My little boy has a t-shirt with a potato telling french fries, “I am your father,” to which the french fries cry, “NO!!!!” The Star Wars spoof makes me laugh, but sometimes the struggle is real. Testicular cancer and the toxic remedies for it can potentially prevent young men from having a successful reproductive life. Survivors of the cancer may one day have to tell their children they are adopted or came from a sperm donor. With the advances in technology and research, however, testicular cancer survivors have a greater chance for their own sperm to be spared or even produced naturally years later to create their offspring.
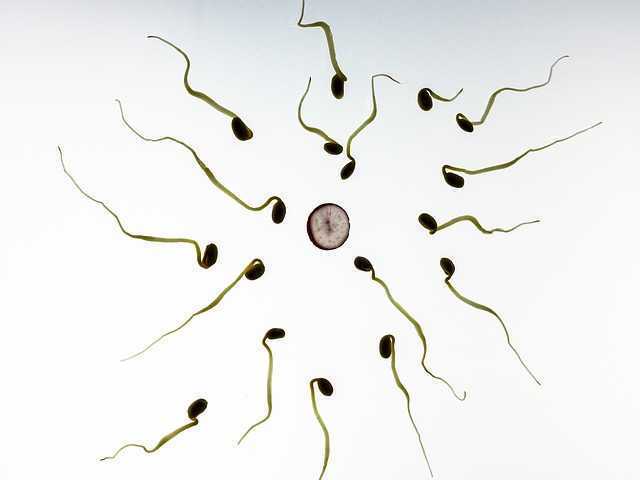 Vakalopoulos et al. (2015) discussed the impact cancer and the related treatments have on fertility of males. Better survival rates for oncology patients have made preservation of reproductive means more imperative for men. Testicular cancer represents 5% of male urologic cancers, disturbing spermatogenesis and impairing fertility. Chemotherapy, radiotherapy, and surgery can all have gonadotoxic effects in men. Thankfully, only 1 in 5000 men die from testicular cancer now with advanced treatments, but fertility does become a long term factor for survivors. This paper showed chemotherapy combined with radiotherapy was most detrimental to sperm than either treatment alone. Gonadal shielding and moving the testes out of the way to target the malignant cells can help decrease the deleterious effects of cancer treatments. Radiotherapy, however, has been shown to damage sperm up to 2 years after recovery of spermatogenesis. Regarding surgery, radical unilateral orchiectomy is the standard for testicular tumors, and within the first few months, a 50% decrease in sperm concentration occurs, and 10% of patients become azoospermic. On a more encouraging note, after receiving Hematopoietic Stem Cell Transplantation, recovery of sperm in the ejaculate was noted in 33% of patients after 1 year and 80% of patients after 7 years.
Vakalopoulos et al. (2015) discussed the impact cancer and the related treatments have on fertility of males. Better survival rates for oncology patients have made preservation of reproductive means more imperative for men. Testicular cancer represents 5% of male urologic cancers, disturbing spermatogenesis and impairing fertility. Chemotherapy, radiotherapy, and surgery can all have gonadotoxic effects in men. Thankfully, only 1 in 5000 men die from testicular cancer now with advanced treatments, but fertility does become a long term factor for survivors. This paper showed chemotherapy combined with radiotherapy was most detrimental to sperm than either treatment alone. Gonadal shielding and moving the testes out of the way to target the malignant cells can help decrease the deleterious effects of cancer treatments. Radiotherapy, however, has been shown to damage sperm up to 2 years after recovery of spermatogenesis. Regarding surgery, radical unilateral orchiectomy is the standard for testicular tumors, and within the first few months, a 50% decrease in sperm concentration occurs, and 10% of patients become azoospermic. On a more encouraging note, after receiving Hematopoietic Stem Cell Transplantation, recovery of sperm in the ejaculate was noted in 33% of patients after 1 year and 80% of patients after 7 years.
Regardless of advancements in decreasing toxicity of cancer treatments and being minimally invasive with surgery, the best guarantee for preservation of sperm is cryopreservation.
A study collecting baseline data for semen quality of cancer patients prior to any gonadotoxic treatment was performed by Auger et al. (2016). Less than 60% of the testicular cancer patients had normal sperm production prior to treatment. The study also looked at patients with Hodgkin’s disease, non-Hodgkin’s Lymphoma, Leukemia, sarcoma, Behcet’s disease, brain tumor, and Multiple Sclerosis. The motility of sperm after freezing (cryopreservation) of the cancer patients was less than half of the healthy sperm donor control group. Intra Cytoplasmic Sperm Injection (ICSI) was shown to provide the best chance of paternity for men, and the authors conclude this as a necessary step in case men do not regain any spermatogenesis after cancer treatment.
There is no perfect circumstance when it comes to cancer. Survival is the primary goal, and then quality of life becomes the “problem,” particularly when it comes to fulfilling dreams of having a family. The toxic cancer treatments are improving but cannot guarantee return of spermatogenesis. Depending on the sperm integrity prior to getting treatment, cryopreservation success can vary but is the most highly recommended step to preserving fertility. In the end, a fresh or frozen spud can still make french fries.
Herman & Wallace has two great courses which can give you the tools needed to help assess and treat male patients who suffer from cancer-related dysfunctions. Consider Oncology and the Male Pelvic Floor: Male Reproductive, Bladder, and Colorectal Cancers or Post-Prostatectomy Patient Rehabilitation for your next continuing education courses.
Vakalopoulos, I., Dimou, P., Anagnostou, I., Zeginiadou T. (2015). Impact of cancer and cancer treatment on male fertility. Hormones. 14(4):579-89. DOI: 10.14310/horm.2002.1620
Auger, J., Sermondade, N., & Eustache, F. (2016). Semen quality of 4480 young cancer and systemic disease patients: baseline data and clinical considerations. Basic and Clinical Andrology, 26, 3. http://doi.org/10.1186/s12610-016-0031-x
My job as a pelvic floor therapist is rewarding and challenging in so many ways. I have to say that one of my favorite "job duties" is differential diagnosis. Some days I feel like a detective, hunting down and piecing together important clues that join like the pieces of a puzzle and reveal the mystery of the root of a particular patient's problem. When I can accurately pinpoint the cause of someone's pain, then I can both offer hope and plan a road to healing.
 Recently a lovely young woman came into my office with the diagnosis of dyspareunia. As you may know dyspareunia means painful penetration and is somewhat akin to getting a script that says "lower back pain." As a therapist you still have to use your skills to determine the cause of the pain and develop an appropriate treatment plan.
Recently a lovely young woman came into my office with the diagnosis of dyspareunia. As you may know dyspareunia means painful penetration and is somewhat akin to getting a script that says "lower back pain." As a therapist you still have to use your skills to determine the cause of the pain and develop an appropriate treatment plan.
My patient relayed that she was 6 months post partum with her first child. She was nursing. Her labor and delivery were unremarkable but she tore a bit during the delivery. She had tried to have intercourse with her husband a few times. It was painful and she thought she needed more time to heal but the pain was not changing. She was a 0 on the Marinoff scare. She was convinced that her scar was restricted. "Oh Goodie," I thought. "I love working with scars!" But I said to her, "Well, we will certainly check your scar mobility but we will also look at the nerves and muscles and skin in that area and test each as a potential pain source, while also completing a musculoskeletal assessment of the rest of you."
Her "external" exam was unremarkable except for adductor and abdominal muscle overactivity. Her internal exam actually revealed excellent scar healing and mobility. There was significant erythemia around the vestibule and a cotton swab test was positive for pain in several areas. There was also significant muscle overactivity in the bulbospongiosis, urethrovaginal sphincter and pubococcygeus muscles. Also her vaginal pH was a 7 (it should normally be a 4, this could indicate low vaginal estrogen). I gave her the diagnosis of provoked vestibulodynia with vaginismus. Her scar was not the problem after all.
Initially for homework she removed all vulvar irritants, talked to her doctor about trying a small amount of vaginal estrogen cream, and worked on awareness of her tendency to clench her abdominal, adductor, and pelvic floor muscles followed by focused relaxation and deep breathing. In the clinic I performed biofeedback for down training, manual therapy to the involved muscles, and instructed her in a dilator program for home. This particular patient did beautifully and her symptoms resolved quite quickly. She sent me a very satisfied email from a weekend holiday with her husband and daughter.
Although this case was fairly straightforward, it is a great example of how differential diagnosis is imperative to deciding and implementing an effective treatment plan for our patients. In Herman & Wallace courses you will gain confidence in your evaluation skills and learn evidence based treatment processes that will enable you to be more confident in your care of both straightforward and complex pelvic pain cases. Hope to see you in class!
We are all familiar with the old saying, “You are what you eat.” A functional medicine lecture I attended recently at the Cleveland Clinic explained how chronic pain can be a result of how the body fails to process the foods we eat. Patients who just don’t seem to get better despite our skilled intervention make us wonder if something systemic is fueling inflammation. Even symptoms of vulvodynia, an idiopathic dysfunction affecting 4-16% of women, have been shown to correlate to diet.
In a single case study of a 28 year old female athlete in Integrative Medicine (Drummond et al., 2016), vulvodynia and irritable bowel syndrome (IBS) were addressed with an elimination diet. After being treated by a pelvic floor specialist for 7 months for vulvodynia, the patient was referred out for a nutrition consultation. Physical therapy was continued during the vegetarian elimination diet. In the patient’s first follow up 2 weeks after starting eliminating meat, dairy, soy, grains, peanuts, corn, sugar/artificial sweeteners, she no longer had vulvodynia. The nutrition specialist had her add specific foods every 2 weeks and watched for symptoms. Soy, goat dairy, and gluten all caused flare ups of her vulvodynia throughout the process. Eliminating those items and supplementing with magnesium, vitamin D3, probiotics, vitamin B12, and omega-3 allowed the patient to be symptom free of both vulvodynia and IBS for 6 months post-treatment.
 On the more scientific end of research, Vicki Ratner published a commentary called “Mast cell activitation syndrome” in 2015. She described how mast cells appear close to blood vessels and nerves, and they release inflammatory mediators when degranulated; however, mast cell activation syndrome (MCAS) involves mast cells that do not get degranulated properly and affect specific organs like the bladder. She proposed measuring the number of mast cells and inflammatory mediators in urine for more expedient diagnosis of interstitial cystisis and bladder pain syndrome.
On the more scientific end of research, Vicki Ratner published a commentary called “Mast cell activitation syndrome” in 2015. She described how mast cells appear close to blood vessels and nerves, and they release inflammatory mediators when degranulated; however, mast cell activation syndrome (MCAS) involves mast cells that do not get degranulated properly and affect specific organs like the bladder. She proposed measuring the number of mast cells and inflammatory mediators in urine for more expedient diagnosis of interstitial cystisis and bladder pain syndrome.
Sigrid Regauer’s correspondence to Ratner’s article followed in 2016 relating MCAS to bladder pain syndrome (BPS), interstitial cystitis (IC), and vulvodynia. He described vulvodynia as a pain syndrome with excessive mast cells and sensory nerve hyperinnervation, often found with BPS and IC. The vulvodynia patients had mast cell hyperplasia, most of which were degranulated, and 70% of the patients had comorbidities due to mast cell activation such as food allergies, histamine intolerance, infections, and fibromyalgia.
Considering the association between mast cells and acute inflammatory responses and how mast cells release proinflammatory mediators, it makes sense that dysfunctions such as vulvodynia as well as IC and BPS can result from an excessive amount and dysfunctional granulation of mast cells. Enhanced activation of mast cells causes histamine release, stimulating peripheral pain neurotransmitters (Fariello & Moldwin 2015). If medication and therapy do not solve a patient’s pain, perhaps eliminating the consumption of inflammatory foods could positively affect the body on a cellular level and relieve irritating symptoms of vulvodynia. Pardon the parody, but patients on the brink of being “insane in the brain” from vulvodynia will likely try anything to resolve being “inflamed in the membrane.”
Drummond, J., Ford, D., Daniel, S., & Meyerink, T. (2016). Vulvodynia and Irritable Bowel Syndrome Treated With an Elimination Diet: A Case Report.Integrative Medicine: A Clinician’s Journal, 15(4), 42–47.
Ratner, V. (2015). Mast cell activation syndrome. Translational Andrology and Urology, 4(5), 587–588. http://doi.org/10.3978/j.issn.2223-4683.2015.09.03
Regauer, S. (2016). Mast cell activation syndrome in pain syndromes bladder pain syndrome/interstitial cystitis and vulvodynia. Translational Andrology and Urology, 5(3), 396–397. http://doi.org/10.21037/tau.2016.03.12
Fariello, J. Y., & Moldwin, R. M. (2015). Similarities between interstitial cystitis/bladder pain syndrome and vulvodynia: implications for patient management. Translational Andrology and Urology, 4(6), 643–652. http://doi.org/10.3978/j.issn.2223-4683.2015.10.09
Help others by helping ourselves
As pelvic rehabilitation practitioners, we have all been there, looking ahead to see what patients are on our schedules and recognizing that several will require immense energy from us… all afternoon! Then we prepare ourselves, hoping we have enough stamina to get through, and do a good job to help meet the needs of these patients. Then we still have to go home, spend time with our families, do chores, run errands, and have endless endurance. This can happen day after day. Naturally, as rehabilitation practitioners, we are helpers and problems solvers. However, this requires that we work in emotionally demanding situations. Often in healthcare, we experience burnout. We endure prolonged stress and/or frustration resulting in exhaustion of physical and/or emotional strength and lack of motivation. Do we have any vitality left for ourselves and our loved ones? How can we help ourselves do a good job with our patients, but to also honor our own needs for our energy?
 How do we as health care practitioners’ prevent burnout?
How do we as health care practitioners’ prevent burnout?
Ever hear of “mindfulness” ... I am being facetious. The last several years we have been hearing a lot about “mindfulness” (behavioral therapy or mindfulness-based stress reduction) and its positive effects in helping patients cope with chronic pain conditions. Mindfulness is defined as “the practice of maintaining a nonjudgmental state of heightened or complete awareness of one's thoughts, emotions, or experiences on a moment-to-moment basis,” according to Merriam-Webster’s Dictionary. One can practice mindfulness in many forms. Examples of mindfulness-based practice include, body scans, progressive relaxation, meditation, or mindful movement. Many of us pelvic rehabilitation providers teach our patients with pelvic pain some form of mindfulness in clinic, at home, or both, to help them holistically manage their pain. Whether it is as simple as diaphragmatic breathing, awareness of toileting schedules/behavior, or actual guided practices for their home exercise program, we are teaching mindfulness behavioral therapy daily.
Why don’t we practice what we preach?
As working professionals, we are stressed, tired, our schedules too full, and we feel pain too, right? Mindfulness behavioral therapy interventions are often used in health care to manage pain, reduce stress, and control anxiety. Isn’t the goal of using such interventions to improve health, wellness, and quality of life? Mindfulness training for healthcare providers can reduce burnout by decreasing emotional exhaustion, depersonalization, and increasing sense of personal accomplishment. Additionally, it can improve mood, empathy for patients, and communication.1 All of these improvements, leads to improved patient satisfaction.
Let’s take what we teach our patients every day and start applying it to ourselves. An informal way to integrate mindfulness is by building it into your day. Such as when washing hands in between patients, or before you walk into the room to greet the patient. However, sometimes we have a need for a tangible strategy to combat stress and the desire to be guided by an expert with this strategy.2 I think one of the easiest ways to begin practicing mindfulness is to try a meditation application (app) on a smart phone or home computer. Meditation is one of the most common or popular ways to practice mindfulness and is often a nice starting point to try meditation for yourself or to suggest to a motivated patient. Many popular guided meditation apps include Headspace, Insight Timer, and Calm, just to name a few. Generally, these guided meditation apps have free versions and paid upgrades. Challenge yourself to complete a 10-minute guided meditation app, daily, for three weeks, and see how you feel. It takes three weeks to make a new habit. Hopefully, guided meditation will be a new habit to help you be present with your patients and improve your awareness and energy. After all, how can we help others heal, if we can’t help ourselves?
To learn more about ways, you as a professional can help yourself or your patients with meditation, consider attending Meditation for Patients and Providers.
1)Krasner, M.S., Epstein, R.M., Beckman, H., Suchman, A.L., Chapman, B., Mooney C.J., et al. (2009). Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA 302(12):1284–93.
2)Willgens, A. M., Craig, S., DeLuca, M., DeSanto, C., Forenza, A., Kenton, T., ... & Yakimec, G. (2016). Physical Therapists' Perceptions of Mindfulness for Stress Reduction: An Exploratory Study. Journal of Physical Therapy Education, 30(2).
Jennafer Vande Vegte, PT, BCB-PMD, PRPC is a H&W faculty member and one of the developers of the advanced Pelvic Floor Capstone course. In this guest post, she reflects on her own clinical and personal experience that informed her work on this advanced course, and her approach with patients.
 Most days I feel like I am on a journey. Some days I make big strides forward, other days I might fall back. But I am always learning, and eventually I hope to grow. I think it is much the same for our patients. And also for ourselves.
Most days I feel like I am on a journey. Some days I make big strides forward, other days I might fall back. But I am always learning, and eventually I hope to grow. I think it is much the same for our patients. And also for ourselves.
My youngest daughter was diagnosed with eczema, allergies (food and others) and asthma at an early age. In my hubris I felt if I could learn all I could about what was going on in her body I could "fix" her. So began a journey that took me outside the realm of traditional medicine into holistic care. I learned so much! My daughter got a lot healthier. The rest of my family got a lot healthier. I got healthier too. And I began to recognize patients in my practice that needed more holistic care. Guess what, they got healthier too.
When she was in first grade she was diagnosed with ADHD. I retraced the steps of my previous journey that had helped her so much with her allergies, eczema and asthma. But ADHD proved to be resistant to diet , supplements, and homeopathy. We visited an OT and got some good suggestions. A family therapist helped us a ton as parents, but I'm not sure how much he helped my daughter. We tried Ritalin to no avail. Energy therapy and essential oils followed before I finally made an appointment with a ADHD child specialist MD. We will see where that step leads. Why
Why am I telling you all this you may ask? Because I realized that my journey with my daughter is very much like our journey walking next to our patients with chronic pain. They/we may try so many things trying to find the "fix" to make their pain go away. As we grow on our own life journeys and experiences and we add quality clinical tools to our toolboxes we very well may be able to help more people experience freedom from pain, improvements in function, and meeting their goals. But there will be always still be those that we feel like we didn't help. Don't despair dear friends. Every person we have come in contact with in the quest to better equip and understand my daughter's mental and physical health has been a wealth of information, inspiration, and resources. Some things I learned some years ago (essential oils for example) and only now am putting into practice. I wasn't ready before but I am now! I realized that there is a similar dynamic for our patients. We may help them take just one step forward. We may walk a whole journey to healing beside them, or we may never know what the impact of our treatment had on them. But in the end we both end up exactly where we needed to be.
Insignia Health developed the PAM (Patient Activation Measure) Survey (http://www.insigniahealth.com/products/pam-survey) to help heath care providers determine where along the pathway of activation of self care a patient falls. What is interesting about the tool is that a single point increase correlates to a 2% decrease in hospitalization and a 2% increase in medication adherence. The science behind the PAM shows that helping our patients to move forward just one step can have a profound influence on their health. The trick is meeting them where they are at.
Pelvic Floor Capstone was a joy to develop with Nari Clemons and Allison Arial. Our goal was to equip you to take one more step in your learning journey in pelvic health. We delve into intense topics like endocrine disorders, pelvic surgery, gynecological cancer, nutrition and pharmacology. Labs are focused on evaluating and treating myofascial restrictions utilizing a gentle, indirect three dimensional system that invites the brain to reconnect with connective tissue in a safe way for powerful change. We would love to see you at Capstone and hear your stories later on how our time together empowered you to help your patients take one more step.
When I bring up the topic of pelvic floor dysfunction in athletes, stress urinary incontinence (SUI) is usually the first aspect of pelvic health that springs to mind – and rightly so, as professional sport is one of the risk factors for stress urinary incontinence Poswiata et al 2014. The majority of studies show that the average prevalence of urinary incontinence across all sports is 50%, with SUI being the most common lower urinary tract symptom. Athletes are constantly subject to repeated sudden & considerable rises in intra-abdominal pressure: e.g. heel striking, jumping, landing, dismounting and racquet loading.
What’s less often discussed is the topic of gastrointestinal dysfunction in athletes. Anal incontinence in athletes is not well documented, although a study from Vitton et al in 2011 found a higher prevalence than in age matched controls (conversely a study by Bo & Braekken in 2007 found no incidence). More recently, Nygaard reported earlier this year (2016) that young women participating in high-intensity activity are more likely to report anal incontinence than less active women.
A presentation by Colleen Fitzgerald, MD at the American Urogynecologic Society meeting in 2014 highlighted the multifaceted nature of pelvic floor dysfunction in female athletes, specifically in this case, triathletes. The study found that one in three female triathletes suffers from a pelvic floor disorder such as urinary incontinence, bowel incontinence and pelvic organ prolapse. One in four had one component of the "female athlete triad", a condition characterized by decreased energy, menstrual irregularities and abnormal bone density from excessive exercise and inadequate nutrition. Researchers surveyed 311 women for this study with a median age range of 35 – 44. These women were involved with triathlete groups and most (82 percent) were training for a triathlon at the time of the survey. On average, survey participants ran 3.7 days a week, biked 2.9 days a week and swam 2.4 days a week.
Of those who reported pelvic floor disorder symptoms, 16% had urgency urinary incontinence, 37.4% had stress urinary incontinence, 28% had bowel incontinence and 5% had pelvic organ prolapse. Training mileage and intensity were not associated with pelvic floor disorder symptoms. 22% of those surveyed screened positive for disordered eating, 24% had menstrual irregularities and 29% demonstrated abnormal bone strength. With direct access becoming a reality for many of us, we must acknowledge the need for specific questioning when it comes to pelvic health issues, as well as the ability to recognise signs and symptoms of the female athlete triad in our patients.
Want to learn more about pelvic health for athletes? Join me in beautiful Arlington this November 5-6 at The Athlete and the Pelvic Floor!
J Hum Kinet. 2014 Dec 9; 44: 91–96 Published online 2014 Dec 30. doi:10.2478/hukin-2014-0114 PMCID: PMC4327384. Prevalence of Stress Urinary Incontinence in Elite Female Endurance Athlete Anna Poświata, Teresa Socha and Józef Opara1
J Womens Health (Larchmt). 2011 May;20(5):757-63. doi: 10.1089/jwh.2010.2454. Epub 2011 Apr 18. Impact of high-level sport practice on anal incontinence in a healthy young female population. Vitton V, Baumstarck-Barrau K, Brardjanian S, Caballe I, Bouvier M, Grimaud JC.
Am J Obstet Gynecol. 2016 Feb;214(2):164-71. doi: 10.1016/j.ajog.2015.08.067. Epub 2015 Sep 6. Physical activity and the pelvic floor. Nygaard IE, Shaw JM.
Our understanding of treating pelvic pain keeps growing as a profession. We have so many manual therapies such as visceral manipulation, strain counter strain, and positional release adding dimension to our treatment strategies for shortened and painful tissues. Pharmacologic interventions such as botox, valium, and antidepressants are becoming more popular and researched in the literature. We are beginning to work more collaboratively with vulvar dermatologists, urogynecologists, OB’s, family practitioners, urologists, and pain specialists.
 Pelvic rehab providers are in a unique position of being able to offer more time with each patient and to see our patients for several visits. Frequently we are the ones being told stories about how a particular condition is really affecting our patient’s life and the emotional struggles around that. We are often the one who gets a clear picture of our patient’s emotional and mental disposition. A rehab provider may realize that a patient seems to exhibit mental patterns in their treatment. It can be anxiety from how the condition is changing their life, difficulty relaxing into a treatment, poor or shallow breathing patterns, frequently telling themselves they will never get better, or being able to perceive their body only as a source of pain or suffering, losing the subtlety of the other sensations within the body. Yet, aside from contacting a physician, who may offer a medication with side effects, or referring to a counselor or psychologist, our options and training may be limited. Patients may be resistant to seeing a mental health counselor, and we have to be careful to stay in our scope.
Pelvic rehab providers are in a unique position of being able to offer more time with each patient and to see our patients for several visits. Frequently we are the ones being told stories about how a particular condition is really affecting our patient’s life and the emotional struggles around that. We are often the one who gets a clear picture of our patient’s emotional and mental disposition. A rehab provider may realize that a patient seems to exhibit mental patterns in their treatment. It can be anxiety from how the condition is changing their life, difficulty relaxing into a treatment, poor or shallow breathing patterns, frequently telling themselves they will never get better, or being able to perceive their body only as a source of pain or suffering, losing the subtlety of the other sensations within the body. Yet, aside from contacting a physician, who may offer a medication with side effects, or referring to a counselor or psychologist, our options and training may be limited. Patients may be resistant to seeing a mental health counselor, and we have to be careful to stay in our scope.
Research is showing us that meditation as an intervention can be very helpful in addressing these chronic pain issues.
In a study in the Journal of Reproductive Medicine, 22 women with chronic pelvic pain were enrolled in an 8 week mindfulness meditation course. Twelve out of 22 enrolled subjects completed the program and had significant improvement in daily maximum pain scores, physical function, mental health, and social function. The mindfulness scores improved significantly in all measures (p < 0.01).
The questions have arisen, if meditation alters opiod pathways, how can it be administered safely with prescription medications. However in a 2016 study in the journal of neuroscience, it was concluded that meditation-based pain relief does not require endogenous opioids.” Therefore, the treatment of chronic pain may be more effective with meditation due to a lack of cross-tolerance with opiate-based medications.” “The risks of chronic therapy are significant and may outweigh any potential benefits”, according the the journal of American Family Medicine. Meditation training can be a tool to help our patients manage their pain without risk of long term opiod use.
In the two day course, Meditation for Patients and Providers, participants will learn several different meditation and mindfulness techniques they can use for patients with different dispositions, and to tailor the most appropriate approach to specific patients. The aim of the course is to be able to work meditation into a treatment and a home program that is best suited for your patient. The course also covers self care, preventing provider burn out and ways to be more mentally quiet as a provider seeking to give optimal care with appropriate boundaries.
Fox, S. D., Flynn, E., & Allen, R. H. (2010). Mindfulness meditation for women with chronic pelvic pain: a pilot study. The Journal of reproductive medicine, 56(3-4), 158-162.
LEMBKE, A., HUMPHREYS, K., & NEWMARK, J. (2016). Weighing the Risks and Benefits of Chronic Opioid Therapy. American Family Physician,93(12).
Zeidan, F., Adler-Neal, A. L., Wells, R. E., Stagnaro, E., May, L. M., Eisenach, J. C., ... & Coghill, R. C. (2016). Mindfulness-Meditation-Based Pain Relief Is Not Mediated by Endogenous Opioids. The Journal of Neuroscience, 36(11), 3391-3397.
Urinary incontinence (UI) can be problematic for both men and women, however, is more prevalent in women. Incontinence can contribute to poor quality of life for multiple reasons including psychological distress from stigma, isolation, and failure to seek treatment. Patients enduring incontinence often have chronic fear of leakage in public and anxiety about their condition. There are two main types of urinary leakage, stress urinary incontinence (SUI) and urge urinary incontinence (UUI).

SUI is involuntary loss of urine with physical exertion such as coughing, sneezing, and laughing. UUI is a form of incontinence in which there is a sudden and strong need to urinate, and leakage occurs, commonly referred to as “overactive bladder”. Currently, SUI is treated effectively with physical therapy and/or surgery. Due to underlying etiology, UUI however, can be more difficult to treat than SUI. Often, physical therapy consisting of pelvic floor muscle training can help, however, women with UUI may require behavioral retraining and techniques to relax and suppress bladder urgency symptoms. Commonly, UUI is treated with medication. Unfortunately, medications can have multiple adverse effects and tend to have decreasing efficacy over time. Therefore, there is a need for additional modes of treatment for patients suffering from UUI other than mainstream medications.
An interesting article published in The Journal of Alternative and Complimentary Medicine reviews the potential benefits of yoga to improve the quality of life in women with UUI. The article details proposed concepts to support yoga as a biobehavioral approach for self-management and stress reduction for patients suffering with UUI. The article proposes that inflammation contributes to UUI symptoms and that yoga can help to reduce inflammation.
Surfacing evidence indicates that inflammation localized to the bladder, as well as low-grade systemic inflammation, can contribute to symptoms of UUI. Research shows that women with UUI have higher levels of serum C-reactive protein (a marker of inflammation), as well as increased levels of inflammatory biomarkers (such as interleukin-6). Additionally, when compared to asymptomatic women and women with urgency without incontinence, patients with UUI have low-grade systemic inflammation. It is hypothesized that the inflammation sensitizes bladder afferent nerves through recruitment of lower threshold and typically silent C fiber afferents (instead of normally recruited, higher threshold A-delta fibers, that respond to stretch of the bladder wall and mediate bladder fullness and normal micturition reflexes). Therefore, reducing activation threshold for bladder sensory afferents and a lower volume threshold for voiding, leading to the UUI.
How can yoga help?
Yoga can reduce levels of inflammatory mediators. According to the article, recent research has shown that yoga can reduce inflammatory biomarkers (such as interleukin -6) and C-reactive protein. Decreasing inflammatory mediators within the bladder may reduce sensitivity of C fiber afferents and restore a more normalized bladder sensory nerve threshold.
Studies suggest that women with UUI have an imbalance of their autonomic nervous system. The posture, breathing, and meditation completed with yoga practice may improve autonomic nervous system balance by reducing sympathetic activity (“fight or flight”) and increasing parasympathetic activity (“rest and digest”).
The discussed article highlights yoga as a logical, self-management treatment option for women with UUI symptoms. Yoga can help to manage inflammatory symptoms that directly contribute to UUI by reducing inflammation and restoring autonomic nervous system balance. Additionally, regular yoga practice can improve general well-being, breathing patterns, and positive thinking, which can reduce overall stress. Yoga provides general physical exercise that improves muscle tone, flexibility, and proprioception. Yoga can also help improve pelvic floor muscle coordination and strength which can be helpful for UUI. Yoga seems to provide many benefits that could be helpful for a patient with UUI.
In summary, UI remains a common medical problem, in particular, in women. While SUI is effectively treated with both conservative physical therapy and surgery, long-term prescribed medication remains the treatment modality of choice for UUI. However, increasing evidence, including that described in this article, suggests that alternative conservative approaches, such as yoga and exercise, may serve as a valuable adjunct to traditional medical therapy.
Tenfelde, S., & Janusek, L. W. (2014). Yoga: a biobehavioral approach to reduce symptom distress in women with urge urinary incontinence. The Journal of Alternative and Complementary Medicine, 20(10), 737-742.
A diagnosis of breast cancer means many different things to many different people. Regardless, receiving this diagnosis means some sort of treatment will likely follow. The types of treatment and outcomes are largely dependent on individual patient scenarios, however, one thing is for certain: A patient’s life will be forever changed after having received this diagnosis.
Historically, comprehensive care for a patient with breast cancer has focused on treatment and prevention. However, more and more women are surviving breast cancer every year. Therefore, more attention needs to be paid to survivorship. Once someone has survived cancer, comprehensive, quality care should obviously focus on preventing recurrence, however, it may also include guidance and counseling on maintaining a healthy lifestyle and addressing physical and psychosocial changes.
 A very recent 2016 article published in the Annals of Surgical Oncology discusses the subject of survivorship in breast cancer patients. This article suggests that the key to achieving successful outcomes for management of a breast cancer survivor is a multidisciplinary approach to help these survivors deal with the physical and psychosocial sequela resulting from their diagnosis.
A very recent 2016 article published in the Annals of Surgical Oncology discusses the subject of survivorship in breast cancer patients. This article suggests that the key to achieving successful outcomes for management of a breast cancer survivor is a multidisciplinary approach to help these survivors deal with the physical and psychosocial sequela resulting from their diagnosis.
As a pelvic rehabilitation provider, this is a very thought-provoking article as it outlines several areas in which I feel breast cancer survivors could benefit from physical therapy. A pelvic rehabilitation provider can be a valuable part of the multidisciplinary team that helps manage a breast cancer survivor towards positive and meaningful outcomes, ultimately enhancing their quality of life. The following are some areas addressed in the article in which a breast cancer survivor may need assistance to improve and support a meaningful quality of life.
Sexuality: According to this article, studies show treatment for breast cancer is associated with significant decrease in sexual interest, desire, arousal, and difficulty achieving orgasm and/or lack of sexual pleasure. Additionally, patients can also report pain with intercourse (dyspareunia) and/or vaginal dryness, which can lead to sexual dysfunction. Physical therapy can help by providing education on normal sexual response and lubricants, as well as help with tissue healing. Therapeutic techniques include exercise and manual treatments to areas that may be damaged from surgery, radiation, and chemotherapy. Additionally, exercise has been shown to improve self-image. Poor body image has been linked to sexual dysfunction following breast surgery (depending on the type “breast sparing techniques” versus mastectomy). This includes only some of the ways a physical therapist can help improve sexual dysfunction.
Lymphedema: According to the article, 30-70% of breast cancer patients experience lymphedema after treatment. Physical therapy can play an important role in the control and/or reduction of lymphedema. A physical therapist can provide helpful education, exercise, weight control, and, if needed, manual techniques and compression garments and bandaging.
Teachable moments after cancer diagnosis: A teachable moment is when you identify and seize an opportunity to educate your patient. After a life altering event or illness, people are more accepting of advice and change of lifestyle. As healthcare providers, we can utilize this time to help our patients improve outcomes by modifying their behavior. The cited article states there is clear evidence that physical activity decreases incidence and recurrence.There is additional evidence to show controlling weight and maintaining a normal body mass index (BMI) improves breast cancer survivor outcomes. A physical therapist can help a breast cancer survivor to develop a guided and progressive home exercise program to help them maintain normal BMI and participate in regular physical activity safely and regularly.
The discussed article, “Breast Cancer Survivorship: Why, What and When?”, sheds light on many areas of physical and psychosocial challenges that patients surviving breast cancer may deal with. This article also advocates that a multidisciplinary approach yields the greatest outcomes. I suggest that physical therapy can be a valuable part of the team when creating patient care plans for breast cancer survivors.
To learn more about breast cancer and outcomes based treatments, consider attending "Physical Therapy Treatment for the Breast Oncology Patient! The next course is taking place in Stockton, CA this September 24-25.
Gass, J., Dupree, B., Pruthi, S., Radford, D., Wapnir, I., Antoszewska, R., ... & Johnson, N. (2016). Breast Cancer Survivorship: Why, What and When?. Annals of Surgical Oncology, 1-6.
In the 16th century, a theory called Preformationism claimed that sperm contained a preformed, exceedingly minute body referred to as a homunculus, which eventually became a person. This idea of a tiny man had staying power, as today the homunculus is a “body map” based on how much of the cerebral cortex is devoted to sensing each part of the body. Although the idea of a 16th alchemist placing little bodies into a flask conjures a variety of tantalizing images, our program focuses on the mundane, contemporary version of the homunculus. So…what does this have to do with a course that addresses pelvic floor dysfunction? Everything.
 Emerging evidence indicates that therapies that include work to enhance body awareness/kinesthetic sense are potent and effective. Our professional training unfortunately, tends to over-emphasize a structural approach. The good news is that manual therapy, to some degree, enhances a client’s body awareness; but when we have more “tools” to capitalize on this synergy between manual therapy and improved body awareness, we have a potent “elixir” to promote change. To quote Deane Juhan, “touching hands are not like pharmaceuticals or scalpels…they are like flashlights in a darkened room.” By using the “flashlight”, we not only contribute to structural change, but neurological change – meaning the more we pay attention to a particular part of our body, the more “real estate” the brain devotes to that part of the body. Increasing the pelvic floor’s “footprint” on the brain can enhance function of the pelvic floor dramatically and quickly. Therefore, rehabilitation to address pelvic floor dysfunction benefits from weaving orthopedic, neurologic and mindfulness practices together.
Emerging evidence indicates that therapies that include work to enhance body awareness/kinesthetic sense are potent and effective. Our professional training unfortunately, tends to over-emphasize a structural approach. The good news is that manual therapy, to some degree, enhances a client’s body awareness; but when we have more “tools” to capitalize on this synergy between manual therapy and improved body awareness, we have a potent “elixir” to promote change. To quote Deane Juhan, “touching hands are not like pharmaceuticals or scalpels…they are like flashlights in a darkened room.” By using the “flashlight”, we not only contribute to structural change, but neurological change – meaning the more we pay attention to a particular part of our body, the more “real estate” the brain devotes to that part of the body. Increasing the pelvic floor’s “footprint” on the brain can enhance function of the pelvic floor dramatically and quickly. Therefore, rehabilitation to address pelvic floor dysfunction benefits from weaving orthopedic, neurologic and mindfulness practices together.
This program is designed to add a new dimension for the skilled pelvic floor practitioner and to also serve practitioners new to this area of practice. There is no internal manual work; rather we draw from our deep knowledge of Yoga, Tai Chi, along with other Chinese internal martial arts (that put lots of emphasis on the pelvic floor for performance) and Feldenkrais to address pelvic floor dysfunction. Some lessons focus directly on the pelvic region and others on integrating the pelvic floor with full body movement. Ultimately, our goal is to help you connect the dots between structural, functional movement and mindfulness practices, as this powerful triad offers practitioners a comprehensive, approach for treating pelvic floor dysfunction.
We hope you’ll come join in New York City on September 18th & 19th. If you do, wear comfortable clothes as the workshop is designed to provide participants opportunities to embody the work…emphasis is placed on labs more than lecture.
Don’t hesitate to contact us if you have any questions.
Bill@EastWestRehab.com
SabelNYC@Aol.com
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/








































