. This post is the next in her series on creating a course about neurologic conditions and pelvic rehabilititation.
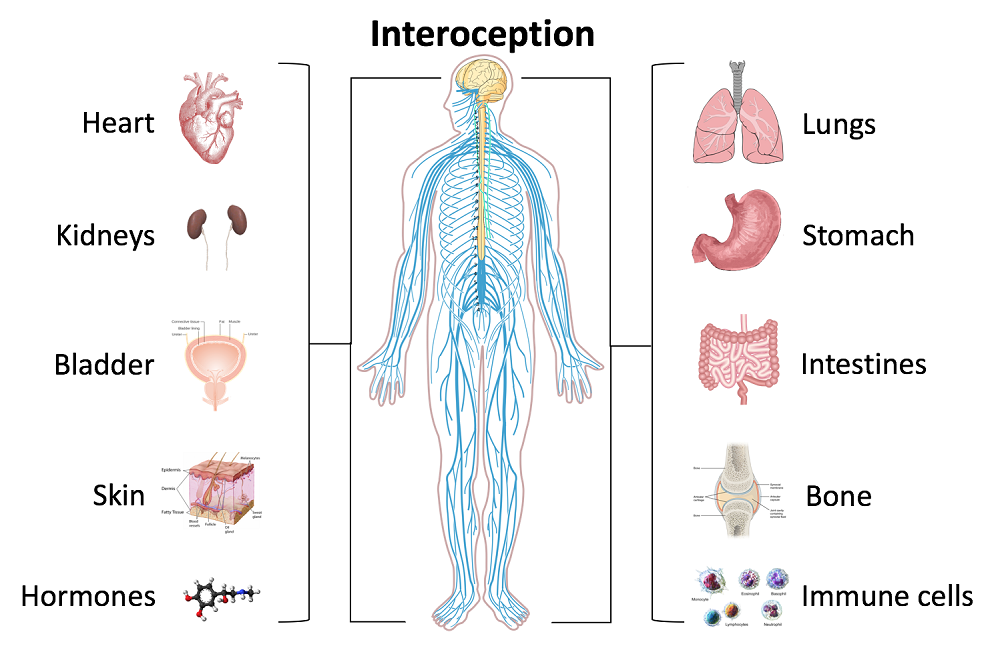
Being a clinician, as we evaluate and treat people with pelvic health conditions, we typically take all systems of the body into account. We take the problem presented to us by the client and we examine, from all angles, how we might go about advice and treatment to best achieve their goals in alleviating the problem. We do a full review of medical history and pharmacology. We examine our client in-depth from a musculoskeletal perspective. We look at psychological contributions to the problem they are facing. We can look at their lifestyle and have them make a detailed diary to help us analyze their bladder, bowel, fluid intake and dietary habits. Do we also always include a look at the neurological components? Do we know what we are looking for? What are the best tools we can have in our toolbox as clinicians to look at our client’s problem through a “neuro brain”?
 In writing each lecture of this course, I have had to step back each time I am developing a new concept and look at it with in-depth thought and contemplation about how I will use this in the clinic to assess my client’s concerns using a neuro-based approach. Taking the concepts and facts about the musculoskeletal system that we know well and then taking a look at the neurological systems contributions and relationship to that dysfunction can be challenging. The main reason for this challenge is that neuro system dysfunction is many times hard explain, presents with inconsistent or changing symptoms, may have motor or sensory deficits together or by themselves, may radiate to different locations than where the true dysfunction is located, and may have developed into central sensitization causing a hypervigilance to typically non-painful stimuli.
In writing each lecture of this course, I have had to step back each time I am developing a new concept and look at it with in-depth thought and contemplation about how I will use this in the clinic to assess my client’s concerns using a neuro-based approach. Taking the concepts and facts about the musculoskeletal system that we know well and then taking a look at the neurological systems contributions and relationship to that dysfunction can be challenging. The main reason for this challenge is that neuro system dysfunction is many times hard explain, presents with inconsistent or changing symptoms, may have motor or sensory deficits together or by themselves, may radiate to different locations than where the true dysfunction is located, and may have developed into central sensitization causing a hypervigilance to typically non-painful stimuli.
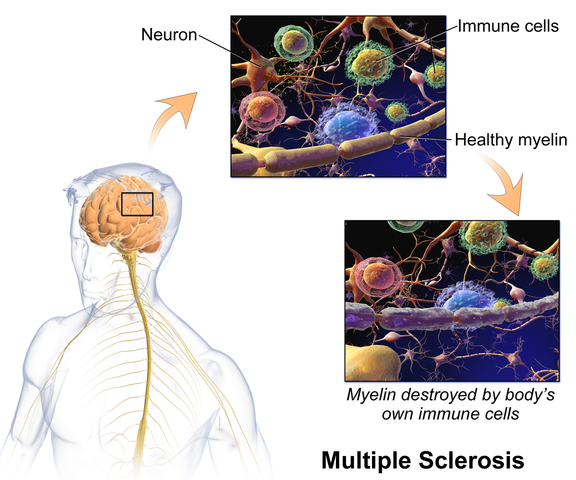
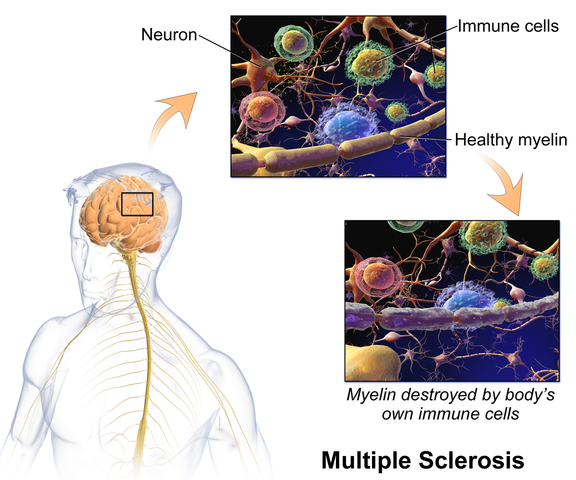
In brain storming our ideas for course creation, much was said about thinking back to college or other continuing education courses and “learning a little about a lot of things neuro” but not the in-depth knowledge one might want to have when focusing their attention on specific neurodegenerative conditions such as Parkinson disease, demyelinating diseases such as Multiple Sclerosis, injury to the brain due to cerebral vascular accident or incomplete or complete spinal cord injury.
As I progress deep into the development of this course, I have my “neuro brain” on and a persistent focus set on providing clinicians with as much in-depth information on neurological contributions to pelvic floor function and dysfunction. I want clinicians to walk away from this course feeling confident that through evaluation of a client that has been diagnosed with Parkinson disease, Multiple Sclerosis or suffered a spinal cord injury, they would have the tools to develop an in-depth treatment plan that would provide these clients with the best results possible to improve their quality of life. I also want clinicians to have the confidence to market themselves to their local neurologists. This is an entirely new avenue for developing a referral base in pelvic health work. Many times for clients who have chronic neurological conditions, the problem list is long and bladder, bowel and sexual health concerns might not even be broached within the very short physician appointment times. We can give our neurologists new treatments to be confident in and excited about to improve their patient’s quality of life!
Sara Chan Reardon, DPT, WCS, BCB-PMD is a pelvic floor dysfunction specialist practicing in New Orleans, LA. Sara was named the 2008 Section on Women’s Health Research Scholar for her published research on pelvic floor dyssynergia related constipation. She was recognized as an Emerging Leader in 2013 by the American Physical Therapy Association. She served as Treasurer of the APTA’s Section on Women's Health and sat on their Executive Board of Directors from 2012-2015. Today she was kind enough to share a bit about her course Post-Prostatectomy Patient Rehabilitation, which is taking place twice in 2018.
 My name is Sara Reardon, and I teach the Post-Prostatectomy Patient Rehabilitation course, which I wrote and developed in the year 2015. At the time, I had been a pelvic health Physical Therapist for over 10 years. Earlier in my career, I had taken the Pelvic Floor 2A course by Herman and Wallace Institute, which was a fantastic and thorough introduction to treating a male patient.
My name is Sara Reardon, and I teach the Post-Prostatectomy Patient Rehabilitation course, which I wrote and developed in the year 2015. At the time, I had been a pelvic health Physical Therapist for over 10 years. Earlier in my career, I had taken the Pelvic Floor 2A course by Herman and Wallace Institute, which was a fantastic and thorough introduction to treating a male patient.
Over the years, I started seeing more and more men with post-prostatectomy urinary incontinence and erectile dysfunction in my clinic. Urinary incontinence is the most common and costly complication in men following prostate removal surgery, and their quality of life is directly related to their duration of experiencing those symptoms. Evidence supports that pelvic floor muscle training started as soon as possible after surgery can help decrease incontinence and improve quality of life. I enjoyed being able to help men decrease their incontinence and improve their other symptoms after all they had been through following a cancer diagnosis and treatment.
No courses focused specifically on treating post-prostatectomy pelvic floor dysfunction were offered at the time, so I scoured the research, shadowed with physicians, observed surgeries, and attended urology conferences to understand how to effectively treat these individuals. Treating this population of men is fun, fulfilling, and rewarding, and I was inspired to help other pelvic health physical therapists dive deeper as I witnessed the impact pelvic health physical therapy can have on the quality of life of these patients. I love teaching this course, and I am excited to help other pelvic health professionals learn evidence based and effective treatment strategies to help these men navigate their recovery after prostatectomy.
Join Dr. Reardon in Philadelphia, PA on June 2-3, 2018 or in Houston, TX on November 10-11, 2018 to learn evaluation and treatment techniques for men recovering from prostatectomy surgery.
In an effort to provide the best possible educational experience for clinical rehabilitation application of neuroanatomy, I was on a mission. Having a core, base knowledge review of the nervous system is essential when leading into talking about dysfunction and disease of that system. I went on a search for anatomical depictions that could clearly identify the structures and processes I was trying to portray. New books from the library and books I own from when I was in college serve as great resources when trying to get back into studying the specifics, but do not offer the opportunity to easily get these images into a powerpoint. Online resources are also challenging. I am learning how time consuming the process can be to determine who owns the online image, if it is free to copy, save and utilize for my own teaching purposes, or if I need to go through the process of requesting permissions for use.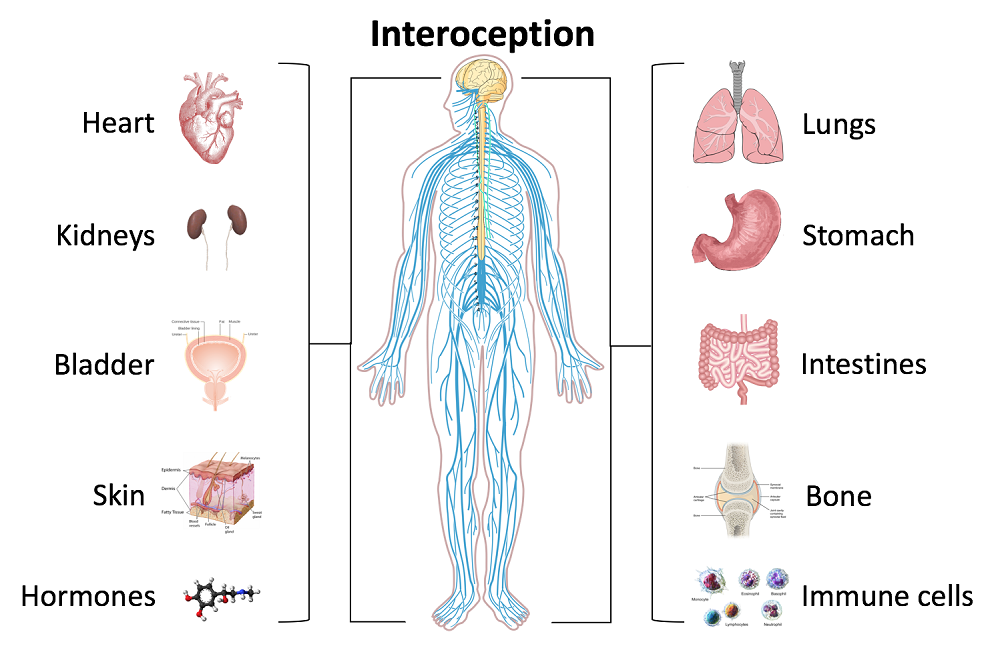
Through my employer, where I treat patients in the clinic, I have access to a program called Primal Pictures. I had used this in the past for clinic related marketing presentations and educational materials for patients and other clinicians I have mentored. Looking into the product further, I came to find out that there is a newer version of the program which offered so many more options. A truly unlimited amount of images which can be manipulated into an optimal position depicting the most clear neuroanatomical views I have ever been able to find. Not only does it provide me with the images I need in order to depict the treacherous pathways of the nerves in our body, but it also provides some amazing depictions of the physiological processes that occur within our nervous system to allow for healthy day to day functioning and protection of our bodies.
I also came across the title of a journal article that I was sure would provide some excellent depictions of neuroanatomy. The article titled, Sectional Neuroanatomy of the Pelvic Floor, provides cross sectional views of both the male and female pelvises. I obtained the article which has an excellent color-coded system, each nerve colored the same as the muscles and skin surface it innervates, going from superior to inferior cross sections. This makes for a clear understanding of each structures anatomical position. It is a great reference when looking at the anatomical relationships to adjacent structures and can help guide palpation skills. The article was more specifically written for physicians to best direct needle procedures/injections in the most accurate location possible when targeting nerves and structures. Neuroanatomy and physiology can be essential to understanding certain patient populations we encounter as we practice pelvic floor rehabilitation. Having clear depictions to refer to can help you provide the best possible base knowledge to your patients as you help them understand the challenges they face and how to overcome them.
Kass, J. S., Chiou-Tan, F. Y., Harrell, J. S., Zhang, H., & Taber, K. H. (2010). Sectional neuroanatomy of the pelvic floor. Journal of computer assisted tomography, 34(3), 473-477.
In 2007, after only speaking on the phone and never meeting in person, my new friend and colleague Stacey Futterman and I presented at the APTA National Conference on the topic of male pelvic pain. It was a 3 hour lecture that Stacey had been asked to give, and she invited me to assist her upon recommendation of one of her dear friends who had heard me lecture. I still recall the frequent glances I made to match the person behind the voice I had heard for so many long phone calls.
 Upon recommendation of Holly Herman, we took this presentation and developed it into a 2 day continuing education course, creating lectures in male anatomy (we definitely did not learn about the epididymis in my graduate training), post-prostatectomy urinary incontinence, pelvic pain, and a bit about sexual health and dysfunction. Although it truly seems like the worst imaginable question, we asked each other “should we allow men to attend?” As strange as this question now seems, it speaks volumes about the world of pelvic health at that time; mostly female instructors taught mostly female participants about mostly female conditions.
Upon recommendation of Holly Herman, we took this presentation and developed it into a 2 day continuing education course, creating lectures in male anatomy (we definitely did not learn about the epididymis in my graduate training), post-prostatectomy urinary incontinence, pelvic pain, and a bit about sexual health and dysfunction. Although it truly seems like the worst imaginable question, we asked each other “should we allow men to attend?” As strange as this question now seems, it speaks volumes about the world of pelvic health at that time; mostly female instructors taught mostly female participants about mostly female conditions.
Make no mistake- women’s health topics were and are deserving of much attention in our typically male-centered world of medicine and research. Maternal health in the US is dreadful, and gone are the days when providers should allow urinary incontinence or painful sexual health to be “normal”, yet it is often described as such to women who are brave enough to ask for help. Times have changed for the better for us all.
The Male Pelvic Floor Course was first taught in 2008, and so far, 22 events have taken place in 18 different cities. 73 men have attended the course to date, with increasing numbers represented at each course. Rather than 20-25 attendees, the Institute is seeing more of the men’s health course filling up with 35-40 participants. In my observations, the men who attend the course are often very experienced, have excellent orthopedic and manual therapy skills, and have personalities that fit very well into the sensitive work that is pelvic rehabilitation.
The course was expanded to include 3 days of lectures and labs, and this expansion allowed more time for hands-on skills in examination and treatment. The schedule still covers bladder, prostate, sexual health and pelvic pain, and further discusses special topics like post-vasectomy syndrome, circumcision, and Peyronie’s disease. In my own clinical practice, learning to address penile injuries has allowed me to provide healing for conditions that are yet to appear in our journals and textbooks. As I often say in the course, we are creating male pelvic rehabilitation in real time.
Because the course often has providers in attendance who have not completed prior pelvic health training, instruction in basic techniques are included. For the experienced therapists, there are multiple lab “tracks” that offer intermediate to advanced skills that can be practiced in addition to the basic skills. Adaptations and models are used when needed to allow for draping, palpation, and education when working with partners in lab, and space is created for those therapists who want to learn genital palpation more thoroughly versus those who are deciding where their comfort zone is at the time. One of the more valuable conversations that we have in the course is how to create comfort and ease in when for most us, we were raised in a culture (and medical training) where palpation of the pelvis was not made comfortable. Hearing from the male participants about their bodies, how they are affected by cultural expectations, adds significant value as well.
We need to continue to create more coursework, more clinical training opportunities so that the representation of those treating male patients improves. If you feel ready to take your training to the next level in caring for male pelvic dysfunction, this year there are three opportunities to study. I hope you will join me in Male Pelvic Floor Function, Dysfunction and Treatment.